Abstract
Background: Coronavirus disease 2019 (COVID-19) is primarily a respiratory disease that has become a global pandemic. Close contact plays an important role in infection spread, while fomite may also be a possible transmission route. Research during the COVID-19 pandemic has identified long-range airborne transmission as one of the important transmission routes although lack solid evidence.
Methods: We examined video data related to a restaurant associated COVID-19 outbreak in Guangzhou. We observed more than 40,000 surface touches and 13,000 episodes of close contacts in the restaurant during the entire lunch duration. These data allowed us to analyse infection risk via both the fomite and close contact routes.
Results: There is no significant correlation between the infection risk via both fomite and close contact routes among those who were not family members of the index case. We can thus rule out virus transmission via fomite contact and interpersonal close contact routes in the Guangzhou restaurant outbreak. The absence of a fomite route agrees with the COVID-19 literature.
Conclusions: These results provide indirect evidence for the long-range airborne route dominating SARS-CoV-2 transmission in the restaurant. We note that the restaurant was poorly ventilated, allowing for increasing airborne SARS-CoV-2 concentration.
Keywords: Airborne, Close contact, Fomite, Human behavior, Covid-19
Introduction
Coronavirus disease 2019 (COVID-19) has threatened human life globally. Since the first cases reported in December 2019, the COVID-19 pandemic has infected over 80 million people in more than 200 countries, with a death toll exceeding 1.75 million as of 31 December 2020 (https://covid19.who.int/). The possible transmission routes for SARS-CoV-2 includes long-range airborne, close interpersonal contact (refers to ‘close contact’ in the remaining text, which includes short-range airborne and large droplets), fomite, and faecal-oral routes[1], [2], [3], [4]. Long-range airborne transmission, overlooked in the early months of the pandemic5, has come to be acknowledged as the important route of transmission6 , 7.
Restaurants are one of the indoor environments which have been reported a high risk for COVID-19 spread possibly due to low mask-wearing rate for eating, possible high occupancy, cross-infection risk by staff, possible close contact, and possible poor ventilation and sanitation in some of the restaurants. In Wisconsin state, USA, 1633 cases (12.1%) were infected in restaurants and bars8. US CDC defined that on-site dining with indoor seating but no reduced capacity and 6-feet-apart table spaces as the highest risk scenario9. Restaurants have been forced to close in many countries during the peak period(s) of the pandemic[10], [11], [12]. In China, infection risk in restaurants may also be increased as diners usually share all dishes as a local culture, although public chopsticks and spoons are becoming popular. The COVID-19 outbreak in a restaurant in Guangzhou, has been studied[13], [14], [15], [16]. Some other studies have also found poor ventilation to be associated with some outbreaks such as Diamond Princess cruise ship, and choir in Washington State, USA14 , 17. In all these studies, it is difficult to rule out the roles of fomites and close contact routes due to lack of relevant data, such that the dominance of airborne transmission, especially including long-range transmission may not be fully supported.
For this study, we obtained a full video recording of a COVID-19 outbreak in a restaurant in Guangzhou as a part of the official epidemic investigation by the Guangdong Centers for Disease Control and Prevention. All diners and staff were monitored by three high-resolution video cameras at the time of exposure. Using an anonymized approach, we analyzed the surface touch and close contact behavior of all diners and restaurant staff in the restaurant from 12:01:30 (time that the index case entered the restaurant) to 14:20:20 (time that the last diner left the restaurant). The infection risk for fomite, close contact, and both routes are analyzed.
Methods
The outbreak
On January 24 2020, 89 diners (coded from D1 to D89) from 17 different family groups (one table for one group), had lunch in the restaurant in Guangzhou. Diners at different tables did not have any relationship. The diner (D9) at table T01, who has been regarded as the index case in previous studies13 , 16, came to Guangzhou with her family from Wuhan on January 23 (Fig. 1 ). D2, D4, D7, and D8 who sat the same table with D9 were infected in the following days (Fig. S1). D11, D12, D14, D15, and D18 who sat the different table with the source patient were tested positively in the following days. Based on the retrospect investigation, five diners (local family) in other tables (T02 and T03) had no contact history with the infected before and after the lunch.
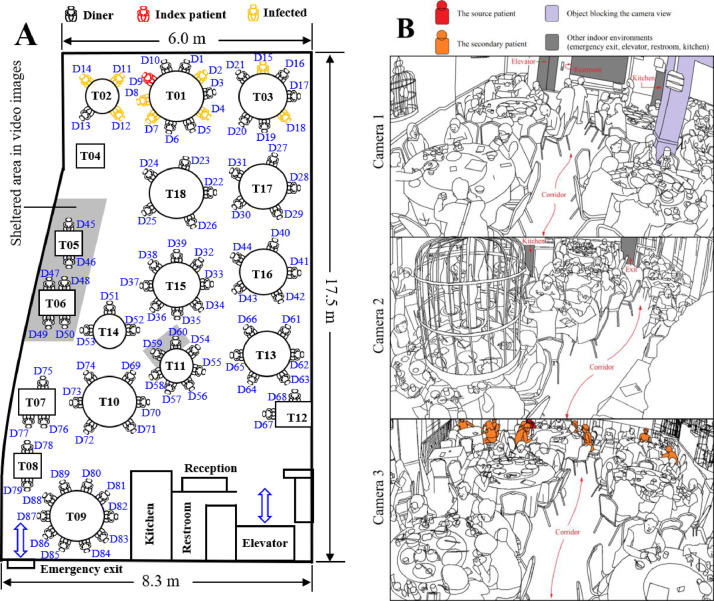
Fig. 1.
