Abstract
Purpose
Inflammatory bowel diseases (IBD), including Crohn’s disease (CD) and ulcerative colitis (UC), are chronic diseases. The aim was to validate diagnoses of IBD among patients aged 50+ years in the Danish National Patient Registry (NPR) by comparison with patient medical records.
Patients and Methods
Men and women in the Diet, Cancer and Health (DCH) cohort were linked to NPR, and cases with a diagnosis of IBD and their respective hospital records were identified. Validation was performed by comparing patient medical records with information on discharge diagnoses of IBD from the NPR.
Results
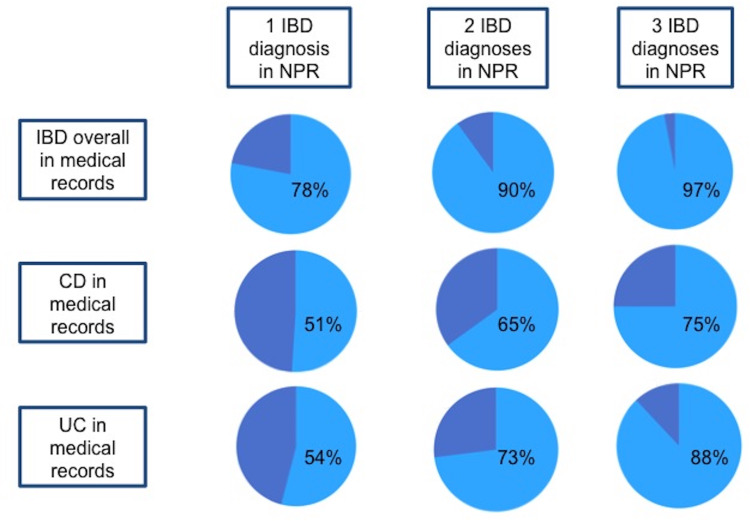
Of 57,053 individuals in the DCH-cohort, 339 were registered with an IBD diagnosis in NPR, with 277 (82%) records available for review. Among 277 patients, the positive predictive values (PPVs) of one CD or UC registration in NPR were 78% for IBD overall, 51% for CD and 54% for UC. One hundred fifty-seven patients had at least two CD and/or UC registrations with PPVs of 90% for IBD overall, 65% for CD and 73% for UC. One hundred and two patients had at least three registrations with PPVs of 97% for IBD overall, 75% for CD and 88% for UC. 96% were diagnosed at a specialized department. Other diagnoses coded as IBD mostly included microscopic colitis, irritable bowel syndrome and cancer.
Conclusion
Validity of IBD diagnoses in the registry of individuals aged 50+ years increased with the number of registrations. It is recommended that these results are taken into consideration in future studies, especially in epidemiology research using NPR as a data source for patients diagnosed with IBD.
Keywords: inflammatory bowel disease, Danish National Patient Registry, register study, diagnostic accuracy, diagnosis
Plain Language Summary
The authors evaluated diagnoses of inflammatory bowel disease among patients aged 50 years or more registered in the Danish National Patient Registry. We evaluated the diagnoses according to the diagnostic criteria of ulcerative colitis and Crohn’s disease by reviewing the patient's medical records.
Inflammatory bowel diseases are chronic diseases and numerous epidemiological studies are being conducted in this field. In epidemiological studies, investigators use national registers, and the quality of the research depends on the accuracy of the registered diagnoses. A direct comparison of diagnoses on an individual level between the Danish National Patient Registry and medical records has not been done before, and it can be challenging to discriminate inflammatory bowel disease from other gastrointestinal diseases among elderly patients.
We calculated the positive predictive value of one, at least two or at least three registrations in the Danish National Patient Registry. We found that:
The positive predictive value of one registered diagnosis was low but increased with the number of registrations.
At least three registrations resulted in a positive predictive value of 97% for inflammatory bowel disease overall, 75% for Crohn’s disease and 88% for ulcerative colitis.
Several patients had a diagnosis of microscopic colitis or other diagnoses, such as cancer, and the risk of these diseases increases with age.
In conclusion, we recommend that investigators consider these results in future epidemiological studies of inflammatory bowel disease to make sure that the diagnoses extracted from these registers are as reliable as possible.
