Abstract
Study Design:
Longitudinal cohort study with 13-year follow-up.
Objective:
To assess whether long-term disability is associated with baseline degenerative magnetic resonance imaging (MRI) findings in patients with low back pain (LBP).
Methods:
In 2004-2005, patients aged 18 to 60 years with chronic LBP were enrolled in a randomized controlled trial and lumbar MRI was performed. Patients completed the Roland-Morris Disability Questionnaire (RMDQ) and the LBP Rating Scale, at baseline and 13 years after the MRI. Multivariate regression analysis was performed with 13-year RMDQ as the dependent variable and baseline disc degeneration (DD, Pfirrmann grade), Modic changes (MC), facet joint degeneration (FJD, Fujiwara grade) smoking status, body mass index, and self-reported weekly physical activity at leisure as independent variables.
Results:
Of 204 patients with baseline MRI, 170 (83%) were available for follow-up. Of these, 88 had Pfirrmann grade >III (52%), 67 had MC (39%) and 139 had Fujiwara grade >2 (82%) on at least 1 lumbar level. Only MC (β = −0.15, P = .031) and weekly physical activity at leisure (β = −0.51, P < .001) were significantly, negatively, associated with 13-year RMDQ-score (R2 = 0.31).
Conclusion:
DD and FJD were not associated with long-term disability. Baseline MC and weekly physical activity at leisure were statistically significantly associated with less long-term disability.
Keywords: Modic changes, disability, low back pain (LBP), degeneration, MRI, long-term follow-up
Introduction
Since the first reports on human magnetic resonance imaging (MRI) in 1977, there has been a vast advancement in its use and functions.1 For patients suffering from back pain and its associated disability, it has become a commonly used diagnostic imaging modality. Whereas certain imaging findings such as nerve impingement and severe canal narrowing has shown a strong association with patient-reported outcomes (PROs), other signs of degeneration found on MRI have a more questionable clinical relevance.2-7 Disc degeneration (DD), Modic changes (MC), and facet joint degeneration (FJD) are all imaging findings and possible causes of LBP.5,8-10 Several different grading systems have been utilized to classify the severity of these degenerative changes. The Pfirrmann classification system has been validated, with excellent inter- and intraobserver agreement, and is widely used to classify DD in 5 grades, Pfirrmann grade I (normal) to V (most severe).11,12
MC, also termed vertebral endplate signal changes (VESC), are endplate and adjacent vertebral body marrow changes visible on MRI. They have been histologically described, and MRI classified into 3 different types, MC 1 to 3.13,14 Their presence, size, location, and the MRI inter- and intraobserver reliability, substantial to an almost perfect agreement, has been validated across studies.15,16
Facet joint changes and degeneration is a common feature, which can be graded on both oblique radiographs, computed tomography (CT) scan, and MRI.9,17 The radiographic assessment of lumbar facet joints is possible through 12 different grading systems.18 The reliability of these systems has been evaluated with varying inter- and intraobserver agreement.18,19 The standard MRI grading system used for lumbar FJD, with an almost perfect interobserver agreement, was developed by Fujiwara et al.9,18 The system developed by Fujiwara classifies facet joint changes into grade 1 (normal) to grade 4 (severe degeneration).9
Several studies have focused on these degenerative imaging findings in the spine and their clinical relevance.3,20,21 Few studies, however, have examined the long-term association between such findings and spine-related disability.22
The aim of the study was to assess whether baseline MRI findings indicating degeneration are associated with long-term disability in patients with LBP.
Materials and Methods
This is an observational cohort study with 13-year follow-up of patients with chronic LBP. The cohort was originally recruited for a randomized control trial (RCT) conducted between 2004 and 2005. The cohort and original study details have been described in previous studies.7,23
Of the original 207 patients in the RCT, 204 had a lumbar MRI performed at baseline. Based on these MRIs, patients were, for the current study, described regarding 3 different radiological parameters:
MC as described by Modic et al, any type on any lumbar level.13,14,25
FJD defined by Fujiwara grade >2 on any lumbar level.9
Study participants completed questionnaires with PRO’s at baseline and at 13-year follow-up, including the Roland-Morris Disability Questionnaire (RMDQ), and the LBP Rating Scale for activity limitations survey (RS).26-28 Demographic data including smoking, body mass index (BMI), and weekly physical activity at leisure (PA) was also recorded both at baseline and at 13-year follow-up. Information regarding antibiotic use, defined as any received course of antibiotics, and spine surgery during the 13-year period was obtained through the follow-up questionnaire.
