Abstract
Objectives
The effect of buccinator muscle on the mandible need to be more clarified. Finite element method used to estimate the effect of the buccinator during abnormal function on the size and shape of the mandible.
Methods
Three-dimensional model of human mandible using Finite element analysis referring to dry normal mandible with teeth as a template, The mechanical characteristic of the materials were supposed to be homogenous, isotropic, and linear elastic. Auto mesh order used to discredit the model under analysis to numerous elements; every element includes numbers of apexes called nodes; the association of elements and nodes called the finite element mesh. The force of (2 gm/cm2) had been applied perpendicular to buccal surface of posterior teeth within the mandible representing normal buccinators muscle function on the mandible. While for simulation of abnormal suckling, buccinators muscle force (21 gm∖cm2) applied to the same area.
Results
abnormal size and shape of the mandible with malocclusion especially at the posterior teeth area in transverse direction in addition to backward pressure on the chin and anterior teeth result from abnormal suckling force.
Conclusion
It could be concluded that abnormal function of buccinators during growth and development could result in size and shape variation of the mandible with concomitant malocclusion.
Keywords: Finite element analysis, Stress, Buccinator muscle, Mandible, Sucking habit
1. Introduction
Many important oral functions like the swallowing, mastication, pronunciation down many times during the day and guided by number of muscles, function as a one-unit system. Of these functions is the swallowing which is a peristaltic-like waves tone starting at the oral cavity and push through into the pharynx. These waves augmented by the buccinators then orbicularis oris. It is important to remember here that always the buccinators push inward.1, 2, 3 These oral functions insist the cranio-cervico-mandibular system muscles to work in part or as a whole in coordination to deliver physiologic forces to the teeth and dental arches.4 The buccinator muscle is a horizontal fibers forming a flat quadrilateral muscle deep to the skin covered in part by masseter muscle and superfacial facial muscles, play a role in the facial expression and aid in swallowing and mastication. It is arise from the buccal alveolar process of the maxilla, the mandible and, the pterygomandibular raphae to interdigitate at the corner of the mouth with orbicularis oris muscles.1,5
Sucking habit like thumb and pacifier sucking, bottle feeding could deliver excessive abnormal inward forces from cheek muscles “buccinators” on the posterior teeth in maxilla and mandible, with the absence of outward balancing forces from the tongue that accompanying these habits, result in possible dentoalveolar arch narrowing that could possibly be accompanied by occlusal deviation.6,7
For correct diagnosis and management of the stomatognathic system dysfunction, it is important to know the natural flow of the stress within the stomatognathic system.8 Finite element model of the mandible built to simulate the activity of buccinator muscle on the mandibular dentoalveolar structure. This model is an indirect, nondestructive approach to study the stress effect in the stomatognathic system. It is easier to do quantitative evaluation of the stress within the mandibular dental arch on a more solid and precise biomechanical basis using Finite element analysis as compared with photo-elastic method and strain gauge.8
In orthodontic literature, much attention has been paid to estimate the effect of abnormal lips and tongue posture and function on the dentofacial growth and development with concomitant malocclusion. Very few studies conducted on the buccinators muscle with no study really estimating approximately the exact effect of buccinators muscle on the jaw form. Here in this study we tried to evaluate the possible effect of buccinators muscle on mandible using finite element analysis.
Aim:
-
1.
We did this study to know the final stress distribution in mandibular dental arch.
-
2.
Analyze the probable form or shape of mandibular defect that could be resulted through the severity of the habit.
-
3.
We take an idea that if we remove the habit or decease its severity we could help to restore the physiologic form and size of the mandible or overcome future defect.
2. Methods and materials
According to FEA method, the main three phases were followed:9, 10, 11, 12
-
1)Pre-processing phase which includes:
-
•Model creation.
-
•Defining the form of elements.
-
•Defining property of given materials.
-
•Boundary condition.
-
•Load application.
-
•
-
2)
Solution phase.
-
3)
Post processing phase.
The previous authorized methods used to create 3D model of human mandible with teeth as a template13, 14, 15 by AutoCAD (2010) Program. For all the linear measurements of the mandible, electronic caliper used. Due to difficulties in mechanical modeling and the complexity of its mesh mathematical calculations, the periodontal ligaments were excluded.15,16 Cancellous bone network is disregarded,so, it will be seen as a solid design inside the inner cortical bone shell.12 The models was transported to finite element program Autodesk Inventor Professional Computer Program version (2020). Mechanical characteristic of the materials were proposed to be isotropic, homogenous, and linear elastic as suggested by many researches.12,17 Young's modulus and Poisson's ratio were presented in an isotropic material. Young's modulus defined as the relationship between stress and strain in the elasticity region of uniaxial deformation.18 Whereas, Poisson ratio represents the ratio of transverse contraction (for expansion) strain to longitudinal extension strain in the direction of stretching force.18 The Young's modulus and Poisson's ratio for cortical and cancellous bone were depend on Rho et al. study19, while teeth properties were relying on the study of Boccaccio et al.20 as in Table (1).