Introduction
Inflammatory bowel diseases (IBD) include Crohn’s disease (CD), ulcerative colitis (UC), and microscopic colitis (MC). They are chronic diseases with increasing incidences in Western Europe around 7/100.000 for CD and 10/100.000 for UC.1,2
IBD is a multifactorial disease in which an inflammatory response occurs in genetically disposed individuals when exposed to environmental and microbiological risk factors. IBD often has its onset in early adulthood.2,3 Numerous epidemiological studies on IBD have added to the information on IBD, eg identified risk factors for developing IBD and the consequences of IBD, including long-term risk of colorectal cancer.4–6
A prerequisite for epidemiology research are registers, such as the Danish National Patient Registry (NPR), and the quality of research depends on the accuracy of hospital discharge diagnoses of IBD.7,8 In a previous validation study, the NPR showed a high consistency of 97% and 90% for CD and UC diagnoses, respectively, with histopathological reports from the Danish Pathology Registry.9 Two Danish studies of pregnant women with CD and UC reported lower positive predictive values (PPV) of 86% and 89%, respectively, when comparing IBD diagnoses from NPR with medical records.10−12 However, a direct comparison at the individual level between IBD diagnoses in NPR and diagnostic criteria in patient medical records has never been conducted. Discriminating IBD from other differential diagnoses among older individuals at risk of other gastrointestinal diseases may be challenging.
Therefore, the aim of this study was to validate IBD diagnoses among patients above the age of 50 in the NPR by comparison with patient medical records from hospitals.
Patients and Methods
This is a validation study of IBD diagnoses given in the Diet, Cancer and Health study (DCH-cohort) and NPR.13 The study uses register data in combination with manual scrutiny of patient medical records.
Study Population
The study was based on patients enrolled in the DCH-cohort. The study design and baseline data for this study cohort have been reported earlier.13 In brief, recruitment was carried out between 1993 and 1997, and 57.053 people (29.875 women, 27.178 men) born in Denmark, living in Copenhagen or Aarhus, aged 50–64 years with no previous cancer diagnosis were enrolled and gave written consent.13
Data Sources
Danish National Registries
All Danish individuals are assigned a unique personal identification number (CPR number), and data from national registers can therefore be linked at an individual level.8 The NPR was used to obtain information on the participants diagnosed with IBD in the DCH-cohort. The NPR contains data on all patients admitted to Danish hospitals since 1977.7 The register covers both inpatient and outpatient records and indicates the main medical reason for diagnostic procedures or treatment. Since 1994, the 10th revision of ICD (ICD-10) has been used.
The following ICD-10 codes for CD were used; K50.0, K50.0A, K50.0B, K50.0C, K50.0D, K50.1, K50.1D, K50.8, K50.8A, K508C, K50.8D and K50.9, and ICD-8 codes; 563.00; 563.01; 563.02; 563.08; 563.09. The following ICD-10 codes for UC were used; K51.0, K51.2, K51.3, K51.4, K51.5, K51.5A, K51.5B, K51.8, K51.8B and K51.9, and ICD-8 codes; 563.19 and 569.04. Data extraction from the NPR occurred on July 25th 2013, to identify the DCH-cohort patients with a first diagnosis of CD and UC from 1998 to 2013. An additional extraction occurred on October 2nd 2015 of all the main IBD diagnoses registered for each patient in this study, to identify which patients had more than one registration of IBD and the number of registrations for each patient.
Patient Records
Hospital identifiers and CPR numbers were used to retrieve information from the NPR to identify patients in hospital systems. Patients were excluded if the medical records could not be located or retrieved from hospital departments or lacked relevant information.
Electronic and paper medical records were reviewed for the period of March–August 2015.
Information on the patient’s sex, age at diagnosis, location of disease in the gastrointestinal tract according to the Montreal Classification,14 symptoms of IBD, gastrointestinal complications, extra intestinal manifestations, and measures such as endoscopy descriptions, radiological features and pathology reports to identify if the Copenhagen Diagnostic Criteria15–17 were fulfilled, were extracted.
Validation
Both the first and last authors reviewed twenty cases under training and all complicated cases. Since there were no disagreements under training, cases were only discussed with the last authors, when the first author was in doubt about the diagnosis.
After a review of the patient's medical records, patients were placed into one of five groups:
Documentation for the Copenhagen Diagnostic Criteria15–17 was presented, and the physician who treated the patient agreed with the diagnosis.
Diagnosis was compatible with IBD: The diagnosis “CD” or “UC” was found in the medical record, but documentation for fulfilment of diagnostic criteria (eg detailed endoscopic description) was not presented.
Undifferentiated IBD (IBDu): The diagnosis was “IBD”, but it was not possible to distinguish between CD and UC on the basis of the medical record.
Diagnosis of microscopic colitis (MC).
Not IBD: The patient was not diagnosed with IBD in the medical record and the diagnostic criteria were not fulfilled.
Groups 1–4 were considered true IBD cases, while group 5 was considered non-cases.
Within the study period, registration of MC in NPR was challenging due to no specific MC ICD-10 code, which could lead to a higher rate of misclassifications. To take this into account, the IBD registrations were validated in two settings; with MC patients included as cases and as non-cases.
If a patient had a change in diagnosis (for example, from UC to CD), we used the first diagnosis in the patient medical record when calculating the PPV of a first registration. When performing the analysis using the criteria of several registrations, the latest diagnosis was used to reflect the medical record history. Two months after the initial diagnosis of IBD, two patients, of whom only one fulfilled the diagnostic IBD-criteria, were diagnosed with a gastrointestinal cancer and hence classified as non-cases in the present study.
