Abstract
Study Design:
Retrospective cohort study.
Objectives:
To assess whether the addition of L5-S1 anterior lumbar interbody fusion (ALIF) improves global sagittal alignment and fusion rates in patients undergoing multilevel spinal deformity surgery.
Methods:
Two-year radiographic outcomes, including lumbar lordosis, pelvic incidence, pelvic tilt, and T1 pelvic angle; hardware complications; and nonunion/pseudarthrosis rates were compared between patients who underwent lumbosacral fusion at 4 or more vertebral levels with and without L5-S1 ALIF between November 2003 and September 2016.
Results:
A total of 51 patients who underwent fusion involving a mean of 11.1 levels with minimum 2-year postoperative radiographic follow-up data were included. Patients who underwent L5-S1 ALIF did not have significant improvement in global sagittal alignment parameters and demonstrated a trend toward a higher rate of nonunion and hardware failure.
Conclusions:
L5-S1 ALIF did not confer significant benefit in terms of global sagittal alignment and fusion rates in patients undergoing multilevel lumbosacral fusion. Given these results and that L5-S1 ALIF is associated with increased surgical morbidity, surgeons should be judicious in including L5-S1 ALIF in large multilevel constructs.
Keywords: lumbar interbody fusion, pseudarthrosis, sagittal balance, sagittal alignment, deformity, scoliosis, degenerative, failed back surgery
Introduction
Adult spinal deformity (ASD) is common and is increasing in prevalence with an aging US population. ASD is estimated to affect >60% of elderly individuals,1 and its treatment imposes a large cost and resource burden on the US health care system. There was an estimated 138% increase in spinal fusions of 3 or more levels performed between 2004 and 2011,2 and a total of $86 billion is spent yearly on spine care in the United States.3
Treatment of ASD often requires surgical intervention to restore spinopelvic alignment parameters. Studies have shown that restoring global spinopelvic alignment, including lumbar lordosis (LL) and pelvic incidence (PI) mismatch (LL-PI) to within 11°, and pelvic tilt (PT) of <25°, correlates with improved patient-reported outcomes on the Oswestry Disability Index.4,5 Additionally, the T1 pelvic angle (T1PA) has been shown to correlate with improved patient outcomes, with a recommended goal of achieving T1PA of <14°.6
Various surgical techniques are used to correct spinopelvic alignment, including anterior lumbar interbody fusion at the L5-S1 level (L5-S1 ALIF). The proposed advantage of L5-S1 ALIF is enabling greater deformity correction through direct anterior spinal column lengthening as well as improved fusion through placement of a larger graft than possible through a posterior approach.7 However, there is a lack of data demonstrating whether addition of L5-S1 ALIF plays a significant role in achieving global sagittal balance in patients already undergoing multilevel corrective procedures for ASD. Understanding the efficacy of L5-S1 ALIF is particularly important because this procedure requires a ventral approach, increasing risk of intra-abdominal vascular injury, blood loss, and operative times.7-11 Given the lack of L5-S1 ALIF efficacy data, this study was conducted to assess whether addition of L5-S1 ALIF in ASD patients undergoing posterior instrumented fusion of ≥4 vertebral levels for ASD provided additional improvement in global sagittal alignment parameters or fusion rates.
Methods
Patient Population
After institutional review board approval was obtained, all patients who underwent lumbosacral fusion of ≥4 vertebral levels for ASD between November 2003 and September 2016 by our institution’s orthopedic spine surgery service were retrospectively identified. Patients were included if they met the following criteria: age ≥18 years, ASD resulting from degenerative scoliosis, preoperative full-length standing radiographs with an open L5-S1 disc space allowing for ALIF, and a minimum 2-year postoperative follow-up, including full-length spinal radiographs. Patients were excluded for missing data if they had previously undergone fusion to the sacropelvis or if they underwent lateral interbody fusion. Patients were subsequently divided into 3 groups based on surgical procedure. All patients underwent posterior spinal fusion (PSF), with the differences between patient groups being the anterior procedures performed. Group 1 (“Anterior”) underwent PSF in conjunction with multilevel anterior spinal surgery that did not include an L5-S1 ALIF. Group 2 (“ALIF”) underwent PSF with anterior spinal surgery that included L5-S1 ALIF. All L5-S1 ALIF procedures were performed using a femoral ring allograft. Group 3 (“Posterior”) underwent PSF only without an anterior approach. Specifically, group 3 underwent PSF to the pelvis without any additional anterior procedures, whereas group 1 underwent PSF to the pelvis with multilevel anterior procedures that did not include anterior fusion at the L5-S1 level.
