Abstract
Research shows that there has been a substantial increase in substance use and abuse during the COVID-19 pandemic, and that substance use/abuse is a commonly reported way of coping with anxiety concerning COVID-19. Anxiety about COVID-19 is more than simply worry about infection. Research provides evidence of a COVID Stress Syndrome characterized by (1) worry about the dangers of COVID-19 and worry about coming into contact with coronavirus contaminated objects or surfaces, (2) worry about the personal socioeconomic impact of COVID-19, (3) xenophobic worries that foreigners are spreading COVID-19, (4) COVID-19-related traumatic stress symptoms (e.g., nightmares), and (5) COVID-19-related compulsive checking and reassurance-seeking. These form a network of interrelated nodes. Research also provides evidence of another constellation or “syndrome”, characterized by (1) belief that one has robust physical health against COVID-19, (2) belief that the threat of COVID-19 has been exaggerated, and (3) disregard for social distancing. These also form a network of nodes known as a COVID-19 Disregard Syndrome. The present study, based on a population-representative sample of 3075 American and Canadian adults, sought to investigate how these syndromes are related to substance use and abuse. We found substantial COVID-19-related increases in alcohol and drug use. Network analyses indicated that although the two syndromes are negatively correlated with one another, they both have positive links to alcohol and drug abuse. More specifically, COVID-19-related traumatic stress symptoms and the tendency to disregard social distancing were both linked to substance abuse. Clinical and public health implications are discussed.
Keywords: COVID-19, COVID stress syndrome, Social distancing, Alcohol abuse, Drug abuse, Network analysis
1. Introduction
For people who consumed alcohol or recreational drugs prior to the COVID-19 pandemic, consumption has increased substantially in the U.S. and Canada during the pandemic. Surveys indicate increases in the consumption of alcohol (10–18% of adults), cannabis (6–8%), and other drugs (3%) (Ipsos, 2020a, Ipsos, 2020b, Ipsos, 2020c, Morning Consult, 2020, Nanos, 2020, Rotermann, 2020). Increases in substance use are correlated with anxiety or distress about COVID-19, and substance use is a commonly reported way of coping with COVID-19-related worries (Rehm et al., 2020, Rodriguez et al., 2020). These findings pertain to substance use. Less is known about pandemic-related substance abuse, defined as a hazardous pattern of substance use that is associated with physical, interpersonal, or legal problems (Galanter et al., 2015, Goodwin, 2016, Pihl and Shakra, 2015, Wright and Henes, 2018).
Empirical investigations have identified two extreme types of emotional and behavioral reactions to the COVID-19 pandemic (Taylor et al., 2020a, Taylor et al., 2020b, Taylor et al., 2020c). At one extreme, some people have reacted with high levels of anxiety or distress. At the other extreme, some people have reacted with disregard for social distancing, believing that the danger of COVID-19 has been exaggerated. Both extremes may be associated with COVID-19-related substance use and abuse, although this remains to be investigated. The primary purpose of this study was to investigate how COVID-19-related distress and disregard are related to substance use and abuse.
COVID-19-related distress is multifaceted. Research provides evidence of a COVID Stress Syndrome, consisting of the following: (1) Worry about the dangers of COVID-19 and worry about coming into contact with objects or surfaces that might be contaminated with the coronavirus, (2) worry about personal socioeconomic impacts of COVID-19, (3) xenophobic worries that foreigners are spreading the coronavirus, (4) COVID-19-related traumatic stress symptoms (e.g., nightmares), and (5) COVID-19-related compulsive checking and reassurance-seeking (Taylor et al., 2020b, Taylor et al., 2020c).
The five elements of the COVID Stress Syndrome are nodes of an interconnected network (Taylor et al., 2020c). An aim of the present study was to investigate how this network is related to substance abuse. According to network analysis, nodes cluster together because they are causally linked to one another (Epskamp, Borsboom, & Fried, 2018). In network analysis, the links between nodes are called “edges.” The presence of statistically significant edges does not assume that nodes are influenced by some underlying latent variable; rather, network analysis posits that nodes can directly influence one another (e.g., symptoms can mutually exacerbate one another; Epskamp et al., 2018). If nodes causally influence one another, then changes in a central node will cause downstream changes in other nodes.
