Abstract
Most patients with primary osteoarthritis of the elbow report a history of heavy lifting with the affected upper extremity
. Conservative treatment, including activity modifications, nonsteroidal anti-inflammatory drugs and the occasional intraarticular corticosteroid injection, may provide adequate pain relief in earlier stages
. When surgery is required, and despite the presence of cartilage wear, many patients with primary elbow osteoarthritis experience substantial pain improvement with joint preserving procedures
. The ulnar nerve needs to be carefully assessed and addressed at the time of surgery
. Although open debridement procedures are effective, arthroscopic osteocapsular arthroplasty has emerged as the surgical procedure of choice
. Total elbow arthroplasty is very successful in terms of pain relief and function, but it is reserved for patients with end-stage osteoarthritis who are relatively older and have failed joint preserving procedures.
1. Introduction
Primary elbow osteoarthritis (OA) is associated with pain and progressive loss of motion. Unlike hip and knee OA, primary elbow OA is characterized by1 the widespread formation of osteophytes and loose bodies,2 capsular contracture, and3 relative preservation of articular cartilage.1,2 Typically, pain is experienced at terminal range of motion and will respond particularly well to joint preserving procedures. This is partly explained by the features mentioned above and the fact that the elbow is a non-weight bearing joint in the majority of individuals (the exception being conditions with lack of adequate lower extremity support for ambulation, such as paraplegia).
2. Primary elbow OA: how common is it? Risk factors
Primary osteoarthritis of the elbow is relatively uncommon, affecting 2–3% of the population.3,4 Its low prevalence, combined with the common use of joint preserving procedures for primary elbow OA, is consistent with the observation that less than 5% of joint replacements are performed in patients with this diagnosis.5 Demographic studies have shown dramatic differences in the incidence of the elbow arthritis in different races, but it is unclear whether this is due to genetic or environmental factors.6,7
Originally recognized in Japan, osteoarthritis of the elbow is most commonly seen in men. In fact, it is a disorder almost exclusively of males.3,4,8 The average age at initial presentation is 50 years, but symptoms may start as early as the second decade of life.3,9 The dominant extremity is involved in about 80%–90% of patients, and bilateral involvement is present in 25%–60% of the patients.7
Occupations or avocations involving repetitive use of the upper extremity are the most common risk factors identified, being present in about 60% of the patients.10 Common conditions associated with a higher prevalence of primary elbow OA include manual laborers, weightlifters, throwing athletes, and wheelchair-dependent individuals.
It is widely accepted that elbow osteoarthritis is initiated at the radiocapitellar joint.1,11 The radiocapitellar joint, with a smaller articular surface than that of the ulnohumeral joint, supports 55% of the axial loads through the elbow with the forearm in neutral rotation.12 Cartilage wear seems to be more pronounced at the radiocapitellar joint, and the arthritic process then progresses to the ulnohumeral joint.1,11
3. History and physical examination
Patients with primary elbow OA usually complain of pain and progressive loss of motion. Occasionally, they refer episodes of catching and locking. When questioned, they also commonly confirm that they feel numbness and tingling in the territory of the ulnar nerve, with or without associated motor deficit. History taking should be directed to record the overall severity of pain, circumstances that aggravate symptoms, any prior injuries or attempted treatments, as well as the patient's occupation, overall activity level and expectations.