Data Collection
Patient and surgical characteristics, including age at the time of surgery, gender, height, weight, body mass index (BMI), L5-S1 ALIF implant type, revision versus primary surgery, indication for surgery, and number of operated levels, were obtained from the electronic medical record. Preoperative and postoperative radiographs were reviewed to calculate the following parameters: thoracic kyphosis, L4-S1 LL, sagittal vertical axis, PI, PT, sacral slope, lumbopelvic angle, and T1PA. Initial postoperative radiographs were obtained at the 6-week postoperative visit. Additional radiographs obtained at the 2-year postoperative visit were assessed for both spinopelvic alignment parameters as well as evidence of nonunion/pseudarthrosis and hardware failure, defined as breakage of pedicle screws or rods.
Statistical Analysis
Descriptive statistics were utilized for baseline characteristics of each group. Differences in baseline characteristics between groups were analyzed using the Fisher exact test for gender, χ2 test for categorical variables, and analysis of variance (ANOVA) for all other variables. Average (mean) postoperative change values in radiographic parameters from baseline were compared between groups with ANOVA. Nonunion rates and hardware failure rates were calculated for each group, and differences between groups were assessed using logistic regression. Statistical analyses were performed using R version 3.5.1, with level of significance at P =.05.
Results
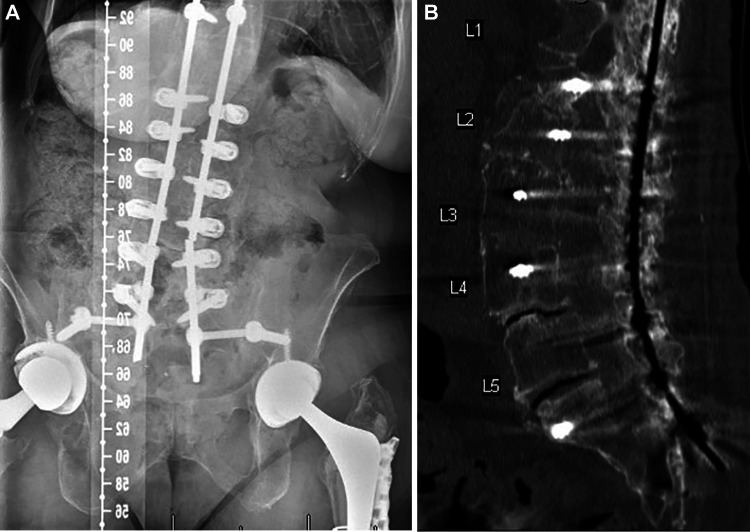
A total of 51 patients were included in this study, with an average age of 67 years. The majority (74.5%) of patients were female. Average height was similar to US population norms, at 1.7 m, and average weight was slightly less than the US population norms, at 73.3 kg. Average BMI was also slightly less than population norms, at 26.3 kg/m2.12 The surgical indication for all patients was degenerative scoliosis, with 1 patient in the Anterior group having postinfectious scoliosis with flat back deformity, 1 patient in the ALIF group having postpolio kyphoscoliosis, 2 patients in the Posterior group having pseudarthrosis, 1 patient in the Posterior group having degenerative scoliosis after prior multilevel laminectomies, 1 patient in the Posterior group with both isthmic spondylolisthesis and degenerative scoliosis, and 1 patient in the Posterior group having degenerative scoliosis and adjacent segment disease. Baseline patient characteristics and preoperative radiographic parameters of each group are shown in Table 1. No significant differences were observed in patient characteristics, revision versus primary surgery, or baseline spinopelvic alignment parameters, including L4-S1 lordosis, between the groups. Fusion procedures involved a mean of 11.1 vertebral levels, with no significant difference in the number of operative levels between groups (P = .08). Figures 1A and 1B are representative preoperative and 2-year postoperative images of a patient who underwent T10-ilium fusion with L2-3, L3-4, L4-5, and L5-S1 interbody fusion.
Table 1.
