Abstract
Background:
Because transthyretin amyloid cardiomyopathy (ATTR-CM) poses unique diagnostic and therapeutic challenges, referral of patients with known or suspected disease to specialized amyloidosis centers is recommended. These centers have developed strategic practices to provide multidisciplinary comprehensive care, but their best practices have not yet been well studied as a group.
Methods:
A qualitative survey was conducted by telephone/email from October 2019 to February 2020 among eligible healthcare providers with experience in the management of ATTR-CM at US amyloidosis centers, patients with ATTR-CM treated at amyloidosis centers, and patient advocates from amyloidosis patient support groups.
Results:
Fifteen cardiologists and 9 nurse practitioners/nurses from 15 selected amyloidosis centers participated in the survey, with 16 patients and 4 patient advocates. Among participating healthcare providers, the most frequently cited center best practices were diagnostic capability, multidisciplinary care, and time spent on patient care; the greatest challenges involved coordination of patient care. Patients described the “ideal” amyloidosis program as one that provides physicians with expertise in ATTR-CM, sufficient time with patients, comprehensive patient care, and opportunities to participate in research/clinical trials. The majority of centers host patient support group meetings, and patient advocacy groups provide support for centers with physician/patient education and research.
Conclusions:
Amyloidosis centers offer comprehensive care based on staff expertise in ATTR-CM, a multidisciplinary approach, advanced diagnostics, and time dedicated to patient care and education. Raising awareness of amyloidosis centers’ best practices among healthcare providers can reinforce the benefits of early referral and comprehensive care for patients with ATTR-CM.
Keywords: Amyloid, transthyretin, cardiomyopathy, heart failure, diagnosis, treatment, rare disease
Introduction
Transthyretin amyloid cardiomyopathy (ATTR-CM) is a rare, progressive, fatal condition that is an under-recognized cause of heart failure (HF).1 Patients with amyloidosis and cardiac involvement are often misdiagnosed and/or diagnosed at a late stage in the disease course due to lack of disease awareness or insufficient screening.2 Because advances in ATTR-CM treatment have improved patient outcomes, early and accurate diagnosis of the disease has become a critical goal.1,2
Over the past several decades, a growing number of centers of excellence (CoE) have been established in which highly skilled healthcare providers work collaboratively to enhance the care and treatment of specific medical conditions.3,4 In the United States (US), these dedicated, specialized clinical centers have come to play an important role in the management of complex, serious diseases, particularly those that are under-diagnosed and/or not optimally treated,5-7 providing multidisciplinary and comprehensive care and applying innovative techniques and technologies that are often beyond the reach of healthcare services available in the community setting.3,4 The unique diagnostic and therapeutic challenges associated with ATTR-CM often prompt healthcare providers in the community to refer patients with suspected or diagnosed ATTR-CM to highly specialized amyloidosis centers for care.8 These centers are typically part of large academic medical institutions, offering a faculty of physicians across multiple specialties, with extensive experience in ATTR-CM and a strategic, coordinated, comprehensive approach to disease management based on current research and state-of-the-art diagnostic technology and treatment.
Although numerous specialized amyloidosis centers have emerged over the past decade across the US, they have not yet been well studied as a group. We conducted a survey to gain insight into the best practices and unique characteristics of US amyloidosis centers. When shared with community healthcare providers who see patients with HF, the survey findings can be used to raise awareness and provide guidance on the benefits of early ATTR-CM diagnosis, comprehensive patient care, improved disease management, and appropriate/prompt patient referral. In addition, the survey captures patients’ perspectives on their journey to seek treatment in amyloidosis centers, including factors that influence their selection of centers and barriers to center access. Finally, by also interviewing representatives from amyloidosis patient advocacy organizations, we aimed to acquire information about their role in providing support for patients with ATTR-CM and amyloidosis centers.
Methods
A qualitative telephone survey (Bench Wing, Greenwich, CT, USA) was conducted between October 2019 and February 2020 among eligible healthcare providers, including cardiologists, nurse practitioners, and nurses, in practice at any of 15 selected multidisciplinary amyloidosis centers across the US. The centers were chosen based on information derived from online research, based on selection criteria such as years of experience; numbers of patients, specialists, and publications; quality of the associated HF program; clinical trial/registry involvement; and national/professional rankings and designations (Supplemental Table S1).
With the assistance of Amyloidosis Support Groups (ASG) (https://www.amyloidosissupport.org/), patients were also identified and recruited to participate in the telephone survey. Adults diagnosed with ATTR-CM and treated by a cardiologist at an amyloidosis center were eligible for the survey. Based on self-reported information, they must have received at least 1 of the following pre-specified transthyretin amyloidosis medications in a clinical trial or as prescribed by their cardiologist: AG10, curcumin, diflunisal, doxycycline, doxycycline plus tauroursodeoxycholic acid, green tea extract, GSK2315698, GSK2398852, inotersen, patisiran, PRX004, tafamidis, and tolcapone.
