Abstract
Introduction: The primary studies demonstrated that fabellar prevalence (FP) varied with ethnic and geographical distribution. Osteoarthritis (OA) and age-related degeneration have a significant association with FP. The prevalence of OA worldwide was doubled with life expectancy. Increased life expectancy has increased exposure to OA and age-related degeneration which could be a possible reason for the rise of FP. The analysis was conducted to provide insight about FP in respect to geographical, ethnic, sex, and laterality distribution.
Methodology: Eighty-six studies were included which have data from 34,733 knee joints. Fifty radiological studies were consisting of 27,293 knees and 36 cadaveric studies had the data of 7,440 knees of dissected specimens, respectively. The prevalence, Odds, and rate ratios were calculated for aging, osteoarthritis, and ethnic variation.
Results: The worldwide FP was 25% (95% CI, 0.22, 0.28). The prevalence of fabella was found to be higher in cadaveric studies (32%) than radiological studies (19%) with significant heterogeneity. The FP was 16-18% till 1950 which was doubled by 2020 (35%). The FP in OA knee was 51% which was thrice of baseline.
Keywords: odds ratio, prevalence, knee joints, osteoarthritis, age-related degeneration
Introduction
The tendon of the lateral head of gastrocnemius has a small fibrocartilaginous or ossified nodule. This nodule is a sesamoid bone named fabella which develops inside the tendon after 8-12 years of age [1]. The fabella is making posterolateral or fourth compartment of the knee and it is articulating with the lateral condyle of the femur at the posterior aspect. The fabella redirects the pull of the lateral head of gastrocnemius to improve the efficiency of this muscle. It prevents friction-induced damage to the tendon [2]. The fabella is present as a cartilaginous nodule that is ossified in the later phase of the first decade by enchondral ossification [3]. The ossified fabella is usually visible in routine radiographs of the knee. This normal anatomical variant is often confused with osteophytes or intra-meniscal calcifications or intra-articular loose bodies in degenerated knees with osteoarthritis (OA). The ossification of fabella is not only under genetic control but also under influence of local mechanical stress and biomechanical need which may lead to larger dimensions of the fabella [2]. The fabella is connected with the apex of the fibula by the fabellofibular ligament. The fabellofibular ligament is the thickening of the distal part of the biceps tendon (short head) and maintains the posterolateral stability of the knee joint. Its thickening is considered to be responsible for the discomfort in the posterolateral corner or compartment of the knee, known as fabella syndrome [4]. Earlier, the fabella is rarely affected by disorders, like chondromalacia, osteoarthritis, dislocation, and fracture which resulted in fabella syndrome or entrapment syndrome of common fibular nerve or popliteal artery [2,4]. The fabellar impingement with prostheses is common after total knee arthroplasty (TKA) and may cause knee disorders. Because of the growing number and expectation of TKA patients, clinicians are becoming more concerned about these issues [1,4].
The fabellar prevalence (FP) is variable, which depends upon the methodologies, and racial or geographical distributions. Berthaume et al. [5] claimed that the median prevalence of fabella has raised by 3.5-folds in the last 150 years that could be evolutionary to meet the biomechanical demands. Some researchers found higher FP in older age groups [6,7]. We aimed to measure the prevalence of fabella and its distribution worldwide in a larger sample size. The prevalence of fabella is studied in the different age groups and geographical distribution. The effect of gender, ethnicity, laterality along with osteoarthritis will also be studied in the larger sample size.
Materials and methods
The inclusion criteria for this meta-analysis were the published articles, conference abstracts, unpublished studies with obtainable data, and electronic mails used to gather unpublished data from authors of published articles. The case series or literature review were included in the analysis if sample sizes were mentioned. Their references may be utilized to explain the findings. Both cadaveric and radiological studies were included. The data of radiographs, CT, and MRI scans were considered.
The mean prevalence mentioned in the textbooks or published literature without sample references was excluded. If the authors of any radiographic study were confused between popliteal artery calcification and fabella, then such data were excluded from the analysis. The data of USG and PET excluded from analysis due to poor sensitivity. The literature associated with mammalian prevalence other than human was excluded based on the titles, abstracts, and full articles. Any reports or case series were excluded if the sample size not mentioned.
The systemic search was conducted in the primary database like Medline, Embase, Pubmed, Ebsco, Google Scholar, Ovid database, AUSPORT, and Cochrane library till June 2020. The print or online journals of anatomy, orthopedics, sports or biomechanics, morphology or anthropology science, radiology, and radiotherapy were thoroughly investigated. The search strategy consisted of MeSH terms in different strings of permutations or combinations with Boolean operators, e.g., prevalence, fabella, osteoarthritis, aging, and knee pain.
Selection of studies and assessment of the risk of bias
The studies collected from search strategies were shortlisted with the help of Reyyan QCRI app. The data of search strategies were imported to Reyyan QCRI and shortlisted based on inclusion and exclusion criteria and reading the abstract. A total of eighty-six studies were found suitable for further assessment (Table 1). The full text was downloaded or collected from other sources. Articles of other languages were translated with the help of google translate and professionals if needed. The iBA-based AQUA was exploited to assess the study integrity or quality. Two of the authors read the full text and analyzed the merits based on the five domains of AQUA tools. The data of few studies pooled from literature reviews or other studies if the full text were not available were marked with unknown risk. We have found low to moderate risk and studies were suitable for data extraction for prevalence studies, but heterogeneity would be expected after combining the outcome. The reporting bias due to different methodologies could be possible because anatomical prevalence considered both cartilaginous and ossified fabella, but the radiological method only considered the ossified fabella. So the prevalence of fabella reported in anatomical studies or magnetic resonance imaging (MRI) might be higher as compared to radiographic prevalence due to existent cartilaginous fabella.
