Abstract
Cancer is a disease with complex pathological process. Current chemotherapy faces problems such as lack of specificity, cytotoxicity, induction of multi-drug resistance and stem-like cells growth. Nanomaterials are materials in the nanorange 1–100 nm which possess unique optical, magnetic, and electrical properties. Nanomaterials used in cancer therapy can be classified into several main categories. Targeting cancer cells, tumor microenvironment, and immune system, these nanomaterials have been modified for a wide range of cancer therapies to overcome toxicity and lack of specificity, enhance drug capacity as well as bioavailability. Although the number of studies has been increasing, the number of approved nano-drugs has not increased much over the years. To better improve clinical translation, further research is needed for targeted drug delivery by nano-carriers to reduce toxicity, enhance permeability and retention effects, and minimize the shielding effect of protein corona. This review summarizes novel nanomaterials fabricated in research and clinical use, discusses current limitations and obstacles that hinder the translation from research to clinical use, and provides suggestions for more efficient adoption of nanomaterials in cancer therapy.
Keywords: Nanomaterial, Cancer therapy, Tumor microenvironment, Exosome, Blood–brain barrier, Drug delivery, Protein corona
Background
Despite significant advances in medical science and technology, cancer remains a disease with limited treatment approaches. Metastasis and recurrence of cancer contribute a lot to disability and mortality, and the exact mechanisms remain to be illuminated [1, 2]. Cancer is generally considered as the consequence of gene mutations [3]. In 2018, there were an estimated 18.1 million new cancer cases and 9.6 million deaths were caused by cancer [4]. According to the Global Cancer Observatory (GCO), approximately 30 million cancer patients will die from cancer each year by 2030 [5]. In addition to the high mortality of cancer, the economic burden on families of cancer patients and society is enormous. Therefore, efforts on cancer prevention, diagnosis and treatment are of great importance.
Cancer is characterized by abnormalities in mechanisms that regulate cell cycle, leading to the survival and proliferation of malignant cancer cells. Signaling pathways are usually altered when cancer occurs. Inhibition of physiological apoptosis contributes to cancer development as well as resistance to radiotherapy and chemotherapy [6]. Inflammation and immune system disorder are also related to cancer. Traditional tumor staging (AJCC/UICC-TNM classification) is based on tumor burden (T), presence of cancer cells in draining and regional lymph nodes (N), and tumor metastases (M). Cancers can also be classified according to organs of origin, such as lung, colon, breast, head and neck, kidney, bladder, prostate, ovary, or various cancer cell types [7].
Current cancer diagnosis approaches include imaging methods, laboratory tests, and morphological analysis of tissues and cells, which is usually considered highly reliable in most cancer diagnosis [8]. Pathological characteristics such as immunohistochemical (IHC) analysis, histological alterations, mutational and molecular genetics analysis also help cancer diagnosis [9]. Common cancer treatment consists of surgical resection, chemotherapy, radiotherapy, and biological therapy. Surgery is an effective measure to remove malignant solid tumors, especially in an early stage of cancer development. Combined therapy involves several therapies such as surgery, chemotherapy, and radiotherapy. The application of chemotherapy has been popular over the years for its simplicity and convenience in treating cancer patients [10, 11].
Chemotherapy is effective for various cancers, including acute myelogenous leukemia, acute lymphoblastic, Hodgkin’s and non–Hodgkin’s lymphoma, small cell lung cancer, germ cell cancer, ovarian cancer and choriocarcinoma [12]. However, the indiscriminate cytotoxicity of chemotherapy causes undesirable side effects, as chemotherapy can also inhibit rapid-growing tissues and cells including hair follicles, gastrointestinal tract cells, and bone marrow. The use of chemotherapy also induces multi-drug resistance (MDR) and has potential association with cancer stem cells (CSCs). Cytotoxic chemical drugs used in chemotherapies are non-specific and heterogeneous in terms of distribution that contribute to MDR in the treatment process [13, 14]. This non-specificity impedes chemotherapy efficacy and impairs inhibition of tumor growth, metastasis and recurrence [15].
Current chemotherapy faces problems such as lack of specificity, cytotoxicity, short half-life, poor solubility, occurrence of multi-drug resistance and stem-like cells growth. To overcome these disadvantages, nanomaterial-based chemotherapy, targeted therapy, molecular therapy, photodynamic therapy (PDT), photothermal therapy (PTT), chemodynamic therapy (CDT), and sonodynamic therapy (SDT) are being used in cancer treatment. In addition, a substantial number of studies on variety of therapies such as molecular therapy, apoptosis regulations, immunotherapy, signal modification therapy, nucleic-acid-based therapy, and anti-angiogenesis therapy for the treatment of cancer have been done in recent years [16–18]. With the advent of nanotechnology nanomedicines used in cancer therapy can possibly reduce drawbacks of chemotherapy and an extensive research studies have been going on along this direction.
Nanotechnology applied in cancer therapy
Properties of nanomaterials
Medical nanotechnology uses materials with nanorange size, which is generally 1–100 nm. These materials are applied in the therapeutic drugs and devices design, manufacture [19]. As the size shrinks to nanoscale, many unique optical, magnetic and electrical properties emerge, making nanomaterials differ from traditional macromolecules. Typical nanomaterials possess several common characteristics: high surface-to-volume ratio, enhanced electrical conductivity, superparamagnetic behavior, spectral shift of optical absorption, and unique fluorescence properties. In the medical field, nanomaterials can be applied in drug transportation, controlled release. Increased permeability enabling crossing through biological barriers and improved biocompatibility are also noticeable features [20].
These particular properties of nanomaterial suggest it can be utilized in cancer therapeutics. The high surface-to-volume ratio of some nanomaterials can assemble with biomolecules or residues, which can enhance the specificity of chemical drug complex in targeted therapy, thereby enhancing the efficacy of nanomaterial-based treatment while reducing its toxicity to normal cells [21]. PDT and PTT are two treatment methods related to optical interference. In PDT, a photosensitizer is accumulated in cancerous sites; when irradiated with certain wavelength light, singlet oxygen and other cytotoxic reactive oxygen materials are generated, causing apoptosis and/or necrosis [22]. PTT uses materials that possess high photothermal conversion efficiency to elevate the temperature of targeted cancerous areas, leading to cancer cell death. PDT and PTT are emerging cancer treatment methods with great potential, and materials used in these two therapies are under intensive research. Some nanomaterials can be used in PDT and PTT because of their unique fluorescence properties [23]. The superparamagnetic behavior of nanomaterials provides several usages for cancer diagnosis and treatment. A common nanomaterial, superparamagnetic iron oxide nanoparticles (SPION), has potential in cancer hyperthermia treatment due to its smaller size, higher targeting specificity, controllable releasing speed, and immune evasion capability [24].
Progress of nanotechnology in targeted delivery
Targeted delivery is one of a major advantage of nanomaterial-based cancer therapy over free drugs. Recent progress has been made in targeted delivery based on nanomaterials. The idea of targeted delivery aims for precise targeting of specific cancer cells, and it is achieved by either passive targeting or active targeting. Enhanced permeability and retention (EPR) effect is used in passive targeting while active targeting is achieved by conjugating with antibodies, peptides, aptamers and small molecules. Compared with free drugs, targeted delivery helps reduce toxicity in normal cells, protect drugs from degradation, increase half-life, loading capacity, solubility [19, 25].
Through delicate design and modification, nano-drugs can maintain better specificity, bioavailability, less cytotoxicity to normal tissue, larger loading capacity, longer half-life period, and unique drug release patterns, overcoming disadvantages of conventional chemical therapy. During the past two decades, tremendous development in cancer pathology and nanoscience, technology, and industry (NSTI) created plenty of nanomaterials for cancer treatment and diagnosis.
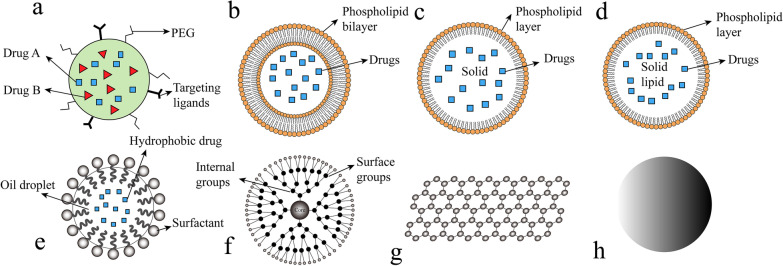
However, only a relatively small number of nano-drugs have been well developed and involved in clinical use. These nanomaterials can be generally classified into several categories (Fig. 1).
Fig. 1.
Categories of nanomaterials applied in cancer treatment. a Nanoparticles. b Liposomes. c Solid lipid nanoparticles. d Nanostructured lipid carriers. e Nanoemulsions. f Dendrimers. g Graphene. h Metallic nanoparticles. PEG, poly(ethylene glycol)
Nanomaterials used for cancer treatment
Nanoparticles
Polymeric nanoparticles
Nanoparticles are particles with size of nanoscale. Polymeric nanoparticles (PNPs), mAb nanoparticles, extracellular vesicles (EVs), metallic nanoparticles are broadly researched nanoparticles (NPs) (Table 1). PNPs are defined as colloidal macromolecules with submicron size of 10–1000 nm. As drug carriers, PNPs carry chemical drugs and achieve the sustained release to targeted cancerous sites [26]. Drugs are encapsulated or attached to the surface of nanoparticles thus forming a nanocapsule or a nanosphere. The ingredients of nanoparticles have changed over the years. Initially, nonbiodegradable polymers such as polymethyl methacrylate (PMMA), polyacrylamide, polystyrene, and polyacrylates were used to fabricate nanoparticles [27, 28]. To avoid toxicity and chronic inflammation, polymeric nanoparticles made by these materials shall be cleared up in time. The accumulation of these types of polymer-based nanoparticles in tissues to a toxic level caused due to the difficulty to get them degraded, excreted, or physically removed have now been solved. Biodegradable polymers have been manufactured to reduce toxicity, improve drug release kinetic patterns and increase biocompatibility. These polymers include polylactic acid (PLA), poly(lactic-co-glycolic acid) (PLGA), poly(amino acids) [29], poly(ε-caprolactone) (PCL), and natural polymers consist chitosan, alginate, gelatin and albumin. These improved polymeric nanoparticles have special advantages due to their properties and structures. For volatile pharmaceutical agents, PNPs help increase stability. For chemical drugs, PNPs provide optional administration methods such as oral and intravenous and higher loading ability compared to free drugs. The ability that protects drugs from degradation helps minimize undesired toxicity to normal tissues; for instance, PNPs loaded with cisplatin such as dexamethasone or α-tocopheryl succinate have been employed in chemotherapy, which prevents cisplatin-induced ototoxicity [30].
Table 1.