Statistical Analyses
Descriptive results are presented as median and quartiles (25% and 75%) for continuous data and as counts and percentages for categorical data.
The validity of the NPR was calculated and presented as PPV with 95% CI. PPV was defined as the proportion of patients in NPR with a confirmed diagnosis of CD or UC in the medical records. We calculated the PPV of IBD overall and of CD and UC separately.
The PPV of having at least one, two and three registrations of CD and/or UC and the PPV of having a registration from a specialized department, which included departments of internal medicine, gastroenterology and abdominal surgery, were also calculated.
The PPV of having IBD overall with and without inclusion of MC cases was calculated.
A sensitive analysis was performed excluding patients with a registration of IBD in the NPR at least one year prior or after the diagnosis date in the patient's medical records.
Statistical analyses were performed using the 15th version of STATA®.
Results
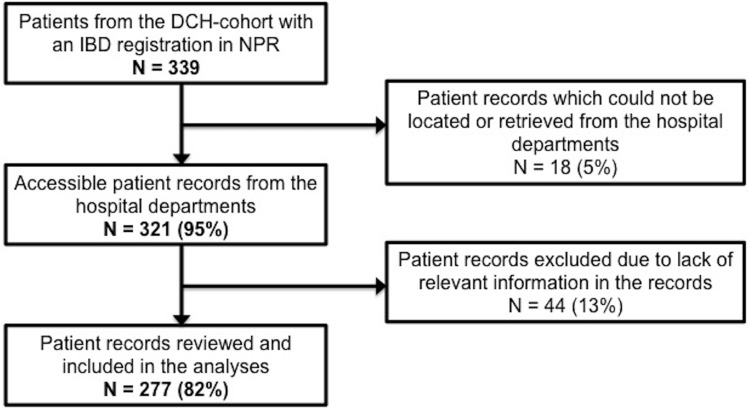
In the DCH-cohort, a total of 339 patients had a first registration of CD or UC during 1998–2013 in the NPR. Medical records could not be located or retrieved from hospital departments in 18 (5%) cases, and thus were excluded. Further, 44 (13%) patients were excluded due to lack of relevant information in the medical records. Thus, 277 patient medical records (82%) were available for reviewing and included in the analyses (Figure 1).
Figure 1.
Flowchart.
Abbreviations: IBD, inflammatory bowel disease; NPR, the Danish National Patient Registry
Baseline Characteristics
A total of 61 (22%) patients had a first registration of CD in the NPR and 216 (78%) had a first registration of UC. Baseline characteristics from NPR are shown in Table 1 and from the medical records in Table 2. Thirteen patients (5%) changed diagnosis according to the medical records; four from CD to UC, two from UC to CD, one from UC to IBDu, one from CD to MC, one from UC to MC, one from CD to peridiverticulitis and three from UC to diverticulitis.
Table 1.
Baseline Characteristics of the 277 Participants Based on Information from the NPR
| First NPR Diagnosis | IBD N=277 N(%) |
CD N=61 N(%) |
UC N=216 N(%) |
|---|---|---|---|
| Sex | |||
| Female | 156 (56) | 38 (62) | 118 (55) |
| Male | 121 (44) | 23 (38) | 98 (45) |
| Age at diagnosisa | |||
| Median [Q1 + Q3] Range |
68 [64, 72] 57, 79 |
69 [64, 72] 53, 82 |
|
| Patients with diagnostic codes referring to specific location in the gastrointestinal tractb | 126 (46) | 19 (31) | 108 (50) |
Notes: aAge is missing from three patients. bK50.0, K50.0D, K50.1. K51.0, K51.1, K51.2, K51.2A, K51.3, K51.5, K518A.
Abbreviations: NPR, the Danish National Patient Registry; IBD, inflammatory bowel disease; CD, Crohn’s disease; UC, ulcerative colitis.
Table 2.
Baseline Characteristics of the 277 Participants Based on Information from Patient Records
| First Diagnosis in the Patient Records | Total N=277 N(%) |
CD N=37 N(%) |
UC N=120 N(%) |
MC N=56 N(%) |
IBDu N=4 N(%) |
Other N=54 N(%) |
Unknown N=6 N(%) |
|---|---|---|---|---|---|---|---|
| Sex | |||||||
| Female | 156 (56) | 27 (73) | 47 (39) | 48 (86) | 2 (50) | 27 (50) | 5 (83) |
| Male | 121 (44) | 10 (27) | 73 (61) | 8 (14) | 2 (50) | 27 (50) | 1 (17) |
| Location at diagnosisa,b: | 143 (52) | 35 (95) | 108 (90) | ||||
| L1 ilieal | 9 (26) | ||||||
| L2 colonic | 18 (51) | ||||||
| L3 ileocolonic | 6 (17) | ||||||
| L1+ L4 | 1 (3) | ||||||
| L2 + L4 | 1 (3) | ||||||
| E1 rectum | 26 (24) | ||||||
| E2 left sided, distal | 54 (50) | ||||||
| E3 extensive, pancolitis | 28 (26) |
Notes: L4: Isolated upper disease. aAccording to Montreal Classification. bExcluding 1 UC patient with the disease located to both sigmoid colon and ascending colon.
