Abstract
AIM
To establish the necessity of silicone tube intubation in acute dacryocystitis (AD) patients undergoing endonasal endoscopic dacryocystorhinostomy (En-DCR).
METHODS
Patients presenting with unilateral AD were randomly assigned to two treatment groups. En-DCR procedures were performed following lacrimal abscess formation, with the operation being performed with silicone intubation for patients in group B but not group A. Functional success was defined by an absence of additional AD episodes, no epiphora, and ostium patency as established via endoscopic evaluation or fluorescein irrigation. Operative success rates and demographic variables were compared between treatment groups.
RESULTS
In total, 66 patients were analyzed in the present study (33 per group), with complete postoperative data having been successfully collected from 27 and 22 patients in group A and group B, respectively. All patients exhibited complete resolution of acute inflammation. Upon follow-up, granulation tissue was detected around the ostium at higher rates in group B (9/22, 40.9%) relative to group A (4/27, 14.8%). At the 12-month follow-up time point, patients in group A exhibited higher success rates (25/27, 92.6%) relative to patients in group B (20/22, 90.9%), but this difference was not significant. Cases of lacrimal passage reconstruction failure in both groups were attributed to excessive fibrous and/or granulation tissue formation proximal to the intranasal ostium.
CONCLUSION
Given that these two operative approaches are associated with similar rates of operative success and in light of differences in granulation tissue formation, cost, and operative duration, these data do not support the routine silicone intubation of AD patients following En-DCR surgery.
Keywords: En-DCR, silicone tube, acute dacryocystitis, granulation
INTRODUCTION
Acute dacryocystitis (AD) is a condition in which the lacrimal sac becomes acutely inflamed as a consequence of the obstruction of the nasolacrimal duct, and may additionally occur due to excessive bacterial growth within the stagnant fluid in the lacrimal sac[1]. Conventional treatments for AD can result in negative outcomes including cutaneous fistula development, recurrent dacryocystitis, and adverse systemic effects of prolonged antibiotic treatment while awaiting external dacryocystorhinostomy (Ex-DCR)[2]–[3]. Ex-DCR is also generally thought to be contraindicated in cases of AD, as it can exacerbate inflammation and has the potential to spread infections to other soft tissues, increasing the risk of causing sepsis[2]–[4]. Endonasal endoscopic dacryocystorhinostomy (En-DCR) surgical approaches, in contrast, have been reported to be associated with good outcomes in AD patients[1]–[2],[5]. En-DCR operations can rapidly alleviate patient pain and expedite the resolution of a given infection, while decreasing the length of hospitalization and eliminating the need for additional DCR operations in most cases. Relative to Ex-DCR, En-DCR also has the potential to expedite the detection of pathological conditions that may interfere with successful DCR procedures, does not leave a visible scar, and does not interfere with the medial canthal tendon complex that is critical for lacrimal pumping[5]–[7]. However, whether or not silicone tube intubation is appropriate during En-DCR surgery in AD patients remains unclear, with some authors reporting the use of such an approach, whereas others forgo it[1],[5]–[9].
The present study was therefore designed to assess whether or not routine bicanalicular silicone tube intubation is necessary for AD patients undergoing En-DCR.
SUBJECTS AND METHODS
Ethical Approval
This study was conducted from September 2015 to October 2018 in the Eye Hospital of Wenzhou Medical University. All protocols were consistent with the Declaration of Helsinki and were approved by the Institutional Medical Ethics Committee (Wenzhou Medical University, Wenzhou, Zhejiang, China). All patients provided informed consent to participate.
All AD patients referred to the Orbit & Oculoplastic Surgery Department were enrolled in this study. Patients were diagnosed based upon medical histories and physical evaluation of lacrimal sac abscess formation. Patient demographic characteristics such as age, gender, affected eye, and disease course were recorded, as was the interval between AD onset and surgical treatment.