Summary of NPs in development or research stage for cancer therapy
| Modification | Payload | Therapies involved | Target cancer model | Outcome | References |
|---|---|---|---|---|---|
| PLGA NP | PTX | Chemotherapy | Human prostate cancer lines PC3 | Drug delivery efficiency was highly improved compared with free PTX | [31] |
| PEG, transferrin modified NP | Nucleic acids | Nucleic-acid-based therapy | Human prostate cancer lines PC3 Chronic myelogenous leukemia cells K562 | Showed higher efficiency over untargeted particles when transfect K562 leukemia cells | [32] |
| Tmab modified NP | Docetaxel | Targeted therapy, chemotherapy | Human HER2-postive BT474 cells and HER2-negative MCF7 cells | Increased cytotoxicity in HER2-positive BT474 cells but not in HER2-negative MCF7 cells | [33] |
| Tmab modified NP | Paclitaxel | Targeted therapy, chemotherapy | Human HER2-postive breast cancer cell lines: BT474, SK-BR-3; HER2-negative cell line: MDA-MB-231 | Better treatment efficacy and lower cytotoxicity to human breast epithelial cell control were exhibited | [34] |
| PLGA NP | Alantolactone Erlotinib | Targeted therapy | Human pancreatic cancer cell lines PANC-1 and Patu8988T | The synthesized NP induced significant cancer cell apoptosis and showed anticancer effect | [35] |
| Exosome | Doxorubicin | Chemotherapy | Human breast cancer cells MDA-MB-231; Mouse ovarian cancer cells; Breast and ovarian cancer mouse models | Cytotoxicity of doxorubicin was enhanced and drug accumulation in mouse heart was avoided | [36] |
| AuNP encapsulated IONPs/Ag cores | IONPs/Ag | PTT | C57BL/6 implanted with B16-F10 melanoma tumors | The gold NP complex acted well as MRI T2 contrast agent and was an effective PTT agent | [37] |
| Trithiol-terminated poly-methacrylic acid modified nanorods | Fe2P | SDT, PTT | Human cervix cancer cells HeLa; non-cancerous mouse fibroblast cells L929 | The nanorod was biocompatible and showed ultrasound, photothermal synergistic therapeutic properties | [38] |
GSH, Glutathione; NP, Nanoparticle; PLGA, poly (lactic-co-glycolic acid); PTT, Photothermal therapy; SDT, Sonodynamic therapy; Tmab, Trastuzumab
There are two main drug delivery methods: passive targeting and active targeting (Fig. 4a). A dense extracellular matrix causes difficulty for drugs to infiltrate while over-activated angiogenesis poses a certain advantage objectively known as EPR. When tumor grows, plenty of nutrition and oxygen are needed; in the meantime, tumor-induced angiogenesis generates many immature vasculatures that suppresses lymphatic drainage [39]. These leaky blood vessels make it possible for chemical drugs to penetrate into cancerous sites. However, the size of drugs is crucial as regular particles are not small enough to percolate through cancerous cells. On the contrary, nanoparticles and related chemical drug vehicles can easily penetrate targeted sites and accumulate because of attenuated lymphatic drainages [40].
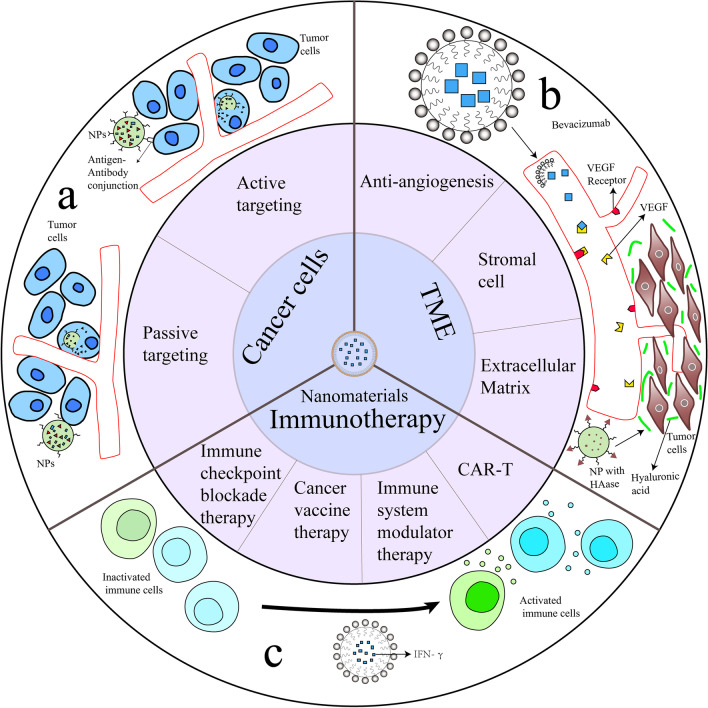
Fig. 4.
Cancer treatment approaches based on nanomaterials. a Targeting cancer cells by passive targeting or active targeting. b Targeting TME including anti-angiogenesis, stromal cell and extracellular matrix. Bevacizumab was loaded in liposome and conjugated with VEGF to inhibit angiogenesis. HAase was modified onto NP surface and enhanced NP penetration ability. c IFN-γ as an immune modulator delivered by liposomes activated immune cells in cancer immunotherapy. HAase: hyaluronidase; IFN-γ: Cytokine Interferon gamma; NP: nanoparticle; TME: tumor microenvironment; VEGF: vascular endothelial growth factor
PNPs share the common property of high surface-to-volume ratio as nanoscale particles, making it convenient to attach targeting polymers onto the surface. A proven research has shown that bioavailability can be enhanced by coating polymers with polysorbates, utilizing polysorbates surfactant effect through endothelial cell membrane solubilization and fluidization. Surface coating helps PNPs interact with blood–brain barrier(BBB) endothelial cell membranes and facilitate endocytosis [41, 42]. As novel nanocarriers function differently from conventional chemical therapy, polymeric nanoparticles can deliver several sorts of chemicals to target sites including anti-cancer drugs, small interfering RNAs (siRNA), radionuclide, and specially designed polymeric nanoparticles possessing the ability to react to ultra-sound. Fluorescent polymeric nanoparticles are used as theragnostic tools. Theragnostic is a strategy combining diagnosis and treatment at the same time. Fluorescent polymeric nanoparticles (FNPs) have been identified as novel theragnostic materials in recent years. To achieve both diagnostic and therapeutic functions, nanomaterials with complex structures are fabricated. A FNP usually consists of fluorescent proteins, biocompatible biopolymers, inorganic quantum dots, and organic dyes [43]. In addition to tumorous imaging, drugs can be loaded by π–π bond or hydrophobic interactions in fluorescence assays that eventually enhances the anti-cancer efficacy of nanomedicine [44]. In siRNA delivery, cyclodextrin polymer (CDP)-based nanoparticles improve delivery efficacy in vivo [45]. Research studies have shown that transferrin modified adamantane-Polyethylene glycol (AD-PEG) and adamantane-PEG-transferrin (AD-PEG-Tf) are appropriate to deliver nucleic acid in vivo [32, 46]. Nanoparticles can be used to encapsule radionuclide such as I125 via electrophilic aromatic substitution which is in high radiochemical yields. Through this straightforward way, radionuclide can be stored in the stable core [47, 48]. Dey [49] developed a self-assembling peptide/protein nanoparticle with the size only 11 nm in diameter and it exhibited good biocompatibility and stability in vivo, indicating it should be suitable for drug delivery in cancer treatment. Ultrasound sensitive polymeric nanoparticles have emerged as an efficient tool for cancer diagnosis and treatment. Several uses of ultrasound interactive nanoparticles have been implemented. Use of ultrasound in NP manufacture helps enhance efficacy of drug delivery, therefore leads to reduction of side effects through improved traversing ability to overcome the barriers in cancer therapy. These barriers include endothelial blood vessels [50], tissue endothelium, interstitium, nuclear membrane and BBB [51, 52]. Since ultrasound can result in a thermal effect that may eventually break the nanoparticles, ultrasound can also be used as a preset trigger through which chemical drugs can be released under control [53]. However, the polymeric nanoparticle has its disadvantages: evidence shows that some polymeric nanoparticles undergo toxic degradation and toxic monomers aggregation thereby needing further studies for their improvement in fabrication and chemical properties [54].
mAb nanoparticles
Recent progress has been made in mAb nanoparticles. In targeted therapies, monoclonal antibodies (mAbs) are vastly used for their specific targeting ability and anti-tumor effect. Moreover, in recent years, mAbs are used in designing novel anti-tumor nanoplatforms and has been forefront in the field.
To further increase therapeutic efficacy of anticancer drugs, mAbs are conjugated with cytotoxic drugs, this is termed as antibody–drug conjugates (ADCs); With specific antigens expressed differently in cancerous cells and normal cells guiding the drug complex, better specificity and less toxicity can be achieved [55]. Trastuzumab (Herceptin) is a mAb used to treat breast cancer with positive expression of human epidermal growth factor receptor 2 (HER2). Research using trastuzumab (Tmab) in ADC system have been conducted, and the result shows improved therapeutic efficacy compared with Tmab alone [56]. Abedin et al. fabricated an antibody–drug nanoparticle, which consists of a core loaded with paclitaxel (PTX) and a surface modified with trastuzumab. Two HER2-positive cell lines and one HER2-negative cell line were treated with this novel NP, PTX, and trastuzumab separately and the result was inspiring: NP complex showed better anti-tumor efficacy than PTX or trastuzumab alone, and relatively lower cytotoxicity in human breast epithelial cell control was observed in NP complex group [34] (Fig. 4a). Trastuzumab NPs based on ADC mechanism are promising nanoplatforms in cancer therapy and vast research are being conducted [57–59].
Extracellular vesicles
EVs are bilayer phospholipid vesicles with the size typically range from 50 to 1000 nm [60]. EVs are secreted continuously by various cell types and differ in size, origin, and content. Based on the origin, EVs are classified into three major groups: exosomes, microvesicles and apoptotic bodies [61, 62]. Exosomes are 40–200 nm nano-scale particles. EVs contain protein, RNA and DNA and are involved in long-distance communications [63]. Because exosome membrane contains similar lipids and molecules to their origin cells, exosome NPs can escape the immune surveillance and internalize smoothly with target cells, and exosome NPs are natural carriers to be combined with existing anti-tumor compositions and methods.
Gene therapy utilizes DNAs/RNAs in cancer treatment to take effect. Several approaches are explored in gene therapy, including restoring mutated proto-oncogene such as p53 [64], inhibitor of growth 4 (ING4), phosphatase and tensin homolog (PTEN) [65] and gene editing using clustered regularly interspaced short palindromic repeats (CRISPR)-associated proteins (Cas) system that disables key oncogenes [66, 67]. RNA interference (RNAi) can be caused by small RNAs such as siRNAs and microRNAs (miRNAs). RNAi contributes to physiological and pathological process. Research that targeting oncogenic mRNAs by siRNA is under evaluation [68]. Gene therapy can also induce cell death by delivering transgene or cell death-triggering gene to tumor cells [69].
Researchers have utilized exosomes as nanoparticle platforms to delivery nucleic acids, small molecules, and proteins [36, 70] (Table 2). Hadla et al. used exosomes loaded with DOX (exoDOX) to treat human breast cancer cells and the result showed that compared with free DOX, exoDOX enhances the cytotoxicity of doxorubicin and avoid drug accumulation in the heart [36]. Exosomes can be engineered for targeted delivery in cancer treatment. A macrophage-derived exosome was modified with aminoethylanisamide-polyethylene glycol (AA-PEG) moiety, and the AA-PEG exosome was loaded with PTX. The engineered exosome showed improved therapeutic outcomes in pulmonary metastases mouse model [71]. Jeong et al. utilized exosomes to deliver miRNA-497 (miR-497) into A549 cells, and the result showed that tumor growth as well as expression of associated genes were suppressed, indicating this exosome-mediated miRNA therapeutic can be used in targeted cancer therapy [72]. Compared with synthetic NPs, exosome NPs possess inherent biocompatibility, higher chemical stability and the ability to manage intercellular communications. However, there are obstacles of exosome NP application, such as lack of uniform criteria of exosomal isolation and purification, unclear mechanism of exosome in cancer treatment, heterogeneity and difficulty preserving [73–75].
