Abstract
Study Design:
Retrospective analysis.
Objective:
Lumbar disc herniation is one the most common condition responsible for low back and radicular pain. Although the symptoms are not proportional to the size of disc prolapse but massive disc herniation frequently needs surgical management. According to literature, the incidence of low back pain, recurrent disc herniation and segmental instability are more in discectomy whereas incidence of adjacent segment degeneration (ASD) is more after fusion surgery. There are very few studies that directly compare long-term functional outcome of both these procedures. We compared the functional outcome of both the procedures in this study.
Methods:
All patients of massive disc prolapse, operated at our center between 2011 to 2017, were contacted. All the patients underwent either discectomy or transforaminal lumbar interbody fusion (TLIF). Functional outcomes of all the patients were collected using visual analogue scale (VAS) (back), VAS (leg), modified Oswestry Disability Index (mODI), Sciatica Bothersomeness Index (SBI), and McNab’s criterion. Various complications were also analyzed.
Results:
There were 144 patients in the discectomy group and 123 patients in the TLIF group. Mean duration of follow-up was 55.07 months and 51.86 months, respectively. Both the groups show no significant difference in VAS. Significant difference was seen in mODI and SBI favoring discectomy. McNab’s criterion showed excellent result in 80% of patients of discectomy compared with 68% patients of TLIF. Overall complication rate in discectomy group was 11% whereas 13% in TLIF group.
Conclusion:
Both show good functional outcome but better in discectomy. Recurrent herniation and instability were noticed more with discectomy and ASD was more common after fusion surgeries. The choice of procedure should be individualized, and it also depends on surgical expertise, but in developing countries where resources are constrained, discectomy should be preferred.
Keywords: massive disc herniation, disc, lumbar, discectomy, TLIF, fusion
Introduction
Lumbar disc herniation refers to displacement of nucleus pulposus beyond its normal place and is considered a common etiology for radiculopathy. About 95% of disc herniation cases occur at level of lower lumbar spine L4-5 and L5-S1. There is a definite familial tendency of lumbar disc herniation.1) Many treatment options are available for lumbar disc herniation, but diagnosis should correlate with patient’s history, clinical examination, and radiological investigations. Treatment options of lumbar disc herniation are either conservative or surgical. Outcomes are quite variable between the categories. Published studies suggest that if surgery is done within the first 3 months of leg pain, then the long-term results of such patients are better compared to those in whom surgery is delayed.2
Only a few studies focus on the size of disc prolapse.3-5) Massive disc prolapse is defined on magnetic resonance imaging as a condition where herniated disc material occupies 50% or more anteroposterior diameter of spinal canal.6,7 However, there are also published studies that show equivalent outcomes of conservative management of massive lumbar disc herniation on long-term follow-up.8 The most common presenting symptom of massive disc herniation is radicular pain, may or may not associated with neurological deficit notably among them is cauda equina syndrome which needs urgent attention.9,10 Controversy still remains about the type of surgery. There are surgeons who feel discectomy is good enough for such patients whereas other group of surgeons has demonstrated better protection against recurrence with primary fusion surgery. Surgeons in favor of fusion believe that after discectomy, residual low back pain and recurrent herniation become an issue, because the remaining disrupted disc must continuously bear and support the trunk for rest of the patient’s life.11 Studies have shown that there are 3% to 18% incidence of reherniation in cases of lumbar discectomy.12 Also, there are increased chances of complication in revision surgery of such cases. Though there are many studies evaluating the long-term results of both the procedures separately, there are very few studies comparing the long-term outcome of both the procedures.
In this study, we aim to retrospectively review cases of massive disc prolapse treated surgically either with microscopic lumbar discectomy alone or transforaminal lumbar interbody fusion (TLIF) and compared their functional outcome.
Materials and Methods
Patient data was collected retrospectively between January 2011 to December 2017. As per institutional ethical committee, it is a registry-based study, so ethical clearance was not required. The inclusion criteria were (1) intracanal herniation that occupies >50% of the spinal canal, (2) age between 18 and 65 years, (3) predominant symptom as leg pain associated with massive disc herniation, (4) visual analogue scale (VAS) score >5 and modified Oswestry Disability Index (mODI) >40, (5) failed conservative treatment of at least 6 weeks, and (6) no segmental instability on dynamic radiograph. The exclusion criteria were (1) patients aged <18 years and >65 years, (2) patients with rheumatoid arthritis or any destructive spondyloarthropathies, (3) patients with far lateral or extraforaminal disc herniation, (4) patients with recurrent disc herniation, (5) patients with segmental instability, (6) patients with neurological deficit, (7) patients with multiple disc herniations, and (8) patients with canal stenosis.
