Abstract
A 52-year-old male was referred for an acute anterior ST-segment elevation myocardial infarction (STEMI). Coronary angiography revealed an acute left anterior descending artery occlusion. The patient was treated with a drug-eluting stent (DES). Despite long and repeated high-pressure inflations (>20 atm) of non-compliant balloons, OPN NCⓇ high-pressure balloon (SIS Medical AG; Frauenfeld, Switzerland), rotational atherectomy, and cutting balloon, there was a severe hourglass stent underexpansion caused by coronary calcification. Thus, intravascular lithotripsy (IVL) (Shockwave Medical, Fremont, CA, USA) was attempted to re-dilate this calcified lesion. Underexpansion was successfully treated after delivering 70 shockwaves to the narrowest segment. IVL delivers localized pulsatile sonic pressure waves inducing circumferential calcium modification and multiple fractures. Our observation illustrates the additional value of coronary lithotripsy as a bail-out procedure to tackle severely calcified, de novo coronary lesions causing stent underexpansion in the context of STEMI, when all other available techniques failed.
<Learning objective: Severe coronary calcification may impair device delivery, stent apposition, and inhibit expansion, thus predisposing to stent thrombosis. Intravascular lithotripsy delivers localized pulsatile sonic pressure waves inducing circumferential calcium modification and multiple fractures. Our observation illustrates the additional value of coronary lithotripsy as a bail-out procedure to tackle severely calcified, de novo coronary lesions causing stent underexpansion in the context of ST-segment elevation myocardial infarction, when all other available techniques failed.>
Keywords: Acute myocardial infarction, Severe coronary calcification, Intravascular lithotripsy, Optical coherence tomography
Introduction
Severe coronary calcification may impair device delivery, stent apposition, and inhibit expansion, thus predisposing to stent thrombosis [1]. There are limited options once non-compliant balloons have failed to achieve optimal stent expansion. Intravascular lithotripsy (IVL) delivers localized pulsatile sonic pressure waves inducing circumferential calcium modification and multiple fractures [2]. IVL seems to be of major help to optimize results of underexpanded stents in heavily calcified vessels and appears to be common practice. Clinical trials evaluating IVL mostly included elective procedures [3]. Clinical experience using this technology is still limited in the context of ST-segment elevation myocardial infarction (STEMI) [4]. However, the context where it is used in the present case might differ here: an infarct-related artery. Our observation demonstrates the additional value of coronary lithotripsy as a bail-out procedure to tackle severely calcified, de novo coronary lesions causing stent underexpansion in the context of STEMI, when all other available techniques failed.
Case report
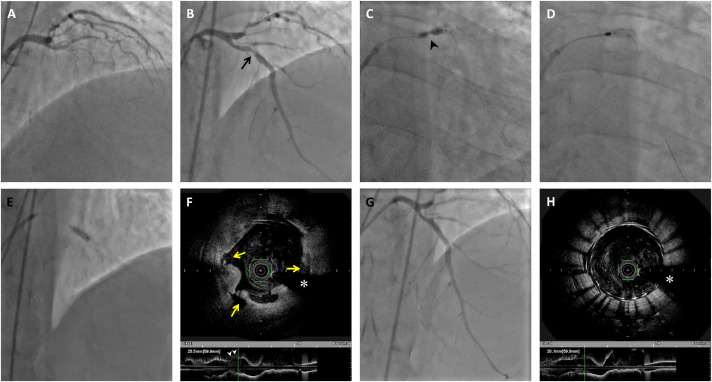
A 52-year-old male was referred to another department after presenting with anterior STEMI. Coronary angiography revealed an acute left anterior descending artery (LAD) occlusion (Fig. 1A) and 3-vessel disease including a chronic total occlusion of the right coronary artery. The LAD occlusion was crossed using a Sion blue wire (Asahi Intecc, Nagoya, Japan). Following pre-dilation of the proximal LAD with compliant balloons (2.0 × 20 mm and 2.5 × 20 mm Emerge balloons; Boston Scientific, Maple Grove, MN, USA), a 3.0 × 30 mm Orsiro (Biotronik, Buläch, Switzerland) drug-eluting stent (DES) was delivered to the LAD. Despite long and repeated high-pressure inflations (>20 atm) of non-compliant balloons, there was a severe hourglass stent underexpansion caused by coronary calcification (Fig. 1B). The next day, the same team attempted to optimize the angioplasty, using gradual sizes of non-compliant balloons, OPN NCⓇ high-pressure balloon (SIS Medical AG; Frauenfeld, Switzerland), rotational atherectomy, and cutting balloon (Fig. 1C and D, Movie 1). The coronary stenosis remained very tight and the patient's status quickly deteriorated with ventricular arrhythmia and pulmonary congestion. The oxygen-dependent patient was urgently transferred to our hospital for a bail-out strategy. At admission to our center, the medical treatment included dual antiplatelet therapy (aspirin 75 mg once daily and ticagrelor 90 mg twice daily) and curative anticoagulation (enoxaparin 0.5 mL/kg twice daily).
Fig. 1.