Diner positions and arrangement of the restaurant. (A) Floor plan sketch; (B) The 3D views of the three cameras.
In addition to the index case, four, three, and two diners on tables T01, T02, and T03 respectively were infected. The relationships among diners at T01, T02, and T03 are listed in Fig. S2. D9 had the earliest symptom onset date, January 2413. Three other infected diners D2, D4, and D8 at Table T1 might also be the source of the exposure as all diners in T01 came from Wuhan and the symptom onset dates for these three patients were also relatively early (before January 29, Fig. S1). There were 18 staff (coded from S1 to S18) who served in the restaurant, 8 of whom (S1 to S7, and S18) served a relatively longer period than others. The index case and her family at T01 stayed at the restaurant for 73 minutes (from 12:01 to 13:23), and the times of stay for all diners and staff are shown in Fig. S3.
Restaurant setting
The restaurant's dining dimensions are 17.5 m × 8.3 m × 3.1 m. There is a restroom, kitchen, elevator exit, emergency exit (stairs), reception desk, 18 tables (coded from T01 to T18), and some corridors (Fig. 1). No diner sat at T04 during the lunch. Among the round tables, T01, T09, T10, and T18 are the largest at 1.8 m diameter; T03, T13, and T15 to T17 are medium size at 1.6 m diameter, while T02, T11, and T14 are the smallest at 1.2 m diameter. Among the rectangular tables, T05 and T08 are 0.9 m × 0.9 m, while T06, T07, and T12 are 1.2 m × 0.9 m.
Data collection
All individuals could only be clearly seen and identified when they were walking in corridors or at their seats. Due to the camera view being blocked, eight un-infected diners D45-D50, D59, and D60 could not be seen and identified during the lunch time (Fig. 1). We collected 380,694 seconds of data on surface touch and close contact behaviors for 81 visible diners and 18 staff. Because some actions of people were obscured by themselves or other individuals, we finally collected 380,229, 292,621, and 317,823 seconds of valid data for contacts, touch actions by left hand, and touch actions by right hand, respectively. All video images were analyzed by six trained analysts. They processed the data second-by-second, recording all visible close contacts and surface touch behaviors in the restaurant. The video was played at normal speed (1 ×) and was paused every 1 second using PotPlayer 64 bit (http://potplayer.daum.net/). The six analysts typed the data into an Excel file (Table S1). The following comprise the data: time, individuals ID, surface touched by both hands, which surface was touched, whose contacts were normal/close/long, the location of each individual, mask-wearing, and hand-washing. No personal identification data such as age and sex were collected. The original videos were only accessed by the six trained analysts in strict confidence at Guangdong CDC. The study was approved by the Medical Research Ethics Review Committee of Guangdong Provincial Center for Disease Control and Prevention (approval No. W96-027E-202106).
All surfaces are divided into seven groups: mucous (M), hand (H), body (B), personal private object (PP), personal object provided by the restaurant for each table's use (PT, personal table's object), table object for all diners at the specific table (T, table's public object), object for public use for all people in the restaurant (R, restaurant's public object). Individual diners and staff had IDs for M, H, B, and PP; each diner had an ID for PT; and each table T had an ID. If a surface is only touched less than 100 seconds, which means few people seldom touched the surface, it was classified into ‘others’ because it is not an important surface in the restaurant. A total of 78 types of sub-surfaces are recorded in Table 1 and Fig. S4. We hypothesized that each object for public use in the restaurant is unique.
Table 1.
Surface introduction.
| Surface | Sub-surface | code | Sub-surface | code | Sub-surface | code |
|---|---|---|---|---|---|---|
| Mucous (M) | Eye | M1 | Mouth | M2 | Nose | M3 |
| Hand (H) | Left hand | H1 | Right hand | H2 | ||
| Body (B) | Head, face, neck | B1 | Other body part | B2 | ||
| Personal private object (PP) | Mobile phone | PP1 | Mask | PP2 | Tissue | PP3 |
| Scarf | PP4 | Overcoat | PP5 | Glasses (case) | PP6 | |
| Necklace | PP7 | Gift | PP8 | Bag | PP9 | |
| Bank card | PP10 | Money/wallet | PP11 | Cigarette | PP12 | |
| Water bottle | PP13 | Hand sanitizer (bottle) | PP14 | Baby cart | PP15 | |
| Walking stick | PP16 | Medical kit | PP17 | |||
| Umbrella | PP18 | Scissors | PP19 | Intercom | PP20 | |
| Pen | PP21 | Others | PP22 | |||
| Personal table's object (PT) | Tablecloth | PT1 | Chair | PT2 | Plate | PT3 |
| Bowl | PT4 | Cup | PT5 | Chopsticks | PT6 | |
| Spoon | PT7 | Toothpick | PT8 | Food | PT9 | |
| Table's public object (T) | To-go box/bag | T1 | Receipt/coupon | T2 | Chair | T3 |
| Lazy Susan | T4 | Table board | T5 | Table card | T6 | |
| Kettle | T7 | Tablecloth | T8 | Tissue (box) | T9 | |
| Chopsticks and spoon | T10 | Plate and bowl | T11 | Flower | T12 | |
| New tableware | T13 | Old tableware | T14 | |||
| New tablecloth | T15 | Others | T16 | |||
| Restaurant public object (R) | Chair | R1 | Sales report | R2 | Elevator button | R3 |
| Bottle opener | R4 | Drawer of reception desk | R5 | Cabinet handle | R6 | |
| Desk of reception | R7 | Computer in reception | R8 | |||
| POS machine | R9 | Door of emergency exit | R10 | |||
| Door curtain of kitchen | R11 | Window | R12 | |||
| Light switch | R13 | Menu | R14 | |||
| Tray for dishes | R15 | Trash cart | R16 | Trash can | R17 | |
| Rag | R18 | Broom | R19 | Dustpan | R20 | |
| Electric rice cooker | R21 | Rice ladle | R22 | New tableware | R23 | |
| Others | R24 |
Infection risk
In this study, we defined infection risk as the exposure to or intake volume of virus via fomite and close contact routes. We evaluated the relative infection risk for each individual in the restaurant except for those who could not be identified in the video. For example, if the relative infection risk of individual A is 5 times that of individual B, it means that A was exposed to or inhaled 4 times more virus volume than B. However, there is no specific definition of a unit volume of virus.