Baseline Characteristics of Each Patient Group.a
| Parameter | All Patients (n = 51) | Group 1 (n = 17) | Group 2 (n = 13) | Group 3 (n = 21) | P Valueb |
|---|---|---|---|---|---|
| Age (years) | 66.6 (8.5) | 66.5 (9.9) | 62.9 (7.7) | 69 (7.3) | .126 |
| Male, n (%) | 13 (25.5%) | 5 (29.4%) | 1 (7.7%) | 7 (33.3%) | .240 |
| Height (m) | 1.7 (0.1) | 1.7 (0.1) | 1.7 (0.2) | 1.7 (0.1) | .837 |
| Weight (kg, SD) | 73.3 (17.2) | 72.8 (15.9) | 74.8 (17.8) | 72.9 (18.7) | .950 |
| BMI (kg/m2, SD) | 26.3 (4.7) | 26.8 (4.9) | 26.6 (4.6) | 25.7 (4.9) | .733 |
| Levels fused, n (SD) | 11.1 (4.2) | 12.5 (3.2) | 11.7 (4.7) | 9.6 (4.3) | .08 |
| Revision surgery, n (%) | 12 (21.8%) | 2 (11.7%) | 3 (23.1%) | 7 (33.3%) | .084 |
| Lumbar lordosis L4-S1 (degrees) | 26.0 (10.9) | 28.2 (12.3) | 22.7 (10.3) | 26.6 (9.8) | .403 |
| Lumbar lordosis T12-S1 (degrees) | 30.2 (12.6) | 26.5 (12.8) | 31.5 (15.9) | 32.8 (8.5) | .682 |
| Pelvic incidence | 55.6 (15.3) | 55.5 (12.7) | 53.4 (14.3) | 57.7 (18.8) | .991 |
| LL-PI mismatch | 26.5 (14.9) | 29.0 (10.4) | 23.8 (17.1) | 26.3 (17.1) | .404 |
| Pelvic tilt | 29.9 (12.0) | 29.8 (9.2) | 32.0 (16.0) | 28.2 (10.9) | .952 |
| T1PA | 29.8 (12.2) | 30.8 (8.2) | 32.6 (15.8) | 23.6 (9.6) | .722 |
Abbreviations: ALIF, anterior lumbar interbody fusion; BMI, body mass index; LL, lumbar lordosis; PI, pelvic incidence; T1PA, T1 pelvic angle.
a Group 1 underwent anterior and posterior spinal fusion without L5-S1 ALIF, Group 2 underwent anterior and posterior spinal fusion including L5-S1 ALIF, and Group 3 underwent posterior spinal fusion only.
b P values for sex are from the Fisher exact test, and P values for all other variables are from ANOVA F-tests.
Figure 1.
A. Preoperative radiograph of a patient who underwent T10-ilium fusion with L2-3, L3-4, L4-5, and L5-S1 interbody fusion for degenerative scoliosis and spinal stenosis. The patient had previously undergone L4-5 anterior lumbar interbody fusion. B. Two-year postoperative radiograph of the patient in Figure 1A.