Surgical Techniques
Microscopic Discectomy
Our technique of microdiscectomy used is the same as that introduced by Caspar et al.13 The midline incision was given at desired level. The fascia to the side of herniation was incised along the spinous process and the muscle was stripped subperiosteally to expose the desired lamina. After proper exposure and placement of retractors, overhanging of caudal lip of rostral lamina was partially removed with the help of high-speed burr or Leksell rongeur. The required amount of ligamentum flavum was removed. The dural sac along with traversing nerve root was retracted. The herniated disc was removed using small forceps. Targeted fragmentectomy was done in all cases. After satisfactory disc removal, retractor was removed, wound was irrigated properly, and closed in layers. Figure 1 shows a case of massive disc prolapse managed with discectomy alone.
Figure 1.
A case of massive disc prolapse managed with discectomy alone.
Transforaminal Lumbar Interbody Fusion
This surgery was also performed by a standard technique as described in Rosenberg et al.14 Vertical incision was given at the desired level. Muscles and soft tissues were retracted laterally to expose spinous process, lamina, facet joints, and transverse process. After the exposure on both sides, pedicle screws were placed in standard fashion followed by removal of spinous process at desired level. Laminectomy was done. Facetectomy of required side was performed. Once the neural elements were adequately decompressed, then disc space was identified, and standard discectomy was performed. Adequate removal of cartilaginous end plates was performed. PEEK (polyetheretherketone) cage of appropriate size was filled with autologous bone graft and inserted in the disc space taking care of exiting nerve root and thecal sac. After the interbody cage was placed, the pedicle screws were attached to and compressed on the rod, thereby restoring the lumbar lordosis while maintaining the restored disc height. The wound was properly irrigated and closed in multiple layers using appropriate sutures. Figure 2 shows a case of massive disc prolapse managed with TLIF.
Figure 2.
A case of massive disc prolapse managed with transforaminal lumbar interbody fusion (TLIF).
Data collected for analysis was age, gender, affected level, duration of follow-up, mODI, Sciatica Bothersomeness Index (SBI), modified McNab’s criterion, and any complications. Back and leg pain were quantified using VAS score collected from the patients at follow-up. The mODI score was used to look how patient’s back and leg pain affecting his daily life. SBI was used to quantify how bothersome patient’s back and leg pain are, if present. Last, we also used modified McNab’s criterion which reflects well surgeon’s impression about surgery overall success in terms of patient’s satisfaction. Broadly, there are 4 categories—excellent, good, fair, and poor. Any patient with significant back and/or leg pain was further evaluated clinically and radiographically.
Adjacent segment degeneration (ASD)15 was defined as a radiologic change in which the narrowing of disc height was >3 mm, the progressive slipping of adjacent segments was >3 mm (in comparison with preoperative lateral flexion and extension radiographs), and the posterior opening of adjacent segments was >5°. For the definition of lumbar instability,16 the intervertebral displacement of the lumbar dynamic X-ray is more than 3 mm or the angle changes more than 15°.
Statistical Analyses
GraphPad Prism V7 software was used for the statistical analysis. The results were presented as mean with standard deviation. P values less than .05 were considered as statistically significant. Unpaired t test was applied to compare age, VAS, mODI, and SBI between 2 groups. Z test was applied to compare McNab’s score.
Results
The data record of 144 patients who had undergone discectomy and 123 patients of TLIF was included for analysis. Both groups were comparable in terms of age, gender, and affected level. The demographic data is summarized in Table 1. The mean duration of follow-up was 55 months in the discectomy group and 51 months in the TLIF group.
Table 1.
Comparison of Demographic Data of Patients in the Discectomy and Transforaminal Lumbar Interbody Fusion (TLIF) Groups.
| Discectomy | TLIF | |
|---|---|---|
| No. of patients, N | 144 | 123 |
| Age, years, mean | 39.26 | 40.87 |
| Gender, n (%) | ||
| Male | 102 (70.83) | 84 (68.3) |
| Female | 42 (29.16) | 39 (31.7) |
| Level, n (%) | ||
| L4-5 | 69 (48) | 85 (69) |
| L5-S1 | 73 (50.7) | 33 (27) |
| Others | 2 | 5 |
| Duration of follow-up, months | 55.07 | 51.86 |
| Mean | ||
| Range | 20-101 | 20-101 |
| Body mass index, kg/m2, mean ± SD | 26 ± 3.5 | 25.5 ± 3.7 |
The age of the patients that were included in the study were comparable to avoid any age-related bias on the outcome of the surgical procedure performed.
