Abstract
People who experience childhood abuse are at increased risk for mental illness. Twin studies suggest that inherited genetic risk for mental illness may account for some of these associations. Yet the hypothesis that individuals who have experienced childhood abuse may carry genetic loading for mental illness has never been tested with genetic data. Using polygenic risk scores for six psychiatric disorders - attention-deficit hyperactivity disorder (ADHD), autism spectrum disorder (ASD), bipolar disorder (BPD), major depressive disorder (MDD), neuroticism, and schizophrenia – we tested whether genetic risk for mental illness was associated with increased risk of experiencing three types of childhood abuse: physical/emotional abuse, physical assault, and sexual abuse, in a cohort of white non-Hispanic women (N=11,315). ADHD and MDD genetic risk scores were associated with higher risk of experiencing each type of childhood abuse, while neuroticism, schizophrenia, BPD, and ASD genetic scores were associated with higher risk of experiencing physical/emotional abuse and physical assault, but not sexual abuse. Sensitivity analyses examining potential bias from differential recall of childhood trauma, parental socioeconomic status, and population stratification were consistent with the main findings. A one standard deviation increase in genetic risk for mental illness was associated with modestly elevated risk of experiencing childhood abuse (OR range: 1.05-1.19). Therefore, inherited genetic risk may partly account for the association of childhood abuse with mental illness. In addition, future treatments for mental illness will benefit from taking into consideration the co-occurrence of childhood trauma and genetic loading.
Introduction
Nearly 30% of US children are exposed to physical, sexual, or emotional abuse1 that is associated with serious physical and mental health outcomes across their lifespans.2 The strong association between childhood abuse and mental illness is assumed to be due to the causal effects of child abuse on later mental illness. However, it has also been proposed that individuals who experienced childhood abuse may carry genetic loading for mental illness, which may account for some of the association between experiencing childhood abuse and mental illness.3–6 Twin studies that compare the mental health outcomes of twins who did and did not experience childhood abuse suggest that the association between childhood abuse and borderline personality disorder,3 major depression,4 panic disorder,4 and alcoholism4 may be in part due to genetic loading. The co-occurrence of environmental factors such as childhood abuse and genetic risk is termed gene-environment correlation (rGE). Prior studies using genome-wide data have found several early-life environmental factors, including maternal and paternal age at gestation,7, 8 maternal years of education, and maternal alcohol use and anxiety during pregnancy7 associated with genetic risk for mental illness.
Three potential pathways exist by which the genetic risk for mental illness could confound the association between mental illness and experiences of childhood abuse (Figure 1). First, passive rGE posits that mentally ill parents (e.g., generation 0, G0) are more likely than those without mental illness both to pass on genetic risk for mental illness and to have children (generation 1, G1) who are abused (Figure 1, Panel A).9 Several studies have shown that parental schizophrenia, bipolar disorder (BPD), ADHD, and mood and anxiety disorders are associated with increased risk of offspring experiencing childhood abuse.10–17 Such mental illnesses are also genetically influenced, such that the child would be at greater risk for these because of genetics inherited from the parents. Thus, rather than abuse causing mental illness in this scenario, abuse and mental illness co-occur due to shared genetic risk.18
Figure 1.
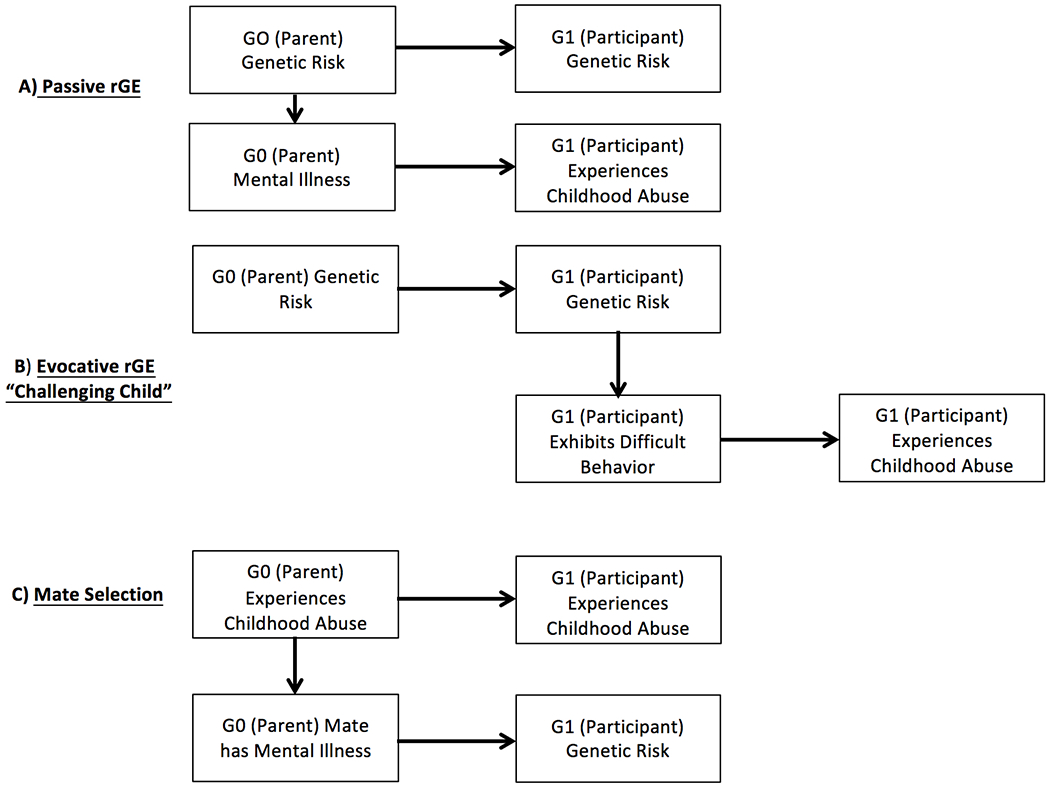
Potential genetic pathways account for the correlation between risk for mental health disorders and childhood abuse. G0 = Generation 0, the Nurses’ Health Study 2 participants’ parents, G1 = Generation 1, the NHS2 participants.