Table 2.
EVs used as nanocarriers in cancer therapy
| Nanocarrier | Pharmaceutical ingredients | Disease | Outcome | References |
|---|---|---|---|---|
| AA-PEG modified exosome | Paclitaxel | Lung cancer | Exhibited high loading capacity, better accumulation in cancer cells and improved therapeutic outcomes | [71] |
| Exosome | Doxorubicin | Osteosarcoma | Anti-tumor effect was enhanced while cytotoxicity to myocardial cells was reduced compared to free DOX | [76] |
| Exosome | miR-497 | Lung cancer | Tumor growth as well as expression of associated genes were suppressed | [72] |
| Microvesicle | Therapeutic mRNA/protein | Schwannoma | The suicide therapeutic mRNA/protein loaded microvesicle converted the prodrug to active form and led to cancer cell death | [77] |
| EV | miR-101 | Osteosarcoma | Osteosarcoma cell invasion and migration were suppressed after taking in miR-101 loaded EVs | [78] |
| Exosome-Liposome Hybrid NP | CRISPR/Cas9 system | / | The hybrid NPs can deliver CRISPR-Cas9 system in MSCs and might be used in cancer therapy | [79] |
| Exosome | Interferon-γ fusion protein | Prostate cancer | The exosomal vaccine induced immune response against prostate cancer derived exosomes and inhibited tumor growth | [80] |
Cas, CRISPR-associated proteins; CRISPR, Clustered regularly interspaced short palindromic repeats; EV, Extracellular vesicle; MSC, Mesenchymal stem cell
Lipid-based nanomaterials
Research on lipid-based nanomaterials is blooming and three main categories have been receiving great attention in current research and clinical trials: liposomes, solid lipid nanoparticles (SLNs), and nanostructured lipid carriers (NLCs). Liposomes were approved in 1965 and considered the first enclosed microscopic phospholipid bilayer nanosystem [81]. Liposomes are spherical vesicles composed mainly of uni-lamellar or multi-lamellar phospholipids, and the size of a liposome usually ranges from 20 nm to more than 1 um [82, 83]. A liposome generally has a hydrophilic core and a hydrophobic phospholipid bilayer. This kind of structure enables entrapment of both hydrophilic and hydrophobic drugs [84] depending on the pharmacokinetic properties of the drug. Liposomes with the typical structure encapsulate hydrophilic drugs within their aqueous core and hydrophobic drugs in the lipid bilayer. Drugs encapsulated within the central cavity of liposome are protected from environmental degradation during the circulation through human bloodstream [85]. The size and number of bilayers are two important parameters that affect the loading amount and half-life of drugs; therefore, liposomes can be classified into two types according to these two conditions: unilamellar vesicles and multilamellar vesicles (MLV). Unilamellar vesicles are further divided into small unilamellar vesicles (SUV) and large unilamellar vesicles (LUV). An onion-like structure is formed in multilamellar liposomes, while several unilamellar vesicles can be formed inside other vesicles and form multilamellar concentric phospholipid spheres separated by water molecules [86].
As per extensive research on nanocarriers, recent liposomes bear plenty of unique properties and characteristics; correspondingly, novel applications have emerged based on liposome materials. Three major issues have been discovered and dealt with over the development of liposomes. Breaking through biological barriers and avoidance of rapid clearance are problems researchers have been encountering. As referred to above, biological barriers have always been major technical obstacles for nanocarriers to overcome. Regarding liposomes, cells of the mononuclear phagocyte system (MPS) predominantly in the liver and spleen are acting as human guards and phagocytizing nanoliposomes. Modifying membrane is one of the major techniques to prolong liposome half-lives. Covering the membrane with proteins, peptides, polymers, or other molecules significantly enhances the ability to escape from the MPS system and therefore helps achieving longer liposomal half-lives [87]. This kind of liposomes was named “Stealth” liposomes. Later polyethylene glycol conjugated liposome was found to have a longer half-life compared to other modified liposomes. Based on this observation, PEG-liposomes loaded with doxorubicin (DOX) were used to treat Kaposi's sarcoma in HIV patients [88].
Drug-loading and controlled release of liposomes are also important issues that need attention in liposome nanocarrier design. For cancer chemotherapy, bioavailability affects drug efficacy. Compared to free DOX, DOX liposome has a lower bioavailability, indicating that improving the bioavailability should be considered when design liposomes [89]. Co-delivery and controlled release are two major applications of liposomes. Combinations with chemical drugs, metals, gene agents, and other chemotherapeutic agents have been formed. Overactivation of certain signaling pathways is one of the patterns of cancer occurrence, and drugs targeting these signaling pathways are applied. To achieve higher efficacy, researchers loaded a novel PEGylated liposomal with ncl-240 and cobimetinib which are small-molecule inhibitors of the phosphoinositide 3-kinase/mammalian target of rapamycin (PI3K/mTOR) pathway and mitogen-activated protein kinase kinase/ extracellular signal regulated protein kinase (MEK/ERK) pathway, respectively. The result showed that the cytotoxic effect was enhanced due to synergistic effects [90]. A novel liposome-encapsulated nanocarrier loaded with both irinotecan and floxuridine showed better efficacy in advanced solid tumors [91]. The delicate structure of a novel liposome with multiple layers enabled it to effectively load up to 3500 siRNA molecules in a single bilayer and codelivery of DOX, which demonstrated better DOX efficacy and shrink of tumor mass in breast cancer treatment [92]. Triggered release and target methods are extensively studied. As cancerous areas have an average 6.8–7.0 extracellular pH value, which is slightly more acidic than healthy tissue [93], liposomes can be designed to release drugs when reaching acidic cancerous areas. With a pH-sensitive material, carboxymethyl chitosan (CMCS) coated to the surface, the cationic liposome (CL) preloaded with sorafenib (Sf) and siRNA (Si) obtained pH-sensitive property. Results showed that sorafenib release was enhanced and cellular uptake was increased at the pH of 6.5 [94]. Other than pH-responsive property, liposomes can also be fabricated with enzyme-responsive, redox-responsive, light-responsive characteristics, depending on tumor microenvironment (TME) and drug properties [95]. TME is the concept of the environment in which tumor cells are living. TME facilitates tumor growth, invasion, migration, angiogenesis, inflammation and it is related with drug resistance [96, 97]. The common characteristics of TME include the presence of EPR, hypoxia (lack of oxygen), acidosis (low pH), extensive angiogenesis, and tumor-associated immune cells that help the immune escape of cancer cells [98]. In general, liposomes' advantages are protecting loaded drugs from enzyme degradation, low toxicity, biocompatibility, flexibility, superior biodegradability, and non-immunogenicity [99]. However, application of liposome is limited due to disadvantages such as short shelf life, low encapsulation efficacy, dissatisfying stability, rapid removal by MPS, cell adsorption, and intermembrane transfer.
SLNs are colloidal nanocarriers with a nanoscale of 1–100 nm. Because of the strict limits on the size, SLNs are referred to as the “zero-dimensional” nanomaterials, as they differ from other larger nanomaterials by at least one dimension in nanoscale. Unlike liposomes, the ingredients of SLNs include solid materials such as solid lipid, emulsifier, and water. Partial glycerides, triglycerides, fatty acids, waxes, steroids and PEGylated lipids are lipid used in SLNs [19]. In terms of structure and function, there are similarities and differences between SLNs and conventional liposomes. The similarities are the lipidic outer layer and delivery function of chemical drugs. Unlike traditional liposomes which consist of lipid bilayers that surround an aqueous pocket, some SLNs do not have a contiguous bilayer; instead a micelle-like structure is formed and drugs are encapsulated in a non-aqueous core [100]. Lipid components of SLNs are solid at body temperature, and SLNs have better stability and prolonged release than liposomes. However, SLNs have limitations that are unpredictable gelation tendency and inherent low incorporation rates because of their crystalline structure [101].
NLC carrier was developed in the past two decades as an improved generation of both liposome and SLN. To improve stability and loading capacity while maintaining intrinsic protection function, biocompatibility, and non-immunogenicity, NLCs are designed as a system consisting of a core matrix loaded with both solid and liquid lipids. NLCs can be administrated through multiple methods: oral, parenteral, inhalational, and ocular. As many drug compounds used in cancer treatment are lipophilic, NLCs have gained lots of attention in recent years [102].
Nanoemulsions
Nanoemulsions (NE) are colloidal nanoparticles made of aqueous phase, emulsifying agents as well as oil [103]. The size of nanoemulsion ranges from 10 to 1000 nm. Nanoemulsions are widely used drug nanocarriers, usually solid spheres with amorphous and lipophilic surface that exhibit negative charge. As nanoemulsions are heterogeneous mixtures containing oil droplets in aqueous media, nanodroplets are distributed with small size, and three typical types of nanoemulsions can be formulated: (a) water in oil nanoemulsion system in which water is dispersed in an aqueous medium; (b) oil in water nanoemulsion system in which oil is dispersed in an aqueous medium; (c) bi-continuous nanoemulsion [103]. Nanoemulsions have several advantages over most lipid-based nanomaterials and nanoparticles: optical clarity, thermodynamic stability, large surface area, convenience in manufacture, biodegradability, and ideal drug release profile [104]. Membrane modified nanoemulsions have been extensively studied. Co-delivery by nanoemulsions is one of the methods to enhance bioavailability and drug efficacy. The test results of a NE drug carrier system loaded with spirulina polysaccharides and PTX showed that it could improve the anti-tumor effect of PTX by regulating immunity through Toll-like receptor 4/nuclear factor kappa B (TLR4/NF-κB) signaling pathways [105]. A nanoemulsion system consisting of temozolomide, rapamycin, and bevacizumab was established to treat advanced melanoma. Through parenteral administration, enhanced cytotoxicity against melanoma cells and improved inhibition of tumor relapse, migration and angiogenesis were observed in vitro human and mouse cell models [106](Fig. 4b).
Nanoemulsions can also be applied to immune therapy by loading certain immune-stimulation moiety. Cytokine Interferon gamma (IFN-γ) was loaded in a modified nanoemulsion to stay stable in extreme temperature changes for three months. The test results showed that this NE suppressed cell viability of MCF-7 human breast cancer cells and induced cellular activity of phagocytes, suggesting a promising potential in cancer treatment [107] (Fig. 4c). One application that gains plenty of attention is using NE as a strategy to overcome MDR. In MDR cancer cells, ATP-binding cassette transporters (ABCs) are responsible for part of MDR occurrence. MDR transporters expressed by ABCs cause resistance to anticancer drugs. P-glycoprotein (P-gp) is the first identified ABC transporter encoded by ABC1 gene which possesses function of pumping colchicine, vinblastine, etoposide and paclitaxel (PCX) from the cell [13]. To overcome this obstacle, a novel NE co-delivering baicalein and paclitaxel was fabricated by Meng and colleagues. By co-encapsulating these two drugs, oxidative stress was elevated, thereby providing a suitable strategy to improve cell sensitivity to paclitaxel. Results showed that reactive oxygen species (ROS) was increased, cellular glutathione (GSH) was decreased, caspase-3 activity was enhanced in MCF-7/Tax cells, and an in-vivo study showed that baicalein-paclitaxel NE exhibited a superior antitumor efficacy than conventional paclitaxel formulations [108, 109]. These studies clearly exhibit the potential benefit of using specially manufactured NEs in MDR management.