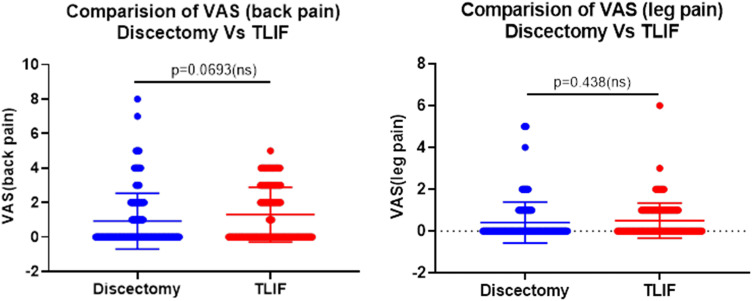
Back pain and leg pain were quantified using VAS collected from the patients at follow-up. Figure 1 is the dot-plot showing the comparison of VAS scores.
The mODI score was used to assess how patient’s back and leg pain affected daily life. SBI was used to quantify how bothersome patient’s back and leg pain are, if present. Figure 2 is the dot-plot showing the comparison of mODI and SBI scores.
Both the groups were found comparable in terms of VAS for back and leg pain and SBI. On the other hand, significant difference was noticed among both groups for mODI, which showed better functional outcome in discectomy. The overall summary of scores is given in Table 2.
Table 2.
Comparison of Functional Outcome Scores Between Discectomy and Transforaminal Lumbar Interbody Fusion (TLIF) Groups.
| Discectomy | TLIF | P | |
|---|---|---|---|
| Mean VAS (back) | 0.92 | 1.29 | .0693 (ns) |
| Mean VAS (leg) | 0.40 | 0.50 | .438 (ns) |
| Mean mODI | 7.734 | 15.61 | .0002 |
| Mean SBI | 1.406 | 1.617 | .58 (ns) |
Abbreviations: VAS, visual analogue scale; mODI, modified Oswestry Disability Index; SBI, Sciatica Bothersomeness Index; ns, nonsignificant.
McNab’s criterion shows significant difference between the 2 groups where 80% patients have excellent outcome in discectomy group compared with 68.42% patients in TLIF group (Figure 3 and Table 3).
Figure 3.
Visual analogue scale (VAS) scores comparison of the patients between the groups. An unpaired t test is applied, which resulted in a 2-tailed P value of .0693 (VAS back pain) and .438 (VAS leg pain), which is statistically nonsignificant.
Table 3.
Comparison of Mcnab’s Score Between Discectomy and Transforaminal Lumbar Interbody Fusion (TLIF) Groups.
| Discectomy (N = 144), % | TLIF (N = 123), % | P | Z | |
|---|---|---|---|---|
| Excellent | 80 | 68.42 105 | .04 036 | 2.0507 |
| Good | 12.8 | 22.80 702 | .04 236 | −2.03 |
| Fair | 5.6 | 7.017 544 | .6527 (ns) | −0.4513 |
| Poor | 1.6 | 1.754 386 | .9282 (ns) | −0.092 |
Abbreviation: ns, nonsignificant.
Figure 4.
Modified Oswestry Disability Index (mODI) and Sciatica Bothersomeness Index (SBI) scores: comparison of the patients between the groups. An unpaired t test is applied, which resulted in a 2-tailed P value of .002 (mODI), which is statistically significant and the P value of .58 (SBI), which is statistically nonsignificant.
Figure 5.
Graphical representation of McNab’s score comparing patients in the discectomy and transforaminal lumbar interbody fusion groups (TLIF).
Complications
Overall, 3 cases of dural tear were observed, with 2 patients in discectomy group and 1 patient in the TLIF group. Both patients were managed successfully with conservative treatment. Seven patients of the discectomy group experienced recurrent herniation and was managed to some extent conservatively. One patient in the discectomy group had foot drop, which has not recovered even at 5 years of follow-up. There was infection postoperatively in 1 discectomy patient and 2 TLIF patients. All 3 patients were managed conservatively with intravenous antibiotics. Five patients in the discectomy group developed instability later in life after successfully recovering with discectomy. Last, 13 patients in the TLIF group were found to develop symptomatic ASD on follow-up.