Abbreviations: CD, Crohn’s disease; UC, ulcerative colitis; MC, microscopic colitis; IBDu, undifferentiated inflammatory bowel disease.
Among the 54 patients (aged 59–79) in the category “Other diagnosis” in Table 2, the majority, 12 patients (22% of “Other diagnosis”, 4% of the study group), had a diagnosis of chronic diarrhea/obstipation or irritable bowel syndrome (IBS), while 10 (19% of “Other diagnosis”, 3.6% of the study group) were diagnosed with cancer, 10 (19% of “Other diagnosis”, 3.6% of the study group) with gastroenteritis and 6 (11% of “Other diagnosis”, 2% of the study group) with drug-induced symptoms or iatrogenic complications in the medical records.
The remaining 16 (30% of “Other diagnosis”, 6% of study group) had either or a combination of diverticulitis, bowel ischemia, ventricular ulcer, perianal abscess/fistulas, bile acid malabsorption, bacterial overgrowth, rectal prolapse/bleeding and/or pseudomembranous colitis.
Disease location/extent was registered in 31% and 50% of the CD and UC cases in NPR, respectively (Table 1), and in 95% and 90% of the CD and UC cases in the patient records, respectively (Table 2).
Validity of IBD Diagnosis in the NPR
The validity of the IBD diagnosis in the NPR was evaluated using the diagnosis of the medical records as the standard. In Table 3, the PPV is calculated for a first registration in the NPR and according to different criteria of retrieving data from NPR. Figure 2 shows the graphical abstract for a graphical presentation of the results.
Table 3.
Validity of the Diagnostic Codes for IBD, CD and UC in the NPR Using Number of Hospital Admissions/Out-Patient Clinic Visits with a Main Discharge Diagnosis Registered in the NPR as Criteria
| No. of Cases According to NPR | No. of Confirmed Cases in the Patient Record | No. of Cases Lost Compared to Using 1 Diagnosis as Criteria | PPV (95% CI) | |
|---|---|---|---|---|
| Including MC as IBD casea | ||||
| At least one diagnosis of IBD Female Male |
277 156 121 |
217 124 93 |
– – – |
0.78 (0.73–0.83) 0.80 (0.72–0.86) 0.77 (0.68–0.84) |
| At least 2 diagnoses of IBD | 157 | 141 | 76 | 0.90 (0.84–0.94) |
| At least 3 diagnoses of IBD Female Male |
102 45 57 |
99 43 56 |
118 81 37 |
0.97 (0.92–0.99) 0.96 (0.85–1.00) 0.98 (0.91–1.00) |
| Excluding MC as caseb | ||||
| At least one diagnosis of IBD Female Male |
277 156 121 |
161 76 85 |
– – – |
0.58 (0.52–0.64) 0.49 (0.41–0.57) 0.70 (0.61–0.78) |
| At least 2 diagnoses of IBD | 157 | 123 | 38 | 0.78 (0.71–0.85) |
| At least 3 diagnoses of IBD Female Male |
102 45 57 |
94 39 55 |
67 37 30 |
0.92 (0.85–0.97) 0.87 (0.73–0.95) 0.97 (0.88–1.00) |
| CD | ||||
| At least one diagnosis of CD Female Male |
61 38 23 |
31 23 8 |
– – – |
0.51 (0.38–0.64) 0.61 (0.43–0.76) 0.35 (0.16–0.57) |
| At least 2 diagnoses of CD | 37 | 24 | 7 | 0.65 (0.48–0.80) |
| At least 3 diagnoses of CD Female Male |
28 18 10 |
21 15 6 |
10 8 2 |
0.75 (0.55–0.89) 0.83 (0.59–0.96) 0.60 (0.26–0.88) |
| UC | ||||
| At least one diagnosis of UC Female Male |
216 118 98 |
117 47 70 |
– – – |
0.54 (0.47–0.61) 0.40 (0.31–0.49) 0.71 (0.61–0.80) |
| At least 2 diagnoses of UC | 124 | 91 | 26 | 0.73 (0.65–0.81) |
| At least 3 diagnoses of UC Female Male |
74 27 47 |
65 20 45 |
52 27 25 |
0.88 (0.78–0.94) 0.74 (0.54–0.89) 0.96 (0.86–0.99) |
Notes: a Using patients with a diagnosis of CD, UC, IBDu and MC in the patient records as cases. b Using patients with a diagnosis of CD, UC and IBDu in the records as cases.