Angiographic and Corresponding Optical Coherence Tomography (OCT) Findings in the Left Anterior Descending (LAD) Coronary Artery. (A) Emergent coronary angiography demonstrating LAD thrombosis. (B) Severe stent underexpansion caused by calcified underlying lesion (black arrow). (C) Waist in the non-compliant balloon during high pressure inflation (black arrowhead). (D) Attempt of rotational atherectomy inside the stent using a 1.75 mm burr. The latter failed to progress through the stenosis (Online Movie #1). (E) Procedure using a 3.5 mm x 12 mm intravascular lithotripsy balloon. (F) OCT cross-sectional (top) and longitudinal (bottom) images acquired post-intravascular lithotripsy demonstrate both calcium (yellow arrows) and disorganized struts (white arrowheads). (G, H) Final result after another stent implantation (minimal stent area: 8.2 mm2, average reference lumen area: 9.4 mm2). White asterisk indicates a guidewire shadow . (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
An urgent heart team meeting with interventional cardiology and cardiac surgery was assembled and as a result of this meeting, it was decided to proceed with primary percutaneous coronary intervention (PCI) in the context of STEMI. Thus, IVL (Shockwave Medical, Fremont, CA, USA) was attempted to re-dilate this calcified lesion. Underexpansion was treated with a 3.5 mm x 12 mm IVL balloon inflated at 4 atm, achieving adequate balloon expansion after delivering 70 shockwaves to the narrowest segment (Fig. 1E). Once 7 cycles of 10 pulses had been delivered, the shockwave balloon was inflated up to 6 atm (nominal pressure) to increase balloon compliance and to assess symmetrical expansion, suggesting calcium modification. Optical coherence tomography (OCT) imaging was performed to confirm this hypothesis. OCT imaging demonstrated multiple calcium fractures and a partial stent dislocation (Fig. 1F). Thus, a new 3.5 mm × 12 mm DES (Xience Sierra, Abbott Vascular, Santa Clara, CA, USA) was deployed inside the previous DES with a good final result (Fig. 1G), as shown by the control OCT imaging (Fig. 1H). The patient was discharged at day 8 and is currently doing fine.
Discussion
PCI of severely calcified lesions is known to result in lower procedural success rates, higher complication rates, and worse long‐term clinical outcomes compared to noncalcified lesions [1]. Calcium modification through adequate pre-dilation is crucial in ensuring procedural success and reducing adverse cardiovascular outcomes. Our case report supports the notion that stents should not be implanted in a poorly dilated severely calcified lesion. Our observation demonstrates the additional value of IVL as a bail-out procedure to tackle severely calcified coronary lesions in the context of STEMI, when all other available techniques failed. The OPN NCⓇ balloon is an option to dilate lesions or underexpanded stents when other noncompliant balloons have failed. Safety seems reasonable, even at pressures as high as 40 atm [5]. Rotational atherectomy may be another alternative and has been described as an effective treatment for resistant stent underexpansion with acceptable outcomes [6]. However, concerns exist regarding safety, particularly in the context of STEMI. In the same way, clinical experience using IVL is still limited in the context of STEMI [4]. Thus, clinical trials evaluating IVL mostly included elective procedures [3,7]. In the present case, where PCI has failed, emergency coronary artery bypass grafting is recommended [8]. However, the patient's status was unstable. The heart team considered that this off-label attempt was the most appropriate strategy. The procedure was fast and efficient. Despite its apparent safety, the IVL device may need to be used in conjunction with various PCI tools including ancillary guide-catheter extenders, in order to facilitate pulsatile sonic pressure waves delivery. Furthermore, we cannot rule out damage to the stent struts, polymer, and drug caused by IVL. The impact of the IVL on stent backbone/polymer integrity and drug elution remains to be shown [2].
There is emerging evidence for intravascular imaging in guiding selection of calcium modification devices using parameters such as calcium distribution and depth that directly impact on procedural success and clinical outcomes. In the present case, OCT imaging was not performed before lithotripsy because the patient's clinical status was unstable and it was apparent that a heavily calcified lesion was responsible for stent underexpansion. Pre-PCI lesion assessment by OCT may help predict stent underexpansion and select cases who require aggressive lesion modification prior to stent implantation. Fujino et al. reported OCT thresholds for predicting calcium fracture in lesions treated with only balloon angioplasty at a maximum calcium angle of 225° and a minimum calcium thickness of 0.24 mm [9]. As previously observed [10], OCT imaging showed that large calcium fragments generated by IVL remained in situ. OCT imaging also demonstrated a partial stent dislocation, probably due to the high-speed impact of the burr with the metallic stent struts. As shown by the Online Movie #1, the 1.75 mm burr of the rotational atherectomy failed to progress through the stenosis. The progression of the burr seemed to halt inside the proximal part of the underexpanded stent. A low burr to artery ratio and/or the use of small burrs (1.25 and 1.50 mm) could have helped to prevent this. The rotational atherectomy burr is capable of ablating metallic stent struts; the abraded metallic particulate generated by stent ablation seems to be similar in size to particles generated by calcific plaque rotablation. Whether or not the rotational atherectomy should be used to pulverize every incompletely expanded stent is still a matter of debate [6]. OCT provides the interventional cardiologist with absence of struts inside the proximal part of the stent, based on which he decided to insert a new DES inside the previous stent. Stent fracture is well known to increase the risk of stent thrombosis. Malapposition of the stent struts as well as discontinuity and fractures in the implanted stents may modify the flow characteristics and affect local blood viscosity. We believe that OCT imaging should be systematically performed in such procedures [9,10]. OCT may also help to select adequate indication of IVL, particularly when circumferential modification of the calcified plaque is necessary. Finally, further studies are needed to investigate the benefits of IVL in the context of STEMI.