During initial interviews, participating healthcare providers suggested that patient advocates from support groups for patients with amyloidosis would also be a valuable source of information for this research. The interview process was therefore expanded to include a representative from each of the following US-based patient organizations: the Amyloidosis Foundation (https://amyloidosis.org); the Amyloidosis Research Consortium (https://arci.org); ASG; and Mackenzie’s Mission (https://mm713.org).
Questions included in the interview guides (Supplemental Table S2) were developed in consultation with 4 experts in ATTR-CM (2 cardiologists, 1 nurse, and 1 patient advocate), who also participated in the survey after the interview guide was finalized. The inquiries developed for the healthcare professional and patient interviews, which helped to systematically organize the data into a structured format, were focused on 8 central topics: (1) characteristics of the amyloidosis centers, patients, and patients’ journey; (2) collaboration, coordination, and outreach between amyloidosis centers and community physicians; (3) best practices and ideal features of the amyloidosis centers; (4) diagnostic approaches followed at amyloidosis centers (including internal or external practices used to identify undiagnosed patients with ATTR-CM); (5) amyloidosis center approaches to multidisciplinary care; (6) barriers to patient access to amyloidosis centers; (7) the role of clinical research and registries; and (8) collaboration between amyloidosis centers and patient support organizations. Interview questions for patient advocates were primarily focused on identifying the amyloidosis center characteristics that their organizations considered most important when recommending or partnering with a center, and the types of support that their organizations generally provide for patients and amyloidosis centers.
As summarized in Supplemental Table S1, the survey was conducted and presented according to the consolidated criteria for reporting qualitative research (COREQ).9
Results
From the 15 selected amyloidosis centers, 15 cardiologists, 5 nurse practitioners, 4 registered nurses, and 16 patients participated in the telephone survey. One of the 15 cardiologists did not complete the interview by telephone but provided responses to several survey questions via email, which are included in this report. Participant responses to inquiries related to the central topics during the interview sessions are described in the following sections and summarized in Table 1.
Table 1.
Summary of main survey findings on best practices and characteristics of specialized amyloidosis centers.
| Topic | Findings |
|---|---|
| Characteristics of the amyloidosis centers, patients, and patients’ journey | Most amyloidosis centers (74%) had been established for ⩾5 y |
| Cardiologists at all centers reported an increased number of patients with ATTR-CM in the past year, which most (73%) attributed to increased disease awareness among community physicians | |
| The centers had more patients with ATTR-CM versus AL amyloidosis (71% vs 29%) and wild-type ATTR-CM versus variant ATTR-CM (73% vs 27%) | |
| Most patients who participated in the survey found their amyloidosis center via clinician referral (44%) or their own research/network (44%) | |
| Most patients (81%) who participated in the survey had received care at ⩾2 amyloidosis centers | |
| The most common reasons for changing centers were location (38%) and dissatisfaction with care (23%) | |
| Collaboration, coordination, and outreach between amyloidosis centers and community physicians | Most patients (74%) treated at the amyloidosis centers were from local or regional areas |
| After referral, 21% of cardiologists at the centers reported sole management of patients (primarily at the request of the community physician) | |
| Educational initiatives were used at most amyloidosis centers (62%) to increase awareness of their expertise | |
| Best practices and ideal features of the amyloidosis centers | Cardiologists most often cited diagnostic capabilities and staff expertise as the best practice of their amyloidosis center (47%), followed by multidisciplinary care and time spent with patients (33% each) |
| Patients most often cited physicians’ expertise as an ideal feature of amyloidosis centers (63%) followed by time spent with patients (38%) | |
| Diagnostic approaches followed at amyloidosis centers | All of the surveyed cardiologists routinely confirmed diagnoses of ATTR-CM with additional testing |
| All of these specialists also ruled out AL amyloidosis: 80% before ordering PYP imaging, 13% at the same time as PYP imaging, and 7% after PYP imaging | |
| At nearly all (93%) of the amyloidosis centers, screening for potential “hot spots” for undiagnosed patients with ATTR-CM was conducted | |
| Amyloidosis center approaches to multidisciplinary care | Most amyloidosis centers (73%) required patients to visit different specialists in different offices within a hospital |
| The majority of amyloidosis centers (64%) held multidisciplinary meetings to discuss patients at least once monthly | |
| Staff at the amyloidosis centers often included multiple specialists, advanced practice clinicians, pharmacists, genetic counselors, and patient and/or research coordinators | |
| Barriers to patient access to amyloidosis centers | The most common challenge for patients was traveling to amyloidosis centers |
| Travel was particularly difficult for patients with neuropathy, and those who required a caregiver to drive them | |
| Approximately 38% of patients had a one-way travel time ⩾3 h | |
| A total of 44% of patients drove to their amyloidosis center with someone | |
| Role of clinical research and registries | All amyloidosis centers participated in clinical trials and had institutional registries; half participated in national/international registries |
| Most patients surveyed were aware of (94%) and had participated in (75%) clinical trials or registries | |
| Collaboration between amyloidosis centers and patient support organizations | Advocacy groups supported amyloidosis centers by providing physician and patient education, sponsoring patient support groups, and providing information about clinical trials |
| When selecting the amyloidosis centers listed on their websites, most advocacy groups considered the program’s multidisciplinary team, number of patients treated, years in existence, and types of amyloidosis treated | |
| Most amyloidosis centers (75%) hosted patient support meetings |
AL, light-chain amyloidosis; ATTR-CM, transthyretin amyloid cardiomyopathy; PYP, 99mtechnetium-pyrophosphate.
