Abstract
Introduction
Some concepts of radiation protection are not well understood and must be refreshed periodically. The basic knowledge that a vascular surgeon must have about radiation protection for patients and staff is summarised.
Report
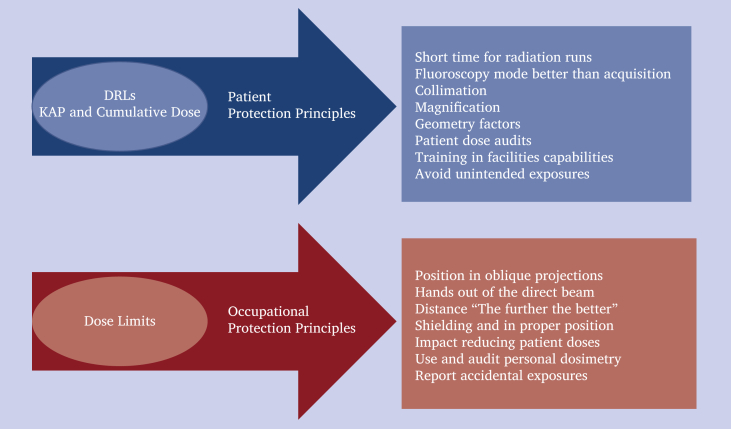
Diagnostic reference levels are a form of investigation into the medical exposure of patients during diagnostic and endovascular procedures that help to optimise them. Radiological quantities such as dose area product, also known as kerma area product and cumulative dose, are the most relevant to the patient. Equivalent dose, in mSv, determines the dose limits for staff. The effective dose (related to absorbed dose), also in mSv, represents the global risk of cancer and hereditary effects. For patient protection, the most important factors are fluoroscopy time, collimation, magnification, keeping the patient as near as possible to the image detector and as far as possible away from the tube, and trying to work in fluoroscope mode. Regarding occupational protection, distance, shielding, and dosimetry are the most important.
Discussion
With the increased use of endovascular procedures, radiation protection is an issue that has grown in importance. Radiation protection is based on three principles: justification; optimisation; and dose limits. Every action focused on reducing a patient's radiation dose will also reduce the dose to staff. Basic principles such as “the further away the better”, “always use a lead apron, thyroid protector, and lead glasses”, and “do not forget to wear personal dosimeters” must be remembered at all times.
Keywords: Diagnostic reference level, Distance shielding time, Dosimetry, Occupational radiation protection, Patient radiation protection, Radiation dose
Highlights
-
•
Radiation protection focuses on healthcare staff and patients.
-
•
Diagnostic reference levels are essential in standard procedures.
-
•
Operators should know their personal dose and radiation limits.
-
•
Time, distance, and shielding are important.
Introduction
The International Commission on Radiological Protection recommends a global approach to the optimisation strategies for interventional procedures.1 The European regulation and the International Atomic Energy Agency2, 3, 4 recommend periodic radiological protection training programmes to refresh knowledge and clarify concepts. This paper summarises the basic knowledge that a vascular surgeon should have about radiation protection for patients and staff.
Report
Diagnostic reference levels
A diagnostic reference level (DRL)5 is a form of investigation of the medical exposure to patients of radiation during diagnostic and endovascular procedures. A DRL is used to indicate whether, under routine conditions, the amount of radiation used for a specified procedure is unusually high or low for that procedure, comparing the radiation doses of procedures that have established DRLs already. The European regulation2 requires the establishment, regular review, and use of DRLs for interventional radiology and endovascular procedures. If these levels are consistently exceeded, appropriate corrective action should be taken without undue delay.