Table 1. Distribution of ossified fabella based on study characteristics, ethnicity, gender, and laterality.
*Number fabella per 100 subjects.
| Characteristics | No of studies | Prevalence | Lower bound | Upper bound |
| Methods | ||||
| Dissection | 36 | 32% | 26% | 40% |
| Radiological | 49 | 20% | 16% | 24% |
| Mode of study | ||||
| Anatomical | 36 | 32% | 26% | 40% |
| CT scan | 2 | 35% | 19% | 54% |
| MRI scan | 7 | 28% | 16% | 43% |
| X-ray | 39 | 19% | 15% | 24% |
| Risk of bias | ||||
| Low | 66 | |||
| Moderate | 14 | 22% | 16% | 30% |
| Unknown | 6 | 19% | 11% | 31% |
| Ethnicity | ||||
| African | 3 | 12% | 6% | 22% |
| Asian Caucasian | 5 | 17% | 11% | 26% |
| Asian Mongoloid | 32 | 41% | 36% | 47% |
| European | 27 | 15% | 12% | 18% |
| North American | 12 | 16% | 12% | 22% |
| Oceanian | 3 | 48% | 30% | 66% |
| South American | 4 | 18% | 10% | 30% |
| Gender | ||||
| Male | 46 | 27% | 22% | 32% |
| Female | 46 | 24% | 18% | 31% |
| Laterality* | ||||
| Bilateral | 48 | 61% | 26% | 96% |
| Unilateral | 48 | 27% | 9% | 46% |
Data extraction and management
The information of publishing year, population characteristics, mode of investigation (anatomical or radiological), sample size (number of individual or knee examined), and number of fabellae were extracted. The distribution of gender, age, laterality, and ethnicity were also noted. The contingency tables were prepared separately and the event rate with a 95% confidence interval was computed. Age, sex, and laterality were considered confounding factors, so the rate estimations were done separately. The unit of analysis for the prevalence of fabella was the number of fabella in 100 knees. The prevalence of fabella was measured with the help of ProMeta 3. The rate estimate for ossified fabella was measured with Revman 5.3 (The Nordic Cochrane Centre, The Cochrane Collaboration, Copenhagen, Denmark). The effect size and standard error for each study were computed with ProMeta 3. The heterogeneity statistic was determined as i2 statistics, Cochrane Q, and Kendall Tau. Random effect model was adopted if i2 was more than 50%, in place of the fixed-effect model. Q Cochrane was computed along with the P-value. Sensitivity and cumulative analysis were also performed. The cumulative meta-analysis was performed in order to evaluate the association prevalence of fabella with osteoarthritis and aging. The subgroup analysis was conducted to compute the rate according to ethnicity, mode of study, type of population, sex, and laterality. Regression analysis was carried out to examine the relationship between outcome and confounders (age, sex, and ethnicity). Finally, the odds ratio (OR), rate ratio (RR), and rate difference (RD) were computed. Funnel plots measured the publication bias. For the funnel plot, the logarithmically transformed odds ratio plotted against the standard error of each study. Additionally, the publication bias was measured with the help of Egger's linear regression test, Begg and Mazumdar's rank correlation test. Rosenthal Fail-Safe Number (FSN) was generated to refute the file drawer effect.
Results
Description of studies
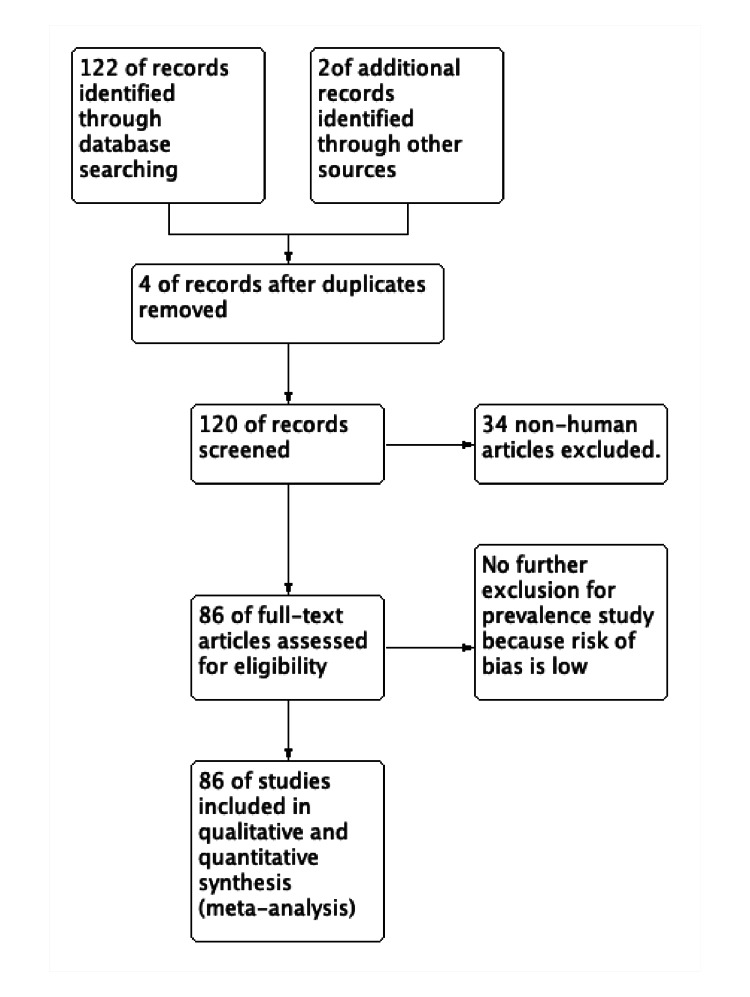
The included publications were observational - cross-sectional, prospective, and retrospective studies. A total of 122 studies were identified by online research and two studies were found in conference proceedings. Due to duplicate titles or abstracts found during searches, four articles were eliminated. Thirty-six studies were excluded for being non-human studies or case reports and series, reviews-based abstract or title evaluation. A study was included after the consensus of both authors, and the third author was consulted in contradicting opinion. For the meta-analysis, 86 studies that dealt with the prevalence of fabella between 1875 and 2020 based on the abstract and full-text analysis were included in this study (Figure 1). The risk of bias was low to moderate. Fifty studies were radiological and 36 studies were cadaveric [1,3,5,7-43].