Characteristics of the amyloid centers, patients, and patients’ journey
According to participating cardiologists, the majority of their amyloidosis centers had been in operation for at least 5 years: 27% (4/15) had been open for 2 to 4 years; 47% (7/15) for 5 to 10 years; and 27% (4/15) for more than 10 years. All 15 of these centers were associated with an academic institution. The number of patients managed at these centers varied widely, from 50 to 1000 a year. A greater proportion of these patients had been diagnosed with ATTR-CM than with light-chain (AL) amyloidosis (71% vs 29%), and a greater proportion had wild-type ATTR-CM than variant (hereditary) ATTR-CM (73% vs 27%).
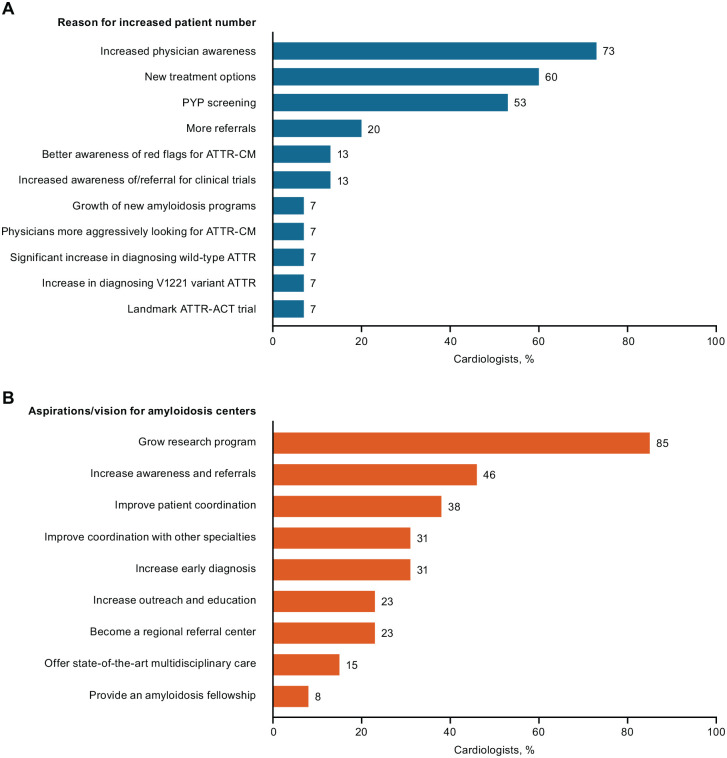
All of the cardiologists reported an increased number of new patients (particularly those with ATTR-CM) at their centers over the past year. The most commonly cited reasons for this increase were greater physician awareness of the disease, new treatment options, and more frequent screening via radionuclide scanning with 99mtechnetium-pyrophosphate (PYP) (Figure 1A).
Figure 1.
(A) Cardiologists’ reasons for the increase in number of patients seeking care at their amyloidosis center over previous year and (B) cardiologists’ aspirations/vision for their amyloidosis center in the future.
ATTR-ACT, Tafamidis in Transthyretin Cardiomyopathy Clinical Trial; ATTR-CM, transthyretin amyloid cardiomyopathy.
When asked about their future aspirations and vision for their amyloidosis centers, cardiologists frequently wished to grow their research program and increase disease awareness/patient referrals (Figure 1B). The participating nurses/nurse practitioners shared very similar aspirations, emphasizing their desire to improve education, research, and patient diagnosis and care, extend community outreach, and enhance relationships and coordination with local healthcare providers.
Patients participating in this survey had a mean age of 69 years (range, 45-81 years); 31% and 69% had received a diagnosis of wild-type and variant ATTR-CM, respectively. When asked to choose the greatest difficulty associated with their disease, 63% of patients cited lack of stamina and difficulty walking, which limit their ability to take part in daily activities; 44%, its effects on emotional well-being, finances, career, and family; and 44%, symptoms of fluid overload, shortness of breath, gastrointestinal disturbances, and polyneuropathy.
Patients with wild-type and variant phenotypes had spent an average of 2.0 and 3.4 years, respectively, at their current amyloidosis center; they reported receiving treatment at 11 different centers. Many of the patients interviewed found their amyloidosis center by means of physician referral (44%), or by their own research (25%) or network (19%), such as attending a conference or support group meeting. The factors that most often influenced their selection of amyloidosis center were physician expertise, research involvement, and a multidisciplinary team approach. Fifty percent of the patients participating in the survey received care and treatment at 3 amyloidosis centers, 31% at 2 centers, and 19% at 1 center. Patients who had received care at more than 1 center had most often switched centers due to location (38%), dissatisfaction with care (23%), consultation (15%), the need for a transplant (15%), or participation in a clinical trial (8%).