MRI Evaluation
All patients underwent a low-tesla MRI of the lumbar region (0.2-T MRI system, Siemens Open Viva). The use of low-field MRI was widely used in the inclusion period from 2004 to 2005. Excellent reliability between low- and high-field MRI has been demonstrated for lumbar degenerative changes.29 MRIs were evaluated by an experienced musculoskeletal radiologist using a standardized evaluation protocol and unaware of the clinical status of the individual patient.23 The MRI description was not available to included patients and did not influence treatment.
Ethical Considerations, Approvals, and Registration
Protocol, data collection, and study ethics were approved by the National Data Protection Agency and The Regional Committees on Health Research Ethics (reference number: S-20 172 000-77).
Statistical Analyses
All analyses were performed using IBM SPSS version 24. Patients with a baseline MRI, baseline and 13-year follow-up questionnaires were included in the analysis. Multivariate linear regression analysis was performed with 13-year RMDQ and RS as dependent variables and DD, MC, FJD as independent variables. Demographic data at 13-year, including smoking, BMI, and PA was included as covariates in the regression models. The association between 13-year RMDQ and the independent variables was evaluated by the standard β coefficient. The goodness-of-fit and explained variation were evaluated by R2.
Results
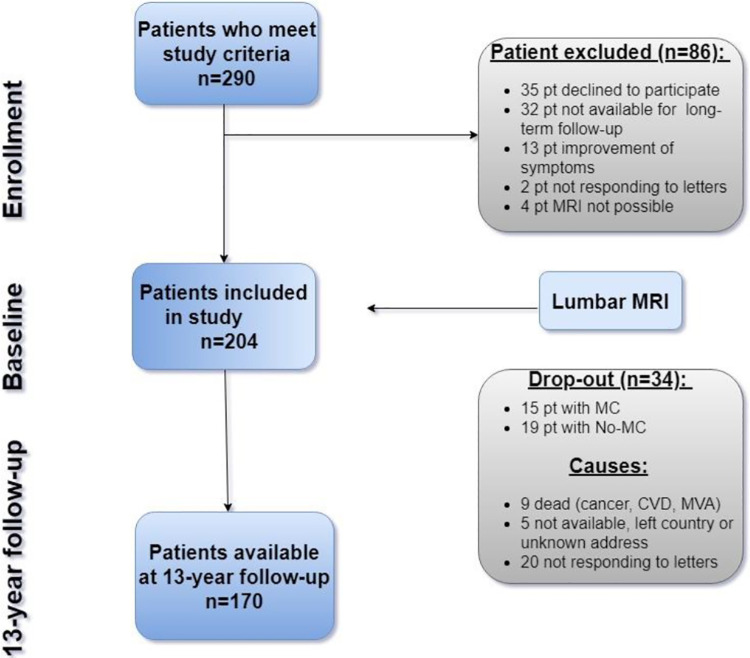
A total of 290 patients fulfilled the criteria for inclusion in the original study, 207 were enrolled with 204 having lumbar MRI and being eligible for inclusion in the current study (Figure 1). Of these, 170 patients (83%) completed their questionnaire at 13 years, 88 had DD (52%), 67 had MC (39%), and 139 had FJD (82%) on their baseline MRIs. Of the 34 dropouts, no difference was seen regarding baseline data on the distribution of spine degeneration on MRI. Demographics for 13-year follow-up data are described in Table 1.
Figure 1.
Study enrollment and follow-up.
Table 1.
