Abstract
The COVID 19 pandemic has greatly affected the world population. SARS CoV2 infection in pediatric patients is related to the development of mild symptoms and in some cases gastrointestinal manifestations. We present the case of a patient with intussusception as a manifestation associated with SARS CoV2 infection, treated by ultrasound-guided hydrostatic reduction with successful results.
Keywords: intussusception, Sars-Cov2, COVID 19, mechanic reduction
Introduction
Intussusception is the most common cause of intestinal obstruction in children, it occurs more frequently in patients between 3 and 12 months of age.1 the etiology of the disease is related to the hypertrophy of the lymphoid tissue of the intestine, generally associated with viral infections.2 The COVID-19 pandemic has represented a global challenge in health care, although it is true that the majority (90%) of pediatric patients are diagnosed as asymptomatic or with mild or moderate disease,3 18% of these patients have gastrointestinal symptoms such as abdominal pain and diarrhea.4 There are few reported cases of intussusception as a manifestation of COVID 19.5-7
Case Presentation
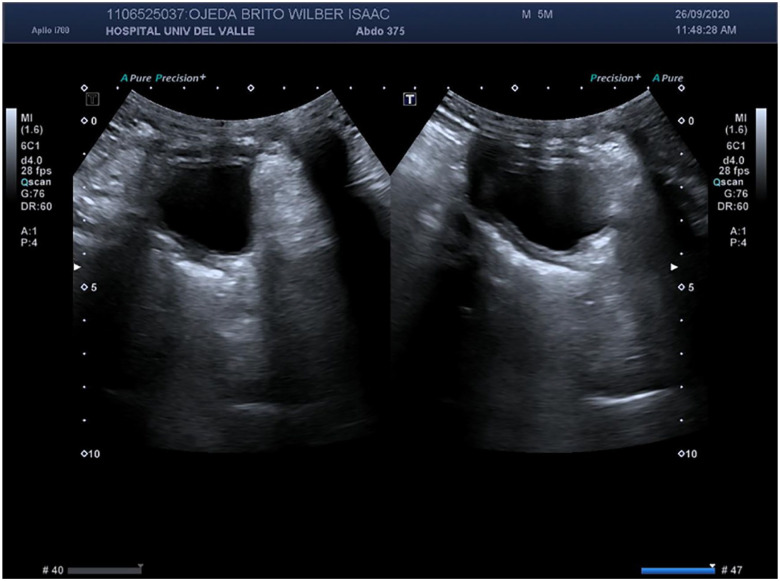
A 5-month-old male patient presents 2 days of symptoms consisting of fever associated with several episodes of vomiting. On the morning of the day before admission, he presented an episode of “jelly stool,” after this, he presented an absence of stools and food intolerance. Respiratory symptoms have not been experienced, there was no contact with people with respiratory symptoms or positive for SARS CoV2 infection. Abdominal ultrasound is performed (Figure 1), founding signs of ileocolic intussusception, with significant colonic parietal thickening of 6 mm on average.
Figure 1.

Intussusception finds in abdominal echography.
A hydrostatic reduction guided by ultrasound was carried out, when the sonde was placed jelly stools were obtained, 800 ml saline solution (NaCl 0.9%) was passed at a height of 1.2 m, verifying the progressive reduction until the image of intussusception was disappeared. Due to the febrile episodes described, it was decided to take a PCR for SARS CoV2, which gave a positive result.
Two days after mechanical reduction, a follow-up ultrasound was performed were no images suggesting intussusception were evident (Figure 2). The patient has clinical improvement and is able to tolerate the food administration on the second day after the intervention, is discharged without complications.
Figure 2.
Abdominal echography without radiological intussusception signs.
Discussion
Gastrointestinal symptoms such as diarrhea, vomiting, and abdominal pain occur in 6.6% to 18% of pediatric patients with SARS CoV2 infection.4,7 It is important to note that the expression of angiotensin-converting enzyme 2 (ACE2) have a fundamental role in coronavirus infection, this enzyme is not exclusive to lung cells, is also present in cells of the gastrointestinal tract, specifically in the epithelial tissue of the esophagus, ileum, and colon,8 and may explain the significant percentage of gastrointestinal symptoms in pediatric patients.
Several viral agents have been considered in the pathogenesis of intussusception, including adenovirus, rotavirus, enterovirus, herpes, cytomegalovirus, and Epstein-Barr virus.2 Besides that, histological analyzes have reported proteins of the viral nucleocapsid of the SARS-COV2 find in the cytoplasm of epithelial cells of the duodenum and rectum.9 Due to this, although a direct pathophysiological relationship between SARS-COV2 infection and intussusception has not been described, this virus may be an important etiological factor.
