Abstract
Importance
Perioperative anemia is a common comorbid condition associated with increased risk of morbidity and mortality in patients undergoing elective surgical procedures.
Objective
We conducted a systematic literature review (SLR) to determine the efficacy and safety of the use of intravenous ferric carboxymaltose (FCM) for the treatment of perioperative anemia in preoperative, intraoperative, and postoperative elective surgical care.
Evidence Review
Studies meeting inclusion criteria for the SLR reported on treatment efficacy in an adult study population randomly allocated to FCM for the treatment of perioperative anemia during the perioperative period. After screening, 10 of 181 identified studies from searches in MEDLINE and EMBASE databases were identified for inclusion in this review.
Findings
Preoperative treatment was reported in six studies, intraoperative treatment in one study, postoperative treatment in two studies, and both pre- and postoperative treatment in one study. Together, 1975 patients were studied, of whom 943 were randomized to FCM, of whom 914 received FCM treatment. The 10 studies reported elective surgical populations for colorectal, gastric, orthopedic, abdominal, urologic, plastic, neck, gynecologic, and otolaryngologic procedures. Given the clinical and methodological heterogeneity of the studies, the analyses were limited to qualitative assessments without meta-analyses. All 10 studies reported statistically greater changes in hemoglobin concentration, serum ferritin, and/or transferrin saturation with FCM treatment compared with comparators (placebo, oral iron, standard care, or a combination of these). Two studies reported statistically significant differences in transfusion rate and 2 studies reported significant differences in length of hospital stay between FCM and its comparator(s).
Conclusions and Relevance
This SLR adds to existing data that administration of FCM in preoperative and postoperative settings improves hematologic parameters. Several studies in the review supported the beneficial effects of FCM in reducing transfusion rate and length of stay. Larger, well-designed, longer-term studies may be needed to further establish the efficacy and safety of FCM in elective surgery patients with perioperative anemia.
Keywords: intravenous iron, hemoglobin, elective surgery, patient blood management, iron-deficiency anemia
Plain Language Summary
Preoperative and postoperative anemia occur frequently in patients undergoing elective surgery.1
Perioperative anemia is associated with an increased risk of morbidity, mortality, and other adverse postoperative outcomes.1–4
Iron deficiency is a common cause of anemia in surgical patients, affecting at least 10% of surgical patients during the preoperative period and at least 20% during the postoperative period.5,6
Blood transfusion is frequently administered as part of the standard of care for perioperative anemia7 and may produce a temporary increase in hemoglobin levels8 but is associated with poor outcomes.9
This systematic review evaluated the effectiveness and safety of ferric carboxymaltose in patients with perioperative anemia, with a focus on patients’ health states during the preoperative and postoperative period.
The 10 identified studies included patient populations undergoing elective colorectal, gastric, orthopedic, abdominal, urologic, plastic, neck, gynecologic, and otolaryngologic procedures.
Comparators were placebo, oral iron, standard care, or a combination of these interventions.
Overall, this review found that ferric carboxymaltose significantly increased hemoglobin level, serum ferritin concentrations, and transferrin saturation in patients with perioperative anemia who were undergoing elective surgery.
Introduction
Perioperative anemia is a common comorbid condition associated with increased risk of morbidity and mortality in patients undergoing elective surgical procedures. The most common etiology of perioperative anemia in adults is iron deficiency. Clinical signs and symptoms of iron-deficiency anemia (IDA) are protean and vary widely, and perioperative health outcomes associated with IDA include reduced physical function, prolonged postoperative recovery, increased length of hospital stay, and mortality.1–4,10 Among orthopedic patients, the preoperative prevalence of anemia is estimated at 24% to 44%, and postoperative estimates are significantly higher.1 Among patients with advanced colon cancer undergoing colectomy, the estimated prevalence of anemia is reported to be as high as 75.8%.11
In preoperative evaluation for IDA, diagnostic assessment and pre-surgical treatment varies. One recognized intervention is blood transfusion, with an estimated 6.6 million red blood cell (RBC) units administered annually to elective surgery patients in the United States.4 To assess the use of an intravenous iron in anemic perioperative patient populations, a systematic literature review (SLR) was conducted and focused on the safety and efficacy of ferric carboxymaltose.
Methods
Study Design
The study protocol was designed and executed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA).12 All review methods were conducted a priori according to the established protocol. Publication screening, selection, and assessments of bias were carried out by the authors, with consensus for reconciliation. Included studies were conducted in adults (≥18 years of age) with anemia (if not IDA) who had been identified for elective surgery and randomly allocated to receive intravenous (IV) FCM or comparator(s). Inclusion also required study publication in peer-reviewed journals. Studies were excluded if the design was nonexperimental, if efficacy was not reported, or if the investigative treatment consisted of only IV FCM in combination with either erythropoietin or an erythropoiesis-stimulating agent; animal and pediatric studies were also excluded. Conference abstracts and grey literature were excluded.
Literature Search
Comprehensive, computer-based literature searches for records were performed systematically using the MEDLINE (PubMed, US National Library of Medicine, National Institutes of Health) and EMBASE databases. The electronic search strategy was peer reviewed and developed with guidance from a university librarian at St. John’s University College of Pharmacy and Health Sciences. Databases were searched from their inception to January 2021 for abbreviations and full-phrase versions of keywords and Medical Subject Headings combined with Boolean operators as outlined in the Supplementary Data, Appendix 1. Two reviewers independently and in duplicate assessed titles and abstracts of identified records for trial eligibility, and a third reviewer resolved any discrepancies by discussion or adjudication until consensus was reached. Relevant records were further assessed by examining the full-text articles. A snowball method (using a key manuscript as a starting point and consulting the bibliography to find other relevant titles on the subject) was used to search the identified literature to additional studies. Data were extracted onto a standardized extraction form.
Risk of Bias and Quality Assessment
Internal validity and risk of bias for each study meeting final inclusion criteria were assessed in duplicate by 2 independent reviewers using the Cochrane Risk of Bias Tool.13 The key types of bias that were examined were selection, performance, detection, attrition, and reporting. The overall quality of evidence was assessed using the Grading of Recommendations Assessment, Development, and Evaluation (GRADE)14 approach to determine the strength of the conclusions/recommendations from this review.
Outcome Measures
The primary outcomes were the absolute or relative change from baseline in hemoglobin (Hb) concentration (g/dL), serum ferritin (ng/mL), and% transferrin saturation (TSAT). Primary outcomes that were reported in alternative units were converted for consistency across studies for ease of interpretability; conversions were quality controlled for accuracy. Secondary outcome measures were the proportion of patients who received a perioperative blood transfusion, the occurrence of adverse events, treatment-related adverse events, postoperative mortality, length of hospital stay, and any validated measure of quality of life (QOL).
Results
Study Selection
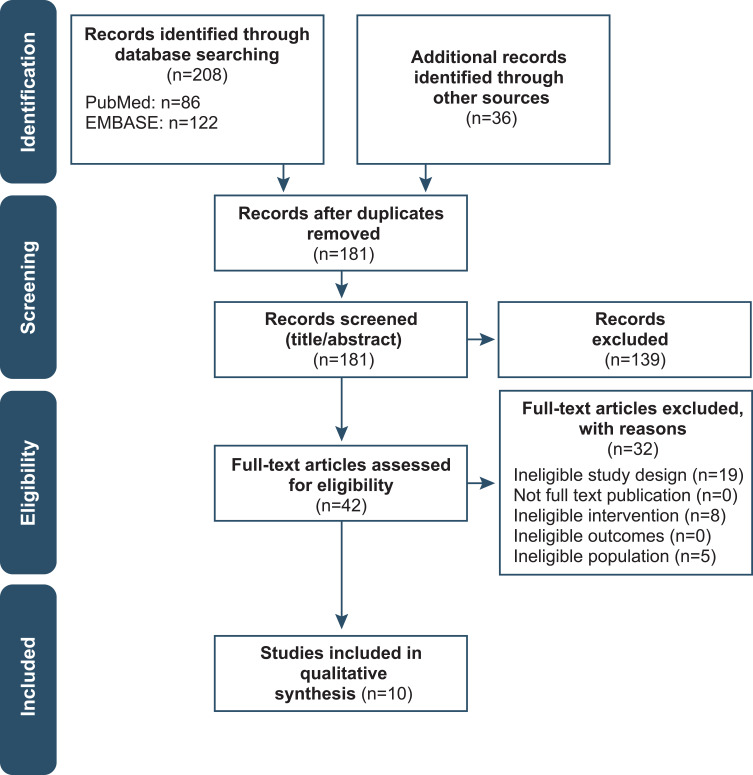
We identified 244 citations, 208 through database searching and 36 through other sources. The number was decreased to 181 after removing duplicates (Figure 1). The 181 citations were screened based on title and abstract, and 139 were excluded. After screening the full-text articles of the remaining 42 citations, 32 were excluded. Ultimately, 10 eligible studies were included in this systematic review.
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses flowchart of the study selection process.
Note: Adapted from Page MJ, Moher D, Bossuyt PM, et al. PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. BMJ. 2021;372:n160.37
Study Characteristics
All 10 studies included in the systematic review were randomized clinical trials and were published between 2014 and 2020.7,15–23 Five studies were conducted in Europe (United Kingdom,15,21,23 Spain15,16), 2 studies in Oceania (Australia7,17), and 3 studies in Asia (South Korea19,20,22).
The design and patient flow of the included studies are summarized in Table 1. Studies investigated the use of FCM in the following surgical populations: cancer (colorectal,18 gastric19), cardiac,21 menorrhagia,20 orthopedic (hip arthroplasty,16,22 total knee arthroplasty15,22), abdominal,17,23 and a combination of orthopedic, abdominal, neck, gynecologic, urologic, plastic, and ear, nose, and throat (ENT).7 Ferric carboxymaltose was administered preoperatively in 5 studies,16,18,20,21,23 intraoperatively in 1 study,22 postoperatively in 3 studies,7,15,19 and perioperatively (both preoperatively and postoperatively) in 1 study.17 With respect to blinding, 2 studies used a double-blind design,16,23 3 were single-blind,15,19,22 and 5 were open-label.7,17,18,20,21 Follow-up periods for patients varied, spanning from 2 weeks post-infusion,20 4 weeks postoperatively15,17,22 to 2 to 6 months after hospital discharge.7,15,16,19,21,23
Table 1.