Demographic Data at 13-Year Follow-up.
| No. of patients, N | 170 |
| Females, n (%) | 92 (54) |
| Weight, kg, mean (SD) | 84.3 (18.4) |
| Body mass index, kg/m2, mean (SD) | 27.3 (5.0) |
| Age, years, mean (range) | 53.3 (31-70) |
| Smokers, n (%) | 39 (24) |
| Married, n (%) | 103 (61) |
| Spine surgery after MRI, n (%) | 18 (11) |
| Antibiotics use, n (%) | 110 (65) |
In patients with MC, MC-1 was present in 75%, MC-2 in 24%, MC-3 in <1% of patients, and mixed (MC-1 and MC-2) in 6% of patients. Baseline and follow-up PROs for the entire cohort are presented in Table 2.
Table 2.
Baseline and 13-Year Follow-up.a
| No. of patients | |
| Baseline | 204 |
| 13-year follow-up | 170 |
| Roland-Morris Disability Questionnaire (disability, 0-23 score) | |
| Baseline | 12.5 [4.5] |
| 13-year follow-up | 8.5 [6.4] |
| Low Back Pain Rating Scale for activity limitation (activity limitation, 0-30 score) | |
| Baseline | 13.6 [4.7] |
| 13-year follow-up | 9.5 [5.9] |
| Low back pain (Numeric Rating Scale) | |
| Baseline | 6.2 [1.4] |
| 13-year follow-up | 4.5 [2.6] |
| Leg pain (Numeric Rating Scale) | |
| Baseline | 2.1 [2.1] |
| 13-year follow-up | 3.0 [2.9] |
| Sick leave due to low back pain (days past year) | |
| Baseline | — |
| 13-year follow-up | 16.0 [48] |
| Back pain medication consumption regularly, (%) | |
| Baseline | 64 (65%) |
| 13-year follow-up | 50 (56%) |
| Physical activity level at leisure (group 1-4) | |
| Baseline | 2.0 [0.7] |
| 13-year follow-up | 2.1 [0.7] |
a Central tendency described as mean with standard deviation given in brackets.
Both MC and PA at leisure were found to be statistically significantly negatively associated with 13-year RMDQ-scores, R2 = 0.31 with standard β coefficients of 0.15 for MC (P = .031) and −0.51 for PA (P < .001). Neither DD (β = 0.060, P = .406) nor FJD (β = −0.017, P = .801) showed any statistically significant association with long-term disability. Smoking status (β = 0.102, P = .127) and BMI (β = 0.092, P = .179) also showed no significant association with the RMDQ scores.
Similar results were found for 13-year RS with R2 = 0.26 and β of −0.18 for MC (P = .015) and −0.45 for PA (P < .001). DD, FJD, smoking status, and BMI did not significantly affect long-term RS.
Disability measured by RMDQ and RS improved over time, resulting in less disability at 13-year follow-up compared with baseline. LBP also decreased from 6.2 (Numeric Rating Scale [NRS]) to 4.5 (NRS) over the 13-year time period. Leg pain increased slightly, from 2.1 (NRS) to 3.0 (NRS) at final follow-up. The consumption of back pain medication decreased from 65% of the group using regularly at baseline to 56% of the group using regularly at 13-year follow-up. There was no change in PA over the 13-year span.
Discussion
Lumbar MRI scans are used to identify the possible causes of back pain, to guide treatment, and as a tool to provide short- and long-term prognosis. In this study, the association between long-term disability and baseline MRI findings was examined in chronic LBP patients. Degenerative changes were found to be present in the majority of patients—DD and FJD in, respectively, 52% and 82% of all patients. Similar results have been found in previous studies of MRI degeneration in patients with LBP.3,10,30
Neither DD at baseline, defined as Pfirrmann grade >III on any lumbar level, nor FJD, defined as Fujiwara grade >2 on any lumbar level, was associated with disability at long-term follow-up. Similar results on the prevalence and limited or lacking association with back pain and disability have been documented in cross-sectional studies and studies with shorter follow-up periods.3-5,8,31,32
Subgroup analysis of the cohorts stratified by imaging findings was not performed in this study, as there was a substantial overlap of patients with 2 or all 3 of the possible imaging findings denoting degeneration. It would be difficult to isolate patients with DD without FJD as well as patients with MC without DD. This overlap of imaging findings has been described, in particular in relation to MC and DD, previously.7,14,25,33
Degenerative disc disease is a commonly used diagnosis and possible indication for spinal fusion in patients with chronic back pain.31,34 However, the term degenerative disc disease is used broadly across studies and should be avoided unless thoroughly defined. In this study, the Pfirrmann and Fujiwara classification systems were used to grade the degenerative MRI findings of the intervertebral discs and the facet joints, respectively.