Figure 1. PRISMA flow diagram of the search strategy.
PRISMA: Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
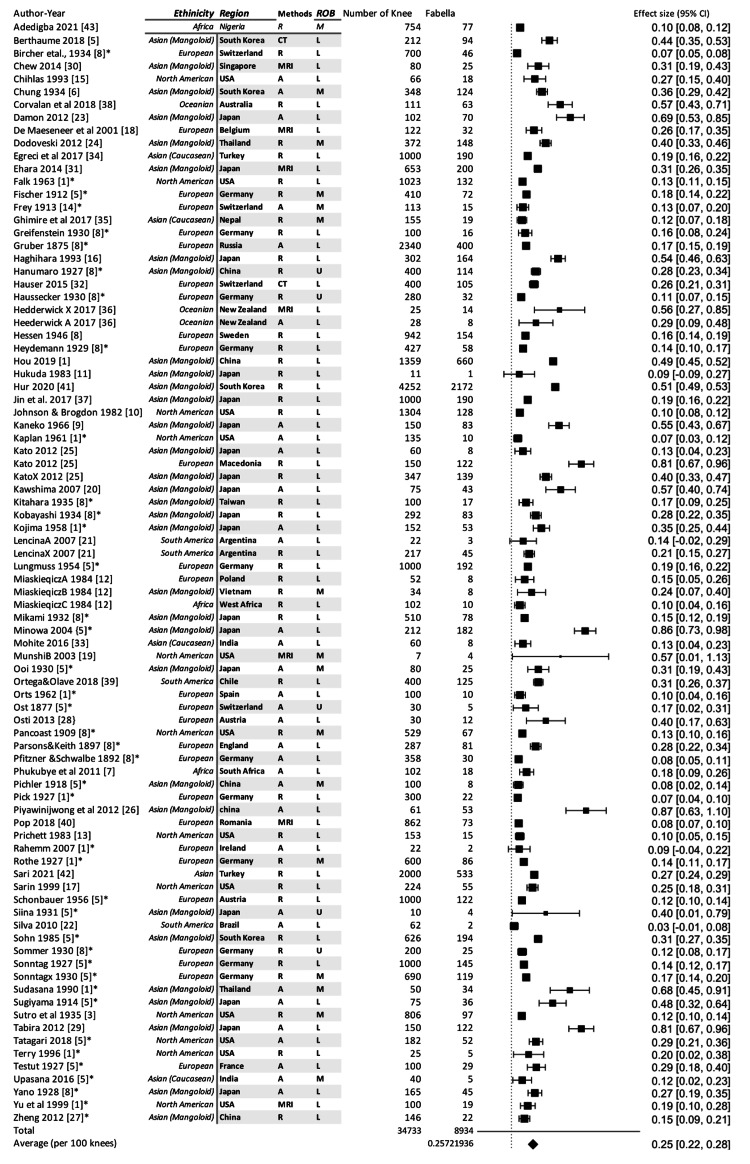
Totally, 34,733 knees were examined for the presence of fabella. The total number of reported fabellae was 8,934 and the prevalence of fabella was 25 per hundred knees (25% or 0.25) (Figure 2). Thirty-six cadaveric studies included 7,440 knees and the prevalence of fabellae was 32%. The FP in radiological studies was 20% on examination of 27,293 knees (Table 1). The existing difference between the two methods is because the cadaveric studies have counted both ossified and cartilaginous fabellae. The meta-regression was conducted to study the relationship between the publication year and FP which revealed that the FP was significantly increased from 1875 to 2020 (P=0.001) Then all studies were classified into 25 years interval for the period between 1875 and 2020 and again meta-analysis operation was conducted to delineate the rising prevalence. The fabellar prevalence was 17-19% for the duration of the years between 1875 and 1950, which got slightly increased to 23% during 1975-2000. A rapid increase to 34% FP was noted during 2000-2020 (almost double of FP of 1875-1950 as shown in Table 2).
Table 2. Prevalence of fabella at different time periods between 1875 and 2020.
*Effect of two world wars.
**Radiograph was invented in 1895 and the first medical X-ray was done in June 1896 by battlefield physicians to locate bullets in wounded soldiers.