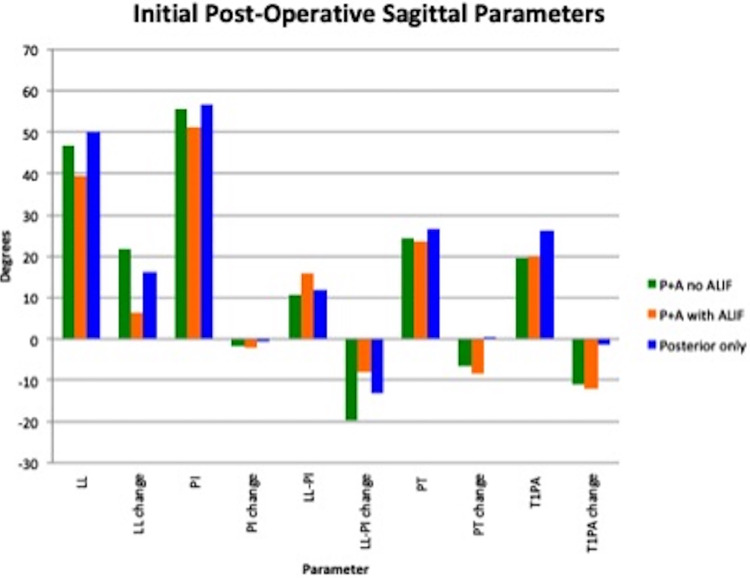
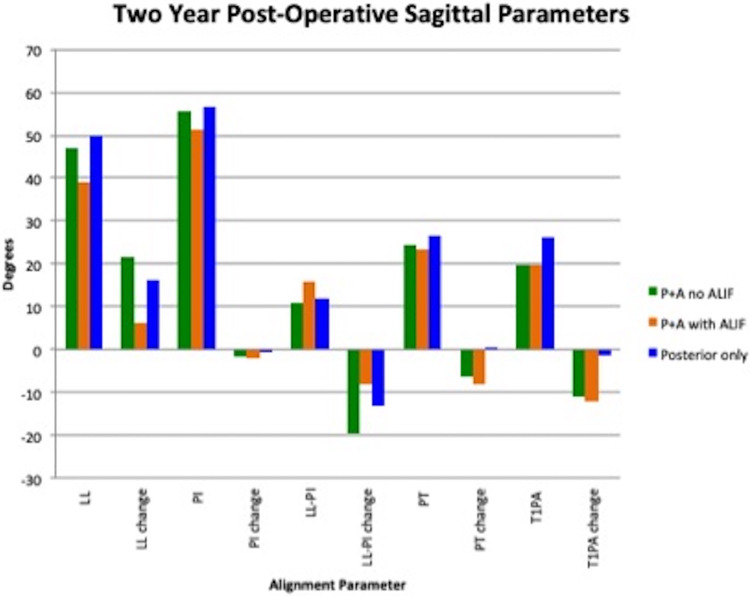
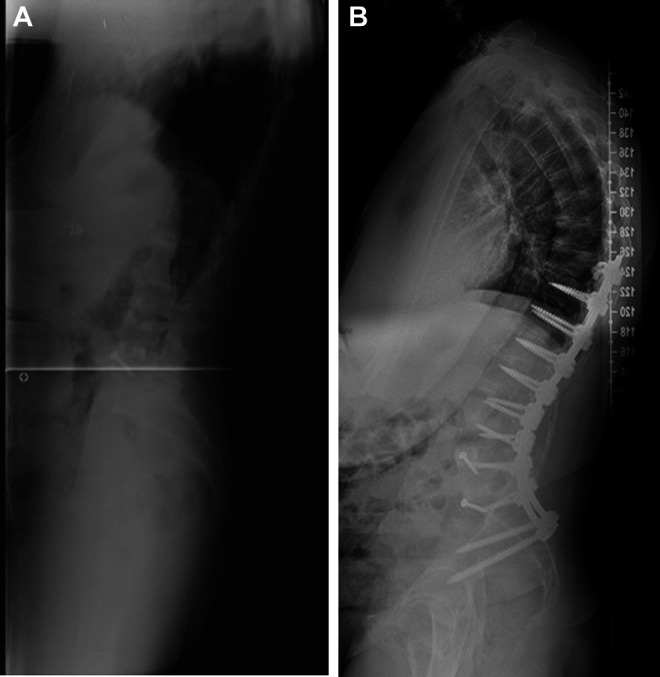
Table 2 lists alignment parameters obtained on initial postoperative radiographs. The group of patients who underwent ALIF had significantly lower initial postoperative LL relative to all other patients and significantly lower initial postoperative change in LL relative to patients who underwent anterior and posterior surgery without L5-S1 ALIF, but not patients who underwent PSF alone. The ALIF group also had the largest initial postoperative LL-PI mismatch and the smallest change in 2-year LL from baseline (Table 3); however, neither of these differences from the other groups was statistically significant. Similarly, no other initial or 2-year postoperative spinopelvic alignment parameters were significantly different between each of the groups. Comparisons between each group’s immediate postoperative and 2-year postoperative changes in alignment parameters are represented graphically in Figures 2 and 3. In regard to radiographic complications, there was no significant difference in rates of nonunion or hardware failure between the groups (Table 4). Figure 4A is an example of hardware failure (broken left rod) and nonunion in the ALIF group; Figure 4B shows subsequent computed tomography (CT) scan confirming L4-5 and L5-S1 pseudarthrosis in the same patient.
Table 2.