For DD, the Pfirrmann classification is the most validated and second most used for LBP patients across studies.11,12,24,26 MC was originally described based not only on MRI changes but also histological changes examined in a few cases by Modic et al.13,14,25 Although it is possible to add information, including size, location, distribution, and so on, to the MC description; it is still the original MC classification of MC type 1 to 3 that is being utilized and validated across studies.8,13,15,16,35,36 It has been questioned whether the classification of MC is related to the MRI field strength—with low-field MRI scanners (defined by fields ≤0.3 T) showing an increased number of MC type-1 compared with high-field MRI (defined by fields ≥1.0 T) scanners showing an increased number of MC type-2.37
In general, excellent reliability between low- and high-field MRI has been demonstrated for lumbar degenerative findings, including disc herniation and lateral stenosis.29 For FJD, the classification systems suffer from certain limitations. Degeneration including osteoarthritis has been described on different imaging systems, including X-rays, CT, and MRI scans.18,19 Some of the grading systems have been adapted from CT to MRI but with limited validation in inter- and intraobserver studies.9,17-19,38 The Fujiwara classification has been examined and found to be reproducible in grading FJD in MRI analysis.9,18
Limitations of this study include possible confounding in terms of different exposure, treatment, and psychosocial factors of the individual patients within the cohort. There could be a possible bias with a single-rater radiologist; however, previous studies have shown excellent interrater reliability and therefore a reliability assessment was not included in the present study.11,12,15,16,18
The primary strengths of this study include a high follow-up rate of 83% at 13 years and the inclusion of relevant potential confounders in the statistical analysis, BMI, smoking, and so on. Also, no patients underwent long-term antibiotic courses aimed at eradicating possible bacterial agents within the disc, including Propionibacterium acnes.39,40
The findings in this study are in accordance with previous studies, showing that lumbar degenerative changes visualized by MRI are common and are to be expected to a certain degree in all mature individuals.3,5,8,17,41-45 However, this cohort study of patients with chronic LBP found more severe degeneration on MRI compared with what is found in cross-sectional population-based MRI studies.3-5,10,30,33 The clinical relevance of these results is the prognostic value at long-term follow-up of patients with LBP. Some studies with short-term follow-up and cross-sectional studies have found an association between MC in particular type-1, severe disc degeneration, and to some degree facet joint degeneration, with LBP.31,32,46,47 In this study, no association was found between baseline MRI findings and 13-year disability in LBP patients with severe DD or FJD. This highlights the limited prognostic value of a single baseline MRI scan on long-term disability.
MC present at baseline was predominantly MC type-1, 75%, this finding was associated with statistically significant less long-term disability in the cohort.7 These results are in contrast to short-term studies.8,33,39,47 Several studies have investigated the effect of both surgical and antibiotic treatment of patients with MC and LBP.39,48,49 The relevance of such invasive treatments or prolonged antibiotic courses of patients with MC can be questioned. In particular, if the MRI findings are not associated with a worse prognosis at long-term follow-up in patients not receiving treatment.22
It is striking that in a between-individual view, DD and MC are rather highly associated with LBP, whereas a longitudinal view within individuals does not show such an association.7,22,45,50 One hypothesis could be that the degenerative process of the disc, including the gradually fibrotic nuclear pulposus and annulus, reduces the risk of disc penetration and thereby activation of peripheral nerve fibers within the disc.
In future studies, it would be interesting (a) to verify the histologic and MRI transgression of MC over time including the timeline and clinical relevance; (b) to further examine the prognostic properties of baseline degeneration found on MRI combined with clinical findings, on long-term PROs in patients with LBP; and (c) to evaluate the long-term outcomes in patients with degeneration on MRI and LBP not undergoing treatment.