Physical examination maneuvers should be directed to identify pain generators, measure motion and carefully assess the ulnar nerve. Range of motion in flexion and extension is best measured with a goniometer, the forearm in complete supination, and the axis of flexion parallel to the floor. The majority of patients will have well preserved pronation and supination, but care must be taken to identify pain on the radius or radiocapitellar joint. Most patients will experience exquisite pain with forced, sudden, terminal flexion and extension; terminal range of motion pain responds particularly well to joint preserving procedures. When the articular surface contributes substantially to pain, there will be increased discomfort with resisted flexion or extension of the elbow in the mid-arc (mid arc, or articular shear pain), When wear of the articular cartilage contributes substantially to pain, not only there will be a positive articular shear test, but patients will also complain more often of pain at rest and pain at night.
Careful assessment of the ulnar nerve cannot be overemphasized. The ulnar nerve may be compressed by osteophytes at the ulnar tunnel, a tight ulnar retinaculum or both. A positive Tinel sign at the elbow, as well as decreased sensory or motor function of the ulnar nerve should be documented. Occasionally, some patients refer constant, burning neuropathic pain indicative of neuritis.13, 14, 15
4. Imaging studies
4.1. Radiographs
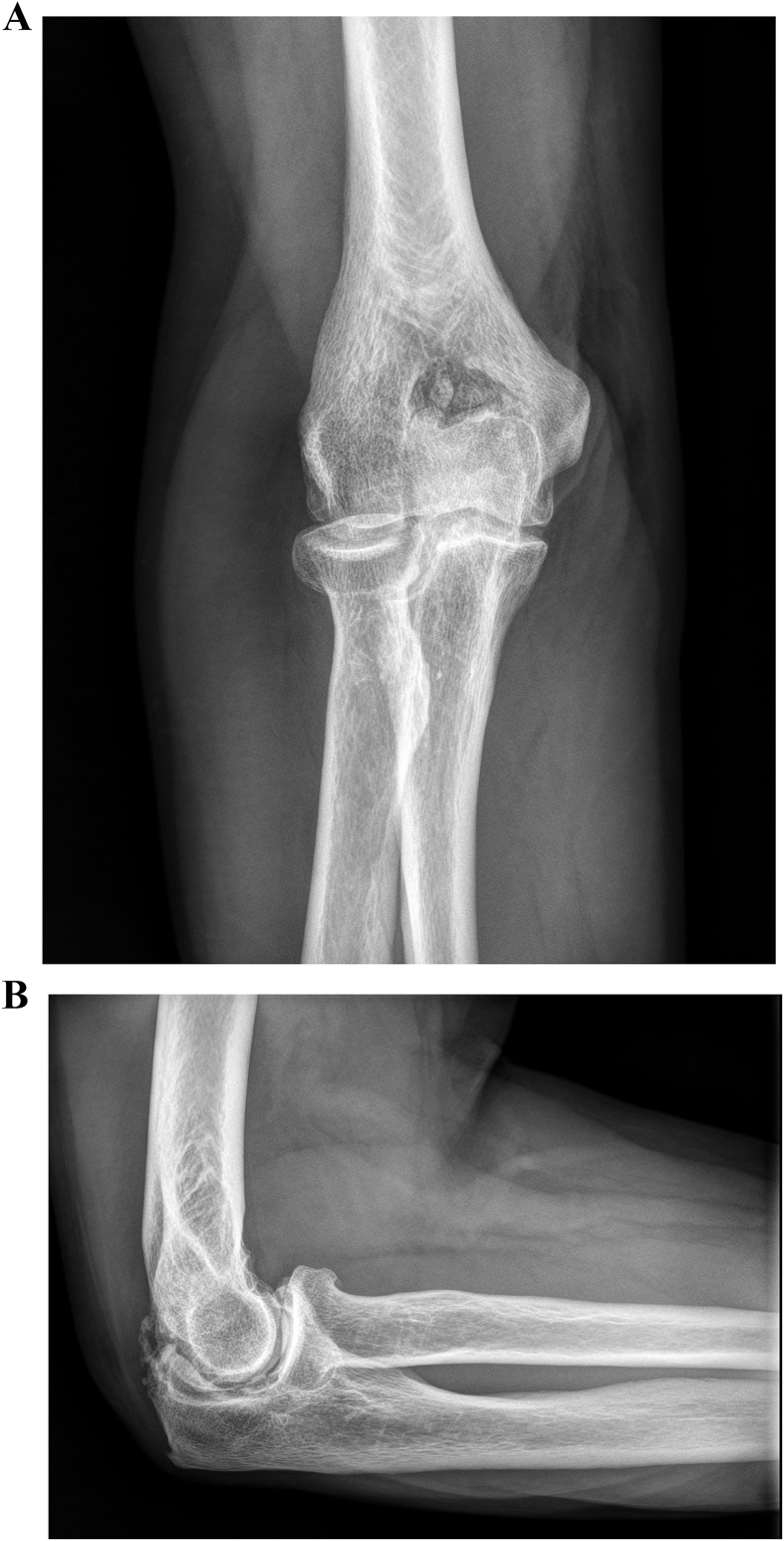
Anteroposterior and lateral radiographs of the elbow will usually confirm the diagnosis (Fig. 1). The radiographic features are classic. In early and moderate stages, osteophytes can be identified at the margin of the olecranon, the coronoid process, the radial head, and the margins of the articular surface of the distal humerus, with osteophytes filling in the olecranon, coronoid and radius fossae. Loose bodies are also commonly present. Osteophyte size has been found to be strongly correlated with decreased ROM in primary elbow OA.16,17 Joint narrowing can be appreciated as well, mostly on the radiocapitellar joint. The presence of ulnohumeral joint space narrowing typically is a sign of advance osteoarthritis and reflects the severity of cartilage destruction that correlates with mid-arc pain as well as pain at night or at rest.18 Accurate assessment of joint line narrowing becomes challenging in elbows with a flexion contracture, since the x-ray beam is not tangential to the joint surface when the elbow is flexed.
Fig. 1.
Anteroposterior (a) and lateral (b) radiographs of demonstrate primary elbow osteoarthritis.
Some authors have described severity grading systems that are mostly of use for research. Broberg and Morrey19 developed a staging system for elbow arthritis based on the condition of the joint line and osteophyte formation as identified on plain radiographs: grade 0 was defined as a normal joint, grade I as slight narrowing of joint space with a minimum formation of osteophytes, grade II as moderate narrowing of joint space with moderate formation of osteophytes, and grade III as severe degenerative changes with a gross destruction of the joint. The Hastings and Retting system20 is based on the presence of subluxation and involvement of the radiocapitellar joint. Class I is defined as degeneration at the margins of the ulnohumeral joint with the presence of coronoid and olecranon spurring and the absence of degenerative changes involving the radiocapitellar joint. Class II is defined as class I plus mild narrowing of joint space at the radiocapitellar joint but without subluxation of the radial head. Class III is defined as class II plus radiocapitellar subluxation.
4.2. Computed tomography
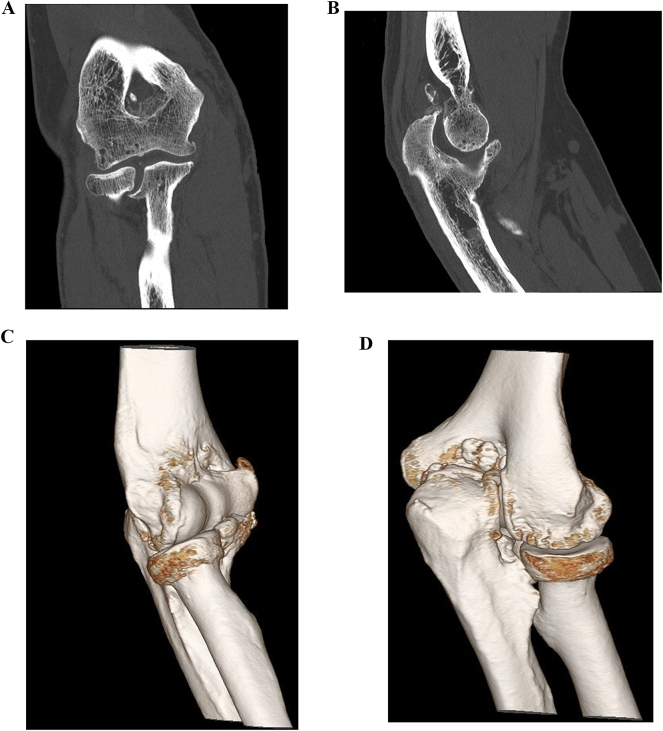
Although computed tomography (CT) is not necessary to make the diagnosis of primary elbow OA, it is an invaluable advance image modality for preoperative planning of joint preserving procedures. Careful analysis of two-dimensional images and three-dimensional renderings depict osteophyte formation and allow identification of loose bodies and fractured osteophytes (Fig. 2). Computed tomography images can be used as a “road map” to facilitate removal of the majority if not all impinging osteophytes. Particular attention should be paid to osteophytes in the medial and lateral elbow gutters, which may be more challenging to remove, and any osteophytes that may encroach on the ulnar nerve. From a research perspective, a CT-based staging system has been reported as highly reproducible and more practically feasible than previous staging systems based on radiographs.21,22
Fig. 2.
Computed tomography with two-dimensional images (a–b) and three-dimensional reconstruction (c–d) is extremely useful for the evaluation and surgical planning of patients undergoing arthroscopic osteocapsular arthroplasty and other joint debridement procedures.
