Abstract
Objective: Hydronephrosis, which may be caused by kidney stones in the collecting system, may induce permanent flank pain and damage to kidney function. In this study, we aimed to examine whether the presence of hydronephrosis in the patient has an effect on the stone-free rates in flexible ureterorenoscopy (FURS) applications. Method: The study was carried out retrospectively with 164 patients. Stone size was calculated as volume in computed tomography. Preoperative patient demographic data, radiographic stone characteristics, operational findings, complication status and postoperative 1st month results were recorded. Result: The mean stone-free rate was found to be 61.5%. It was determined that age, gender, side, number, size and the Hounsfield Unit of the stone, the presence of preoperative extracorporeal shock wave lithotripsy (ESWL) history and the presence of hydronephrosis and its degree did not affect the stone-free rate. However, it was concluded that preoperative percutaneous nephrolithotomy (PNL) application and prolonged operation time were found to affect statistically significant stone-free rate. In addition, ‘2’ was found to be the cut-off value for hydronephrosis in the receiver operating characteristic analysis. Conclusion: The presence of preoperative hydronephrosis does not decrease the success of FURS. However, it can be expected that the success of FURS will decrease as grade 2 or more severe grade of hydronephrosis. Therefore, we think that other treatment modalities such as ESWL and PNL should be prioritized in patients with grade 2 and more severe grade of hydronephrosis.
Keywords: Flexible ureterorenoscopy, hydronephrosis grade, kidney stone, stone-free rate
Introduction
Urinary system stone disease is one of the most important diseases that affect human health and social life. Its incidence varies according to geographical regions. The lifetime risk of urinary tract stone disease is estimated to be between 5% and 12% [1]. There is not a single treatment method in the treatment of these stones, but there are several different approaches. Procedures such as extracorporeal shock wave lithotripsy (ESWL), semirigid ureteroscopy (URS), antegrade ureterolithotripsy, flexible ureterorenoscopy (FURS), percutaneous nephrolithotomy (PNL), laparoscopy and rarely open surgery are used in the treatment of these stones [2].
With the spread of minimally invasive techniques, controversy arose about the indications of these methods. Considering the most suitable treatment options according to the current guidelines on stone, PNL is recommended in the first place in kidney stones of 2 centimeters (cm) and above, while FURS and ESWL are recommended in the second place. For 1 cm and smaller kidney stones, the recommended treatment method is FURS and ESWL while PNL is the second. The recommended treatment method for 1 to 2 cm kidney stones is presented as FURS, ESWL or PNL depending on the characteristics of the patient and the stone [3].
Following the publication of the first FURS experiences identified by Fuchs in the early 1990s, flexible ureterorenoscopes have been further developed over the last 15 years, and have been used extensively with increasing success and decreasing complication rates. With the developing technology, the deflection ability has been increased and reached high mobility, more miniaturized, high optical quality with fiber optic lighting and relatively more durable flexible ureterorenoscopes are used in the treatment of kidney stones smaller than 2 cm. The biggest factor in the development of FURS is the use of holmium laser technology and nickel-titanium alloy baskets in endourology [4]. Thanks to these advances in technology, FURS indications can be extended to use in ESWL and PNL failure, obese patients and patients with musculoskeletal deformities [5].
During all kinds of ureterorenoscopy procedures, dilatation proximal of the stone procedures may cause the migration of the stone into the kidney due to the strong retrograde fluid pressure and the impulse power applied by the energy source to the stone. However, in these migration situations, it is possible to continue the operation uninterruptedly only with flexible ureterorenoscope. In a study of 208 patients, 55 of whom had proximal ureteral stones, the migration rate of the stone was reported as 3.3% [6]. It is obvious that dilation has a significant effect on this rate. Moreover, proximal ureter stones constitute a certain part of the stones in similar studies.
Hydronephrosis, which kidney stones can cause in the collecting system, may induce permanent flank pain and damage to kidney function [7]. As small-caliber flexible ureterorenoscopes and holmium lasers used in treatment become more common, results with less complications and higher success rates are obtained in FURS applications [8,9]. However, there are no studies in the literature that directly evaluate the effect of hydronephrosis in the kidney on FURS success. The novelty of this study is to evaluate the effect of kidney hydronephrosis on stone-free rate in patients undergoing FURS with the primary outcome and most importantly, to present a threshold value to the literature for hydronephrosis, which affects FURS success.