Patients were excluded if they were under 18 years of age, had a history of nasal trauma, stenosis, or obstruction of the lacrimal canaliculus, were suffering from severe nasosinusitis, primary neoplasms of the nasolacrimal system, or systemic diseases associated with coagulopathy or increased bleeding risk. A senior otorhinolaryngologist diagnosed all comorbid nasal diseases in enrolled patients.
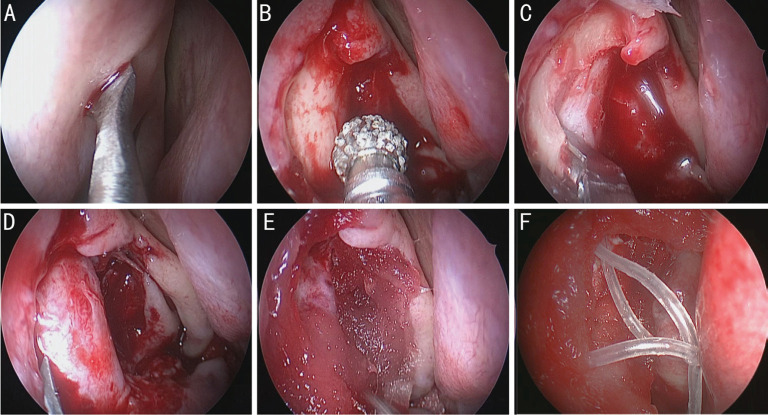
AD patients underwent early intravenous treatment with broad-spectrum antibiotics, and En-DCR was performed immediately following abscess formation. Patients were randomly assigned to two treatment groups (group A and group B), with all surgical procedures being performed by one surgeon (Yu B) via a previously described approach[7],[10]. Briefly, patients were placed under general anesthesia. The lateral nasal wall was then infiltrated with 1 mL of 0.9% sodium chloride containing epinephrine (1:100 000). A 0-degree endoscope (Karl Storz, Tuttlingen, Germany) was used for visualization, after which a blade was used to incise the lateral nasal mucosa in the lacrimal sac fossa region (Figure 1A). The underlying maxilla and frontal process were then thinned with a power burr (XPS3000; Medtronic Xomed, MN, USA; Figure 1B), and removed with a Kerrison rongeur (Figure 1C). An ultrasharp 9# MVR knife (EdgePlus Trocar Blade, Alcon, TX, USA) was then utilized to anteriorly incise a portion of the lacrimal sac in order to release the purulent material from the abscess, after which the blind tip of the soft probe was inserted through the superior punctum and slowly rotated into the lacrimal sac to tent its medial wall, with the MVR knife being used to fully open the sac using the probe as a guide (Figure 1D). Saline irrigation via the lower canalicular puncta was then used to assess patency, after which the nasalmucosal flap was trimmed and positioned such that it covered the exposed maxilla, followed by Merogel (Medtronic Xomed) packing of the wound (Figure 1E). Patients in group B then had a bicanalicular silicone tube inserted into the ostium from the superior and inferior puncta, with the tube ends being tied together within the nasal cavity (Figure 1F).
Figure 1. Depicts the steps of the surgical methods.
A: A blade was used to incise the lateral nasal mucosa wall proximal to the lacrimal sac fossa; B: A power burr was used to thin the maxilla and frontal process of the maxilla; C: Maxilla was removed with a Kerrison rongeur; D: An ultrasharp 9# MVR knife was utilized to anteriorly incise a portion of the lacrimal sac in order to release the purulent material from the abscess; E: The sac was fully opened with the knife, and a nasalmucosal flap was trimmed and positioned such that it covered the exposed maxilla, after which Merogel was packed around the wound; F: Patients in group B had a bicanalicular silicone tube inserted into the ostium from the superior and inferior puncta, with the tube ends being tied together within the nasal cavity.
After surgery, patients were administered methylprednisolone (20 mg/kg·d) and ceftriaxone (2.0 g/d) for 3d, with lacrimal syringing with dexamethasone and tobramycin being conducted once per day for 3d. All subjects were directed to utilize an intranasal Rhinocort Aqua Nasal Spray (Astra Zeneca, DE, USA) twice per day for 6wk, and all subjects were monitored for evidence of acute inflammation.