4.3. Other investigations
Magnetic resonance is rarely used for the evaluation of primary elbow OA, although it has the potential to grade the severity of cartilage wear better than CT. Electromyography with nerve conduction studies may be considered to grade the severity of ulnar nerve entrapment, particularly in patients with motor changes that may be interested in the potential for recovery of hand strength.
5. Management
5.1. Conservative treatment
In early stages, when the patient reports mild to moderate pain and motion loss is relatively minor, conservative treatment is appropriate because symptoms are oftentimes slowly progressive and relatively well tolerated. Pain may respond to a combination of acetaminophen and nonsteroidal anti-inflammatory drugs. However, the most important aspect of conservative treatment is to explain to the patient the cause of the pain and the natural history of the process, and to recommend activity modifications. Avoiding pressure over the area of the cubital tunnel is recommended if there are ulnar nerve symptoms.
5.2. Surgical treatment
Surgical procedures are recommended for patients with moderate to severe pain that has not responded to conservative treatment. Surgery may also be indicated for patients with substantial motion loss, even if pain if less of a concern. Indications for surgery based on pain and motion need to be individualized. The majority of manual laborers do not consider surgery unless their pain is severe, or motion loss is substantially under the functional range.23 On the contrary, an isolated posterior fractured osteophyte may lead high-performance athletes such as tennis players to consider surgery, since otherwise they find it impossible to perform at their desired level. Similarly, relatively minor loss of extension may become a severe impediment to gymnastics and may lead athletes involved in gymnastics to consider surgery even though their motion loss would be considered perfectly functional for most activities of daily living.24
Once patients with primary elbow OA are considered candidates for surgery, the most common procedure is a joint-preserving debridement of the elbow joint. The goals of surgery include removal of loose bodies and fractured osteophytes, as well as removal of marginal osteophytes responsible for impingement with terminal motion. Anterior and posterior capsulectomies are commonly performed as well, but the need to perform capsulectomy in patients with less severe contractures is debated. Occasionally, the radiocapitellar joint or radial head are very painful and addressed with partial or complete radial head removal. Similarly, the ulnar nerve may be decompressed or transposed selectively or routinely, which largely depends on surgeon's preference. In our practice, we have migrated to arthroscopic debridement as the procedure of choice for all patients with primary elbow osteoarthritis. However, open exposures for joint debridement are very reliable as well.
Elbow replacement surgery is rarely considered for patients with primary OA. However, there is a small number of patients with severe pain at rest and complete loss of articular cartilage that do benefit from total elbow arthroplasty. When the radiocapitellar joint is a major source of discomfort, the role of radial head replacement, capitellar replacement or even unicompartimental elbow arthroplasty remains to be defined.
5.2.1. Open debridement
The concept of debridement of the elbow joint for management of primary elbow OA was originally described independently by Outerbridge in England and Kashiwagi in Japan.16,25 Early adaptors of the Outerbridge-Kashiwagi procedure utilized a triceps splitting approach for debridement of the posterior compartment and accessed the anterior compartment through a fenestration performed at the olecranon fossa. Morrey subsequently coined the term ulnohumeral arthroplasty (UHA) when he adopted this procedure and expanded it by adding a deep lateral approach to the anterior compartment for selected cases.26
Various alternative exposures described for management of posttraumatic elbow stiffness (the lateral column procedure, the medial column procedure, anterior exposures and combined exposures) can all be used for open debridement of the elbow joint.27, 28, 29 When used for primary elbow osteoarthritis, most surgeons favor the lateral column procedure described by Mansat and Morrey.30
When the lateral column procedure is used for management of elbow osteoarthritis, a lateral skin incision is placed over the lateral aspect of the distal humerus and extends distally over the location of the radial head. Access to the anterior compartment is gained by elevating the brachialis and common extensor group from the lateral aspect of the distal humerus proximally, while distally the common extensor group is split in line with Lister's tubercle. Access to the posterior compartment is gained underneath the anconeus and triceps. The capsule is excised first, followed by removal of loose bodies and osteophytes. The ulnar nerve is decompressed or transposed through a separate medial skin incision, when needed.
Open debridement can also be performed using the medial column procedure, which mirrors the lateral column procedure.31,32 The anterior compartment is accessed by elevating and splitting the common flexor group and the posterior compartment is accessed underneath the triceps. Although alternative anterior exposures33 have been described, they are rarely used due to the proximity of the anteromedial neurovascular bundle and the lack of access to the posterior compartment.
5.2.2. Arthroscopic osteocapsular arthroplasty (OCA)
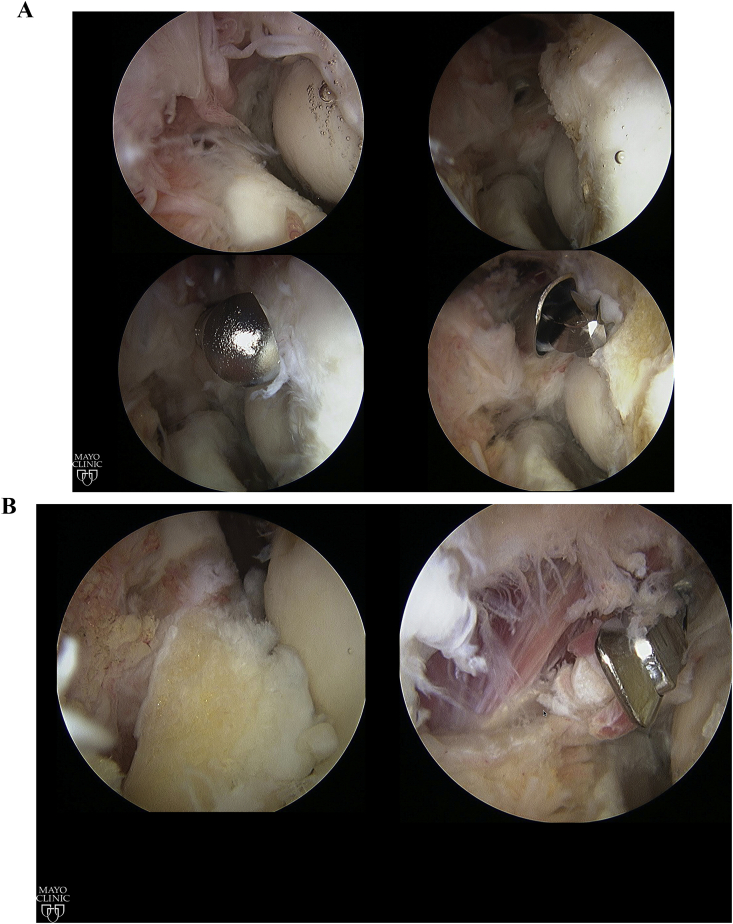
Arthroscopic debridement, also known as arthroscopic ulnohumeral arthroplasty or osteocapsular arthroplasty, involves removal of the impinging osteophytes, capsular release, and joint debridement with removal of loose bodies (Fig. 3), with or without ulnar nerve decompression. This technique has become the procedure of choice for many in recent years since it is generally believed to provide results that are at least comparable with those of traditional open procedures, but it allows better visualization of intra-articular lesions, a quicker recovery, and better cosmetic results.34 However, this procedure is technically demanding and is associated with risk of injury to the neurovascular structures. Surgeon experience and familiarity with this technique are perhaps the most important factors in preventing neurovascular injury during arthroscopic debridement.