Design and Patient Flow of Included Studies
| Study Description | |||||||
|---|---|---|---|---|---|---|---|
| Study | Perioperative State (Surgery) | Study Group Assignment | Design | Prespecified Blood Transfusion Criteria | Randomized N |
Treated N |
Withdrawn N |
| Bisbe et al (2014)15 | Postoperative (orthopedic) |
G1: IV FCM 700–1000 mg single dose on postop day 1 G2: Oral ferrous sulfate 100 mg/d from postop day 7 to 30 |
Single-blinded | 3. Hb <70 g/L=3 RBC transfusions independent of symptoms 4. Hb 71–89 g/L=2 RBC transfusions in presence of severe symptoms (HF with NYHA Class ≥III dyspnea, ACS, hemodynamic instability [hypotension, orthostatism], and/or acute or exacerbated chronic respiratory failure) |
122 G1: 60 G2: 62 |
121 G1: 59 G2: 62 |
G1: 7 (LTFU) G2: 11 (LTFU) |
| Bernabeu-Wittel et al (2016)16 | Preoperative (orthopedic hip) |
G1: EPO 40,000 IU/1 mL EPO SC + IV FCM 1000 mg (2500 mg vials diluted in 250 mL of saline) infused over 20 min G2: 1 mL placebo (saline) SC + IV FCM 1000 mg (2500 mg vials diluted in 250 mL of saline) infused over 20 min G3: 1 mL placebo (saline) SC + IV placebo (250 mL of saline) infused over 20 min |
Double-blind | 1. Hb <70 g/L=3 RBC transfusions independent of symptoms 2. Hb 71–89 g/L=2 RBC transfusions in presence of severe symptoms (HF with NYHA Class ≥III dyspnea, ACS, hemodynamic instability [hypotension, orthostatism], and/or acute or exacerbated chronic respiratory failure) |
303 G1: 100 G2: 103 G3: 100 |
293 G1: 97 (hip surgery— osteosynthesis, n=66 [68%]; partial arthroplasty, n=27 [28%]; total arthroplasty, n=4 [4%]) G2: 101 (hip surgery—osteosynthesis, n=70 [69%]; partial arthroplasty, n=28 [28%]; total arthroplasty, n=3 [3%]) G3: 97 (hip surgery— osteosynthesis, n=60 [62%]; partial arthroplasty, n=33 [34%]; total arthroplasty, n=4 [4%]) |
G1: 14 (discontinued intervention, n=6 [not operated, n=3, iron sucrose administration in follow-up period, n=3]); excluded from per protocol analysis,a n=8) G2: 17 (discontinued intervention, n=6 [not operated, n=2; iron sucrose administration in follow-up period, n=4]); excluded from per protocol analysis,a n=11) G3: 11 (discontinued intervention, n=4 [not operated, n=3, iron sucrose administration in follow-up period, n=1]); excluded from per protocol analysis, n=7)a |
| Froessler et al (2016)17 | Perioperative (abdominal) |
G1: Preop―IV FCM single 15 mg/kg injection (maximum: 1000 mg) administered over 15 min Postop―IV FCM 0.5 mg per recorded 1 mL blood loss if blood loss ≥100 mL, given within 2 days of surgery G2: Usual care consisting of no treatment, observation, oral iron recommendations, and ABT; prescription and administration of IV iron allowed |
Open (masking not used) | Not reported | 72 G1: 40 G2: 32 |
72 G1: 40 G2: 32 |
Not reported |
| Khalafallah et al (2016)7 | Postoperative (orthopedic, abdominal, ENT, plastic, gynecologic, urologic) |
G1: IV FCM single 15 mg/kg injection (maximum: 1000 mg) over 15 min G2: No intervention (standard care) |
Open-label | Not reported | 201 G1: 103 G2: 98 |
201 G1: 97 G2: 94 |
G1: 6 (withdrawn from study, n=5; LTFU, n=1) G2: 4 (withdrawn from study, n=2; LTFU, n=2) |
| Keeler et al (2017)18 | Preoperative (oncological) |
G1: IV FCM diluted in 250 mL 0.9% NS over 15 min; dose calculated using body weight and inclusion hemoglobin value. Maximum dose 1000 mg/wk and 2000 mg during trial; second dose ≥7 days after first, if needed G2: Oral ferrous sulphate 200 mg BID continued until surgery (patients advised to take without food and with liquid high in ascorbic acid to maximize enteric absorption) |
Open-label | Not reported | 116 G1: 55 G2: 61 |
116 G1: 55 G2: 61 |
G1: 4 (did not undergo surgical resection) G2: 2 (did not undergo surgical resection) |
| Kim et al (2017)19 | Preoperative (oncological) |
G1: IV FCM 1–2 1000 mg injections for patients <50 kg or 500 mg injections for ≥50 kg over 6–15 min G2: IV saline placebo |
Single-blinded | Per guidelines, Hb <7 g/dL | 454 G1: 228 G2: 226 |
445 G1: 222 G2: 223 |
G1: 5 (did not complete study [LTFU, n=3; withdrew consent after treatment, n=1; physician withdrew patient for surgical complication, n=1]) G2: 10 (did not complete study [withdrew consent after treatment, n=6; LTFU, n=2; eligibility criteria violation recognized after treatment/received blood transfusion before treatment, n=2]) |
| Lee et al (2019)20 | Preoperative (benign uterine diseases) |
G1: IV FCM single dose administered over 15 min (maximum: 1000 mg); amount determined based on patient’s body weight (<50 kg, 500 mg iron; ≥50 kg, 1000 mg iron). G2: IV IS single administration over 3 dosing visits per week (maximum: 600 mg iron/week in 200 mg iron doses. Dosage based on calculated iron deficit using the Ganzoni formula |
Open-label | Not reported | 101 G1: 52 G2: 49 |
101 G1: 52 G2: 49 |
G1: 0 G2: 0 |
| Padmanabhan et al (2019)21 | Preoperative (cardiac) |
G1: IV FCM diluted in 250 mL of NS administered over 30 min (maximum: 1000 mg dose). A second dose was offered when required. Calculation of dosing regimen as follows: Hb > 100 and weight < 70 kg = 1000 mg; Hb > 100 and weight > 70 kg = 1500 mg; Hb 70–100 and weight < 70 kg = 1500 mg; Hb 70–100 and weight > 70 kg = 2000 mg G2: 200 mg ferrous sulphate PO BID |
Open-label | Not reported | 50 G1: 26 G2: 24 |
44 G1: 22 G2: 22 |
G1: 4 (LTFU) G2: 1 (LTFU) |
| Park et al (2019)22 | Intraoperative (Unilateral TKA or THA) |
G1: IV FCM 1000 mg diluted in 100 mL NS administered over 15 min. G2: IV 100 mL NS placebo |
Single-blinded | Hb < 8 g/dL throughout entire perioperative period. If significant hemodynamic instability was observed despite adequate fluid administration or a requirement of an increasing amount of vasopressor was essential, allogenic transfusion of packed RBC was permitted with the Hb ≥ 8 g/dL. In case of transfusion, the subjects received one unit of packed RBC and the Hb level was followed to assess the further administration of additional packed RBC. | 69 G1: 32 G2: 34 |
58 G1: 29 G2: 29 |
G1: 3 (withdrew consent, n=1, LTFU, n=2) G2: 5 (unnoticed cancer diagnosis, n=1; withdrew consent, n=1; LTFU, n=3) |
| Richards et al (2020)23 | Preoperative (abdominal) |
G1: IV FCM single dose 1000 mg in 100 mL NS administered over 15 min G2: IV 100 mL NS placebo |
Double-blinded | Not reported | 487 G1: 244 G2: 243 |
481 G1: 240 G2: 241 |
G1: 8 (not treated, n=4; withdrew consent, n=4) G2: 6 (not treated, n=2; withdrew consent, n=4) |
Note: aPatients did not receive intervention, were not operated, or received iron sucrose administration in the follow-up period.
Abbreviations: ABT, allogeneic blood transfusion; ACS, acute coronary syndrome; BID, twice daily; EPO, erythropoietin; FCM, ferric carboxymaltose; G, treatment group; Hb, hemoglobin; HF, heart failure; IV, intravenous; IS, iron sucrose; LTFU, lost to follow-up; NS, normal saline; NYHA, New York Heart Association; PO, by mouth; RBC, red blood cell; SC, subcutaneous; TDD, total daily dose; TID, three times daily; THA, total hip arthroplasty; TKA, total knee arthroplasty.