Because infection spread via the long-range airborne route in this restaurant has been thoroughly studied by other researchers16, we considered only close contact and fomite routes. The detailed infectious disease transmission model via fomite (Appendix A) and close contact (Appendix B) routes are introduced in Appendix and literatures18 , 21 , 22.
Although the index case D9 had the earliest symptom onset date, the three diners (D2, D4, D8) in T01 were also possible sources of exposure because all had come from Wuhan and had symptoms early. For our analysis to be comprehensive, we analyzed the infection risk via surface touch and close contact in the restaurant for 8 combinations of index patients (Table S3).
Results
Human surface touch behavior
We collected 40,935 valid touches for hands of both diners and staff. As shown in Table 2 , diners and staff on average spent 90.6% and 88.5% of their time respectively touching surfaces. Average touch frequency for both hands of diners and staff were 7.7 and 12.5 times per minute. Each diner on average touched surfaces of items belonging to 3.0 other individuals, while each staff touched surfaces of items belonging to 16.0 other individuals. In the restaurant, diners had most frequently touched objects provided by the restaurant for each diner's private use. Almost half of staff touches were on objects for public use on each table. Finally, 7.5% of diner touches and 1.3% of staff touches were on mucous surfaces. Diners and staff washed their hands 0.77 and 0.42 times per hour respectively.
Table 2.
Surface touch behavior of diners and staff.
| Parameter | Diner Mean (SD1) | Staff2 Mean (SD1) |
|---|---|---|
| Percent of time spent on surface touch (%) | 90.6 (6.5) | 88.5 (5.7) |
| Touch frequency of left hand (min−1) | 4.0 (1.4) | 4.1 (1.3) |
| Touch frequency of right hand (min−1) | 3.7 (1.3) | 8.4 (3.0) |
| No. of people2 connected by a private surface | 3.0 (1.8) | 16.0 (13.2) |
| Percent of touch related to M (%) | 7.5 | 1.3 |
| Percent of touch related to B (%) | 27.2 | 21.1 |
| Percent of touch related to PP (%) | 22.4 | 24.9 |
| Percent of touch related to PT (%) | 36.0 | 5 |
| Percent of touch related to T (%) | 6.7 | 45.1 |
| Percent of touch related to R (%) | 0.2 | 2.8 |
| Frequency of hand-washing | 0.77 | 0.42 |
3Number of other diners whose private items were touched.
SD: standard deviation.
Only staff who stayed more than 10 minutes were included.
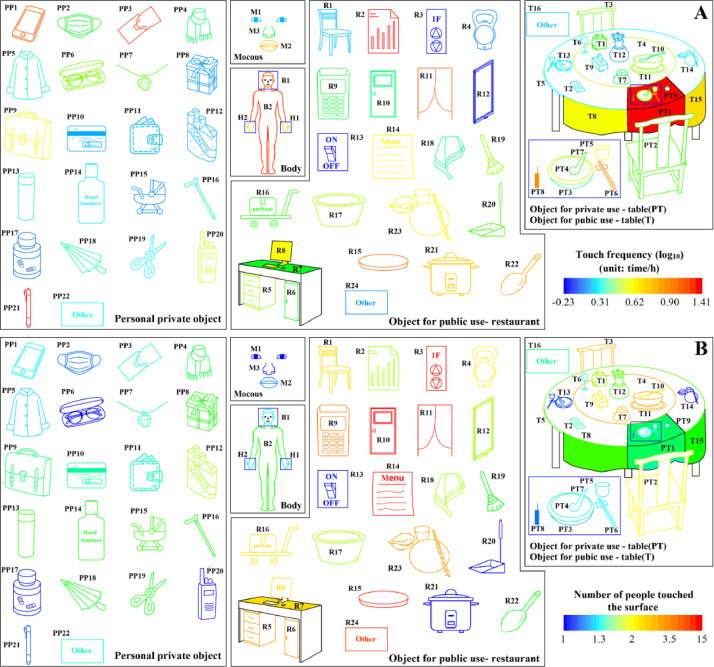
The average touch frequency on each sub-surface of mucous, hand, body, personal private object, private table's object, public table's object, and public restaurant's objects were 5.3, 9.3, 19.1, 5.8, 9.1, 4.7, and 7.8 times per hour, respectively (Fig. 2 A). Mobile phone, tissue (bag), pen, body, kitchen curtain, and tablecloth for private use had the highest touch frequencies. Each sub-surface of mucous, hand, body, personal private object, private table's object, public table's object, and public restaurant's object averagely touched by 1.1, 1.4, 1.7, 1.7, 1.6, 3.5, and 9.8 individuals (Fig. 2B). Elevator button, door of emergency exit, curtain of kitchen, and menu were touched by a large number of individuals.
