Dear Editor,
I am Dr. Norashikin Maslan, from the Department of Ophthalmology of University Kebangsaan Malaysia Medical Centre in Kuala Lumpur, Malaysia. I am writing to present a case report on central retina artery occlusion (CRAO) and optic neuropathy secondary to platelet rich plasma (PRP) injection.
In recent times, PRP injection is increasingly being used in medical specialties especially in aesthetic industry. PRP injection delays ageing with the presence of cytokines and growth factors in it[1]–[2]. It is administered either topically, superficially or through deep dermal injections[3]. The injection promotes the production of type 1 procollagen (skin fibroblast) and hyaluronic acid which in turn improves the skin texture, firmness and color homogeneity[4]. There are, however, some minor adverse effects of PRP such as discomfort, small prick bleeding and swelling that have been reported[4]. Although many have noted its efficacy[4]–[5], we would like to highlight a visually threatening complication caused by pure PRP injection in this report.
CASE PRESENTATION
A 48-year-old woman with no known medical illness arrived with a sudden onset loss of vision in left eye (OS) immediately after receiving a PRP injection on the glabellae region by an aesthetic practitioner. The monocular loss of vision was accompanied by an ocular discomfort. It is important to also note that her previous PRP injection, however, was uneventful and patient denies skin filler injections.
Patient was referred to a nearby ophthalmology clinic within 3h after the initial complaint. Ocular massage was performed for 10-15min before patient was hyperventilated. Oral medication was given to lower her intraocular pressure (IOP). Her vision did not improve regardless, so she decided to seek treatment at our center.
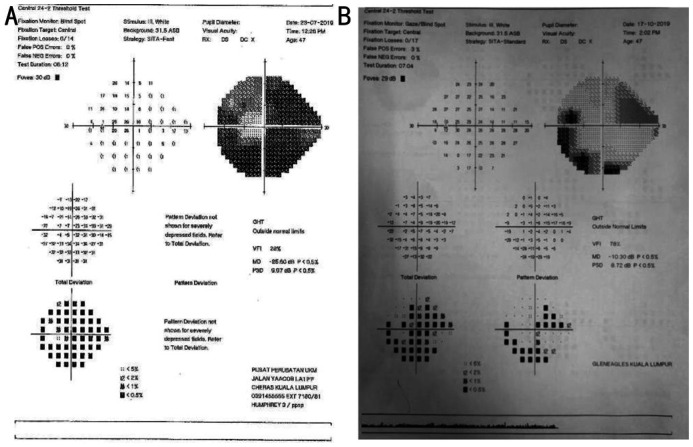
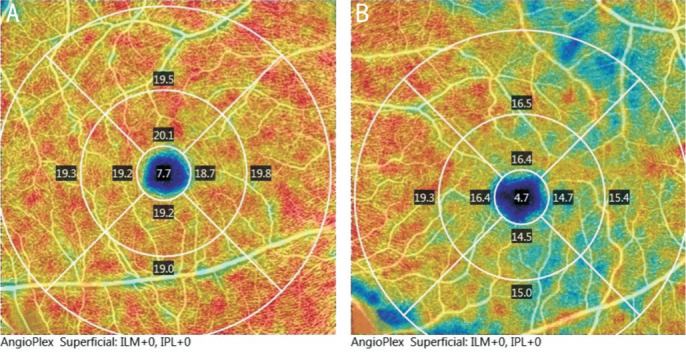
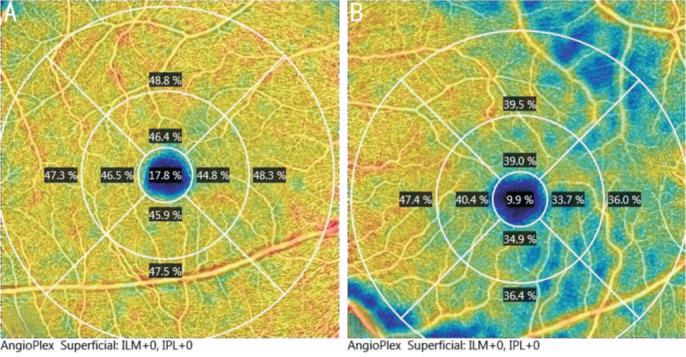
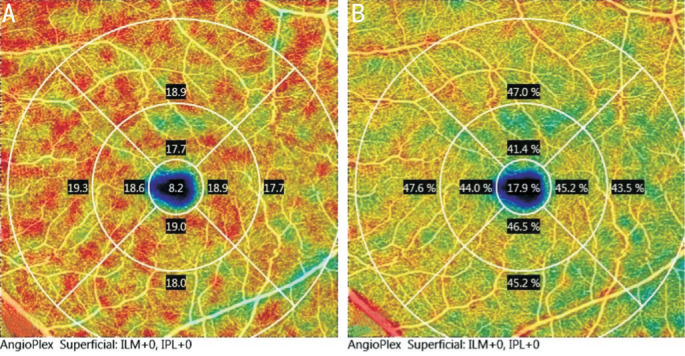