In total, 1975 study patients were randomized across the 10 studies, 943 (48%) of whom were randomized to receive IV FCM, and of these, 914 (97%) received their assigned treatment. Three studies compared IV FCM with oral ferrous sulfate (dose: 100 mg per day15 to 200 mg twice daily15,21), 1 study compared IV FCM with IV iron sucrose (dose: 200 mg iron x 3/week),20 and 2 studies compared IV FCM with standard of care (no intervention7 or no treatment, continued observations, oral iron recommendations, and allogeneic blood transfusion [ABT]).17 The comparator for 3 of the remaining 4 studies was IV saline placebo,19,22,23 and the comparators for the other remaining study (triple-arm, parallel design) were 1 mL subcutaneous (SC) saline placebo with 250 mL of IV saline placebo and 40,000 IU/1 mL SC erythropoietin (EPO) with 1000 mg IV FCM diluted in 250 mL saline.16 The dosages of IV FCM across studies varied in terms of total dose and dosage calculation as well as administration time, which spanned 6 to 30 minutes. In 3 studies, IV FCM was given in a single dose of 1000 mg;7,22,23 in the 7 others, the dose was determined by the Ganzoni formula to correct the total iron deficit,15 manufacturer recommendation (15 mg/kg),7,17 weight cutoffs (<50 or ≥50 kg),19,20 weight cutoffs in combination with inclusion Hb values,18,21 or blood loss (5 x 10−7 mcg/L) if blood loss was ≥100 mL.17 For 8 of the 10 studies, the maximum single dose of IV FCM was 1000 mg;7,15–17,19,22,23 Keeler et al and Padmanabhan et al allowed a maximum total dose of up to 2000 mg (2 doses of 1000 mg administered 7 days apart and when required).15,21
The hematologic inclusion criteria varied among the studies, with 5 requiring IDA with Hb limits (9–12 g/dL,16 <11 g/dL [women] or <12 g/dL [men],18 <12 g/dL [women] or <13 g/dL [men]21,23 and ≥7–<10 g/dL19); 4 requiring IDA with specific hematologic profiles (serum ferritin <300 μg/L, transferrin saturation <25%, and Hb <12 g/dL [women] or <13 g/dL [men];17 Hb 7–12 g/dL with serum ferritin ≤100 µg/L or TSAT ≤20%;7 serum ferritin <300 μg/L and Hb <10 g/dL);20,22 and 1 requiring anemia and/or IDA with a specific hematologic profile (Hb 8.5–12 g/dL, TSAT <20%, or both15).
Institution-specific medical care standards specifically relating to perioperative blood management (PBM) were explicitly stated in 3 of the 10 studies.15–17 The first study used thromboprophylaxis with low-molecular-weight heparin and prophylaxis with proton pump inhibitors for upper gastrointestinal bleeding.16 The second used a robust PBM protocol including preoperative treatment with iron, SC EPO, or both 1 month before surgery, discretionary tranexamic acid during and after surgery, and antithrombotic treatment with SC bemiparin (a low-molecular-weight heparin not approved in the United States); additionally, shed blood exceeding 400 mL was automatically reinfused via an autotransfusion device.15 In the third study, patients in the usual care group received perioperative anemia management, which did not disallow prescription or administration of IV iron.17 Five of the 10 studies prespecified blood transfusion thresholds; 3 specified Hb <7 g/dL,7,15–17,19 and 1 of these set the number of RBC transfusions at 3.16 Three of the 5 studies specified Hb <8 g/dL15,22 or 7.1–8.9 g/dL in the presence of severe symptoms.16
Study Populations
Baseline characteristics of patients are provided in Table 2. Most of the study populations (9/10) had an average age of 60 years or older, and 9 of the 10 were generally evenly distributed with respect to age across treatment groups. The difference in age distribution between the FCM group and the comparator arm in the sixth study occurred by chance and was not explained by the authors. Eight studies had a greater percentage of women.7,15,16,19–22 Mean weight was lowest among patients undergoing surgery for menorrhagia20 and highest among those undergoing abdominal surgery.17 The American Society of Anesthesiologists (ASA) physical status (grades ranged from I [defined as normal and healthy] to VI [declared brain-dead, organs to be donated]) varied by surgical population in the intervention group; 27–58% of patients undergoing abdominal surgery,17,23 45% undergoing colorectal cancer surgery,18 and 20% undergoing orthopedic surgery had ASA Grade III (presence of severe systemic disease) or greater.15,24 In each of the studies reporting baseline hematopoietic parameters, the patients met criteria for IDA (mean baseline Hb <11 g/dL, serum ferritin <300 ng/mL, and TSAT <25%).
Table 2.
Baseline Patient Characteristics of Included Studies
| Author | Age, y, Mean ± SD | Sex, n (%) | Weight, kg, Mean ± SD | ASA Physical Status Classification, n (%) | Preoperative Hb, g/dL, Mean ± SD | Serum Iron, μg/dL, Mean ± SD | Preoperative Serum Ferritin, ng/mL, Mean ± SD | Preoperative TSAT, %, Mean ± SD |
|---|---|---|---|---|---|---|---|---|
| Bernabeu-Wittel (2016)16 |
G1: 84.6 ± 6.2 G2: 83.4 ± 6.4 G3: 82.3 ± 6.9 |
G1: 84 (81.5%) (F) G2: 87 (87.0%) (F) G3: 87 (87.0%) (F) |
Not reported |
G1: III (II–III)a G2: III (II–III)a G3: III (II–III)a |
G1: 11.0 ± 0.8 G2: 11.0 ± 0.7 G3: 11.0 ± 0.7 |
Not reported |
G1: 155 ± 170 G2: 137 ± 150 G3: 141 ± 130 |
Not reported |
| Keeler (2017)18 |
G1: Median (IQR): 73.8 (67.4–78.6) G2: Median (IQR): 74.7 (67.9–80.8) |
G1: 35:20 (M:F) G2: 37:24 (M:F) |
G1: Mean (95% CI): 79.0 (74.9, 83.2) G2: Mean (95% CI): 72.8 (68.7, 76.9) |
G1: I–II, n=30; III–IV, n=25 G2: I–II, n=43; III–IV, n=18 |
G1: Recruitment: ~10.1; day of surgery: ~11.9 G2: Recruitment: ~10.4; day of surgery: ~11.0 |
Not reported | Not reported | Not reported |
| Kim (2017)19 |
G1: 60.9 ± 13.7 G2: 61.2 ± 12.6 |
G1:125 (54.8%) (F) G2:124 (54.9%) (F) |
G1: 57.6 ± 9.7 G2: 58.1 ± 9.9 |
Not reported |
G1: 11.6 ± 1.6 G2: 11.8 ± 1.6 |
G1: 24.6 ± 15.2 G2: 24.0 ± 11.1 |
G1: 115.9 ± 104.8 G2: 137.1 ± 123.9 |
G1: 10.8 ± 7.2 G2: 10.5 ± 5.4 |
| Froessler (2016)17 |
G1: 64 ± 15 G2: 68 ± 15 |
G1: 19:21 (M:F) G2: 17:15 (M:F) |
G1: 86 ± 27 G2: 88 ± 20 |
G1: II: 17 (42.5); III: 22 (55); IV: 1 (2.5) G2: II: 17 (53.1); III: 15 (46.9); IV: 0 |
G1: Randomization: 10.7 ± 1.3 (n=40); admission: 11.5 ± 1.3 (n=36) G2: Randomization: 10.6 ± 1.4 (n=32; P=0.76); admission: 10.7 ± 1.7 (n=29; P=0.12) Difference between randomization and admission: G1: 0.8 ± 0.8 (n=36) G2: 0.1 ± 1.3 (n=29; P=0.010) |
Not reported |
G1: Randomization, median (IQR): 19 (6–48) G2: Randomization, median (IQR): 37 (11–82) |
G1: Randomization, median (IQR): 6 (3–10) G2: Randomization, median (IQR): 9 (7–15) |
| Bisbe (2014)15 |
G1: Mean (range): 72.7 (56–86) G2: Mean (range): 72.8 (40–86) |
G1: 47 (78.3%) (F) G2: 50 (80.6%) (F) |
G1: 79.6 ± 14.9 G2: 76.2 ± 11.9 |
G1: ≥III: 12 (20.0) G2: ≥III: 12 (19.4) |
G1: 13.6 ± 0.9 G2: 13.6 ± 0.9 |
G1: 77 ± 22 G2: 74 ± 21 |
G1: 120 ± 111 G2: 164 ± 95 |
G1: 20.1 ± 6.6 G2: 20.4 ± 6.7 |
| Khalafallah (2016)7 |
G1: Median (IQR): 65 (55–73) G2: Median (IQR): 67 (60–76) |
G1: 65 (63%) (F) G2: 50 (51%) (F) |
G1: Median (IQR): 82 (70–91) G2: Median (IQR): 81 (69–88) |
Not reported |
G1: Median (IQR), postop day 1: 10.9 (9.9–12.0) G2: Median (IQR), postop day 1: 10.6 (9.6–11.7) |
G1: Preop: 81.6 ± 15.6; postop, day 1: 33.5 ± 21.2; period effect,† mean difference (95% CI): −48.0 (−54.8 to −41.9) [P<0.0001] G2: Preop: 81.0 ± 21.2; postop, day 1: 33.5 ± 25.1; period effect,† mean difference (95% CI): −47.4 (−53.9 to −41.0) [P<0.0001] |
G1: Postop, day 1, median (IQR): 170 (108–284) G2: Postop, day 1, median (IQR): 243 (134–471) |
G1: Postop day 1, median (IQR): 10 (7–15) G2: Postop day 1, median (IQR): 11 (9–15) |
| Lee (2019)20 |
G1: 44.0 ± 5.7 G2: 43.4 ± 5.0 |
G1: 52 (100%) (F) G2: 49 (100%) (F) |
G1: 56.2 ± 6.7 G2: 57.6 ± 9.1 |
Not reported |
G1: 8.4 ± 1.4 G2: 8.4 ± 1.1 |
Not reported |
G1: 58 ± 57 G2: 57 ± 39 |
G1: 6.1 ± 7.3 G2: 4.8 ± 5.9 |
| Padmanabhan (2019)21 |
G1: 73 ± 12 G2: 75 ± 10 |
G1: 9 (41%) (F) G2: 8 (36%) (F) |
G1: 78.9 ± 18.2 G2: 80.5 ± 13.1 |
Not reported |
G1: 11.9 ± 0.89 G2: 113.9 ± 1.11 |
Not reported |
G1: median (IQR) 62.8 (26.2–86.4) G2: median (IQR) 49.7 (19.7–88.8) |
Not reported |
| Parl22 (2019) |
G1: 65.1 ±10.2 G2: 62.0 ± 9.5 |
G1: 19 (65.5%) (F) G2: 21 (72.4%) (F) |
G1: 64.2 ± 9.8 G2: 67.1 ± 11.8 |
G1: ≥III: 0 G2: ≥III: 0 |
G1: 12.5 ± 1.3 G2: 13.4 ± 1.1 |
G1: 92.4 ± 37.0 G2: 101.0 ± 46.5 |
G1: 90.6 ± 82.5 G2: 87.0 ± 105.2 |
G1: 29.4 ± 16.3 G2: 33.2 ± 17.2 |
| Richards (2020)23 |
G1: Mean (range): 66 (57–72) G2: Mean (range): 65 (50–72) |
G1: 125 (51%) (F) G2: 142 (58%) (F) |
Not reported |
G1: ≥III: 57 (23.4) G2: ≥III: 66 (27.2) |
G1: 11.1 ± 1.2 G2: 11.1 ± 1.2 |
Not reported |
All Groups: <100 – 57% |
All Groups: <20 – 76% |
Notes: aN’s were not specified; †Estimated in the standard care group (G2) using repeated measures mixed effects linear regression with time from operation as a random factor, adjusted for sex. Outcomes were compared with preoperative sample concentrations: postoperative samples were taken on the first day after the operation.
