Abstract
Background
This prospective research aimed to determine the incidence of and risk factors for localized pain at the epidural insertion site following nonobstetric surgery performed with epidural anesthesia.
Methods
A total of 5083 surgical inpatients at the teaching hospital undergoing epidural anesthesia were included in the study. The characteristics of the patients, preoperative basic diseases, details of the epidural techniques, surgical procedures and complications were recorded pre-anesthesia until the complications resolved. Multivariate logistic regression analysis was performed to identify predictors of localized pain at the epidural insertion site.
Results
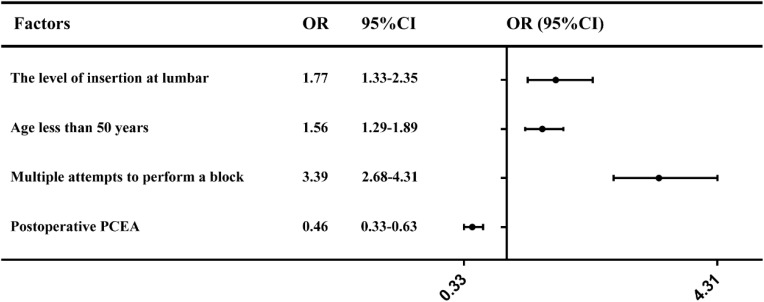
In our analysis, target complications were reported in 532 (10.5%) patients; localized pain at the epidural insertion site occurred in 460 (9.05%) patients, while other major complications occurred in 72 (1.45%) patients. A total of 334 patients had mild pain, and 126 patients had moderate pain. The incidence of localized pain at the epidural insertion site was highest among all complications, and the identified risk factors in the multivariate analysis were as follows: lumbar insertion (odds ratio, 1.77; 95% CI 1.33–2.35), age less than 50 years old (odds ratio, 1.56; 95% CI 1.29–1.89), multiple block attempts (odds ratio, 3.39; 95% CI 2.68–4.31), and postoperative patient-controlled epidural analgesia (odds ratio, 0.46; 95% CI 0.33–0.63).
Conclusion
Localized pain at the epidural insertion site is the most common complaint after epidural anesthesia and requires adequate clinical attention. Improving the proficiency of anesthesiologists to avoid repeated punctures is the best way to reduce injuries.
Keywords: anesthesia, epidural, localized pain, epidural insertion site, postoperative complications
Central nerve block (CNB), especially epidural block, is widely used in surgical anesthesia, postoperative analgesia and cesarean analgesia. Epidural anesthesia is widely applied clinically, but it is associated with some major complications. Among them, lower back pain is one of the most common sequelae;1–3 however, most lower back pain reports are not due to epidural block but rather to broader back pain or sacro-joint strain,4 which needs to be differentiated clinically.
With the development of enhanced recovery after surgery (ERAS), the complications caused by epidural analgesia have received increasing attention. We previously reported serious complications caused by epidural analgesia,5 and it has been found that the incidence of localized pain at the epidural site is the most common complication. It is often ignored by medical staff because of its favorable prognosis without serious sequelae. Published series about epidural blockades have generally included epidural analgesia for chronic pain patients,1,6 obstetric epidural analgesia, or spinal-epidural anesthesia.7 Rates quoted in these studies vary substantially and are often difficult to generalize to a general surgical population. In addition, public information about serious events associated with epidural blocks has been primarily reported in retrospective studies2 or case reports.8 Therefore, the incidence and influencing factors of localized pain are underestimated. Localized pain in pregnant women is often and easily confused with postpartum lower back pain, and it is not easy to accurately observe it.9
Thus, a large prospective study was performed in a single, large tertiary teaching facility; the aim was to determine the incidence of localized pain at the epidural insertion site after the administration of epidural anesthesia and to identify the factors that may predispose patients to it.
Methods
Data Sheet
All anesthesiologists were provided and completed a detailed data sheet for each patient undergoing continuous epidural anesthesia. Data on the number of epidural attempts were recorded, as well as the operator’s level of experience, type and size of the epidural needle and the punctured spinal level (lumbar or thoracic). Other data included preoperative underlying diseases; baseline information regarding the procedure, type and duration of surgery; the details of local anesthetic administration; clinical course of the anesthesia; technical aspects of epidural procedure; block efficacy; accidents during needle/catheter placement; and the presence of major complications during the operation.
Accidents during needle/catheter placement, such as traumatic block placement (evidence of blood), accidental dural puncture, and paresthesia elicitation, were noted. Block efficacy was categorized as 1) satisfactory (surgery performed without additional intervention); 2) unilateral anesthesia; 3) segmental or incomplete anesthesia; or 4) no block/block failure.10,11 The process of epidural puncture was performed according to the practices of each anesthesiologist. Data sheets were deposited in a receptacle after the completion of surgery.