Collaboration, coordination, and outreach between amyloidosis centers and community physicians
Based on information provided by participating cardiologists, the patients with ATTR-CM treated at most of the amyloidosis centers were from local (41%) or regional (33%) areas. Patients rarely (1%) traveled internationally to receive care at an amyloidosis center, but a substantial proportion of patients (15%) traveled within the US for this purpose.
Most cardiologists (79%) at amyloidosis centers opted to continue their collaboration and coordination with community physicians during the course of patients’ care. This decision appeared to be influenced by factors such as patient location, preference, and disease severity. When these specialists provided exclusive management of patients at amyloidosis centers, the decision was based primarily on the preferences of the community physicians, due to their discomfort managing the complex disease or time constraints.
To raise awareness of their expertise, most amyloidosis centers (62%) relied on educational initiatives. However, other tools were also commonly used for this purpose, including websites (23%) and patient support groups (23%).
Best practices and ideal features of the amyloidosis centers
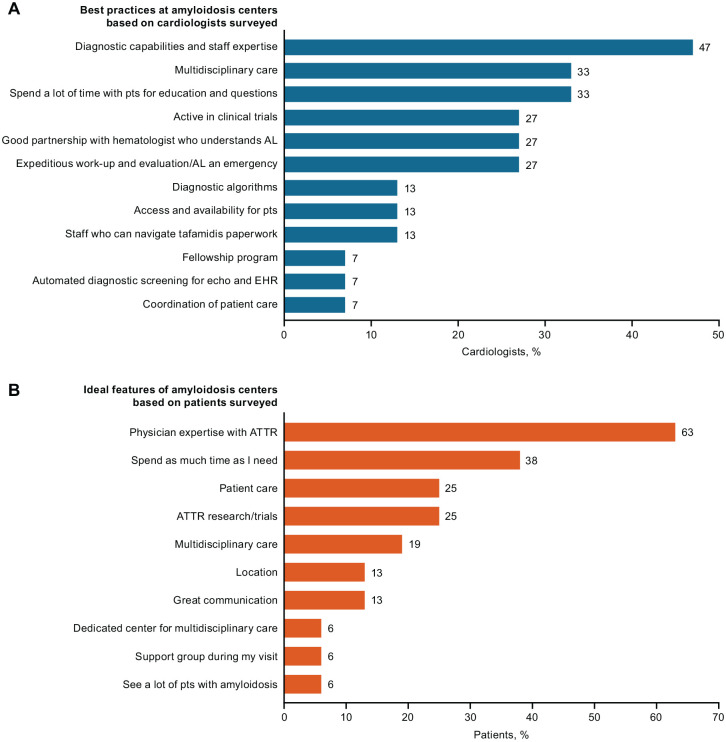
In the cardiologists’ interviews, the most often cited best practices followed at the amyloidosis centers involved diagnostic capability, multidisciplinary care, and time spent with patients (Figure 2A). The nurse practitioners and nurses who participated in the survey also stressed the importance of these practices, as well as strengths in communication and accessibility, symptom management, treatment adjustments, and support for life/care decision-making. The latter healthcare providers considered their role as educators as integral to their work, providing information about the disease and its management on an ongoing basis to patients and their families in person, on the telephone, and via printed materials or online resources.
Figure 2.
(A) Best practices of amyloidosis centers based on cardiologist interviews and (B) features of an “ideal” amyloidosis center based on patient interviews.
AL, light-chain amyloidosis; ATTR, transthyretin amyloidosis; echo, echocardiogram; EHR, electronic health record; pts, patients.
Although there are no consistent metrics used to assess the amyloid centers’ success, some cardiologists defined success by the growing numbers of patients seen at the centers (50%), the numbers of patients involved in clinical trials (42%), and patient outcomes such as survival and hospital readmission rates (33%). The most common challenges facing these centers, based on cardiologists’ responses, were finding better ways to coordinate patient care (29%), overcoming difficulties related to treatment (eg, paperwork, patients’ ability to travel for treatment) (29%), and obtaining adequate institutional support (eg, funding, time required for patients) (29%). Nurse practitioners/nurses most often described the difficulty of coordinating appointments, obtaining diagnostic test results from referring clinicians, and communicating with healthcare providers within the multidisciplinary team as important challenges.
If advising healthcare professionals who planned to establish new amyloidosis centers, the cardiologists would recommend taking a multidisciplinary approach, ensuring that staff have expertise with diagnostic modalities, allocating time for patient education, and involving the centers in multicenter clinical trials. In addition, they suggested that center administrators hire patient coordinators and other staff to navigate insurance approval of treatments, establish an institutional patient database, and confirm that hematologists/oncologists on the multidisciplinary team are proficient in managing AL amyloidosis and plasma cell dyscrasias.