Initial Postoperative Sagittal Alignment Parameters, Including LL, PI, PT, and T1PA: The Change Value for Each Parameter Reflects Degree of Change From Preoperative Measurements.
| Parameter | Group 1 | Group 2 | Group 3 | P Value |
|---|---|---|---|---|
| LL postoperative | 46.8 (11.2) | 39.2 (9.3)a | 49.9 (9.1) | .043b |
| LL change | 21.6 (9.4) | 6.2 (19.0)c | 16.2 (10.6) | .030b |
| PI postoperative | 55.5 (10.6) | 51.3 (14.6) | 56.5 (9.4) | .512 |
| PI change | −1.6 (10.3) | −2.1 (13.8) | −0.5 (22.3) | .970 |
| LL-PI postoperative | 10.8 (12.0) | 15.8 (13.6) | 11.8 (8.0) | .498 |
| LL-PI change | −19.6 (10.0) | −8.1 (17.1) | −13.1 (20.9) | .232 |
| PT postoperative | 24.3 (8.6) | 23.5 (12.2) | 26.6 (9.1) | .752 |
| PT change | −6.5 (8.4) | −8.2 (10.4) | 0.2 (13.0) | .149 |
| T1PA postoperative | 19.6 (6.5) | 19.8 (13.9) | 26.3 (9.6) | .530 |
| T1PA change | −10.9 (11.1) | −12.0 (11.5) | −1.4 (16.8) | .117 |
Abbreviations: LL, lumbar lordosis; PI, pelvic incidence; PT, pelvic tilt; T1PA, T1 pelvic angle.
a Group 2 significantly lower than groups 1 and 3.
b Significant at level P =.05.
c Group 2 significantly lower than group 1, but not group 3.
Table 3.
Two-Year Postoperative Sagittal Alignment Parameters, Including LL, PI, PT, and T1PA: the Change Value for Each Parameter Reflects Degree of Change From Preoperative Measurements.
| Parameter | Group 1 | Group 2 | Group 3 | P Value |
|---|---|---|---|---|
| LL postoperative | 42.3 (11.3) | 37.3 (12.4) | 39.4 (20.3) | .702 |
| LL change | 15.1 (14.8) | 4.5 (13.5) | 13.4 (15.6) | .165 |
| PI postoperative | 53.6 (8.7) | 54.1 (12.4) | 52.2 (10.0) | .891 |
| PI change | −3.3 (14.4) | 1.8 (12.7) | −4.9 (15.7) | .462 |
| LL-PI postoperative | 14.4 (8.4) | 15.7 (15.0) | 18.7 (12.6) | .639 |
| LL-PI change | −15.3 (9.2) | −8.2 (17.5) | −11.7 (18.4) | .490 |
| PT postoperative | 25.9 (7.7) | 26.1 (10.5) | 25.0 (8.5) | .946 |
| PT change | −5.1 (10.6) | −4.3 (7.6) | −1.25 (10.0) | .564 |
| T1PA postoperative | 22.0 (.4) | 22.0 (12.7) | 23.4 (8.9) | .916 |
| T1PA change | −8.4 (9.7) | −8.8 (10.9) | −2.0 (12.5) | .248 |
Abbreviations: LL, lumbar lordosis; PI, pelvic incidence; PT, pelvic tilt; T1PA, T1 pelvic angle.
Figure 2.
Initial postoperative sagittal radiographic parameters in patients who underwent posterior and anterior spinal fusion without L5-S1 anterior lumbar interbody fusion (ALIF; P+A no ALIF), patients who underwent posterior and anterior spinal fusion including L5-S1 ALIF (P+A with ALIF), and patients who underwent posterior spinal fusion alone (posterior only). Radiographic parameters include lumbar lordosis (LL), pelvic incidence (PI), pelvic tilt (PT), and T1 pelvic angle (T1PA). The change value for each parameter reflects degree of change from preoperative measurements.
Figure 3.
Two-year postoperative sagittal radiographic parameters in patients who underwent posterior and anterior spinal fusion without L5-S1 anterior lumbar interbody fusion (ALIF; P+A no ALIF), patients who underwent L5-S1 ALIF (P+A with ALIF), and patients who underwent posterior spinal fusion alone (posterior only). Radiographic parameters include lumbar lordosis (LL), pelvic incidence (PI), pelvic tilt (PT), and T1 pelvic angle (T1PA). The change value for each parameter reflects degree of change from preoperative measurements.