Abbreviations: ASA, American Society of Anesthesiologists; CI,confidence interval; G, treatment group (as defined in Table 1 in Intervention Groups and Regimen row); IQR, interquartile range; SD, standard deviation; TSAT, transferrin saturation.
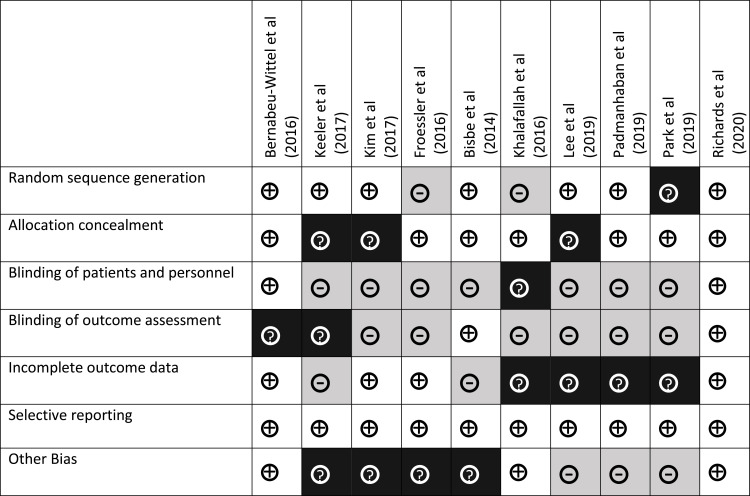
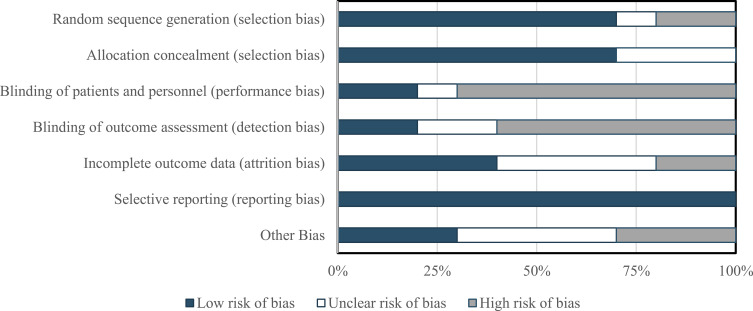
Risk of Bias Assessment
Overall, the studies were considered to have a high risk of bias, largely with regard to the blinding of patients and personnel and blinding of outcome assessments (Figures 2 and 3).
Figure 2.
Risk of bias summary: authors’ judgment about risk of bias for each item for each of the 6 included studies. The symbol “+” indicates low risk of bias, “?” indicates unclear risk of bias, and “–” indicates high risk of bias.
Figure 3.
Risk of bias: authors’ judgment about risk of bias presented as percentages across all 6 included studies.
Random Sequence Generation
Eight out of 10 studies were considered to have a low risk of bias for random sequence generation, as they clearly reported appropriate randomization Che techniques.15,17–21,23,25 However, the random sequence method using Excel in Khalafallah et al7 was questionable and not described in Park et al,22 making the risk of bias unclear.
Allocation Concealment
Eight out of 10 studies were rated as having low risk of bias for allocation concealment.7,15,17,19,22,23,25 The studies by Keeler et al18 and Lee et al20 did not adequately describe the concealment methods of treatment allocation by an independent unit; selection bias was thus deemed unclear in the risk of bias for allocation concealment.
Blinding
Five of the 10 studies had an open-label design,7,17,18,20,21 and 3 were patient-blinded only,15,19,22 leading to a high risk of performance bias; the remaining studies had a double-blind design, which were assigned a low risk of bias.16,23 Three studies had an unclear risk of detection bias; neither Keeler et al18 nor Kim et al19 clearly stated who performed the outcome assessments, and Bernabeu-Wittel et al16 did not describe the study’s blinding measures. Detection bias was low in Bisbe et al15 and Richards et al23 but was high in Froessler et al, Lee, Padmanabhan, and Park owing to a lack of description of outcome blinding measures in these open-label studies17,20–22 and in Khalafallah et al owing to the recording of adverse events (AEs) by personnel who administered the study drug.7
Incomplete Outcome Data
Risk of attrition bias was considered low in 3 studies, in Bernabeu-Wittel et al because losses to follow-up were disclosed and the attrition was reasonable and not expected to affect results,16 in Froessler et al because the rationale was given for study termination17 and Richards et al because attrition was described and accounted for in statistical analysis.23 Risk of attrition bias was deemed unclear for 6 studies because no explanations were offered for withdrawal for either treatment group,7 for the relevance of incomplete data sets available at the end of the study period,15,21,22 for the impact of incomplete adherence―which was assessed in 1 study―to allocated treatment,18 and for interpolation of missing data using linear regression analysis when the total sample size is very small.20 The risk of attrition bias was high for Kim et al, in which a modified intention-to-treat analysis was used.19
Selective Reporting
In Keeler et al, the treatment effects for secondary endpoints of serum ferritin and TSAT were not reported and reported outcomes, including postoperative length of hospital stay and 90-day mortality rates, were not prespecified,18 suggesting a high risk of reporting bias. For the other 9 included studies, all planned outcomes were reported.
Other Potential Sources of Bias
One of the 6 studies had a robust institution-specific patient blood management program in place that may have influenced outcome assessments.15 In 1 study, IV iron was not considered part of usual care at the time of study commencement, but was nonetheless not prohibited.17 A differential number of patients experiencing protocol deviations was noted in the study groups of 1 study.18 Kim et al elected to examine a binary primary outcome measure instead of a continuous outcome measure, which may have skewed response.19 Subjects in the Lee et al study who were assigned to iron sucrose returned to the study site for three dosing visits, whereas those assigned to FCM only had one visit, which may have skewed the results in favor of IS.20 A large portion of patients in the Padmanabhan et al study did not return to receive their second dose of FCM, which may have skewed the results against IV iron.21 Lastly, the Park et al study was significantly underpowered for the primary outcomes selected resulting in potential high risk of bias.22
Outcomes
All studies included reported absolute or relative change from baseline Hb concentrations. Change from baseline Hb concentration ranged from 1.3 g/dL21 to 4.7 g/dL23 among patients receiving preoperative FCM (including in the perioperative study) and 1.7 g/dL15 to 3.2 g/dL7 among those receiving postoperative FCM (Table 3). Six of the 10 studies15,20,21,23 reported this outcome to be statistically significant versus comparators.7,16–19,22 A key outcome measure was change from baseline in iron stores; findings showed that preoperative FCM administration resulted in an increase in serum ferritin concentrations of 229 μg/L (vs 19 μg/L at baseline)17 to 558 μg/L (levels at randomization not reported)18 and a 15%17 to 35%19 increase in TSAT. Postoperative administration resulted in a 1147 to 571 μg/L15 increase in serum ferritin concentration and 7.2%15 to 20%17 increase in TSAT. Both Bernabeu-Wittel et al16 and Lee et al20 did not report change from baseline TSAT.
Table 3.