Table 1.
Material mechanical properties.
| Material | Young's modulus (GPaa) | Poissons Ratio |
|---|---|---|
| Cortical bone | 20.7 | 0.3 |
| Cancellous bone | 14.8 | 0.3 |
| Teeth | 18.6 | 0.31 |
GPa Gaga Pascal.
The boundary condition is a restraint applied to the model, from which potential energy and solutions are derived.21 Any false result can be attributed to the areas adjacent to the constraints. In our model, boundary conditions were designed so that the mandible was fixed to avoid bodily movement of model by supporting the outer surface of the condyle. The mandible was supported by restricting all the movements at the top of the Condyle12,20 resembling Glenoid fossa.
Auto mesh order used to discredit the model under analysis to numerous elements; each element includes numerous of apexes called nodes; the association of elements and nodes is named the finite element mesh, which extremely sensitive to the number of elements involved in the model. The final mesh of our study model was consisted of 1,916,436 nodes, 1322161 elements.
The force of (2 gm/cm2) had been applied perpendicular to buccal surface of posterior teeth within the mandible representing normal buccinators muscle function on the mandible. while for simulation of abnormal suckling, buccinators muscle force (21 gm∖cm2) was applied to the same area.(3)
3. Result
The results illustrated in terms of Von mises and displacement in three directions. A color scale with thirteen values and twelve color were used for quantitative visualization of the stress distribution and displacement of the mandible; these values vary according to the range of variable, minimum variable value was represented in the blue range. while the maximum variable value was represented in red rang. The maximum values for Von mises stress and displacement for both models were labeled in Table (2)
Table 2.
Maximum Von mises stress and displacement values.
| variables | 2 g | 21 g |
|---|---|---|
| Von mises (Mpaa) | 0.02066 | 0.204 |
| X-Displacement (mmb) | 3.528 | 5.998 |
| Y-Displacement (mm) | 5.9 | 7.719 |
| Z-Displacement (mm) | −3.459 | −5.557 |
(MPa) Mega Pascal.
(mm) millimeter.
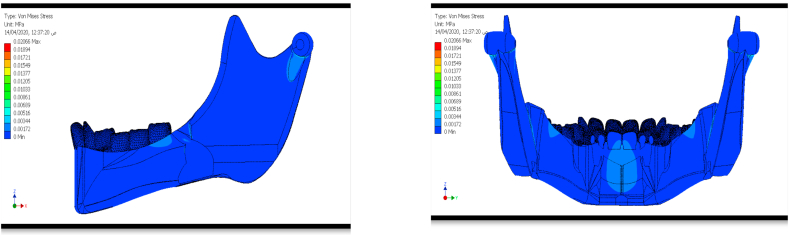
3.1. Von mises stress
The maximum stress value within normal muscle was 0.02066 Mpa, while the maximum value for abnormal muscle function 0.204 Mpa. Both muscle condition have the same stress distribution pattern, the stress was concentration adjcent to the area of fixation and force application and chin area Fig. 1, Fig. 2.
Fig. 1.
Von mises stress distribution within (2 g/cm2).
Fig. 2.
Von mises stress distribution within (21 g/cm2).
3.2. Displacement
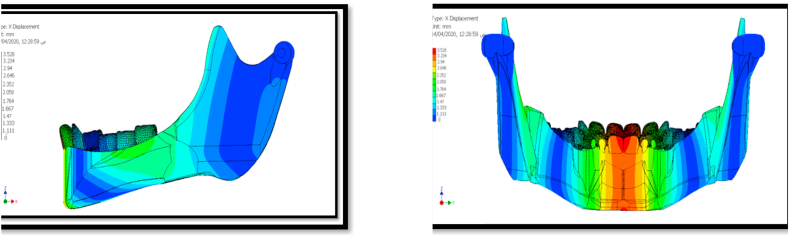
3.2.1. X-displacement
X-displacement illustrate (sagittal) movement of mandible, positive value represent a back ward displacement, while the negative value indicate forward displacement. For both muscle conditions all, the mandible move posteriorly, the high posterior movement can be seen within central and within chin prominence area. Middle range of posterior movement was detected within area of force application, ascending ramus, Fig. 3, Fig. 4.