Ethical Considerations
This research was registered prior to data collection in the Chinese Clinical Trial Registry, http://www.chictr.org/usercenter/project/edit.aspx?proj=2353 (number: ChiCTR-OCS-11001887). The study protocol conformed to the Declaration of Helsinki and was approved by the institutional review board (Local Ethics Committee of First Affiliated Hospital, College of Medicine, Zhejiang University). We simply followed up the patients without adding intervention measures, and observed the postoperative outcome of the patients through an observational study. All inpatients who were scheduled to undergo nonobstetric surgeries with epidural anesthesia were invited to participate in the study within 2 years. All participants gave informed consent after having been informed about the objectives and had benefits of our study. The collected data were stored in a password-protected computer to prevent unauthorized access.
Outcome Variable
Localized pain, including the duration and severity of pain, was observed and recorded in our study. Other major complications were also observed and recorded:5 (1) cardiac arrest; (2) seizure; (3) acute respiratory failure; (4) systemic toxicity of local anesthetics; (5) spinal anesthesia; (6) abnormally wide block of spinal nerve; (7) postdural puncture headache (PDPH); (8) epidural hematoma; (9) infectious complications (epidural abscess, meningoencephalitis, or catheter site infection); and (10) adverse neurological outcomes, defined as the presence of motor deficits, sensory deficits, painful paresthesia, dysesthesias or hyperreflexia at the time of subsequent epidural anesthesia; (11) paraplegia; (12) cauda equina syndrome; (13) epidural catheter break; and (14) death.
Postoperative Management
Postoperative follow-up was performed by three trained anesthesiologists who were blinded to all information except the name of the patient, medical record number, procedure and date of surgery. Each patient was visited twice in the ward on the first and second postoperative days (24–48 hours after surgery) by the same anesthesiologist, and a neurological examination was also performed by the anesthesiologist on the ward to identify major complications. In addition, patients reporting localized pain were asked to indicate their level of pain on an 11-point numerical rating scale: 0 represented no pain, 1–3 represented mild pain, 4–6 represented moderate pain, and 7–10 represented severe pain.12 After the initial interview or the patients were discharged from the hospital, all patients who had reported complications were contacted by telephone on the seventh postoperative day. They were followed until the complications had completely resolved or the patient was unable or unwilling to be contacted again. The details regarding the duration of complications and the length of follow-up were recorded. Neurological sequelae that lasted more than 3 months were considered permanent. The final follow-up outcomes of each patient were declared by the two experienced anesthesiologists, especially these controversial issues.
Statistical Analysis
The collected data were analyzed to evaluate the frequency of recorded major complications in the study patients. Univariate comparisons of the patients’ characteristics were performed using chi-square analysis or Fisher’s exact test. Fisher’s exact test was used when the expected values in a cell were less than five. Furthermore, odds ratios and 95% confidence intervals (CIs) were obtained from multiple logistic regression analyses to estimate their independent contributions to complications. The variables used in multiple logistic regression include sex, age, BMI, ASA class, diabetes mellitus, previous CNB history, lumbar intervertebral disk hernia, type of surgery, duration of surgery, puncture level, multiple attempts to perform a block, Satisfactory block efficacy, combined general anesthesia, Traumatic blood, unintentional paresthesia, local anesthetic (ropivacaine) and postoperative PCEA. A P value of less than 0.05 was considered statistically significant. Mean values are expressed as means ± standard deviations (SDs). Analysis was performed using SPSS statistical software version 18.0.
Results
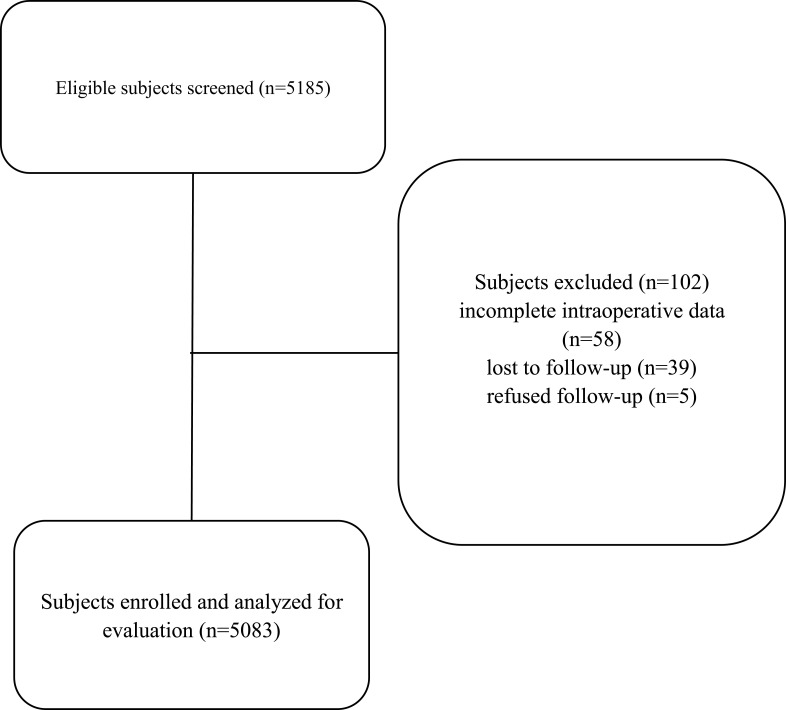
During the study period, data for 5185 surgical inpatients who underwent epidural procedures were collected. A total of 5083 (98% capture rate) patients had complete data, and the other 102 patients with incomplete information were excluded, among whom 58 had incomplete intraoperative data, 39 were lost to follow-up and 5 refused follow-up (Figure 1).