From the perspective of cognitive-behavioral approaches to health anxiety, pandemics, and trauma-related fears (e.g., Taylor, 2017, Taylor, 2019), a network approach makes theoretical sense because cognitive-behavioral models predict that the nodes in the network interact with one another. Here, negative beliefs (e.g., worry about the dangers of COVID-19) leads to COVID-19-related checking behaviors, in an attempt to make the threat more predictable and controllable. Such checking often backfires, leading the person to encounter new, fear-evoking information (e.g., graphic images or descriptions of sick people on the mainstream news or social media), which can lead to traumatic stress symptoms such COVID-19-related nightmares (Taylor et al., 2020c).
McKay and Asmundson (2020) proposed that each node in the COVID Stress Syndrome could exacerbate substance use and abuse, in that the distress associated with each node could motivate a person to use alcohol or drugs as a means of coping with COVID-19-related distress. Findings from pre-COVID-19 research are broadly consistent with this idea. Substance abuse is correlated with: (1) Excessive worry (Grant et al., 2016), (2) threats to one’s socioeconomic status (Bosque-Prous et al., 2015), (3) xenophobia in general (i.e., not specific to COVID-19) (Basanez et al., 2019), (4) posttraumatic stress symptoms (Smith, Goldstein, & Grant, 2016), and (5) compulsive checking (Hasler et al., 2005). The relationship between specific nodes of the COVID Stress Syndrome and substance use and abuse remains to be empirically investigated. This issue is important because targeting particular nodes could lead to downstream reductions in substance use/abuse.
In addition to the COVID Stress Syndrome, research provides evidence of a second constellation of interconnected nodes (“syndrome”) characterized by a disregard or denial of the COVID-19 threat (Taylor, Landry, Paluszek, & Asmundson, 2020a). This COVID Disregard Syndrome consists of three nodes: (1) Belief that one has robust physical health against COVID-19, (2) belief that the threat of COVID-19 has been exaggerated, and (3) disregard for social distancing. The relationship between the nodes of this syndrome and substance use/abuse is potentially important because of the public health implications concerning the way that government agencies regulate the consumption of substances, particularly alcohol, as described below.
During the COVID-19 pandemic there have been a range of government reactions to alcohol regulation. Some governments have declared that retail alcohol vendors are an essential service (e.g., Canada, New Zealand, U.S.) (Rehm et al., 2020, Reynolds and Wilkinson, 2020). Here, alcohol sales were continued during the pandemic partly because of concerns about the number of people who would go into alcohol withdrawal and require emergency hospital services if alcohol sales were closed. In comparison to these countries, the sale of alcohol has been severely restricted in other countries (e.g., South Africa, Thailand, India) in an effort to minimize the risks of alcohol-fueled domestic violence during self-isolation (colloquially called “lockdown”) and to limit the spread of infection because of concerns that intoxicated people would ignore social distancing guidelines (Nadkarni et al., 2020, Rehm et al., 2020, Reynolds and Wilkinson, 2020). To our knowledge, there has yet to be an empirical investigation of the relationship between the consumption of drugs and alcohol and non-adherence to social distancing.
Given the many unknowns about the relationships among substance use/abuse and COVID-19-related distress and disregard, the goals of the present study were largely exploratory in nature. The specific aims were: (1) To assess the magnitude of increase of COVID-19-related alcohol and drug use and abuse in a population representative sample of U.S. and Canadian adults, (2) to investigate how COVID-19-related stressors (e.g., stressors associated with self-isolation) are related to COVID-19-related substance use and abuse, (3) to investigate the extent to which the nodes of COVID-19-related distress and disregard are correlated with various indices of alcohol and drug use and abuse, and (4) to conduct a network analysis to investigate how the nodes of the COVID Stress Syndrome and the COVID Disregard Syndrome are specifically linked to alcohol and drug abuse.
2. Materials and methods
2.1. 1. Sample
The sample consisted of 3,075 adults from the U.S. (n = 1,496) and Canada (n = 1,579). The mean age was 51 years old (SD = 14 years, range 18–94 years), which is population representative of the mean age of adults (≥18 years) in the U.S. and Canada. Approximately half of the respondents (51%) were female, most (91%) were employed full- or part-time, and most (82%) had completed full or partial college. Most (63%) were Caucasian, with the remainder being Asian (14%), African American/Black (10%), Latinx/Hispanic (7%), or other (5%). Only 2% of the sample reported being diagnosed with COVID-19.