Fig. 3.
X-Displacement within (2 g/cm2).
Fig. 4.
X-Displacement within (21 g/cm2).
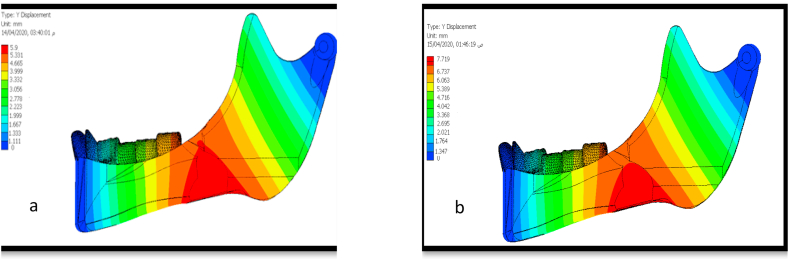
3.2.2. Y-displacement
It identify transverse movement. positive value mean inward twisting of the mandible (lingually). In this study, we found that the mandible under buccinators muscle force was bended in lingual direction, Figure (5).
Fig. 5.
Y-Displacement within a.(2 g/cm2) b. (21 g/cm2).
3.2.3. Z-displacement
Z-displacement specify vertical movement, positive values represent the upward mandibular displacement, while the negative values point out to the downward movement of the mandible. In the study we found that the mandible under buccinators muscle force was move in downward direction, Figure (6).
Fig. 6.
Z-Displacement within a. (2 g/cm2) b. (21 g/cm2).
4. Discussion
Growth and development of the Maxilla and mandibule will continue uninterrupted as the function still active. Genetic will determine the range for the sizes of structures, in that, if functional activity is within normal physiologic limit the structure will continue to grow until it reach proper shapes and relation. while if the function is low or improperly done that will lead to variation in size of the structure.3 Muscles of tongue, face, mastication, supra hyoid and infra hyoid muscles, position of cervical spines and positions of condyle within the TMJ, affect the Jaw size and shape. So, the activity of any of structure within the craniocervicomandibular structure will have an effect on the position, form and activity of other structure/s within the system.
The size and shape of the mandible is genetically determined, guided by the function of the associated soft tissue and organ. If the function within the normal physiologic limit, so the structure “mandible” will reach its predetermined full size and shape with good room for the teeth.3 The extra oral forces acting on the jaws from facial muscles like buccinators and oribicularis oris muscles balanced form inside by tongue. Many habits like thumb sucking or tongue thrust could deteriorate this balance with concomitant abnormal configuration in size and shape of the jaws.22
During chewing, buccinators muscles hold the cheek to the teeth and by this action, the food bolus will be pushed back to the occluding surface of posterior teeth, as when a person chews, so assists the muscles of mastication.23, 24, 25 The parent should be informed about the bad impact of the habit on dental arch. Kohler and Holst,26 and Warren et al.27 showed that impaired dentoalveolar development from finger-sucking habits and dummies with abnormal buccinators. On aberrant swallow, the buccinator showing over activity pulling the corner of the mouth that possibly suppress the anterior oral seal which oppose by mentalis overactivity in an attempt to control the anterior oral seal which possibly followed by impaired jaw development. This explain the pressure exerted by the over activity of mentalis during aberrant swallow.28 Hyperactivity of the buccinator muscle may causes narrow arches and malocclusion.29 Positive pressures measured on buccal surfaces in the oral cavity of humans are typically increased with mastication and increased even more during swallowing. Appliances with buccal shields, like Frankle gauge or the Myobrace have been designed to alleviate the abnormal force of the facial muscles surrounding the dental arches. Clinical trials have proofed the benefit of these appliances for expanding the dental arches transversely.30,31 Additional action of the buccal shields is an osteogenic stimulution to the alveolar attachment areas produced by stretching the buccinators muscle.29
The main goal of this preliminary study was to estimate the final stress distributions in the mandibular dental arch exerted by the buccinator muscle during normal and abnormal oral function with the probable form or shape of mandibular defect using FEA.
According to the result of the present study, higher stress estimated in the group of aberrant muscle forces than in group of normal muscular function with higher concentration detected at the areas of force application, fixation and at the chin. It could be postulated, logically, that the area of force application will express higher concentration of forces a result of direct contact of muscle to the bone probably with the resultant lateral jaw narrowing. This is accompanied with Y displacement that showed marked lingual displacement of that part of the mandible at the area of force application in the abnormal functional group. The pressure exerted by buccinators, which act as muscular hydrostate, is, inward, lingually directed. Probably so, in parafunction with abnormal pressure we could see jaw narrowing.24,25,and 32 At the fixation areas, the higher stress accumulation possibly be due to the limitation of jaw displacement at these points.