Table 4.
Comparison of Complication Rates, Including Nonunion and Hardware Breakage Rates as Noted on Full-Length Spine Standing Films, Between Each Group Included in the Study.
| Parameter | Group 1 (n = 17) | Group 2 (n = 13) | Group 3 (n = 21) | Group 1/Group 2 | Group 3/Group 1 | Group 3/Group 2 | |||
|---|---|---|---|---|---|---|---|---|---|
| Odds Ratio | P | Odds Ratio | P | Odds Ratio | P | ||||
| Nonunion, n (%) | 2 (11.8%) | 3 (23.1%) | 3 (14.3%) | 2.2 | .417 | 1.2 | .819 | 0.6 | .517 |
| Rod breakage, n (%) | 2 (11.8%) | 2 (15.4%) | 1 (4.8%) | 1.4 | .773 | 0.4 | .440 | 0.3 | .314 |
Figure 4.
A. Two-year postoperative follow-up imaging in a patient who underwent L5-S1 anterior lumbar interbody fusion (ALIF) in combination with posterior spinal fusion, demonstrating L4-5 and L5-S1 nonunion and breakage of the left rod at the L4-5 level. B. Two-year postoperative lumbar spine computed tomography scan from the patient in Figure 4A, confirming L4-5 and L5-S1 nonunion.
Discussion
Restoration of sagittal balance is crucial for optimizing clinical outcomes in patients with ASD.4-6,13 With this study, we aimed to assess whether addition of L5-S1 ALIF, with the theoretical potential of augmenting LL,7 would improve correction of spinopelvic parameters in patients undergoing multilevel surgery for ASD. We also aimed to assess whether L5-S1 ALIF in conjunction with PSF would improve fusion rates in multilevel constructs spanning greater than 4 vertebral segments. Importantly, all patients had similar preoperative radiographic parameters, including L4-S1 lordosis, and underwent fusion involving a similar number of levels. Additionally, the indication for surgery in all patients was degenerative scoliosis, and there was no significant difference between groups in the proportion of patients undergoing primary versus revision surgery. Our results showed that patients who underwent L5-S1 ALIF achieved significantly less correction of LL on initial postoperative radiographic assessment as compared with patients who underwent anterior and posterior correction of ASD without L5-S1 ALIF and patients who underwent surgery from a posterior approach only. The finding that patients who underwent anterior procedures and PSF without L5-S1 ALIF achieved greater sagittal correction than patients who underwent anterior procedures plus L5-S1 ALIF in conjunction with PSF may be related to stiffness of patients’ curves. Addition of L5-S1 ALIF also did not provide relative improvement in correction of other key spinopelvic parameters, including LL-PI mismatch, PT, and T1PA at initial postoperative and 2-year postoperative radiographic assessment. Finally, patients who underwent L5-S1 ALIF exhibited slightly increased odds of nonunion and hardware failure at the 2-year postoperative time point.
Although L5-S1 ALIF has demonstrated utility in increasing LL and improving sagittal balance in shorter constructs spanning ≤3 levels,7 results of our study suggest that addition of L5-S1 ALIF may be of lesser utility in patients requiring larger constructs for correction of ASD. All patients in our study had similar preoperative sagittal alignment parameters, yet those who underwent L5-S1 ALIF to augment additional anterior spinal fusion achieved a lesser, albeit nonsignificant, degree of improvement in their sagittal balance at the initial and 2-year postoperative time points. Results of this study also suggest that L5-S1 ALIF may have lower efficacy in promoting fusion in large fusion constructs because patients who underwent L5-S1 ALIF did not exhibit improved rates of nonunion/pseudarthrosis or hardware failure.7-10
Previous studies have shown ALIF to provide improved correction of LL relative to posterior surgery only at the L4-5 and L5-S1 levels in patients undergoing surgery for 3 or fewer levels,7 whereas a meta-analysis comparing ALIF with transforaminal lumbar interbody fusion showed L4-5 and L5-S1 ALIF to be superior in restoring LL.14 In contrast, patients in our study undergoing longer fusions involving a mean of 11.1 vertebral levels did not demonstrate improved postoperative sagittal alignment parameters with addition of L5-S1 ALIF. The lack of additional improvement in sagittal parameters with L5-S1 ALIF is likely influenced by the extent of surgery in our study because all patients underwent surgery at 4 or more vertebral levels. As mentioned, patients who underwent L5-S1 ALIF may also have had stiffer curves, reducing the amount of overall sagittal correction they were likely to achieve regardless of the intervention they received.