Second, in the evocative rGE pathway, or “challenging child hypothesis”, persons (G1) with genetic risk for mental illnesses may exhibit psychopathology-associated difficult behaviors as children, leading to an increased risk of experiencing child abuse (Figure 1, Panel B).3 For example, behavioral difficulties in children with ADHD and ASD,19 such as aggression, inattention, and oppositional behavior, have been linked to negative and controlling parental practices and reduced parental affection.20–25
Finally, mate selection may lead to rGE (Figure 1, Panel C). Persons (G0) who have experienced childhood abuse may be more likely as adults to select mates (also G0) with mental illness. Studies have indicated, for example, that persons exposed to child abuse are more likely to select mates with autistic traits26 and alcoholism.27 Their children (G1) would be at elevated risk of experiencing abuse due to behavioral transmission of abuse from the parent who experienced abuse, and would be at risk of inheriting the mentally ill parent’s genetic loading for mental illness.15, 28
However, the hypothesis that genetic risk for mental illness confounds the association between experiencing childhood abuse and later mental illness, which could occur through any of the three pathways depicted in Figure 1, has never been tested with molecular genetic data. The question of the degree to which childhood abuse causes psychopathology is a key question, relevant to both etiologic research and the development of interventions.29 Individual-level genetic risk for mental illness can be estimated using polygenic risk scores (PRS) that apply results from published genome-wide association studies (GWAS) to individuals’ measured genetic variants to estimate their genetic risk. The present study investigated rGE for child abuse and mental illness using molecular genetic data. We applied publicly available summary statistics from GWAS of ADHD,30 ASD,31 bipolar disorder,32 major depressive disorder (MDD),33 neuroticism,34 and schizophrenia35 to genetic data from the Nurses’ Health Study 2 (NHS2) to examine whether genetic risk for mental illness was associated with childhood physical, emotional, and sexual abuse (through any of the pathways described). We aimed to assess the presence of rGE, but not to distinguish among the specific pathways described in Figure 1.
Materials and methods
The NHS2 is an on-going cohort of 116,430 female nurses recruited in 1989 and assessed every two years. Participants were 24-44 years old at baseline. Blood samples were collected from 29,611 participants between 1996 and 1999, as previously described.36 Genome-wide data was available for 13,313 women based on three genotyping platforms: 1) Illumina Human Hap Array (N = 781), 2) Illumina OncoArray (N = 2,722), and 3) Illumina HumanCore Exome Chip (Batch 1 N = 3,276; Batch 2 N = 4,568). Following a standard quality control pipeline (call rate >0.90), participant genotype data were imputed using 1000 Genomes phase 3 reference data.37 Participants were restricted to those of European ancestry, given that PRS for mental illness were developed from GWAS of Europeans and may perform poorly for other ancestries due to differences in linkage disequilibrium patterns and the frequency of minor alleles.38 Informed consent was received from all participants and the study protocol was approved by the Institutional Review Boards of the Brigham and Women’s Hospital and the Harvard T.H. Chan School of Public Health.
Polygenic Risk Scores
PRS for ADHD,30 ASD,31 BPD,32 MDD,33 neuroticism,34 and schizophrenia35 were calculated using the summary statistics from the largest published GWAS, with p-value thresholds, clumping parameters, minor allele frequencies, and imputation score cutoffs based on those found to explain maximum variance based on Nagelkerke’s R2 from each analysis (see Supplemental Table 1).39, 40 Participant’s PRS for each mental illness were calculated by taking the weighted sum of risk alleles, with each allele weighted by the log odds ratio reported in published GWAS summary statistics using PRSice-2.41, 42 PRS were then standardized using z-score transformations.
Childhood Abuse
Childhood physical, emotional, and sexual abuse were assessed in a 2001 questionnaire. More than 11,000 women with genetic data responded to this questionnaire (n=11,347, 85% of women with genetic data). Five questions from the Physical and Emotional Abuse Subscale of the Childhood Trauma Questionnaire (CTQ) were used to assess physical/emotional abuse before age 12 years.43 The frequency of family members: 1) hitting so hard it left bruises, 2) punishing in a way that seemed cruel, 3) insulting, 4) screaming and yelling, and 5) punishing with a belt or other hard object was queried. In a validation study for the Childhood Trauma Questionnaire, these questions were found to load on a common factor of physical and emotional abuse (Cronbach’s alpha = 0.94, test-retest reliability = 0.82).44 Responses of never (0), rarely (1), sometimes (2), often (3), or very often (4) were summed, with the resulting scale dividing into quartiles.
Physical assault before age 18 was assessed for two time periods, ages 0-11 and 12-17 years, using items from the Physical Assault Subscale of the Revised Conflict Tactics Scale (CTS).45 Five questions were asked for each time period about whether a participant’s parent, step-parent, or adult guardian ever 1) pushed, grabbed or shoved you, 2) kicked, bit, or punched you, 3) hit you with something that hurt your body, 4) choked or burned you, and 5) physically attacked you in some other way. Response options were “Never” (0), “Once” (1), “A few times” (3), and “More than a few times” (4). Responses were summed, following coding recommendations.45 46% of respondents reported no events; the remainder were classified as having experienced mild, moderate, or severe physical assault.
Sexual abuse was assessed with the Sexual Maltreatment Scale of the Conflict Tactics Scales46, which consists of two questions regarding unwanted sexual touching and forced or coerced sexual contact by an adult or older child before age 12 years and two questions about experiences between ages 12-17 years. Participants could respond, “No this never happened” (0), “Yes this happened once” (1), or “Yes this happened more than once” (2). Responses were summed and individuals classified as having experienced none (score=0), infrequent (score=1 or 2), moderately frequent (score=3 or 4), or frequent sexual abuse (score≥5).
Covariates
In 2005, the highest level of education completed by parents was queried, which were coded as: ≤ high school, some college, or ≥ 4 years college. Parents’ occupations were classified as: “skilled/service”, “unskilled”, “farmer”, “managerial /professorial”, or “other” worker. Depressive symptoms were ascertained by the 5-item Mental Health Inventory (MHI-5) in 1993, 1997 and 2001. Women who scored <60 at any of these time points were considered to have had probable depression before or at the time of the childhood abuse questionnaire.47, 48 In addition, we account for residual population stratification – systematic differences in allele frequencies among those of varying exposures to childhood abuse across ancestries that can lead to spurious results – by including 10 principal components derived from the GWAS data as covariates.49
Statistical Analyses
We first examined the distribution of parental education and occupation across each level of childhood abuse. Next, to determine the co-occurrence of the three types of child abuse, we calculated Spearman rank correlations. To determine the clustering of mental illness PRS in our sample, we calculated Pearson correlations between each pair of PRS.
To ascertain whether genetic risk for mental illness was associated with childhood abuse, we fit separate ordinal logistic models to estimate odds ratios (ORs) of child abuse level (e.g., quartiles for the CTQ and severity levels for the CTS and sexual abuse) in association with a one-standard deviation increase in PRS score. All models adjusted for parental education, parental occupation, genomic assay, and 10 GWAS principal components. The validity of the proportional odds assumption was assessed using Brant tests,50 graphical assessment of the parallel slopes across all levels of each outcome,51 and a likelihood test comparing an ordinal logistic model and multinomial (unconstrained) logistic model.
We conducted three sensitivity analyses. First, as depressive symptoms may influence the reporting of childhood abuse52 and are also likely associated with the MDD and neuroticism PRS, we calculated associations between PRS of MDD and neuroticism and each of the child abuse measures among women without probable depression at or before the 2001 assessment of childhood abuse (e.g., in 1993, 1997, or 2001). Second, to determine whether there may have been residual confounding by childhood socioeconomic status, we compared associations of PRS with child abuse with and without adjustment for parental education and occupation. Third, to examine whether there was an association with type rather than frequency of sexual abuse, we fit an ordinal logistic model using an alternative coding for sexual abuse, where individuals were classified as experiencing no sexual abuse, touching only, or forced sexual activity.