Despite potential benefit NEs possess, there are challenges to clinical application. The production of NEs usually involves high temperature and pressure. Therefore, not all starting materials are suitable in NE application. This is one of the obstacles in applying NEs to massive commercial production. In NE preparation, high-energy methods such as homogenizer and microfluidizer are used, which makes NE costlier than other conventional formulation. Because of lack of understanding of chemistry in NE production, detailed research should be conducted about component interaction and NE metabolism in human body to assess the safety in clinical use [104].
Dendrimers
Dendrimers are a kind of unique macromolecules with hyperbranched defined architecture. The most apparent characteristic of dendrimers is their highly branched and easily modifiable surfaces. The size of these dendrimer polymers is ranging mainly from 1 to 10 nm, while some specially fabricated large dendrimers can reach up to diameters of 14–15 nm [110, 111]. Three major structural parts form the dendrimer molecules: central core that loads theragnostic agents through noncovalent encapsulation, branches that form the interior dendritic structure, and the exterior surface conjugated with functional surface groups. Several dendrimers have been developed for cancer therapeutics: polyamidoamine (PAMAM), PPI (polypropylenimine), PEG (poly(ethylene glycol)), Bis-MPA (2,2-bis(hydroxymethyl) propionic acid), 5-ALA (5-aminolevulinic acid), and TEA (triethanolamine) [112].
Due to specific structure, dendrimers have unique features over other nanomaterials: defined molecular weight, versatile adjustable branches, narrow polydispersity index, superior solubility and bioavailability of hydrophobic drugs. Cationic dendrimers with positively charged surfaces can form complexes with nucleic acids; therefore, dendrimers can be used as efficient nucleic acid nanocarriers. PAMAM and PPI are two widely studied dendrimers with various application strategies. A PAMAM dendrimer/carbon dot nanohybrid was designed to achieve MDR management and cancer cell monitor simultaneously via fluorescence imaging. Two complexes were manufactured separately. The first part was a CDs/DOX complex consisting of blue-emitting carbon dots (CDs) and anticancer drug DOX through non-covalent interactions. The other part was G5-RGD-TPGS, which consists of generation 5 (G5) PAMAM dendrimers, targeting ligand cyclic arginine-glycine-aspartic (RGD) peptide and drug efflux inhibitor d-α-tocopheryl polyethylene glycol 1000 succinate (TPGS). Two parts were connected by electrostatic interaction and formed a dual drug-loaded nanohybrid system. In vitro fluorescence was achieved by the luminescence of CDs, and targeting specificity was achieved by the presence of RGD ligands that targets αvβ3 integrin receptors overexpressed in cancer cells [113]. The results showed that TPGS had a significant inhibitory effect on cancer cells. The Co-delivery ability of dendrimer can also be used in delivering completely different materials. DOX is commonly used to treat colon cancers. The tumor necrosis factor-related apoptosis-inducing ligand (TRAIL) is a crucial factor in the apoptotic pathway, capable of binding to death receptors 4 and 5 (DR4 and DR5), which are overexpressed in various cancer cells. Pishavar group encapsulated DOX and TRAIL plasmid in a dendrimer nanocarrier, which exhibited a stronger antitumor effect than modified carriers containing DOX or TRAIL plasmid alone [114]. A PAMAN nanocarrier based on dendrimer was synthesized and used for chemotherapy combined with photothermal treatment of liver cancer cells. Though PAMAN dendrimers without modification have disadvantages such as low transfection efficiency, inefficient cellular internalization and instability of encapsulation [115], the nanomaterial has competitive contrast properties, showing great potential in combination therapy [116].
Carbon nanomaterials
Carbon nanomaterials (CNMs) are a kind of nanosized material with many categories based on carbon element. CNMs have been widely used in many industrial and medical fields because of their unique electronic, thermal, optical, and mechanical properties (Table 3). In cancer theragnostic applications, CNMs are considered more biocompatible and safer than metal-based nanomaterials [117, 118]. CNMs can load chemical drugs through π–π stacking or hydrophobic interactions due to inherent hydrophobic nature, making CNMs as efficient drug delivery platforms [119, 120]. Several carbon nanomaterials have been massively studied in cancer treatment: graphenes, fullerenes, carbon nanotubes (CNTs), carbon nanohorns (CNHs), carbon quantum dots (CQDs) and graphyne (GDY). Although all these materials are based on carbon elements, the morphological structure, properties, and functions of these nanomaterials vary greatly.
Table 3.
Recent studies on CNMs for cancer therapy
| Type of materials | Loaded drug | Feature | Anti-cancer effect | References |
|---|---|---|---|---|
| rGO | PTX | Phosphorylcholine oligomer grafted perylene-modified | Cytotoxicity of PTX against SGC7901 tumor cell line was improved compared with free PTX | [166] |
| rGO | DOX | Folic acid-conjugated | Enhanced specificity and cytotoxicity of DOX to MBA-MB 231 human breast cancer cells | [167] |
| rGO | MTX | Gold NPs-coated | Activity of MTX on MCF-7 was improved compared to free MTX | [168] |
| GO | MTX | Dopamine-conjugated | Capacity of MTX targeting dopamine receptors expressing cancer cells was enhanced | [169] |
| GO | DOX | Carboxymethyl cellulose-functionalized | DOX was released pH-dependently and showed good antitumor activity and biocompatibility without no obvious cytotoxicity | [170] |
| Fullerene | C60 (OH)22 | Targeting at cancer stem cells | Biological communication of stem cells and tumor cells was inhibited | [171] |
| Fullerene | Gd@C82 (OH)22 | Angiogenesis | 10 proangiogenic factors were downregulated in mice model | [172] |
| CNT | Hydrazine–SWNT–DOX | pH-sensitive drug release | Great cytotoxicity toward HepG2 tumor cells with high weight loading | [173] |
| CNT | Chitosan–MWCNT–DOX | Used in photothermal/chemotherapy | Sustained release of DOX and significant hyperthermia exhibiting remarkably enhanced anti-tumor efficacy | [174] |
| CQD | CQD–mesoporous silica nanoparticle–DOX | pH-sensitive drug release | 80% DOX load released at pH 5.0 and a remarkably enhanced anti-tumor efficiency was exhibited | [175] |
CNTs, Carbon nanotubes; CQDs, Carbon quantum dots; DOX, Doxorubicin; GO, Graphene oxide; MTX, Methotrexate; MWCNTs, Multiwalled carbon nanotubes; PTX, Paclitaxel; rGO, Reduced graphene oxide
Graphene is a two-dimensional crystal with sp2 -hybridized carbon sheet which possesses remarkable mechanical and electronic properties. It has also been heavily researched in biomedical applications, including cancer treatment [121]. Graphene-based nanomaterials can be classified into several types depending on their composition, structure, and properties: single-layer graphene, multi-layer graphene, graphene oxide (GO) and reduced graphene oxide (rGO) [122]. Graphene has unique electrochemical and mechanical properties, for example, optical transmittance, chemical inertness, high density, molecular barrier abilities and high hydrophobicity [123, 124]. Graphene also has other remarkable features that contribute to cancer theragnostic such as high planar surface enabling higher drug-loading capacity [125] and thermal conductivity (5000 W/mK) [126]. However, van der Waals forces and π–π stacking interactions cause poor solubility and agglomeration of nanosheets formed by graphene in solution, which significantly affects toxicity and hampers its fabrication [127, 128]. These drawbacks have driven researchers to look for more bioavailable graphene-based nanomaterials that retain graphene’s advantages while being easy to fabricate. GO is a chemically modified material based on graphene. Functional oxygen groups such as carboxyl (–COOH) and Hydroxyl (C–OH) locate at the edge of graphene, while carbonyl (C=O) and epoxy groups (C–O–C) locate on the basal plane, thereby forming a typical GO molecule [125]. A rGO is the reduced derivative of GO. Compared to graphene, GO and rGO have improved properties regarding to biological usage. Defective oxygen-bound sp3 carbon atoms exhibit strong hydrophilicity and help forming of dispersions in aqueous solvents that are highly stable colloidal, preventing uncontrolled van der Waals, hydrophobic interaction induced aggregation [129]. Meanwhile, hydrophilic functional groups on the GO surface make the nanosheets a versatile platform for conjugating of various materials, which provides great potential in targeted therapy, PDT, PTT, and cancer diagnosis [130, 131].
Compared to other nanomaterials, graphene shows direct immunogenicity toward the immune system, and lateral size can regulate the extent of immunostimulatory capability both in vitro and in vivo [132]. Research shows that graphene activates the main components of the human immune system, macrophages and dendritic cells, indicating its potential in cancer treatment. Feito et al. studied the effect of the GO nanosheets specifically designed for hyperthermia cancer therapy on macrophage and lymphocyte function. The result showed that the 6-armed GO (6-GOs) significantly increased secretion of tumor necrosis factor alpha (TNF-α) by RAW-264.7 macrophages without changing IL-6 and IL-1β levels. In the presence of concanavalin A, lipopolysaccharide and anti-CD3 antibody, treatment of primary splenocytes involved 1-GOs and 6-GOs leading to significant dose-dependent cell proliferation and a decreased IL-6 level, which suggested the inherent weak inflammatory properties of GOs that are favorable for hyperthermia cancer therapy [133]. Graphene has also been found to inhibit some tumor cells. Burnett [134] treated human osteosarcoma (OS) cell and normal osteoblast cell with GO, and found that the apoptosis rate of OS cells was significantly higher than that of hFOB1.19 normal osteoblast cells. GO showed significant effects on cytotoxicity against OS, Nrf-2 decrease, ROS and cytomorphological changes. CSCs are generally considered a cancer cell population of high tumorigenic potency with self-renewable ability. CSCs interact with the TME and are believed to be involved in MDR formation [135]. Destruction of CSCs is one of the therapeutic approaches to avoid malignancy. It has been claimed that GO can specifically target CSCs rather than normal cells, and by inhibiting several key signaling pathways including WNT, Notch and STAT-signaling, GO induces CSC differentiation and inhibits tumor-sphere formation in multiple cell lines including breast, ovarian, prostate, lung, pancreatic and glioblastoma [136]. The researchers named this phenomenon, “differentiation-based nano-therapy”. However, few studies have been conducted over the past years, and more evidence may be needed. The interaction of graphene-immune cell interaction, effect graphene casts upon immune system and the direct anti-CSC phenomenon require further research.
As a nanomaterial with a high surface-to-volume ratio and plenty of oxygen-containing branches, graphene is a suitable platform for drug delivery, PDT, PTT. A GO-peptide hybrid was fabricated via irreversible physical adsorption of the Ac-(GHHPH)4-NH2 peptide sequence known to mimic the anti-angiogenic domain of histidine-proline-rich glycoprotein (HPRG). The hybrid nanomaterial was tested in prostate cancer cells (PC-3), human neuroblastoma (SH-SY5Y), and human retinal endothelial cells (primary HREC). The results showed that this GO-peptide nanoassembly effectively induced toxicity in the prostate cancer cells, blocked the cell migration, and inhibited prostaglandin-mediated inflammation in PC-3 and HRECs. Since poor nucleation, internalization of liposomal doxorubicin (L-DOX) limited its application in breast cancer, a novel DOX-loaded GO nanocarrier was created. The GO-DOX exhibited much higher anticancer activities when administered to cellular models of breast cancer. Through live-cell confocal imaging and fluorescence lifetime imaging microscopy, researchers found that GO-DOX achieved its high efficacy by inducing massive intracellular DOX release when bonded to the cell plasma membrane [137]. Many research indicates that GOs and rGOs can target at hypoxia [138] and abnormal angiogenesis in cancer TME [139, 140]. GOs and rGOs are also widely used in PDT and PTT [141, 142]. GDY is an allotrope of graphene that contains two acetylenic linkages in each unit cell, which double the length of the carbon chains connecting the hexagonal rings [143]. As a result, GYD is softer than either graphyne or graphene. In the past three years, several studies have been conducted using GYD as a drug delivery platform for photothermal/chemotherapy combinatorial approach in cancer diagnosis [144–146].