Our study also evaluated the impact of L5-S1 ALIF on fusion rates in multilevel constructs spanning 4 or more levels. There is currently no consensus on the addition of L5-S1 ALIF to improve fusion rates. However, our results do agree with prior studies demonstrating no additional benefit from L5-S1 ALIF increasing construct stiffness. A cadaveric biomechanical study by Dahl et al15 found that while interbody fusion helped maintain disc height, it did not significantly restrict intervertebral body motion relative to posterior instrumentation. Similarly, Schroeder et al16 found that addition of bilateral posterior instrumentation negated any additional fusion benefit from L5-S1 ALIF in patients undergoing surgery for 1- or 2-level degenerative conditions, whereas the biomechanical cadaver study by Lee et al17 found that addition of L5-S1 ALIF to long constructs from L2-S1 and T10-S1 did not significantly decrease range of motion relative to posterior iliac screw fixation.
Results of our study suggest that L5-S1 ALIF is of limited utility in patients undergoing correction of ASD over 4 or more vertebral levels because L5-S1 ALIF showed no additional benefit in correction of sagittal balance or improvement of fusion rates. Based on these results, we recommend judicious use of L5-S1 ALIF in multilevel correction of ASD, especially given inherent risks of the procedure, including vascular complications, increased operating time, and elevated blood loss.7-11
To our knowledge, ours is the first study to specifically investigate the efficacy of L5-S1 ALIF in improving sagittal alignment parameters and fusion rates in patients undergoing ASD correction with large constructs spanning 4 or more vertebral segments. Additional strengths include use of a regression analysis for evaluating complication rates between groups and utilizing data from procedures performed by multiple surgeons, which increases generalizability of our results. Our stringent inclusion criteria, including 2-year radiographic follow-up and our requirement that all patients have a diagnosis of degenerative scoliosis, is an important strength of our study. However, the strict inclusion requirements also severely limited the sample size despite this study being performed at a high-volume ASD center. Additional limitations of the study include single-center data, lack of clinical outcomes data reflecting disability and quality of life, and lack of CT data in all patients to confirm spinal fusion. Additionally, this was not a randomized trial. Instead, experienced spinal deformity surgeons selected procedures on a case-by-case basis, potentially biasing inclusion of L5-S1 ALIF toward cases with the greatest risk of nonunion and patients with stiffer curves who were less likely to achieve improved sagittal balance regardless of the procedure performed.
In conclusion, addition of L5-S1 ALIF to multilevel procedures spanning 4 or more vertebral segments for correction of ASD was not found to improve sagittal alignment or fusion rates. Therefore, L5-S1 ALIF should be used cautiously when planning ASD corrective procedures involving large constructs of 4 or more vertebral levels, especially given its potential for increased surgical morbidity. Future studies may further investigate specific indications for L5-S1 ALIF in large constructs, such as implications of curve stiffness.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Joseph B. Wick, MD  https://orcid.org/0000-0002-0030-0367
https://orcid.org/0000-0002-0030-0367
References
- 1. Schwab F, Dubey A, Gamez L, et al. Adult scoliosis: prevalence, SF-36, and nutritional parameters in an elderly volunteer population. Spine (Phila Pa 1976). 2005;30:1082–1085. [DOI] [PubMed] [Google Scholar]
- 2. Waldrop R, Cheng J, Devin C, McGirt M, Fehlings M, Berven S. The burden of spinal disorders in the elderly. Neurosurgery. 2015;77(suppl 4):S46–S50. [DOI] [PubMed] [Google Scholar]