Abbreviations: IBD, inflammatory bowel disease; CD, Crohn’s disease; UC, ulcerative colitis; NPR, the Danish National Patient Registry; IBDu, undifferentiated IBD; MC, microscopic colitis; PPV, positive predictive value; CI, confidence interval.
Figure 2.
Validity of diagnoses of IBD in the NPR among patients more than 50 years of age: review of 277 patient records.
Abbreviations: IBD, inflammatory bowel disease; NPR, the Danish National Patient Registry.
At Least One IBD Registration in NPR
Including MC patients as true IBD cases: The PPV of at least one IBD diagnosis (including CD, UC, IBDu or MC) in the NPR was 78% (73–83%) compared to the diagnoses made from review of the medical records. The PPV of one registration of IBD was 80% (72–86%) among females and 77% (68–84%) among males.
Excluding MC patients as true IBD cases: The PPV of one registration of CD or UC in NPR was 58% (52–64%) for having a diagnosis of either CD, UC or IBDu in the medical records. PPV for having one registration of IBD was 49% (41–57%) among females and 70% (61–78%) among males.
CD and UC: The PPV of one registration in NPR of CD was 51% (38–64%) for having a diagnosis of CD in the medical records, while the PPV of one registration in NPR of UC was 54% (47–61%) for having a diagnosis of UC in the medical records. Among females, the PPV of the first CD registration in the NPR was 61% (43–76%) for having CD in the records, while the PPV of a first registration of UC was 40% (31–49%) for having UC. Among males, the PPV of the first CD registration was 35% (16–57%) for having CD, while the PPV of the first registration of UC was 71% (61–80%) for having UC in the records.
Excluding the patients with a registration in the NPR more than one year before or after the diagnosis date in the patient medical records, the PPV was 76% (70–82%) for IBD including MC as cases, 55% (49–62%) for IBD excluding MC as cases, 50% (36–64%) for CD and 49% (42–57%) for UC (not shown in table).
In Table 4, the PPV of having IBD is calculated if the patient had a registration from a specialized department. The PPV was 79% (74–84%) for having IBD including MC as cases, 58% (52–64%) for having IBD excluding MC as cases, 50% (36–64%) for having CD and 54% (47–67%) for having UC.
Table 4.
Validity of the Diagnostic Codes for IBD, CD and UC in the NPR Using Department Specialization as Criteria, Including Abdominal Surgical Departments as Specialized Departments of Gastroenterology
| Diagnosis Department Specialization |
No. of Cases According to NPR with at Least One Registration | No. of Confirmed Cases | PPV (95% CI) |
|---|---|---|---|
| Including MC as IBD casea Departments of internal medicine, surgery or gastroenterology Other/unknown |
266 |
210 |
0.79 (0.74–0.84) |
|
11 |
7 |
0.64 (0.31–0.89) |
|
| Excluding MC as caseb Departments of internal medicine, surgery or gastroenterology Other/unknown |
266 |
154 |
0.58 (0.52–0.64) |
|
11 |
7 |
0.64 (0.31–0.89) |
|
| CD Departments of internal medicine, surgery or gastroenterology Other/unknown |
56 |
28 |
0.50 (0.36–0.64) |
|
5 |
3 |
0.60 (0.15–0.95) |
|
| UC Departments of internal medicine, surgery or gastroenterology Other/unknown |
210 |
113 |
0.54 (0.47–0.67) |
|
6 |
4 |
0.67 (0.22–0.96) |
Notes: a Using patients with CD, UC, IBDu and MC in the patient records as cases.
bUsing patients with CD, UC and IBDu in the records as cases.
Abbreviations: NPR, the Danish National Patient Registry; IBD, inflammatory bowel disease; CD, Crohn’s disease; UC, ulcerative colitis; IBDu, undifferentiated IBD; MC, microscopic colitis; PPV, positive predictive value; CI, confidence interval.
At Least Three IBD Registrations in NPR
Including MC patients as true cases: The PPV of at least three registrations in NPR of CD and/or UC was 97% (92–99%) for having CD, UC, IBDu or MC in the records. The PPV for having at least three registrations of IBD was among females 96% (85–100%) and 98% (91–100%) among males.
Excluding MC patients as cases: The PPV of at least three registrations in NPR of CD and/or UC was 92% (85–97%) for having CD, UC or IBDu in the records. The PPV for having at least three registrations of IBD was among females 87% (73–95%) and 97% (88–100%) among males.
CD and UC: The criteria of having at least three registrations of CD increased the PPV to 75% (55–89%) for having CD in the records. The PPV of having at least three registrations of UC was 88% (78–94%) for having UC in the records. Among females, the PPV of at least three registrations of CD in the NPR was 83% (59–96%) for having CD in the records, while the PPV of at least three registrations of UC was 74% (54–89%) for having UC. Among males, the PPV of at least three registrations of CD was 60% (26–88%) for having CD, while the PPV of at least three registrations of UC was 96% (86–99%) for having UC in the records.