Figure 1.
Patient flow diagram.
Overview of 5083 Epidural Anesthesia Patients
The characteristics of the 5083 surgical inpatients who received epidural anesthesia are shown in Table 1. There were 3560 (70%) men and 1523 (30%) women, and their mean age was 52.7±17.0 years. Most patients were American Society of Anesthesiologists (ASA) class 1–2 status and underwent lumbar block for urologic, orthopedic, or general surgery. Preexisting neurological conditions were present in these patients; 54 (1.1%) patients had an intervertebral disk hernia, 165 (3.2%) patients had diabetes, and 306 (6%) patients had a previous CNB history. We used a uniform 18-gauge Tuohy epidural needle and a multiport epidural catheter for all procedures. Intraoperative epidural anesthesia was performed with ropivacaine (0.375–0.75%) and pure or combined lidocaine (1–2%). Of note, no vasoconstrictors were added to the local anesthetic.
Table 1.
Characteristics of the Study Population
| Number of Patients (N=5083) | Percentage (%) | |
|---|---|---|
| Sex | ||
| Male | 3560 | 70 |
| Female | 1523 | 30 |
| Age | ||
| < 50 | 2068 | 40.7 |
| ≥50 | 3015 | 59.3 |
| Body mass index (BMI) | ||
| <25 | 3862 | 76.0 |
| ≥25 | 1221 | 24.0 |
| ASA class | ||
| 1 | 2633 | 51.8 |
| 2 | 2233 | 43.9 |
| 3–4 | 217 | 4.3 |
| Preexisting neurological condition | ||
| Diabetes mellitus | 165 | 3.2 |
| Previous CNB history | 306 | 6.0 |
| Lumbar intervertebral disk hernia |
54 | 1.1 |
| Type of surgery | ||
| Orthopedic | 1043 | 20.5 |
| Urologic | 1928 | 37.9 |
| General | 1302 | 25.6 |
| Anorectal | 336 | 6.6 |
| Gynecological | 71 | 1.4 |
| Thoracic | 38 | 0.7 |
| Vascular | 365 | 7.2 |
| Puncture level | ||
| Lumbar | 4090 | 80.5 |
| Thoracic | 993 | 19.5 |
| Technical difficulty (multiple attempts at >1 interspace) | ||
| Yes | 491 | 9.7 |
| No | 4592 | 90.3 |
| Block efficacy | ||
| Satisfactory | 4821 | 94.8 |
| Unilateral | 31 | 0.6 |
| Segmental or incomplete | 122 | 2.4 |
| No block (block failure) | 109 | 2.2 |
| Combined general anesthesia | ||
| Yes | 618 | 12.2 |
| No | 4465 | 87.8 |
| Technical complications | ||
| Traumatic bleeding | 65 | 1.3 |
| Accidental dural puncture | 24 | 0.5 |
| Unintentional paresthesia | 160 | 3.1 |
| Local anesthetic | ||
| Lidocaine | 221 | 4.3 |
| Mixture of lidocaine and ropivacaine | 4243 | 83.5 |
| Ropivacaine | 590 | 11.6 |
| Postoperative PCEA | ||
| Yes | 873 | 17.2 |
| No | 4210 | 82.8 |
Note: Percentages (%) are based on those patients with available data.
Abbreviations: ASA, American Society of Anesthesiologists; PCEA, patient-controlled epidural analgesia.
A total of 491 (9.7%) procedures were successful and required multiple attempts. There were 160 cases of paresthesia during needle or catheter placement; in 12 cases, epidural anesthesia was abandoned completely, and in the remaining cases, patient-controlled epidural analgesia (PCEA) was not used. Accidental dural puncture occurred in 24 (0.5%) procedures; in 9 cases, epidural anesthesia was abandoned, and in 15 cases, epidural anesthesia was administered in the lower intervertebral space. No spinal anesthesia was applied in any of the patients. Bleeding when placing a needle or catheter occurred in 65 patients (3.3%), and the epidural catheter was successfully placed after a new attempt.
There were 4821 cases (94.8%) of satisfactory anesthesia. A total of 873 patients (17.2%) underwent extended postoperative PCEA; ropivacaine (concentration 0.125–0.18%) was the only local anesthetic used for PCEA.