Materials and methods
Inclusion and exclusion criteria
This study was carried out retrospectively after the ethics committee approval of our hospital was obtained with the decision number 2020/12-8. Patients who underwent FURS due to kidney from January 2014 to March 2020. Patients who underwent FURS only for kidney stones, using computed tomography (CT) for diagnosis and not using a combined procedure were included in the study. Patients with kidney anomalies, under 18 years of age, primary ureteral stones or ureteral stones with kidney stones, preoperative double j stent (DJS) or nephrostomy tube for any reason were excluded from the study. After the exclusion criteria, a total of 164 patients were evaluated. Preoperative patient demographic data, radiographic stone characteristics, operational findings, complication status and stone-free states at the first postoperative month were recorded. The study was performed after obtaining written and verbal informed consent before the operation of all patients.
Volume calculation
The patients were preoperatively evaluated with non-contrast stone protocol (low radiation dose) abdominal CT. For kidney stones are in 3-dimensional configuration; in this study, we calculated the volume of the stones because of the concern that the longest measurement in one plane or the calculation of the surface area in the two planes can give false results for each parameter affecting success in kidney stone treatment modalities. While calculating the volume of the stones in CT, the longest measurements in axial, coronal and sagittal plane were used. Volume calculation was recorded as cm3 by multiplying the lengths of these 3 planes. In case of more than one stone, the total size was calculated by measuring the size of each stone separately and adding together.
Hydronephrosis classification
A rating similar to the Society of Fetal Urology system was used in the rating of hydronephrosis based on the appearance of the renal parenchyma and pelvicalyceal system on CT. According to this classification; grade 0 is normal. In grade 1 a slight enlargement of the renal pelvis; in grade 2 marked enlargement of the renal pelvis and calyx; in grade 3 advanced enlargement in pelvis and calices and in grade 4 decrease in renal parenchyma thickness with excessive enlargement in pelvis and calices is seen [10].
Postoperative stone-free status and complications
Postoperative stone-free status was assessed by KUB X-Ray on postoperative day 1 if the patient’s stone was opaque or postoperative CT scan at 1st month. The absence of stones or ≤4 mm stone fragments in imaging were considered stone-free/clinically insignificant fragments [3]. Postoperative complications were evaluated according to the modified Clavien classification (Table 1). According to this classification, grade 1-3 complications were considered minor complications and grade 4 and 5 complications were considered major complications [11].
Table 1.
Modified Clavien classification
| Grade | Definition |
|---|---|
| 1 | Any deviation from the normal postoperative course without the need for pharmacologic/surgical/radiological intervention |
| 2 | Requiring pharmacologic treatment with drugs other than such allowed for grade 1 complication |
| 3A | Complications needing surgical, endoscopic or radiologic intervention under local anesthesia |
| 3B | Complications needing surgical, endoscopic or radiologic intervention under general anesthesia |
| 4A | Life threatening conditions with single organ dysfunction |
| 4B | Life threatening conditions with multi organ dysfunction |
| 5 | Death |
Surgery
Cefuroxime axetil was administered intravenously to all patients in accordance with the principles of prophylaxis before starting the operation. After general anesthesia was applied to the patients, the procedure was started in the modified dorsal lithotomy position. Then, hydrophilic guide wire (Boston Scientific, 0.035 inch, 150 cm) was placed in the ureter to be processed under the guidance of C-arm fluoroscopy unit (Ziehm 8000, Ziehm Imaging GmbH. Nuremberg Germany). The diagnostic URS was made with insertion of the the Semirigid 9.5 Fr ureterorenoscope (Karl Storz, Tuttlingen, Germany) for there was no stone in the ureter, the ureteral access sheath (9.5-11.5 Fr or 12-14 Fr; 35 cm or 45 cm; hydrophilic; Cook Medical Bloomington, IN) was placed in the ureteropelvic junction under fluoroscopy guidance. Balloon dilator was not used in any patient. A flexible ureterorenoscope (Flex-X2, Karl Storz, Tuttlingen, Germany) with an external diameter of 7.5 Fr was inserted through the ureteral access sheath. Lithotripsy procedure was performed with a 272 or 365 μm holmium laser probe (Ho: YAG Laser; Quanta System lithotripsy fiber, Solbiate Olona, Italy). Isotonic sodium chloride was used as irrigation during the procedure. DJS (4,8 Fr; 24-26-28 cm Geotek Medical Co., Ltd., Ankara, Turkey) was placed in all patients after the procedure. As the operation period; the time elapsed between the introduction of the semirigid ureterorenoscope from the urethra and the insertion of DJS. At the postoperative 1st month, DJSs were taken under local anesthesia.