Primary Outcome Measures: Change from Baseline in Hb, Serum Ferritin, and TSAT
| Study | Surgery | Surgical Setting | Change from Baseline Hb (g/dL) | Change from Baseline Serum Ferritin (μg/L), Mean (SD) | Change from Baseline TSAT (%), Mean (SD) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Group 1 | Group 2 | Group 3 | Group 1 | Group 2 | Group 3 | Group 1 | Group 2 | Group 3 | |||
| Bisbe et al (2014)15 | Orthopedic | Postop | 1.7 (1.2)a | 1.3 (1.0)a | — | 571 (229)a | 60 (88)a | — | 7.2 (−5.2)a | 0.7 (−5)a | — |
| Bernabeu-Wittel et al (2016)16 | Hip fracture | Preop | 1.38 (0.72)b | 1.53 (0.56)b | 0.88 (0.43)b | 317 (140)b | 288 (110)b | −4 (−10)b | — | — | — |
| Froessler et al (2016)17 | Abdominal | Periop | 1.9 (1.4)c | 0.9 (1.4)c | — | 229 (131–498)d | 62 (24–146)d | — | 15 (13–16)d | 5 (0–3)d | — |
| Khalafallah (2016)7 | Orthopedic, abdominal, ENT, plastic, gynecologic, urologic | Postop | 3.2 (0.16)e | 2.81 (0.18)e | — | 114 (73.2)e | −133 (−41.1)e | — | 20 (1.1)e | 13.3 (1.4)e | — |
| Keeler et al (2017)18 | Colorectal cancer | Preop | 1.55 (0.93–2.58)f | 0.50 (−0.13–1.33)f | — | 558 (330–1085)f | 27.5 (17–51.5)f | — | 19 (16–29)f | 9 (5–14)f | — |
| Kim et al (2017)19 | Gastrectomy (cancer) | Preop | 3.3g | 1.6g | — | 233.3h | 53.4h | — | 35.0h | 19.3h | — |
| Lee et al (2019)20 | Benign uterine diseases | Preop | 2.2 (0.3) | 1.9 (0.2) | — | — | — | — | — | — | — |
| Padmanabhan et al (2019)21 | Cardiac | Preop | 1.3 (0.9)i | 4.4 (0.9)i | — | 313 [228, 496]j | 5.5 [−1.4, 19.4]j | — | —k | —k | — |
| Park et al (2019)22 | Unilateral TKA or THA | Intraop | 0.3 (1.00)l | −0.8 (0.78)l | — | 1157.5 (412.3)m | 83.8 (52.5)m | — | 8.7 (10.4)m | −19.5 (−5.2)m | — |
| Richards et al (2020)23 | Open abdominal surgery | Preop | 4.7 (2.7–6.8)n; 10.7 (8–13.8)°; 7.3 (3.6–11.1)p | — | — | — | — | — | — | — | — |
Notes: Treatment groups are defined in Table 1 in Intervention Groups and Regimen row; aValues are increase in mean (SD) from postoperative day 4 to postoperative day 30; bValues are increase in mean (SD) from baseline to 60 days postdischarge (change in SD from baseline to 60 days postdischarge); cValues are increase in mean (SD) from discharge to postoperative week 4; dValues are increase in median (first quartile–third quartile) from randomization to postoperative week 4. eValues are increase in mean (SD) from postoperative day 1 to postoperative week 12; fValues are increase in median (first quartile–third quartile) from baseline to day of surgery; gValues are increase in median from baseline to postoperative week 12; hValues are increase in mean from baseline to postoperative week 12; iValues are increase in mean (SD) between enrolment and surgical admission; jValues are increase in median (interquartile range) between enrolment and surgical admission; kStatistical difference reported in favor of FCM (P=0.001); no data provided; lValues are increase in mean (SD) from baseline to postoperative day 30; mValues are increase in median (interquartile range) from baseline to postoperative day 5; nValues are increase in mean (95% CI) from baseline to time of surgery; oValues are increase in mean (95% CI) from baseline to 8 weeks following intervention; pValues are increase in mean (95% CI) from baseline to 6 months following intervention.
Abbreviations: ENT, ear, nose, and throat; FCM, ferric carboxymaltose; Hb, hemoglobin; THA, total hip arthroplasty; TKA, total knee arthroplasty; TSAT, transferrin saturation.
A secondary efficacy outcome measure was proportion of patients who received perioperative ABT (Table 4). Two7,17 of the 10 studies found statistically significantly lower rates of ABT in patients receiving FCM versus comparators in the perioperative surgical settings (absolute difference: 18.75%)17 and postoperative (absolute difference: 4%).7 The highest proportion of FCM–treated patients who received an ABT was 51.5% (53/103) in Bernabeu-Wittel et al, compared with 52% (52/100) in the FCM plus EPO group and 54% (54/100) in the placebo group;16 in Khalafallah et al, 1% (1/103) of patients receiving FCM versus 5% (5/98) receiving standard of care received an ABT.7
Table 4.
Secondary Outcome Measures: ABT, AEs, and Mortality
| Study | Surgery | Surgical Setting | Proportion of Patients Receiving an ABT, n/N (%) | Proportion of Patients Experiencing AEs, n/N (%) | Postoperative Mortality, n/N (%) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Group 1 | Group 2 | Group 3 | Group 1 | Group 2 | Group 3 | Group 1 | Group 2 | Group 3 | |||
| Bisbe (2014)15 | Orthopedic | Postop | 3/59 (5.1) | 2/62 (3.2) | — | 20/59 (33.9) | 20/62 (32.3) | — | — | — | — |
| Bernabeu-Wittel (2016)16 | Hip fracture | Preop | 53/103 (51.5) | 52/100 (52.0) | 54/100 (54) | — | — | — | 12/103 (11.7) | 12/100 (12.0) | 10/100 (10.0) |
| Froessler (2016)17 | Abdominal | Periop | 5/40 (12.5) | 10/32 (31.3) | — | — | — | — | 1/40 (2.5) | 0/32 (0) | — |
| Khalafallah (2016)7 | Orthopedic, abdominal, ENT, plastic, gynecologic, urologic | Postop | 1/103 (0.1) | 5/98 (5.1) | — | — | — | — | — | — | — |
| Keeler (2017)18 | Colorectal cancer | Preop | 6/55 (10.9) | 6/61 (9.8) | — | — | — | — | 5/55 (9.1) | 4/61 (6.6) | — |
| Kim (2017)19 | Gastrectomy (cancer) | Preop | 3/218 (1.4) | 4/219 (1.8) | — | 15/222 (6.8) | 1/223 (0.4) | — | — | — | — |
| Lee et al (2019)20 | Benign uterine diseases | Preop | 0/52 | 0/49 | — | 0/52 | 0/49 | — | 0/52 | 0/49 | — |
| Padmanabhan et al (2019)21 | Cardiac | Preop | 16/20 (80) | 12/20 (60) | — | 0/20 | 3/20 | — | 1/20 (5) (unrelated causes) | 0/29 | — |
| Park et al (2019)22 | Unilateral TKA or THA | Intraop | 2/29 (6.9) | 4/29 (12.8) | — | 0/29 | — | — | — | — | — |
| Richards et al (2020)23 | Open abdominal surgery | Preop | 68/237 (29) | 67/237 (28) | — | 11/237 (5) | 5/237 (2) | — | 12/238 (5) | 10/236 (4) | — |
Note: Treatment groups are defined in Table 1.
Abbreviations: ABT, allogenic blood transfusion; AE, adverse event; ENT, ear, nose, and throat; FCM, ferric carboxymaltose; IV, intravenous; THA, total hip arthroplasty; TKA, total knee arthroplasty.
Outcome measures included the proportion of patients who experienced AEs, postoperative mortality rate, and hospital length of stay (Table 4). The proportion of patients with AEs was 6.8% (15/222) in the FCM group and 0.4% (1/223) in the placebo group in the study by Kim et al.19 Bisbe et al reported AEs in 33% (20/60) of patients in the FCM group and 32% (20/62) in the ferrous glycine sulfate comparator group (P=NS);15 this included all AEs reported during hospitalization (ie, before initiation of iron replacement therapy) and AEs related to surgical complications from initiation to 30 days postoperatively.15 Five percent of patients experienced AEs in the FCM group compared to 2% in the placebo group (risk ratio 2.20, 95% CI 0.78–6.24).23 Zero AEs among treatment groups were reported in both Lee et al20 and Park et al.22 Postoperative mortality was reported in 6 of the 10 included studies and ranged from 1% (2/237)23 to 11.7% (12/103) among patients receiving FCM16 compared with 017,20,21 to 10% (10/100) receiving placebo.16 The deaths were not attributed to study drug in the 5 studies; 3 studies did not discuss the possibility of a relationship between the deaths and study drug,17,18,23 1 study stated that the single death was due to unrelated causes,21 and 1 study stated that the causes of death were similar among the 3 treatment groups (IV FCM, IV FCM in combination with EPO, and placebo).16
The length of hospital stay ranged from 617,18 to 10.7 days19 with FCM versus618 to 11.6 days7 with comparators (Table 5). Two of the 8 studies reported statistically significant differences in transfusion rate7,17 and 2 studies reported significant differences in length of hospital stay between FCM and its comparators; the absolute difference in hospital stay was 3 days in Froessler et al17 and 2.8 days in Khalafallah et al.7 The variations in discharge criteria at the different institutions may have contributed to the differences in lengths of stay.
Table 5.
Secondary Endpoint Outcomes: Hospital Length of Stay and QOL
| Study | Surgery | Surgical Setting | Length of Hospital Stay, d | Instrument | Validated QOL Measure | ||||
|---|---|---|---|---|---|---|---|---|---|
| Group 1 | Group 2 | Group 3 | Group 1 | Group 2 | Group 3 | ||||
| Bisbe (2014)15 | Orthopedic | Postop | 7.9 (1.7)a | 7.6 (0.9)a | — | EQ-5D Barthel questionnaire |
Total EQ-5D increase: 0.6 (0.9)b Barthel increase: 92.6 (6.2)b |
Total EQ-5D increase: 0.6 (0.17)b Barthel increase: 93.0 (8)b |
— |
| Bernabeu-Wittel (2016)16 | Hip fracture | Preop | 7 (5–10)c | 8 (6–11)c | 8 (6–10)c | SF-36v2 | Physical decrease: 4.4 (14)d Mental decrease: 2.7 (20)d |
Physical decrease: 7.4 (11)d Mental decrease: 1.2 (13)d |
Physical: 4.5 (15)d Mental: −2 (20)d |
| Froessler (2016)17 | Abdominal surgery | Periop | 6 (1, 19)e | 9 (1, 23)e | — | SF-36 | SF-26 decrease (pre-post): 8 (18)f | Decrease (preop to postop): 6 (17)f | — |
| Khalafallah (2016)7 | Orthopedic, abdominal, ENT, plastic, gynecologic, urologic | Postop | 7.8 (10.3)a | 11.6 (15.6)a | — | SF-36 | SF-36 increase: 13.4g Physical increase: 13.4g Mental increase: 13.3g |
SF-36 increase: 9.1g Physical increase: 7.9g Mental increase: 9.9g |
— |
| Keeler (2017)18 | Colorectal cancer | Preop | 6 (5–10)c | 6 (4–9)c | — | — | — | — | — |
| Kim (2017)19 | Gastrectomy (cancer) | Preop | 10.7 (7.9)a | 10.9 (13.8)a | — | EORTC QLQ-C30v3 QLQ-STO22 |
Fatigue (week 3): 30.0 (26.8, 33.1)h Dyspnea (week 12): 9.5 (7.2, 11.8)h |
Fatigue (week 3): 34.6 (31.3, 37.9)h Dyspnea (week 12) 14.2 (11.3, 17.1)h |
— |
| Lee et al (2019)20 | Benign uterine diseases | Preop | — | — | — | SF-12 | PCS (visit 3 vs visit 1): 3.7 ± 10.0 MCS (visit 3 vs visit 1): 4.5 ± 8.0 |
PCS (visit 3 vs visit 1): 2.3 ± 8.0 MCS (visit 3 vs visit 1): 1.6 ± 6.5 |
— |
| Padmanabhan et al (2019)21 | Cardiac | Preop | 7 (6–12)c | 9 (6–14))c | — | EQ-5D SF-36 |
— | — | — |
| Park et al (2019)22 | Unilateral TKA or THA | Intraop | — | — | — | — | — | — | — |
| Richards et al (2020)23 | Open abdominal surgery | Preop | 9 (7–14)c | 9 (5–14)c | — | EQ-5D-5L MFI |
EQ-5D-5L Utility score: 10-day: 0.80 (0.20); 8-week: 0.79 (0.20); 6-month: 0.82 (0.22) EQ-5D-5L Health score: 10-day: 70.6 (20.5); 8-week: 70.7 (19.4); 6-month: 75.0 (18.4) MFI: 10-day: 53.2 (18.4); 8-week: 52.9 (17.1); 6-month: 48.8 (18.9) |
EQ-5D-5L Utility score: 10-day: 0.81 (0.21); 8-week: 0.77 (0.21); 6-month: 0.82 (0.21) EQ-5D-5L Health score: 10-day: 73.8 (19.6); 8-week: 71.1 (19.5); 6-month: 76.2 (19.2) MFI: 10-day: 50.5 (18.9); 8-week: 53.9 (17.7); 6-month: 47.4 (19.1) |
— |
Notes: Treatment groups are defined in Table 1; aValues are mean (standard deviation); bValues are the mean (standard deviation) increase from before surgery to postoperative day 30; cValues are median (first quartile–third quartile); dValues are mean (standard deviation) decrease from baseline to 60 days postdischarge; eValues are median (minimum, maximum); fValues are mean (standard deviation) increase from presurgery/intervention to postoperative week 4; gValues are the increase from postoperative day 1 to postoperative week 12; hValues are mean (95% confidence interval).