Epidural Complications
The major complications observed after the epidural procedures are shown in Table 2. Noted complications were reported in 532 (10.5%) patients, and localized pain at the epidural insertion site was reported in 460 (9.05%) patients. Other complications included epidural hematoma in 1 (0.02%) patient, adverse neurological outcomes in 57 (1.12%) patients, systemic toxicity of local anesthetics in 4 (0.08%) patients, abnormal wide block of the spinal nerve in 3 (0.06%) patients and PDPH in 7 (0.14%) patients. The mean duration of adverse neurological outcomes (9.9 days) was the longest. The mean duration of localized pain at the epidural insertion site was 2.2 days, and PDPH lasted for an average of 4.7 days. Accidents during needle/catheter placement are also shown in Table 1.
Table 2.
Major Complications Related to Outcomes in 5083 Patients
| Type of Complication | Number of Patients (n) | Incidence (%) | Proportion of All Complications (%) |
|---|---|---|---|
| Localized pain at epidural insertion site | 460 | 9.05 | 86.5 |
| Systemic local anesthetic toxicity | 4 | 0.08 | 0.8 |
| Adverse neurological outcomes | 57 | 1.12 | 10.7 |
| PDPH | 7 | 0.14 | 1.3 |
| Abnormally wide block of the spinal nerve | 3 | 0.06 | 0.6 |
| Epidural hematoma | 1 | 0.02 | 0.2 |
| Total | 532 | 10.5 | 100 |
Abbreviation: PDPH, postdural puncture headache.
Localized Pain at the Epidural Insertion Site
A total of 460 (9.05%) patients experienced localized pain at the epidural insertion site, and all symptoms occurred within 48 hours after the operation. A total of 334 patients reported mild pain, and 126 patients reported moderate pain. The duration of pain lasted less than 48 hours in 404 patients, from 3–7 days in 38 patients, and less than 3 months in 18 patients (Table 3). No permanent sequelae occurred in 460 cases.
Table 3.
Localized Pain at the Epidural Insertion Site Assessment After Epidural Analgesia
| <2 Days | 3–7 Days | 8 Days–3 Months | >3 Months | |
|---|---|---|---|---|
| Duration of pain | 404 | 38 | 18 | 0 |
Factors that were analyzed for their association with the development of postoperative localized pain at the epidural insertion site are listed in Table 4. The univariate analysis showed that the low incidence of localized pain at the epidural insertion site was associated with younger age (age<50 years), lumbar insertion, multiple attempts to perform a block, accidental dural puncture, postoperative PCEA, lumbar intervertebral disk hernia, ropivacaine use, paresthesia during needle/catheter placement, type of surgery, ASA class, combined general anesthesia and a previous CNB history. The incidence of localized pain at the epidural insertion site was higher among younger patients (11.3%) and those who underwent lumbar insertion (9.9%). Patients who had a previous CNB history (13.1%) and lumbar intervertebral disk hernia (25.9%) were more likely to experience localized pain at the epidural insertion site. The type of surgery (9.9%) also had an impact. We found that compared with a single attempt, multiple attempts increased the incidence by 5.5%. Accidental dural puncture (9.3%) and unintentional paresthesia (16.9%) during surgery increased the incidence of localized pain at the epidural insertion site, while combined general anesthesia (6.1%) and the use of ropivacaine (8.8%) decreased the incidence of localized pain at the epidural insertion site. Our study showed that localized pain at the epidural insertion site was twice as likely in patients who did not receive postoperative PCEA. Furthermore, multiple logistic regression analysis showed that the following factors were independent determinants: lumbar insertion (odds ratio, 1.77; 95% CI 1.33–2.35), age less than 50 years, (odds ratio, 1.56; 95% CI 1.29–1.89), multiple attempts to perform a block (odds ratio, 3.39; 95% CI 2.68–4.31), and postoperative PCEA (odds ratio, 0.46; 95% CI 0.33–0.63) (Figure 2).
Table 4.