Statistical analysis
Firstly, descriptive statistics (arithmetic mean, standard deviation, standard error, etc.) of the data obtained from the study were calculated. Pearson chi-square test was used to investigate the relationship between categorical variables such as ‘gender, presence of preoperative PNL, presence of preoperative ESWL, side of the stone, presence of hydronephrosis, grade of hydronephrosis, presence of postoperative complications and the presence of additional interference to complications’. The suitability of the data to normal distribution was investigated with the Shapiro-Wilk test. The data were found to be suitable for normal distribution (P>0.05). Independent sample t test was used for comparisons between two groups for the ‘age’ variable. Mann-Whitney Test was used for ‘number of stone, Hounsfield Unit (HU) of stone, grade of hydronephrosis, volume of stone and operation time variables’. The cut-off value in hydronephrosis degree was determined by receiver operating characteristic (ROC) analysis. P value less than 0.05 was considered statistically significant. SPSS 25.0 (IBM Corp., Armonk, NY, USA) package program was used for statistical analysis of the data.
Results
Preoperative data
One hundred ninety three patients were examined for our study. The study was performed with a total of 164 patients after the exclusion criteria. 103 (62.8%) of the patients were male; 61 (37.1%) were women. The mean age of patients included in the study was 45.43±13.98 years. In the preoperative period, 84 patients (51.2%) had ESWL and 18 patients (10.9%) had PNL. 77 (46.9%) of the operated kidneys were on the right side and 97 (53%) were on the left side. The stone was in the lower calix in 41 (25%); in the middle calyx in 8 (5.4%); in the renal pelvis in 80 (48.7%); in the upper calyx in 8 (5.4%) of the patients. In 27 (16.4%) patients stones were located in multiple locations. The number of stones operated ranged from 1 to 4. There were one stone in 134 (81.7%); two stones in 26 (15.8%); three stones in 1 (0.06%) and four stones in 3 (0.1%) patients. The average HU of the stones was 1.063.7±354.65. The stone volumes of the patients in our study ranged from 0.24 cm3 to 21.6 cm3. The mean operation time was 56.93±19.44 min. The mean length of hospital stay was found to be 2.11±0.40 days. None of the patients required postoperative intensive care. The median American Society of Anesthesiologists score was calculated as 2.
The average stone-free rate was found to be 61.5%. Additional interventions were applied to 12 of the patients in the group in which stone-free status could not be achieved. As a secondary procedure, FURS, PNL and ESWL was applied to 2, 6 and 4 patients, respectively. Other patients were followed up at their own request.
PNL history and operation time affect FURS success
In Table 2, preoperative patient demographic data, radiographic stone characteristics and operational findings affecting stone-free status are shown. It was determined that age, gender, side, number, size and the Hounsfield Unit of the stone, the presence of preoperative ESWL history and the presence hydronephrosis and its degree did not affect the stone-free rate. However, it was concluded that preoperative PNL application and operation time were found to affect statistically significant stone-free rate. With these results, it was concluded that operationally secondary FURS application and prolonged operation time were successfully negative correlations.
Table 2.