Fig. 3.
A and B. Arthroscopic osteocapsular arthroplasty.
5.3. Surgical technique
Dr. O'Driscoll has been a pioneer in the development of a standardized sequence of four steps that is extremely useful when performing arthroscopic OCA34: (1) Get in and establish a view, (2) create a space in which to work, (3) bone removal, and (4) capsulectomy.
Our preference is to place the patient in the lateral decubitus position with the arm resting on a dedicated elbow arthroscopic arm holder. The shoulder must be forward elevated at least 90° with the elbow as high as the shoulder and flexed 90°. Prior to osteocapsular arthroplasty, when indicated, a limited open ulnar nerve decompression is performed through a small posteromedial skin incision 3–4 cm proximal and 3–4 cm distal to the medial epicondyle (a total of 7–8 cm decompression). Removal of medial osteophytes under the ulnar nerve may be accomplished through this posteromedial skin incision, which also allows removal of the posterior and transverse bundles of the medial collateral ligament and the posteromedial capsule off the olecranon to facilitate elbow flexion. Alternatively, the osteophyte removal can be done arthroscopically.
The decision to begin the procedure in the anterior compartment or the posterior compartment is a matter of personal preference. However, as described by O'Driscoll et al.,34 working in the posterior compartment and in the medial and lateral gutters may be challenging once substantial soft tissue swelling occurs, whereas swelling that occurs while working in the anterior compartment can be more effectively overcome with use of retractors.
Debridement of the posterior compartment is accomplished using two portals, one central and one posterolateral. A blunt Steinmann pin is used to enter into the joint through the posterolateral portal, because it is pointed enough to penetrate scar tissue and capsule but blunt enough to avoid cartilage damage. The arthroscopic canula is inserted through the posterolateral portal by sliding it over the Steinmann pin and working instruments (radiofrequency ablation device, shaver and bur) are inserted into the central portal.
After getting into the joint, space in which to work is created by removing debris, scar tissue and loose bodies with a shaver or a radiofrequency ablation device. The capsule is stripped off the humerus with a periosteal elevator. To recreate the olecranon fossa, the original floor of the fossa is identified, and osteophytes removed from it and from surrounding margins. The olecranon is restored to its normal shape by removing osteophytes from the tip and the sides. After osteophyte removal, a posterior capsulectomy is performed along the medial and lateral supracondylar ridges according to the severity of the flexion loss. If the patient lacks flexion, as is usually the case, the posterior capsulectomy includes not only release along the supracondylar ridges but also posteromedial and posterolateral capsular releases. With severe loss of flexion, the release is continued through the posterior bundle of the medial collateral ligament on the medial side (unless already released at the time of ulnar nerve decompression) and the radial head on the lateral side.
To work in the lateral gutter, the scope is placed in the posterior central portal and instruments in the posterolateral portal. Osteophytes are removed from the posterior capitellum and the lateral ridges of the trochlea and olecranon. The entire lateral compartment must be carefully inspected for loose bodies, as this is a typical location in which loose bodies may be nestled.
After completing work in the posterior compartment and the medial and lateral gutters, access to the anterior compartment is performed. For the anterior compartment three anterior portals are used routinely. The proximal anteromedial and anterolateral portals are used for the arthroscope and working instruments, and the proximal anterolateral portal is used for a retractor. Our preference is to first establish a proximal anteromedial portal with a blunt Steinmann pin inserted into the anterior compartment. Once the Steinmann pin is in place, the sheath is inserted into the joint over it and the arthroscope is inserted into the anterior compartment. In severely contracted elbows, the intracapsular space is very limited, sometimes severely, and space has to be created. This step includes removal of debris, scar tissue, and loose bodies as well as stripping the capsule off the humerus.
A retractor is routinely placed in the proximal anterolateral portal, greatly facilitating exposure and execution of surgery in the anterior compartment. Periosteal elevators are good instruments to be used as retractors. Osteophytes from the coronoid, coronoid fossae and radial fossae are removed and their normal shape is restored. After complete bone removal, an anterior capsulectomy is performed following four consistent steps: first, capsular detachment from the humerus proximally and along the medial and lateral supracondylar ridges; second, synovectomy and removal of loose tissue from its surface; third, the capsule is incised from medial to lateral with a wide Duckling™ punch using a “bite and peel” technique to incise the capsule over to the lateral edge of the brachialis, indicated by a strip of fatty tissue surrounding the radial nerve. The capsulotomy is performed distally, where the interval between the brachioradialis and extensor carpi radialis longus is readily identifiable; as the fourth and final step, the capsule is excised with a shaver disconnected from suction, to the exposed lateral edge of the brachialis. Removal of the anterior capsule carries the highest risk of injury to the posterior interosseous nerve and must be performed with extreme care.
5.4. Management of the ulnar nerve
The potential adverse effect of subclinical ulnar neuropathy was first identified in a study by Antuña et al.26 on open ulnohumeral arthroplasty procedures performed at Mayo Clinic. We now understand that the ulnar nerve is subject to compressive neuropathy by osteophytes, a tight ulnar retinaculum, or both. The indications to perform an ulnar nerve decompression or transposition at the time of open or arthroscopic debridement vary from surgeon to surgeon. Many surgeons would agree that the ulnar nerve should be decompressed or transposed at the time of debridement for patients with ulnar nerve symptoms, a positive Tinel sign along the location of the ulnar nerve, or flexion under 90°. Our preference is to decompress the ulnar nerve in the vast majority of arthritic elbows to completely eliminate the possibility of delayed-onset ulnar neuropathy (DOUN). We only perform a transposition if there is evidence of preoperative neuritis (neurogenic ulnar pain).