#Prevalence of fabella (%)=0.568* life expectancy (in years) - 0.11, correlation coefficient = 0.56 (95% CI, 0.45-0.67), P<0.0001.
| 25 years interval | Studies (C+R) | Total prevalence (95%CI) | Cadaveric prevalence (95%CI) | Radiological prevalence (95%CI) |
| 1875-1900 | 4+0 | 16% (8-30%) | 17% (10-26%) | No studies** |
| 1901-1925 | 3+2 | 17% (10-30%) | 20% (9-37%) | 15% (6-32%) |
| 1926-1950 | 5+15 | 18% (13-23%) | 32%* (23-41%) | 15% (12-18%) |
| 1951-1975 | 4+3 | 19% (11-29%) | 24% (14-26%) | 15% (8-25%) |
| 1976-2000 | 2+11 | 23% (16-32%) | 27% (18-78%) | 19% (11-31%) |
| 2001-2020 | 18+19 | 35% (29-41%) | 41% (31-52%) | 28% (21-38%) |
| 1875-2020# | 36+50 | 25% (22-28%) | 32% (26-40%) | 20% (16-24%) |
Figure 2. Forest plot computing the effective size of fabellar prevalence.
A: anatomical studies, R: radiographic studies based on X-ray, ROB: risk of bias, L: low, M: moderate, U: unknown, H: high.
*Secondary reference.
FP in Different Age-Group and Osteoarthritis
The FP in 0-10 years of the subject was 0.98% and it was increasing with age. The FP was 33.84% in more than 70 years of the aged population (Table 3). The rate of developing fabella was 1.19 at the age of 20 years which was increased to 1.81 by the age of 70 years. The mean age of the study population was showing a significant correlation with FP. Prevalence (%) =0.708* mean age of study population (in years) - 3.845, R=0.708, (95% CI, 0.568-0.809, P<0.001). The FP in OA knee was 51% but, the same in non-OA was 18%. The RR of developing fabella in the OA knee was 2.55. So, the mean age of the population and OA were determining FP.
Table 3. Distribution of fabella in different age groups and OA status of knees.
#The regression analysis of prevalence of fabella: prevalence (%)=0.708* age (in years) - 3.845, correlation coefficient=0.708, 95% CI (0.568-0.809), P<0.001.
^Overall rate ratio due to aging = 1.71(1.59-1.86).
| Age# (years) | Fabellar prevalence (%) | 95% Confidence interval | Rate/risk ratio^ (95%CI) |
| 0-10 | 0.98 | 0.74-1.26 | NA (ossified at 8-12 years) |
| 10-20 | 4.56 | 4.14-4.98 | Baseline |
| 20-30 | 14.52 | 13.77-15.27 | 1.19 (1.12-1.31) |
| 30-40 | 18.88 | 18.02-19.73 | 1.5 (1.42-1.59) |
| 40-50 | 23.44 | 22.49-24.39 | 1.63 (1.48-1.81) |
| 50-60 | 25.38 | 24.39-26.36 | 1.62 (1.49-1.8) |
| 60-70 | 29.45 | 28.39-30.51 | 1.64 (1.55-1.75) |
| >70 | 33.84 | 32.7-34.98 | 1.81 (1.86-2.21) |
| Non-OA | 18 | (7-28) | Baseline |
| OA | 51 | (45-57) | 2.55 (2.15-3.02) |
Ethnic and Geographical Distribution
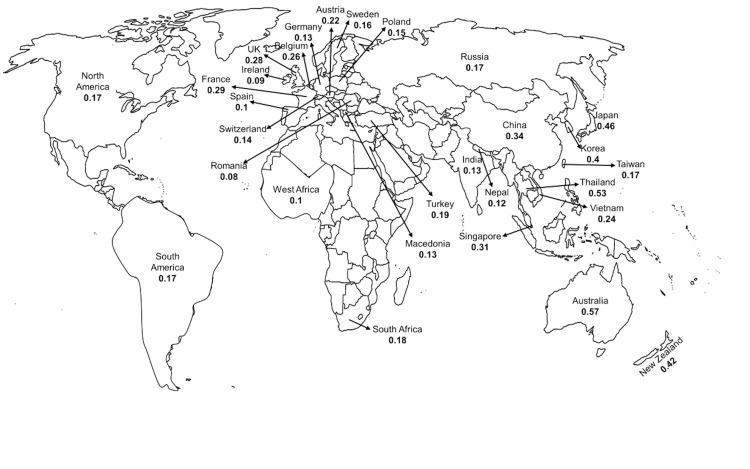
The prevalence of fabellae was very high in Oceanian populations (includes Australia and New Zealand; 48%) and Asian mongoloid populations (includes southeast Asian countries; 41%). The Oceanian population had the highest FP which would be an over-estimation with a wide confidence interval due to fewer studies (Table 1). The FP in Asian Caucasian, European, North, and South American population had almost similar confidence intervals (Figure 3). The African population had a slightly lower FP which would be due to the small sample size.
Figure 3. Geographical distribution of fabella (mean fabellar prevalence) observed during 1875-2020.
Sex and Laterality Distribution (Table 1)
FP was 27% in males and 24% in females. Bilateral occurrence of fabella was more common than unilateral occurrence. The laterality distribution was estimated per hundred subjects. The bilateral and unilateral occurrences were 61% and 27%, respectively. In the case of unilateral distribution, the right and the left side had equal distribution.