Univariate Analysis of Factors Associated with Localized Pain at the Epidural Insertion Site
| Risk Factor | Number of Patients (n) | Incidence (%) | P value | |
|---|---|---|---|---|
| Sex | Male | 3560 | 8.7 | 0.16 |
| Female | 1523 | 9.9 | ||
| Age | <50 | 2068 | 11.3 | <0.001 |
| ≥50 | 3015 | 7.5 | ||
| BMI | <25 | 3862 | 9 | 0.954 |
| ≥25 | 1221 | 9.1 | ||
| ASA class | 1 | 2633 | 10.1 | 0.007 |
| 2–4 | 2450 | 7.9 | ||
| Diabetes mellitus | Yes | 164 | 6.1 | 0.18 |
| No | 4919 | 9.1 | ||
| Previous CNB history | Yes | 306 | 13.1 | 0.017 |
| No | 4777 | 8.7 | ||
| Lumbar intervertebral disk hernia | Yes | 54 | 25.9 | <0.001 |
| No | 5029 | 8.9 | ||
| Type of surgery | Orthopedic | 1043 | 11.3 | 0.002 |
| Urologic | 1883 | 9.6 | ||
| General | 1302 | 6.5 | ||
| Anorectal | 336 | 7.4 | ||
| Gynecological | 71 | 7 | ||
| Thoracic | 38 | 7.9 | ||
| Vascular | 365 | 11 | ||
| Duration of surgery | <60 | 2498 | 9.7 | 0.098 |
| ≥60 | 2585 | 8.4 | ||
| Puncture level | Lumbar | 4090 | 9.9 | <0.001 |
| Thoracic | 993 | 5.7 | ||
| Technical difficulty (more attempts at >1 interspace) | Yes | 4592 | 7.7 | <0.001 |
| No | 491 | 22 | ||
| Satisfactory block | Yes | 4821 | 8.9 | 0.242 |
| No | 262 | 11.1 | ||
| Combined general anesthesia | Yes | 618 | 6.1 | 0.007 |
| No | 4465 | 9.5 | ||
| Traumatic bleeding | Yes | 65 | 15.4 | 0.073 |
| No | 5018 | 9.0 | ||
| Accidental dural puncture | Yes | 24 | 9.3 | <0.001 |
| No | 5059 | 8.3 | ||
| Unintentional paresthesia | Yes | 160 | 16.9 | <0.001 |
| No | 4923 | 8.8 | ||
| Ropivacaine | Yes | 4817 | 8.8 | 0.016 |
| No | 266 | 13.2 | ||
| Postoperative PCEA | Yes | 873 | 4.8 | <0.001 |
| No | 4210 | 9.9 |
Abbreviations: ASA, American Society of Anesthesiologists; PCEA, patient-controlled epidural analgesia.
Figure 2.
Multivariate analysis of factors associated with localized pain at the epidural insertion site.
Discussion
We studied 5083 patients who underwent epidural anesthesia and found that the incidence of epidural-related complications was 1:100. In fact, localized pain at the epidural insertion site was the most common postoperative complaint and was noted as a major complication in our study, in accordance with previous data.9 Severe epidural complications are described in detail in our previous report.5 Localized pain at the epidural insertion site is often underestimated because it does not cause severe sequelae. However, the high incidence and potential impact of localized pain should serve as a warning. The reasons why we believe that our study is reliable are as follows. First, we used a prospective research design to enroll eligible patients before surgery and collect relevant information. Then, anesthesia and various conditions during surgery were recorded, including various puncture problems and complications that may affect postoperative puncture site pain. However, this was an observational study without a control group, which did not interfere with the selection and judgment of the anesthesiologist. We tried our best to present the real clinical situation related to the research; in addition, our aim was to prevent missed diagnoses and to ensure that we had a substantial amount of data. Second, only 102 patients were excluded, and the rate of loss to follow-up was very low in our study. Finally, there were no obstetric patients in our study. It has been described in previous studies13 that neurological complications associated with pregnancy and labor are considerably more common than those associated with nonpregnancy-related operations. Consequently, the unspecified inclusion of obstetric patients will distort any analysis. As mentioned above, we believe that our current design contributes to improved reporting.
In our study, 460 patients experienced localized pain at the epidural insertion site; localized pain had the highest incidence rate of all complications (9.05%). Massey Dawkins reported that the incidence of immediate postoperative localized backache after surgery was 2–30%; the incidence of lower back pain was 2% when using a nonpassivated epidural needle and 30% when using a blunt needle.14 Most studies have no clear definition of localized pain at the epidural insertion site, and this pain is therefore often confused with lower back pain. We needed to clearly differentiate pain at the puncture site from pain due to lumbar disc herniation or low back pain caused by surgery or other reasons. After the operation, through careful questioning and physical examination, it was clear that there was obvious tenderness or tension pain in the case of puncture site pain, as determined by professional anesthesiologists. If a clear diagnosis could not be made, imaging and other auxiliary examinations were performed to determine the diagnosis. Therefore, after large-scale clinical observation, we also proposed a preliminary definition and interpretation of puncture pain, instead of general postoperative back pain. Based on our research results and literature review, localized pain is defined as a new occurrence of limited pain after epidural puncture and obvious tenderness around the puncture site. The majority of studies have generally described localized pain as acute pain following epidural anesthesia, most of which is self-limiting and partly relieved by epidural steroid injection.3,15 In our study, the pain lasted for approximately 2 days and was significantly relieved; however, in 18 patients, the pain lasted nearly 3 months. This prolonged pain should be noted.
Most localized pain was relieved within three days and did not cause long-term sequelae,16 and more than 90% of patients experienced significant pain relief within 1 week. However, some patients had a negative attitude toward epidural anesthesia due to localized pain that lasted nearly 3 months.17 Since many patients received routine analgesics after surgery, only six patients with moderate pain in our study were administered additional analgesics, and no patients required other types of treatment; this finding needs to be further clarified. Patients who experienced localized pain at the epidural site emphasized that they would not choose epidural anesthesia for future operations. In this era of ERAS, localized pain at the epidural insertion site after epidural analgesia needs additional attention.