The incidence of DOUN has been reported to be 11% after the arthroscopic contracture release of the elbow.35 Three factors seem to be significantly associated with increased DOUN risk: preoperative hypertrophic ossification, preoperative neurological symptoms, and severity of preoperative loss of motion. In cases of rapidly progressive ulnar neuritis (which is characterized by increasing pain in the cubital tunnel, progressive loss of elbow motion, and neuropathy),36 urgent reoperation is recommended to transpose the ulnar nerve; if ulnar nerve transposition is delayed beyond 2 weeks after surgery, a complete recovery in neurological function may not occur.
5.5. Postoperative management
After surgery, elbow motion may be maintained using either continuous passive motion (CPM) or physical therapy. Unpublished data from our institution seems to indicate that CPM provides a gain of approximately 10° more when compared to physical therapy, and that the benefits of CPM are greater, the more severe the contracture is before surgery. As such, we offer CPM for patients interested in potentially regaining normal motion, as well as those with a high degree contracture. We have also adopted administration of 25 mg of oral indomethacin three times daily for 4–6 weeks.9 Some authors have reported intraarticular or oral steroids after surgery, but the risk of infection may be increased with intraarticular steroids.37
When CPM is selected, after confirming normal nerve function, an indwelling axillary catheter for a continuous brachial plexus block is performed. Following placement of the catheter, the arm is placed in a continuous passive motion (CPM) machine, using the largest arc that can be tolerated. The patient is given detailed instructions to come out of the machine every hour for 5 min to minimize soft-tissue or nerve problems due to continuous pressure or stretching. After the third postoperative day, the duration of each period out of the machine is determined by how long the patient can be out of the machine without losing some motion or experiencing difficulty regaining that motion as soon as he/she recommences CPM. The patient may be discharged on the second or third postoperative day, depending on the need for pain control. Removal of the indwelling axillary catheter 12 h prior to the anticipated time of discharge from the hospital permits confirmation for recovery of neurologic function.
Alternatively, for patients with less severe contracture the arm can be placed in a sling for comfort after surgery. From postoperative day 1, immediate active and active assisted motion is encouraged under the guidance of a physical therapist. With assistance from the contralateral hand, the patient gradually increases both extension and flexion, and nighttime splints may be considered for the first 3–4 weeks.28,36
5.5.1. Elbow arthroplasty
Primary elbow osteoarthritis rarely requires total elbow arthroplasty. This is due to the fact that most patients respond extremely well to joint debridement procedures, but also to the typical gender, age and activity level of patients with primary elbow osteoarthritis, which would increase the likelihood of mechanical failure of the implant. However, recent retrospective studies have reported that patients with radiologic evidence of ulnohumeral joint space narrowing experience worse clinical outcomes and higher radiologic recurrence rates after OCA when compared to those with intact joint spaces.21,22,28 There are older patients with severe involvement of the joint line space when elbow arthroplasty is the only procedure that can provide adequate pain relief.36
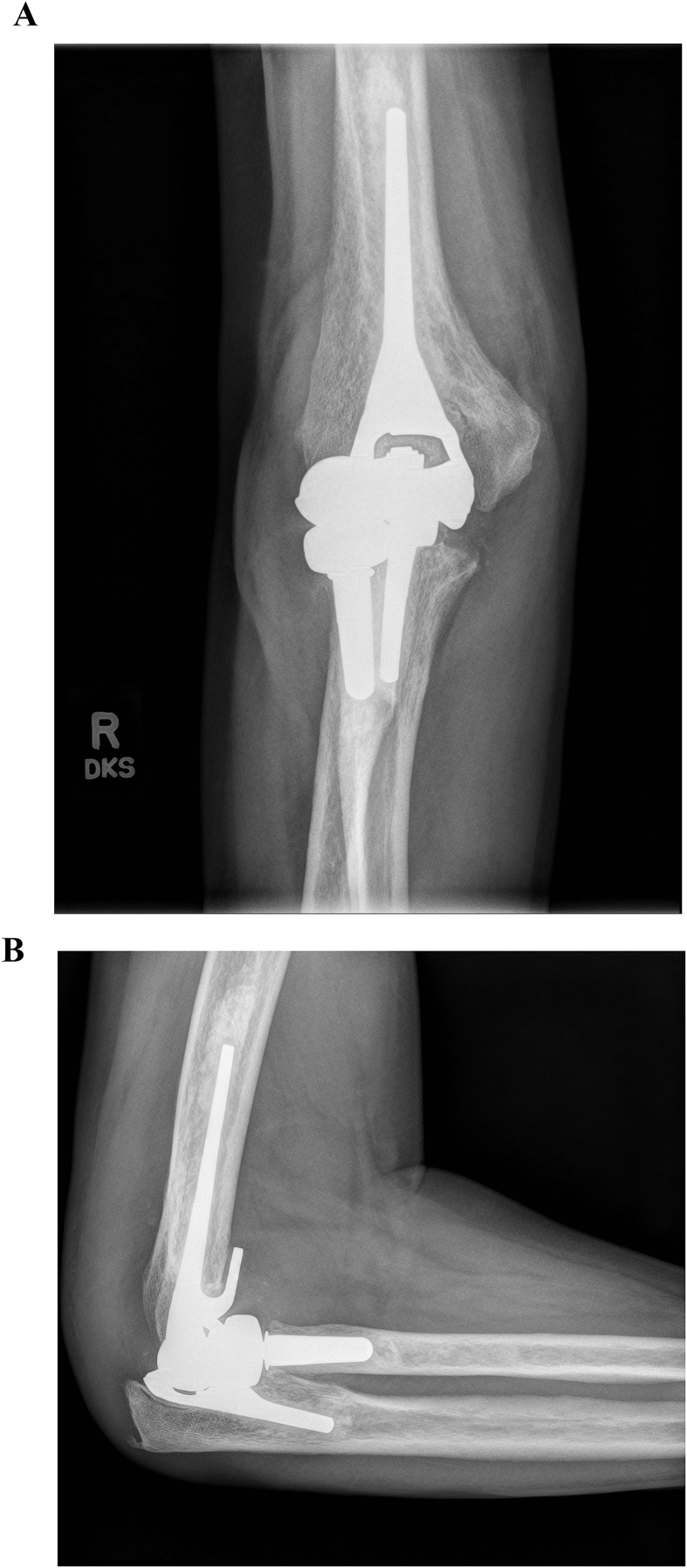
When elbow arthroplasty is considered for patients with primary osteoarthritis, consideration should be given to implantation of a high-performance implant (Fig. 4). A detailed discussion of all nuances associated with contemporary elbow replacement surgery exceed the scope of this study, but a few important details should be taken into consideration. Every effort should be made to avoid postoperative ulnar neuropathy and triceps insufficiency. In addition, consideration should be given to use of an unlinked implant with adequate ligamentous stability and sharing of the joint loads through the lateral column by having the humeral implant articulate with the native radial head or a radial head component. Finally, expectations and postoperative restrictions should be discussed at length with the patient both before and after surgery.