Discussion
Although the amount of disc prolapse has nothing to do with the intensity of clinical symptoms, but it is usually seen that surgery for massive lumbar disc herniation is more urgently required compared to normal disc herniation due to greater severity of radicular pain and also greater risk of developing cauda equina syndrome. Most commonly performed surgery for massive lumbar disc herniation is either discectomy alone or discectomy along with interbody fusion. According to some surgeons, discectomy alone for massive lumbar disc prolapse can lead to various complications such as intraoperative neural injury or cauda equina syndrome, chronic low back pain, or postoperative segmental instability.17 To avoid such complications, such group of surgeons perform interbody fusion because they prefer cutting facet to create more space for discectomy. Not only do they avoid the aforementioned complications but they also claim to produce better functional results as compared with discectomy.
DePalma et al18 mentioned about the incidence of chronic low back pain after surgical discectomy. They conclude that discogenic low back pain is the most common cause of low back pain after surgical discectomy. They also mentioned that one of the limitations of their study was small sample size. Solberg et al19 also mentioned the same in their publication. They followed 180 patients of microdiscectomy for mean follow-up period of 12 months. Their main follow-up score was ODI, which is a functional scoring used in this study too. They found that mean ODI score of those patients had increased on follow- up. They showed failure rate of 8.9% and if they also add cases of recurrent disc herniation (which they have otherwise excluded while analyzing data) then their failure rate increases to 12.3%. There are groups of surgeons20-23 who believe that fusion surgery is better than discectomy alone in cases of massive lumbar disc prolapse. Satoh et al24 published their study and clearly mentioned massive disc herniation as one of the indications of fusion.
They further added that incidence of residual low back pain and recurrent herniation are much lesser in fusion group compared to nonfusion or discectomy group.
In our study, we have 144 patients in discectomy group and 123 patients in TLIF group. VAS scores for back and leg pain in our study for both groups were comparable. Most of the patients reported no pain in back after discectomy as well as after TLIF. The highest VAS score we have in our discectomy group was 9. This patient also developed foot drop after surgery, which was not recovered. Otherwise, the mean VAS score for discectomy patients in our study was 0.92. Similarly, in the TLIF group, maximum VAS score we noticed was 5. Although the maximum score is higher in the discectomy group but the mean VAS score in TLIF group was 1.29, which is higher than the mean of the discectomy group. On statistical analyses, both groups were found comparable and no procedure is found to be superior to the other in terms of back pain. Many different studies claim more incidence of back pain in discectomy due to heavy loss of nucleus pulposus and massive defect in annulus fibrosus. But our study showed no difference of back pain between the two groups. Similar comparable results were observed in VAS for leg pain.
Li et al25 also found no difference in ODI score of patients of the 2 groups. They concluded that discectomy procedure is better to fusion procedure because it offers less operative time, less blood loss, and less hospitalization time. In our study, mODI and SBI show better functional improvement in discectomy group of patients compared with TLIF group. The possible explanation for this outcome could be derangement in total sagittal balance of spine. The relation of functional outcome and lumbar lordosis is well known.26-28 Although the sagittal parameters were not collected in this study, but this has important role in final functional outcome. The other reason could be, TLIF is a circumferential fusion construct and hence more rigid with higher stiffness. Therefore, more chances of development of ASD.29,30
Mohapatra et al31 reported outcomes of lumbar disc herniation after microdiscectomy. They used McNab’s criterion to look for surgical outcome. They included 53 patients in their study. They reported 57% of patients with excellent outcome and 35% with good outcome. The remaining patients had fair outcome with no patient with poor outcome. In our study, we have used the same McNab’s criterion to report patient’s outcome after surgery. It analyses the patient’s satisfaction looking from surgeon’s perspective. Though most of the patients in both groups have satisfactory outcome, in discectomy group, excellent result was obtained in 80% of patients whereas in TLIF group only 68.42% of patients have excellent results. Overall, more percentage of patients in discectomy group has better outcome.
We found 5 cases of instability in discectomy group. One of the reasons for this could be overzealous removal of bone creating iatrogenic instability. Surgeons favoring discectomy sometimes have narrow margin of safety for iatrogenic instability to prevent inappropriate retraction of dural sac. Also, there were 7 cases of recurrent disc herniation in this group. However, we have 13 (10.5%) cases who developed symptomatic ASD on follow-up in TLIF group. As discussed before, it is considered to be due to development of more rigid construct. The incidence of symptomatic ASD reported in literature is about 18.5%.29,30 whereas incidence of overall ASD reaches up to 50%. No case of symptomatic ASD was reported in discectomy group. Overall, complications seen in the discectomy group were 11% and in the TLIF group were 13%.