2.2. Data collection procedures
Participants were recruited during May 6–19, 2020 as part of the COVID Stress Study (Taylor et al., 2020a, Taylor et al., 2020b, Taylor et al., 2020c). Unlike previous studies from this ongoing research program, the present study is the first to investigate substance use and abuse during the COVID-19 pandemic. The sample was recruited using an internet-based self-report survey delivered in English by Qualtrics, a commercial survey sampling company. Qualtrics maintains a pool of potential participants who have agreed to be contacted in order to respond to surveys. Qualtrics selected and contacted participants to meet sampling quotas based on age, gender, ethnicity, socioeconomic status, and geographic region within each country. All respondents provided written informed consent prior to completing the survey. The research described in this article was approved by the Research Ethics Board of the University of Regina (REB# 2020–043). Filters were used to eliminate data from careless responders. Embedded in the assessment battery were four attention-check items (e.g., “This is an attention check, please select Strongly Agree”; “For our research, it is really important that you paid attention while responding to our survey. How attentive were you when responding?”: “Very Inattentive” to “Very Attentive”). Participants were included only if they provided correct responses to three or more of the four attention checks (e.g., “Strongly agree” or “Very attentive”), indicating that they were sufficiently attentive. In addition, at the end of the assessment battery, participants were asked to indicate whether, in their honest opinion, their data should be used. Those who responded “no” were excluded from data analysis, regardless of their score on the attention-check items.
2.3. Measures
Participants completed a battery of questionnaires. For each multi-item scale, McDonald (1999) ω total was used to measure the scale’s reliability (internal consistency). McDonald’s ω was used instead of Cronbach’s α because the latter tends to underestimate reliability (McNeish, 2018). Values of ω are interpreted in the same way as α; that is, values in the range of 0.70–0.79 indicate acceptable reliability, 0.80–0.89 indicate good reliability, and values greater than 0.90 indicate excellent reliability. All scales had good to excellent reliability, as shown below. Further details of the scales are as follows.
The COVID Stress Syndrome was assessed by the five COVID Stress Scales (Taylor et al., 2020b): (1) Worry about the dangerousness of COVID-19 and worry about coming into contact with objects or surfaces potentially contaminated with the coronavirus (12 items, ω = 0.96), (2) worry about the socioeconomic consequences of COVID-19 (e.g., worry about personal finances and worry about disruption in the supply chain) (6 items, ω = 0.94), (3) xenophobic fears that foreigners are spreading the coronavirus (6 items, ω = 0.96), (4) traumatic stress symptoms associated with direct or vicarious exposure to COVID-19 (e.g., nightmares, intrusive thoughts) (6 items, ω = 0.96), and (5) COVID-19-related compulsive checking and reassurance-seeking (6 items, ω = 0.90).
The COVID Disregard Syndrome was assessed by three measures (Taylor et al., 2020a): (1) Belief that the dangerousness of COVID-19 has been exaggerated (e.g., “The dangerousness of COVID-19 has been exaggerated by the media”) (3 items, ω = 0.89), (2) belief in one’s robust physical health in the face of COVID-19 (e.g., “If I was infected, I would experience only mild symptoms”) (3 items, ω = 0.91), and (3) disregard for social distancing (e.g., “If I was infected, it would be no big deal if I went out and socialized with friends”) (3 items, ω = 0.88).1
The assessment battery contained two measures of substance abuse (alcohol abuse and drug abuse), measures of whether substance use (alcohol or drugs) had increased during the pandemic, and measures of whether substance use had increased as a means of coping during self-isolation. Details are as follows.
The measures of alcohol and drug abuse were adapted from the World Health Organization’s 10-item Alcohol Use Disorders Identification Test (AUDIT; Babor, Higgins-Biddle, Saunders, & Monteiro, 2001). The AUDIT was used to create both the drug and alcohol abuse measures so that the scales had a comparable methodology (i.e., to reduce any complications in comparing drug and alcohol scores that might be due to differences in method variance). We selected the AUDIT because it is widely used and could be readily adapted to create two scales assessing COVID-19-related alcohol and drug abuse, using a common response format. The result was a scale assessing COVID-19-related alcohol abuse (9 items, ω = 0.88) and a scale measuring recreational drug abuse (6 items, ω = 0.82).
The original version of the AUDIT assesses alcohol consumption over the past year, whereas the COVID-19-related alcohol and drug scales adapted from the AUDIT specifically assessed substance abuse since the COVID-19 outbreak. Modifications to the AUDIT to create the COVID-19-related alcohol and drug scales were as follows. One item from the original AUDIT (“How often during the last year have you failed to do what was normally expected of you because of drinking?”) was removed from both the alcohol and drug scales because the COVID-19 pandemic entailed restrictions on what was normally expected of a person (e.g., COVID-19-related limitations on the person’s social and occupational functioning, due to self-isolation and workplace closures). Three other items from the AUDIT were dropped from the drug abuse scale because they were not relevant to the consumption of recreational drugs: (1) “How often do you have six or more drinks on one occasion?”; (2) “how often have you found that you were not able to stop drinking once you had started?”; and (3) “how often have you needed a first drink in the morning to get yourself going after a heavy drinking session?”