Fig. 4.
When patients with primary elbow osteoarthritis are considered for total elbow arthroplasty, a high-performance implant should be selected.
6. Reported outcomes in the literature
Arthroscopic osteocapsular arthroplasty and open debridement procedures have both been reported to be successful in improving pain, motion and function for patients with primary elbow osteoarthritis.22,39, 40, 41, 42 Arthroscopic OCA remains our procedure of choice since it has been reported to provide improved joint visualization with less surgical trauma and a faster postoperative recovery.10,43, 44, 45 However, the proximity of surrounding nerves and vessels requires expert knowledge of the anatomy and familiarity with proper portal placement to avoid complications associated with this procedure.24
A few studies have tried to report on the outcomes of open and arthroscopic debridement in a comparative fashion. Cohen et al.46 in a randomized controlled trial comparing the effectiveness of arthroscopic and open debridement of the elbow for osteoarthritis using the Outerbridge-Kashiwagi procedure, at a mean of 2.9 years follow up, reported that the open procedure might be more effective in improving flexion whereas patients treated with arthroscopy had a trend toward better pain relief, likely because of lesser intraoperative trauma and scar formation. Guerrero et al.,47 in a recent systematic review including patients with primary elbow OA treated with osteocapsular arthroplasty open or arthroscopic, reported no difference in patient functional outcomes between both procedures. However, the open group presented a larger improvement in flexion that the arthroscopic group (19° vs 10°), while the arthroscopic group had greater final postoperative flexion (128° cs 123°). They suggested that change in flexion and final flexion are limited by selection bias, with patients treated with open procedure having less flexion preoperatively and subsequently more ROM to improve. This finding is in contrast to that for elbow extension, for which both procedures demonstrated similar improvements. Kwak et al.28 reported as well that the outcomes of arthroscopic procedure are comparable to the open procedure in terms of pain relief and MEPS, although the open procedure shows better outcomes in improvement of flexion. They suggested that the degree of flexion may be due to incorrect placement of the anteromedial portal, which could preclude adequate debridement of the coronoid fossa.
Regarding complications, in a systematic review, Kim et al.48 reported that open debridement is associated with a relatively higher complication and reoperation rates than arthroscopic OCA. Neuropraxia seems to be the most prevalent complication.47 DOUN has already been discussed above. Other transient nerve injuries seem to be due to prolonged tourniquet times, cutaneous dysesthesia attributed to open incisions, simultaneous nerve transposition or retractor use. Guerrero et al.47 reported that more patients in the open group had postoperative ulnar nerve symptoms, but the open group had more patients with these symptoms preoperatively. This finding can be likely attributed to surgeons being more likely to select an open approach if an incision is already being made to release the cubital tunnel and possible transpose the ulnar nerve.
Although we have not been successful in predicting who will or will not experience this complication, our experience over the past few years has revealed that a prophylactic limited decompression of the ulnar nerve greatly reduces the risk. This has the benefit of probably making the surgery safer for less experienced surgeons. Our current preference is to decompress the ulnar nerve before the procedure when indicated, rather than transpose, through a small posteromedial incision and avoid end-range stretching if it causes symptoms such as ulnar neuritis or pain near the cubital tunnel.
Finally, there is limited information published on the outcome of total elbow arthroplasty specifically for primary osteoarthritis of the elbow. This is partly due to the fact that the vast majority of patients with primary osteoarthritis are treated with joint preserving procedures. Schoch et al.,38 in a series of 20 TEA performed for primary elbow OA reported that TEA represents a reliable surgical option for pain relief to this group. However, mechanical implant failure was documented in 17% of patients and moderate polyethylene wear occurred in 29%. In addition, elbow arthroplasty failed to significantly improve motion in all patients and restoration of extension was not always obtained.
7. Summary
Primary elbow osteoarthritis is commonly referred to elbow surgeons for evaluation and management. Most patients with primary osteoarthritis of the elbow report a history of heavy lifting with the affected upper extremity. Conservative treatment, including activity modifications, nonsteroidal anti-inflammatory drugs and the occasional intraarticular corticosteroid injection, may provide adequate pain relief in earlier stages. When surgery is required, and despite the presence of cartilage wear, many patients with primary elbow osteoarthritis experience substantial pain improvement with joint preserving procedures. Although open debridement procedures are effective, arthroscopic osteocapsular arthroplasty has emerged as the surgical procedure of choice. The ulnar nerve needs to be carefully assessed and addressed at the time of surgery. Total elbow arthroplasty is very successful in terms of pain relief and function, but it is reserved for patients with end-stage osteoarthritis who are relatively older and have failed joint preserving procedures.