Fullerenes are molecules composed of carbon allotropes. The conformation of fullerenes includes hollow sphere, ellipsoid, or tube. Typical fullerenes include C60, C70, C82, etc. Metal atoms can be incorporated inside and form a metallofullerene [117]. Metal atoms encapsulated in the fullerene are usually Group III transition elements or a lanthanide. Since electrons of the intra-fullerene can transfer from encapsulated metal atom to the fullerene cage, metallofullerenes can be used as magnetic resonance imaging material. Properties of fullerenes also include free radical scavenging ability; therefore fullerenes can act as antioxidants [147, 148]. Compared to other nanomaterials, fullerene shows extraordinary properties in PDT and PTT. Chen et al. demonstrated that two critical factors leading to errors in photothermal efficiency estimation were laser irradiation time and nanoparticle concentration, and determined that photothermal conversion efficiency of polyhydroxy fullerenes was 69% [149]. The facts that the photothermal response of fullerenes remained stable with repeated laser irradiation, and the fullerene structure did not change, indicated that fullerenes were ideal candidates for photothermal therapy. A near-infrared (NIR) light-harvesting fullerene-based nanoparticles (DAF NPs) was tested for photoacoustic (PA) imaging-guided synergetic tumor photothermal and PDT. Compared to fullerene and antenna nanoparticles (DA NPs), DAF NPs showed better reactive oxygen species and heat generation efficacy. In vitro and in vivo studies demonstrated that DAF NPs could effectively inhibit tumor growth through synergetic PDT and PTT [150]. As a nanocarrier, fullerene has also been used in chemical drug delivery combined with PDT or PTT [150, 151].
CNTs are cylindrical tubes formed by sp2 -hybridized carbon atoms considered as rolls of graphene. The size of CNTs can vary from 1 nm to several micrometers. According to the number of layers formed in a CNT, CNTs can be divided into single-walled carbon nanotubes (SWCNTs) and multiwalled carbon nanotubes (MWCNTs). Poor water solubility and toxicity are two drawbacks of CNTs. Many studies on surface functionalization and material modifications have been carried out to solve the above problems and make CNTs more bioavailable. As a carbon-based nanomaterial, CNTs can interact with immune cells and induce immune response, therefore elevate immunity to suppress tumor growth [152, 153]. As a nanocarrier with a long research history being researched, CNTs are commonly considered an efficient PDT and PTT vehicle. Sundaram and his co-workers [154] coupled SWCNTs with hyaluronic acid (HA) and chlorin e6 (Ce6), and test this novel material in colon cancer cells using PDT. After 24 h, cellular changes were observed via microscopy, LDH cytotoxicity assay, and cell death induction. The result showed that the synthesized material enhanced the ability of PDT. Another synthesized NIR active photothermal agent, CNTs-PAMAM-Ag2S, was found to be highly efficient in PTT. The experiment showed that under irritation with 980 nm laser, photothermal efficacy of this complex was higher than that of copper-based and popular gold photothermal agents. Moreover, the complex demonstrated excellent stability against photo-bleaching and photo-corrosiveness, indicating the novel nanoagent could be promising in PTT [155].
Drug delivery systems (DDSs) based on CNTs loaded with DOX, PTX [156], cis‑platinum (CDDP) have been intensively studied [157–159]. CNHs belong to the carbon allotrope family. The conical structure is usually between 2 and 5 nm in diameter and the length of the larger spherical superstructures forming with sp2 hybridized carbon atoms is typically around 100 nm, which partly resembles the CNTs [160]. Similar to CNTs, CNHs lack solubility and require surface modification to be a nanocarrier in human tissue. Solutions include adding organic species onto the outer skeleton [161], conjugate planar aromatic molecules through electrostatic association or π–π stacking interactions [162, 163]. CNHs possess both drug-loading and photothermal abilities and were used in design of DDS with combined characteristics. Yang et al. made a dual chemo drug-loaded single-walled CNHs system. SWNHs were modified with poly and mPEG-PLA via hydrophobic-hydrophobic and π–π stacking interactions. Cisplatin and DOX were loaded onto modified nanohorns separately. The nanocarrier exhibited loading ability and efficient photothermal ability with a pH-dependent releasing capacity. Results showed that both primary breast tumors and the lung metastases were eradicated [164]. CNHs can also be modified with specific targeting molecules and applied in target chemical therapy. A cisplatin loaded CNH attached with a mAb D2B, selective for prostate specific membrane antigen (PSMA) + prostate cancer cells, showed superior efficacy and specificity to kill PSMA + prostate cancer cells compared to hybrids Ab-CNHs and cisplatin-CNHs [165].
Toxicity and side effects of CNMs used in cancer therapy have been studied in depth. Serum protein adsorption, hemolysis, cytotoxicity, and immunotoxicity have been reported for GO and rGO (93). As GO and rGO have a large surface area, they can be substrates for protein adsorption in the biological environment [176, 177]. With proteins adsorbed to the nanomaterial, loss of designed function and blockage of blood capillary might occur. In vitro and animal experiments indicated that the dose and size of GO and rGO could affect the toxicity of nanomaterials [178]. One study showed that large amounts hydrophobic rGO, accumulated on cell membrane, could induce high ROS stress and eventually lead to cell apoptosis [179]. In vivo studies revealed that CNTs could elicit chronic inflammation, granuloma formation, fibrosis, along with mesothelioma-like pathology [180]. Yan et al. summarized factors influencing CNT-induced toxicity such as surface modification, degree of aggregation, concentration, CNT size and shape, and listed up sites of CNTs accumulation after separation from anticancer drugs, which eventually suffer from CNT toxicity [181]. However, among this vast evidence achieved from various cells and animals, which aspect of CNMs plays a central role and the exact mechanisms of cellular toxicity caused by CNMs remain to be addressed [182].
Quantum dots
Quantum dots are widely researched biomedical imaging probes due to their distinctive optical and electronic characteristics. They are typically nanometer-scale semiconductor crystallites and are broadly used to improve the efficacy of fluorescent markers in biological imaging [183]. Compared with organic fluorophores, QDs possess unique optical and electronic properties such as size and composition leading tunable fluorescence emission from visible to infrared wavelengths, large absorption coefficients, and high brightness levels photostability [184]. There are three common QDs based on carbon: graphene quantum dots (GQDs), nanodiamond and CDs. The most common use of carbon QDs is bioimaging, which can be applied to cancer imaging and sensing. GQDs are considered emerging nanomaterials in biosensing and cancer therapy because of the inherent grand surface suitable for molecular conjugation, superior biocompatibility, and rapid excretion. A photoluminescent glycodendrimer with terminal β-cyclodextrin molecules system was designed and used for DOX delivery with biocompatibility and pH-sensitivity. GQDs were used to provide the surface for PAMAM to grow from. After excitation at 365 nm by UV light, the emission spectra from GQDs and GQDs-PAMAM-β-CD were recorded. The result showed higher efficiency in killing cancer cells than that achieved by DOX alone and containing the GQDs made it a potential imaging agent with photoluminescent activity [185].
The fluorescent ability of GQDs was also used in a novel nanocarrier for targeted therapy. Researchers conjugated folic acid to sulfur-doped graphene quantum dots (FA-SGQDs) through simple pyrolysis of citric acid (CA), FA and 3-mercaptopropionic acid (MPA). The complex exhibited blue fluorescence with an emission band at 455 nm upon excitation at 370-nm wavelength, and a non-immunogenic FR-mediated endocytosis process for TA-SGQDs to enter the FR-positive cancer cells was revealed. In addition to bioimaging and biosensing, GQDs were also being investigated for PTT and PDT. A specifically modified GQD which exhibited strong absorption (1070 nm) in NIR-II region was prepared. The so-called 9T-GQDs having uniform size distribution, tunable fluorescence, and high photothermal conversion efficacy (33.45%) made it effective for ablating tumor cells and thus inhibited tumor growth under NIR-II irradiation, showing the potentiality of GQDs in PTT [186]. A combined photodynamic-chemotherapy DDS was designed based on carbon quantum dots. Researchers conjugated 5-aminolevulinic acid (5-ALA) with mono-(5-BOC-protected-glutamine-6-deoxy) β-cyclodextrin (CQD-glu-β-CD) moiety, and these materials were conjugated to CQDs loaded with DOX. High cytotoxicity and morphological changes of MCF-7 cancer cells were observed; also, ROS were induced by 15 min 635 nm (25 mW cm−2) radiation and achieved higher therapeutic effects [187]. CDs and nanodiamond have also been studied in cancer treatment utilizing its function of targeted therapy [188–190], PDT [191], cancer imaging [192] and antitumor immunity mediation [193, 194]. Compared with other carbon materials, research on carbon QDs is in its rising stage. Major obstacles in clinical translation of QDs are lack of standard protocol in high-quality QD production and their exact reaction mechanism and formation process [195].