5. Conclusion
From the result of this study, it could be concluded that the abnormal pressure exerted by buccinators muscle during growth and development stage could result in abnormality in mandibular size and shape including the mandible bended in lingual direction, move posteriorly, the high posterior movement can be seen within central and within chin prominence area, as well as move in downward direction.
Declaration of competing interest
The author declared that there is no conflict of interest.
Acknowledgement
Thanks for Dr. Rameriz Yanies for access to his book “Early treatment of malocclusion".
Contributor Information
Saba H. Al Zubaidi, Email: dr.sabahalzubaidi@uomosul.edu.iq, dr.sabahalzubaidi@uomosul.edu.iq.
Mustafa M.H. Alsultan, Email: mustafa.muath@uomosul.edu.iq.
Lamiaa A. Hasan, Email: lamiaaabdulrhman@uomosul.edu.iq.
References
- 1.Perkins R.E., Blanton P.L., Biggs N.L. Electromyographic analysis of the buccinator mechanism in human beings. J Dent Res. 1977;56:783–794. doi: 10.1177/00220345770560071301. [DOI] [PubMed] [Google Scholar]
- 2.Kang Hc, Kwak H.H., Hu K.S. An anatomical study of buccinator muscle fibers that extend to the terminal portion of the parotid duct, and their functional roles in salivary secretion. J Anat. 2006;208:601–607. doi: 10.1111/j.1469-7580.2006.00574.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ramirez G.Y. Calle 0 No. 11E-71 Quienta Oriental Cucuta; Colombia: 2009. Early Treatment of Malocclusion, Prevention and Interception in Primary Dentition. ISBN 978 0 9812527 04; pp. 40–42. [Google Scholar]
- 4.Dutra E.H., Caria P.H., Rafferty Kl, Herring S.W. The buccinator during mastication: a functional and anatomical evaluation in minipigs. Arch Oral Biol. 2010;55(9):627–638. doi: 10.1016/j.archoralbio.2010.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Baghele O.N. Buccinator muscle repositioning. J Indian Soc Periodontol. 2012;16(3):456–460. doi: 10.4103/0972-124X.100930. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 6.Graber T.M. The “three M's”: muscles, malformation, and malocclusion. 1963;49(6):418–450. [Google Scholar]
- 7.Mew J.R. The postural basis of malocclusion: a Philosophical overview. Am J Orthod Dentofacial Orthop. 2004;126(6):729–738. doi: 10.1016/j.ajodo.2003.12.019. [DOI] [PubMed] [Google Scholar]
- 8.Pileicikiene G., Surna A., Barauska R., Surna R., Basevicius A. Finite Element analysis of stresses in the maxillary and mandibular dental arches and TMJ articulatar discs during clenching into maximum intercuspation, anterior and unilateral posterior occlusion. Stomatol. 2007;9(4):121–128. [PubMed] [Google Scholar]
- 9.Mohammed S.D., Desai H. Basic concepts of finite element analysis and its applications in dentistry. Journal of Oral Hygiene & Health. 2014;2(5) [Google Scholar]
- 10.Pritam M., Priyam M., Nivedita S., Sah S., Debapreeti M. Finite element method: a research tool in orthodontics. Journal of Research and Advancement in Dentistry. 2015;4(3):58–63. [Google Scholar]
- 11.Şteţiu A.A., Oleksik V., Şteţiu M. Modelling and finite element method in dentistry. Romanian Biotechnological Letters. 2015;20(4) [Google Scholar]
- 12.Hsu M.L., Chang C.L. Finite element analysis. Application of Finite Element Analysis in Dentistry. 2010:43–46. [Google Scholar]
- 13.Al-Khatib A.R., Hasan L.A., Alrawi M.N., Alhajar E.H. A finite element analysis of biomechanics in distraction osteogenesis of ascending ramus lengthening between males and females—a comparative study. Journal of Orofacial Sciences. 2020;12:41–46. [Google Scholar]
- 14.Hasan L.A., Al-Sayagh N.M., Al-Banaa L.R. Influence of different orientations and rates of bidirectional distraction osteogenesis of the mandibular corpus: a three-dimensional study. J Oral Res Special. 2019;S1:11–14. [Google Scholar]