Methodological Distribution
The FP in dissected specimens was 32%. The FP in CT scan, MRI, and X-ray studies were 35%, 28%, and 19%, respectively (Table 1). Only two CT studies reported FP in which Hur et al. estimated the FP in OA of mongoloid population. So, the pooled FP for the CT scan was overestimated with a wider confidence interval. The FP in dissected specimens and MRI studies were almost similar in confidence intervals. The radiographic studies (X-ray) had lower FP because cartilaginous fabella was not observed and counted.
Publication bias
On examination of the funnel plot (asymmetrical funnel plot) and the result of Egger's regression test, some publication bias was suspected (P=0.02). But, Begg and Mazumdar's rank correlation test (P=0.126) refuted the asymmetrical funnel plot because of publication bias and it was possibly due to sample variation.
Discussion
Fabellar presence is decided by the genetic constitution as seen in near-human species. The formation of fabella takes place in intrauterine life as a cartilaginous nodule. The cartilaginous nodule is derived from pre-cartilaginous condensations of fibroblast named as a sesamoid precursor in the gastrocnemius tendon during the embryonic period. Hox gene and genes encoding for the TGF-beta family played a crucial role in the sesamoid precursor. Drachman and Sokoloff studied the development of sesamoids in embryonic chicken. The above experiment had explained the fabella development not only determined by the genetic constitution but also by a biomechanical stimulus which led to epigenetic changes [44].
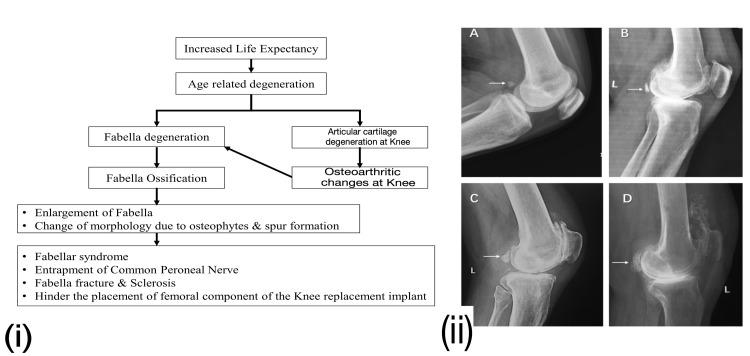
The present study demonstrated that the prevalence of fabella was 25% in 34,733 knees in over 150 years. The FP since the last two decades is estimated at 35% which was 16-18% in 1875-1950. The current meta-analysis has shown a doubling of FP. Berthaume and Bull [2] estimated that FP became 3.5 times in the last 150 years in 21,000 knees. They have computed a median FP which could be over-estimation due to lower sample size. According to them, the rising FP was either evolutionary or a certain biomechanical stimulus. They have tested the evolutionary model by taking the reference of Sarin et al. [17} but their evidence seems a hypothetical assumption without any scientific evidence. They presumed that an increased ratio of tibial and femoral (T/F) length and atrophy of gastrocnemius in the knee and hip osteoarthritis would be the stimulus for fabellar ossification [2]. Weinberg et al. documented that increased T/F ratio is a good predictor of hip and knee OA. They found that males, African and American races have higher T/F values than the female and white population [45]. If we presumed the above plea, then FP should be higher in Americans and Africans. But current data did not support this plea because Mongoloid and Oceanian population have higher fabellar prevalence than American or African populations. They have given another reason for this high prevalence in mongoloids. Kneeling, squatting, and tailor sitting are preferred by Mongoloids. Such habits may cause the fabella to strain against the posterior part of the lateral femoral condyle, promoting fabella formation, and ossification. But this plea is unable to explain the higher prevalence in Oceanian populations. The knee alignment significantly varied among different ethnic groups. The knee valgus alignment was highest for Oceanians, followed by Asian mongoloids, Caucasians, and Afro-Americans. The valgus alignment shifts the weight-bearing from the medial compartment to the lateral compartment. The FP was higher in lateral compartment OA [1,32]. Asian mongoloid like Chinese and Japanese have a valgus alignment of femoral angle in OA as compared to varus alignment seen in Caucasian, American, Middle-east, and Indian populations. Obesity and body mass index (BMI) may aggravate existing valgus knee alignment [46]. The loss of joint space and alteration of condyle plateau angle were attributed to such alignment [47,48]. This will shift the mechanical loading towards the lateral compartment which may lead to lateral tibiofemoral OA. Due to proximity with the femoral articular surface, the lateral tibiofemoral OA may induce osteoarthritic changes in fabella which would advance with age. Age-related degeneration and OA at the knee joint caused fabellar degeneration which resulted in fabellar ossification [1]. When the articular cartilage and menisci of the knee undergo OA changes, cartilaginous degeneration of fabella takes place, or sclerotic changes occur if fabella was already ossified. Following cartilaginous degeneration of fabella (fabellar degeneration), it ossifies or gets sclerosed, leading to fabellar enlargement [1]. The earlier meta-analysis has demonstrated a significant association of FP with OA which could be explained by fabellar degeneration [49]. The possible mechanism is the calcification of articular cartilage, menisci, and fabellar cartilage following degeneration. OA might be the reason behind the increased FP as its prevalence has doubled from 1950 to 2000. The prevalence of OA has increased because of improved life expectancy worldwide [49,50].
Fabella is exposed to such changes due to its vicinity to the knee joint. Such changes contribute to alteration in the shape and size of fabella (Figure 4). The enlarged fabella may cause compression of surrounding structures like nerve or tendon or implants. Knee valgus alignment and obesity are also possible contributors [48].