Patients underwent follow-up at 1, 2wk, 1, 2, 3, 6, and 12mo after surgery. During each follow-up vising, any symptoms, purulent secretions, or epiphora incidence were recorded, and intranasal ostium patency was assessed through lacrimal irrigation and endonasal endoscopic examinations. Dye tests were also performed as appropriate.
Lacrimal tubing remained in the ostium for 3mo. When granulation tissue was detected around the ostium during follow-up, a novel suction and cutter instrument was used to cut it off, after which the wound was filled for 1min with cotton paced with dexamethasone. The patient was then directed to use an intranasal spray for an additional 2wk.
Surgery was defined as a functional success when there was no evidence of postoperative epiphora or purulent secretions, functional endoscopic dye test results were normal, ostial patency with an apparently normal epithelized mucosa was observed upon endonasal endoscopic evaluation, and the lacrimal system exhibited free-flowing irrigation.
Statistical Analysis
Data were analyzed with SPSS v17.0. Demographic data were compared using independent t-tests and Chi-squared tests, while operative success rates were compared with Pearson's Chi-squared tests or Fisher's exact tests. P<0.05 was the significance threshold for these analyses.
RESULTS
In total, 66 patients were initially enrolled in this study (n=33/group), with En-DCR being performed for 33 patients in group A and 32 patients in group B. The remaining group B patient declined surgical treatment. During surgery, three patients (1 in group A; 2 in group B) were found to exhibit canaliculus stenosis or obstruction. These four patients were excluded from the study.
Overall, 27 and 22 patients in groups A and B, respectively, completed postoperative follow-up and were retained for final analyses. The clinical characteristics of these patients are compiled in Table 1. There were no significant differences between groups with respect to patient age (t=0.179, P=0.858), gender (χ2=0.002, P=0.961), or disease course (t=-0.334, P=0.740). In total, 3 patients (2 in group A; 1 in group B) underwent plasty of nasal septum deviation. Pain in these patients was relieved within 3d post-surgery, with medial canthal swelling having resolved within 5d postoperatively.
Table 1. Patient clinical characteristics.
| Characteristic | Group A | Group B |
| Gender | ||
| Male | 10 (37.0) | 8 (36.4) |
| Female | 17 (63.0) | 14 (63.6) |
| Age (y) | 54.04±13.69 | 53.32±14.26 |
| Eye | ||
| Right | 13 (48.1) | 12 (54.5) |
| Left | 14 (51.9) | 10 (45.5) |
| Disease course (d) | 3.78±1.85 | 3.95±1.84 |
n (%)
Over the course of follow-up, 40.9% of patients in group B (9/22) exhibited ostial granulation tissue, with this rate being significantly higher than that observed in group A (14.8%, 4/27; χ2=4.235, P<0.05; Figure 2). Granulation tissue was detected at 6.22±2.56wk postoperatively in group A (range: 4-12wk) and 4.00±2.47wk in group B (range: 2-12wk), with this interval being significantly shorter in group B relative to group A (t=3.069, P<0.05).
Figure 2. Granulation tissue around the ostium.

A: Granulation tissue around the ostium in group A; B: Granulation tissue around the ostium in group B.
At the 3-month follow-up time point, 96.3% of patients in group A (26/27) and 100% of patients in group B (22/22) exhibited successful surgical outcomes, with no significant differences in these rates between groups (χ2=0.832, P>0.05). At the 6-month follow-up time point, three additional cases of failure were observed (1 in group A; 2 in group B), with success rates in these two respective groups having fallen to 92.6% (25/27) and 90.9% (20/22). At the 12-month follow-up time point, no new cases of failure had been identified, such that there were 25 and 20 successful cases in groups A and B, respectively (Figure 3). There was no significant difference in success rates between these groups (χ2=0.046, P>0.05). Lacrimal passage reconstruction failure as a consequence of excess fibrous and/or granulation tissue formation around the intranasal ostium was observed in 2/27 patients in group A and 2/22 patients in group B (Figure 4).