Limitations of Study
This is a retrospective study. There is a possibility of selection bias as it was the surgeon’s choice for selection of particular procedure. Preoperative functional scoring was not considered. Radiographic parameters were not taken into consideration.
Conclusion
On analysis, functional outcome is favorable in both the groups. However, both groups have different set of complications. Recurrent disc herniation and instability is seen after discectomy whereas ASD is seen after fusion surgery. Discectomy procedure has advantage of avoidance of fusion disease like ASD. Discectomy patients shows more overall satisfaction and overall complication rates on long-term follow-up are also less. In developing countries, where the resources are limited, discectomy is the preferred procedure. However, more multicenter, randomized, prospective, and long-term studies should be conducted to better understand the outcome of both the procedures.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Anuj Gupta  https://orcid.org/0000-0001-6816-2995
https://orcid.org/0000-0001-6816-2995
References
- 1. Varlotta GP, Brown MD, Kelsey JL, Golden AL. Familial predisposition for herniation of a lumbar disc in patients who are less than twenty-one years old. J Bone Joint Surg Am. 1991;73:124–128. [PubMed] [Google Scholar]
- 2. Støttrup CC, Andresen AK, Carreon L, Andersen MØ. Increasing reoperation rates and inferior outcome with prolonged symptom duration in lumbar disc herniation surgery—a prospective cohort study. Spine J. 2019;19:1463–1469. [DOI] [PubMed] [Google Scholar]
- 3. Carragee EJ, Han MY, Suen PW, Kim D. Clinical outcomes after lumbar discectomy for sciatica: the effects of fragment type and anular competence. J Bone Joint Surg Am. 2003;85:102–108. [PubMed] [Google Scholar]
- 4. Halldin K, Lind B, Rönnberg K, et al. Three-dimensional radiological classification of lumbar disc herniation in relation to surgical outcome. Int Orthop. 2009;33:725–730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Long D. Decision making in lumbar disc disease. Clin Neurosurg. 1992;39:36–51. [PubMed] [Google Scholar]
- 6. Akhaddar A, Belfquih H, Salami M, Boucetta M. Surgical management of giant lumbar disc herniation: analysis of 154 patients over a decade. Neurochirurgie. 2014;60:244–248. [DOI] [PubMed] [Google Scholar]
- 7. Jeon CH, Chung NS, Son KH, Lee HS. Massive lumbar disc herniation with complete dural sac stenosis. Indian J Orthop. 2013;47:244–249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Benson RT, Tavares SP, Robertson SC, Sharp R, Marshall RW. Conservatively treated massive prolapsed discs: a 7-year follow-up. Ann R Coll Surg Engl. 2010;92:147–153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Black HA. Massive Herniation of the intervertebral disc producing compression of the cauda equina. Calif Med. 1948;69:271–274. [PMC free article] [PubMed] [Google Scholar]
- 10. Louison R, Barber JB. Massive herniation of lumbar discs with compression of the cauda equina—a surgical emergency; report of two cases. J Nat Med Assoc. 1968;60:188–190. [PMC free article] [PubMed] [Google Scholar]
- 11. Yorimitsu E, Chiba K, Toyama Y, Hirabayashi K. Long-term outcomes of standard discectomy for lumbar disc herniation: a follow-up study of more than 10 years. Spine (Phila Pa 1976). 2001;26:652–657. [DOI] [PubMed] [Google Scholar]
- 12. McGirt MJ, Ambrossi GL, Datoo G, et al. Recurrent disc herniation and long-term back pain after primary lumbar discectomy: review of outcomes reported for limited versus aggressive disc removal. Neurosurgery. 2009;64:338–345. [DOI] [PubMed] [Google Scholar]
- 13. Caspar W. A new surgical procedure for lumbar disc herniation causing less tissue damage through a microsurgical approach. In: Wullenweber R, Brock M, Hamer J, Klinger M, Spoerri O, eds. Lumbar Disc Adult Hydrocephalus. Springer; 1977:74–80. [Google Scholar]