Metallic and magnetic nanomaterials
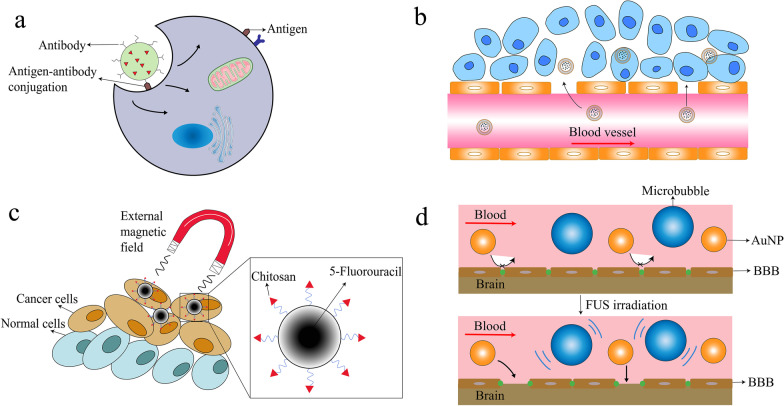
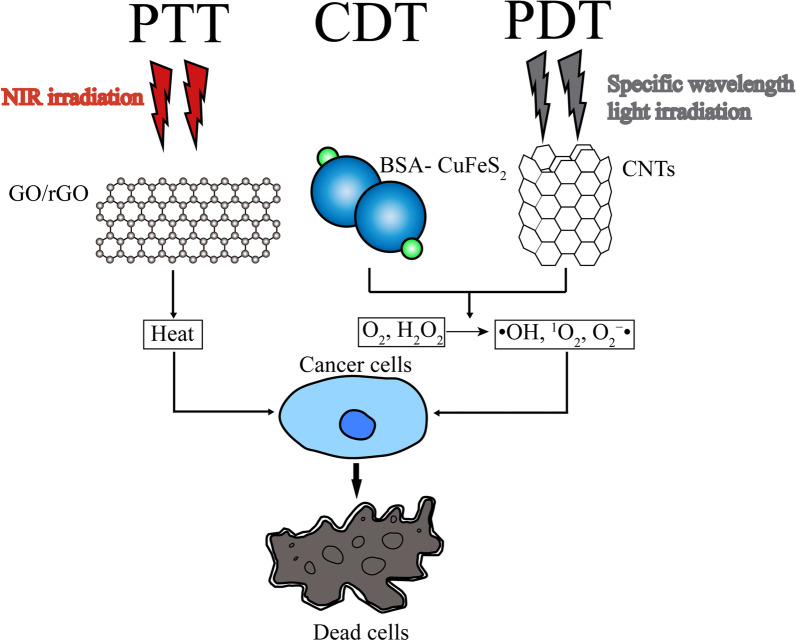
Metallic nanoparticles have been extensively studied in bio-imaging and drug delivery because of their distinct optical, magnetic, and photothermal features. Metallic materials can be used in many forms in conjugation with versatile carriers such as NPs, liposomes, dendrimers or CNMs. Magnetic nanomaterials are mainly applied in MRI imaging. Guided by external magnetic field, magnetic NPs loaded with chemical drugs can target cancer cells, and therefore side effects of conventional chemotherapy are reduced [196] (Fig. 3). With metal particle conjugated, the nanosystem possesses both bio-imaging and PTT function. Iron oxide nanoparticles (IONPs) consisting of Fe3O4/Ag were encapsulated with a gold shell. MRI contrast capability was showed from IONPs and PTT due to the gold shell in the NIR region [37]. In cancer treatment, metallic materials are widely used in PTT, PDT, CDT, and immunotherapy. CDT is a Fenton or Fenton-like reaction-based therapeutic modality that relies on nanocatalyst [197]. Similar to PDT, highly oxidative hydroxyl radicals (·OH) are produced and toxic ·OH radicals take effect in cancer cells by triggering chain reactions with surrounding organic molecules, eventually leading to irreversible damage to DNA, lipids, and proteins [198]. During the process, iron-based nanostructures including FeS2, Fe2P, Fe3O4, SnFe2O4, and amorphous iron are used to catalyze disproportionation of H2O2 to generate ·OH radicals [38, 199, 200]. For PTT and PDT, as NIR possesses much stronger tissue penetration ability than ultraviolet (UV) and visible light, NIR triggered materials are crucial in these therapies. In PTT, cancer cells are eliminated to the generation of thermal energy, while ROS including ·OH, singlet oxygen (1O2), and superoxide (O2 − ·) induce cytotoxic reactions in PDT [201]. Au (gold), Cu (copper), Fe (iron) are commonly used metallic materials in these therapies [202–204] (Fig. 2). The disadvantage of metallic nanomaterials lies in their toxicity. Attarilar et al. summarized the mechanisms of metallic NPs: ROS generation and influence on cell structures, characteristics of metallic NP toxicity are similar to other NPs, that toxicity is related to size, shape, dimensionality, surface charge [205]. Therefore, metallic NPs should be carefully examined before use on human patients.
Fig. 3.
Illustration of interaction between nanomaterials and tumor cells. a Antigen–antibody conjugation modified nanoparticle endocytosis and transcytosis; b Liposome reaches cancerous area from blood vessels through EPR effect. c The magnetic nanoparticle coated with chitosan carries 5-Fluorouracil. Under external magnetic field, the nanoparticle shows passive targeting ability at cancer cells. d Therapeutic AuNP is blocked by BBB under normal status. After FUS exposure, the BBB is opened temporarily by microbubble inertial or stable cavitation and allows AuNPs to get through. BBB: blood–brain barrier; EPR: enhanced permeability and retention; FUS: focused ultrasound
Fig. 2.
Schematic illustration of nanomaterial involved PTT, CDT, PDT. With NIR irradiation, PTT materials such as GO/rGO generate heat and cause cancer cell death. CDT material BSA-CuFeS2 and specific wavelength light irradiated PDT material CNTs generate ·OH, 1O2, O2 − · from O2, H2O2 in cells and cause cancer cell death. CDT, chemodynamic therapy; CNT: carbon nanotube; GO: graphene oxide; NIR: near-infrared; PDT: photodynamic therapy; PTT, photothermal therapy; rGO: reduced graphene oxide
Cancer treatment and nanomaterial design
Approaches in cancer treatment
To date, several mainstream approaches toward cancer treatment have been broadly applied to tackle cancer. Moreover, despite differences in working platforms, functional ingredients, and mechanisms, most researchers adopt two main targets: tumor cells and TME which include the immune system related to the tumor (Fig. 3).
Strategies targeting cancer cells
Targeting cancer cells is a natural method to eliminate cancer. With EPR and active targeting, modified nanocarriers such as NPs, dendrimers, or CNMs can reach cancer cells and release chemical drugs or biomaterials [206, 207]. Antibodies targeting specific antigens overexpressed on cancer cell surfaces are widely used in these platforms. After endocytosis by cancer cells, encapsulated chemical drugs exert cytotoxicity or nucleic acid materials induce cell apoptosis, depending on the encapsulated cargo. Progress has been made in nucleic acid delivery and nano-DDS based on exosomes [72, 78], PNPs, liposomes [208], dendrimers [115] are massively researched in cancer therapy.
Strategies targeting TME
Another strategy is about the TME that contain tumor cells. As mentioned above, angiogenesis is extremely active in almost all tumors because of uncontrolled cell proliferation and massive energy is needed for that. Research on this specific characteristic showed promising results. Sengupta designed a NP system specifically targeting abnormal tumor angiogenesis with combretastatin, and this medicine was co-encapsulated into the PLGA core with DOX. As a result, the DOX was efficiently taken up by the tumor after a rapid shutdown of the cancerous vessels induced by combretastatin, and an improved overall therapeutic index was achieved along with reduced toxicity [209]. In addition to abnormal vasculature, extracellular matrix (ECM) has also been researched in cancer treatment. ECM acts as a guiding scaffold in cancer proliferation, migration, invasion and angiogenesis [210]. Several main materials contributing to these cancerous properties are collagen, HA, various enzymes. As the main structural protein of the ECM, collagen forms migration tracks for tumor cells, while HA contributes to high interstitial fluid pressure (IFP), preventing drug diffusion and penetration [211, 212]. Enzymes, for example, matrix metalloproteinases (MMPs), can regulate TME by manipulating the activity of non-ECM molecules, including growth factors, receptors, and cytokines [213]. In nanocarrier design, ECM is one of the factors to be considered. Combined with conventional chemical drugs, recombinant human hyaluronidase (PEGPH20) in PEGylated form that targets at ECM hyaluronic acid exerted therapeutic effects for metastatic pancreatic cancer patients, especially in those with high hyaluronidase expression [214]. Efforts have been made to enhance chemical drugs loaded nanocarrier penetration ability in solid tumors by coating carriers with hyaluronidase (HAase) (Fig. 4b). This simple but effective strategy shows better anti-tumor efficacy [215].
Nanomaterials and cancer immunotherapy
The immune system plays a vital role in cancer formation and progression. There are several approaches in immunotherapy including immune checkpoint blockade therapy, chimeric antigen receptor (CAR)-T cell therapy, cancer vaccine therapy and immune system modulator therapy [216]. In these cancer immunotherapies, natural molecules or synthetic molecules are used to enhance or restore immune system function and exert anti-tumor effect. Programmed cell death protein 1 (PD-1) and programmed cell death ligand 1 (PD-L1) are important immune checkpoints and immune check point inhibitors (ICIs) targeting PD-1/PD-L1 has been researched to be loaded in nanocarriers targeting cancer [217]. In a research conducted by Bu and colleges, over-expression of PD-1 was considered to allow cancer cells to perform antitumor immunity evasion, and traditional immune checkpoint inhibitors (ICIs) of PD-1/PD-L1 showed inconsistent benefits. To ensure bonding of PD-L1 and ICIs, multivalent poly (amidoamine) dendrimers were employed; as a result, PD-L1 blockade effect was improved, and tumor site drug accumulation was enhanced [218]. CTLA-4 (cytotoxic T-lymphocyte-associated protein 4) is as an immune checkpoint with the function to downregulate immune responses [219]. Among these molecules are antibodies, small molecular inhibitors, proteins. Nanomaterials play an important role as drug vehicles to deliver these moieties (Table 4). Through these strategies, novel nanoplatforms can be developed and might achieve better efficacy and bioavailability than conventional therapies (Fig. 4) [106, 134].
Table 4.
Nanomaterials applied in cancer immunotherapy
| Name of drug | Component | Cancer types tested | Outcome | References |
|---|---|---|---|---|
| G7-aPD-L1 | Dendrimer and anti-PD-L1 antibody | Human renal carcinoma and breast cancer cells | G7-aPD-L1 showed significantly enhanced binding strength to PD-L1 proteins compared to free aPD-L1 | [218] |
| Doxil synergized with mAbs | Liposomal doxorubicin, anti-PD-1 and CTLA-4 mAbs | Mouse colon cancer cells and mouse fibrosarcoma cells | Doxil synergized with anti-PD-1 and CTLA-4 mAbs in a preventative CT26 mouse tumor model and Doxil activity increased in the presence of a functional immune system | [220] |
| NPsiCTLA-4 | Nanoparticle, CTLA-4 siRNA | B16 melanoma mouse model | NPsiCTLA-4 delivered CTLA-4-siRNA into tumor sites and affected T cell subsets, exhibiting augmented T cell activation. Induced anti-tumor immune responses | [221] |
| NP-based mRNA vaccine | Nanoparticle, mRNA encoding tumor antigen Mucin-1 | Mouse triple negative breast cancer cells and female BALB/c mice | The NP-based mRNA vaccine successfully expressed tumor antigen in mouse lymph node and a synergic anti-tumor effect was shown | [222] |
| rGO/MTX/SB | rGO, MTX, transforming growth factor beta inhibitor SB-431542 (SB) | Triple negative breast cancer mouse model | A synergistic chemo-immuno-photothermal anti-tumor effect by in situ vaccination and TME inhibition was exhibited after laser irradiation | [223] |
| IFN-γNE2 | Nanoemulsion, IFN-γ | Human breast cancer cells | IFN-γNE2 reduced MCF-7 cell viability without affecting phagocytes and induced cellular activity of phagocytes | [107] |
CTLA-4, Cytotoxic T-lymphocyte-associated protein 4; mAbs, Monoclonal antibodies; MTX, Methotrexate; IFN-γ, Cytokine Interferon gamma; NE, Nanoemulsions; PD-L1, Programmed cell death ligand 1; rGO, Reduced graphene oxide
Advantages and challenges of nanomaterial applications in cancer therapy
Nanomaterials applied in cancer therapy have advantages over conventional chemical drugs as well as challenges in application. Several significant hallmarks in tumorigenesis and tumor development have been elucidated: continuous proliferative signaling, growth suppressors evasion, cell death resistance, replicative immortality, induced angiogenesis, activating invasion and metastasis, inflammation, genomic instability, and mutation [224, 225]. Traditional chemotherapy and radiotherapy have disadvantages in efficacy and side effects because of unspecific distribution and indiscriminate cytotoxicity to cancer cells and normal cells. Therefore, a delicate balance of dosing and an advanced targeting DDS is of great importance in cancer treatment [226]. To reach cancerous target sites, chemical drugs taken orally or intravenously shall pass several “fortifications”: TME and vasculature, MPS, BBB and kidney filtration. In physiological conditions, barriers like normal tissue microenvironment, vasculature, RES, BBB, and kidney filtration contribute significantly to pathogen resistance. However, in cancer treatment, intake of anticancer chemical drugs is affected by these defenses. Cancer cells hold a different proliferation pattern than normal cells. Cancer tissues exhibit distinctly in the dense extracellular matrix, over-activated angiogenesis induced by excessive angiogenic factors and high interstitial fluid.