DRLs are set at the 75th percentile of the distribution of the medians of distributions of the patient dose values observed at a number of healthcare facilities (“local DRL value”) or multiple facilities throughout a country (“national DRL value”).5 Establishing DRLs involves the collection of data from several, or single, procedures, which are then conveyed to the health authorities.6,7
The application of the DRL process is not sufficient. Optimisation is generally concerned with maintaining the quality of the diagnostic information provided by the examination commensurate with the medical purpose. In some cases, optimisation may result in an increase in patient dose. DRLs are not “limits” and do not apply to individual patients. They are established for groups of patients and for specific clinical tasks or clinical indications.5
Radiological quantities
Patient doses during interventional procedures are usually measured as “dose area product” (DAP; also named kerma area product [KAP]) in Gy.cm2.8 KAP indicates the radiation produced by the Xray system and the irradiated area during the radiological procedure. A second dosimetric quantity, called “cumulative dose” (or cumulative air kerma), measured in mGy, is also reported for these procedures. This is measured at the patient entrance reference point. Some new Xray systems offer skin dose maps or “peak skin dose” during procedures.
For occupational protection doses are usually measured as “personal dose equivalent” (Hp[10]), which is the dose equivalent in soft tissue at a depth of 10 mm on the human body. mSv is the unit used to measure different radiation quantities as “organ doses” (e.g., the lens of the eyes) and the “effective dose”. The dose limit for lenses are 20 mSv per year average over five years, or 50 mSv in a single year. For skin, 500 mSv per year.4
The “effective dose” is used to estimate the global risk of the person exposed to ionising radiation and accounts for the doses in different tissues and the radiosensitivity of that tissue. This quantity can be related to the increases of the probability of cancer and hereditary effects. Currently, the limit is 20 mSv per year average over five years, or 50 mSv in a single year.4
Patient protection
Some surgeons are mainly concerned about self protection.3 Their rationale is that patients undergo radiation exposure for their benefit and are only exposed to radiation for medical purposes a few times in their life (this is changing drastically). In general, every action to reduce the patient's dose will also reduce the occupational dose, but the reverse is not true. For one unit of radiation that a staff receives, the patient may receive it up to a thousand fold.
Time
Use short fluoroscopy runs and low fluoroscopy modes when possible (for most endovascular procedures no more than 7.5 pulses per second (pps), or even 3 pps for ordinary manoeuvres, is adequate). Mind the foot on the switch and do not make the length of the series unnecessarily long.
Digital subtraction angiography and cone beam computed tomography
Digital subtraction angiography (DSA) and cone beam computed tomography imaging require higher patient doses than fluoroscopy. Consider the use of DSA only for recording and think twice about whether it is really needed. Image acquisition is usually no more than 2–3 frames per second. However, in most of the new Xray systems, it is possible to archive fluoroscopy images.
Collimate
Collimate the radiation field to the area of interest. This reduces the radiation dose and improve the image quality. This is a simple and effective action in reduction of radiation dose and getting better images. Most current devices allow setting the collimation without radiation using Last Image Hold (LIH) as a reference.
Magnification
Magnification is a very useful tool for obtaining details and accuracy of, for example, visceral arteries, tibial vessels, contralateral limb capture, and stents. However, it may increase the entrance dose. Remove magnification when it is not needed. Try using the digital zoom.
Set up
Maintain the flat panel detector or image intensifier close to the patient, and the Xray tube far from the patient (but try to maintain the volume of interest at the isocentre of the imaging system).
Training
Providing training on the capabilities of the facility is essential for taking advantage of all features of the equipment, such as fusion image, fade, mask, and LIH. Image quality can be enhanced without radiation with the application of various image processing techniques.
Audit
Perform periodic audits of patient dose values and compare the median values with the national or local DRLs.
Accidental/unintended exposure
Identify accidental, or unintended, exposures and produce the appropriate reports (as required by the European regulations).2 Implement corrective actions when appropriate.
Occupational protection
Projection
If you use oblique projections (especially lateral projections), the riskiest position is near the Xray tube. Through knowledge of anatomical landmarks and the appropriate geometric adjustments, such as parallax, proper oblique projections will display the origin of vessels and landing zones optimally, and excessive angulations will be avoided. Restore the tube's upright position when it is not in use.
Hands
Avoid placing the hands in the direct radiation beam. The use of leaded gloves is controversial in vascular surgery, as they can increase the dose to the patient and staff through the automatic exposure control due to the feedback from the equipment.