Figure 4. (i) Fabellar degeneration and ossification flow diagram. (ii) Different grades of fabellar degeneration and ossification are shown in the lateral knee radiographs.
(A) Normal fabella: oval-shaped with anterior smooth surface articulating with the posterolateral condyle of the femur (arrow); (B) sclerosed fabella: subchondral sclerosis of anterior surface (arrow); (C) severe sclerosis of the fabella with osteophyte formation (arrow); (D) enlargement of fabella with marked osteophyte formation (arrow) [1]. Permitted under Creative Commons Attribution 4.0.
Limitation of study
Despite the fact that this study offers useful information about the prevalence of fabella, and its relation with OA, the main limitation of this study is the inadequacy of information regarding weight, height, and BMI. The studies used in the assessment were of various ethnicities and methodologies, leading to even greater heterogeneity. Height, gender, physical habitus or profession, and BMI all seem to be potential confounders in the pooled estimates. Prevalence estimates can be influenced by sample variance.
Conclusions
This study demonstrated the doubling of FP in the last 70 years. OA knee has three times FP of baseline. The incidence of fabella is higher in the Oceanian and Mongoloid populations, male participants, and on the right side of the knee, which is consistent with previous findings. Bilateral occurrence of fabella is far more common than unilateral occurrence, which corresponds to OA distribution. The valgus positioning of the knee, along with obesity, causes lateral compartment OA in the knee, which can raise the FP. The further scope of the study is to evaluate the prevalence of fabella in severe osteoarthritis with and without valgus knee alignment. The stratification of the proposed study would include a final estimation of FP based on the biomechanical load on the knee, as well as aid in understanding the function of fabella in knee biomechanics.
Appendices
Prospero registration: CRD42020161834 (dated 28-04-2020)
Search strategy (PubMed):
(((((((Fabella[Title/Abstract]) OR Knee sesamoid[Title/Abstract]) OR Popliteal Sesamoid[Title/Abstract]) OR Sesamoid[Title/Abstract])) AND ((((Prevalence[Title/Abstract]) OR Incidence[Title/Abstract]) OR event rate[Title/Abstract]) OR events[Title/Abstract])) AND (((((Osteoarthritis[Title/Abstract]) OR Knee Degeneration[Title/Abstract]) OR Knee Pain[Title/Abstract]) OR Knee aging[Title/Abstract]) OR Genu pain[Title/Abstract])) NOT Animal').
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
The authors have declared that no competing interests exist.
Human Ethics
Consent was obtained or waived by all participants in this study
Animal Ethics
Animal subjects: All authors have confirmed that this study did not involve animal subjects or tissue.
References
- 1.Fabellar prevalence, degeneration and association with knee osteoarthritis in the Chinese population. Hou W, Xu L, Wang J, et al. Sci Rep. 2019;9:13046. doi: 10.1038/s41598-019-49174-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Human biological variation in sesamoid bone prevalence: the curious case of the fabella. Berthaume MA, Bull AM. J Anat. 2020;236:228–242. doi: 10.1111/joa.13091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fabella (sesamoid in the lateral head of the gastrocnemius) Sutro CJ, Pomeranz MM, Simon SM. Arch Surg. 1935;30:777–782. [Google Scholar]
- 4.Treatment of fabella syndrome with manual therapy: a case report. Zipple JT, Hammer RL, Loubert PV. https://www.jospt.org/doi/10.2519/jospt.2003.33.1.33. J Orthop Sports Phys Ther. 2003;33:33–39. doi: 10.2519/jospt.2003.33.1.33. [DOI] [PubMed] [Google Scholar]
- 5.Fabella prevalence rate increases over 150 years, and rates of other sesamoid bones remain constant: a systematic review. Berthaume MA, Di Federico E, Bull AM. https://doi.org/10.1111/joa.12994. J Anat. 2019;235:67–79. doi: 10.1111/joa.12994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Uber das vorkommen der fabella bei Koreanern. Chung L. Keijo J Med. 1934;5:1–13. [Google Scholar]
- 7.The incidence and structure of the fabella in a South African cadaver sample. Phukubye P, Oyedele O. https://doi.org/10.1002/ca.21049. Clin Anat. 2011;24:84–90. doi: 10.1002/ca.21049. [DOI] [PubMed] [Google Scholar]
- 8.Fabella: sesamum genu superius laterale. Hessén I. Acta Radiol. 1946;177:96. doi: 10.3109/00016924609133785. [DOI] [PubMed] [Google Scholar]
- 9.Consideration about the Japanese gastrocnemius muscle sesamoid bone (Fabella) Kaneko K. J Nippon Med Sch. 1966;33:337–340. [Google Scholar]
- 10.Dorsal effect of the patella: incidence and distribution. Johnson JF, Brogdon BG. AJR Am J Roentgenol. 1982;139:339–340. doi: 10.2214/ajr.139.2.339. [DOI] [PubMed] [Google Scholar]