Nanomaterial and drug metabolism
Drug metabolism is a complex process. MPS, also called as reticuloendothelial system or macrophage system [227], consists of blood monocytes, tissue macrophages, and other immune cells. When dealing with extrinsic molecules, in this case, chemical drugs, parts of the MPS such as immune cells in the liver, spleen, or lungs will react, and activated macrophages or leukocytes quickly eliminate the drugs, causing short drug half-life [228]. Nanocarriers with surface modification such as PEG or specific peptide possess lower MPS clearance and therefore prolong drug half-life [229]. Kidney filtration is an essential function of the renal system. Renal clearance rate associates with several properties, including particle size, shape, and surface charge. For traditional chemical drugs, renal clearance is one of the key points needed in drug delivery [230]. Proper renal clearance helps to minimize toxicity of nanocarrier. These barriers are obstacles for many conventional drug deliveries, diminishing drug efficacy in cancerous sites and indirectly increasing dosage and toxicity for normal tissue.
Nanomaterials and BBB
The BBB is a highly specialized protection structure that protects the central nervous system from harmful agents and provides essential nutrition. BBB consists of brain capillary endothelial cells, which are arranged to form a “wall.” Due to the blocking function of BBB, current post-surgery chemotherapy methods for brain cancer are mainly intraventricular or intracerebral direct injections, infusion, even implantation. However, these methods aiming at increased permeability might result in risks associated with high toxicity or inadequate drug distribution, that demands for a better solution to deliver anticancer drugs through BBB [231]. In brain tumor treatment, conventional free chemical drugs are hard to reach cancerous sites through intravenous method due to BBB, and nanomaterials are researched to overcome this obstacle. EPR effect, peptide-modified endocytosis and transcytosis, focused ultrasound (FUS) are major approaches currently utilized to help deliver nanomaterials (Fig. 3). Several nanomaterials have been researched for delivery through BBB, including NLCs [232], liposomes, and AuNPs. A glutathione PEGylated liposome loaded with methotrexate (MTX) was tested in rats and the result showed the nanocarrier improves the brain uptake of MTX [233]. AuNPs are vastly researched among these materials. Research concerning glioma and other intracranial cancers are conducted mainly in the mouse model, and the result shows that EPR effect allows gold nanoparticles (AuNPs) of certain size to accumulate in the tumor [234]. To gain better specificity, inorganic NPs such as AuNPs can also be modified with peptides and antibodies on the surface. AuNPs and gold liposomes are used as biocargo for chemical drugs and nucleic acid, and AuNPs are also used in PTT and immune therapy. Ruan et al. fabricated a novel NP AuNPs-A&C-R that were composed of two functional particles, and both particles were peptide modified AuNPs. Peptide attached on the surface helps mediate AuNPs-A&C-R transcytosis across BBB and target receptors on glioblastoma cell surface. This AuNP loaded DOX and showed better chemotherapeutic effect than free DOX treatment [235]. Research indicates that ultrasound can widen BBB tight junction therefore offers a temporary pathway for NPs to get through, and size of AuNPs affects delivery efficiency. This research shows ultrasound might help AuNPs with therapeutic function to penetrate BBB with ultrasound treatment [236] (Fig. 3). Current mouse experiments show that modified AuNPs can help transport chemical drugs, induce lethal autophagy and apoptosis [237] and exert photothermal effect in intracranial cancer PTT [238].
Targeting strategies of nanomaterials applied to cancer therapy
Targeted therapy aims at specific biological pathways or proteins that function in tumor growth. Molecules related to apoptosis and angiogenesis are also common targets in targeted therapies. Small molecules inhibitors and mAbs are two major tools to be utilized in targeted therapies [14]. Through antigen–antibody conjugation, better specificity can be achieved. Compared with non-targeted therapies, free chemical drugs for example, targeted therapies specifically affect tumor-related molecular targets, while free chemical drugs kill both rapidly dividing normal cells and cancer cells. NPs loaded with targeted therapy drugs or modified with specifically targeted mAbs in the surface gain better efficacy and lower toxicity compared to nanocarriers loaded with anti-tumor chemical drugs (Table 1).
The EPR effect is a fundamental mechanism applied in nanocarrier targeting strategy. Passive targeting based on EPR effect involves interactions between the nanoplatform and TME, MPS, and barriers in the human body. It should be noted that EPR also functions in active targeting strategy achieved by conjugating with antibodies, peptides, aptamers and small molecules, and the efficacy of active targeting is affected by MPS, immune system, and other nanocarrier–environment interactions. Both passive targeting and active targeting strategies are used in DDS design. By loading the nanocarrier or modifying the surface with therapeutic ingredients in targeted therapy, the fabricated nanoplatform can be utilized to improve current targeted therapy and achieve better efficacy.
Current challenges of nano-DDS designing
Three key issues should be considered in anti-cancer nano-DDS designing: enhancement of efficacy, reduction of side effects, and resistance prevention. In many cases, a nano-DDS can solve several problems simultaneously due to instinct mechanism. A SLN synthesized with the material dexamethasone (Dexa)-conjugated lipid is linked with PEG-phosphatidylethanolamine (PEG-PE) and obtains Tf (transferrin)-PEG-PE ligands. As many cancer cells over-express the Tf receptor and use it to obtain certain molecular epitope, Tf is considered the target moiety that binds to the TfR molecular on the HepG2 cells [239]. This kind of surface modification makes it a better delivery vehicle for gene, and the experiment shows that it displays remarkably higher transfection efficiency than both non-modified SLNs/pEGFP and vectors that do not contain Dexa in vitro or in vivo [240]. The increased specificity results in higher drug accumulation in targeted cancer sites than other vital organs, leading to reduced toxicity and drug-related MDR prevention [241].
Despite rapidly growing research concerning nanomaterials in cancer treatment, some issues still remain unsolved. Toxicity is still one of the main concerns of nanomaterials. Because of the extremely small size, physiological barriers can be penetrated through, which may pose potential health hazards [242]. Evidence shows that cellular membranes, organelles, and DNA suffer from free radicals caused by NPs [243]. Nanomaterials delivered intracellularly might stimulate an immune response by reacting with cell surface receptors [244, 245]. As referred to above, nanomaterial toxicity relates to many factors and thus, modification to reduce toxicity is essential in the fabrication process.
As the primary passive delivery method utilizing nanomaterials, the EPR effect has been closely studied for a long time. However, most designed nanomaterials failed to reach the stage of clinical use. Some researchers tried to re-consider the concept of EPR and explore the real efficacy of this “royal gate” toward cancer treatment. The EPR effect works in rodents differently as in humans [246]. Sindhwani et al. investigated the mechanism by which NPs enter solid tumors. The experiments used four different mouse models, three types of human tumor cells, mathematical simulation and modeling, two imaging techniques, and the results were stunning. The frequency of gaps in tumors did not account for nanoparticle accumulation in tumor. Trans-endothelial pathways were the dominant mechanism of nanoparticle tumor extravasation. Finally, combined evidence from TEM and 3D microscopy showed that there were not enough gaps, which resulted in rare opportunities for cancer nanomedicine to enter tumors passively [247]. These studies indicate that the differences in EPR efficacy in various cells and tissues need further investigations. Studies have been conducted to stratify cancer patients by accumulating NPs through EPR and to find predictive EPR markers [248, 249]. These results indicate that the EPR effect varies in different species and tumors. To better exploit the EPR effect in cancer therapy, more research is needed to explore different patterns and efficiencies of the EPR effect and elucidate the mechanism of nano-carrier transport.
Another knotty obstacle of nanomaterial implementation in cancer treatment lies in clinical translation. Although plenty of nanocarrier research for cancer therapy has been conducted (Table 5), most of these researches involve cell and animal models that may not reflect coherent responses in actual human organs. A single model is hard to imitate real reaction in the human body, and previous studies exhibited more consistency of EPR in animals than in human patience [250]. Models of cancer metastasis should also be considered in research as metastasis is common for malignant cancers. The specific solution to these problems is hard to reach; however, innovative modeling methods can be explored to accelerate the process. Biomimetic ‘organ/tumor-on-a-chip’ tools, organoid model systems are possible solutions to imitate in vivo situation of nanocarriers used in cancer patients [251–253]. Proper animal models are also recommended in these assessments. Properties of nanomaterials, including size, shape, chemical composition, surface charge, have an enormous influence on nanocarriers' overall efficacy, and adjustment of these properties needs researchers' cooperation in both medicine and material fields. So far, approved nanocarriers used in cancer therapies are mostly liposomes and nanoparticles, and nanocarriers with more complex structures and manufacturing procedures generally face greater difficulties in clinical translation (Table 5). Searching for technology that helps manufacture vast nanomaterials with combined required properties is one important goal in anticancer nanomaterial clinical translation.
Table 5.
Examples of nanocarriers for anticancer therapy
| Nanotechnology platform | Description | Pharmaceutical ingredients | Disease | Status | References |
|---|---|---|---|---|---|
| PNP | Decorated with somatostatin analogue | Cetuximab | Colon cancer | Phase 1 | NCT03774680 |
| NP | Combined with enzalutamide | Camptothecin | Metastatic castration resistant prostate cancer | Phase 2 | NCT03531827 |
| NP | Co-coated drug | Nab-paclitaxel rituximab | B-Cell Non-Hodgkin Lymphoma | Phase 1 | NCT03003546 |
| Liposome | Liposome | irinotecan | Small cell lung cancer | Phase 3 | NCT03088813 |
| Liposome | Pegylated liposomal carrier | Doxorubicin trastuzumab | HER2-positive metastatic breast cancer | Phase 2 | NCT03933319 |
| Nanoemulsion | Photosensitizer in PDT therapy | Aminolevulinic acid nanoemulsion | Basal cell carcinomas | Phase 2 | NCT02367547 |
| Quantum dot | Coated with drug | veldoreotide | Breast cancer | Phase 1 | NCT04138342 |
| Albumin NP | NP bound albumin (Abraxane) | Paclitaxel | Breast cancer, NSCLC, pancreatic cancer | Approved by FDA | [254] |
| Liposome | Liposome (DepoCyt) | Cytarabine | Lymphomatous malignancies | Approved by FDA | [255] |
| Liposome | Liposome (Marqibo) | Vincristine sulfate | Acute lymphoblastic leukemia | Approved by FDA | [256] |
| Liposome | Liposome (Doxil) | Doxorubicin | HIV-related Kaposi sarcoma, ovarian cancer, multiple myeloma | Approved by FDA | [19] |
| Liposome | Liposome (DaunoXome) | Daunorubicin | HIV-related Kaposi sarcoma | Approved by FDA | [257] |
| Polymer protein conjugate | Multi-agent chemotherapy-eutic regimen (Oncaspar) | L-asparaginase | leukemia | Approved by FDA | [258] |
NP, nanoparticle; PDT, Photodynamic therapy; PNP, Polymeric nanoparticle
US Clinical trials website (http://clinicaltrials.gov/) [259]–US Food and Drug Administration website (http://www.accessdata.fda.gov/) [260]
Proteomics and anti-cancer nanoplatform design
When injected into a biological system, nanomaterials are surrounded by serum and cellular proteins, structures formed by these substances are termed protein corona (PC) [261]. Searching for technology that helps manufacture vast nanomaterials with combined required properties is one important goal in anticancer nanomaterial clinical translation. It has been found that since different binding affinities toward NPs are shown by proteins, “hard” corona can form with higher binding affinity proteins, while “soft” corona forms with proteins that bind loosely to nanoparticles. As a result, the most abundant proteins that form a PC first, with time they will be replaced by the proteins with higher affinities. This phenomenon is named as Vroman effect [262]. Various proteomic methods have been used in PC research, especially in quantitative analysis: MS, LC–MS, SDS-PAGE [263], surface plasmon resonance (SPR), isothermal microcalorimetry (ITC). PC affects the interaction of NP with biological environment and therefore, determines whether a NP carrier could be applied in medical use to a degree. Thus, proteomic methods help study NP-protein interaction and achieve a deeper understanding of PC formation.