She arrived in 9h after the loss of vision. Her vision was 20/20 in right eye (OD) and 20/60 OS. There was a grade 3 relative afferent pupillary defect (RAPD) OS. Anterior segment examination OS was unremarkable with an IOP of 16 mm Hg. A fundus examination revealed generalized edematous retina with dull foveal reflex but no cherry red spot present (Figure 1A). Ocular examination OD was unremarkable. Her blood pressure was 150/90 mm Hg, with a pulse rate of 90 beats per minute and regular rhythm. A diagnosis of left CRAO secondary to PRP injection was then made. She was started on topical timolol 0.5%, topical dexamethasone 0.1%, and oral Acetazolamide. Optical coherence tomography angiography (OCTA) OS showed significant reduction in both vessel and perfusion density of the superficial capillary plexus (SCP) compared with the fellow eye (Figures 2 and 3). Humphrey visual field (HVF) 24-2 test showed-generalized constricted visual field OS with normal finding OD (Figure 4A).
Figure 1. Fundus photos of the left eye at first presentation (A) and after 2mo showing pale and cupped optic disc (B).
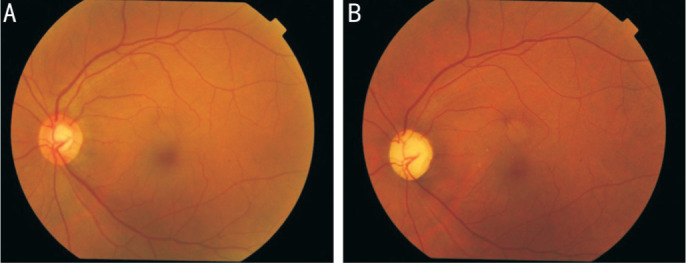
Figure 2. OCTA images of the patient.
Reduced vessel density in the superficial capillary plexus of the left eye (B) compared to the right eye (A) at initial presentation.
Figure 3. OCTA images of the patient.
Reduced perfusion density in the superficial capillary plexus of the left eye (B) compared to the right eye (A) at initial presentation.
Figure 4. HVF 24-2 showing generalized constricted visual field in the left eye at presentation (A) and 3mo after treatment showing significant improvement (B).
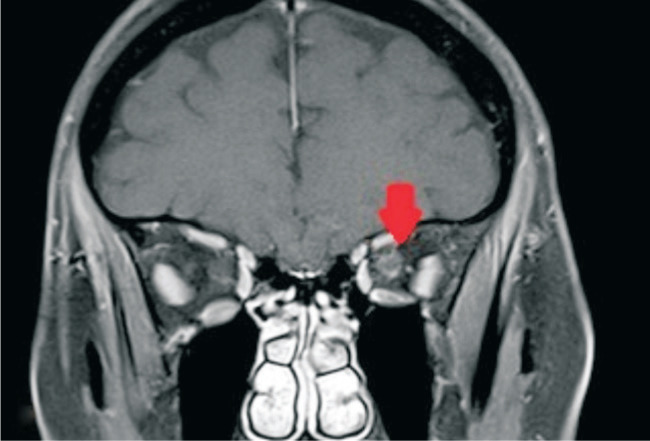
Four days after the PRP injection, the patient developed left periorbital hematoma associated with worsening of vision, occasional headache, and numbness over the glabella site. Her visual acuity dropped to 10/200 in OS. There was subconjunctival hemorrhage with anterior chamber cells of 4+. The fundus was hazy but no vitritis was seen. MRI orbit showed perineural enhancement of the optic nerve (Figure 5). The magnetic resonance venography (MRV) was normal and there was no retro-orbital hemorrhage. She was therefore treated for optic neuropathy and covered with intravenous methylprednisolone 250 mg q.i.d. for 3d followed by an oral prednisolone (1 mg/kg·d) for 11d.