After adjusting for covariates in the multivariate analysis, patients who had a lumbar intervertebral disk hernia and a previous CNB history did not report more severe localized pain than those without a hernia and previous CNB history, which may be due to the low number of patients. The rate of localized pain was decreased with long-acting local anesthetics (ropivacaine) during the operation in the univariate analysis, which may suggest the use of intraoperative anesthetics. The multivariate analysis showed that multiple epidural punctures, lumbar insertion, age less than 50 years and use of PCEA were independent factors influencing pain at the puncture site. The use of multiple attempts to perform a block in our study was the most important and direct factor affecting localized pain, consistent with previous studies.1 Repeated puncture leads to severe damage to the supraspinous ligament, interspinous ligament, and periosteum, which exacerbates local aseptic inflammation.18 Therefore, we recommend that the operation should be performed by an experienced anesthesiologist to avoid multiple attempts when encountering difficult punctures. In addition, it may be necessary to change the anesthesia method after multiple puncture failures occur. In this regard, some studies have advocated the use of steroid injections before lumbar puncture to reduce the pain associated with lumbar puncture points.19 Importantly, the epidural insertion operator should strive to improve proficiency in epidural puncture to avoid inaccurate and multiple punctures.
Notably, the incidence of localized pain was independently related to the insertion position (waist, 9.9%; chest 5.7%). We speculate that this may be related to the position at the time of puncture. To obtain a good puncture gap, the patients needed to lie on their side and bend their knees. The degree of flexion of the waist is greater than that of the chest, leaving the ligaments in a tight state, potentially resulting in severe puncture injuries. Therefore, we suggest that the patient maintains an appropriate degree of flexion. The use of PCEA reduced the incidence of pain at the epidural site. This may be because the use of PCEA affected the level of sensory block, which partially eliminated pain and soreness at the puncture site. In our study, almost all patients experienced local back pain within 48 hours after surgery, and PCEA was used for 2–3 days. Therefore, the feeling of pain in the epidural insertion site was reduced.
In general, age is considered a predictor of postoperative pain and analgesia consumption. Due to differences in previous research methods, such as the size of the included samples, different statistical methodologies, and different age exclusion criteria, there may be a positive or negative correlation between age and postoperative pain.20 We analyzed pain incidence at the puncture point according to age group, and we found that it was higher in the group less than 50 years old. This can be interpreted as lower peripheral nociceptive function, in some cases changing the pain threshold.20 Elderly individuals have a high pain threshold, reducing the perception of pain and even reducing the use of postoperative pain medications. There is also evidence that increasing age seems to reduce the effects of specific genes on pain perception.21 However, there is not enough evidence to support a causal relationship, and this topic warrants discussion in future studies. We collected data on preoperative morbidities, but there were no statistically significant results, which may be related to the small number of preoperative patients with comorbid diseases.
It should be emphasized that the localized pain at the epidural insertion site should be well distinguished from other epidural complications to avoid misdiagnosis and prevent additional serious complications. Localized pain is usually limited to the waist, and most patients report pain or tenderness at the puncture site and can recover on their own in a short period of time without accompanying lower limb pain or paresthesia. This pain should be distinguished from lower back pain caused by epidural hematoma or infection, which is very rare.
The puncturing of blood vessels in the venous plexus may cause bleeding into the closed epidural space with or without preexisting coagulopathy.22 Notably, during puncture, several patients with bleeding had high postoperative pain scores and experienced delayed postoperative recovery. Epidural hematoma usually manifests as deep pain; the pain is more severe than that reported for insertion site pain and can reach a moderate to severe level. It is accompanied by rapid progressive sensory dyskinesia and sphincter dysfunction. These symptoms usually appear within 24 hours after epidural insertion or removal, but they may be delayed.23 It is worth noting that epidural hemorrhage may increase direct pressure on the spinal cord or coccyx, increase the risk of ischemia or infarction, and cause permanent neurological deficits.22 In addition, epidural abscess is also very rare, but it is a serious complication that can cause permanent neurological sequelae and even fatal consequences.24 The initial signs of an epidural abscess may be nonspecific because the typical triad of fever, spinal pain, and neurological dysfunction may not be observed early.25 Although epidural hematomas and abscesses also manifest as symptoms of lower back pain, they usually have unique accompanying symptoms to aid in diagnosis. The most important aspect in addressing any complication is timely and thorough observation. Therefore, when visiting patients after surgery, trained anesthesiologists should consider the patient’s medical history, conduct a relevant physical examination, and carefully observe any redness and swelling at the puncture site. If necessary, timely magnetic resonance imaging (MRI) and laboratory tests should be conducted to detect and treat complications as soon as possible.