Figure 3. Success cases in each group.

A: Ostial patency with an epithelized mucosal layer exhibiting a normal appearance under endonasal endoscopic examination in group A; B: Normal functional endoscopic dye test results in group A; C: Silicone tube placement in the ostium; D: Ostial patency with an epithelized mucosal layer exhibiting a normal appearance under endonasal endoscopic examination in group B.
Figure 4. Failed cases in each group.

A: A failed case in group A exhibiting granulation tissues occluding the lacrimal sac ostium; B: Another failed case in group A exhibiting scar synechia occluding the lacrimal sac ostium; C: A failed case in group B exhibiting silicone tube placement in the ostium; D: The same case in group B exhibiting ostium closure at 9mo following tube removal.
DISCUSSION
AD is an ophthalmic emergency wherein patients experience pain and swelling in the lacrimal sac region that is commonly linked to contiguous preseptal tissue inflammation[11]. Recently, many researchers have sought to clarify whether Ex-DCR or En-DCR are preferable for the treatment of AD[2],[5]–[7],[9]–[10]. En-DCR enables surgeons to approach the lacrimal sac through uninfected tissues, thereby reducing many of the risks associated with Ex-DCR, making the former operation particularly promising for the treatment of AD as a means of rapidly resolving patient symptoms, reducing the duration of hospitalization, and eliminating the need for subsequent lacrimal surgery[7]–[8],[12].
Whether silicone tube intubation following En-DCR is necessary when treating AD patients has not been evaluated in detail to date. Such an intubation approach was reported in studies conducted by Lee and Woog[5], Wu et al[7], Chisty et al[13], and Kamal et al[14], whereas it was not be applied in studies performed by Duggal et al[15], Joshi and Deshpande[6]. Despite this variation in approach, success rates have been reported to be quite high (81.8% to 94.3%)[5]–[7],[13]–[15]. Silicone tube implantation has been suggested to eliminate the need for lacrimal-passage cicatrization by minimizing the stimulation of connective tissue hyperplasia while supporting and reinforcing nasolacrimal duct formation[5]. Even so, such tubing is rarely used in the context of chronic dacryocystitis as it is an inorganic material with the potential to promote intranasal tissue granulation, peripunctal granulation, postoperative infection, canalicular laceration, and punctal adhesions. This tubing also has the potential to be dislodged from the rhinostomy site or to otherwise cause discomfort to patients[16]–[17]. In these prior reports, silicone intubation was only applied in cases with canalicular stenosis, a small scarred lacrimal sac, or a narrow upper nasal cavity[16]–[18]. Herein, we found that granulation tissue formation rates were significantly higher in patients that had undergone silicone tube intubation, and this tissue formed at an earlier time point than in non-intubated patients. This further confirms the ability of silicone tubing to promote intranasal granulation formation. We did not observe other previously reported complications such as premature tube loss, peripunctal granulation, postoperative infection, or canalicular laceration. No significant differences in success rates were observed between patients that did and did not undergo silicone tube intubation during En-DCR.
The formation of granulation tissue at the ostium is a major cause of En-DCR surgical failure[7]–[8],[19]. A number of approaches have been used to assess and maintain rhinostomy site patency after surgery in an effort to prevent the development of such granulation tissue. Topical corticosteroid nasal sprays are the primary approach to preventing this debilitating process[19]–[20]. As this approach only applies the drug to the anterior edges of the inferior and middle turbinates, we do not believe that this noninvasive treatment approach is sufficient to promote the regression of extant granulation tissue[21]. As such, we utilized a low-suction cutting instrument (New Direction Medical Optic Instrument Co., Ltd., Dezhou, China; Figure 5) to directly excise observed granulation tissue. This instrument was composed of a negative pressure suction device with a suction regulator, and a cutting portion with a sharp edge and a blunt tip. This device was operated manually by compressing its handles, and has a suction opening measuring 2.5×2.7 mm2. After this treatment approach, we found that granulation tissue regression was evident in 8/11 patients exhibiting ostial granulation tissue. There are certain limitations to the present study. For example, the sample size of this analysis was limited. Future large-scale prospective analyses will thus be essential to validate our results.