In their interviews, patients described the “ideal” amyloidosis center as having physicians with expertise in ATTR-CM who spend as much time as needed with them (Figure 2B). In addition, patients indicated that the quality of patient care and potential for participation in clinical trials were also important features of these centers.
Diagnostic approaches followed at amyloidosis centers
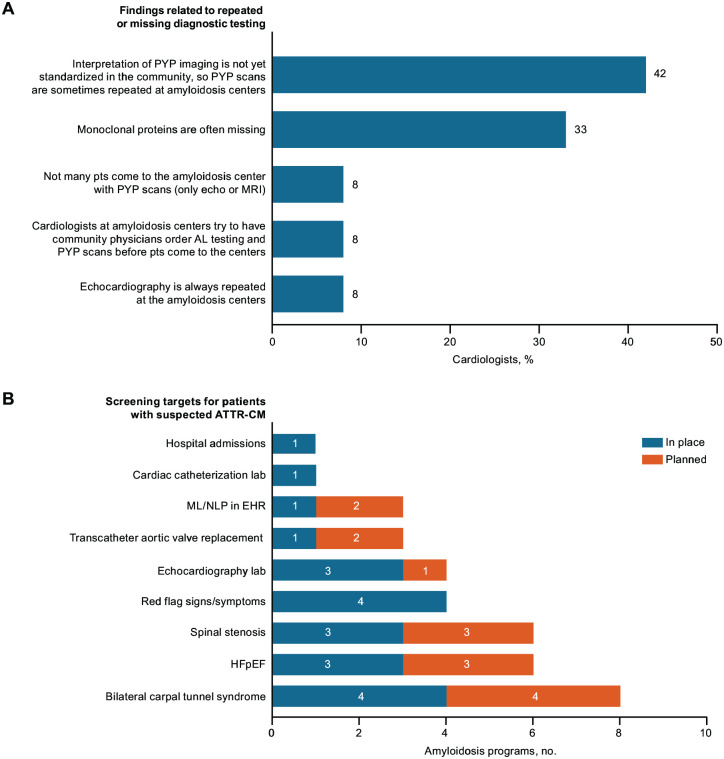
All cardiologists reported that additional testing was conducted to confirm a diagnosis of ATTR-CM in patients entering their amyloidosis centers (Figure 3A). Many (42%) of these specialists noted a lack of standardization in the interpretation of PYP scans by referring clinicians in the community, and they therefore ordered repeat tests as part of patients’ diagnostic work-up at the centers. At most amyloidosis centers (80%), AL amyloidosis is ruled out before PYP scans are ordered. Additionally, one-third of cardiologists indicated that referred patients required proteomic analysis with mass spectroscopy—the gold standard for identifying amyloid protein subtypes—when they arrived at the centers, as these tests had not been previously conducted.
Figure 3.
(A) Practices at amyloidosis centers related to repeated or missing diagnostic tests and (B) “hot spots” monitored by cardiologists in amyloidosis centers to help identify patients with undiagnosed ATTR-CM.
AL, light-chain amyloidosis; ATTR-CM, transthyretin amyloid cardiomyopathy; echo, echocardiogram; EHR, electronic health record; HFpEF, heart failure with preserved ejection fraction; ML, machine learning; MRI, magnetic resonance imaging; NLP, natural language processing; pts, patients; PYP, 99mtechnetium-pyrophosphate.
According to most cardiologists, their amyloidosis centers had processes already in place, or planned, to screen for undiagnosed ATTR-CM in patients visiting the center (Figure 3B). The most commonly cited approaches for screening at-risk patients were collaborating with orthopedic surgeons to identify patients undergoing bilateral carpal tunnel release or spinal stenosis procedures, checking electronic health records for newly admitted patients with HF and preserved ejection fraction (HFpEF), and ensuring that red flags for suspected ATTR-CM were included in the diagnostic assessment of patients with HFpEF.
When diagnosing new patients with suspected ATTR-CM, a majority of cardiologists reported first ordering serum and urine electrophoresis with immunofixation and immunoglobulin free AL assays, to exclude AL amyloidosis. For patients with normal AL test results, PYP scintigraphy is then requested to detect potential myocardial amyloid deposition. At all but 1 center, cardiologists reported that approximately 75% to 100% of patients underwent PYP nucleotide imaging. Across amyloidosis centers, the majority of these specialists ordered endomyocardial biopsy in <20% of patients with ATTR-CM, particularly in patients with equivocal AL or imaging findings. More than one-third of patients (38%) who underwent a cardiac biopsy alone (ie, in the absence of scintigraphy) were diagnosed more than 4 years prior to the survey.