We also assessed potential bias from residual population stratification within our data, which may affect PRS,53, 54 by fitting our original ordinal logistic regression model without GWAS principal components, to assess whether population stratification affected the results. Additionally, we fit a second set of models including both GWAS principal components and self-reported ancestry (Southern European, Scandinavian, mixed, or other Caucasian) to investigate whether residual population stratification existed after controlling for GWAS principal components. Finally, we assessed whether residual population stratification within the NHS2 population was driving the association between PRS for mental illnesses and childhood abuse by simulating 1,000 sets of summary statistics containing 500,000 randomly selected SNPs and effect sizes (mean = 0, SD = 0.3, based on the SNPs we selected from the mental illness GWAS). These summary statistics, unassociated with childhood abuse but reflective of underlying allele frequency differences across populations within the NHS, were then used to create 1000 PRS for each participant. We estimated the association between each PRS and measure of child abuse and calculated the false positive rate as the percentage of simulated PRS associated with childhood abuse.
To assess whether a single PRS was responsible for the associations between each PRS and the outcome, for each outcome we fit an ordinal logistic regression with all six PRS, adjusted for parental education, parental occupation, assay, and GWAS principal components. Additionally, we generated new PRS for each mental illness by removing SNPs that were included in more than one PRS. Thus, these new PRS included SNPs unique to each mental illness.
Results
Women who experienced childhood abuse were more likely to have parents who had a high school degree or less and were unskilled workers, compared with women who experienced the lowest level of childhood abuse (Table 1). As anticipated, physical/emotional abuse (the CTQ) was strongly associated with physical assault (the CTS, r = 0.69). Sexual abuse was moderately associated with physical/emotional abuse (r = 0.23) and physical assault (r = 0.21) (Supplemental Table 2).
Table 1.
Descriptive statistics for age, parent education, and parent occupation across child abuse outcomes.
| Outcome | Levels | |||||
|---|---|---|---|---|---|---|
| Physical/Emotional Abuse (CTQ) | Quartile 1: Low | Quartile 2 | Quartile 3 | Quartile 4: High | Total | |
| N | 3,749 | 2,363 | 2,257 | 2,946 | 11,315 | |
| Age, Mean (SD) | 46.629 (4.491) | 46.337 (4.393) | 46.488 (4.441) | 46.858 (4.279) | 46.600 (4.409) | |
| Parent Education | ||||||
| HS or less | 1681 (44.8%) | 1132 (47.9%) | 1141 (50.6%) | 1567 (53.2%) | 5521 (48.8%) | |
| Some college | 1014 (27.0%) | 656 (27.8%) | 622 (27.6%) | 831 (28.2%) | 3123 (27.6%) | |
| College or more | 1054 (28.1%) | 575 (24.3%) | 494 (21.9%) | 548 (18.6%) | 2671 (23.6%) | |
| Parent Occupation | ||||||
| Skilled / Service Worker | 1871 (49.9%) | 1296 (54.8%) | 1262 (55.9%) | 1712 (58.1%) | 6141 (54.3%) | |
| Unskilled Worker | 306 (8.2%) | 209 (8.8%) | 201 (8.9%) | 345 (11.7%) | 1061 (9.4%) | |
| Farmer | 276 (7.4%) | 151 (6.4%) | 139 (6.2%) | 145 (4.9%) | 711 (6.3%) | |
| Managerial/Professorial | 1176 (31.4%) | 629 (26.6%) | 555 (24.6%) | 602 (20.4%) | 2962 (26.2%) | |
| Other | 120 (3.2%) | 78 (3.3%) | 100 (4.4%) | 142 (4.8%) | 440 (3.9%) | |
| Physical Assault (CTS) | None | Mild | Moderate | Severe | Total | |
| N | 5,044 | 2,247 | 2,824 | 1,207 | 11,322 | |
| Age, Mean (SD) | 46.415 (4.492) | 46.645 (4.344) | 46.628 (4.402) | 47.225 (4.129) | 46.600 (4.409) | |
| Parent Education | ||||||
| HS or less | 2280 (45.2%) | 1088 (48.4%) | 1470 (52.1%) | 685 (56.8%) | 5523 (48.8%) | |
| Some college | 1401 (27.8%) | 621 (27.6%) | 795 (28.2%) | 306 (25.4%) | 3123 (27.6%) | |
| College or more | 1363 (27.0%) | 538 (23.9%) | 559 (19.8%) | 216 (17.9%) | 2676 (23.6%) | |
| Parent Occupation | ||||||
| Skilled / Service Worker | 2565 (50.9%) | 1244 (55.4%) | 1637 (58.0%) | 697 (57.7%) | 6143 (54.3%) | |
| Unskilled Worker | 422 (8.4%) | 201 (8.9%) | 281 (10.0%) | 157 (13.0%) | 1061 (9.4%) | |
| Farmer | 366 (7.3%) | 140 (6.2%) | 149 (5.3%) | 56 (4.6%) | 711 (6.3%) | |
| Managerial/Professorial | 1516 (30.1%) | 575 (25.6%) | 633 (22.4%) | 243 (20.1%) | 2967 (26.2%) | |
| Other | 175 (3.5%) | 87 (3.9%) | 124 (4.4%) | 54 (4.5%) | 440 (3.9%) | |
| Sexual Abuse | None | Infrequent | Moderate | Frequent | Total | |
| N | 7,213 | 2,797 | 847 | 460 | 11,317 | |
| Age, Mean (SD) | 46.442 (4.454) | 46.855 (4.334) | 46.864 (4.252) | 46.941 (4.349) | 46.596 (4.410) | |
| Parent Education | ||||||
| HS or less | 3421 (47.4%) | 1396 (49.9%) | 452 (53.4%) | 250 (54.3%) | 5519 (48.8%) | |
| Some college | 1999 (27.7%) | 776 (27.7%) | 221 (26.1%) | 127 (27.6%) | 3123 (27.6%) | |
| College or more | 1793 (24.9%) | 625 (22.3%) | 174 (20.5%) | 83 (18.0%) | 2675 (23.6%) | |
| Parent Occupation | ||||||
| Skilled / Service Worker | 3841 (53.3%) | 1571 (56.2%) | 478 (56.4%) | 250 (54.3%) | 6140 (54.3%) | |
| Unskilled Worker | 650 (9.0%) | 261 (9.3%) | 100 (11.8%) | 48 (10.4%) | 1059 (9.4%) | |
| Farmer | 439 (6.1%) | 175 (6.3%) | 61 (7.2%) | 36 (7.8%) | 711 (6.3%) | |
| Managerial/Professorial | 2013 (27.9%) | 684 (24.5%) | 174 (20.5%) | 96 (20.9%) | 2967 (26.2%) | |
| Other | 270 (3.7%) | 106 (3.8%) | 34 (4.0%) | 30 (6.5%) | 440 (3.9%) | |
Correlations among the six mental illness PRS revealed three clusters: 1) schizophrenia, BPD and ADHD; 2) neuroticism and MDD; and 3) ASD (Figure 2). The schizophrenia, BPD, and ADHD PRS were each negatively correlated with the neuroticism and MDD PRS. The ASD PRS was uncorrelated with any other PRS.