Factors affecting stone-free status
| Stone Free Status | p value | ||
|---|---|---|---|
|
| |||
| Yes (n = 101) | No (n = 63) | ||
| Age (mean ± sd) | 44.49±14.05 | 46.95±13.82 | 0.275¥ |
| Gender (%) | 0.634* | ||
| Male | 62 (37.8) | 41 (25) | |
| Female | 39 (23.7) | 22 (13.4) | |
| Presence of preoperative PNL (%) | 7 (4.2) | 11 (6.7) | 0.033* |
| Presence of preoperative ESWL (%) | 49 (29.8) | 35 (21.3) | 0.415* |
| Side of the Stone (%) | 0.407* | ||
| Right | 50 (30.4) | 27 (16.4) | |
| Left | 51 (31) | 36 (21.9) | |
| Number of Stone | 0.055§ | ||
| min/max | 1/3 | 1/4 | |
| mean | 1.14±0.3 | 1.34±0.9 | |
| HU of Stone | 0.310§ | ||
| min/max | 250/1700 | 400/1650 | |
| mean | 1039.6±35.6 | 1101.2±37.3 | |
| Presence of hydronephrosis (%) | 58 (35.3) | 42 (25.6) | 0.238* |
| Grade of Hydronephrosis | 0.803§ | ||
| min/max | 1/4 | 1/4 | |
| mean | 1.79±0.11 | 1.71±0.11 | |
| Grade of Hydronephrosis | 0.48* | ||
| 1 | 28 | 19 | |
| 2 | 16 | 17 | |
| 3 | 12 | 5 | |
| 4 | 2 | 1 | |
| Volume of stone (cm3) | 0.211§ | ||
| min/max | 0.24/8.64 | 0.45/21.6 | |
| mean | 2.23±0.17 | 2.79±0.38 | |
| Operation time (min) | 0.018§ | ||
| min/max | 30/145 | 30/125 | |
| mean | 53.89±1.91 | 61.9±2.84 | |
(sd: standard deviation, PNL: percutaneous nephrolithotomy, ESWL: extracorporeal shock wave lithotripsy, min/max: minimum/maximum, HU: Hounsfield Unit, cm3: cubic centimeter, min: minute)
Independent Samples Test;
Chi-Square Tests;
Mann-Whitney Test.
FURS success decreases with hydronephrosis grade 2 and above
In the ROC analysis (Figure 1), ‘2’ was found as the cut-off value in the degree of hydronephrosis. Although the degree of hydronephrosis does not have a significant effect on stone-free rate, it is concluded that the stone-free rate decreases as the grade 2, 3 and 4 according to the results of the analysis. The stone free rate is 28% for hydronephrosis grade 1, 16% for grade 2; 12% for grade 3 and 2% for grade 4. In other words, it can be predicted that success in FURS operations to be performed in patients with hydronephrosis degree 2 and above will decrease. When the cross table is examined (Table 3), the values after grade 2 show the difference (AUC = 0.514; SE = 0.059; 95% CI = 0.411-0.615).
Figure 1.
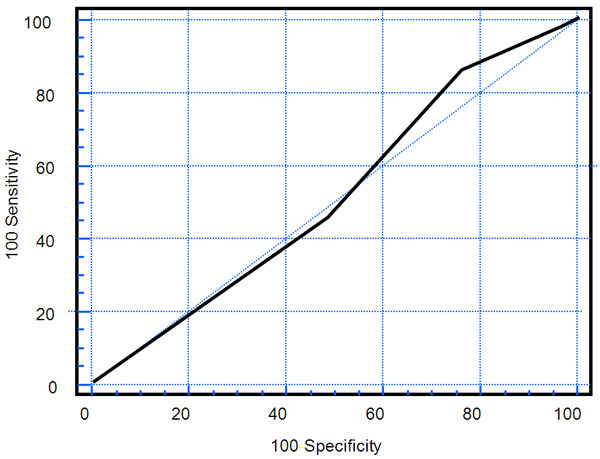
The ROC curve of the cut-off threshold value in hydronephrosis (ROC: receiver operating characteristic).
Table 3.
Cross table indicating the cut-off threshold value in hydronephrosis degree
| Criterion | Sensitivity (95% C.I.) | Specificity (95% CI) |
|---|---|---|
| <1 | 0.0 (0.0-0.0) | 100.0 (100.0-100.0) |
| ≤1 | 45.2 (29.9-61.3) | 51.7 (38.2-65.0) |
| ≤2* | 85.7 (71.4-94.5) | 24.1 (13.9-37.2) |
| ≤3 | 97.6 (87.4-99.6) | 3.4 (0.5-11.9) |
| ≤4 | 100.0 (100.0-100.0) | 0.0 (0.0-0.0) |
Cut-off value;
CI: Confidence interval.