- 3. Arutyunyan GG, Angevine PD, Berven S. Cost-effectiveness in adult spinal deformity surgery. Neurosurgery. 2018;83:597–601. [DOI] [PubMed] [Google Scholar]
- 4. Schwab F, Patel A, Ungar B, Farcy JP, Lafage V. Adult spinal deformity-postoperative standing imbalance: how much can you tolerate? An overview of key parameters in assessing alignment and planning corrective surgery. Spine (Phila Pa 1976). 2010;35:2224–2231. [DOI] [PubMed] [Google Scholar]
- 5. Schwab FJ, Blondel B, Bess S, et al. Radiographical spinopelvic parameters and disability in the setting of adult spinal deformity: a prospective multicenter analysis. Spine (Phila Pa 1976). 2013;38:E803–E812. [DOI] [PubMed] [Google Scholar]
- 6. Protopsaltis T, Schwab F, Bronsard N, et al. TheT1 pelvic angle, a novel radiographic measure of global sagittal deformity, accounts for both spinal inclination and pelvic tilt and correlates with health-related quality of life. J Bone Joint Surg Am. 2014;96:1631–1640. [DOI] [PubMed] [Google Scholar]
- 7. Hsieh PC, Koski TR, O’Shaughnessy BA, et al. Anterior lumbar interbody fusion in comparison with transforaminal lumbar interbody fusion: implications for the restoration of foraminal height, local disc angle, lumbar lordosis, and sagittal balance. J Neurosurg Spine. 2007;7:379–386. [DOI] [PubMed] [Google Scholar]
- 8. Crandall DG, Revella J. Transforaminal lumbar interbody fusion versus anterior lumbar interbody fusion as an adjunct to posterior instrumented correction of degenerative lumbar scoliosis: three year clinical and radiographic outcomes. Spine (Phila Pa 1976). 2009;34:2126–2133. [DOI] [PubMed] [Google Scholar]
- 9. Inamasu J, Guiot BH. Vascular injury and complication in neurosurgical spine surgery. Acta Neurochir (Wien). 2006;148:375–387. [DOI] [PubMed] [Google Scholar]
- 10. Sasso RC, Best NM, Mummaneni PV, Reilly TM, Hussain SM. Analysis of operative complications in a series of 471 anterior lumbar interbody fusion procedures. Spine (Phila Pa 1976). 2005;30:670–674. [DOI] [PubMed] [Google Scholar]
- 11. Wood KB, Devine J, Fischer D, Dettori JR, Janssen M. Vascular injury in elective anterior lumbosacral surgery. Spine (Phila Pa 1976). 2010;35(9, suppl):S66–S75. [DOI] [PubMed] [Google Scholar]
- 12. Fryar CD, Kruszon-Moran D, Gu Q, Ogden CL. Mean body weight, height, waist circumference, and body mass index among adults: United States, 1999-2000 through 2015-2016. Natl Health Stat Report. 2018;(122):1–16. [PubMed] [Google Scholar]
- 13. Korovessis P, Repantis T, Papazisis Z, Iliopoulos P. Effect of sagittal spinal balance, levels of posterior instrumentation, and length of follow-up on low back pain in patients undergoing posterior decompression and instrumented fusion for degenerative lumbar spine disease: a multifactorial analysis. Spine (Phila Pa 1976). 2010;35:898–905. [DOI] [PubMed] [Google Scholar]
- 14. Ajiboye RM, Alas H, Mosich GM, Sharma A, Pourtaheri S. Radiographic and clinical outcomes of anterior and transforaminal lumbar interbody fusions: a systematic review and meta-analysis of comparative studies. Clin Spine Surg. 2018;31:E230–E238. [DOI] [PubMed] [Google Scholar]
- 15. Dahl BT, Harris JA, Gudipally M, Moldavsky M, Khalil S, Bucklen BS. Kinematic efficacy of supplemental anterior lumbar interbody fusion at lumbosacral levels in thoracolumbosacral deformity correction with and without pedicle subtraction osteotomy at L3: an in vitro cadaveric study. Eur Spine J. 2017;26:2773–2781. [DOI] [PubMed] [Google Scholar]
- 16. Schroeder GD, Kepler CK, Millhouse PW, et al. L5/S1 fusion rates in degenerative spine surgery: a systematic review comparing ALIF, TLIF, and axial interbody arthrodesis. Clin Spine Surg. 2016;29:150–155. [DOI] [PubMed] [Google Scholar]
- 17. Lee BS, Walsh KM, Healy AT, et al. Biomechanics of L5/S1 in long thoracolumbosacral constructs: a cadaveric study. Global Spine J. 2018;8:607–614. [DOI] [PMC free article] [PubMed] [Google Scholar]