References
- 1.Tsuge K., Mizuseki T. Debridement arthroplasty for advanced primary osteoarthritis of the elbow. Results of a new technique used for 29 elbows. J Bone Joint Surg Br. 1994;76:641–646. [PubMed] [Google Scholar]
- 2.Suvarna S.K., Stanley D. The histologic changes of the olecranon fossa membrane in primary osteoarthritis of the elbow. J Shoulder Elbow Surg. 2004;13:555–557. doi: 10.1016/j.jse.2004.02.014. [DOI] [PubMed] [Google Scholar]
- 3.Gramstad G.D., Galatz L.M. Management of elbow osteoarthritis. J Bone Joint Surg Am. 2006 Feb;88(2):421–430. doi: 10.2106/JBJS.E.00568. PMID: 16452758. [DOI] [PubMed] [Google Scholar]
- 4.Stanley D. Prevalence and etiology of symptomatic elbow osteoarthritis. J Shoulder Elbow Surg. 1994;3:386–389. doi: 10.1016/S1058-2746(09)80024-4. [DOI] [PubMed] [Google Scholar]
- 5.Kozak T.K., Adams R.A., Morrey B.F. Total elbow arthroplasty in primary osteoarthritis of the elbow. J Arthroplasty. 1998;13:837–842. doi: 10.1016/s0883-5403(98)90041-9. [DOI] [PubMed] [Google Scholar]
- 6.Kashiwagi D. Intraarticular changes of the osteoarthritic elbow, especially about the fossa olecrani. J Jpn Orthop Assoc. 1978;52:1367–1382. [Google Scholar]
- 7.Morrey B.F. Primary degenerative arthritis of the elbow: treatment by ulnohumeral arthroplasty. J Bone Joint Surg Br. 1992;74:409–413. doi: 10.1302/0301-620X.74B3.1587890. [DOI] [PubMed] [Google Scholar]
- 8.Papatheodorou L.K., Baratz M.E., Sotereanos D.G. Elbow arthritis: current concepts. J Hand Surg Am. 2013;38:605–613. doi: 10.1016/j.jhsa.2012.12.037. [DOI] [PubMed] [Google Scholar]
- 9.Cheung E.V., Adams R., Morrey B.F. Primary osteoarthritis of the elbow: current treatment options. J Am Acad Orthop Surg. 2008;16:77–87. doi: 10.5435/00124635-200802000-00005. [DOI] [PubMed] [Google Scholar]
- 10.Kroonen L.T., Piper S.L., Ghatan A.C. Arthroscopic management of elbow osteoarthritis. J Hand Surg Am. 2017;42:640–650. doi: 10.1016/j.jhsa.2017.05.023. [DOI] [PubMed] [Google Scholar]
- 11.Murata H., Ikuta Y., Murakami T. An anatomic investigation of the elbow joint, with special reference to aging of the articular cartilage. J Shoulder Elbow Surg. 1993;2:175–181. doi: 10.1016/1058-2746(93)90060-T. [DOI] [PubMed] [Google Scholar]
- 12.Hwang J.T., Kim Y., Shields M.N. Effects of axial forearm instability on force transmission across the elbow. J Shoulder Elbow Surg. 2019;28:170–177. doi: 10.1016/j.jse.2018.07.016. [DOI] [PubMed] [Google Scholar]
- 13.Williams B.G., Sotereanos D.G., Baratz M.E. The contracted elbow: is ulnar nerve release necessary? J Shoulder Elbow Surg. 2012;21:1632–1636. doi: 10.1016/j.jse.2012.04.007. [DOI] [PubMed] [Google Scholar]
- 14.Blonna D., O'Driscoll S.W. Delayed-onset ulnar neuritis after release of elbow contracture: preventive strategies derived from a study of 563 cases. Arthroscopy. 2014;30:947–956. doi: 10.1016/j.arthro.2014.03.022. [DOI] [PubMed] [Google Scholar]
- 15.Chen N.C., Liu A. The role of prophylactic ulnar nerve release during elbow contracture release. J Hand Surg Am. 2014;39:1837–1839. doi: 10.1016/j.jhsa.2014.04.009. [DOI] [PubMed] [Google Scholar]
- 16.Kashiwagi D. Excerpta Medica; 1985. Elbow Joint. [Google Scholar]
- 17.Nishiwaki M., Willing R., Johnson J.A., King G.J., Athwal G.S. Identifying the location and volume of bony impingement in elbow osteoarthritis by 3-dimensional computational modeling. J Hand Surg. 2013;38(7):1370e6. doi: 10.1016/j.jhsa.2013.03.035. [DOI] [PubMed] [Google Scholar]
- 18.Ratzlaff C., Ashbeck E.L., Guermazi A., Roemer F.W., Duryea J., Kwoh C.K. A quantitative metric for knee osteoarthritis: reference values of joint space loss. Osteoarthritis Cartilage. 2018;26(9):1215e24. doi: 10.1016/j.joca.2018.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Broberg M.A., Morrey B.F. Results of delayed excision of the radial head after fracture. J Bone Joint Surg Am. 1986;68:669–674. [PubMed] [Google Scholar]
- 20.Rettig L.A., Hastings H., II, Feinberg J.R. Primary osteoarthritis of the elbow: lack of radiographic evidence for morphologic predisposition, results of operative debridement at intermediate follow-up, and basis for a new radiographic classification system. J Shoulder Elbow Surg. 2008;17:97–105. doi: 10.1016/j.jse.2007.03.014. [DOI] [PubMed] [Google Scholar]
- 21.Kwak J.M., Kholinne E., Sun Y. Intraobserver and interobserver reliability of the computed tomography-based radiographic classification of primary elbow osteoarthritis: comparison with plain radiograph-based classification and clinical assessment. Osteoarthritis Cartilage. 2019;27:1057–1063. doi: 10.1016/j.joca.2019.03.004. [DOI] [PubMed] [Google Scholar]
- 22.Kwak J.M., Kim H., Sun Y. Arthroscopic osteocapsular arthroplasty for advanced-stage primary osteoarthritis of the elbow using a computed tomography-based classification. J Shoulder Elbow Surg. 2020;29:989–995. doi: 10.1016/j.jse.2019.09.036. [DOI] [PubMed] [Google Scholar]
- 23.Morrey B.F., Askew L.J., Chao E.Y. A biomechanical study of normal functional elbow motion. J Bone Joint Surg Am. 1981;63:872–877. [PubMed] [Google Scholar]
- 24.Blonna D., Lee G.C., O'Driscoll S.W. Arthroscopic restoration of terminal elbow extension in high-level athletes. Am J Sports Med. 2010 Dec;38(12):2509–2515. doi: 10.1177/0363546510376727. [DOI] [PubMed] [Google Scholar]
- 25.Minami M., Ishii S. Elsevier Science; New York, NY: 1985. Outerbridge- Kashiwagi Arthroplasty for Osteoarthritis of the Elbow Joint; pp. 189–196. [Google Scholar]
- 26.Antuña S.A., Morrey B.F., Adams R.A., O'Driscoll S.W. Ulnohumeral arthroplasty for primary degenerative arthritis of the elbow: long-term out- come and complications. J Bone Joint Surg Am. 2002;84:2168–2173. doi: 10.2106/00004623-200212000-00007. [DOI] [PubMed] [Google Scholar]