Conclusion
Degeneration on MRI was a frequent finding in patients with LBP. None of the MRI changes suggesting degeneration were associated with a worse outcome at 13-year follow-up. Baseline MC was associated with statistically significant less long-term disability.
We encourage further studies to validate these findings and assess the long-term clinical consequences of abstaining from treatment in patients with LBP.
Acknowledgments
All baseline data have kindly been provided to us by Pia Havn Sørensen, who conducted the original RCT. Radiologist Joan Sørensen described all the original MRI scans.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was supported by a grant received from the University of Southern Denmark (SDU).
ORCID iD: Peter Muhareb Udby, MD  https://orcid.org/0000-0001-9675-9123
https://orcid.org/0000-0001-9675-9123
Søren Ohrt-Nissen, MD, PhD  https://orcid.org/0000-0002-8234-9948
https://orcid.org/0000-0002-8234-9948
Stig Brorson, MD, PhD, DmSci  https://orcid.org/0000-0001-5337-758X
https://orcid.org/0000-0001-5337-758X
Leah Y. Carreon, MD, MSc  https://orcid.org/0000-0002-7685-9036
https://orcid.org/0000-0002-7685-9036
References
- 1. Edelman RR. The history of MR imaging as seen through the pages of radiology. Radiology. 2014;273(2 suppl):S181–S200. doi:10.1148/radiol.14140706 [DOI] [PubMed] [Google Scholar]
- 2. Teraguchi M, Yoshimura N, Hashizume H, et al. The association of combination of disc degeneration, end plate signal change, and Schmorl node with low back pain in a large population study: the Wakayama Spine Study. Spine J. 2015;15:622–628. doi:10.1016/j.spinee.2014.11.012 [DOI] [PubMed] [Google Scholar]
- 3. Steffens D, Hancock MJ, Maher CG, Williams C, Jensen TS, Latimer J. Does magnetic resonance imaging predict future low back pain? A systematic review. Eur J Pain. 2014;18:755–765. doi:10.1002/j.1532-2149.2013.00427.x [DOI] [PubMed] [Google Scholar]
- 4. Herlin C, Kjaer P, Espeland A, et al. Modic changes—their associations with low back pain and activity limitation: a systematic literature review and meta-analysis. PLoS One. 2018;13:e0200677. doi:10.1371/journal.pone.0200677 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kovacs FM, Arana E, Royuela A, et al. Disc degeneration and chronic low back pain: an association which becomes nonsignificant when endplate changes and disc contour are taken into account. Neuroradiology. 2014;56:25–33. doi:10.1007/s00234-013-1294-y [DOI] [PubMed] [Google Scholar]
- 6. Kim YU, Kong YG, Lee J, et al. Clinical symptoms of lumbar spinal stenosis associated with morphological parameters on magnetic resonance images. Eur Spine J. 2015;24:2236–2243. doi:10.1007/s00586-015-4197-2 [DOI] [PubMed] [Google Scholar]
- 7. Udby PM, Bendix T, Ohrt-Nissen S, et al. Modic changes are not associated with long-term pain and disability—a cohort study with 13-year follow-up. Spine (Phila Pa 1976). 2019;44:1186–1192. doi:10.1097/BRS.0000000000003051 [DOI] [PubMed] [Google Scholar]
- 8. Jensen TS, Karppinen J, Sorensen JS, Niinimäki J, Leboeuf-Yde C. Vertebral endplate signal changes (Modic change): a systematic literature review of prevalence and association with non-specific low back pain. Eur Spine J. 2008;17:1407–1422. doi:10.1007/s00586-008-0770-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Fujiwara A, Tamai K, Yamato M, et al. The relationship between facet joint osteoarthritis and disc degeneration of the lumbar spine: an MRI study. Eur Spine J. 1999;8:396–401. doi:10.1007/s005860050193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Brinjikji W, Diehn FE, Jarvik JG, et al. MRI findings of disc degeneration are more prevalent in adults with low back pain than in asymptomatic controls: a systematic review and meta-analysis. AJNR Am J Neuroradiol. 