Complications do not affect stone-free status
There was no peroperative complication in any of these patients. A total of 11 patients had minor postoperative complications and 4 of these patients underwent additional intervention (Table 4). Seven of the complications were febrile urinary tract infection which were followed up with parenteral antibiotic treatment without intervention (Clavien 2), 3 of them were renal colic due to obstructive ureteral stones and 1 of them were ascending migration of the DJS placed peroperatively. It was concluded that complications affected stone-free state insignificant. The treatment was completed with surgical intervention in 4 patients which URS (Clavien 3B) in 1 patient, DJS insertion under local anesthesia in 2 patients (Clavien 3A) and withdrawal of DJS (Clavien 3A) in 1 patient.
Table 4.
Postoperative complications
| Stone-Free Status | p value | ||
|---|---|---|---|
|
| |||
| Yes (n = 101) | No (n = 63) | ||
| Presence of Postoperative Complications (%) | 6 (3.7) | 5 (3) | 0.619* |
| The Presence of Additional Interference to Complications (%) | 1 (0.6) | 3 (1.8) | 0.159* |
Chi-Square Tests.
Discussion
The main goal in the treatment of kidney stones is to provide stone-free state by giving the least harm to the patient. Stone fragments remaining in the kidney after treatment constitute a source for the formation of new stones. These stones can also be symptomatic again and cause infection. During the times when open stone surgeries were widespread, there was no disagreement over the definition of surgical success due to complete stone-free treatment. However, today, when minimally invasive techniques develop, some differences of opinion stand out in the definition of success [12-14]. On the other hand, we accept ≤4 mm stones as clinically insignificant fragments and describe the patients who have ≤4 mm stones or who are stone-free postoperatively as successful.
Flexible ureterorenoscopy operations alone have been shown to be much more cost-effective as they do not require additional procedures compared to combined endoscopic approaches [15]. In one study, the early postoperative stone-free rate of the single-session FURS procedure applied to stones in all localizations was determined to be 69.7% [16]. One of the strengths of our study is that stone-free rate was achieved in the early period in accordance with the literature at a rate of 61.5% without using a combined procedure.
According to the study by Lim et al. FURS indications are divided into two categories as primary and secondary. The group in secondary FURS consists of patients with previous failed ESWL and PNL. According to the results of the study, there was a statistically significant difference between the stone-free rates in the group of patients who underwent secondary FURS and in which primary FURS was performed, in favor of the patient group in whom primary FURS was applied [16]. Similarly, in our study, it was shown that preoperative unsuccessful PNL had a statistically significant negative effect on success in secondary FURS which was an ineffective treatment method in this patient group. On the other hand, it was shown that preoperative unsuccessful ESWL did not affect stone-free rates in secondary FURS which was an effective treatment method in these patients.
According to the study of Kıraç et al. the mean operation time in patients undergoing FURS was 66.4±15.8 minutes [17]. According to our findings, the mean operation time in the group in which stone-free could not be achieved was 61 minutes, and in the group where stone-free was achieved, it was 53 minutes. According to our results, the average operation times of both groups were found to be shorter compared to the literature data, and this situation became statistically significant. With the prolonged operation time, the reduction of stone-free rate can be explained by lack of experience, increased complication rate in prolonged surgeries, decreased maneuverability of the flexible ureterorenoscope due to difficult localization of stones such as lower calyx, more fatigue of the surgeons and the development of the surgeon’s attention deficit.
Placing preoperative DJS for passive dilation is a matter of debate in FURS operations. With this application, it can be facilitated in the application of ureteral access sheath used peroperatively. At the same time, the possibility of working in a dilated lumen, not delaying the operation and reducing the risk of developing ureteral strictures in the long term may be considered. However, in one study, it was reported that performing FURS without preoperative DJS insertion will not cause ureteral stricture even with a wide ureteral access sheath [18]. All our operations were carried out by using a ureteral access sheath. In addition, none of the patients had preoperative DJS. However, similar to the literature, no ureteral stricture was observed in any of our patients in the long term follow-up.