Cardiologists reported that genetic testing was conducted at all amyloidosis centers, and that the centers also provided access to genetic counseling. The majority of centers incorporated genetic counselors into their patient management scheme (79%), while at a smaller number of centers, cardiologists discussed the topic with patients, and the centers offered genetic counseling (14%) or involved genetic testing companies (7%). However, a lack of consistency was observed among these specialists in their approach to surveillance of asymptomatic family members who tested positive for an amyloid transthyretin genetic mutation, which may reflect an absence of standardized surveillance recommendations or guidelines. Commonly mentioned screening approaches included echocardiography, electrocardiography, and/or PYP imaging every few years in such patients, with patient age and low/high penetrance of mutations influencing the frequency and extent of screening. In interviews with patients, 88% indicated that they had genetic testing, but only 27% reported receiving genetic counseling.
Amyloidosis center approaches to multidisciplinary care
The majority of amyloidosis centers (73%) did not have a distinct physical location, that is, patients visited different offices within a hospital to see different specialists. In half of the centers, patients with ATTR-CM were seen on specific days of the week, which, according to some specialists, allowed for more efficient coordination of care.
Most amyloidosis centers (64%) had multidisciplinary group meetings to discuss individual patients. Among these centers, 29% had the meetings once weekly, 7% twice monthly, 21% once monthly, and 7% once quarterly. Genetic counselors and specialty pharmacists plus a range of nurses and advanced practice clinicians were included on many of the centers’ teams.
Most cardiologists (79%) considered working with specialty pharmacies within their institutions to be a positive experience because pharmacy staff offered valuable patient care services such as coordinating health insurance coverage for prescribed ATTR-CM medications. Most nurses/nurse practitioners (78%) also reported regular interaction with specialty pharmacies, and several praised the level of support provided. However, some cardiologists (29%) reported that they were unused to working with specialty pharmacies, and they had received some patients by referral whose original cardiologists preferred not to handle the ATTR-CM treatment-related paperwork.
Barriers to patient access to amyloidosis centers
Among the patients interviewed, nearly one-third (31%) identified travel as the greatest challenge to accessing care at amyloidosis centers. One-way travel to a center required 30 minutes or less in 25% of patients, 1 to 2 hours in 38%, 3 to 4 hours in 13%, and 5 hours or more in 25%. Approximately 37% of patients traveled alone by car or bus for center visits, 44% drove with someone else, and 19% traveled by airplane.
Traveling long distances was particularly problematic for patients with ATTR-CM and concomitant neuropathy. The physical demands of patients’ travel were also potentially complicated by other commonly reported symptoms of their condition, such as decreased stamina, fluid overload, and shortness of breath. Due to these challenges, some patients (13%) expressed concern about their ability to continue to receive future care at their center.
During the survey, 13% of patients and 75% of patient advocates indicated that problems related to insurance coverage were obstacles to receiving treatment for amyloidosis. Other less common treatment-related concerns expressed by patients were uncertainty about where to receive treatment and healthcare provider awareness of treatment, high treatment costs, and waiting for regulatory approval of new therapies.
In their interviews, 67% of nurses/nurse practitioners indicated that they provided assistance in addressing barriers to patients accessing care. The majority worked in tandem with social workers to help patients overcome travel or financial obstacles.
Role of clinical research and registries
All of the amyloidosis centers were involved in clinical trials and had institutional registries. Most centers participated in or planned to participate in national registries, such as the Cedars Sinai Amyloidosis Registry and the Transthyretin Amyloidosis Outcomes Survey (THAOS). Among the patients interviewed, 94% were made aware of clinical trials or registries for ATTR-CM by their amyloidosis centers, and 75% had participated in these types of research initiatives.
Collaboration between amyloidosis centers and patient support organizations
More than half of the cardiologists interviewed (56%) were uncertain whether patients had found their amyloidosis centers based on the recommendations of patient advocacy groups—such as the Amyloidosis Foundation, ASG, and the National Organization for Rare Disorders—or the online tool My Amyloidosis Pathfinder. Of the remaining cardiologists, half (22%) responded that patients had used these pathways to find their institution and half (22%) responded that they had not. Regardless of their response, the cardiologists recognized the value of their centers’ earning the recommendation of such organizations to raise patient awareness.
All of the patient advocates participating in the interviews indicated that an amyloidosis center’s multidisciplinary team approach was an essential consideration when selecting the centers listed on their organizations’ websites. Other important criteria were the number of patients with amyloidosis treated annually at the center, the number of years of experience treating patients with the condition, and the types of amyloidosis treated. According to these patient advocates, their organizations provided a wide range of support for amyloidosis centers via physician education (eg, grand rounds); patient education (eg, materials available free or online); patient support groups (eg, events featuring guest speakers at amyloidosis centers); and research (eg, patient information on clinical trials and grant programs). Three-quarters of the amyloidosis centers involved in this survey hosted support group meetings for patients with ATTR-CM.