Figure 2.
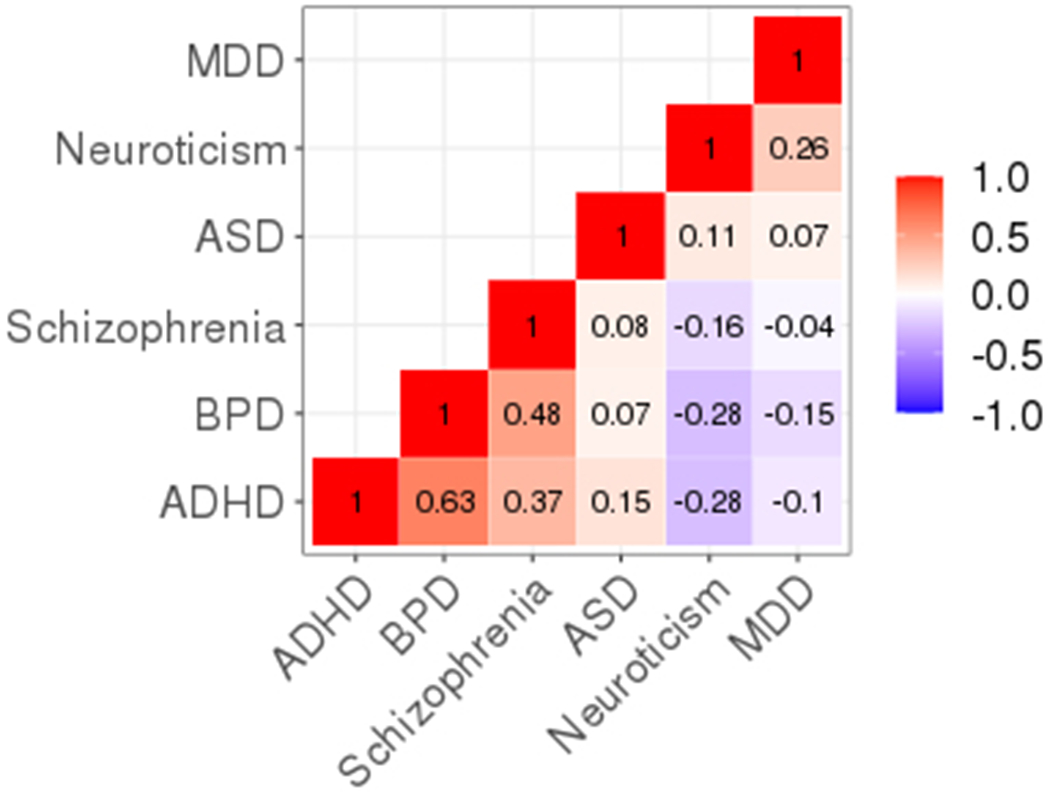
Correlations between polygenic risk scores for ADHD, ASD, BPD, MDD, neuroticism, and schizophrenia.
A one standard deviation increase in any of the six PRS was associated with increased risk of experiencing physical/emotional abuse: ADHD (OR=1.19, 95% CI=1.12, 1.26), MDD (OR=1.14, 95% CI=1.10, 1.18), neuroticism (OR=1.11, 95% CI=1.07, 1.15), schizophrenia (OR=1.11, 95% CI=1.07, 1.16), BPD (OR=1.09, 95% CI=1.03, 1.15), and ASD (OR=1.05, 95% CI=1.02, 1.09; Figure 3, Panel 1; Supplemental Table 3). PRS were similarly associated with physical assault (Figure 3, Panel 2). However, only the ADHD (OR=1.15, 95% CI=1.07, 1.23), and MDD (OR=1.07, 95% CI=1.03, 1.11) PRS were associated with sexual abuse (Figure 3, Panel 3).
Figure 3.
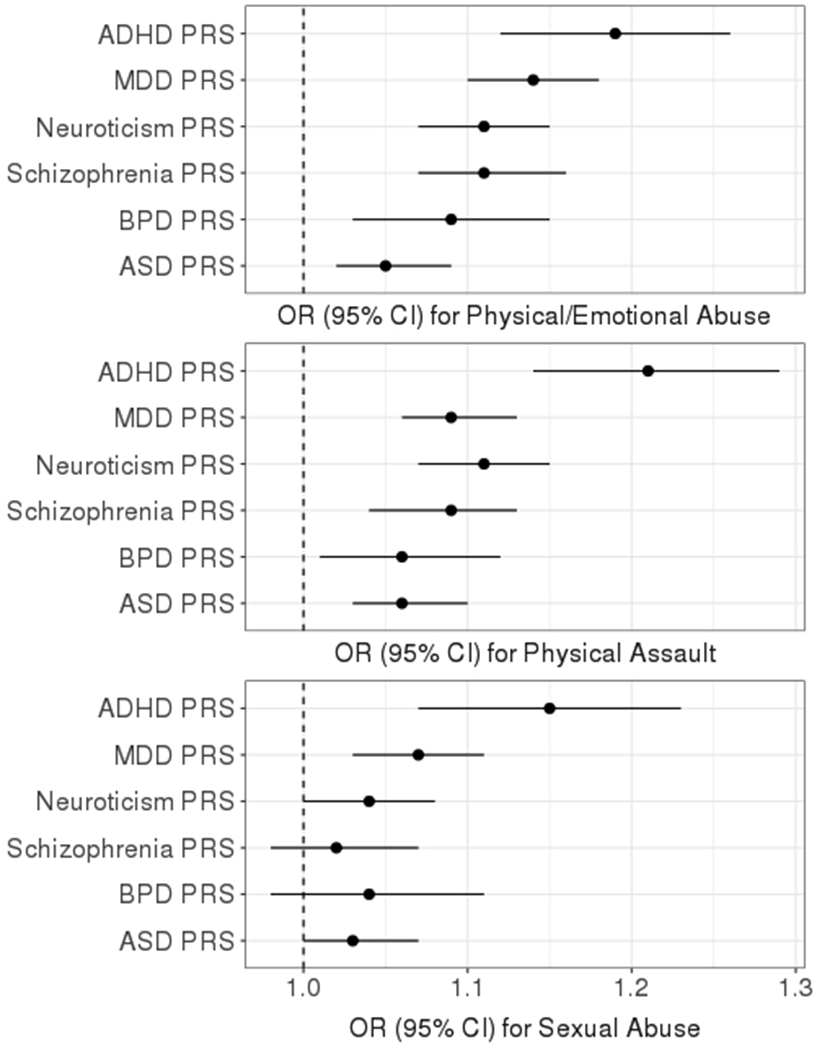
Odds ratios and 95% confidence intervals (CI) associated with a one standard deviation increase in each mental health polygenic risk score (PRS) for being in a higher level of childhood abuse adjusted for parental education, parental occupation, genomic assay, and 10 GWAS principal components.