As a result of the developments in technology reflected on endoscopy, FURS complications decreased significantly. In our study, Ho:YAG laser was used as an energy source in all patients and Ho:YAG laser is considered to be safe and effective with very low complication rates in intracorporeal lithotripsy [19]. Similarly, in our study, no significant complication related to either laser use or other has occured peroperatively. When the postoperative complications are analyzed, the general complication rate is between 9-25% according to the European Urology Guidelines in patients undergoing FURS [6]. In a meta-analysis, a total of 10 studies were evaluated and the postoperative general complication rate in patients undergoing FURS was stated to be 10.4% [20]. In our study, the postoperative general complication rate was 6.7%. This rate is very low compared to the literature data and no major complication was observed in our cases.
The strengths of our study are that only patients with kidney stones are included in the study, all patients are evaluated by CT as the gold standard diagnostic method for the diagnosis of kidney stones, considering the 3D structure of the stones in space, its size was calculated as volume, no combined procedure was performed in any patient, in the literature there is no study evaluating the direct effect of hydronephrosis on FURS operation success and there is no threshold value for hydronephrosis especially in cases where FURS will be performed. On the other hand, the limitations of our study are that the study is retrospective; in the measurement of stone volume, since the configuration of each stone is different from each other, no standard volume calculation can be made (there is no software program that can calculate volume), the operations were performed by several surgeons with different experience.
Among the minimally invasive endourological techniques, FURS is increasingly used in the treatment of kidney stones. According to our findings, the presence of hydronephrosis does not decrease the success of this operation. However, it can be expected that the success of FURS will decrease as hydronephrosis grade 2, 3 and 4. Therefore, we think that other treatment modalities such as ESWL and PNL should be prioritized in patients with grade 2, 3 and 4 hydronephrosis. We believe that our results will be supported by other studies and will be a new milestone in stone surgery and will shed light on the guidelines.
Disclosure of conflict of interest
None.
References
- 1.Khan SR, Pearle MS, Robertson WG, Gambaro G, Canales BK, Doizi S, Traxer O, Tiselius HG. Kidney stones. Nat Rev Dis Primers. 2016;25:16008. doi: 10.1038/nrdp.2016.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Legemate JD, Wijnstok NJ, Matsuda T, Strijbos W, Erdogru T, Roth B, Kinoshita H, Palacios-Ramos J, Scarpa RM, de la Rosette JJ. Characteristics and outcomes of ureteroscopic treatment in 2650 patients with impacted ureteral stones. World J Urol. 2017;35:1497–1506. doi: 10.1007/s00345-017-2028-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Türk C, Neisius A, Petrik A, Seitz C, Skolarikos A, Knoll T. EAU guidelines on ınterventional treatment for urolithiasis. Eur Urol. 2016;69:475–82. doi: 10.1016/j.eururo.2015.07.041. [DOI] [PubMed] [Google Scholar]
- 4.Fuchs GJ, Fuchs AM. Flexible endoscopy of the upper urinary tract. A new minimally invasive method for diagnosis and treatment. Urologe A. 1990;29:313–320. [PubMed] [Google Scholar]
- 5.Süer E, Gülpinar Ö, Özcan C, Göğüş Ç, Kerimov S, Şafak M. Predictive factors for flexible ureterorenoscopy requirement after rigid ureterorenoscopy in cases with renal pelvic stones sized 1 to 2 cm. Korean J Urol. 2015;56:138–143. doi: 10.4111/kju.2015.56.2.138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chen S, Zhou L, Wei T, Luo D, Jin T, Li H, Wang K. Comparison of holmium: YAG laser and pneumatic lithotripsy in the treatment of ureteral stones: an update meta-analysis. Urol Int. 2017;98:125–133. doi: 10.1159/000448692. [DOI] [PubMed] [Google Scholar]