Abbreviations: ED-5Q, EuroQol 5-dimension quality of life scale; EORTC, European Organization for Research and Treatment of Cancer; FCM, ferric carboxymaltose; IV, intravenous; MCS, mental health composite scores; MFI, Multidimensional Fatigue Inventory; PCS, physical health composite scores; QLQ-C30v3, Quality of Life Questionnaire-Core 30 version 3; QLQ-STO22, Quality of Life Questionnaire-Stomach; QOL, quality of life; SF-12, Short Form-12 Health Survey; SF-36, 36-Item Short Form Survey; THA, total hip arthroplasty; TKA, total knee arthroplasty.
Validated measures of QOL included the Short Form Health Survey (SF-36 and SF-12) in 5 studies,7,16,17,20,21 the EuroQol 5-dimension quality of life scale (EQ-5D) in 3 studies,15,21,23 the Barthel Index questionnaires in 1 study,15 the Multidimensional Fatigue Inventory (MFI),23 and the European Organization for Research and Treatment of Cancer Quality of Life Questionnaire-Core 30 (EORTC QLQ-C30) questionnaire and the QLQ Gastric Cancer Module (QLQ-STO22) in 1 study.19 There were no statistically significant differences between IV FCM and comparators in QOL (overall score, change in score, or treatment effect) in any of these 7 studies.7,15–17,19,21,23 Bisbe et al reported no significant differences between IV FCM and the comparator (ferrous glycine sulfate) in total EQ-5D and Barthel scores.15 However, among patients with preoperative iron deficiency (serum ferritin <100 ng/mL), the IV FCM group had significantly better (ie, lower) mean ± SD EQ-5D subscores than the comparator group for “usual activities” (1.9 ± 0.3 vs 2.1 ± 0.3; P=0.026) and “anxiety or depression” (1.3 [0.6] vs 1.6 [0.7]; P=0.074) at the end of the study.15 In addition, among patients with severe postoperative anemia (Hb <10.0 g/dL), the FCM group had significantly better scores for “usual activities” than the comparator group at the end of the study (1.9 vs 2.3 [SD not reported]; P=0.04).15
Overall Quality of Evidence
The GRADE criteria were applied to rate the quality of evidence for all specified outcomes in this review (Supplementary Data, Appendix 2). Evidence quality was downgraded for risk of bias, inconsistency, indirectness, and imprecision. Across both primary and secondary endpoints, the overall quality of evidence was determined to be very low (Table 6). Publication bias was not detected. The rationale for these judgments are outlined in the Supplementary Data, Appendix 3.
Table 6.
Quality of Evidence (GRADE) Assessment
| Outcome | Studies | Risk of Bias | Inconsistency | Indirectness | Imprecision | Publication Bias | Other Considerations | Quality of Evidence |
|---|---|---|---|---|---|---|---|---|
| Absolute or relative change in hemoglobin concentration | ||||||||
| Rationale | 10/10 | 8/10 RCTs inadequately blinded outcome assessments; 8/10 RCTs inadequately blinded participants and personnel. The proportion of information from studies at high risk of bias is sufficient to affect the interpretation of results. | Positive effect demonstrated in 10/10 RCTs. Both clinical and methodologic heterogeneity are high. Therefore, some inconsistency exists. | Secondary endpoint in 6/10 studies (primary in 4/10) and therefore may not be powered appropriately. The intervention was given preop. in 7/10 studies, postop. in 3/10, and intraop. in 1/10. Difficult to make direct comparisons because of difference in comparators and populations. | 1 study terminated early; no CIs reported for 6/10 studies; wide CI/IQR for 5/10 studies. Insufficient sample sizes (<400 total) in 8/10 studies. | Undetected | There are potentially many subgroups in this analysis (eg, type of surgery, severity of condition, age) that may have affected findings that cannot be considered because of small sample sizes. | We have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of the effect. There generally appears to be a consistent effect with low risk of AEs. Most articles report positive outlook on use in future similar patient populations. Patients appear neutral to positive. |
| Absolute or relative change in iron stores (serum ferritin) | ||||||||
| Rationale | 8/10 (Not Lee or Richards) | 7/8 RCTs inadequately blinded outcome assessments; 7/8 RCTs inadequately blinded participants and personnel. The proportion of information from studies at high risk of bias is sufficient to affect the interpretation of results. | Positive effect demonstrated in 8/8 RCTs. Both clinical and methodologic heterogeneity are high. Direction appears consistent but variation appears large and therefore inconsistent. | Secondary endpoint in 6/8 studies (primary in 1 study) and therefore not sufficiently powered. Difficult to make direct comparisons because of differences in comparators and populations. | 1 study terminated early; no CI reported for 4/8; wide CI/IQR range for 4/4 studies. Insufficient sample sizes (<400 total) in 8/8 studies. | Undetected | Selective reporting in 2/8 studies (TSAT/ferritin endpoint not prespecified). | We have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of the effect |
| Absolute or relative change in iron stores (TSAT) | ||||||||
| Rationale | 6/10 (Not Lee,Bernabeau-Wittlel, Padmanabhan, or Richards) | 5/6 RCTs inadequately blinded outcome assessments; 6/6 RCTs inadequately blinded participants and personnel. The proportion of information from studies at high risk of bias is sufficient to affect the interpretation of results | Positive effect demonstrated in 6/6 RCTs. Both clinical and methodologic heterogeneity are high. Direction appears consistent but variation appears large and therefore inconsistent. | Secondary endpoint in 5/6 studies (primary in 1 study) and therefore not sufficiently powered. Difficult to make direct comparisons because of difference in comparators and populations | 1 study terminated early; no confidence interval reported for 3/6; wide CI/IQR for 3/3 studies. Insufficient sample sizes in each study (<400 total). | Undetected | Selective reporting in 2/6 studies (TSAT/ferritin endpoint not prespecified). | We have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of the effect. |
| Proportion of participants who received a perioperative ABT | ||||||||
| Rationale | 10/10 | 5/10 RCTs inadequately blinded outcome assessments; 7/10 RCTs inadequately blinded participants; 6/10 inadequately blinded personnel. The proportion of information from studies at high risk of bias is sufficient to affect the interpretation of results. | Positive effect reported in 2/10 studies (no difference in 8/10 studies). Consistency in findings may be an artifact of the disease severity/age/complexity of the surgery. Large variations in degree to which outcome is affected. | Primary endpoint in 4/10; percentage of blood transfusions secondary endpoint in 3/10; number of transfused blood units primary endpoint (1/10); reported as an absolute number in 8/10. Difference in populations and intervention schedules may have influenced outcome. | 1 study terminated early; no CI reported for 6/10; wide CI/IQR for 3/6. Uncertain if there was a large enough sample size despite a large enough number of events to calculate a precise effect estimate. Several studies had only 1 participant with the outcome of interest. | Undetected | N/A | We have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of the effect. The studies in this review looked at populations who had a large range of bleed/transfusion risk perioperatively. Need to assess ABT risk and adequately power the studies to detect sufficient number of events. Event may be too rare in some cases. |
| Proportion of participants who experienced adverse events | ||||||||
| Rationale | 6/10 (Not Bernabeu-Wittel, Froessler, Khalafallah, Keeler,) | 5/6 RCTs inadequately blinded outcome assessments; 5/6 RCTs inadequately blinded participants and personnel. The proportion of information from studies at high risk of bias is sufficient to affect the interpretation of results. | No SAE (4/6); no significant difference in safety reported for 4/6 studies. | Prespecified secondary endpoint (3/6). Safety was not assessed similarly within or between. Studies also had different comparators. | 1 study terminated early. Not clear how safety was assessed. | Undetected | N/A | We have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of the effect. Lack of evidence, high inconsistency in reporting, high indirectness, and high imprecision. |
| Postoperative mortality | ||||||||
| Rationale | Directly reported in 6/10 studies; indirectly in 4/10 as apparently no deaths occurred during follow-up. | 8/10 RCTs inadequately blinded outcome assessments; 8/10 RCTs inadequately blinded participants and personnel. The proportion of information from studies at high risk of bias is sufficient to affect the interpretation of results. | Results were not consistent; may be an artifact of severity of disease in population under study. | Not a surrogate outcome; prespecified secondary endpoint (2/6); primary endpoint composite (1/6) all-cause (2/6); 30-day (1/6). Death is dichotomous; however, the assumption in 4/10 studies is that no one had died. | Insufficient number of events to make a conclusion. Not a primary outcome in 9/10 studies, so likely underpowered to observe the true effect. | Undetected | N/A | We have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of the effect. |
| Length of hospital stay | ||||||||
| Rationale | 8/10 (Not Lee or Parks) | 4/10 RCTs inadequately blinded outcome assessments; 5/8 RCTs inadequately blinded participants and personnel. The proportion of information from studies at high risk of bias is sufficient to affect the interpretation of results. | Both clinical and methodologic heterogeneity are high. Heterogeneity among healthcare systems may also have influenced this outcome. Inconsistent results. | Not a surrogate outcome; prespecified secondary endpoint in 4/10 studies. | Wide CIs present in most studies. | Undetected | N/A | We have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of the effect. |
| Any validated measure of quality of life | ||||||||
| Rationale | 7/10 (Not Padmanabhan, Keeler, or Parks) | 6/7 RCTs inadequately blinded outcome assessments; 5/7 RCTs inadequately blinded participants and personnel. The proportion of information from studies at high risk of bias is sufficient to affect the interpretation of results. | Both clinical and methodologic heterogeneity are high. Results reported inconsistently owing to different instruments. No difference of effect is consistent. | Surrogate marker; outcome not assessed similarly within and among studies, yielding very indirect comparisons. | Wide CIs present in most studies. Extreme imprecision present. Concentrated on certain subscores in some studies. | Undetected. | Selective reporting was present for this outcome in a few studies. | We have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of the effect. |
Abbreviations: AE, adverse event; CI, confidence interval; IQR, interquartile range; RCT, randomized clinical trial; SAE, serious adverse event; TSAT, transferrin saturation.