Sensitivity Analyses
Depressive symptoms may influence the reporting of childhood abuse and induce an association of experiencing childhood abuse with the MDD PRS. However, in the sensitivity analysis restricted to women with no probable depression, associations between the PRS for MDD and neuroticism, which is closely linked to MDD, with physical/emotional abuse, physical assault, and sexual abuse were consistent with those in the full sample (Figure 4; Supplemental Table 4).
Figure 4.
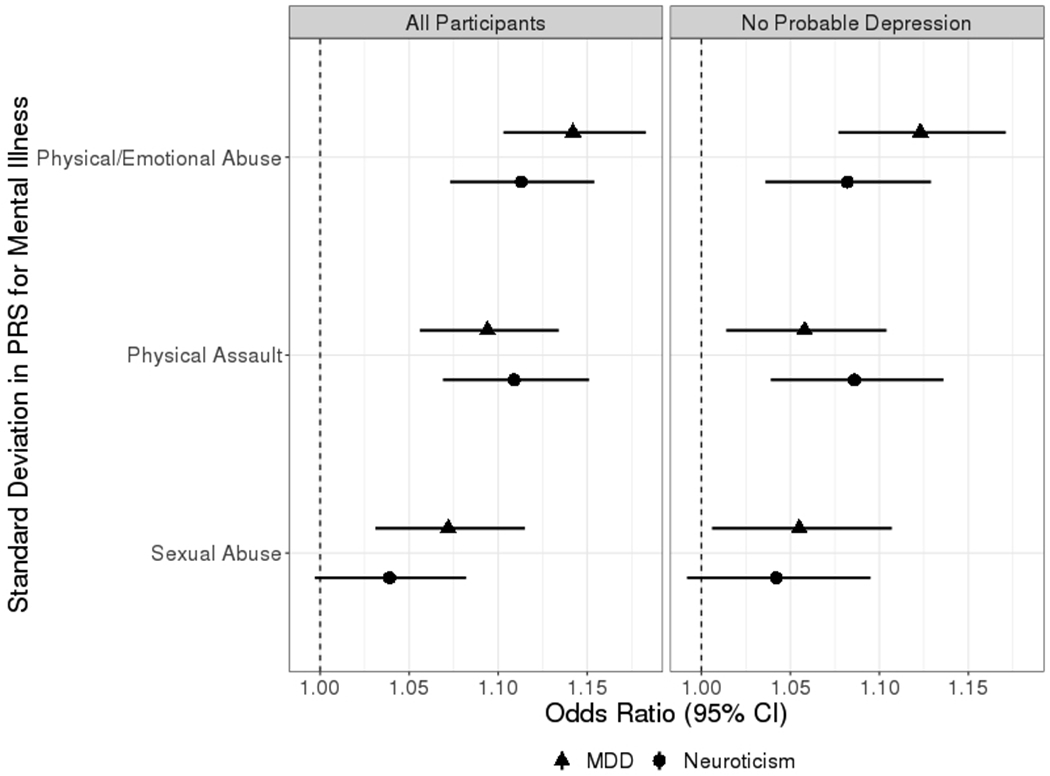
Odds ratios and 95% confidence intervals (CI) associated with a one standard deviation increase in the MDD and neuroticism polygenic risk score (PRS) for being in a higher level of childhood abuse, adjusted for parental education, parental occupation, genomic assay, and 10 GWAS principal components among all participants (Nphysical/emotional abuse = 11,315, Nphysical assault = 11,322, Nsexual abuse = 11,317) and among those with no probable depression (N = 7,994).
Results of models excluding parental occupation and education were consistent in direction and significance with the main results (Supplemental Table 5). Analyses examining residual population stratification in our population did not indicate bias. Models excluding GWAS principal components (Supplemental Table 5) and those including self-reported ancestry (Supplemental Tables 5, 6) were consistent with the main results. Simulated PRS indicated that GWAS principal components provided adequate adjustment for population structure, with false positive rates within the expected range: physical/emotional abuse 5.2%, physical assault 4.8%, and sexual abuse 4.7%. Analyses with childhood sexual abuse coded as none, touching-only, or forced sexual activity were consistent with the main results (Supplemental Table 7).
In analyses with PRS for all disorders included in a single model, results were consistent in direction with the main results (Supplemental Table 8). In models using PRS comprised only of SNPs unique to each disorder, associations were also consistent with the main results, except ASD was more strongly associated with childhood abuse in these analyses (Supplemental Table 9).
Discussion
This is the first study to use molecular genetics to examine the association of genetic risk for mental illnesses with the experience of childhood physical, emotional, and sexual abuse. We found that genetic loading for ADHD and MDD were associated with higher likelihood of experiencing childhood physical/emotional abuse, physical assault, and sexual abuse. In addition, we found that genetic risk for neuroticism, schizophrenia, BPD, and ASD were associated with higher risk of experiencing physical/emotional abuse and physical assault. These results were robust to possible recall bias, confounding by parental education and occupation, and residual population stratification. Furthermore, the effect of the PRS for each mental illness was independent of the other mental illness PRS, implying no single PRS was driving the associations between mental illness and experiencing childhood abuse.
Associations between genetic risk for mental illness and sexual abuse were smaller compared to associations with physical/emotional abuse and physical assault. This may be because physical and emotional abuse questions specifically queried actions by people in the family, parents, or step-parents, whereas sexual abuse queried actions by any adult or older child. It is therefore possible that the physical and emotional abuse items better captured family dysfunction that may be related to heritable genetic risk of mental illness.
Our findings suggest that rGE may explain part of the association between childhood abuse and adulthood mental illness. However these results do not discount other pathways.55 First, childhood abuse can lead to dysregulation of the HPA-axis, which controls the body’s stress response, with repeated activation resulting in deleterious effects on the brain that have been associated with developing MDD.56 Second, experiencing childhood abuse can lead to poor behavioral regulation, poor social support, and maladaptive coping that put individuals at risk for later mental illness.57 As genetic risk scores become further refined, the role of genetic factors in these associations can be explored more precisely.
Maternal abuse has also been associated with elevated risk of mental illness among offspring, including depression58, 59, anxiety60, 61, ADHD62, and ASD.63 Our findings suggest that genetic pathways may partly explain the co-occurrence of maternal experiences of childhood abuse with offspring mental illness. Previous studies have focused on two explanations for this intergenerational association. First, women who experience abuse are more likely to have children who also experience abuse, via behavioral transmission of childhood abuse across generations.15, 28 Therefore, these children are also at increased risk of mental illness as experiencing childhood abuse is a strong risk factor for many mental illnesses.58, 64–66 Second, women who experience childhood abuse are more likely to have perinatal risk factors that may place their children at increased risk of mental illness, including smoking and alcohol use during pregnancy, gestational diabetes, and preterm birth.60, 63, 67–70 Both pathways may be confounded by rGE, though no studies have examined the association between genetic risk for mental illness and perinatal risk factors for mental illnesses. As our understanding of the biology and genetics of these mental illnesses improves, interventions may become more targeted and effective.
