Abstract
Background & aims
Systemic inflammation has been reported as a new predictor for COVID-19 outcomes. Thus, we hypothesized that ICU patients infected by COVID-19 had lower blood vitamin D levels and increased systemic inflammation. Therefore, this is the first Brazilian study to evaluate the vitamin D concentrations and NLR as a systemic inflammation in patients infected by COVID-19 admitted in ICU.
Methods
This cross-sectional study selected twenty-six patients from COVID-19 Data Sharing/FAPESP, Brazil. Twenty-five patients were enrolled from a single hospital and those with blood vitamin D and neutrophil and lymphocyte data were included and had all available data analyzed. Patients were divided in two groups: low vitamin D concentration when ≤20 ng/mL (low Vit D group, n = 8, 5M/3F, 62.7 ± 8.4 years old), and normal vitamin D when > 20 ng/mL (normal Vit D group, n = 17, 9M/8F, 74 ± 8.2 years old). Serum 25-hydroxy-vitamin D, C reactive protein (CRP), and count of neutrophils and lymphocytes concentrations were collected from COVID-19 Data Sharing/FAPESP. Statistical analyses were performed using the Prism version 5.0 and Student T test was applied to verify any difference between the groups.
Results
Low vitamin D group had 15.5 ± 3.3 ng/mL of 25OH Vit D concentrations and normal vitamin D group had 35.9 ± 8.8 ng/mL. Although no difference between groups for CRP concentrations (low Vit D: 4.5 ± 3.3 vs. normal Vit D: 4.2 ± 4.0 mg/dL, p = 0.45), we found higher neutrophil count and NLR values in the low Vit D group when compared to normal Vit D group (low Vit D: 6049.8 ± 3719.7 vs. normal Vit D: 3741.8 ± 1704.1 ng/mL, p = 0.02) and (low Vit D: 9.0 ± 8.6 vs. normal Vit D: 4.2 ± 4.0 ng/mL, p = 0.03), respectively.
Conclusion
This data sharing-derived cases of COVID-19 in patients admitted at ICU showed that patients infected by COVID-19 had lower serum 25-hydroxy vitamin D and enhanced systemic inflammation when assessed by NLR values.
Keywords: Vitamin D, COVID-19, Inflammation, ICU, Neutrophil, Lymphocytes
1. Introduction
The coronavirus COVID-19 pandemic has significantly increased the number of hospitalizations [1]. During the hospitalization, many patients suffered of an aggravation of their symptoms related to COVID-19 infection (i.e. cough, fever, acute respiratory failure, fatigue, and inflammation) associated with 15–20% of hospital mortality and about 40% of infected patients requiring ICU admission [2]. A meta-analysis showed that patients with serum vitamin D concentrations <20 ng/mL had an increased risk of pneumonia [3]. Although, no negative correlation between blood vitamin D concentration and deaths (r = −0.35, p = 0.12) was found, there is a negative correlation between the vitamin D concentration and the number of case of COVID-19 infected patients in the general population [4]. In previous study, we found that low blood vitamin D (<17.7 ng/mL) concentrations are associated with the ICU clinical outcomes, such as acute respiratory failure, infections and acute liver failure [5].
Many studies reported some effects immunomodulatory of vitamin D, no randomized controlled trial was performed to test whether or not vitamin D supplementation is able to reduce the rate of ICU admission of COVID-19 infected patients, and to blunt the viral infection and the level of proinflammatory cytokines [6]. Systemic inflammation markers, such as increased neutrophil-lymphocyte ratio (NLR) are used as a prognostic marker for severity and mortality in COVID-19 patients [7]. However, the relationship between vitamin D and systemic inflammation observed in Brazilian patients remains to be elucidated.
Thus, we hypothesized that ICU patients infected by COVID-19 had lower blood vitamin D levels and increased systemic inflammation. Therefore, this is the first study to evaluate the vitamin D concentrations and NLR as a systemic inflammation in Brazilian patients infected by COVID-19 admitted in ICU.
2. Methods
This cross-sectional study selected twenty-six patients from COVID-19 Data Sharing/FAPESP, Brazil, that included data from Hospital Sírio Libanês, Brazil (i.e. 20 patients came from Sao Paulo State, 5 from Pará State and 1 from Maranhão State, but one patient was excluded because of outlier values of biochemical parameters). Thus, twenty-five patients were enrolled from a single hospital and those with blood vitamin D and neutrophil and lymphocyte data were included and had all available data analyzed. Patients were divided in two groups: low vitamin D concentration when ≤20 ng/mL (low Vit D group, n = 8, 5M/3F, 62.7 ± 8.4 years old), and normal vitamin D when > 20 ng/mL (normal Vit D group, n = 17, 9M/8F, 74 ± 8.2 years old). Serum 25-hydroxy-vitamin D, C reactive protein (CRP), and count of neutrophils and lymphocytes concentrations were collected from COVID-19 Data Sharing/FAPESP, Hospital Sírio Libanês, Brazil. Statistical analyses were performed using the Prism version 5.0 and Student T and Pearson's correlation tests were applied to verify any difference between the groups.