- 11.The pattern of spinal and extraspinal hyperostosis in patients with ossification of the posterior longitudinal ligament and the ligamentum flavum causing myelopathy. Hukuda S, Mochizuki T, Ogata M, Shichikawa K. Skeletal Radiol. 1983;10:79–85. doi: 10.1007/BF00360789. [DOI] [PubMed] [Google Scholar]
- 12.Fabella in men of three human races. Miaśkiewicz C, Partyka B. Folia Morphol (Warsz) 1984;43:369–374. [PubMed] [Google Scholar]
- 13.The incidence of fabellae in osteoarthrosis of the knee. Pritchett JW. https://pubmed.ncbi.nlm.nih.gov/6501334/ J Bone Joint Surg Am. 1984;66:1379–1380. [PubMed] [Google Scholar]
- 14.Knee dysfunction secondary to dislocation of the fabella. Frey C, Bjorkengen A, Sartoris D, Resnick D. https://pubmed.ncbi.nlm.nih.gov/3621725/ Clin Orthop Relat Res. 1987:223–227. [PubMed] [Google Scholar]
- 15.Position of the fabella relative to the path of the common peroneal nerve across the lateral head of the gastrocnemius muscle. Chihlas CN, Ladocsi LT, Sholley MM, Loughran TP, Krieg RJ Jr. Clin Anat. 1993;6:163–166. [Google Scholar]
- 16.Incidence and size of fabella in osteoarthrosis of the knee. Hagihara H, Nakaie K, Kishikawa Y, Tsutsumi Y. Orthop Traumatol. 1993;42:995–997. [Google Scholar]
- 17.Coincident development of sesamoid bones and clues to their evolution. Sarin VK, Erickson GM, Giori NJ, Bergman AG, Carter DR. Anat Rec. 1999;257:174–180. doi: 10.1002/(SICI)1097-0185(19991015)257:5<174::AID-AR6>3.0.CO;2-O. [DOI] [PubMed] [Google Scholar]
- 18.Posterolateral supporting structures of the knee: findings on anatomic dissection, anatomic slices and MR images. De Maeseneer M, Shahabpour M, Vanderdood K, De Ridder F, Van Roy F, Osteaux M. Eur Radiol. 2001;11:2170–2177. doi: 10.1007/s003300100983. [DOI] [PubMed] [Google Scholar]
- 19.MR imaging, MR arthrography, and specimen correlation of the posterolateral corner of the knee: an anatomic study. Munshi M, Pretterklieber ML, Kwak S, Antonio GE, Trudell DJ, Resnick D. AJR Am J Roentgenol. 2003;180:1095–1101. doi: 10.2214/ajr.180.4.1801095. [DOI] [PubMed] [Google Scholar]
- 20.Anatomical study of the fabella, fabellar complex and its clinical implications. Kawashima T, Takeishi H, Yoshitomi S, Ito M, Sasaki H. Surg Radiol Anat. 2007;29:611–616. doi: 10.1007/s00276-007-0259-4. [DOI] [PubMed] [Google Scholar]
- 21.Estudio anatómico y radiológico del sesamoídeo del gemelo externo de la rodilla. Lencina O. https://www.aaot.org.ar/revista/2007/n3_vol72/art7.pdf Rev Asoc Argent Ortop Traumatol. 2007;72:248–255. [Google Scholar]
- 22.Morphological analysis of the fabella in Brazilians. Silva JG, Chagas CA, Torres DF, Servidio L, Vilela AC, Chagas WA. https://pdfs.semanticscholar.org/8b17/9afe8e34f151f963d1fc43b9889798e71874.pdf Int J Morphol. 2010;28:105–110. [Google Scholar]
- 23.The role of plain film radiography in the diagnosis and management of knee pain. [Apr;2021 ];Damon CA. https://openscholar.dut.ac.za/handle/10321/711 2012
- 24.Clinical significance of the fabella. Dodevski A, Lazarova-Tosovska D, Zhivadinovik J, Lazareska M. Rentgenol Radiol. 2012;51:258. [Google Scholar]
- 25.The incidence and structure of the fabella in Japanese population - anatomical study, radiographic study, and clinical cases. [Apr;2021 ];Kato Y, Oshida M, Ryu K. https://www.ors.org/Transactions/58/1797.pdf ORS. 2012 2012:1797. [Google Scholar]
- 26.The fabella, fabellofibular and short lateral ligaments: an anatomical study in Thais cadavers. Piyawinijwong S, Sirisathira N, Sricharoenvej S. https://www.researchgate.net/publication/277210919_The_fabella_fabellofibular_and_short_lateral_ligaments_an_anatomical_study_in_Thais_cadavers Siriraj Med J. 2012;64:15–18. [Google Scholar]
- 27.Anatomic study of fabella and its surrounding structures in a Chinese population. Zeng S-X, Dong X-L, Dang R-S, et al. https://link.springer.com/article/10.1007/s00276-011-0828-4. Surg Radiol Anat. 2012;34:65–71. doi: 10.1007/s00276-011-0828-4. [DOI] [PubMed] [Google Scholar]
- 28.Posterolateral corner of the knee: microsurgical analysis of anatomy and morphometry. Osti M, Tschann P, Künzel KH, Benedetto KP. Orthopedics. 2013;36:0–20. doi: 10.3928/01477447-20130821-11. [DOI] [PubMed] [Google Scholar]
- 29.Influence of a fabella in the gastrocnemius muscle on the common fibular nerve in Japanese subjects. Tabira Y, Saga T, Takahashi N, Watanabe K, Nakamura M, Yamaki K. https://doi.org/10.1002/ca.22153. Clin Anat. 2013;26:893–902. doi: 10.1002/ca.22153. [DOI] [PubMed] [Google Scholar]
- 30.Incidence and radiological characteristics of fabellae in an Asian population. Chew CP, Lee KH, Koh JS, Howe TS. Singapore Med J. 2014;55:198–201. doi: 10.11622/smedj.2014052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Potentially symptomatic fabella: MR imaging review. Ehara S. https://doi.org/10.1007/s11604-013-0253-1. Jpn J Radiol. 2014;32:1–5. doi: 10.1007/s11604-013-0253-1. [DOI] [PubMed] [Google Scholar]