Movie #1: Attempt of rotational atherectomy inside the stent using a 1.75 mm burr. The latter failed to progress through the stenosis.
Declaration of Competing Interest
Dr Gerbaud has served as consultant for Terumo Corporation and Abbott Vascular.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jccase.2020.12.014.
Appendix. Supplementary materials
References
- 1.Fan LM, Tong D, Mintz GS, Mamas MA, Javed A. Breaking the deadlock of calcified coronary artery lesions: a contemporary review. Catheter Cardiovasc Interv. 2020 doi: 10.1002/ccd.29221. [DOI] [PubMed] [Google Scholar]
- 2.Forero MNT, Daemen J. The coronary intravascular lithotripsy system. Interv Cardiol. 2019;14:174–181. doi: 10.15420/icr.2019.18.R1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ali ZA, Nef H, Escaned J, Werner N, Banning AP, Hill JM, De Bruyne B, Montorfano M, Lefevre T, Stone GW, Crowley A, Matsumura M, Maehara A, Lansky AJ, Fajadet J. Safety and effectiveness of coronary intravascular lithotripsy for treatment of severely calcified coronary stenoses. Circ Cardiovasc Interv. 2019;12 doi: 10.1161/CIRCINTERVENTIONS.119.008434. [DOI] [PubMed] [Google Scholar]
- 4.Wong B, El-Jack S, Newcombe R, Glenie T, Armstrong G, Khan A. Shockwave intravascular lithotripsy of calcified coronary lesions in ST-elevation myocardial infarction: first-in-man experience. J Invasive Cardiol. 2019;31:E73–E75. [PubMed] [Google Scholar]
- 5.Díaz JF, Gómez-Menchero A, Cardenal R, Sánchez-González C, Sanghvi A. Extremely high-pressure dilation with a new noncompliant balloon. Tex Heart Inst J. 2012;39:635–638. [PMC free article] [PubMed] [Google Scholar]
- 6.Ferri LA, Jabbour RJ, Giannini F, Benincasa S, Ancona M, Regazzoli D, Mangieri A, Montorfano M, Colombo A, Latib A. Safety and efficacy of rotational atherectomy for the treatment of undilatable underexpanded stents implanted in calcific lesions. Catheter Cardiovasc Interv. 2017;90:E19–E24. doi: 10.1002/ccd.26836. [DOI] [PubMed] [Google Scholar]
- 7.Aksoy A, Salazar C, Becher MU, Tiyerili V, Weber M, Jansen F, Sedaghat A, Zimmer S, Leick J, Grube E, Gonzalo N, Sinning JM, Escaned J, Nickenig G, Werner N. Intravascular lithotripsy in calcified coronary lesions: a prospective, observational, multicenter registry. Circ Cardiovasc Interv. 2019;12 doi: 10.1161/CIRCINTERVENTIONS.119.008154. [DOI] [PubMed] [Google Scholar]
- 8.Ibanez B, James S, Agewall S, Antunes MJ, Bucciarelli-Ducci C, Bueno H, Caforio ALP, Crea F, Goudevenos JA, Halvorsen S, Hindricks G, Kastrati A, Lenzen MJ, Prescott E, Roffi M. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC) Eur Heart J. 2018;39:119–177. doi: 10.1093/eurheartj/ehx393. [DOI] [PubMed] [Google Scholar]
- 9.Fujino A, Mintz GS, Lee T, Hoshino M, Usui E, Kanaji Y, Murai T, Yonetsu T, Matsumura M, Ali ZA, Jeremias A, Moses JW, Shlofmitz RA, Kakuta T, Maehara A. Predictors of calcium fracture derived from balloon angioplasty and its effect on stent expansion assessed by optical coherence tomography. JACC Cardiovasc Interv. 2018;11:1015–1017. doi: 10.1016/j.jcin.2018.02.004. [DOI] [PubMed] [Google Scholar]
- 10.Ali ZA, Brinton TJ, Hill JM, Maehara A, Matsumura M, Karimi Galougahi K, Illindala U, Götberg M, Whitbourn R, Van Mieghem N, Meredith IT, Di Mario C, Fajadet J. Optical coherence tomography characterization of coronary lithoplasty for treatment of calcified lesions: first description. JACC Cardiovasc Imaging. 2017;10:897–906. doi: 10.1016/j.jcmg.2017.05.012. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.