- 15.Rees J.S. An investigation into the importance of periodontal ligament and alveolar bone as supporting structures in finite element studies. J Oral Rehabil. 2001;28:425–432. doi: 10.1046/j.1365-2842.2001.00686.x. [DOI] [PubMed] [Google Scholar]
- 16.Gei M., Genna F., Bigoni D. An interface model for the periodontal ligament. J Biomech Eng. 2002;124:538–546. doi: 10.1115/1.1502664. [DOI] [PubMed] [Google Scholar]
- 17.Kim Ki, Cha B.K., Choi D.S., Jang I., Yi Y.J., Jost-Brinkmann P.G. A finite element study on the effects of mid symphyseal distraction osteogenesis on the mandible and articular disc. Angle Orthod. 2012;82(3):464–471. doi: 10.2319/041211-262.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Evans F.G. The mechanical properties of bone. Artif Limbs. 1969;13:37–48. [PubMed] [Google Scholar]
- 19.Rho J.Y., Ashman R.B., Turner C.H. Young's modulus of trabecular and cortical bone material: ultrasonic and microtensile measurements. J Biomech. 1993;26:111–119. doi: 10.1016/0021-9290(93)90042-d. [DOI] [PubMed] [Google Scholar]
- 20.Boccaccio A., lamberti L., pappalettere c, cozzani M., siciliani G. Comparison of different orthodontic devices for mandibular symphyseal distraction osteogenesis : a finite element study. Am J Orthod Dentofacial Orthop. 2008;134:260–269. doi: 10.1016/j.ajodo.2006.09.066. [DOI] [PubMed] [Google Scholar]
- 21.Singh J.R., Kambalyal P., Jain M., Khandelwal P. Revolution in orthodontics: finite element analysis. Journal of international society of preventive and community dentistry. Mach-April. 2016;6(2) doi: 10.4103/2231-0762.178743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jacobson A. Psychology and early orthodontic treatment. Am J Orthod. 1979;76:511–5293. doi: 10.1016/0002-9416(79)90256-2. [DOI] [PubMed] [Google Scholar]
- 23.Brand R.W., Isselhard D.E., Satin E. Mosby; St. Louis, MO: 2013. Anatomy of Orofacial Structures: A Comprehensive Approach. [Google Scholar]
- 24.Westbrook K.E., Nessel T.A., Varacallo M. Anatomy, head and neck, facial muscles. Treasure Island (FL): StatPearls Publishing. 2020 Apr NBK493209. [PubMed] [Google Scholar]
- 25.Mioche L., Hiiemae K.M., Palmer J.B. A postero-anterior videofluorographic study of the intra-oral management of food in man. Arch Oral Biol. 2002 Apr;47(4):267–280. doi: 10.1016/s0003-9969(02)00007-9. [DOI] [PubMed] [Google Scholar]
- 26.Kohler L., Holst K. Malocclusion and sucking habits of four years old children. Acta Paediatr Scand. 1973;62:373–379. doi: 10.1111/j.1651-2227.1973.tb08122.x. [DOI] [PubMed] [Google Scholar]
- 27.Warren J., Bishara S., Steinbock K., Yonezu T., Nowak A. Effects of oral habits' duration on dental characteristics in the primary dentition. J Am Dent Assoc. 2001;132:1685–1693. doi: 10.14219/jada.archive.2001.0121. [DOI] [PubMed] [Google Scholar]
- 28.Grippaudo C., Paolantonio E.G., Antonini G., Saulle R., La Torre G., Deli R. Association between oral habits, mouth breathing and malocclusion. Acta Otorhinolaryngol Ital. 2016;36(5):386. doi: 10.14639/0392-100X-770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fränkel R. Decrowding during eruption under the screening influence of vestibular shields. Am J Orthod. 1974;65:372–406. doi: 10.1016/0002-9416(74)90271-1. [DOI] [PubMed] [Google Scholar]
- 30.Moin K., Bishara S.E. An evaluation of buccal shield treatment. A clinical and cephalometric study. Angle Orthod. 2007;77:57–63. doi: 10.2319/120405-423R.1. [PubMed: 17029546] [DOI] [PubMed] [Google Scholar]
- 31.Li Xiaowei, Wang Hongmei, Song Li, Bai Yuxing. Treatment of a class II division 1 malocclusion with the combination of a myofunctional trainer and fixed appliances. Am J Orthod Dentofacial Orthop. 2019;156(4):545–554. doi: 10.1016/j.ajodo.2018.04.032. [DOI] [PubMed] [Google Scholar]
- 32.Mew J., Guest editorial. The influence of the tongue on dentofacial growth. Angle Orthod. 2015;85(4):715–716. doi: 10.2319/angl-85-04-715-715.1. [DOI] [PMC free article] [PubMed] [Google Scholar]