Figure 5. MRI of the orbit showing perineural enhancement of the left optic nerve.
Fortunately, her vision improved slowly. Three months after the event, visual acuity has improved to 20/20 OS, but RAPD remained positive (grade 2) and red color saturation was 8/10 OS. Her periorbital hematoma resolved. Anterior segment examination was unremarkable, but optic disc OS became pale with an increase cupping to 0.9 (Figure 1B). Repeated OCTA showed improvement in perfusion and vessel density of the SCP (Figure 6). Her latest HVF also showed significant improvement (Figure 4B).
Figure 6. OCTA images of the patient.
Improved vessel (A) and perfusion density (B) on heat map of the superficial capillary plexus of the left eye after 2mo of follow up.
DISCUSSION
Treatment with PRP is generally safe and effective. While it appears simple to administer, devastating intravascular complications can still occur. Periocular vascular events are particularly important to be aware of as immediate intervention may restore the ocular circulation and prevent permanent blindness. Inadvertent intravascular injection of materials, either fillers, PRP or local anesthetic medications can cause retrograde flow to the original artery resulting in the obstruction of the retinal vascular lumen[1],[6]–[7]. The inner retina layer is supplied by central retinal artery and occlusion will result in ischemia of the inner retina layer, leading to edema and subsequently atrophy. In CRAO, some vision may be preserved since the choroidal circulation also supplies part of the inner retinal tissue. Experiments on animal models have demonstrated irreparable retinal damage occurs after 105min of vascular occlusion[1],[8].
Visual loss following filler injections has been reported although its occurrence is very rare. Facial injections can be performed at various locations such as at the glabella, nasolabial fold, or periorbital region. These regions are rich in blood supply. Injections at the glabella is commonly associated with compression or obstruction of blood vessel because the supratrochlear artery which supplies this region does not have a strong collateral circulation[9].
Blood supply to the face is from branches of the external and internal carotid arteries. Collaterals between the anterior and posterior ethmoidal arteries medial to the orbit, between the supraorbital and infraorbital artery anteriorly and the zygomaticotemporal branches laterally provides a rich supply to the periorbital and orbital region. Angular artery supplies the dorsal part of the nose and inferomedial fossa of the orbit[8]. Connections between the terminal branches of angular artery with supraorbital/supratrochlear artery plays an important role in establishing anastomosis[8].
In our case, the patient received PRP injections at the glabella area which is an area known to have arterial anastomosis. Hu et al[1] highlighted three essential concomitant factors that eventually lead to spread into the ophthalmic circulation which are retrograde movement of material, forceful injection with high pressure and adequate amount of injectable material. Following that, the embolus can travel along the central retinal artery causing occlusion of the retinal vessels.
Currently, limited literature suggested a correlation between CRAO and optic neuropathy and to our knowledge, this is the first case of unilateral CRAO with optic neuropathy after a PRP injection. In this patient, optic neuropathy was diagnosed based on perineural optic nerve enhancement seen on MRI. Optic neuropathy may be caused by either ischemia or inflammation, leading to disturbance of the blood-optic nerve barrier. We postulate that the retrograde flow of the PRP material may have affected both the central retinal artery and the posterior ciliary artery that mainly supplies the intra-orbital and intraocular portion of the optic nerve, resulting in impairment of small nutrient vessels feeding the nerve by ischemic or inflammatory process and consequently causing optic neuropathy.