Determining the pain score is a subjective evaluation, and there is accumulating evidence of the role of psychological factors in the etiology of lower back pain.26 During the study, patients with particularly severe mental problems or even patients who could not communicate with others were not included in our study. Performing a physical examination of the lower back is also very important for patients who complain of pain at the puncture site. Even necessary imaging examinations are performed for special cases to confirm that there is real pain and tenderness confined to the puncture site accompanied by muscle tension. The diagnosis is made after repeated confirmation, which can minimize the influence of psychological factors. Therefore, we will pay more attention to and differentiate pain in future clinical practice.
In conclusion, localized pain at the epidural insertion site after epidural analgesia requires clinical attention. Our study also suggests that prevention and management should start at the first preoperative visit, with a careful evaluation of the patient’s medical history. Appropriate judgment of the risks could decrease the incidence of major complications of epidural techniques. Avoiding multiple punctures and aseptic procedures should be emphasized.
Acknowledgments
This work was supported by Bethune Charitable Foundation (BCF-RF-WSQZTZJ-202011-031) and the National Key Research and Development Program of China (Grant No. 2018YFC2001905).
Abbreviations
PDPH, postdural puncture headache; ASA, American Society of Anesthesiologists; PCEA, patient-controlled epidural analgesia; BMI, body mass index; ERAS, enhanced recovery after surgery.
Data Sharing Statement
The datasets supporting the conclusions of this are available from the corresponding authors (smzhu20088@zju.edu.cn) on direct request.
Ethical Approval and Consent to Participate
The study was approved by the Ethics Committee of First Affiliated Hospital, College of Medicine, Zhejiang University. All participants gave informed consent after having been informed about the objectives and had benefits of our study.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Hakim SM, Narouze S, Shaker NN, Mahran MA. Risk factors for new-onset persistent low-back pain following nonobstetric surgery performed with epidural anesthesia. Reg Anesth Pain Med. 2012;37(2):175–182. PMID: 22286517. doi: 10.1097/AAP.0b013e3182411048 [DOI] [PubMed] [Google Scholar]
- 2.Chia YY, Lo Y, Chen YB, Liu CP, Huang WC, Wen CH. Risk of chronic low back pain among parturients who undergo cesarean delivery with neuraxial anesthesia: a Nationwide Population-Based Retrospective Cohort Study. Medicine (Baltimore). 2016;95(16):e3468. PMID: 27100449 PMCID: PMC4845853. doi: 10.1097/MD.0000000000003468 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gao W, Ren Y, Cui GX. Dexamethasone added to local lidocaine for infiltration along the spinal-epidural needle pathway decreases incidence and severity of backache after gynecological surgery. Med Sci Monit. 2015;21:821–827. PMID: 25785683 PMCID: PMC4374485. doi: 10.12659/MSM.892620 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Arnbak B, Jensen TS, Egund N, et al. Prevalence of degenerative and spondyloarthritis-related magnetic resonance imaging findings in the spine and sacroiliac joints in patients with persistent low back pain. Eur Radiol. 2016;26(4):1191–1203. PMID: 26194456. doi: 10.1007/s00330-015-3903-0 [DOI] [PubMed] [Google Scholar]
- 5.Kang XH, Bao FP, Xiong XX, et al. Major complications of epidural anesthesia: a prospective study of 5083 cases at a single hospital. Acta Anaesthesiol Scand. 2014;58(7):858–866. PMID: 24961586. doi: 10.1111/aas.12360 [DOI] [PubMed] [Google Scholar]
- 6.de Seze MP, Sztark F, Janvier G, Joseph PA. Severe and long-lasting complications of the nerve root and spinal cord after central neuraxial blockade. Anesth Analg. 2007;104(4):975–979. PMID: 17377116. doi: 10.1213/01.ane.0000253485.75797.e7 [DOI] [PubMed] [Google Scholar]
- 7.Klimek M, Rossaint R, van de Velde M, Heesen M. Combined spinal-epidural vs. spinal anaesthesia for caesarean section: meta-analysis and trial-sequential analysis. Anaesthesia. 2018;73(7):875–888. PMID: 29330854. doi: 10.1111/anae.14210 [DOI] [PubMed] [Google Scholar]
- 8.Domenicucci M, Marruzzo D, Pesce A, Raco A, Missori P. Acute spinal epidural hematoma after acupuncture: personal case and literature review. World Neurosurg. 2017;102:695 e611–695 e614. PMID: 28377250. doi: 10.1016/j.wneu.2017.03.125 [DOI] [PubMed] [Google Scholar]