Distance
“The further the better”. Try to avoid (if possible) being close to the patient's radiation field. The irradiated volume is the main source of scatter radiation in the room.
Shielding
Always use personal protection tools: lead apron; thyroid protector; and goggles. Also use ceiling suspended screens, and protective under table curtains, if available. This is the more important factor in self protection.
Reduce the dose
If the patient's dose is reduced, the level of scatter radiation is reduced, and, in general, the occupational doses of all staff present in the operating theatre will be reduced.
Personal dosimetry
The new regulatory dose limit will be considered. Use personal dosimeters for all procedures. If you they are not being used for all procedures, occupational doses will not be representative of the real radiation risk.
Auditing radiation protection
Pay attention to monthly personal dose values, in order to audit the level of radiation protection. Active electronic dosimeters with real time information on occupational doses may be helpful in reducing unnecessary occupational doses.
Reporting
Report any accidental relevant exposure and ask for the advice of a medical physics expert or radiation protection expert to optimise occupational protection. In the European Union there is a “right” to ask for the support of these specialists (Fig. 1).2
Figure 1.
Visual summary of radiation protection principles and the topics related to patients and staff. DRLs = diagnostic reference levels; KAP = kerma area product.
Discussion
Radiological protection is based on three principles: justification; optimisation; and dose limits. Justification refers to the balance between benefit and risk (the use of radiation should do more good than harm). Optimisation means that the level of protection should be the best under the prevailing circumstances, maximising the margin of benefit over harm. The acronym ALARA (As Low As Reasonably Achievable) is sometimes used as an equivalent to optimisation, but the concept implies keeping patient exposure to the minimum necessary to achieve the required medical objective. The dose limits apply to professionals and members of the public but not to the medical exposure of patients.
References
- 1.ICRP Publication 105 Radiological protection in medicine. Ann ICRP. 2007;37:1–63. doi: 10.1016/j.icrp.2008.08.001. [DOI] [PubMed] [Google Scholar]
- 2.Council directive 2013/59/EURATOM of 5 December 2013 laying down basic safety standards for protection against the dangers arising from exposure to ionising radiation. Euratom. Available at: https://eur-lex.europa.eu/LexUriServ/LexUriServ.do?uri=OJ:L:2014:013:0001:0073:EN:PDF [Accessed 3 March 2021].
- 3.International Atomic Energy Agency Radiation protection in interventional fluoroscopy. https://www.iaea.org/resources/rpop/health-professionals/interventional-procedures Available from:
- 4.International Atomic Energy Agency . IAEA; Vienna: 2018. Occupational radiation protection.https://www-pub.iaea.org/MTCD/Publications/PDF/PUB1785_web.pdf IAEA Safety Standards Series No. GSG-7. Available from: [Google Scholar]
- 5.ICRP Publication 135 Diagnostic reference levels in medical imaging. Ann ICRP. 2017;46:1–143. doi: 10.1177/0146645317717209. [DOI] [PubMed] [Google Scholar]
- 6.Tuthill E., O'Hora L., O'Donohoe M., Panci S., Gilligan P., Campion D. Investigation of reference levels and radiation dose associated with abdominal EVAR procedures across several European Centres. Eur Radiol. 2017;27:4846–4856. doi: 10.1007/s00330-017-4791-2. [DOI] [PubMed] [Google Scholar]
- 7.Rial R., Vañó E., Del Río-Solá M.L., Fernández J.M., Sánchez R.M., Camblor L.A. National diagnostic reference levels for endovascular aneurysm repair and optimisation strategies. Eur J Vasc Endovasc Surg. 2020;60:837–842. doi: 10.1016/j.ejvs.2020.08.006. [DOI] [PubMed] [Google Scholar]
- 8.ICRU Report Committee 26 on Operational Radiation Protection Quantities for External Radiation Operational quantities and new approach by ICRU. Ann ICRP. 2016;45(1 Suppl):178–187. doi: 10.1177/0146645315624341. [DOI] [PubMed] [Google Scholar]