Discussion
This SLR supports the use of FCM as treatment for adult patients with IDA in the preoperative and postoperative health states. In both the preoperative and postoperative elective surgery settings, IDA is a modifiable risk factor for elective surgical management.26,27 The 10 studies identified for inclusion in this SLR consistently reported change from baseline improvement in the three primary outcome measures: hemoglobin, ferritin, and TSAT.7,15–19 For these studies, there was less consistency for the association of FCM as treatment for perioperative IDA with each of the five secondary outcomes: ABT, adverse events, postoperative mortality, hospital length of stay, and QoL measures (see Tables 4 and 5).
Current guidelines from the Australian National Health and Medical Research Council29 and the United Kingdom National Institute for Health and Care Excellence30 recommend consideration of alternatives to blood transfusions for patients undergoing surgery and advise restrictive hemoglobin thresholds (<7.0 g/dL) for blood transfusions. In this SLR, three of the postoperative surgery studies reported either significantly fewer total ABT events17 or a significantly smaller proportion of patients receiving ABT7,19 with FCM than with the comparator. In the six preoperative surgery studies, the percentage of patients receiving ABT was not significantly different between assigned groups.16,18–21,23 In one preoperative surgery study, FCM was associated with reduced hospital readmission for post-surgical complications.23 Nonetheless, additional studies will be needed to fully assess the association of perioperative IV iron repletion, averted ABT, and associated ABT complications.28,32 Adverse events during hospitalization were recorded in three studies;15,21,23 as either estimated blood loss,21 number of blood transfusions,23 or gastrointestinal AEs.21,33 Post-operative mortality rates varied across the studies and was lowest in the study of benign uterine surgery and highest in the study of hip fractures.16,20 Length of hospital stay and measures of QoL also varied across studies (Table 5). Advanced age, as well as multiple comorbidities may have played a role in the lack of significance between FCM and comparators in these studies.7
While all 10 studies were randomized controlled trials, clinical and methodological heterogeneity was evident across the studies (Table 1), along with variation in the design elements (eg, type of blinding, duration of follow-up, timing of preoperative and postoperative assessments, comparator used, dosage, treatment schedule), All of these factors are important considerations when evaluating the utility of the exposure for the reported primary and secondary outcomes. A meta-analysis was not deemed feasible for this SLR, given the heterogeneity across the studies. Nonetheless, our findings are consistent with two prior quantitative syntheses of IV iron repletion in surgical patients which reported the efficacy of FCM associated with postoperative hemoglobin in elective surgeries.34,36 Additionally, for this SLR we conducted a thorough systematic qualitative assessment, which permitted a quality of evidence GRADE assessment (Table 6) for each of the primary and secondary outcomes. Although the overall quality of evidence scores were very low, future SLRs with GRADE assessments and consensus guideline considerations will likely benefit from assessment of iron repletion for elective surgeries partitioned as preoperative versus postoperative interventions. Together, the totality of data from these studies support the beneficial effect of FCM for hematological parameters in elective surgery, while continuing to inform on the role of iron repletion in perioperative patient management.31
Limitations
Several methodologic limitations in this systematic review are noteworthy. Physicians were not blinded in 5 studies (4 open-label7,18,20,21 and 1 patient-blinded19). In 3 other studies, the physician was blinded to treatment allocation, but the comparators used in those studies (eg, oral iron15 or usual care consisting of no treatment, oral iron recommendation, and transfusion17,22) might allow the physician to distinguish which patients were assigned to receive IV FCM vs the comparator in others. Overall, the risks of performance and biases were high or uncertain, highlighting the need for more effective blinding of patients and study personnel involved in the administration of study drug or outcome assessments. Blinding in some studies may not be feasible, despite the impact of blinding on the measurement of study outcomes. For example, a difference in route of administration between treatment arms, ethical considerations (possibility of exposing study patients to risks when blinding with placebo), or logistical hurdles (eg, limited economic support or authorization to use or access appropriate placebos and masking procedures) may be challenging in independent investigator-initiated studies.7,35
Other limitations of study heterogeneity may limit generalizability of the findings resulting from differing thresholds of Hb level, inclusion criteria, baseline clinical characteristics (eg, Hb, serum iron, serum ferritin, TSAT, ASA classification), IV FCM dosing and timing of administration, Hb thresholds for intervention (IV iron and transfusion). Heterogeneity or absence of reporting of secondary outcomes such as duration of follow-up, differences in criteria for hospital discharge (which would affect length of stay and may explain differences observed between the studies), and QOL instrument used (SF-36,7,16 EQ-5D and Barthel questionnaire,15 and EORTC QLQ-C30 and QLQ-STO2219) did not allow for a more in-depth review. Bias assessments in this review were qualitative, and meta-analysis was not feasible.
Conclusion
The preoperative correction of anemia and other hematological parameters with IV FCM appears to be a viable intervention to mitigate known risks associated with postsurgical anemia and consequent events such as the need for transfusion.36 IPostoperative patients with IDA, in whom oral iron is contra-indicated who are not able to tolerate oral iron or achieve a satisfactory response to oral iron may also benefit from FCM administration.7,28 The benefits of IV iron suggested by this SLR support the recommendations of guidelines that incorporate the use of IV iron in patients undergoing elective surgery.
Acknowledgments
We would like to thank Jaclyn Vialet, BS, MLS, Director of the Health Education Resource Center at St. John’s University College of Pharmacy and Health Sciences for her peer review and assessment of the electronic search strategies.
Funding Statement
Editorial support for the preparation of this article was provided by Peloton Advantage, LLC (Parsippany, NJ, USA), an OPEN Health company, funded by American Regent, Inc. (Shirley, NY, USA), a wholly owned subsidiary of Daiichi Sankyo.
Abbreviations
ABT, allogeneic blood transfusion; AE, adverse event; ASA, American Society of Anesthesiologists; ENT, ear, nose, and throat; EORTC-QLQ-C30, the European Organization for Research and Treatment of Cancer Quality of Life Questionnaire-Core 30; EPO, erythropoietin; EQ-5D, EuroQol 5-dimension quality of life scale; FCM, ferric carboxymaltose; GRADE, Grading of Recommendations Assessment, Development, and Evaluation; Hb, hemoglobin; IDA, iron-deficiency anemia; IV, intravenous; NHMRC, National Health and Medical Research Council; NICE, National Institute for Health and Care Excellence; NS, not significant; PBM, perioperative blood management; PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses; QLQ-ST022, Quality of Life Questionnaire-Gastric Cancer Module; QOL, quality of life; RBC, red blood cell; SC, subcutaneous; SD, standard deviation; SLR, systematic literature review; TSAT, transferrin saturation.
Author Contributions
JJJ, LMM, NB, MS: Main contribution to the study concepts and study design as well as supervision and revision of the manuscript.
JJJ, MS, LMM: Main contribution to the data acquisition, analysis, and interpretation.
JJJ and LMM: Main contribution to manuscript preparation.
NB: Main contribution to statistical support.
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Disclosure
John Jeffrey Jones was a postdoctoral fellow employed by St. John’s University (Jamaica, NY, USA) through a grant funded by American Regent, Inc. John Jeffrey Jones is currently employed by AVROBIO, Inc.; AVROBIO, Inc. was not involved in the content of this research or manuscript preparation. Linda M. Mundy, Nicole Blackman, and Michelle Shwarz are employees of American Regent, Inc., a wholly owned subsidiary of Daiichi Sankyo.