Figure 5. A low-suction cutting instrument utilized to excise granulation tissues from patients in which they had formed following En-DCR.

The cutting edge and aspiration port are respectively marked by white and black arrows.
In summary, as we found that success rates were slightly higher in patients that did not undergo silicone tube intubation, and such intubation was associated with prolonged operative duration, increased costs, the need for an additional operation to remove the tubing, and the potential for persistent epiphora when the tubing is present in the ostium, we do not recommend routine intubation of AD patients undergoing En-DCR surgery at present.
Acknowledgments
Conflicts of Interest: Yu B, None; Xia Y, None; Sun JY, None; Ye Q, None; Tu YH, None; Zhou GM, None; Wu WC, None.
REFERENCES
- 1.Ali MJ, Joshi SD, Naik MN, Honavar SG. Clinical profile and management outcome of acute dacryocystitis: two decades of experience in a tertiary eye care center. Semin Ophthalmol. 2015;30(2):118–123. doi: 10.3109/08820538.2013.833269. [DOI] [PubMed] [Google Scholar]
- 2.Cahill KV, Burns JA. Management of acute dacryocystitis in adults. Ophthalmic Plast Reconstr Surg. 1993;9(1):38–41. doi: 10.1097/00002341-199303000-00005. [DOI] [PubMed] [Google Scholar]
- 3.Huber-Spitzy V, Steinkogler FJ, Huber E, Arocker-Mettinger E, Schiffbänker M. Acquired dacryocystitis: microbiology and conservative therapy. Acta Ophthalmol (Copenh) 1992;70(6):745–749. doi: 10.1111/j.1755-3768.1992.tb04880.x. [DOI] [PubMed] [Google Scholar]
- 4.Coden DJ, Hornblass A, Haas BD. Clinical bacteriology of dacryocystitis in adults. Ophthalmic Plast Reconstr Surg. 1993;9(2):125–131. doi: 10.1097/00002341-199306000-00008. [DOI] [PubMed] [Google Scholar]
- 5.Lee TS, Woog JJ. Endonasal dacryocystorhinostomy in the primary treatment of acute dacryocystitis with abscess formation. Ophthalmic Plast Reconstr Surg. 2001;17(3):180–183. doi: 10.1097/00002341-200105000-00006. [DOI] [PubMed] [Google Scholar]
- 6.Joshi RS, Deshpande AS. Success rate of conventional dacryocystorhinostomy in post-acute dacryocystitis compared to endonasal dacryocystorhinostomy in acute dacryocystitis. J Ophthalmic Vis Res. 2017;12(3):290–295. doi: 10.4103/jovr.jovr_264_15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wu WC, Yan WT, MacCallum JK, Tu YH, Jiang AC, Yang Y, Xiao TL, Li J, Wang QM, Qu J. Primary treatment of acute dacryocystitis by endoscopic dacryocystorhinostomy with silicone intubation guided by a soft probe. Ophthalmology. 2009;116(1):116–122. doi: 10.1016/j.ophtha.2008.09.041. [DOI] [PubMed] [Google Scholar]
- 8.Madge SN, Chan W, Malhotra R, Ghabrial R, Floreani S, Wormald PJ, Tsirbas A, Selva D. Endoscopic dacryocystorhinostomy in acute dacryocystitis: a multicenter case series. Orbit. 2011;30(1):1–6. doi: 10.3109/01676830.2010.535952. [DOI] [PubMed] [Google Scholar]
- 9.Chong KK, Abdulla HAA, Ali MJ. An update on endoscopic mechanical and powered dacryocystorhinostomy in acute dacryocystitis and lacrimal abscess. Ann Anat. 2020;227:151408. doi: 10.1016/j.aanat.2019.07.009. [DOI] [PubMed] [Google Scholar]