- 32.Functional and structural details about the fabella: what the important stabilizer looks like in the central European population. Hauser NH, Hoechel S, Toranelli M, Klaws J, Müller-Gerbl M. Biomed Res Int. 2015;2015:343728. doi: 10.1155/2015/343728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Morphological study of the plantaris muscle. Mohite S, Mohite H, More R. Int J Health Sci Res. 2016;6:125–130. [Google Scholar]
- 34.Prevalence and distribution of the fabella: a radiographic study in Turkish subjects. Egerci OF, Kose O, Turan A, Kilicaslan OF, Sekerci R, Keles-Celik N. Folia Morphol (Warsz) 2017;76:478–483. doi: 10.5603/FM.a2016.0080. [DOI] [PubMed] [Google Scholar]
- 35.Evaluation of occurrence of sesamoid bones in the lower extremity radiographs. Ghimire I, Maharjan S, Pokharel GB, Subedi K. J Chitwan Med Coll. 2017;7:11–14. [Google Scholar]
- 36.The oblique popliteal ligament: an anatomic and MRI investigation. Hedderwick M, Stringer MD, McRedmond L, Meikle GR, Woodley SJ. Surg Radiol Anat. 2017;39:1017–1012. doi: 10.1007/s00276-017-1838-7. [DOI] [PubMed] [Google Scholar]
- 37.A new insight into the fabella at knee: the foetal development and evolution. Jin ZW, Shibata S, Abe H, Jin Y, Li XW, Murakami G. Folia Morphol (Warsz) 2017;76:87–93. doi: 10.5603/FM.a2016.0048. [DOI] [PubMed] [Google Scholar]
- 38.Fabella and cyamella of the human knee joint: discovery by dissection and ultrasound examination. Corvalan C, Tang C, Robinson M. https://eurjanat.com/data/pdf/eja.170142cc.pdf Eur J Anat. 2018;22:103–109. [Google Scholar]
- 39.Presence, location and biometry of the fabella in Chilean individuals: radiological study/Presencia, localizacion y biometria de la fabela en individuos Chilenos: estudio radiologico. Ortega M, Olave E. Int J Morphol. 2018;36:358–362. [Google Scholar]
- 40.Prevalence of the fabella and its association with pain in the posterolateral corner of the knee: A cross-sectional study in a Romanian population. Pop TS, Pop AM, Olah P, Trâmbiţaş C. Medicine (Baltimore) 2018;97:0. doi: 10.1097/MD.0000000000013333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.The prevalence of fabella and its association with the osteoarthritic severity of the knee in Korea. Hur JW, Lee S, Jun JB. Clin Rheumatol. 2020;39:3625–3629. doi: 10.1007/s10067-020-05078-4. [DOI] [PubMed] [Google Scholar]
- 42.The prevalence of fabella in Turkish population and the association between the presence of fabella and osteoarthritis. Sari A, Dincel YM, Cetin MU, Gunaydin B, Guney M. SN Compr Clin Med. 2021;3:805–811. [Google Scholar]
- 43.Fabella and patella variants: radiographic prevalence, distribution and clinical relevance in a population of black African descent [PREPRINT] Adedigba JA, Idowu BM, Hermans SP, et al. Anat Cell Biol. 2021 doi: 10.5115/acb.20.217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.The role of movement in embryonic joint development. Drachman DB, Sokoloff L. Dev Biol. 1966;14:401–420. [Google Scholar]
- 45.The association of tibia femur ratio and degenerative disease of the spine, hips, and knees. Weinberg DS, Liu RW. J Pediatr Orthop. 2017;37:317–322. doi: 10.1097/BPO.0000000000000658. [DOI] [PubMed] [Google Scholar]
- 46.Frequency of varus and valgus thrust and factors associated with thrust presence in persons with or at higher risk of developing knee osteoarthritis. Chang A, Hochberg M, Song J, et al. Arthritis Rheum. 2010;62:1403–1411. doi: 10.1002/art.27377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Analysis of limb alignment in the pathogenesis of osteoarthritis: a comparison of Saudi Arabian and Canadian cases. Cooke TD, Harrison L, Khan B, Scudamore A, Chaudhary MA. Rheumatol Int. 2002;22:160–164. doi: 10.1007/s00296-002-0218-7. [DOI] [PubMed] [Google Scholar]
- 48.Knee alignment differences between Chinese and Caucasian subjects without osteoarthritis. Harvey WF, Niu J, Zhang Y, et al. Ann Rheum Dis. 2008;67:1524–1528. doi: 10.1136/ard.2007.074294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Does the prevalence of ossified fabella vary in knee osteoarthritis and age-related degeneration? A meta-analysis of about 11,000 knees. Asghar A, Naaz S, Narayan RK, Kumar A. Cureus. 2021;13:0. doi: 10.7759/cureus.12535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Knee osteoarthritis has doubled in prevalence since the mid-20th century. Wallace IJ, Worthington S, Felson DT, et al. Proc Natl Acad Sci U S A. 2017;114:9332–9336. doi: 10.1073/pnas.1703856114. [DOI] [PMC free article] [PubMed] [Google Scholar]