Participants also completed yes/no questions as to whether their consumption of alcohol or recreational drugs had increased since the outbreak of the COVID-19 pandemic. These questions were answered by those participants who indicated that they consumed drugs or alcohol. At the time of assessment, it had been only two months since the pandemic had been officially declared. We asked participants a simple yes/no question as to whether their consumption of substances had increased during versus before the pandemic. Retrospective assessments based on longer follow-back intervals are commonly used in substance use research (e.g., Rodriguez et al., 2020) and have been found to have acceptable levels of reliability and validity (e.g., Robinson, Sobell, Sobell, & Leo, 2014). In the present study, the recall interval was brief, the assessment was a simple yes/no question, and assessment was anonymous. Accordingly, there was no reason to expect that the assessment would have been subject to systematic error.
At the time of data collection, self-isolation guidelines varied widely across communities, and only some communities were asking people to self-isolate. Moreover, many people had jobs that were regarded as essential services (e.g., grocery store workers, workers in some types of factories, workers in the energy sector) and so were not subjected to the same stay-at-home advisories as those of other people in the community. For those people in self-isolation, they were asked to complete measures that were prefaced by the following statement: “The following questions pertain to self-isolation and quarantine. Please note: ‘self-isolation’ refers to voluntary separation from others. ‘Quarantine’ refers to mandatory separation from others.” Participants were then asked whether they were in quarantine or self-isolation. Participants who were in self-isolation at the time of the study (n = 1079) completed the following questions: (1) Whether they were using alcohol or other drugs to cope with self-isolation (yes/no response), (2) a 12-item scale assessing a range of stressors associated with self-isolation (e.g., difficulty taking care of children, crowding; yes/no responses; ω = 0.83), and (3) a 6-item scale assessing the severity of distress reactions to self-isolation (e.g., anxiety, depression, irritability; 0 = not at all to 4 = extremely; ω = 0.93).
2.4. Statistical procedures
2.4.1. Alpha level and interpretation of effect sizes
The alpha was set at 0.01 instead of the conventional 0.05. Unlike more stringent methods (e.g., Bonferroni correction), this adjustment corrects for inflated Type I error without simultaneously inflating Type II error. Given the large sample size, substantively trivial effect sizes would be statistically significant (e.g., for r = 0.05, p < .01). Accordingly, to facilitate the interpretation of correlations, we used Cohen (1988) criteria to classify effect sizes as small (r = 0.10), medium (r = 0.30), or large (r = 0.50). To give precision to these classifications for rs falling between these values, we classified r in terms of ranges, using the midpoint between 0.10 and 0.30, and midpoint between 0.30 and 0.50, so as to distinguish among small, medium, and large rs; that is, small = 0.10 to 0.19, medium = 0.20 to 0.39, and large greater than 0.39. To correct for measurement error, correlations were disattenuated (Osborne, 2002) according to the following formula: r disattenuated = r xy/√(ωx*ωy), where ωx and ωy are the reliabilities (McDonald’s ω) for each variable.
2.4.2. Network analysis
Glasso networks (regularized partial correlation networks) were computed using the R qgraph package (Epskamp et al., 2016, Epskamp et al., 2018). Two network analyses were conducted, including one for people who consumed alcohol (n = 2128) and another for people who reported using recreational drugs (n = 495). Separate network analyses were conducted because most people who used alcohol (77%) did not use recreational drugs. The network analyses focused on substance abuse rather than use because of the clinical and public health importance of substance abuse.
3. Results
3.1. COVID-19-related increases in substance use
Most of the sample (69%, n = 2128) reported consuming alcohol during the pandemic. A total of 23% of people who drank alcohol prior to the pandemic reported that their consumption had increased. For people who reported consuming recreational drugs during the pandemic (16%, n = 495), 31% reported that their consumption had increased since the COVID-19 outbreak.
The increased pandemic-related consumption of alcohol was significantly correlated with AUDIT alcohol abuse scores (r = 0.44, p < .001), and the pandemic-related increase in substance use was significantly correlated with AUDIT drug abuse scores (r = 0.51, p < .001). This indicates that pandemic-related increases in substance use tended to be hazardously high increases (i.e., increases in degree of substance abuse).
