Abstract
Leiomyosarcoma (LMS) accounts for approximately 7% of all soft tissue sarcomas and occurs most frequently in the gastrointestinal tract and uterus. In the head and neck, however, LMS makes up only 2.3%. LMS of the nasal cavity and Para nasal sinuses are very rare and only about 20 cases of LMS of the nose and Para nasal sinuses have been reported in the literature. Initially, LMS should be treated by extensive surgical excision, long-term follow-up is essential due to the high rate of local recurrence. Radiotherapy and chemotherapy are insufficient therapeutic approaches. Frequency of recurrence and prognosis depend on the tumor site.
Keywords: Leiomyosarcoma, Inferior turbinate, Nasal obstruction, Headache, Epistaxis
Case Report
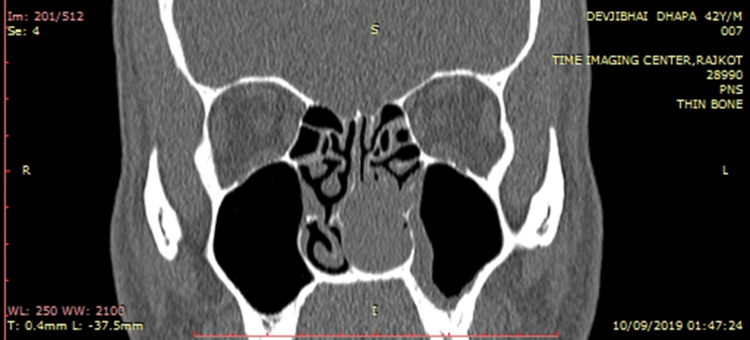
We report a case of Leiomyosarcoma of Lt nasal inferior turbinate. 42 years old male patient presented with complaint of left side nasal obstruction headache and occasional bleeding from left nostril since 4 months. Radiological investigation CT Scan Para nasal sinus showing mass lesion involving left nasal cavity and arising from inferior turbinate leading to destruction of turbinate.
In-office nasal endoscopy examination revealed Lt side nasal mass arising from Lt inferior turbinate and occupying whole nasal cavity. The decision was taken to proceed for left side endoscopic removal of nasal mass under general anesthesia. Complete wide excision of nasal mass done. Tissue sent for histopathological examination and immuno histochemistry study result revels Leiomyosarcoma of inferior turbinate.
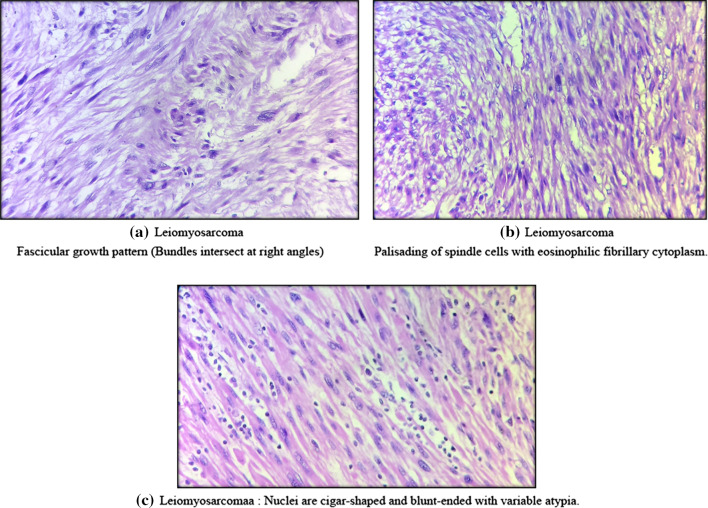
Histopathologic examination and high-power H&E-stained microscopy demonstrated (Fig. 1a) Fascicular growth pattern (Bundles intersect at right angles (Fig. 1b) demonstrate Palisading of spindle cells with eosinophilic fibrillary cytoplasm. Figure 1c demonstrate Nuclei are cigar-shaped and blunt-ended with variable atypia (Fig. 2). CT Scan paranasal sinus showing soft tissue mass lesion involving left nasal cavity with destruction of inferior turbinate.
Fig. 1.
Leiomyosarcoma: a fascicular growth pattern (bundles intersect at right angles), b palisading of spindle cells with eosinophilic fibrillary cytoplasm, c nuclei are cigar-shaped and blunt-ended with variable atypia
Fig. 2.
Soft tissue mass lesion involving left nasal cavity with erosion of left inferior turbinate
A diagnosis of leiomyosarcoma of the left inferior nasal turbinate was made. Subsequent PET and CT scans were negative for distal and local malignancies.
Discussion
Dobben et al. reported the first case of LMS arising from the nasopharynx in 1958, and since that time fewer than 20 cases have been reported worldwide Across reports thus far, the mean age of onset is 53, with a slight male predominance of 1.1:1. Similar to other Sino nasal malignancies, the most common presenting symptoms are nasal obstruction, epistaxis, pain, local swelling, and rhinorrhea.