Fig. 2.
Characteristics of surface touch classified by sub-surfaces: (A) touch frequency; (B) number of people who touched the surface. (Touch frequency () and average number of people ( who touched the sub-surface A is calculated by considering only the individual who had touched A: , where is the total number of people who had touched A during the statistical period, is the total number of touches on A by individual i, is the total valid time of individual i staying in the restaurant; , where is the total number of A in the restaurant.).
From the surface touch network, no diner touched the mucous, body, personal private objects of diners from other tables (Fig. 3 A). However, surfaces of items belonging to other individuals at the same table were sometimes touched. Six staff never touched personal objects of belonging to other staff, and some staff touched 6 other staff's items (Fig. 3B). Diners sitting at the same table had many interpersonal touches on personal table's objects (PT) (Fig. 3C). There were few touches by diners of other diners’ table surfaces, but some public table's surfaces, for example the chair closest to the narrow walking corridor (e.g. chair of diner D22 at Table T18 in Fig. 1) were frequently touched by diners from other tables. Some staff who served dishes for a table had several touches on a table's public objects (e.g. public serving dishes and spoons) (Fig. 3D). With respect to the restaurant's public objects (Fig. 3E), diners touched the elevator button (R3), the door of emergency exit (R10), and the menu (R14) most, while staff touched R10, the curtain of the kitchen (R11), R14, serving tray (R15), and new tableware (R23) the most. Detailed probability distribution of touches on M, H, B, PP, PT, and T are shown in Table 3 .
Fig. 3.
Surface touch network between (A) diners and personal surfaces (e.g. mucous, hand, body, and personal private objects) of diners; (B) staff and personal surfaces of staff; (C) individuals and private table objects; (D) individuals and public table objects; (E) individuals and public restaurant objects. (Circle, ellipse, and square show the individual, table, and public restaurant objects, respectively. Blue lines show that diners touched individual surfaces of diners sitting in the same table; red lines show diners touched individual surfaces of diners from other tables or touched the public table surfaces of other tables; blue numbers in (E) show the ID of public restaurant objects, which are shown in Fig. S4 and Table S2.
Table 3.
Probability distribution of touches on different surfaces.
| Surface | 1Diner touches (%) | 2Staff touches (%) | ||||||
|---|---|---|---|---|---|---|---|---|
| Self | Same table | Other table | Staff | Self | Diner | Other staff | ||
| M | 97.9 | 2.1 | 0 | 0 | 100.0 | 0 | 0 | |
| H | 94.1 | 5.9 | 0 | 0 | 99.3 | 0.4 | 0.4 | |
| B | 92.7 | 7.3 | 0 | 0 | 95.0 | 1.0 | 4.0 | |
| PP | 90.0 | 10.0 | 0 | 0 | 98.2 | 1.6 | 0.2 | |
| PT | 92.9 | 6.8 | 0.2 | 0.2 | 6.3 | 93.7 | 0 | |
| T | - | 98.9 | 1.1 | - | - | - | - | |
Self, same table, other table, and staff columns refer to what is touched: the person's own surface, the surface of an individual at the same table, the surface of individual at another table, and surface of a staff person, respectively.
Self, diner, and other staff columns refer to the staff touching his/her own surface, the surface of diners, and the surface of other staff, respectively.
Human close contact behavior
We collected 13,892 episodes of close contacts, of which 94.9% were close contacts (Table S4). 86.6%, 5.6%, and 7.8% of contacts happened between diner and diner, diner and staff, and staff and staff, respectively. Diners and staff on average spent 19.2% and 23.5% of their time in the restaurant in contact (Table 4 ). Diners and staff on average contacted 5.2 diners and 16.4 diners, respectively. The contact frequency of diners and staff were 2.2 and 2.6 times per minute, respectively. Among all contacts, 96.6% of contacts of diners and 76.0% of contacts of staff were close contacts. The average duration per contact of diners and staff were 5.5 s and 8.6 s, respectively. Diners wore masks 2.5% of the time, while staff wore masks 8.6% of the time.
Table 4.
Contact behavior of diners and staff.
| Parameter | Diner Mean (SD1) | Staff2 Mean (SD1) |
|---|---|---|
| No. of contacted diners | 5.2 (2.3) | 16.4 (12.0) |
| No. of contacted staff | 2.7 (2.0) | 10.4 (4.0) |
| Contact frequency with diner (times/min) | 2.1 (1.1) | 0.7 (0.6) |
| Contact frequency with staff (times/min) | 0.1 (0.1) | 1.9 (1.5) |
| Percentage of close contacts (%) | 96.6 (12.4) | 76.0 (25.2) |
| Duration per close contact (s) | 5.5 (2.4) | 8.6 (2.0) |
| Time spent on contact (percentage, %) | 19.2 (10.5) | 23.5 (16.8) |
| Time spent of mask wearing (percentage, %) | 2.5 | 8.6 |
SD: standard deviation.
Only staff who stayed more than 10 minutes were considered.
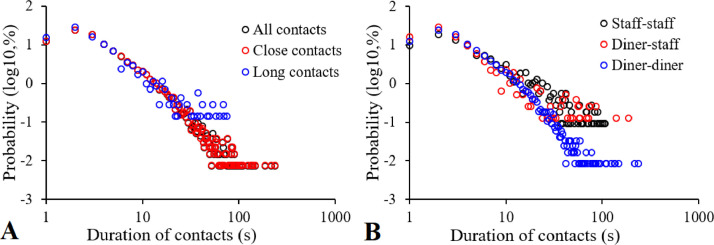
Close contacts were usually longer duration than long contacts (Fig. 4 A). Roughly 71% of close contacts and 77% of long contacts were no longer than 5 s. Only 0.5% of close contacts were longer than 1 minute. No long contact was longer than 80 s. Duration of contacts between diners were shorter than between staff (Fig. 4B). For interpersonal contacts, 73%, 76%, and 57% of contacts between diner-diner, diner-staff, and staff-staff were no longer than 5 s.