3.2. Correlates of COVID-19-Related substance use and abuse
Table 1 shows that demographic variables had mostly small or nonsignificant correlations with substance use/abuse variables. A notable exception was age, in which younger adults, compared to older individuals, tended to have higher levels of alcohol and drug use and abuse. The table further shows that various indices of the severity of alcohol and drug abuse were correlated with the nodes of both the COVID Stress Syndrome and the COVID Disregard Syndrome, with the strongest correlations being between substance abuse and COVID-19-related traumatic stress symptoms and compulsive checking.
Table 1.
Disattenuated correlations among substance-use variables, COVID Stress Syndrome variables (CSS), COVID Disregard Syndrome variables (DRS), and demographic variables.
 |
*p < .01, **p < .005, ***p < .001. Effect sizes: Red = large, pink = medium, yellow = small.
CHE = COVID-19-related compulsive checking and reassurance-seeking; DAN = Worry about the dangers of COVID-19 and worry about coming into contact with coronavirus contaminated objects or surfaces; DIS = Disregard for social distancing; EXG = Belief that the threat of COVID-19 has been exaggerated; ROB = Belief that one has robust physical health against COVID-19; SEC = Worry about the personal socioeconomic impact of COVID-19; TSS = COVID-19-related traumatic stress symptoms; XEN = Xenophobic worries that foreigners are spreading COVID-19.
3.3. Substance use and abuse during Self-Isolation
For people in self-isolation at the time of the study (35%, n = 1079), the mean duration of self-isolation was 48 days (SD = 20 days, range 1–100 days). Only a subsample was in self-isolation at the time of data collection because not all communities had imposed voluntary self-isolation restrictions and also because some participants were essential service workers (e.g., grocery store workers) and therefore not subjected to the self-isolation restrictions that were imposed on other members of their communities.
For people in self-isolation, 26% reported that they tried to cope with self-isolation by consuming more drugs or alcohol than they normally would. This coping strategy was correlated with self-isolation stressors (r = 0.23, p < .001), self-isolation distress (r = 0.29, p < .001), AUDIT alcohol abuse scores (r = 0.52, p < .001), and AUDIT drug abuse scores (r = 0.39, p < .001). The AUDIT findings suggest that coping via substance use tended to be associated with hazardous levels of substance consumption.
3.4. Network analyses
3.4.1. Alcohol abuse
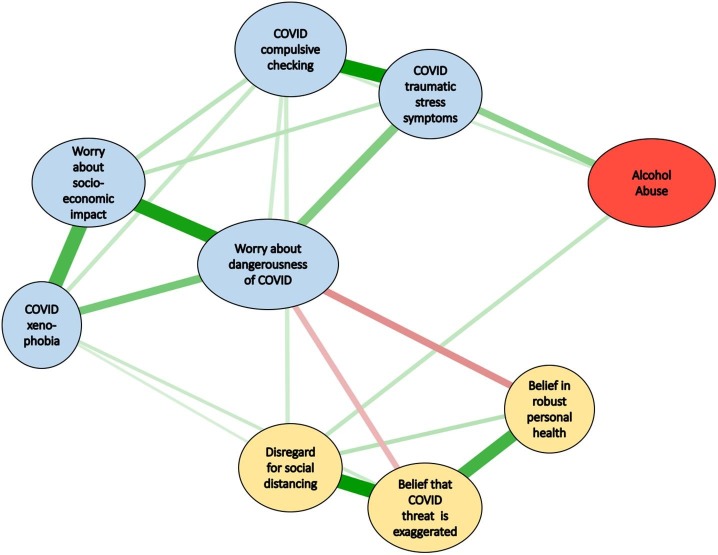
Fig. 1 shows the edges (regularized partial correlations) between nodes (for all edges, p < .001). The more important edges are indicated by shorter, thicker lines, with positive correlations in green and negative correlations in red. The numerical values of the edges are in Supplement 1. For Fig. 1, the Coefficients of Stability were r = 0.75 for both edges and strength of nodes. These values exceed the cutoff of 0.50 (Epskamp et al., 2018), indicating that the relative strength (i.e., relative importance) of the values of the nodes and their edges were stable (reliable). In Fig. 1 the blue ellipses represent the COVID Stress Syndrome and the yellow ellipses represent the COVID Disregard Syndrome. Fig. 1 shows that COVID-19-related alcohol abuse was most closely related to COVID-19-related traumatic stress symptoms, followed in strength by a connection with COVID-19-related disregard for social distancing.
Fig. 1.