Our study has at least four limitations. First, the PRS for ADHD,30 ASD,31 BPD,31 MDD,33 and neuroticism34 have been found to explain a small proportion of the variation when predicting out-of-sample mental health outcomes (Nagelkerke R2 range: 0.01 to 0.05, Supplemental Table 1). The use of PRS that explain little of the variation in mental illness may lead to attenuated estimates of the true associations between genetic risk and childhood abuse.71 This possibility is supported by our finding that the MDD PRS (Nagelkerke R2 = 0.05) was associated with sexual abuse, while the neuroticism PRS (Nagelkerke R2 = 0.028) was not significantly associated with sexual abuse, despite the neuroticism and MDD PRS being highly correlated (Figure 2). As sample sizes in discovery GWAS increase and the variability explained increases, we would expect concordance of associations across highly correlated PRS. Second, childhood abuse was queried retrospectively at ages 36-56 years, which may have resulted in misclassification. Third, while the inclusion of the first 10 principal components controlled for populations stratification in our sample, and our simulations also showed no bias, we are unable to adequately assess the residual population structure from the cohorts that were used to develop the PRS. Fourth, our study was conducted in a sample of high-functioning participants who are unlikely to include individuals with the greatest levels of risk for mental illness. Fifth, we were unable to elucidate which rGE pathway(s) affect the association between childhood trauma and later mental illness.
Future studies with measurement of mental illness, childhood trauma, and genetics in both parents and offspring will be needed to provide evidence for passive rGE, evocative rGE, or mate selection. For example, the passive and evocative rGE pathways could be examined through the associations of parent and offspring genetic risk, parental mental illness, offspring behaviors, and offspring experiences of childhood abuse. The presence of mate selection could be explored by examining the extent to which childhood abuse is associated with mate’s PRS, and whether this differs by sex. Although large samples would be likely be required, such studies could identify the degree to which each pathway accounts for the association between experiencing childhood abuse and later mental illness, albeit with the caveat that PRS currently explain only a portion of genetics-related phenotypic variance.
Our results suggest possible future research directions relevant to the etiology of mental illness. First, our findings suggest that rGE may be occurring in other circumstances. For example, rGE may account for some of the association between maternal perinatal health behaviors, e.g. smoking, and offspring neurodevelopmental risk. Maternal perinatal smoking has been found to be associated with offspring cognitive development.63 However, in a large sibling study (N=52,919) that examined discordant smoking behaviors across births using a sibling matching analysis to account for shared genetic risk, perinatal smoking was not associated with cognitive development, suggesting that rGE may account for the association of some perinatal risk factors with cognitive development.72
Our results indicate that genetic risk for mental illness is associated with modestly elevated risk of experiencing childhood abuse. Therefore, inherited genetic risk may account for part of the increased risk for mental illness in individuals who have experienced childhood abuse, and the increased risk for mental illness in their children. Improved genetic instruments will assist in developing targets for intervention to prevent mental illness and to better elucidate the role that experiencing childhood abuse has on later mental illness. Finally, future treatments for mental illness will benefit from taking into consideration the co-occurrence of childhood trauma and genetic risk.
Supplementary Material
Acknowledgements
This research was funded in part by R01HD094725 (to ALR). The Nurses’ Health Study II is funded by U01 CA176726. We would like to thank the participants and staff of the NHS2 for their valuable contributions and acknowledge the Channing Division of Network Medicine, Department of Medicine, Brigham and Women’s Hospital for its management of the NHS2. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Conflict of Interest
The authors have no conflicts of interest to declare.
References
- 1.Centers for Disease Control. Adverse Childhood Experiences Study. 1997. [Google Scholar]
- 2.Gilbert R, Widom CS, Browne K, Fergusson D, Webb E, Janson S. Burden and consequences of child maltreatment in high-income countries. The Lancet 2009; 373(9657): 68–81. [DOI] [PubMed] [Google Scholar]
- 3.Bornovalova MA, Huibregtse BM, Hicks BM, Keyes M, McGue M, Iacono W. Tests of a direct effect of childhood abuse on adult borderline personality disorder traits: a longitudinal discordant twin design. Journal of Abnormal Psychology 2013; 122(1): 180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dinwiddie S, Heath AC, Dunne MP, Bucholz KK, Madden PA, Slutske WS et al. Early sexual abuse and lifetime psychopathology: a co-twin–control study. Psychological medicine 2000; 30(1): 41–52. [DOI] [PubMed] [Google Scholar]
- 5.Distel MA, Middeldorp CM, Trull TJ, Derom CA, Willemsen G, Boomsma DI. Life events and borderline personality features: the influence of gene–environment interaction and gene–environment correlation. Psychological medicine 2011; 41(4): 849–860. [DOI] [PubMed] [Google Scholar]
- 6.Kendler KS. Twin studies of psychiatric illness: an update. Archives of general psychiatry 2001; 58(11): 1005–1014. [DOI] [PubMed] [Google Scholar]
- 7.Ensink JB, de Moor MH, Zafarmand MH, de Laat S, Uitterlinden A, Vrijkotte TG et al. Maternal environmental risk factors and the development of internalizing and externalizing problems in childhood: The complex role of genetic factors. American Journal of Medical Genetics Part B: Neuropsychiatric Genetics 2020; 183(1): 17–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Krapohl E, Hannigan L, Pingault J-B, Patel H, Kadeva N, Curtis C et al. Widespread covariation of early environmental exposures and trait-associated polygenic variation. Proceedings of the National Academy of Sciences 2017; 114(44): 11727–11732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Smoller JW, Andreassen OA, Edenberg HJ, Faraone SV, Glatt SJ, Kendler KS. Psychiatric genetics and the structure of psychopathology. Molecular psychiatry 2019; 24(3): 409–420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Walsh C, MacMillan H, Jamieson E. The relationship between parental psychiatric disorder and child physical and sexual abuse: findings from the Ontario Health Supplement. Child Abuse Negl 2002; 26(1): 11–22. [DOI] [PubMed] [Google Scholar]
- 11.De Bellis MD, Broussard ER, Herring DJ, Wexler S, Moritz G, Benitez JG. Psychiatric co-morbidity in caregivers and children involved in maltreatment: a pilot research study with policy implications. Child Abuse & Neglect 2001; 25(7): 923–944. [DOI] [PubMed] [Google Scholar]