Fig. 4.
Probability distribution of duration per contact. (A) Close and long contacts; (B) between diner-diner, diner-staff, and staff-staff.
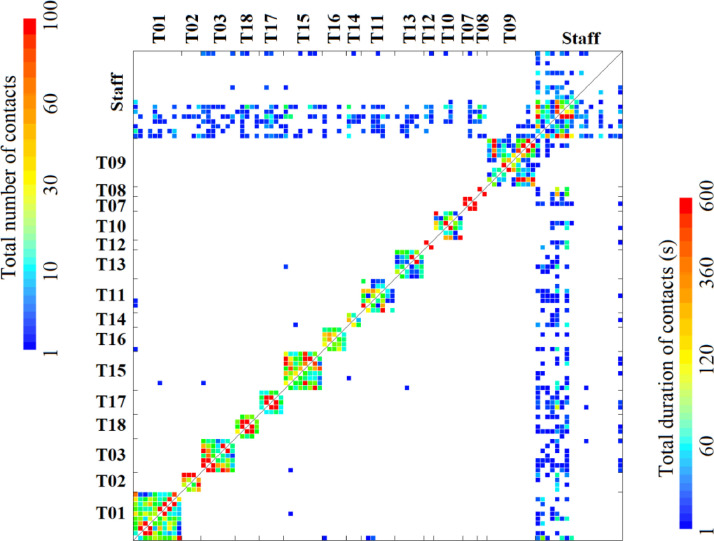
A contact matrix (Fig. 5 ) shows that there were almost no contacts between diners from different tables. Many grids near the diagonal line are red and orange showing that the diners had the most contact with the closest individuals. Almost all diners sitting at the same table had at least one episode of close contact. Some staff seldom contacted with diners but frequently contacted with staff. The time ratio for close contact slowly increased with increasing number of diners per table, but the total contact duration between two specific diners decreased significantly.
Fig. 5.
Close contact matrices of number of contacts (left-upper triangle) and total duration of contacts (right-bottom triangle) between two individuals. (ID of diners increases from bottom to top and from left to right on y and x axes, respectively. T01 to T18 are tables).
Infection risk via fomite and close contact routes
All diners and eight staff (S1, S3 to S8, S14) were contaminated via surface routes. Fig. 6 shows the virus absorption from mucous via surface routes under the condition of the index case pressing the elevator button when entering the restaurant, while Fig. S6 shows the results under the condition of susceptible diners pressing the button. No matter the identity of index patients, the virus absorption via the mucous route of diners in Table A is roughly 3,000 times higher than diners in other tables and 300 times higher than staff. D10 had the highest virus absorption of 0.10 unit volume, S7 had the highest virus absorption (2.8 × 10−4) of all staff, and D67 had the highest virus absorption (1.1 × 10−4) in all diners sitting at other tables (T02-T18).
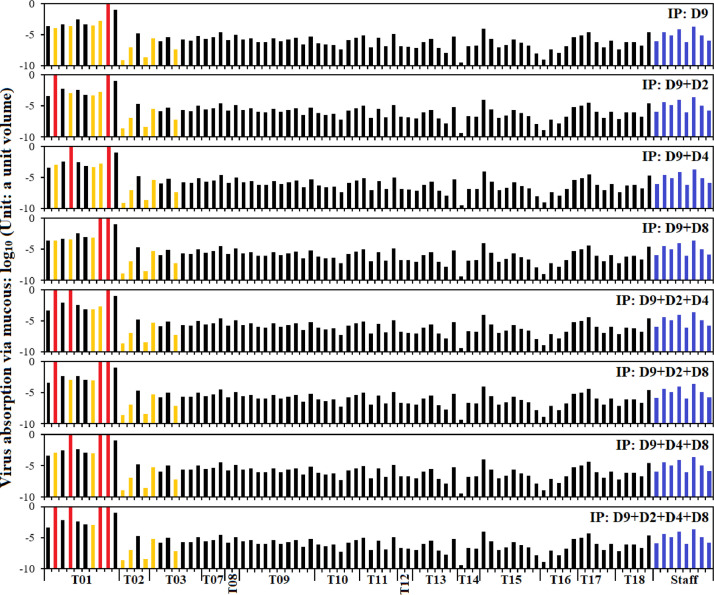
Fig. 6.
Virus absorption from mucous surface via fomite route under different combinations of possible index case (IP) (Fig. S3): the inside elevator button was touched by the index patient. (Red, yellow, black, and blue bars indicate possible index patient, secondary infected diner, non-infected diner, and staff, respectively).
There was no close contact between potential index patients (D9, D2, D4, D7, and D8) and diners from other tables. Only staff S1, S2, S4, S5, and S7 had close contacts with potential index patients, therefore, we only calculated the relative infection risk for five staff and 10 diners at T01 (Fig. 7 ). Except D2, who only frequently contacted with her daughter (D3), all potential index patients had the highest contact frequency with the two diners next to him/her. Compared to the relative infection risk of diners at T01, all staff had a very low infection risk. The average aerosol intake of diners at T01 is roughly 370 times higher than that of staff.
Fig. 7.