2015;36:2394–2399. doi:10.3174/ajnr.A4498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Urrutia J, Besa P, Campos M, et al. The Pfirrmann classification of lumbar intervertebral disc degeneration: an independent inter- and intra-observer agreement assessment. Eur Spine J. 2016;25:2728–2733. doi:10.1007/s00586-016-4438-z [DOI] [PubMed] [Google Scholar]
- 12. Pfirrmann CWA, Metzdorf A, Zanetti M, Hodler J, Boos N. Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine (Phila Pa 1976). 2001;26:1873–1878. doi:10.1097/00007632-200109010-00011 [DOI] [PubMed] [Google Scholar]
- 13. Modic MT, Masaryk TJ, Ross JS, Carter JR. Imaging of degenerative disk disease. Radiology. 1988;168:177–186. doi:10.1148/radiology.168.1.3289089 [DOI] [PubMed] [Google Scholar]
- 14. Modic MT, Steinberg PM, Ross JS, Masaryk TJ, Carter JR. Degenerative disk disease: assessment of changes in vertebral body marrow with MR imaging. Radiology. 1988;166(1 pt 1):193–199. doi:10.1148/radiology.166.1.3336678 [DOI] [PubMed] [Google Scholar]
- 15. Jones A, Clarke A, Freeman BJC, Lam KS, Grevitt MP. The Modic classification: inter- and intraobserver error in clinical practice. Spine (Phila Pa 1976). 2005;30:1867–1869. doi:10.1097/01.brs.0000173898.47585.7d [DOI] [PubMed] [Google Scholar]
- 16. Jensen TS, Sorensen JS, Kjaer P. Intra- and interobserver reproducibility of vertebral endplate signal (Modic) changes in the lumbar spine: the Nordic Modic Consensus Group Classification. Acta Radiol. 2007;48:748–754. doi:10.1080/02841850701422112 [DOI] [PubMed] [Google Scholar]
- 17. Weishaupt D, Zanetti M, Boos N, Hodler J. MR imaging and CT in osteoarthritis of the lumbar facet joints. Skeletal Radiol. 1999;28:215–219. [DOI] [PubMed] [Google Scholar]
- 18. Varlotta GP, Lefkowitz TR, Schweitzer M, et al. The lumbar facet joint: a review of current knowledge: part 1: anatomy, biomechanics, and grading. Skeletal Radiol. 2011;40:13–23. doi:10.1007/s00256-010-0983-4 [DOI] [PubMed] [Google Scholar]
- 19. Kettler A, Wilke HJ. Review of existing grading systems for cervical or lumbar disc and facet joint degeneration. Eur Spine J. 2006;15:705–718. doi:10.1007/s00586-005-0954-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Jensen MC, Brant-Zawadzki MN, Obuchowski N, Modic MT, Malkasian D, Ross JS. Magnetic resonance imaging of the lumbar spine in people without back pain. N Engl J Med. 1994;331:69–73. doi:10.1056/NEJM199407143310201 [DOI] [PubMed] [Google Scholar]
- 21. el Barzouhi A, Vleggeert-Lankamp CL, van der Kallen BF, et al. Back pain’s association with vertebral end-plate signal changes in sciatica. Spine J. 2014;14:225–233. doi:10.1016/j.spinee.2013.08.058 [DOI] [PubMed] [Google Scholar]
- 22. Romero-Munoz LM, Barriga-Martin A, Segura-Fragoso A, Martin-Gonzalez C. Are Modic changes in patients with chronic low back pain indicative of a worse clinical course? 10 years of follow-up. Rev Esp Cir Ortop Traumatol. 2018;62:274–281. doi:10.1016/j.recot.2018.01.005 [DOI] [PubMed] [Google Scholar]