References
- 1.Spahn DR. Anemia and patient blood management in hip and knee surgery: a systematic review of the literature. Anesthesiology. 2010;113(2):482–495. doi: 10.1097/ALN.0b013e3181e08e97 [DOI] [PubMed] [Google Scholar]
- 2.Beattie WS, Karkouti K, Wijeysundera DN, Tait G. Risk associated with preoperative anemia in noncardiac surgery: a single-center cohort study. Anesthesiology. 2009;110(3):574–581. doi: 10.1097/ALN.0b013e31819878d3 [DOI] [PubMed] [Google Scholar]
- 3.Foss NB, Kristensen MT, Kehlet H. Anaemia impedes functional mobility after hip fracture surgery. Age Ageing. 2008;37(2):173–178. doi: 10.1093/ageing/afm161 [DOI] [PubMed] [Google Scholar]
- 4.Napolitano LM. Perioperative anemia. Surg Clin North Am. 2005;85(6):1215–1227. doi: 10.1016/j.suc.2005.10.012 [DOI] [PubMed] [Google Scholar]
- 5.Avgerinos DV, Llaguna OH, Seigerman M, Lefkowitz AJ, Leitman IM. Incidence and risk factors for the development of anemia following gastric bypass surgery. World J Gastroenterol. 2010;16(15):1867–1870. doi: 10.3748/wjg.v16.i15.1867 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Theusinger OM, Leyvraz PF, Schanz U, Seifert B, Spahn DR. Treatment of iron deficiency anemia in orthopedic surgery with intravenous iron: efficacy and limits: a prospective study. Anesthesiology. 2007;107(6):923–927. doi: 10.1097/01.anes.0000291441.10704.82 [DOI] [PubMed] [Google Scholar]
- 7.Khalafallah AA, Yan C, Al-Badri R, et al. Intravenous ferric carboxymaltose versus standard care in the management of postoperative anaemia: a prospective, open-label, randomised controlled trial. Lancet Haematol. 2016;3(9):e415–425. doi: 10.1016/S2352-3026(16)30078-3 [DOI] [PubMed] [Google Scholar]
- 8.Munoz M, Gomez-Ramirez S, Campos A, Ruiz J, Liumbruno GM. Pre-operative anaemia: prevalence, consequences and approaches to management. Blood Transfus. 2015;13(3):370–379. doi: 10.2450/2015.0014-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hofmann A, Ozawa S, Farrugia A, Farmer SL, Shander A. Economic considerations on transfusion medicine and patient blood management. Best Pract Res Clin Anaesthesiol. 2013;27(1):59–68. doi: 10.1016/j.bpa.2013.02.001 [DOI] [PubMed] [Google Scholar]
- 10.Camaschella C. Iron-deficiency anemia. N Engl J Med. 2015;372(19):1832–1843. doi: 10.1056/NEJMra1401038 [DOI] [PubMed] [Google Scholar]
- 11.Shander A, Knight K, Thurer R, Adamson J, Spence R. Prevalence and outcomes of anemia in surgery: a systematic review of the literature. Am J Med. 2004;116(Suppl 7A):58s–69s. doi: 10.1016/j.amjmed.2003.12.013 [DOI] [PubMed] [Google Scholar]
- 12.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. doi: 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Higgins JP, Altman DG, Gotzsche PC, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. doi: 10.1136/bmj.d5928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Balshem H, Helfand M, Schunemann HJ, et al. GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidemiol. 2011;64(4):401–406. doi: 10.1016/j.jclinepi.2010.07.015 [DOI] [PubMed] [Google Scholar]
- 15.Bisbe E, Molto L, Arroyo R, Muniesa JM, Tejero M. Randomized trial comparing ferric carboxymaltose vs oral ferrous glycine sulphate for postoperative anaemia after total knee arthroplasty. Br J Anaesth. 2014;113(3):402–409. doi: 10.1093/bja/aeu092 [DOI] [PubMed] [Google Scholar]
- 16.Bernabeu-Wittel M, Romero M, Ollero-Baturone M, et al. Ferric carboxymaltose with or without erythropoietin in anemic patients with hip fracture: a randomized clinical trial. Transfusion. 2016;56(9):2199–2211. doi: 10.1111/trf.13624 [DOI] [PubMed] [Google Scholar]
- 17.Froessler B, Palm P, Weber I, Hodyl NA, Singh R, Murphy EM. The important role for intravenous iron in perioperative patient blood management in major abdominal surgery: a randomized controlled trial. Ann Surg. 2016;264(1):41–46. doi: 10.1097/SLA.0000000000001646 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Keeler BD, Simpson JA, Ng O, Padmanabhan H, Brookes MJ, Acheson AG. Randomized clinical trial of preoperative oral versus intravenous iron in anaemic patients with colorectal cancer. Br J Surg. 2017;104(3):214–221. doi: 10.1002/bjs.10328 [DOI] [PubMed] [Google Scholar]
- 19.Kim YW, Bae JM, Park YK, et al. Effect of intravenous ferric carboxymaltose on hemoglobin response among patients with acute isovolemic anemia following gastrectomy: the FAIRY randomized clinical trial. JAMA. 2017;317(20):2097–2104. doi: 10.1001/jama.2017.5703 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lee S, Ryu KJ, Lee ES, Lee KH, Lee JJ, Kim T. Comparative efficacy and safety of intravenous ferric carboxymaltose and iron sucrose for the treatment of preoperative anemia in patients with menorrhagia: an open-label, multicenter, randomized study. J Obstet Gynaecol Res. 2019;45(4):858–864. doi: 10.1111/jog.13893 [DOI] [PubMed] [Google Scholar]
- 21.Padmanabhan H, Siau K, Nevill AM, et al. Intravenous iron does not effectively correct preoperative anaemia in cardiac surgery: a pilot randomized controlled trial. Interact Cardiovasc Thorac Surg. 2019;28(3):447–454. doi: 10.1093/icvts/ivy226 [DOI] [PubMed] [Google Scholar]
- 22.Park HS, Kim TY, Kim HJ, Ro YJ, Jang HY, Koh WU. The effect of intraoperative ferric carboxymaltose in joint arthroplasty patients: a randomized trial. J Clin Med. 2019;8(10):1674. doi: 10.3390/jcm8101674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Richards T, Baikady RR, Clevenger B, et al. Preoperative intravenous iron to treat anaemia before major abdominal surgery (PREVENTT): a randomised, double-blind, controlled trial [published online ahead of print, 2020 Sep 4]. Lancet. 2020;396(10259):1353–1361. doi: 10.1016/S0140-6736(20)31539-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.American Society of Anaesthesiologists House of Delegates/Executive Committee. ASA physical status classification system. 2014. Available from: https://www.asahq.org/standards-and-guidelines/asa-physical-status-classification-system. Accessed August12, 2019.
- 25.Bernabeu-Wittel M, Aparicio R, Romero M, et al. Ferric carboxymaltose with or without erythropoietin for the prevention of red-cell transfusions in the perioperative period of osteoporotic hip fractures: a randomized contolled trial. The PAHFRAC-01 project. BMC Musculoskelet Disord. 2012;13:27. doi: 10.1186/1471-2474-13-27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Clevenger B, Richards T. Pre-operative anaemia. Anaesthesia. 2015;70(Suppl 1):20–28. doi: 10.1111/anae.12918 [DOI] [PubMed] [Google Scholar]
- 27.Auerbach M. Intravenous iron in the perioperative setting [letter]. Am J Hematol. 2014;89(9):933. doi: 10.1002/ajh.23793 [DOI] [PubMed] [Google Scholar]
- 28.Munoz M, Auerbach M. Postoperative intravenous iron: a simple strategy to improve outcomes. Lancet Haematol. 2016;3(9):e401–402. doi: 10.1016/S2352-3026(16)30083-7 [DOI] [PubMed] [Google Scholar]
- 29.National Blood Authority. Patient Blood Management Guidelines: Module 2 Perioperative. Canberra, Australia: National Blood Authority; 2012. [Google Scholar]
- 30.Padhi S, Kemmis-Betty S, Rajesh S, Hill J, Murphy MF. Blood transfusion: summary of NICE guidance. BMJ. 2015;351:h5832. doi: 10.1136/bmj.h5832 [DOI] [PubMed] [Google Scholar]
- 31.Thakrar SV, Clevenger B, Mallett S. Patient blood management and perioperative anaemia. BJA Educ. 2017;17(1):28–34. doi: 10.1093/bjaed/mkw061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Maxwell MJ, Wilson MJA. Complications of blood transfusion. Continuing Educ Anaesth Crit Care Pain. 2006;6(6):225–229. doi: 10.1093/bjaceaccp/mkl053 [DOI] [Google Scholar]
- 33.Tolkien Z, Stecher L, Mander AP, Pereira DI, Powell JJ. Ferrous sulfate supplementation causes significant gastrointestinal side-effects in adults: a systematic review and meta-analysis. PLoS One. 2015;10(2):e0117383. doi: 10.1371/journal.pone.0117383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Koo CH, Shin HJ, Cho H, Ryu JH. The effect of perioperative intravenous iron on hemoglobin in surgical patients: a meta-analysis. J Surg Res. 2020;246:42–51. doi: 10.1016/j.jss.2019.08.023 [DOI] [PubMed] [Google Scholar]
- 35.Laso-Morales MJ, Vives R, Vallejo-Tarrat A, Calo N, Valle-Beltran A, Pontes C. Single dose of intravenous ferric carboxymaltose infusion versus multiple fractionated doses of intravenous iron sucrose in the treatment of postoperative anaemia in colorectal cancer patients: study protocol for a randomised controlled trial. Trials. 2019;20(1):23. doi: 10.1186/s13063-018-3125-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Muñoz M, Gomez-Ramirez S, Cuenca J, et al. Very-short-term perioperative intravenous iron administration and postoperative outcome in major orthopedic surgery: a pooled analysis of observational data from 2547 patients. Transfusion. 2014;54(2):289–299. doi: 10.1111/trf.12195 [DOI] [PubMed] [Google Scholar]
- 37.Page MJ, Moher D, Bossuyt PM, et al. PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. BMJ. 2021;372:n160. doi: 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed] [Google Scholar]