Network analysis for alcohol abuse: Strength of edges (regularized partial correlations) among nodes in the network (green = positive and red = negative edges). Stronger edges are indicated by shorter and thicker lines. For all edges, p < .001. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
3.4.2. Drug abuse
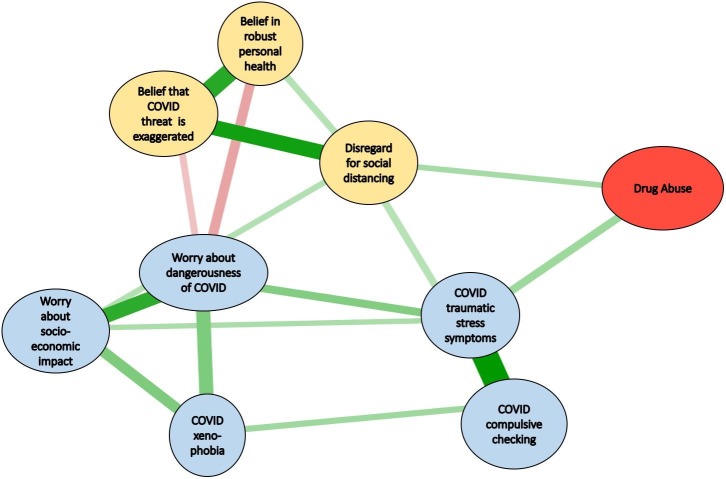
Fig. 2 shows the edges between nodes in the network (for all edges, p < .01). Numerical values of the edges appear in Supplement 1. For Fig. 2, the Coefficients of Stability were r = 0.75 for edges and r = 0.67 for strength of nodes, indicating that the relative strength edges and nodes were reliable. Fig. 2 shows that COVID-19-related drug abuse was closely related to COVID-19-related traumatic stress symptoms, with a secondary link with COVID-19-related disregard for social distancing.
Fig. 2.
Network analysis for drug abuse: Strength of edges (regularized partial correlations) among nodes in the network (green = positive and red = negative edges). Stronger edges are indicated by shorter and thicker lines. For all edges, p < .01. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
4. Discussion
For people who consumed recreational drugs or alcohol prior to the COVID-19 pandemic, substance use increased substantially during the pandemic, and many people increase their consumption of substances in order to cope with self-isolation. The COVID Stress Syndrome and COVID Disregard Syndrome were both associated with substance use and abuse. Traumatic stress symptoms and disregard for social distancing had especially strong links to alcohol and drug abuse. Fig. 1, Fig. 2 shows that worry about the dangerousness of COVID-19 was central to the network (i.e., linked to most other nodes), suggesting that targeting this node might lead to reductions in substance abuse. A complicating factor, however, is that this worry was negatively correlated with the disregard syndrome. These findings highlight the complexities in managing pandemics at a community level. Messages from health authorities that alleviate concerns for highly anxious people might exacerbate the disregard for social distancing among people who view the risks of COVID-19 as being exaggerated. That said, the network analyses suggest that targeting both COVID-19-related traumatic stress symptoms (e.g., via cognitive-behavior therapy) and the disregard for social distancing (via community announcements) might both have beneficial impacts on COVID-19-related substance abuse.
This study has a number of limitations that warrant consideration and provide directions for future investigation. First, the measures of drug and alcohol abuse were based on adaptations of the 10-item AUDIT. It was necessary to create adaptations because there were no measures of substance abuse available that were adapted to the specifics of the constraints imposed by the COVID-19 pandemic. The adaptations involved, for example, omitting items such as “How often during the last year have you failed to do what was normally expected of you because of drinking?” The omission of this item was unavoidable given that normal expectations for functioning were ambiguous, given the limitations on functioning imposed by pandemic control measures such as social distancing and self-isolation. Further research is needed to develop COVID-19-specific (or pandemic-specific) measures of substance abuse.
A second limitation is that we did not assess the type of drugs used. It is likely that the primary drug used in our sample was cannabis, which is legal in Canada and in some parts of the U.S. Nor did we assess use of other addictive substances, such as nicotine. Finally, the causal status of the links in the networks remains to be investigated. If the links are causal in nature, then the question arises as to the nature of causality (e.g., unidirectional, bidirectional).
5. Conclusion
Results indicated substantial COVID-19-related increases in alcohol abuse (23%) and drug abuse (16%) for people who consumed substances prior to the pandemic. Network analyses indicated that, although the COVID Stress Syndrome and COVID Disregard Syndrome are negatively correlated, they both have positive links to alcohol and drug abuse. COVID-19-related traumatic stress symptoms and the tendency to disregard social distancing were both linked to alcohol and drug abuse. Although further research is needed to investigate the causal nature of these associations, the findings are consistent with previous research suggesting that substance abuse is a common means of coping with traumatic stress symptoms. To our knowledge, this study is the first to provide evidence supporting concerns that substance abuse may undermine social distancing programs.