- 12.Egami Y, Ford DE, Greenfield SF, Crum RM. Psychiatric profile and sociodemographic characteristics of adults who report physically abusing or neglecting children. American Journal of Psychiatry 1996; 153(7): 921–928. [DOI] [PubMed] [Google Scholar]
- 13.Dinwiddie SH, Bucholz KK. Psychiatric diagnoses of self-reported child abusers. Child Abuse & Neglect 1993; 17(4): 465–476. [DOI] [PubMed] [Google Scholar]
- 14.Sidebotham P, Heron J. Child maltreatment in the “Children of the Nineties”: A cohort study of risk factors. Child Abuse & Neglect 2006; 30(5): 497–522. [DOI] [PubMed] [Google Scholar]
- 15.Medley A, Sachs-Ericsson N. Predictors of parental physical abuse: The contribution of internalizing and externalizing disorders and childhood experiences of abuse. Journal of affective disorders 2009; 113(3): 244–254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kim-Cohen J, Caspi A, Rutter M, Tomás MP, Moffitt TE. The Caregiving Environments Provided to Children by Depressed Mothers With or Without an Antisocial History. American Journal of Psychiatry 2006; 163(6): 1009–1018. [DOI] [PubMed] [Google Scholar]
- 17.Dubowitz H, Kim J, Black MM, Weisbart C, Semiatin J, Magder LS. Identifying children at high risk for a child maltreatment report. Child Abuse & Neglect 2011; 35(2): 96–104. [DOI] [PubMed] [Google Scholar]
- 18.Dalvie S, Maihofer AX, Coleman JR, Bradley B, Breen G, Brick LA et al. Genomic influences on self-reported childhood maltreatment. Translational psychiatry 2020; 10(1): 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Roberts AL, Koenen KC, Lyall K, Robinson EB, Weisskopf MG. Association of autistic traits in adulthood with childhood abuse, interpersonal victimization, and posttraumatic stress. Child Abuse Negl 2015; 45(July): 135–142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mash EJ, Johnston C. Parental perceptions of child behavior problems, parenting self-esteem, and mothers’ reported stress in younger and older hyperactive and normal children. Journal of consulting and clinical psychology 1983; 51(1): 86. [DOI] [PubMed] [Google Scholar]
- 21.Podolski C-L, Nigg JT. Parent stress and coping in relation to child ADHD severity and associated child disruptive behavior problems. Journal of clinical child psychology 2001; 30(4): 503–513. [DOI] [PubMed] [Google Scholar]
- 22.Barkley RA. The effects of methylphenidate on the interactions of preschool ADHD children with their mothers. Journal of the American Academy of Child & Adolescent Psychiatry 1988; 27(3): 336–341. [DOI] [PubMed] [Google Scholar]
- 23.McLaughlin DP, Harrison CA. Parenting practices of mothers of children with ADHD: The role of maternal and child factors. Child and Adolescent Mental Health 2006; 11(2): 82–88. [DOI] [PubMed] [Google Scholar]
- 24.Gau SSF, Chou MC, Lee JC, Wong CC, Chou WJ, Chen MF et al. Behavioral problems and parenting style among Taiwanese children with autism and their siblings. Psychiatry and clinical neurosciences 2010; 64(1): 70–78. [DOI] [PubMed] [Google Scholar]
- 25.Chang L-R, Chiu Y-N, Wu Y-Y, Gau SS-F. Father’s parenting and father–child relationship among children and adolescents with attention-deficit/hyperactivity disorder. Comprehensive Psychiatry 2013; 54(2): 128–140. [DOI] [PubMed] [Google Scholar]
- 26.Roberts AL, Lyall K, Weisskopf MG. Maternal exposure to childhood abuse, mate selection, and autism spectrum disorder in offspring. Journal of Autism & Developmental Disorders 2017; 47(7): 1998–2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dube SR, Anda RF, Whitfield CL, Brown DW, Felitti VJ, Dong M et al. Long-term consequences of childhood sexual abuse by gender of victim. American journal of preventive medicine 2005; 28(5): 430–438. [DOI] [PubMed] [Google Scholar]
- 28.Madigan S, Cyr C, Eirich R, Fearon RP, Ly A, Rash C et al. Testing the cycle of maltreatment hypothesis: Meta-analytic evidence of the intergenerational transmission of child maltreatment. Development and psychopathology 2019; 31(1): 23–51. [DOI] [PubMed] [Google Scholar]
- 29.Danese A Annual Research Review: Rethinking childhood trauma-new research directions for measurement, study design and analytical strategies. Journal of child psychology and psychiatry 2019. [DOI] [PubMed] [Google Scholar]
- 30.Demontis D, Walters RK, Martin J, Mattheisen M, Als TD, Agerbo E et al. Discovery of the first genome-wide significant risk loci for attention deficit/hyperactivity disorder. Nature genetics 2019; 51(1): 63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Grove J, Ripke S, Als TD, Mattheisen M, Walters RK, Won H et al. Identification of common genetic risk variants for autism spectrum disorder. Nature genetics 2019; 51(3): 431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Stahl EA, Breen G, Forstner AJ, McQuillin A, Ripke S, Trubetskoy V et al. Genome-wide association study identifies 30 loci associated with bipolar disorder. Nature genetics 2019; 51(5): 793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wray NR, Ripke S, Mattheisen M, Trzaskowski M, Byrne EM, Abdellaoui A et al. Genome-wide association analyses identify 44 risk variants and refine the genetic architecture of major depression. Nature genetics 2018; 50(5): 668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Luciano M, Hagenaars SP, Davies G, Hill WD, Clarke T-K, Shirali M et al. Association analysis in over 329,000 individuals identifies 116 independent variants influencing neuroticism. Nature genetics 2018; 50(1): 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ripke S, Neale BM, Corvin A, Walters JT, Farh K-H, Holmans PA et al. Biological insights from 108 schizophrenia-associated genetic loci. Nature 2014; 511(7510): 421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tworoger SS, Sluss P, Hankinson SE. Association between plasma prolactin concentrations and risk of breast cancer among predominately premenopausal women. Cancer Research 2006; 66(4): 2476–2482. [DOI] [PubMed] [Google Scholar]
- 37.Consortium GP. A global reference for human genetic variation. Nature 2015; 526(7571): 68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Duncan L, Shen H, Gelaye B, Meijsen J, Ressler K, Feldman M et al. Analysis of polygenic risk score usage and performance in diverse human populations. Nature communications 2019; 10(1): 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Psychiatric GWAS Consortium Bipolar Disorder Working Group. Large-scale genome-wide association analysis of bipolar disorder identifies a new susceptibility locus near ODZ4. Nature genetics 2011; 43(10): 977–983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Power RA, Tansey KE, Buttenschon HN, Cohen-Woods S, Bigdeli T, Hall LS et al. Genome-wide Association for Major Depression Through Age at Onset Stratification: Major Depressive Disorder Working Group of the Psychiatric Genomics Consortium. Biol Psychiatry 2017; 81(4): 325–335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Consortium IS. Common polygenic variation contributes to risk of schizophrenia and bipolar disorder. Nature 2009; 460(7256): 748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Choi SW, O’Reilly PF. PRSice-2: Polygenic Risk Score software for biobank-scale data. GigaScience 2019; 8(7): giz082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bernstein DP, Fink L, Handelsman L, Foote J, Lovejoy M, Wenzel K et al. Initial reliability and validity of a new retrospective measure of child abuse and neglect. The American journal of psychiatry 1994. [DOI] [PubMed] [Google Scholar]