3. Results and discussion
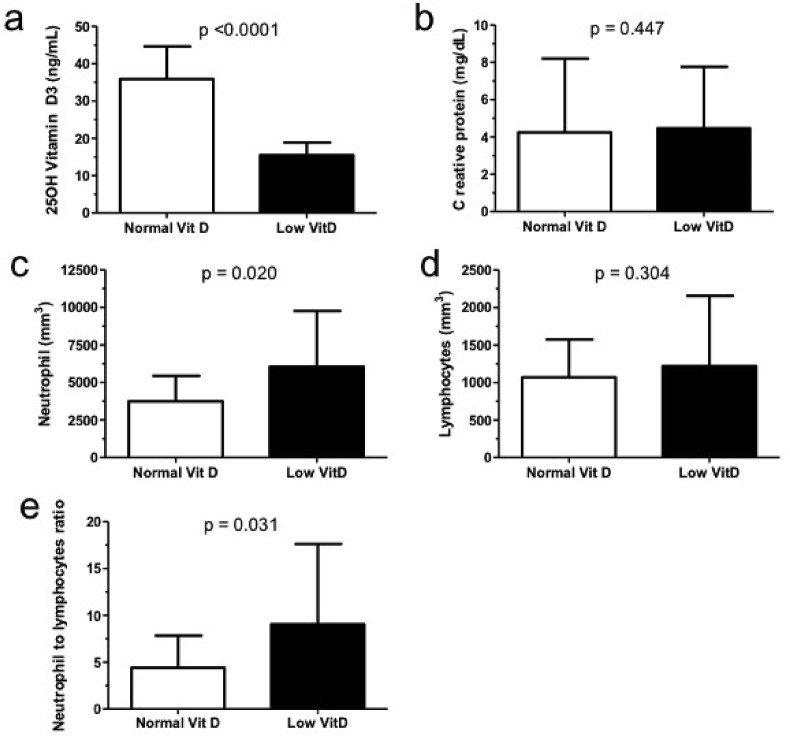
As result, we found that the low vitamin D group had 15.5 ± 3.3 ng/mL of 25OH Vit D concentrations and normal vitamin D when >20 ng/mL had 35.9 ± 8.8 ng/mL (Fig. 1 A). Although there is no difference between groups for blood CRP concentrations (low Vit D: 4.5 ± 3.3 vs. normal Vit D: 4.2 ± 4.0 mg/dL, p = 0.45) (Fig. 1B), we found higher neutrophil count and NLR values in the low Vit D group when compared with the normal Vit D group (low Vit D: 6049.8 ± 3719.7 vs. normal Vit D: 3741.8 ± 1704.1 ng/mL, p = 0.02) and (low Vit D: 9.0 ± 8.6 vs. normal Vit D: 4.2 ± 4.0 ng/mL, p = 0.03), respectively (Fig. 1C and E). However, there is no difference among the groups for blood lymphocytes count (Fig. 1D). Additionally, no correlation was found between the 25OH Vit D concentrations and neutrophil values (r = −0.31, p = 0.11).
Fig. 1.
The 25-OH vitamin D3 and systemic inflammation markers in COVID-19 patients admitted at ICU single hospital in Sao Paulo, Brazil. NLR: neutrophil-lymphocytes ratio, CRP: C reactive protein. Data are expressed as mean ± standard deviation. p < 0.05 was considered as significant statistically.
Additionally, the mortality rate was higher in the low Vit D group (20%) when compared to normal Vit D group (17.6%). COVID-19 patients had increased NLR which is accompanied with poorer prognosis and increased mortality [8]. In addition, a large retrospective and observational identified that SARS-CoV-2 infection positivity rate was higher in patients with <20 ng/mL 25(OH)D concentrations than in patients with 25(OH)D higher or equal to 30 ng/mL [9]. Although, the paricalcitol infusion therapy, a vitamin D analog has been recently FDA-approved to detain the COVID19-induced cytokines [10], also is suggested supplementation with vitamin D based on deficiency or insufficiency of this vitamin [11]. In addition, an adequate diet in vegetables and fruits ensure a ingestion of vitamin A, B, C and D and minerals which is imperative to boost to immune system [12].
Vitamin D is linked to immune system regulation, gut microbiota and epithelial tight junctions' regulation. Moreover, hospitalized patients with SARS-CoV2 present gastrointestinal problems which may be prevented by several nutritional strategies, including the vitamin D [13].
The present study had some limitations. First, no data are available in the Data Sharing/FAPESP, Brazil about respiratory indicator and nutrition status, for e.g. body mass index, which would be useful to provide the correlation between vitamin D and body mass index, since vitamin D is stored in adipose tissue. Second, we did not find the correlation among the 25OH Vit D concentrations and neutrophil values, which did not allow to establish the relationship of causality, however, lack of correlation may be due to low sample size, and Third, the lack of data on sunlight exposure did not allow generalize these data for other countries and therefore, further studies are warranted. Some strength is highlighted, such as it is the first Brazilian study on vitamin D in COVID19 patients which allow to create a strategy to use the vitamin D supplementation in these patients.