Our case study shows that OCTA is a useful tool to establish reduced perfusion and vessel density, conforming to the study by Yang et al[10] that vessel density of the SCP and a 300 µm area around the foveal avascular zone is significantly reduced in retinal artery occlusion. OCTA is also a non-invasive alternative diagnostic tool to monitor progression of patients with vascular occlusions[11].
To conclude, our case highlights a potentially blinding complication of PRP injection around the ocular region. Even though it is a rare complication, ophthalmologist need to be aware of this due to its devastating complication. Prompt recognition and appropriate intervention may help prevent irreversible visual loss.
Acknowledgments
Authors' contributions: Maslan N analyzed, interpreted investigation result and major contributor in the writing manuscript, Tang SF analysed, interpreted, managed the patient and contribute in the writing manuscript, Wan Abdul Halim WH contributed in the writing of the manuscript, Din NM analyzed and contributed in the writing of the manuscript”.
Conflicts of Interest: Maslan N, None; Wan Abdul Halim WH, None; Din NM, None; Tang SF, None.
REFERENCES
- 1.Hu XZ, Hu JY, Wu PS, Yu SB, Kikkawa DO, Lu W. Posterior ciliary artery occlusion caused by hyaluronic acid injections into the forehead: a case report. Medicine (Baltimore) 2016;95(11):e3124. doi: 10.1097/MD.0000000000003124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Charles-de-Sá L, Gontijo-de-Amorim NF, Takiya CM, Borojevic R, Benati D, Bernardi P, Sbarbati A, Rigotti G. Effect of use of platelet-rich plasma (PRP) in skin with intrinsic aging process. Aesthet Surg J. 2018;38(3):321–328. doi: 10.1093/asj/sjx137. [DOI] [PubMed] [Google Scholar]
- 3.Banihashemi M, Nakhaeizadeh S. An introduction to application of platelet rich plasma (PRP) in skin rejuvenation. Reviews in Clinical Medicine. 2014;1(2):38–43. [Google Scholar]
- 4.Aust M, Pototschnig H, Jamchi S, Busch KH. Platelet-rich plasma for skin rejuvenation and treatment of actinic elastosis in the lower eyelid area. Cureus. 2018;10(7):e2999. doi: 10.7759/cureus.2999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Amini F, Abiri F, Ramasamy TS, Tan ESS. Efficacy of platelet rich plasma (PRP) on skin rejuvenation: a systematic review. Iranian Journal of Dermatology. 2015;18(3):119–127. [Google Scholar]
- 6.DeLorenzi C. Complications of injectable fillers, part 2: vascular complications. Aesthet Surg J. 2014;34(4):584–600. doi: 10.1177/1090820X14525035. [DOI] [PubMed] [Google Scholar]
- 7.Park KH, Kim YK, Woo SJ, Kang SW, Lee WK, Choi KS, Kwak HW, Yoon IH, Huh K, Kim JW, Korean Retina Society Iatrogenic occlusion of the ophthalmic artery after cosmetic facial filler injections: a national survey by the Korean Retina Society. JAMA Ophthalmol. 2014;132(6):714–723. doi: 10.1001/jamaophthalmol.2013.8204. [DOI] [PubMed] [Google Scholar]
- 8.Loh KT, Chua JJ, Lee HM, Lim JT, Chuah G, Yim B, Puah BK. Prevention and management of vision loss relating to facial filler injections. Singapore Med J. 2016;57(8):438–443. doi: 10.11622/smedj.2016134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lafaille P, Benedetto A. Fillers: contraindications, side effects and precautions. J Cutan Aesthet Surg. 2010;3(1):16–19. doi: 10.4103/0974-2077.63222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yang S, Liu XQ, Li H, Xu J, Wang F. Optical coherence tomography angiography characteristics of acute retinal arterial occlusion. BMC Ophthalmol. 2019;19(1):147. doi: 10.1186/s12886-019-1152-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nakayama LF, Bergamo VC, Silva LSC, Moraes NSB. Optical coherence tomography (OCT) angiography of central retinal artery occlusion in the patent cilioretinal artery: a case report. Arq Bras Oftalmol. 2018;81(3):242–246. doi: 10.5935/0004-2749.20180048. [DOI] [PubMed] [Google Scholar]