Aerosol intake (ml) via close contact routes for different combinations of index patients (IP) (Fig. S3). (Red, yellow, black, and blue bars show the index patient, secondary infected cases, and susceptible diners, and susceptible staff. Only D1 to D10 were shown because there was no close contact between diners in T01 and diners at other tables.).
After considering both fomite and close contact routes under 8 different combinations of index patients, we found no significant correlation between estimated relative infection risk and the reported infection data. Therefore, the COVID-19 outbreak in the restaurant was not transmitted via fomite, and/or close contact routes.
Discussion
In this study, we provide indirect evidence for the risk of indoor long-range airborne transmission of SARS-CoV-2 by ruling out other possible transmission routes, namely close contact (large droplets and short-range airborne) and fomites. Our evidence is based on video analysis of all activities during the time that one known index case and three possible index cases had lunch in a Guangzhou restaurant.
The possible transmission routes of SARS-CoV-2 are airborne, both short-range and long-range, short range droplets, and surface fomites[23], [24], [25]. Early in the COVID-19 pandemic, it was believed that contact with fomites plays a critical role in SARS-CoV-2 transmission because virus has a high stability on surfaces26 , 27. However, it has become increasingly clear that the fomite route is less important than previously thought28 , 29. Evidence has accumulated, especially since the outbreak of COVID-19, of the primacy of the airborne transmission route. The most important evidence of airborne transmission is that for long-range airborne transmission, especially in poorly ventilated indoor environments30 , 31. Such studies include analyses of COVID-19 outbreaks on a bus, a choir32 , 33, a cruise ship14 , 34, a gym[35], [36], [37], and a restaurant16. It has also become clear that poor ventilation augments long-range airborne transmission16 , 33 , 38 , 39.
Nonetheless, transmission by close contact and/or fomite routes cannot be ruled out in any of these reports. In the present study, we had video images from surveillance cameras with which to analyze the close contact and surface touch behaviors of both diners and staff, second by second. With analysis of this information, we can rule out both close contact and fomite routes, thus strengthening the argument for the long-range airborne route of SARS-CoV-2 transmission.
With respect to close contact, five staff had close contacts with index patients, but no staff became infected. There was no face-to-face contact between any two index patients (D9, D2, D4, D8) at T01 or with any of the five secondary cases at T02 and T03. For the five diners at tables other than the table with the known and possible index cases, transmission was by a route other than close contact. Any two diners walking by each other happens over such a brief time as to have a low probability for infection transmission.
The other possible route is via infectious material on surfaces, that is fomites. From the video images, all diners were exposed to potential fomite contaminated surfaces because all touched both potentially contaminated surfaces as well as their own mucous surfaces (e.g. eye, nostril, lip). In the surface touch network, all diners and 8 staff were connected by different types of surfaces. From the simulation, the virus absorption of five secondary infected diners at T02 and T03 via fomite route is 1/7 that of uninfected diners at T02 and T03, 1/5 of diners at other tables (T07 to T18), and 1/48 of staff (Fig. 6 and S6). That is, there was no significant correlation between virus absorption via the fomite route and infection status. In addition, after the outbreak, staff from Guangdong CDC collected 6 samples from surface of T01 and outlets of the air conditioning, and found all samples to be negative. By ruling out both close contact droplet and fomite transmission, we deduce that five secondary infected diners at T02 and T03, that is, seated at tables that included no index cases, were infected via the long-range airborne route.
In the Guangzhou restaurant, the ventilation rate was only 0.75–1.04 L/s per person16, which is much less than the Chinese40 (5 L/s per person) and ASHRAE41 (6-8 ACH per hour, 7.0-8.8 L/s per person in Guangzhou's restaurant) standard for restaurants. Low ventilation when there is an index patient results in the concentration of SARS-CoV-2 increasing over time. Thus, poor ventilation in the restaurant strengthens the case for the long-range airborne route dominating SARS-CoV-2 transmission in this restaurant.
Our data shows that only 7 (out of 11,778) episodes of close contacts happened between diners from different tables. Therefore, cross infection risk via the close contact route between diners from different tables is very small. However, close contacts between diners and staff were frequent, and the infection risk for diners might have been greater if a staff person had been infected. Guangzhou had started the highest-emergency response to COVID-19 on 24 January, 2020, requiring staff in restaurants were required to wear a mask at all times indoors. However, the staff wore masks only 8.6% of the time.
Surface touch is known to be to be a transmission route in viral diseases that can be spread by food ingestion, such as norovirus42. Staff would be a vector of virus transmission via the fomite route. For prevention of disease transmitted by fomites, hand-washing is essential. In the present study, the staff hand-washing frequency (0.42 time/h) appeared to be lower than that of the diners (0.77 time/h). However, staff hand-washing was likely under-counted, as the video does not contain hand-washing of the staff elsewhere (e.g. in the kitchen, outside the lunch floor and camera view).
There are some limitations in this study. First, although the five secondary cases at T02 and T03 can be shown to have been infected via long-range airborne, the same cannot be said for the infected family members at Table T01. This family had traveled together from Wuhan to Guangdong for sightseeing, and stayed in the same hotel in Guangzhou. Thus, they likely had frequent close contacts before and after the lunch in the restaurant, so that their transmission route cannot be confirmed. Second, the close-contact distance was assessed by referencing the location of diner's seats, which more precisely would be a range of values. Third, the virus exposure was assessed by using mechanistic modelling. Although the surface touch and close-contact data are accurate, other input data such as virus transfer rate during touch, the assumed amount of virus on root surfaces contaminated by the index case, the assumed of contact areas during touch etc would affect the predicted exposure.