- 23. Sorensen PH, Bendix T, Manniche C, Korsholm L, Lemvigh D, Indahl A. An educational approach based on a non-injury model compared with individual symptom-based physical training in chronic LBP. A pragmatic, randomised trial with a one-year follow-up. BMC Musculoskelet Disord. 2010;11:212. doi:10.1186/1471-2474-11-212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Yu LP, Qian WW, Yin GY, Ren YX, Hu ZY. MRI assessment of lumbar intervertebral disc degeneration with lumbar degenerative disease using the Pfirrmann grading systems. PLoS One. 2012;7:e48074. doi:10.1371/journal.pone.0048074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. de Roos A, Kressel H, Spritzer C, Dalinka M. MR imaging of marrow changes adjacent to end plates in degenerative lumbar disk disease. AJR Am J Roentgenol. 1987;149:531–534. doi:10.2214/ajr.149.3.531 [DOI] [PubMed] [Google Scholar]
- 26. Smeets R, Köke A, Lin CW, Ferreira M, Demoulin C. Measures of function in low back pain/disorders: Low Back Pain Rating Scale (LBPRS), Oswestry Disability Index (ODI), Progressive Isoinertial Lifting Evaluation (PILE), Quebec Back Pain Disability Scale (QBPDS), and Roland-Morris Disability Questionnaire. Arthritis Care Res (Hoboken). 2011;63(suppl 11):S158–S173. doi:10.1002/acr.20542 [DOI] [PubMed] [Google Scholar]
- 27. Manniche C, Asmussen K, Lauritsen B, Vinterberg H, Kreiner S, Jordan A. Low back pain rating scale: validation of a tool for assessment of low back pain. Pain. 1994;57:317–326. doi:10.1016/0304-3959(94)90007-8 [DOI] [PubMed] [Google Scholar]
- 28. Roland M, Fairbank JC. The Roland-Morris Disability Questionnaire and the Oswestry Disability Questionnaire. Spine (Phila Pa 1976). 2000;25:3115–3124. [DOI] [PubMed] [Google Scholar]
- 29. Lee RKL, Griffith JF, Lau YYO, et al. Diagnostic capability of low- versus high-field magnetic resonance imaging for lumbar degenerative disease. Spine (Phila Pa 1976). 2015;40:382–391. doi:10.1097/BRS.0000000000000774 [DOI] [PubMed] [Google Scholar]
- 30. Ract I, Meadeb JM, Mercy G, Cueff F, Husson JL, Guillin R. A review of the value of MRI signs in low back pain. Diagn Interv Imaging. 2015;96:239–249. doi:10.1016/j.diii.2014.02.019 [DOI] [PubMed] [Google Scholar]
- 31. Luoma K, Riihimäki H, Luukkonen R, Raininko R, Viikari-Juntura E, Lamminen A. Low back pain in relation to lumbar disc degeneration. Spine (Phila Pa 1976). 2000;25:487–492. doi:10.1097/00007632-200002150-00016 [DOI] [PubMed] [Google Scholar]
- 32. de Schepper EIT, Damen J, van Meurs JBJ, et al. The association between lumbar disc degeneration and low back pain: the influence of age, gender, and individual radiographic features. Spine (Phila Pa 1976). 2010;35:531–536. doi:10.1097/BRS.0b013e3181aa5b33 [DOI] [PubMed] [Google Scholar]
- 33. Kjaer P, Korsholm L, Bendix T, Sorensen JS, Leboeuf-Yde C. Modic changes and their associations with clinical findings. Eur Spine J. 2006;15:1312–1319. doi:10.1007/s00586-006-0185-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Udby PM, Bech-Azeddine R. Clinical outcome of stand-alone ALIF compared to posterior instrumentation for degenerative disc disease: a pilot study and a literature review. Clin Neurol Neurosurg. 2015;133:64–69. doi:10.1016/j.clineuro.2015.03.008 [DOI] [PubMed] [Google Scholar]
- 35. Määttä JH, Karppinen JI, Luk KDK, Cheung KMC, Samartzis D. Phenotype profiling of Modic changes of the lumbar spine and its association with other MRI phenotypes: a large-scale population-based study. Spine J. 2015;15:1933–1942. doi:10.1016/j.spinee.2015.06.056 [DOI] [PubMed] [Google Scholar]
- 36. Määttä JH, Karppinen J, Paananen M, et al. Refined phenotyping of Modic changes: imaging biomarkers of prolonged severe low back pain and disability. Medicine (Baltimore). 2016;95:e3495. doi:10.1097/MD.0000000000003495 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Bendix T, Sorensen JS, Henriksson GAC, Bolstad JE, Narvestad EK, Jensen TS. Lumbar Modic changes-a comparison between findings at low- and high-field magnetic resonance imaging. Spine (Phila Pa 1976). 2012;37:1756–1762. doi:10.1097/BRS.0b013e318257ffce [DOI] [PubMed] [Google Scholar]