Role of Funding Sources
This research was funded by the Canadian Institutes of Health Research (#439751) and the University of Regina. These funding agencies had no role in the study design, collection, analysis or interpretation of the data, writing the manuscript, or the decision to submit the paper for publication.
CRediT authorship contribution statement
Steven Taylor: Conceptualization, Formal analysis, Writing - original draft, Funding acquisition, Methodology, Writing - review & editing. Michelle M. Paluszek: Methodology, Data curation, Project administration, Writing - review & editing. Geoffrey S. Rachor: Methodology, Data curation, Project administration, Writing - review & editing. Dean McKay: Writing - review & editing. Gordon J.G. Asmundson: Funding acquisition, Methodology, Writing - review & editing.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Note that for the measure of disregard for social distancing, the scale measures an extreme disregard for social distancing; that is, disregard even if the respondent had COVID-19.
References
- Babor T.F., Higgins-Biddle J.C., Saunders J.B., Monteiro M.G. 2nd ed. World Health Organization; Geneva: 2001. The Alcohol Use Disorders Identification Test: Guidelines for use in primary care. [Google Scholar]
- Bosque-Prous M., Espelt A., Sordo L., Guitart A.M., Brugal M.T., Bravo M.J. Job loss, unemployment and the incidence of hazardous drinking during the late 2000s recession in Europe among adults aged 50–64 years. PLoS ONE. 2015;10 doi: 10.1371/journal.pone.0140017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J. 2nd ed. Erlbaum; Hillsdale, NJ: 1988. Statistical Power Analyses for the Behavioral Sciences. [Google Scholar]
- Epskamp S., Borsboom D., Fried E.I. Estimating psychological networks and their accuracy. Behavior Research Methods. 2018;50:195–212. doi: 10.3758/s13428-017-0862-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epskamp S., Maris G., Waldorp L.J., Borsboom D. Network psychometrics. In: Irwing P., Booth T., Hughes D.J., editors. vol. 2. Wiley; New York: 2016. pp. 953–985. (Wiley Handbook of Psychometric Testing). [Google Scholar]
- Galanter M., Kleber H.D., Brady K.T. 5th ed. American Psychiatric Publishing; Arlington, VA: 2015. American Psychiatric Publishing Textbook of Substance Abuse Treatment. [Google Scholar]
- Goodwin L.R. Substance abuse assessment. In: Marini I., Stebnicki M.A., editors. The professional counselor's desk reference. 2nd ed. Springer; New York: 2016. pp. 449–455. [Google Scholar]
- Grant B.F., Saha T.D., Ruan W.J., Goldstein R.B., Chou S.P., Jung J.…Hasin D.S. epidemiology of DSM-5 drug use disorder: Results from the national epidemiologic survey on Alcohol and related conditions–III. JAMA Psychiatry. 2016;73:39–45. doi: 10.1001/jamapsychiatry.2015.2132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasler G., LaSalle-Ricci V.H., Ronquillo J.G., Crawley S.A., Cochran L.W., Kazuba D.…Murphy D.L. Obsessive-compulsive disorder symptom dimensions show specific relationships to psychiatric comorbidity. Psychiatry Research. 2005;135:121–132. doi: 10.1016/j.psychres.2005.03.003. [DOI] [PubMed] [Google Scholar]
- Ipsos (2020a). CMHO/AMHO mental health week poll. Addictions and mental health Ontario. https://amho.ca/wp-content/uploads/CMHO-AMHO-Ipsos-SLIDES_-May-6.pdf, accessed September 28, 2020.
- Ipsos (2020b). US COVID-19 aggregated topline report. https://www.google.com/search?client=firefox-b-e&q=Ipsos+US+COVID-19+aggregated+topline+report, accessed September 28, 2020.
- Ipsos (2020c). More suffering from under exercising, anxiety than other health concerns due to COVID-19: Poll. https://www.ipsos.com/en/more-suffering-under-exercising-anxiety-other-health-concerns-due-covid-19-poll, accessed September 28, 2020.