Discussion
Over the past few decades, a growing number of CoEs have emerged across the US. These centers are dedicated to improving the quality of care for patients with complex, serious medical conditions, and expanding the depth and breadth of healthcare services available in the community.4 No single definition can be applied to CoEs, although they generally share several important traits, including, most notably, the provision of highly skilled experts and related resources to enhance disease management and support innovation in a specific disease state. However, in the absence of accepted guidance on their constitution, administrators at healthcare institutions seeking to establish such centers must improvize their approach to some extent, diminishing the likelihood of success in expanding healthcare services in their communities.3
With our current research, we sought to provide expert opinions and insights on the best practices and other salient characteristics of specialized amyloidosis centers in the US for healthcare providers and institution administrators who may be planning to establish a new amyloidosis center or to improve an existing one. Specialized amyloidosis centers offer comprehensive expert care of patients with ATTR-CM characterized by staff expertise, a multidisciplinary approach, advanced diagnostics, and time dedicated to patient education. These centers play an integral role in amyloidosis assessment and treatment, but we know relatively little about their operations, interactions with community physicians and patients, or approaches to disease management as a whole.
We designed and conducted this survey to gather information about specialized amyloidosis centers, including best practices, from the perspective of healthcare providers who see patients with ATTR-CM at the centers. The survey also provides insights into the patient journey to amyloidosis specialists at the centers, encompassing a range of patient decisions (eg, center selection) and experiences (eg, overcoming barriers to care). Lastly, patient advocates were included in the survey to provide a description of their organization’s role in supporting patients with amyloidosis and specialized amyloidosis centers.
The specialized amyloidosis centers participating in this survey provide support for many patients with ATTR-CM in the US, often managing their care from first suspicion of the disease through diagnosis confirmation and treatment. These centers are dedicated to improving patients’ healthcare experience, regardless of their particular location or situation. As described here, multidisciplinary teams of cardiologists, nurses, neurologists, imaging and pathology experts, specialty pharmacists, and genetic counselors at amyloidosis centers can provide a broad range of coordinated services for patients with this rare disease. The specialists at these centers follow currently recommended diagnostic pathways,10 using sensitive and accurate testing modalities, to identify patients with suspected amyloidosis and confirm the disease phenotype. In addition, the centers often serve as a gateway for patients interested in enrolling in clinical trials or seeking additional support via patient advocacy groups.
By elucidating the best practices and strengths of these centers, our findings may help to raise awareness of them and to inform healthcare providers and patients in the community about the high level of multidisciplinary care and expertise required to successfully manage this complex, life-threatening disease. For example, the survey highlighted several approaches adopted at amyloidosis centers to identify patients with potentially undiagnosed amyloidosis, including screening patients undergoing bilateral carpal tunnel release or spinal stenosis procedures and those with HFpEF or other known red flags for ATTR-CM, which may encourage early suspicion and diagnosis of ATTR-CM among community healthcare providers.
Information provided by the cardiologists participating in this survey about the diagnostic expertise and use of recommended protocols at amyloidosis centers may help reinforce the advantages of referring patients with suspected disease to amyloidosis specialists. Moreover, the description of the varied models of collaboration among community healthcare providers and amyloidosis specialists in our findings may help foster a better understanding of these relationships and improve communication when managing patients with ATTR-CM. Patients’ identification of their greatest difficulties and barriers to center access may be useful to amyloidosis centers in developing services and support systems tailored to address unmet patient needs. Finally, the information provided by patient advocates about selection criteria for amyloidosis center recommendations on their websites and the broad range of activities and resources their organizations provide may help improve cooperation between these organizations and amyloidosis centers in the future.
Although our qualitative survey provides some useful insights about these centers, additional work is needed to improve access/referral, evaluate practices and procedures, and enhance outcomes. Closer partnerships with amyloidosis patient support groups could be forged to help increase referral of patients with HF to specialized amyloidosis centers. In addition, metrics that allow evaluation of center success in managing patients with ATTR-CM have not yet been designed or implemented.
The research initiative employed in this study has several strengths, including an interview format that enabled in-depth examination of the best practices followed and the challenges facing healthcare providers and patients at US amyloidosis centers. Our qualitative approach yielded more nuanced and complex perspectives than would have been obtained with a quantitative approach. Moreover, the theoretical framework of this research allowed for revision of our original approach based on emerging information provided by some interviewees, with the subsequent inclusion of representatives from amyloidosis patient advocacy groups adding an important dimension to the survey findings. Finally, in conducting the survey and reporting the survey findings, we adhered to established guidelines for qualitative research (COREQ).9
The limitations of our research are largely associated with its qualitative nature. The sample size of participating specialized amyloidosis centers was limited, primarily because ATTR-CM is a rare disease, but nonetheless represented approximately one-fifth of the total number of US centers in existence (estimated to be 66 centers11). Publicly available online data for amyloidosis centers in the US varies, and selection bias is possible as we considered multiple standards when choosing centers for inclusion in the absence of an established definition of a CoE. Data were collected from relatively few individuals based on their opinion, experience, and judgment. The findings are not statistically representative and would be difficult to replicate; they cannot be objectively verified or generalized to a larger population. Finally, the survey was conducted before the onset of the COVID-19 pandemic in the US and therefore does not address changes in practice that may subsequently have occurred, for example, increased reliance on telehealth, and possible delays in ATTR-CM diagnosis and treatment monitoring due to social distancing requirements.