- 38. Pathria M, Sartoris DJ, Resnick D. Osteoarthritis of the facet joints: accuracy of oblique radiographic assessment. Radiology. 2014;164:227–230. doi:10.1148/radiology.164.1.3588910 [DOI] [PubMed] [Google Scholar]
- 39. Albert HB, Sorensen JS, Christensen BS, Manniche C. Antibiotic treatment in patients with chronic low back pain and vertebral bone edema (Modic type 1 changes): a double-blind randomized clinical controlled trial of efficacy. Eur Spine J. 2013;22:697–707. doi:10.1007/s00586-013-2675-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Stirling A, Worthington T, Rafiq M, Lambert PA, Elliott TSJJ. Association between sciatica and Propionibacterium acnes. Lancet. 2001;357:2024–2025. doi:10.1016/S0140-6736(00)05109-6 [DOI] [PubMed] [Google Scholar]
- 41. Portella ST, Acioly MA. The course of Modic vertebral body changes after posterolateral lumbar fusion on fused and adjacent levels: a systematic review of the literature. J Clin Neurosci. 2017;41:6–10. doi:10.1016/j.jocn.2017.04.007 [DOI] [PubMed] [Google Scholar]
- 42. Kim JH, Sharan A, Cho W, Emam M, Hagen M, Kim SY. The prevalence of asymptomatic cervical and lumbar facet arthropathy: a computed tomography study. Asian Spine J. 2019;13:417–422. doi:10.31616/asj.2018.0235 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Li J, Muehleman C, Abe Y, Masuda K. Prevalence of facet joint degeneration in association with intervertebral joint degeneration in a sample of organ donors. J Orthop Res. 2011;29:1267–1274. doi:10.1002/jor.21387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Modic MT, Obuchowski NA, Ross JS, et al. Acute low back pain and radiculopathy: MR imaging findings and their prognostic role and effect on outcome. Radiology. 2007;237:597–604. doi:10.1148/radiol.2372041509 [DOI] [PubMed] [Google Scholar]
- 45. Cheung KMC, Karppinen J, Chan D, et al. Prevalence and pattern of lumbar magnetic resonance imaging changes in a population study of one thousand forty-three individuals. Spine (Phila Pa 1976). 2009;34:934–940. doi:10.1097/BRS.0b013e3181a01b3f [DOI] [PubMed] [Google Scholar]
- 46. Manchikanti L, Manchikanti KN, Cash KA, Singh V, Giordano J. Age-related prevalence of facet-joint involvement in chronic neck and low back pain. Pain Physician. 2008;11:67–75. [PubMed] [Google Scholar]
- 47. Rahme R, Moussa R. The Modic vertebral endplate and marrow changes: pathologic significance and relation to low back pain and segmental instability of the lumbar spine. AJNR Am J Neuroradiol. 2008;29:838–842. doi:10.3174/ajnr.A0925 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Laustsen AF, Bech-Azeddine R. Do Modic changes have an impact on clinical outcome in lumbar spine surgery? A systematic literature review. Eur Spine J. 2016;25:3735–3745. doi:10.1007/s00586-016-4609-y [DOI] [PubMed] [Google Scholar]
- 49. Ohtori S, Yamashita M, Yamauchi K, et al. Change in Modic type 1 and 2 signals after posterolateral fusion surgery. Spine (Phila Pa 1976). 2010;35:1231–1235. doi:10.1097/BRS.0b013e3181bde562 [DOI] [PubMed] [Google Scholar]
- 50. Jensen RK, Kent P, Jensen TS, Kjaer P. The association between subgroups of MRI findings identified with latent class analysis and low back pain in 40-year-old Danes. BMC Musculoskelet Disord. 2018;19:62. doi:10.1186/s12891-018-1978-x [DOI] [PMC free article] [PubMed] [Google Scholar]