- McDonald R.P. Erlbaum; Hillsdale, NJ: 1999. Test theory: A unified approach. [Google Scholar]
- McKay D., Asmundson G.J.G. COVID-19 stress and substance use: Current issues and future preparations. Journal of Anxiety Disorders. 2020;74 doi: 10.1016/j.janxdis.2020.102274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNeish D. Thanks coefficient alpha: We’ll take it from here. Psychological Methods. 2018;23:412–433. doi: 10.1037/met0000144. [DOI] [PubMed] [Google Scholar]
- Morning Consult (2020). Cooped up at home, millennials most likely among all adults to turn to food, alcohol. https://morningconsult.com/2020/04/06/coronavirus-social-distancing-millennials-eating-drinking/, accessed September 28, 2020.
- Nadkarni A., Kapoor A., Pathare S. COVID-19 and forced alcohol abstinence in India: The dilemmas around ethics and rights. International Journal of Law and Psychiatry. 2020;71 doi: 10.1016/j.ijlp.2020.101579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nanos (2020). COVID-19 and increased alcohol consumption: Nanos poll summary report. https://www.ccsa.ca/covid-19-and-increased-alcohol-consumption-nanos-poll-summary-report, accessed September 28, 2020.
- Osborne J.W. Effect Sizes and the disattenuation of correlation and regression coefficients: Lessons from educational psychology. Practical Assessment, Research, and Evaluation. 2002;8:1–7. doi: 10.7275/0k9h-tq64. [DOI] [Google Scholar]
- Pihl R.O., Shakra M.A. Substance abuse: Etiological considerations. In: Blaney P.H., Krueger R.F., Millon T., editors. Oxford textbook of psychopathology. 3rd ed. Oxford University Press; New York: 2015. pp. 275–311. [Google Scholar]
- Rehm J., Kilian C., Ferreira-Borges C., Jernigan D., Monteiro M., Parry C.D.H.…Manthey J. Alcohol use in times of the COVID-19: Implications for monitoring and policy. Drug and Alcohol Review. 2020;39:301–304. doi: 10.1111/dar.13074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reynolds J., Wilkinson C. Accessibility of “essential” alcohol in the time of COVID-19: Casting light on the blind spots of licensing? Drug and Alcohol Review. 2020;39:305–308. doi: 10.1111/dar.13076. [DOI] [PubMed] [Google Scholar]
- Robinson S.M., Sobell L.C., Sobell M.B., Leo G.I. Reliability of the timeline Followback for cocaine, cannabis, and cigarette use. Psychology of Addictive Behaviors. 2014;28:154–162. doi: 10.1037/a0030992. [DOI] [PubMed] [Google Scholar]
- Rodriguez L.M., Litt D.M., Stewart S.H. Drinking to cope with the pandemic: The unique associations of COVID-19-related perceived threat and psychological distress to drinking behaviors in American men and women. Addictive Behaviors. 2020;110 doi: 10.1016/j.addbeh.2020.106532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rotermann M. Statistics Canada; Ottawa: 2020. Canadians Who Report Lower Self-Perceived Mental Health During the COVID-19 Pandemic More Likely to Report Increased Use of Cannabis, Alcohol and Tobacco. [Google Scholar]
- Smith S.M., Goldstein R.B., Grant B.F. The association between post-traumatic stress disorder and lifetime DSM-5 psychiatric disorders among veterans: Data from the National Epidemiologic Survey on Alcohol and Related Conditions-III (NESARC-III) Journal of Psychiatric Research. 2016;82:16–22. doi: 10.1016/j.jpsychires.2016.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor S. 2nd ed. Guilford; New York: 2017. Clinician’s guide to PTSD. [Google Scholar]
- Taylor S. Cambridge Scholars Publishing; Newcastle upon Tyne: 2019. The psychology of pandemics: Preparing for the next global outbreak of infectious disease. [Google Scholar]
- Taylor S., Landry C.A., Paluszek M.M., Asmundson G.J.G. Reactions to COVID-19: Differential predictors of distress, avoidance, and disregard for social distancing. Journal of Affective Disorders. 2020;277:94–98. doi: 10.1016/j.jad.2020.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor S., Landry C.A., Paluszek M.M., Fergus T.A., McKay D., Asmundson G.J.G. Development and initial validation of the COVID Stress Scales. Journal of Anxiety Disorders. 2020;72 doi: 10.1016/j.janxdis.2020.102232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor S., Landry C.A., Paluszek M.M., Fergus T.A., McKay D., Asmundson G.J.G. COVID stress syndrome: Concept, structure, and correlates. Depression and Anxiety. 2020;37:706–714. doi: 10.1002/da.23071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright A.J., Henes R. Preventing substance abuse and addiction. In: MacMillan T., Sisselman-Borgia A., editors. New directions in treatment, education, and outreach for mental health and addiction. Springer; Cham, Switzerland: 2018. pp. 231–254. [Google Scholar]