- 7.Kreshover JE, Dickstein RJ, Rowe C, Babayan RK, Wang DS. Predictors for negative ureteroscopy in the management of upper urinary tract stone disease. Urology. 2011;78:748–752. doi: 10.1016/j.urology.2011.03.008. [DOI] [PubMed] [Google Scholar]
- 8.Bhojani N, Mandeville JA, Hameed TA, Soergel TM, McAteer JA, Williams JC Jr, Krambeck AE, Lingeman JE. Lithotripter outcomes in a community practice setting: comparison of an electromagnetic and an electrohydraulic lithotripter. J Urol. 2015;193:875–879. doi: 10.1016/j.juro.2014.09.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sfoungaristos S, Gofrit ON, Katafigiotis I, Pode D, Landau EH, Yutkin V, Constantinides CA, Duvdevani M. Comparing the efficacy and safety of 365- and 550-μm laser fibers in semirigid ureteroscopic Ho:YAG lithotripsy. Int Urol Nephrol. 2015;47:1947–1952. doi: 10.1007/s11255-015-1130-x. [DOI] [PubMed] [Google Scholar]
- 10.Odibo AO, Raab E, Elovitz M, Merrill JD, Macones GA. Prenatal mild pyelectasis: evaluating the thresholds of renal pelvic diameter associated with normal postnatal renal function. J Ultrasound Med. 2004;23:513–517. doi: 10.7863/jum.2004.23.4.513. [DOI] [PubMed] [Google Scholar]
- 11.Akin Y, Erdoğru T. Standards for reporting complications in endourology. Endourol Bull. 2013;6:86–89. [Google Scholar]
- 12.Fine JK, Pak CY, Preminger GM. Effect of medical management and residual fragments on recurrentstone formation following shock wave lithotripsy. J Urol. 1995;153:27–32. doi: 10.1097/00005392-199501000-00010. discussion 32-33. [DOI] [PubMed] [Google Scholar]
- 13.Osman MM, Alfano Y, Kamp S, Haecker A, Alken P, Michel MS, Knoll T. 5 year follow up of patients with clinically insignificant residual fragments after extracorporeal shockwave lithotripsy. Eur Urol. 2005;47:860–864. doi: 10.1016/j.eururo.2005.01.005. [DOI] [PubMed] [Google Scholar]
- 14.Patodia M, Sinha RJ, Singh S, Singh V. Management of renal caliceal diverticular stones: a decade of experience. Urol Ann. 2017;9:145–149. doi: 10.4103/UA.UA_95_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Goldberg H, Holland R, Tal R, Lask DM, Livne PM, Lifshitz DA. The İmpact of retrograde intrarenal surgery for asymptomatic renal stones in patients undergoing ureteroscopy for a symptomatic ureteral stone. J Endourol. 2013;27:970–973. doi: 10.1089/end.2013.0055. [DOI] [PubMed] [Google Scholar]
- 16.Lim SH, Jeong BC, Seo SI, Jeon SS, Han DH. Treatment outcomes of retrograde intrarenal surgery for renal stones and predictive factors of stone-free. Korean J Urol. 2010;51:777–782. doi: 10.4111/kju.2010.51.11.777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kirac M, Bozkurt ÖF, Tunc L, Guneri C, Unsal A, Biri H. Comparison of retrograde intrarenal surgery and minipercutaneous nephrolithotomy in management of lower-pole renal Stones with a diameter of smaller than 15 mm. Urolithiasis. 2013;41:241–246. doi: 10.1007/s00240-013-0552-0. [DOI] [PubMed] [Google Scholar]
- 18.Shvero A, Herzberg H, Zilberman D, Mor Y, Winkler H, Kleinmann N. Is it safe to use a ureteral access sheath in an unstented ureter? BMC Urol. 2019;19:80–86. doi: 10.1186/s12894-019-0509-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jiang H, Wu Z, Ding Q. Ureteroscopy and holmium: YAG laser lithotripsy as emergency treatment for acute renal failure caused by impacted ureteral calculi. Urology. 2008;72:504–507. doi: 10.1016/j.urology.2008.05.041. [DOI] [PubMed] [Google Scholar]
- 20.De S, Autorino R, Kim FJ, Zargar H, Laydner H, Balsamo R, Torricelli FC, Palma CD, Molina WR, Monga M, Sio MD. Percutaneous nephrolithotomy versus retrograde intrarenal surgery: a systematic review and meta-analysis. Eur Urol. 2015;67:125–137. doi: 10.1016/j.eururo.2014.07.003. [DOI] [PubMed] [Google Scholar]