- 27.Wada T., Ishii S., Usui M. The medial approach for operative release of post-traumatic contracture of the elbow. J Bone Joint Surg Br. 2000;82:68–73. doi: 10.1302/0301-620x.82b1.9782. [DOI] [PubMed] [Google Scholar]
- 28.Kwak J.M., Kholinne E., Sun Y. Clinical outcome of osteocapsular arthroplasty for primary osteoarthritis of the elbow: comparison of arthroscopic and open procedure. Arthroscopy. 2019;35:1083–1089. doi: 10.1016/j.arthro.2018.11.057. [DOI] [PubMed] [Google Scholar]
- 29.Hattori Y., Doi K., Sakamoto S., Hoshino S., Dodakundi C. Capsulectomy and debridement for primary osteoarthritis of the elbow through a medial trans-flexor approach. J Hand Surg Am. 2011 Oct;36(10):1652–1658. doi: 10.1016/j.jhsa.2011.07.018. [DOI] [PubMed] [Google Scholar]
- 30.Mansat P., Morrey B.F. The column procedure: a limited lateral approach for extrinsic contracture of the elbow. J Bone Joint Surg Am. 1998;80:1603–1615. [PubMed] [Google Scholar]
- 31.Mansat P., Morrey B.F. fourth ed. W. B. Saunders; Philadelphia: 2009. Extrinsic Contracture: Lateral and Medial Column Procedures. Chapter 32. The Elbow and its Disorders; p. 487. [Google Scholar]
- 32.Tan V., Daluiski A., Simic P., Hotchkiss R.N. Outcome of open release for posttraumatic elbow stiffness. J Trauma. 2006;61:673–678. doi: 10.1097/01.ta.0000196000.96056.51. [DOI] [PubMed] [Google Scholar]
- 33.Aldridge J.M., 3rd, Atkins T.A., Gunneson E.E., Urbaniak J.R. Anterior release of the elbow for extension loss. J Bone Joint Surg Am. 2004;86:1955–1960. doi: 10.2106/00004623-200409000-00014. [DOI] [PubMed] [Google Scholar]
- 34.O'Driscoll S.W., Blonna D. Osteocapsular arthroplasty of the elbow: surgical technique. JBJS Essent Surg Tech. 2013;3(3):e15. doi: 10.2106/JBJS.ST.M.00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Blonna D., Huffmann G.R., O'Driscoll S.W. Delayed-onset ulnar neuritis after release of elbow contractures: clinical presentation, pathological findings, and treatment. Am J Sports Med. 2014;42:2113–2121. doi: 10.1177/0363546514540448. [DOI] [PubMed] [Google Scholar]
- 36.Kwak J.M., Jeon I.H. Surgical management for primary osteoarthritis of the elbow. J Orthop Surg. 2021;29(1) doi: 10.1177/2309499020988174. 2309499020988174. [DOI] [PubMed] [Google Scholar]
- 37.Nelson G.N., Wu T., Galatz L.M., Yamaguchi K., Keener J.D. Elbow arthroscopy: early complications and associated risk factors. J Shoulder Elbow Surg. 2014 Feb;23(2):273–278. doi: 10.1016/j.jse.2013.09.026. Epub 2013 Dec 14. PMID: 24332953. [DOI] [PubMed] [Google Scholar]
- 38.Schoch B.S., Werthel J.D., Sanchez-Sotelo J. Total elbow arthroplasty for primary osteoarthritis. J Shoulder Elbow Surg. 2017;26:1355–1359. doi: 10.1016/j.jse.2017.04.003. [DOI] [PubMed] [Google Scholar]
- 39.Kwak J.M., Kim H., Sun Y., Kholinne E., Koh K.H., Jeon I.H. Arthroscopic osteocapsular arthroplasty for advanced-stage primary osteoarthritis of the elbow using a computed tomography-based classification. J Shoulder Elbow Surg. 2020 May;29(5):989–995. doi: 10.1016/j.jse.2019.09.036. Epub 2019 Dec 9. [DOI] [PubMed] [Google Scholar]
- 40.Steinmann S.P., King G.J., Savoie F.H., III Arthroscopic treatment of the arthritic elbow. J Bone Joint Surg Am. 2005;87:2114–2121. doi: 10.2106/00004623-200509000-00026. [DOI] [PubMed] [Google Scholar]
- 41.Karelson M., Launonen A.P., Jokihaara J. Pain, function, and patient satisfaction after arthroscopic treatment of elbow in a retrospective series with minimum of 5-year follow-up. J Orthop Surg. 2019;27 doi: 10.1177/2309499019832808. 2309499019832808. [DOI] [PubMed] [Google Scholar]
- 42.Sochacki K.R., Jack R.A., 2nd, Hirase T. Arthroscopic debridement for primary degenerative osteoarthritis of the elbow leads to significant improvement in range of motion and clinical outcomes: a systematic review. Arthroscopy. 2017 Dec;33(12):2255–2262. doi: 10.1016/j.arthro.2017.08.247. [DOI] [PubMed] [Google Scholar]
- 43.Kim S.J., Kim J.W., Lee S.H., Choi J.W. Retrospective comparative analysis of elbow arthroscopy used to treat primary osteoarthritis with and without release of the posterior band of the medial collateral ligament. Arthroscopy. 2017;33:1506–1511. doi: 10.1016/j.arthro.2017.02.013. [DOI] [PubMed] [Google Scholar]
- 44.Lubiatowski P., Slezak M., Walecka J., Breborowicz M., Romanowski L. Prospective outcome assessment of arthroscopic arthrolysis for traumatic and degenerative elbow contracture. J Shoulder Elbow Surg. 2018;27:e269–e278. doi: 10.1016/j.jse.2018.02.068. [DOI] [PubMed] [Google Scholar]
- 45.Merolla G., Buononato C., Chillemi C., Paladini P., Porcellini G. Arthroscopic joint debridement and capsular release in primary and post-traumatic elbow osteoarthritis: a retrospective blinded cohort study with minimum 24-month follow-up. Musculoskel Surg. 2015;99(suppl 1):S83–S90. doi: 10.1007/s12306-015-0365-0. [DOI] [PubMed] [Google Scholar]
- 46.Cohen A.P., Redden J.F., Stanley D. Treatment of osteoarthritis of the elbow: a comparison of open and arthroscopic debridement. Arthroscopy. 2000;16:701–706. doi: 10.1053/jars.2000.8952. [DOI] [PubMed] [Google Scholar]
- 47.Guerrero E.M., Bullock G.S., Helmkamp J.K. The clinical impact of arthroscopic vs. open osteocapsular debridement for primary osteoarthritis of the elbow: a systematic review. J Shoulder Elbow Surg. 2020 Apr;29(4):689–698. doi: 10.1016/j.jse.2019.12.003. [DOI] [PubMed] [Google Scholar]
- 48.Kim D.M., Han M., Jeon I.H. Range-of-motion improvement and complication rate in open and arthroscopic osteocapsular arthroplasty for primary osteoarthritis of the elbow: a systematic review. Int Orthop. 2020;44:329–339. doi: 10.1007/s00264-019-04458-z. [DOI] [PubMed] [Google Scholar]