- 14. Rosenberg WS, Mummaneni PV. Transforaminal lumbar interbody fusion: technique, complications, and early results. Neurosurgery. 2001;48:569–575. [DOI] [PubMed] [Google Scholar]
- 15. Park P, Garton HJ, Gala VC, Hoff JT, McGillicuddy JE. Adjacent segment disease after lumbar or lumbosacral fusion: review of the literature. Spine (Phila Pa 1976). 2004;29:1938–1944. [DOI] [PubMed] [Google Scholar]
- 16. Frymoyer JW, Gordon SL. New Perspectives on Low Back Pain. American Academy of Orthopaedic Surgeons; 1989:217–248. [Google Scholar]
- 17. Hedtmann A. The so-called post-discotomy syndrome—failure of intervertebral disk surgery? [in German] Z Orthop Ihre Grenzgeb. 1992;130:456–466. [DOI] [PubMed] [Google Scholar]
- 18. DePalma MJ, Ketchum JM, Saullo TR, Laplante BL. Is the history of a surgical discectomy related to the source of chronic low back pain? Pain Physician. 2012;15:E53–E58. [PubMed] [Google Scholar]
- 19. Solberg TK, Nygaard ØP, Sjaavik K, Hofoss D, Ingebrigtsen T. The risk of “getting worse” after lumbar microdiscectomy. Eur Spine J. 2005;14:49–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Vaughan PA, Malcolm BW, Maistrelli GL. Results of L4-L5 disc excision alone versus disc excision and fusion. Spine (Phila Pa 1976). 1988;13:690–695. [PubMed] [Google Scholar]
- 21. Frymoyer JW, Hanley EN, Jr, Howe J, Kuhlmann D, Matteri RE. A comparison of radiographic findings in fusion and nonfusion patients ten or more years following lumbar disc surgery. Spine (Phila Pa 1976). 1979;4:435–440. [DOI] [PubMed] [Google Scholar]
- 22. Rish BL. A comparative evaluation of posterior lumbar interbody fusion for disc disease. Spine (Phila Pa 1976). 1985;10:855–857. [DOI] [PubMed] [Google Scholar]
- 23. Young H, Love J. End results of removal of protruded lumbar intervertebral discs with and without fusion. Instruction Course Lecture. Am Acad Orthop Surg. 1959;16:213–216. [Google Scholar]
- 24. Satoh I, Yonenobu K, Hosono N, Ohwada T, Fuji T, Yoshikawa H. Indication of posterior lumbar interbody fusion for lumbar disc herniation. J Spinal Disord Tech. 2006;19:104–108. [DOI] [PubMed] [Google Scholar]
- 25. Li YW, Wang HJ, Wang YS, Cui W, Zhou P, Li C. Comparison of percutaneous endoscopic lumbar discectomy versus transforaminal lumbar interbody fusion in treating upper lumbar disc herniation [in Chinese]. Zhonghua Yi Xue Za Zhi. 2018;98:113–116. [DOI] [PubMed] [Google Scholar]
- 26. Glassman SD, Bridwell K, Dimar JR, Horton W, Berven S, Schwab F. The impact of positive sagittal balance in adult spinal deformity. Spine (Phila Pa 1976). 2005;30:2024–2029. [DOI] [PubMed] [Google Scholar]
- 27. Kawakami M, Tamaki T, Ando M, Yamada H, Hashizume H, Yoshida M. Lumbar sagittal balance influences the clinical outcome after decompression and posterolateral spinal fusion for degenerative lumbar spondylolisthesis. Spine (Phila Pa 1976). 2002;27:59–64. [DOI] [PubMed] [Google Scholar]
- 28. Schwab FJ, Smith VA, Biserni M, Gamez L, Farcy JP Pagala M. Adult scoliosis: a quantitative radiographic and clinical analysis. Spine (Phila Pa 1976). 2002;27:387–392. [DOI] [PubMed] [Google Scholar]
- 29. Guigui P, Lambert P, Lassale B, Deburge A. Long-term outcome at adjacent levels of lumbar arthrodesis [in French]. Rev Chir Orthop Reparatrice Appar Mot. 1997;83:685–696. [PubMed] [Google Scholar]
- 30. Kumar MN, Baklanov A, Chopin D. Correlation between sagittal plane changes and adjacent segment degeneration following lumbar spine fusion. Eur Spine J. 2001;10:314–319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Mohapatra A, Bhandary B, Kartik Raj K. Functional outcome of patients with lumbar intervertebral disc herniation after minimally invasive microdiscectomy. IOSR J Dent Med Sci. 2017;16:35–39. [Google Scholar]