Discussion
In this register study, the validity of having a diagnosis of IBD in NPR among patients above 50 years of age was evaluated. The medical records of all the patients were reviewed and included patients as IBD cases if they had IBD according to the treating physician. For cases having one registration in NPR, the PPV was 51% for CD, 54% for UC, and 78% for IBD overall. The PPV was improved by the number of registrations, and for cases having at least three registrations in NPR the PPV was 75% for CD, 88% for UC and 97% for IBD overall.
The validity of the IBD diagnosis in NPR has been evaluated in other Danish studies.9–12 Fonager et al reported a PPV of 97% (CD) and 92% (UC) when comparing the NPR with the pathological reports.9 However, in contrast to the present study, Fonager et al only reviewed patient medical records if there were inconsistencies between the NPR and the pathological reports. Further, by comparing NPR diagnosis to pathological samples only, erroneous diagnoses or diagnoses where endoscopic procedures were not successful were not included. Furthermore, Julsgaard et al found PPVs of 86% for CD and 89% for UC among a group of CD (154, median age 30) and UC (115, median age 31) women, respectively.10−12 These women were selected based on giving birth between 2000 and 2005 and diagnosed more than 1 year prior to conception. The patients were identified by combining the Regional Patient Administrative System (that transfers data to NPR) with the Danish Medical Birth Registry, and the diagnoses were confirmed by review of the patient medical record for each patient by a specialist at the respective hospital. The number of IBD registrations in NPR was not stated. In the present study, when the criteria of at least three registrations was applied, the PPV was similar to the PPVs in the studies by Julsgaard et al with 75% for CD and 88% for UC. The age of the women and thereby the year of diagnosis in the study by Julsgaard et al may explain the higher PPV compared to the present study.
Various methods for improving the PPV have been suggested. Using at least two registrations in the Swedish Quality Register for IBD (SWIBREG) lead to PPVs of 72%, 79% and 93% for CD, UC and any IBD, respectively, which supports the present study.18 Similarly, in a Canadian study, Benchimol et al found that five physician contacts or hospitalizations within four years were the most accurate algorithm to identify IBD patients aged 18 to 64 years at diagnosis, while incorporating pharmacy claim for IBD-related medication improved the accuracy for patients ≥65 years old.19 Furthermore, Rezaie et al reported that having at least two hospitalizations, four physician claims or two contacts in the Ambulatory Care Classification System database (ACCS) with an IBD diagnostic code within a two-year period qualified for an IBD diagnosis.20 Although an additional pharmacy claim may have improved the PPV, no such data were provided.
Another strategy to improve the PPV in data from NPR may be to require an IBD diagnosis from a specialized department. For example, in a Danish registry study with a similar design as in the present study, the PPV for diagnosing acromegaly increased from 40% (34.4–45.9) to 53% (46.4–59.8) when restricted to cases diagnosed by a specialized department.21 Two other validation studies using the NPR, Lasota et al and Delekta et al, also found a significantly higher PPV when they used diagnoses from specialized departments.22,23 However, in the present study, restriction of the criteria to cases diagnosed at specialized departments according to the NPR did not improve the PPV most likely because nearly all cases (266, 96%) were diagnosed at specialized departments. Similarly, requiring a diagnosis from an internal medicine/gastroenterology/surgery department did not improve the prevalence estimate of IBD in a register study from Sweden by Busch et al.
The diagnoses of misclassified patients were evaluated. The majority of the patients in the “Other diagnosis” group had a diagnosis of chronic diarrhea/obstipation or irritable bowel syndrome (IBS), cancer, gastroenteritis, drug-induced symptoms or iatrogenic complications. These findings correspond well to what can be expected in this specific age group between 59 and 79 years of age.25–28
This study has important strengths: first, the validation of the diagnosis of IBD among persons above 50 years of age in NPR versus the information in the individual patient medical record is comprehensive. Second, the same person reviewed the patient medical records, eliminating inter-individual differences.
Several limitations ought to be acknowledged in the present study. First, many MC cases were registered as CD or UC in the NPR. MC is most commonly diagnosed in elderly patients.29 In the study period (1998–2013), registration of MC in NPR was difficult, as there was not an MC ICD-10 code to use, which could lead to a higher rate of misclassifications. Second, diagnostic codes are not registered in NPR before discharge, which may lead to a delay between the time of diagnosis in the patient's medical records and the time of registration in the NPR, particularly for patients followed-up in the outpatient clinic. However, excluding the patients with a registered diagnosis more than one year prior to or after the diagnosis date in the medical record did not affect the PPV in the present study, indicating that a delay does not seem to be a major problem in the validation of IBD-diagnoses. Finally, we were not able to investigate disease location/extent as this data was only registered in approximately half of the cases in the NPR.