- 44.Bernstein DP, Fink L, Handelsman L, Foote J, Lovejoy M, Wenzel K et al. Initial reliability and validity of a new retrospective measure of child abuse and neglect. American Journal of Psychiatry 1994; 151(8): 1132–1136. [DOI] [PubMed] [Google Scholar]
- 45.Straus MA, Hamby SL, Boney-McCoy S, Sugarman DB. The revised conflict tactics scales (CTS2) development and preliminary psychometric data. Journal of family issues 1996; 17(3): 283–316. [Google Scholar]
- 46.Straus MA, Hamby SL, Finkelhor D, Moore DW, Runyan D. Identification of child maltreatment with the Parent-Child Conflict Tactics Scales: development and psychometric data for a national sample of American parents. Child Abuse & Neglect 1998; 22(4): 249–270. [DOI] [PubMed] [Google Scholar]
- 47.Thorsen SV, Rugulies R, Hjarsbech PU, Bjorner JB. The predictive value of mental health for long-term sickness absence: the Major Depression Inventory (MDI) and the Mental Health Inventory (MHI-5) compared. BMC medical research methodology 2013; 13(1): 115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ware JE. Scoring the SF-36. SF-36 Health Survey: Manual and Interpretation Guide 1993. [Google Scholar]
- 49.Price AL, Patterson NJ, Plenge RM, Weinblatt ME, Shadick NA, Reich D. Principal components analysis corrects for stratification in genome-wide association studies. Nature genetics 2006; 38(8): 904–909. [DOI] [PubMed] [Google Scholar]
- 50.Brant R Assessing proportionality in the proportional odds model for ordinal logistic regression. Biometrics 1990: 1171–1178. [PubMed] [Google Scholar]
- 51.Harrell FE Jr. Regression modeling strategies: with applications to linear models, logistic and ordinal regression, and survival analysis. Springer; 2015. [Google Scholar]
- 52.Widom CS, Morris S. Accuracy of adult recollections of childhood victimization, part 2: childhood sexual abuse. Psychological assessment 1997; 9(1): 34. [Google Scholar]
- 53.Berg JJ, Harpak A, Sinnott-Armstrong N, Joergensen AM, Mostafavi H, Field Y et al. Reduced signal for polygenic adaptation of height in UK Biobank. ELife 2019; 8: e39725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Sohail M, Maier RM, Ganna A, Bloemendal A, Martin AR, Turchin MC et al. Polygenic adaptation on height is overestimated due to uncorrected stratification in genome-wide association studies. ELife 2019; 8: e39702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Stith SM, Rosen KH, Middleton KA, Busch AL, Lundeberg K, Carlton RP. The intergenerational transmission of spouse abuse: A meta-analysis. Journal of Marriage and Family 2000; 62(3): 640–654. [Google Scholar]
- 56.Pariante CM, Lightman SL. The HPA axis in major depression: classical theories and new developments. Trends in neurosciences 2008; 31(9): 464–468. [DOI] [PubMed] [Google Scholar]
- 57.Shields AM, Cicchetti D, Ryan RM. The development of emotional and behavioral self-regulation and social competence among maltreated school-age children. Development and psychopathology 1994; 6(1): 57–75. [DOI] [PubMed] [Google Scholar]
- 58.Roberts AL, Chen Y, Slopen N, McLaughlin KA, Koenen KC, Austin SB. Maternal Experience of Abuse in Childhood and Depressive Symptoms in Adolescent and Adult Offspring: A 21-Year Longitudinal Study. Depress Anxiety 2015; 32(10): 709–719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Mahedy L, Heron J, Stapinski LA, Pearson RM, Evans J, Joinson C et al. MOTHERS’OWN RECOLLECTIONS OF BEING PARENTED AND RISK OF OFFSPRING DEPRESSION 18 YEARS LATER: A PROSPECTIVE COHORT STUDY. Depression and anxiety 2014; 31(1): 38–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Choi KW, Houts R, Arseneault L, Pariante C, Sikkema KJ, Moffitt TE. Maternal depression in the intergenerational transmission of childhood maltreatment and its sequelae: Testing postpartum effects in a longitudinal birth cohort. Development and psychopathology 2019; 31(1): 143–156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Jovanovic T, Smith A, Kamkwalala A, Poole J, Samples T, Norrholm SD et al. Physiological markers of anxiety are increased in children of abused mothers. Journal of Child Psychology and Psychiatry 2011; 52(8): 844–852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Roberts AL, Liew Z, Lyall K, Ascherio A, Weisskopf MG. Association of Maternal Exposure to Childhood Abuse With Elevated Risk for Attention Deficit Hyperactivity Disorder in Offspring. Am J Epidemiol 2018; 187(9): 1896–1906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Roberts AL, Lyall K, Rich-Edwards JW, Ascherio A, Weisskopf MG. Association of maternal exposure to childhood abuse with elevated risk for autism in offspring. JAMA Psychiatry 2013; 70(5): 508–515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Cougle JR, Timpano KR, Sachs-Ericsson N, Keough ME, Riccardi CJ. Examining the unique relationships between anxiety disorders and childhood physical and sexual abuse in the National Comorbidity Survey-Replication. Psychiatry research 2010; 177(1-2): 150–155. [DOI] [PubMed] [Google Scholar]
- 65.Green JG, McLaughlin KA, Berglund PA, Gruber MJ, Sampson NA, Zaslavsky AM et al. Childhood adversities and adult psychiatric disorders in the national comorbidity survey replication I: associations with first onset of DSM-IV disorders. Archives of general psychiatry 2010; 67(2): 113–123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.McLaughlin KA, Green JG, Gruber MJ, Sampson NA, Zaslavsky AM, Kessler RC. Childhood adversities and adult psychiatric disorders in the national comorbidity survey replication II: associations with persistence of DSM-IV disorders. Archives of general psychiatry 2010; 67(2): 124–132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Myhre MC, Dyb GA, Wentzel-Larsen T, Grøgaard JB, Thoresen S. Maternal childhood abuse predicts externalizing behaviour in toddlers: a prospective cohort study. Scandinavian journal of public health 2014; 42(3): 263–269. [DOI] [PubMed] [Google Scholar]
- 68.Roberts R, O’Connor T, Dunn J, Golding J, Team AS. The effects of child sexual abuse in later family life; mental health, parenting and adjustment of offspring. Child abuse & neglect 2004; 28(5): 525–545. [DOI] [PubMed] [Google Scholar]
- 69.Pluess M, Bolten M, Pirke K-M, Hellhammer D. Maternal trait anxiety, emotional distress, and salivary cortisol in pregnancy. Biological Psychology 2010; 83(3): 169–175. [DOI] [PubMed] [Google Scholar]
- 70.Rice F, Harold GT, Boivin J, Hay DF, van den Bree M, Thapar A. Disentangling prenatal and inherited influences in humans with an experimental design. Proceedings of the National Academy of Sciences 2009; 106(7): 2464–2467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Chatterjee N, Shi J, García-Closas M. Developing and evaluating polygenic risk prediction models for stratified disease prevention. Nature Reviews Genetics 2016; 17(7): 392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Gilman SE, Gardener H, Buka SL. Maternal smoking during pregnancy and children’s cognitive and physical development: a causal risk factor? American Journal of Epidemiology 2008; 168(5): 522–531. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