Leiomyosarcoma usually begins as a rapidly growing painless tumor grossly lesions are smooth, firm and discretely circumscribed. In our case tumor originates from left side inferior turbinate that itself is rare entity and leading to destruction of inferior turbinate.
PET scan should be done to rule out distant metastasis here in our case PET scan is suggestive of no distant metastasis.
The rarity at which LMS presents in the Sino nasal cavity is likely attributed to the paucity of smooth muscle in this region. Some suggest that the cells of origin are found in the tunica media of blood vessel walls, while others have suggested the tumor arises from undifferentiated mesenchymal tissue or even myoepithelial cells in sub mucosal glands.
H&E staining of LMS shows intersecting fascicles of malignant spindle cells with cigar-shaped or atypically lobulated nuclei; however, LMS can be difficult to distinguish from other soft tissue sarcomas by light microscopy alone. Differential diagnoses include fibrosarcoma, rhabdomyosarcoma, malignant schwannoma and benign spindle-cell tumors. To differentiate between these various tumors, IHC staining methods are often necessary. As was used in our case, IHC staining with antibodies to smooth muscle actin and desmin as well as vimentin as a marker for mesenchymal tissue are useful in demonstrating LMS as the diagnosis.
The prognosis of Sino nasal leiomyosarcomas is poor. Although there is a case report that etoposide and high-dose ifosfamide caused significant tumor shrinkage, chemotherapy and radiation therapy are generally considered to be ineffective in the management of Sino nasal tract leiomyosarcomas. Wide surgical excision is the treatment of choice because the tumor is characterized as locally aggressive rather than as having high metastatic potential. Precise identification of the extent of tumor involvement and subsequent complete surgical resection are essential.
Conclusion
Sino nasal leiomyosarcoma is a rare entity. When encountered, wide surgical excision should be considered the primary treatment modality, with reservation of chemotherapy for advanced disease and metastasis.
Funding
No funding has been taken from any sources.
Compliance with Ethical Standards
Conflict of interest
None.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Huang HY, Antonescu CR. Sino nasal smooth muscle cell tumors: a clinicopathologic and immunohistochemical analysis of 12 cases with emphasis on thelow-gradeendofthespectrum. Arch Pathol Lab Med. 2003;127:297–304. doi: 10.5858/2003-127-0297-SSMCT. [DOI] [PubMed] [Google Scholar]
- 2.Fusconi M, Magliulo G, Della Rocca C, et al. Leiomyosarcoma of the sinonasal tract: a case report and literature review. Am J Otolaryngol. 2002;23:108–111. doi: 10.1053/ajot.2002.30628. [DOI] [PubMed] [Google Scholar]
- 3.Vogl TJ, Mack MG, Juergens M, et al. MR diagnosis of head and neck tumors: comparison of contrast enhancement with triple-dose gadodiamide and standard-dose gadopentetated imeglumine in the same patients. AJR Am J Roentgenol. 1994;163:425–432. doi: 10.2214/ajr.163.2.8037044. [DOI] [PubMed] [Google Scholar]
- 4.Fu YS, Perzin KH. Nonepithelial tumors of the nasal cavity, paranasal sinuses, and nasopharynx: a clinicopathologic study. IV. Smooth muscle tumors (leiomyoma, leiomyosarcoma) Cancer. 1975;35:1300–1308. doi: 10.1002/1097-0142(197505)35:5<1300::AID-CNCR2820350508>3.0.CO;2-Z. [DOI] [PubMed] [Google Scholar]
- 5.Pimpinella RJ, Marquit B. Leiomyosarcoma of nose, nasopharynx and paranasal sinuses. Ann Otol Rhinol Laryngol. 1965;74:623–630. doi: 10.1177/000348946507400304. [DOI] [PubMed] [Google Scholar]
- 6.Dobben GD. Leiomyosarcoma of the nasopharynx. AMA Arch Otolaryngol. 1958;68:211–213. doi: 10.1001/archotol.1958.00730020219013. [DOI] [PubMed] [Google Scholar]
- 7.Lippert BM, Godbersen GS, Luttges J, et al. Leiomyosarcoma of the nasal cavity: case report and literature review. ORL J Otorhinolaryngol Relat Spec. 1996;58:115–120. doi: 10.1159/000276810. [DOI] [PubMed] [Google Scholar]
- 8.Ulrich CT, Feiz-Erfan I, Spetzler RF, et al. Sinonasal leiomyosarcoma: review of literature and case report. Laryngoscope. 2005;115:2242–2248. doi: 10.1097/01.mlg.0000183767.97518.09. [DOI] [PubMed] [Google Scholar]
- 9.Kuruvilla A, Wenig BM, Humphrey DM, et al. Leiomyosarcoma of the sinonasal tract: a clinicopathologic study of nine cases. Arch Otolaryngol Head Neck Surg. 1990;116:1278–1286. doi: 10.1001/archotol.1990.01870110050005. [DOI] [PubMed] [Google Scholar]