Conclusion
In conclusion, the PPV of register diagnoses of IBD in a population aged 50 years and above increased substantially with a minimum of three registrations in the Danish National Patient Registry, when a register IBD diagnosis was compared with data from patient medical records. This study emphasizes the importance of selecting specific criteria for data extraction for the individual study purpose, and testing the effect such choices infer on study results.
Acknowledgments
We acknowledge secretaries and clinical directors at the involved hospitals, including the staff at OPEN, OUH who contributed with technical and practical knowledge. Karen Mai Møllegaard is thanked for submission.
Funding Statement
This work was supported by the Faculty of Health Sciences, University of Southern Denmark, and Region of Southern Denmark (IBD-CARE).
Abbreviations
IBD, inflammatory bowel disease; CD, Crohn’s disease; UC, ulcerative colitis; NPR, the Danish National Registry; DCH-cohort, Diet, Cancer and Health cohort; CPR, personal identification number; MC, microscopic colitis; IBDu, undifferentiated IBD; PPV, positive predictive value; CI, confidence interval.
Data Sharing Statement
Data are stored at Open Patient data Explorative Network (OPEN). Bonafide researchers can apply to use the dataset by applying to open@rsyd.dk.
Ethical Considerations
The present validation study was approved by the Danish ethical committee as a part of the DCH-cohort study (No. KF01-345/93 alias H-KF-312413 and KF11-80-03) and by the Danish Data Protection Agency (No. 2008-58-03).
Consent for Publication
Participants enrolled in the DCH-cohort gave written consent.
Disclosure
M. Julsgaard has served on the advisory board of Janssen and Tillotts Pharma, has received grants for other investigator-initiated studies from Takeda Pharma, has received consultation fees from Ferring and Takeda, personal fees from Janssen, and has received speaker’s fees from MSD, Ferring, Tillotts Pharma and Takeda. Vibeke Andersen reports personal fees from Merck, outside the submitted work. The remaining authors have no relevant conflicts of interest to disclose.
References
- 1.Molodecky NA, Soon IS, Rabi DM, et al. Increasing incidence and prevalence of the inflammatory bowel diseases with time, based on systematic review. Gastroenterology. 2012;142(1):46–54e42; quiz e30. [DOI] [PubMed] [Google Scholar]
- 2.Burisch J, Pedersen N, Cukovic-Cavka S, et al. East-West gradient in the incidence of inflammatory bowel disease in Europe: the ECCO-EpiCom inception cohort. Gut. 2014;63(4):588–597. [DOI] [PubMed] [Google Scholar]
- 3.Khor B, Gardet A, Xavier RJ. Genetics and pathogenesis of inflammatory bowel disease. Nature. 2011;474(7351):307–317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lewis JD. A review of the epidemiology of inflammatory bowel disease with a focus on diet, infections and antibiotic exposure. Nestle Nutr Inst Workshop Ser. 2014;79:1–18. [DOI] [PubMed] [Google Scholar]
- 5.Burisch J, Munkholm P. The epidemiology of inflammatory bowel disease. Scand J Gastroenterol. 2015;50(8):942–951. [DOI] [PubMed] [Google Scholar]
- 6.Jess T, Horvath-Puho E, Fallingborg J, Rasmussen HH, Jacobsen BA. Cancer risk in inflammatory bowel disease according to patient phenotype and treatment: a Danish population-based cohort study. Am J Gastroenterol. 2013;108(12):1869–1876. [DOI] [PubMed] [Google Scholar]
- 7.Schmidt M, Schmidt SA, Sandegaard JL, Ehrenstein V, Pedersen L, Sorensen HT. The Danish National Patient Registry: a review of content, data quality, and research potential. Clin Epidemiol. 2015;7:449–490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schmidt M, Schmidt SAJ, Adelborg K, et al. The Danish health care system and epidemiological research: from health care contacts to database records. Clin Epidemiol. 2019;11:563–591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fonager K, Sorensen HT, Rasmussen SN, Moller-Petersen J, Vyberg M. Assessment of the diagnoses of Crohn’s disease and ulcerative colitis in a Danish hospital information system. Scand J Gastroenterol. 1996;31(2):154–159. [DOI] [PubMed] [Google Scholar]
- 10.Julsgaard M, Norgaard M, Hvas CL, Buck D, Christensen LA. Self-reported adherence to medical treatment prior to and during pregnancy among women with ulcerative colitis. Inflamm Bowel Dis. 2011;17(7):1573–1580. [DOI] [PubMed] [Google Scholar]