Declaration of Competing Interests
The authors declare that they have no competing interests.
Acknowledgements
This work was supported by the Health and Medical Research Fund Commissioned Research on the Novel Coronavirus Disease (COVID-19) (No. COVID190113); the National Natural Science Foundation of China (No. 42005069); the National Natural Science Foundation of China (No. 82041030).
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jinf.2021.05.030.
Appendix. Supplementary materials
References
- 1.Morawska L, Tang JW, Bahnfleth W, Bluyssen PM, Boerstra A, Buonanno G. How can airborne transmission of COVID-19 indoors be minimised? Environ Int. 2020;142 doi: 10.1016/j.envint.2020.105832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Heller L, Mota CR, Greco DB. COVID-19 faecal-oral transmission: Are we asking the right questions? Sci Total Environ. 2020;729 doi: 10.1016/j.scitotenv.2020.138919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tian S, Hu N, Lou J, Chen K, Kang X, Xiang Z. Characteristics of COVID-19 infection in Beijing. J Infect. 2020;80(4):401–406. doi: 10.1016/j.jinf.2020.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhang N, Jia W, Lei H, Wang P, Zhao P, Guo Y. Effects of Human Behavior Changes During the Coronavirus Disease 2019 (COVID-19) Pandemic on Influenza Spread in Hong Kong. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa1818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Morawska L, Milton DK. It is time to address airborne transmission of coronavirus disease 2019 (COVID-19) Clin Infect Dis. 2020;71:2311–2313. doi: 10.1093/cid/ciaa939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.US CDC Scientific Brief . .; 2020. SARS-CoV-2 and potential airborne transmission.https://www.cdc.gov/coronavirus/2019-ncov/more/scientific-brief-sars-cov-2.html (accessed November 15, 2020) [Google Scholar]
- 7.World Health Organization . 2020. Coronavirus disease (COVID-19): How is it transmitted?https://www.who.int/news-room/q-a-detail/coronavirus-disease-covid-19-how-is-it-transmitted (accessed November 15, 2020) [Google Scholar]
- 8.Pray IW, Kocharian A, Mason J, Westergaard R, Meiman J. Trends in outbreak-associated cases of COVID-19-Wisconsin, March-November 2020. MMWR-Morb Mortal Wkly Rep. 2021;70:114. doi: 10.15585/mmwr.mm7004a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.US CDC (Centers for Disease Control and Prevention), Considerations for restaurant and bar operators. https://www.cdc.gov/coronavirus/2019-ncov/community/organizations/business-employers/bars-restaurants.html (accessed May 20, 2021)
- 10.Killeen BD, Wu JY, Shah K, Zapaishchykova A, Nikutta P, Tamhane A, et al. A county-level dataset for informing the United States' response to COVID-19. arXiv preprint arXiv:2004.00756, 2020. Available from: https://arxiv.org/abs/2004.00756v2
- 11.Guy GP, Jr, Lee FC, Sunshine G, McCord R, Howard-Williams M, Kompaniyets K. Association of state-issued mask mandates and allowing on-premises restaurant dining with county-level COVID-19 case and death growth rates—United States, March 1–December 31, 2020. MMWR-Morb Mortal Wkly Rep. 2021;70:350. doi: 10.15585/mmwr.mm7010e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Liu H, He S, Shen L, Hong J. Simulation-based study of COVID-19 outbreak associated with air-conditioning in a restaurant. Phys Fluids. 2021;33 doi: 10.1063/5.0040188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lu J, Gu J, Li K, Xu C, Su W, Lai Z. COVID-19 outbreak associated with air conditioning in restaurant, Guangzhou, China, 2020. Emerg Infect Dis. 2020;26:1628. doi: 10.3201/eid2607.200764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Almilaji O, Thomas P. Air recirculation role in the infection with COVID-19, lessons learned from Diamond Princess cruise ship. medRxiv. 2020 doi: 10.1101/2020.07.08.20148775. [DOI] [Google Scholar]
- 15.Tang S, Mao Y, Jones RM, Tian Q, Ji JS, Li N. Aerosol transmission of SARS-CoV-2? Evidence, prevention and control. Environ Int. 2020;144 doi: 10.1016/j.envint.2020.106039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Li Y, Qian H, Hang J, Chen X, Cheng P, Ling H. Probable airborne transmission of SARS-CoV-2 in a poorly ventilated restaurant. Build Environ. 2021;196 doi: 10.1016/j.buildenv.2021.107788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ma J, Qi X, Chen H, Li X, Zhang Z, Wang H. Coronavirus Disease 2019 Patients in Earlier Stages Exhaled Millions of Severe Acute Respiratory Syndrome Coronavirus 2 Per Hour. Clin Infect Dis. 2020;72:e652–e654. doi: 10.1093/cid/ciaa1283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhang N, Wang P, Miao T, Chan PT, Jia W, Zhao P. Real human surface touch behavior based quantitative analysis on infection spread via fomite route in an office. Build Environ. 2021;191 [Google Scholar]
- 19.Zhang N, Su B, Chan PT, Miao T, Wang P, Li Y. Infection spread and high-resolution detection of close contact behaviors. Int J Environ Res Public Health. 2020;17:1445. doi: 10.3390/ijerph17041445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhang N, Chen W, Chan PT, Yen HL, Tang JWT, Li Y. Close contact behavior in indoor environment and transmission of respiratory infection. Indoor Air. 2020;30:645–661. doi: 10.1111/ina.12673. [DOI] [PubMed] [Google Scholar]