Raising awareness of the best practices of the specialized amyloidosis centers among healthcare providers in the US may reinforce the benefits of early referral and comprehensive care for patients with ATTR-CM. The center practices described in this survey may provide a model for healthcare providers in the community to consider when managing patients with suspected or diagnosed ATTR-CM or planning additional centers dedicated to their care.
Supplemental Material
Supplemental material, sj-pdf-1-cic-10.1177_11795468211015230 for Best Practices in Specialized Amyloidosis Centers in the United States: A Survey of Cardiologists, Nurses, Patients, and Patient Advocates by Jose Nativi-Nicolau, Nitasha Sarswat, Johana Fajardo, Muriel Finkel, Younos Abdulsattar, Adam Castaño, Lori Klein and Alexandra Haddad-Angulo in Clinical Medicine Insights: Cardiology
Acknowledgments
The authors would like to thank all of the healthcare providers, patients, and patient advocates who participated in this study for their valuable contributions. Medical writing support was provided by Donna McGuire of Engage Scientific Solutions and was funded by Pfizer.
Footnotes
Declaration of conflicting interests:The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: JNN or his institution receives funding for research and serving on advisory boards from Alnylam, Akcea, Pfizer, and Eidos. NS has served as a consultant and participated in advisory boards for Pfizer, Alnylam, and Akcea; and has received funding for research grants from Pfizer. JF and MF have no conflicts of interest to report. YA, AC, and AH are full-time employees of Pfizer and own Pfizer stock/stock options. LK received funding from Pfizer to conduct this research and owns Pfizer stock.
Funding:The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was sponsored by Pfizer.
Author Contributions: All authors made substantial contributions to the concept/design of the work or to the acquisition, analysis or interpretation of the data; drafted the article and/or revised it critically for important intellectual content; approved the submitted version of the article; and participated sufficiently to take public responsibility for appropriate portions of the content. All authors also had access to the data.
Supplemental Material: Supplemental material for this article is available online.
References
- 1. Ruberg FL, Grogan M, Hanna M, et al. Transthyretin amyloid cardiomyopathy: JACC state-of-the-art review. J Am Coll Cardiol. 2019;73:2872-2891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Witteles RM, Bokhari S, Damy T, et al. Screening for transthyretin amyloid cardiomyopathy in everyday practice. JACC Heart Fail. 2019;7:709-716. [DOI] [PubMed] [Google Scholar]
- 3. Elrod JK, Fortenberry JL., Jr. Centers of excellence in healthcare institutions: what they are and how to assemble them. BMC Health Serv Res. 2017;17(suppl 1):425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Pakizegee M, Stefanacci RG. Centers of excellence: criteria and comprehensive clinical pathways. J Clin Pathways. 2019;5:28-30. [Google Scholar]
- 5. Shah SJ, Cogswell R, Ryan JJ, et al. How to develop and implement a specialized heart failure with preserved ejection fraction clinical program. Curr Cardiol Rep. 2016;18:122. [DOI] [PubMed] [Google Scholar]
- 6. Grosse SD, Schechter MS, Kulkarni R, et al. Models of comprehensive multidisciplinary care for individuals in the United States with genetic disorders. Pediatrics. 2009;123:407-412. [DOI] [PubMed] [Google Scholar]
- 7. Gumnit RJ, Labiner DM, Fountain NB, et al. Data on specialized epilepsy centers: report to the Institute of Medicine’s Committee on the Public Health Dimensions of the Epilepsies. In: England MJ, Liverman CT, Schultz AM, Strawbridge LM. eds. Epilepsy Across the Spectrum: Promoting Health and Understanding. National Academies Press (US); 2012. [PubMed] [Google Scholar]
- 8. Donnelly JP, Hanna M. Cardiac amyloidosis: an update on diagnosis and treatment. Cleve Clin J Med. 2017;84:12-26. [DOI] [PubMed] [Google Scholar]
- 9. Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19:349-357. [DOI] [PubMed] [Google Scholar]
- 10. Maurer MS, Bokhari S, Damy T, et al. Expert consensus recommendations for the suspicion and diagnosis of transthyretin cardiac amyloidosis. Circ Heart Fail. 2019;12:e006075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Amyloidosis Support Groups. United States amyloidosis centers. Accessed September 30, 2020. https://www.amyloidosissupport.org/amyloidosis_centers.html
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-cic-10.1177_11795468211015230 for Best Practices in Specialized Amyloidosis Centers in the United States: A Survey of Cardiologists, Nurses, Patients, and Patient Advocates by Jose Nativi-Nicolau, Nitasha Sarswat, Johana Fajardo, Muriel Finkel, Younos Abdulsattar, Adam Castaño, Lori Klein and Alexandra Haddad-Angulo in Clinical Medicine Insights: Cardiology