- 10.Li EY, Wong ES, Wong AC, Yuen HK. Primary vs secondary endoscopic dacryocystorhinostomy for acute dacryocystitis with lacrimal sac abscess formation: a randomized clinical trial. JAMA Ophthalmol. 2017;135(12):1361–1366. doi: 10.1001/jamaophthalmol.2017.4798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jain S, Ganguly A, Singh S, Mohapatra S, Tripathy D, Rath S. Primary nonendoscopic endonasal versus delayed external dacryocystorhinostomy in acute dacryocystitis. Ophthalmic Plast Reconstr Surg. 2017;33(4):285–288. doi: 10.1097/IOP.0000000000000759. [DOI] [PubMed] [Google Scholar]
- 12.Morgan S. The treatment of acute dacryocystitis using laser assisted endonasal dacryocystorhinostomy. Br J Ophthalmol. 2004;88(1):139–141. doi: 10.1136/bjo.88.1.139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chisty N, Singh M, Ali MJ, Naik MN. Long-term outcomes of powered endoscopic dacryocystorhinostomy in acute dacryocystitis. Laryngoscope. 2016;126(3):551–553. doi: 10.1002/lary.25380. [DOI] [PubMed] [Google Scholar]
- 14.Kamal S, Ali MJ, Pujari A, Naik MN. Primary powered endoscopic dacryocystorhinostomy in the setting of acute dacryocystitis and lacrimal abscess. Ophthalmic Plast Reconstr Surg. 2015;31(4):293–295. doi: 10.1097/IOP.0000000000000309. [DOI] [PubMed] [Google Scholar]
- 15.Duggal P, Mahindroo NK, Chauhan A. Primary endoscopic dacryocystorhinostomy as treatment for acute dacryocystitis with abscess formation. Am J Otolaryngol. 2008;29(3):177–179. doi: 10.1016/j.amjoto.2007.05.007. [DOI] [PubMed] [Google Scholar]
- 16.Onerci M. Dacryocystorhinostomy. Diagnosis and treatment of nasolacrimal canal obstructions. Rhinology. 2002;40(2):49–65. [PubMed] [Google Scholar]
- 17.Unlu HH, Gunhan K, Baser EF, Songu M. Long-term results in endoscopic dacryocystorhinostomy: is intubation really required? Otolaryngol Head Neck Surg. 2009;140(4):589–595. doi: 10.1016/j.otohns.2008.12.056. [DOI] [PubMed] [Google Scholar]
- 18.Longari F, Dehgani Mobaraki P, Ricci AL, Lapenna R, Cagini C, Ricci G. Endoscopic dacryocystorhinostomy with and without silicone intubation: 4 years retrospective study. Eur Arch Otorhinolaryngol. 2016;273(8):2079–2084. doi: 10.1007/s00405-015-3876-2. [DOI] [PubMed] [Google Scholar]
- 19.Kansu L, Aydin E, Avci S, Kal A, Gedik S. Comparison of surgical outcomes of endonasal dacryocystorhinostomy with or without mucosal flaps. Auris Nasus Larynx. 2009;36(5):555–559. doi: 10.1016/j.anl.2009.01.005. [DOI] [PubMed] [Google Scholar]
- 20.Ali MJ, Wormald PJ, Psaltis AJ. The dacryocystorhinostomy ostium granulomas: classification, indications for treatment, management modalities and outcomes. Orbit. 2015;34(3):146–151. doi: 10.3109/01676830.2015.1014510. [DOI] [PubMed] [Google Scholar]
- 21.Jo A, Lee SH, Song WC, Shin HJ. Effects of ostium granulomas and intralesional steroid injections on the surgical outcome in endoscopic dacryocystorhinostomy. Graefes Arch Clin Exp Ophthalmol. 2018;256(10):1993–2000. doi: 10.1007/s00417-018-4024-7. [DOI] [PubMed] [Google Scholar]