In conclusion, this data sharing-derived cases of COVID-19 in patients admitted at ICU showed that patients infected by COVID-19 had lower serum 25-hydroxy vitamin D and enhanced systemic inflammation when assessed by NLR values. Therefore, our data further strengthen the positive role of the vitamin D on immunity and suggests that 1000–2000 IU of vitamin D3 per day may be beneficial [6]. Additionally, a large scale randomized and well-controlled trial is required to confirm that vitamin D3 is able to blunt the viral infection and boost the immune system in COVID-19 pandemic.
Authorship
GDP, MCMDV, and CP wrote the article and approved the final version of this manuscript.
Funding
No funding was received for this work.
Declaration of competing interest
None declared.
Acknowledgements
GDP would like to The Brazilian National Council for Scientific and Technological Development (CNPq, Brazil, 312252/2019-6). We thank to COVID-19 Data Sharing/FAPESP. This work used data obtained from the COVID-19 Data Sharing/BR, available at https://repositoriodatasharingfapesp.uspdigital.usp.br/.
References
- 1.Wiersinga W.J., Rhodes A., Cheng A.C., Peacock S.J., Prescott H.C. Pathophysiology, transmission, diagnosis, and treatment of coronavirus disease 2019 (COVID-19): a review. JAMA. 2020;324(8):782–793. doi: 10.1001/jama.2020.12839. [DOI] [PubMed] [Google Scholar]
- 2.Richardson S., Hirsch J.S., Narasimhan M., Crawford J.M., McGinn T., Davidson K.W., et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York city area. Jama. 2020;323(20):2052–2059. doi: 10.1001/jama.2020.6775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhou Y.F., Luo B.A., Qin L.L. The association between vitamin D deficiency and community-acquired pneumonia: a meta-analysis of observational studies. Medicine. 2019;98(38):e17252. doi: 10.1097/MD.000000000001725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ali N. Role of vitamin D in preventing of COVID-19 infection, progression and severity. J Infect Publ Health. 2020;13(10):1373–1380. doi: 10.1016/j.jiph.2020.06.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gomes T.L., Fernandes R.C., Vieira L.L., Schincaglia R.M., Mota J.F., Nobrega M.S., et al. Low vitamin D at ICU admission is associated with cancer, infections, acute respiratory insufficiency, and liver failure. Nutrition. 2019;60:235–240. doi: 10.1016/j.nut.2018.10.018. [DOI] [PubMed] [Google Scholar]
- 6.Bergman P. The link between Vitamin D and Covid-19: distinguishing facts from fiction. J Intern Med. 2020;289(1):131–133. doi: 10.1111/joim.13158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Liao D., Zhou F., Luo L., Xu M., Wang H., Xia J., et al. Haematological characteristics and risk factors in the classification and prognosis evaluation of COVID-19: a retrospective cohort study. Lancet Haematol. 2020;7(9):E671–E678. doi: 10.1016/S2352-3026(20)30217-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Liu Y., Du X., Chen J., Jin Y., Peng L., Wang H.H.X., et al. Neutrophil-to-lymphocyte ratio as an independent risk factor for mortality in hospitalized patients with COVID-19. J Infect. 2020;81(1):e6–e12. doi: 10.1016/j.jinf.2020.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kaufman H.W., Niles J.K., Kroll M.H., Bi C., Holick M.F. SARS-CoV-2 positivity rates associated with circulating 25-hydroxyvitamin D levels. PloS One. 2020;15(9):e0239252. doi: 10.1371/journal.pone.0239252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Evans R.M., Lippman S.M. Shining light on the COVID-19 pandemic: a vitamin D receptor checkpoint in defense of unregulated wound healing. Cell Metabol. 2020;32(5):704–709. doi: 10.1016/j.cmet.2020.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Biesalski H.K. Obesity, vitamin D deficiency and old age a serious combination with respect to coronavirus disease-2019 severity and outcome. Curr Opin Clin Nutr Metab Care. 2021;24(1):18–24. doi: 10.1097/MCO.0000000000000700. [DOI] [PubMed] [Google Scholar]
- 12.Richardson D.P., Lovegrove J.A. Nutritional status of micronutrients as a possible and modifiable risk factor for COVID-19: a UK perspective. Br J Nutr. 2020;125(6):678–684. doi: 10.1017/S000711452000330X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Daoust L., Pilon G., Marette A. Perspective: nutritional strategies targeting the gut microbiome to mitigate COVID-19 outcomes. Adv Nutr. 2021 doi: 10.1093/advances/nmab031. [DOI] [PMC free article] [PubMed] [Google Scholar]
Further reading
- 1.Pimentel G.D., Dela Vega M.C.M., Laviano A. High neutrophil to lymphocyte ratio as a prognostic marker in COVID-19 patients. Clin Nutr ESPEN. 2020;40:101–102. doi: 10.1016/j.clnesp.2020.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]