- 21.Zhang N, Li Y. Transmission of influenza A in a student office based on realistic person-to-person contact and surface touch behaviour. Int J Environ Res Public Health. 2018;15(8):1699. doi: 10.3390/ijerph15081699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chen W, Zhang N, Wei J, Yen HL, Li Y. Short-range airborne route dominates exposure of respiratory infection during close contact. Build Environ. 2020;176 doi: 10.1016/j.buildenv.2022.109166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Huang L, Zhang X, Zhang X, Wei Z, Zhang L, Xu J. Rapid asymptomatic transmission of COVID-19 during the incubation period demonstrating strong infectivity in a cluster of youngsters aged 16-23 years outside Wuhan and characteristics of young patients with COVID-19: A prospective contact-tracing study. J Infect. 2020;80(6):e1–e13. doi: 10.1016/j.jinf.2020.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sia SF, Yan LM, Chin AWH, Fung K, Choy KT, Wong AYL. Pathogenesis and transmission of SARS-CoV-2 in golden hamsters. Nat. 2020;583:834–838. doi: 10.1038/s41586-020-2342-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Feng B, Xu K, Gu S, Zheng S, Zou Q, Xu Y. Multi-route transmission potential of SARS-CoV-2 in healthcare facilities. J Hazard Mat. 2020;402 doi: 10.1016/j.jhazmat.2020.123771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pastorino B, Touret F, Gilles M, de Lamballerie X, Charrel RN. Prolonged infectivity of SARS-CoV-2 in fomites. Emerg Infect Dis. 2020;26:2256–2257. doi: 10.3201/eid2609.201788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bloise I, Gómez-Arroyo B, García-Rodríguez J. Detection of SARS-CoV-2 on high-touch surfaces in a clinical microbiology laboratory. J Hosp Infect. 2020;105:784–786. doi: 10.1016/j.jhin.2020.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mondelli MU, Colaneri M, Seminari EM. Low risk of SARS-CoV-2 transmission by fomites in real-life conditions. Lancet Infect Dis. 2020 doi: 10.1016/S1473-3099(20)30678-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Goldman E. Exaggerated risk of transmission of COVID-19 by fomites. Lancet Infect Dis. 2020;20:892–893. doi: 10.1016/S1473-3099(20)30561-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lee J, Lee YH, Chang HH, Choi SH, Seo H, Yoo SS. Comparison of short-term mortality between mechanically ventilated patients with COVID-19 and influenza in a setting of sustainable healthcare system. J Infect. 2020;81(2):e76. doi: 10.1016/j.jinf.2020.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Favre G, Pomar L, Qi X, Nielsen-Saines K, Musso D, Baud D. Guidelines for pregnant women with suspected SARS-CoV-2 infection. Lancet Infect Dis. 2020;20:652–653. doi: 10.1016/S1473-3099(20)30157-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Charlotte N. High rate of SARS-CoV-2 transmission due to choir practice in France at the beginning of the COVID-19 pandemic. J Voice. 2020 doi: 10.1016/j.jvoice.2020.11.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Miller SL, Nazaroff WW, Jimenez JL, Boerstra A, Buonanno G, Dancer SJ. Transmission of SARS-CoV-2 by inhalation of respiratory aerosol in the Skagit Valley Chorale superspreading event. Indoor Air. 2021;31:314–323. doi: 10.1111/ina.12751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Xu P, Qian H, Miao T, Yen HL, Tan H, Kang M. Transmission routes of Covid-19 virus in the Diamond Princess cruise ship. medRxiv. 2020 doi: 10.1101/2020.04.09.20059113. [DOI] [Google Scholar]
- 35.Bae S, Kim H, Jung TY, Lim JA, Jo DH, Kang GS. Epidemiological characteristics of COVID-19 outbreak at fitness centers in Cheonan, Korea. J Korean Med Sci. 2020;35:e288. doi: 10.3346/jkms.2020.35.e288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Jang S, Han SH, Rhee JY. Cluster of coronavirus disease associated with fitness dance classes, South Korea. Emerg Infect Dis. 2020;26:1917–1920. doi: 10.3201/eid2608.200633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hamner L. High SARS-CoV-2 attack rate following exposure at a choir practice—Skagit County, Washington, March 2020. MMWR-Morb. Mortal Wkly Rep. 2020;69:606–610. doi: 10.15585/mmwr.mm6919e6. [DOI] [PubMed] [Google Scholar]
- 38.Jones NR, Qureshi ZU, Temple RJ, Larwood JPJ, Greenhalgh T, Bourouiba L. Two metres or one: what is the evidence for physical distancing in covid-19? BMJ. 2020;370:m3223. doi: 10.1136/bmj.m3223. [DOI] [PubMed] [Google Scholar]
- 39.Chen Y, Wang Y, Wang H, Hu Z, Hua L. Controlling urban traffic-one of the useful methods to ensure safety in Wuhan based on COVID-19 outbreak. Safety Sci. 2020;131 doi: 10.1016/j.ssci.2020.104938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.GB 50736-2012. Design Code for Heating Ventilation and Air Conditioning of Civil Buildings. Published on August 1, 2012.
- 41.ASHRAE . 2016. ANSI/ASHRAE Standard 62.2-2016 Ventilation for acceptable indoor air quality in residential buildings. Atlanta, GA, USA. [Google Scholar]
- 42.Eigner U, Verstraeten T, Weil J. Decrease in Norovirus infections in Germany following COVID-19 containment measures. J Infect. 2021 doi: 10.1016/j.jinf.2021.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.