- 9.Sehmbi H, D’Souza R, Bhatia A. Low back pain in pregnancy: investigations, management, and role of neuraxial analgesia and anaesthesia: a systematic review. Gynecol Obstet Invest. 2017;82(5):417–436. PMID: 28514779. doi: 10.1159/000471764 [DOI] [PubMed] [Google Scholar]
- 10.Tawfik MM, Atallah MM, Elkharboutly WS, Allakkany NS, Abdelkhalek M. Does Preprocedural ultrasound increase the first-pass success rate of epidural catheterization before cesarean delivery? A Randomized Controlled Trial. Anesth Analg. 2017;124(3):851–856. PMID: 27183373. doi: 10.1213/ANE.0000000000001325 [DOI] [PubMed] [Google Scholar]
- 11.Chin A, Crooke B, Heywood L, Brijball R, Pelecanos AM, Abeypala W. A randomised controlled trial comparing needle movements during combined spinal-epidural anaesthesia with and without ultrasound assistance. Anaesthesia. 2018;73(4):466–473. PMID: 29322504. doi: 10.1111/anae.14206 [DOI] [PubMed] [Google Scholar]
- 12.Bailey CS, Rasoulinejad P, Taylor D, et al. Surgery versus conservative care for persistent sciatica lasting 4 to 12 months. N Engl J Med. 2020;382(12):1093–1102. PMID: 32187469. doi: 10.1056/NEJMoa1912658 [DOI] [PubMed] [Google Scholar]
- 13.Malevic A, Jatuzis D, Paliulyte V. Epidural analgesia and back pain after labor. Medicina (Kaunas). 2019;55(7). PMID: 31324024 PMCID: PMC6681359. doi: 10.3390/medicina55070354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dawkins CJ. An analysis of the complications of extradural and caudal block. Anaesthesia. 1969;24(4):554–563. PMID: 4242599. doi: 10.1111/j.1365-2044.1969.tb02909.x [DOI] [PubMed] [Google Scholar]
- 15.Choi HJ, Hahn S, Kim CH, et al. Epidural steroid injection therapy for low back pain: a meta-analysis. Int J Technol Assess Health Care. 2013;29(3):244–253. PMID: 23769210. doi: 10.1017/S0266462313000342 [DOI] [PubMed] [Google Scholar]
- 16.Mandal NG. Randomized controlled comparison of epidural bupivacaine versus pethidine for analgesia in labour. Br J Anaesth. 2000;85(4):665–666. PMID: 11064640. [PubMed] [Google Scholar]
- 17.Rhee WJ, Chung CJ, Lim YH, Lee KH, Lee SC. Factors in patient dissatisfaction and refusal regarding spinal anesthesia. Korean J Anesthesiol. 2010;59(4):260–264. PMID: 21057616 PMCID: PMC2966707. doi: 10.4097/kjae.2010.59.4.260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kalso E. IV. Persistent post-surgery pain: research agenda for mechanisms, prevention, and treatment. Br J Anaesth. 2013;111(1):9–12. PMID: 23794639. doi: 10.1093/bja/aet211 [DOI] [PubMed] [Google Scholar]
- 19.C. Nguyen, I. Boutron,G. Baron, K. Sanchez, et al. Steroid injections for patients with low back pain. Ann Intern Med. 2017;166(8). PMID: 28320019. doi: 10.7326/P17-9034 [DOI] [PubMed] [Google Scholar]
- 20.Ip HY, Abrishami A, Peng PW, Wong J, Chung F. Predictors of postoperative pain and analgesic consumption: a qualitative systematic review. Anesthesiology. 2009;111(3):657–677. PMID: 19672167. doi: 10.1097/ALN.0b013e3181aae87a [DOI] [PubMed] [Google Scholar]
- 21.Edwards RR. Genetic predictors of acute and chronic pain. Curr Rheumatol Rep. 2006;8(6):411–417. PMID: 17092439. doi: 10.1007/s11926-006-0034-2 [DOI] [PubMed] [Google Scholar]
- 22.Liu H, Brown M, Sun L, et al. Complications and liability related to regional and neuraxial anesthesia. Best Pract Res Clin Anaesthesiol. 2019;33(4):487–497. PMID: 31791565. doi: 10.1016/j.bpa.2019.07.007 [DOI] [PubMed] [Google Scholar]
- 23.Christie IW, McCabe S. Major complications of epidural analgesia after surgery: results of a six-year survey. Anaesthesia. 2007;62(4):335–341. PMID: 17381568. doi: 10.1111/j.1365-2044.2007.04992.x [DOI] [PubMed] [Google Scholar]
- 24.Alerhand S, Wood S, Long B, Koyfman A. The time-sensitive challenge of diagnosing spinal epidural abscess in the emergency department. Intern Emerg Med. 2017;12(8):1179–1183. PMID: 28779448. doi: 10.1007/s11739-017-1718-5 [DOI] [PubMed] [Google Scholar]
- 25.Schwab JH, Shah AA. Spinal epidural abscess: diagnosis, management, and outcomes. J Am Acad Orthop Surg. 2020;28(21):e929–e938. PMID: 32694325. doi: 10.5435/JAAOS-D-19-00685 [DOI] [PubMed] [Google Scholar]
- 26.Tampin B, Royle J, Bharat C, Trevenen M, Olsen L, Goucke R. Psychological factors can cause false pain classification on painDETECT. Scand J Pain. 2019;19(3):501–512. PMID: 30901319. doi: 10.1515/sjpain-2018-0355 [DOI] [PubMed] [Google Scholar]