Intussusception is a frequent pathology in the practice of pediatric surgery, it has a mortality that ranges from 1% to 9%.10 The treatment has evolved greatly, pneumatic or hydrostatic reduction with radiological support implies minimal morbidity and shorter hospitalization time for the patient compared to surgical management.10,11 In the case reports that relate SARS-COV2 infection with intussusception and management with pneumatic or hydrostatic reduction, there have been no complications related to this treatment.
Conclusion
The association between intussusception and SARS CoV2 has not been fully clarified, although most pediatric patients present with mild symptoms, it is important to pay attention to the possible complications that may arise from this viral infection. Intussusception is an important cause of morbidity and mortality in pediatric patients; management with mechanical reduction with radiological support continues to be the first line of management for these patients.
Footnotes
Author Contributions: All authors participated in substantial contributions to the conception and design of the manuscript, acquisition, analysis and interpretation of the data; the drafting of the manuscript and critical review of important intellectual content.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Informed Consent and Approval of the Ethics Committee: The elaboration of this product received the approval of the ethics committee of the Hospital Universitario del Valle. Similarly, the guardian of the patient involved signed informed consent for the publication of clinical information.
ORCID iD: Nicolás Guerrón  https://orcid.org/0000-0002-9336-5978
https://orcid.org/0000-0002-9336-5978
References
- 1. Mandeville K, Chien M, Willyerd FA, Mandell G, Hostetler MA, Bulloch B. Intussusception: clinical presentations and imaging characteristics. Pediatr Emerg Care. 2012;28:842-844. doi: 10.1097/PEC.0b013e318267a75e [DOI] [PubMed] [Google Scholar]
- 2. Ntoulia A, Tharakan SJ, Reid JR, Mahboubi S. Failed intussusception reduction in children: correlation between radiologic, surgical, and pathologic findings. Am J Roentgenol. 2016;207:424-433. doi: 10.2214/AJR.15.15659 [DOI] [PubMed] [Google Scholar]
- 3. Tezer H, Bedir Demirdağ T. Novel coronavirus disease (COVID-19) in children. Turk J Med Sci. 2020;50:592-603. doi: 10.3906/sag-2004-174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Han MS, Choi EH, Chang SH, et al. Clinical characteristics and viral RNA detection in children with Coronavirus disease 2019 in the Republic of Korea. JAMA Pediatr. 2021:175:73-80. doi: 10.1001/jamapediatrics.2020.3988 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Bazuaye-Ekwuyasi EA, Camacho AC, Saenz Rios F, et al. Intussusception in a child with COVID-19 in the USA. Emerg Radiol. 2020;27:761-764. doi: 10.1007/s10140-020-01860-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Moazzam Z, Salim A, Ashraf A, Jehan F, Arshad M. Intussusception in an infant as a manifestation of COVID-19. J Pediatr Surg Case Rep. 2020;59:101533. doi: 10.1016/j.epsc.2020.101533 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Cui X, Zhang T, Zheng J, Zhang J, Si P, Xu Y. Children with coronavirus disease 2019 (COVID-19): a review of demographic, clinical, laboratory and imaging features in 2,597 pediatric patients. J Med Virol. 2020;92:1501-1510. doi: 10.1002/jmv.26023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Zhang H, Kang Z, Gong H, et al. The digestive system is a potential route of 2019-nCov infection: a bioinformatics analysis based on single-cell transcriptomes. Preprint. Posted online Jan 1, 2020. bioRxiv 2020.01.30.927806. 10.1101/2020.01.30.927806 [DOI] [Google Scholar]
- 9. Tian Y, Rong L, Nian W, He Y. Review article: gastrointestinal features in COVID-19 and the possibility of faecal transmission. Aliment Pharmacol Ther. 2020;51:843-851. doi: 10.1111/apt.15731 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Gluckman S, Karpelowsky J, Webster AC, McGee RG. Management for intussusception in children. Cochrane Database Syst Rev. 2017;6:CD006476. doi: 10.1002/14651858.CD006476.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Beres AL, Baird R. An institutional analysis and systematic review with meta-analysis of pneumatic versus hydrostatic reduction for pediatric intussusception. Surgery. 2013;154:328-334. doi: 10.1016/j.surg.2013.04.036 [DOI] [PubMed] [Google Scholar]