- 11.Nielsen MJ, Norgaard M, Holland-Fisher P, Christensen LA. Self-reported antenatal adherence to medical treatment among pregnant women with Crohn’s disease. Aliment Pharmacol Ther. 2010;32(1):49–58. [DOI] [PubMed] [Google Scholar]
- 12.Julsgaard M, Norgaard M, Hvas CL, Grosen A, Hasseriis S, Christensen LA. Influence of medical treatment, smoking and disease activity on pregnancy outcomes in Crohn’s disease. Scand J Gastroenterol. 2014;49(3):302–308. [DOI] [PubMed] [Google Scholar]
- 13.Tjonneland A, Olsen A, Boll K, et al. Study design, exposure variables, and socioeconomic determinants of participation in Diet, Cancer and Health: a population-based prospective cohort study of 57,053 men and women in Denmark. Scand J Public Health. 2007;35(4):432–441. [DOI] [PubMed] [Google Scholar]
- 14.Satsangi J, Silverberg MS, Vermeire S, Colombel JF. The Montreal classification of inflammatory bowel disease: controversies, consensus, and implications. Gut. 2006;55(6):749–753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Binder V, Both H, Hansen PK, Hendriksen C, Kreiner S, Torp-Pedersen K. Incidence and prevalence of ulcerative colitis and Crohn’s disease in the County of Copenhagen, 1962 to 1978. Gastroenterology. 1982;83(3):563–568. [PubMed] [Google Scholar]
- 16.Munkholm P. Crohn’s disease–occurrence, course and prognosis. An epidemiologic cohort-study. Dan Med Bull. 1997;44(3):287–302. [PubMed] [Google Scholar]
- 17.Langholz E. Ulcerative colitis. An epidemiological study based on a regional inception cohort, with special reference to disease course and prognosis. Dan Med Bull. 1999;46(5):400–415. [PubMed] [Google Scholar]
- 18.Jakobsson GL, Sternegard E, Olen O, et al. Validating inflammatory bowel disease (IBD) in the Swedish National Patient Register and the Swedish Quality Register for IBD (SWIBREG). Scand J Gastroenterol. 2017;52(2):216–221. [DOI] [PubMed] [Google Scholar]
- 19.Benchimol EI, Guttmann A, Mack DR, et al. Validation of international algorithms to identify adults with inflammatory bowel disease in health administrative data from Ontario, Canada. J Clin Epidemiol. 2014;67(8):887–896. [DOI] [PubMed] [Google Scholar]
- 20.Rezaie A, Quan H, Fedorak RN, Panaccione R, Hilsden RJ. Development and validation of an administrative case definition for inflammatory bowel diseases. Can J Gastroenterol. 2012;26(10):711–717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dal J, Skou N, Nielsen EH, Jorgensen JO, Pedersen L. Acromegaly according to the Danish National Registry of Patients: how valid are ICD diagnoses and how do patterns of registration affect the accuracy of registry data? Clin Epidemiol. 2014;6:295–299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lasota AN, Overvad K, Eriksen HH, Tjonneland A, Schmidt EB, Gronholdt MM. Validity of peripheral arterial disease diagnoses in the Danish national patient registry. Eur j Vascular Endovasc Surg. 2017;53(5):679–685. [DOI] [PubMed] [Google Scholar]
- 23.Delekta J, Hansen SM, AlZuhairi KS, Bork CS, Joensen AM. The validity of the diagnosis of heart failure (I50.0-I50.9) in the Danish National Patient Register. Dan Med J. 2018;65:4. [PubMed] [Google Scholar]
- 24.Busch K, Ludvigsson JF, Ekstrom-Smedby K, Ekbom A, Askling J, Neovius M. Nationwide prevalence of inflammatory bowel disease in Sweden: a population-based register study. Aliment Pharmacol Ther. 2014;39(1):57–68. [DOI] [PubMed] [Google Scholar]
- 25.Dumic I, Nordin T, Jecmenica M, Stojkovic Lalosevic M, Milosavljevic T, Milovanovic T. Gastrointestinal Tract disorders in older age. Can j Gastroenterol Hepatol. 2019;2019:6757524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lovell RM, Ford AC.Global prevalence of and risk factors for irritable bowel syndrome: a meta-analysis. Clin Gastroenterol Hepatol. 2012;10(7):712–721. [DOI] [PubMed] [Google Scholar]
- 27.Talley NJ, Fleming KC, Evans JM, et al. Constipation in an elderly community: a study of prevalence and potential risk factors. Am J Gastroenterol. 1996;91(1):19–25. [PubMed] [Google Scholar]
- 28.Phillips C, Polakoff D, Maue SK, Mauch R. Assessment of constipation management in long-term care patients. J Am Med Dir Assoc. 2001;2(4):149–154. [PubMed] [Google Scholar]
- 29.Tong J, Zheng Q, Zhang C, Lo R, Shen J, Ran Z. Incidence, prevalence, and temporal trends of microscopic colitis: a systematic review and meta-analysis. Am J Gastroenterol. 2015;110(2):265–276; quiz 277. [DOI] [PubMed] [Google Scholar]