Cancer proteomics analyzes protein quantity in cancer cells and serum, which helps find proteins and surface biomarkers useful in cancer diagnosis and prognosis [264]. Proteomics has also been applied to help understand cancer pathogenesis, elucidate the mechanism of drug resistance, and search for biomarkers for early detection of cancer [265]. In the pathological process, PTMs (post-translational modifications) are important mechanisms related to cancer occurrence, metastasis and reoccurrence, and kinase plays essential roles in these modifications and pathways. Although chemical drugs are the current focus of research, kinase inhibitors and other novel therapeutic agents such as siRNA, mRNA, and gene editing materials cognized through cancer proteomics approaches can be loaded within a nanocarrier to achieve higher drug efficacy. New molecular targets can also be identified by proteomic methods, enriching currently recognized targeting moieties. High throughput proteomics and many novel ways are also enhancing the capability of proteomic methods to identify specific molecules potential for manufacturing anticancer nanocarriers.
Conclusions
Nanomaterials share similar size but differ in composition, structure, hydrophobicity, magnetism, immunogenicity and other properties. Cancer therapies based on these unique properties have been vastly researched. In general, various surface modification can be achieved on different nanomaterials, and in many cases, conventional anti-tumor chemical drugs can be loaded into different nanocarriers. It is crucial for researchers to be well aware of the characteristics of the selected nanoplatform as well as properties of therapeutic agents. For instance, EVs are biocompatible vesicles with ability to escape the immune surveillance and internalize smoothly with target cells, a possible strategy might be using antibody modified EV to deliver key gene therapy agents to targeted cancer cells. Based on photothermal properties CNTs and metallic materials possess, nanoplatform functions with chemotherapy and PTT can be designed to produce synergistic effect. CNTs have the potential to achieve better anti-tumor efficacy for the feature that they can provide several kinds of therapies at the same time. Both targeted delivery and non-targeted delivery employ nanomaterials as vehicles to transport chemical drugs, peptide/protein molecules, small molecule inhibitors or use the material as immune system stimulant, photothermal medium, chemodynamic medium. Modification of the nanomaterial platform including inner content and external moiety plays an important role in the efficacy, targeting ability, biocompatibility and toxicity of the nanoplatform complex.
In this article, we mainly focus on characteristics of common nanomaterials and progress of their application in cancer therapy rather than the chemical synthesis process and drug-loading technique which are also important issues limiting clinical translation of nanomaterials. Targeting therapy and immunotherapy that involve molecules in newly discovered pathways are being massively researched. It is expected in the future, with development in proteomic research on mechanism of cancer genesis, MDR occurrence, more nanomaterial-based targeting therapy and immunotherapy approaches will be explored.
Compared to the enormous amount of research, only a few nanomaterial-based drugs are applied in clinical. To improve this situation, more efforts should be taken into toxicity reduction, illumination of EPR and PC mechanism in the human body. It is expected that in the near future, nanoplatforms will be designed to target not only on cancer cells, but also on the TME environment including immune system. Precise targeting methods, TME triggered release strategy, combined therapies, self-assembly nanoplatform are practical approaches to enhance targeting specificity, drug capacity, efficacy, bioavailability; and reduce the toxicity of nanomaterials and loaded drugs toward normal cells. Testing nanomaterials in models that resemble more in vivo environment is also an important issue to be considered. Overall, with the advancement of nanobiotechnology and cancer therapy development, we believe that the breakthrough in clinical translation for treating cancer, a deadly disease, will be achieved, and more nanomaterial-based drugs will benefit cancer patients.
Acknowledgements
Not applicable.
Abbreviations
- 5-ALA
5-Aminolevulinic acid
- AA-PEG
Aminoethylanisamide-polyethylene glycol
- ABCs
ATP-binding cassette transporters
- ADCs
Antibody–drug conjugates
- AuNPs
Gold nanoparticles
- BBB
Blood–brain barrier
- Bis-MPA
2,2-Bis(hydroxymethyl) propionic acid
- CA
Citric acid
- CAR
Chimeric antigen receptor
- Cas
CRISPR-associated proteins
- CDP
Cyclodextrin polymer
- CDs
Carbon dots
- CDT
Chemodynamic therapy
- Ce6
Chlorin e6
- CL
Cationic liposome
- CMCS
Carboxymethyl chitosan
- CNHs
Carbon nanohorns
- CNTs
Carbon nanotubes
- CQDs
Carbon quantum dots
- CRISPR
Clustered regularly interspaced short palindromic repeats
- CSCs
Cancer stem cells
- CTLA-4
Cytotoxic T-lymphocyte-associated protein 4
- DDS
Drug delivery system
- Dexa
Dexamethasone
- DOX
Doxorubicin
- ECM
Extracellular matrix
- EPR
Enhanced permeability and retention
- EVs
Extracellular vesicles
- exoDOX
Exosomes loaded with DOX
- FA-SGQDs
Folic acid to sulfur-doped graphene quantum dots
- FNPs
Fluorescent polymeric nanoparticles
- FUS
Focused ultrasound
- GDY
Graphyne
- GO
Graphene oxide
- GQDs
Graphene quantum dots
- GSH
Glutathione
- HA
Hyaluronic acid
- HAase
Hyaluronidase
- HER2
Human epidermal growth factor receptor 2
- HPRG
Histidine–proline-rich glycoprotein
- HREC
Human retinal endothelial cells
- ICIs
Immune check point inhibitors
- IFN-γ
Cytokine Interferon gamma
- IFP
High interstitial fluid pressure
- IHC
Immunohistochemical
- ING4
Inhibitor of growth 4
- IONPs
Iron oxide nanoparticles
- ITC
Isothermal microcalorimetry
- L-DOX
Liposomal doxorubicin
- LUV
Large unilamellar vesicles
- mAbs
Monoclonal antibodies
- MDR
Multi-drug resistance
- MEK/ERK
Mitogen-activated protein kinase kinase/extracellular signal regulated protein kinase
- miR-497
MiRNA-497
- miRNAs
MicroRNAs
- MLV
Multilamellar vesicles
- MMPs
Matrix metalloproteinases
- MPA
Mercaptopropionic acid
- MPS
Mononuclear phagocyte system
- MTX
Methotrexate
- MWCNTs
Multiwalled carbon nanotubes
- NE
Nanoemulsions
- NIR
Near-infrared
- NLCs
Nanostructured lipid carriers
- NPs
Nanoparticles
- NSTI
Nanoscience, technology, and industry
- OS
Osteosarcoma
- PA
Photoacoustic
- PAMAM
Polyamidoamine
- PC
Protein corona
- PCL
Poly(ε-caprolactone)
- PCX
Etoposide and paclitaxel
- PD-1
Programmed cell death protein 1
- PD-L1
Programmed cell death ligand 1
- PDT
Photodynamic therapy
- PEG
Poly(ethylene glycol)
- PEG-PE
PEG-phosphatidylethanolamine
- P-gp
P-glycoprotein
- PI3K/mTOR
Phosphoinositide 3-kinase/mammalian target of rapamycin
- PLA
Polylactic acid
- PLGA
Poly(lactic-co-glycolic acid)
- PMMA
Polymethyl methacrylate
- PNPs
Polymeric nanoparticles
- PPI
Polypropylenimine
- PTEN
Phosphatase and tensin homolog
- PTMs
Post-translational modifications
- PTT
Photothermal therapy
- PTX
Paclitaxel
- rGO
Reduced graphene oxide
- RGD
Arginine-glycine-aspartic
- RNAi
RNA interference
- ROS
Reactive oxygen species
- SDT
Sonodynamic therapy
- Sf
Sorafenib
- Si
SiRNA
- siRNA
Small interfering RNAs
- SLNs
Solid lipid nanoparticles
- SPION
Superparamagnetic iron oxide nanoparticles
- SPR
Surface plasmon resonance
- SUV
Small unilamellar vesicles
- SWCNTs
Single-walled carbon nanotubes
- TEA
Triethanolamine
- Tf
Transferrin
- TLR4/NF-κB
Toll-like receptor 4/nuclear factor kappa B
- Tmab
Trastuzumab
- TME
Tumor microenvironment
- TNF-α
Tumor necrosis factor alpha
- TPGS
Tocopheryl polyethylene glycol 1000 succinate
- TRAIL
Tumor necrosis factor-related apoptosis-inducing ligand
- UV
Ultraviolet
- VEGF
Vascular endothelial growth factor
Authors' contributions
YC conceived and supervised the project; ZC wrote the paper, ML and RD provided critical suggestions; ZC revised the paper. All authors read and approved the final manuscript.
Funding
This work was supported by grants from the National Natural Science Foundation of China (81974074 and 81570537), Outstanding Youth Project of Hunan Education Department (19B475).
Availability of data and materials
Not applicable.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Zhe Cheng and Maoyu Li have contributed equally to this work.
References
- 1.Lopez-Soto A, Gonzalez S, Smyth MJ, Galluzzi L. Control of metastasis by NK cells. Cancer Cell. 2017;32(2):135–154. doi: 10.1016/j.ccell.2017.06.009. [DOI] [PubMed] [Google Scholar]
- 2.Gallaher JA, Enriquez-Navas PM, Luddy KA, Gatenby RA, Anderson ARA. Spatial heterogeneity and evolutionary dynamics modulate time to recurrence in continuous and adaptive cancer therapies. Cancer Res. 2018;78(8):2127–2139. doi: 10.1158/0008-5472.CAN-17-2649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nigro JM, Baker SJ, Preisinger AC, Jessup JM, Hostetter R, Cleary K, Bigner SH, Davidson N, Baylin S, Devilee P, et al. Mutations in the p53 gene occur in diverse human tumour types. Nature. 1989;342(6250):705–708. doi: 10.1038/342705a0. [DOI] [PubMed] [Google Scholar]
- 4.Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424. doi: 10.3322/caac.21492. [DOI] [PubMed] [Google Scholar]
- 5.The L. GLOBOCAN 2018: counting the toll of cancer. Lancet. 2018;392(10152):985. doi: 10.1016/S0140-6736(18)32252-9. [DOI] [PubMed] [Google Scholar]
- 6.Mortezaee K, Salehi E, Mirtavoos-Mahyari H, Motevaseli E, Najafi M, Farhood B, Rosengren RJ, Sahebkar A. Mechanisms of apoptosis modulation by curcumin: implications for cancer therapy. J Cell Physiol. 2019;234(8):12537–12550. doi: 10.1002/jcp.28122. [DOI] [PubMed] [Google Scholar]
- 7.Galon J, Pagès F, Marincola FM, Angell HK, Thurin M, Lugli A, Zlobec I, Berger A, Bifulco C, Botti G, Tatangelo F, Britten CM, Kreiter S, Chouchane L, Delrio P, Arndt H, Asslaber M, Maio M, Masucci GV, Mihm M, Vidal-Vanaclocha F, Allison JP, Gnjatic S, Hakansson L, Huber C, Singh-Jasuja H, Ottensmeier C, Zwierzina H, Laghi L, Grizzi F, et al. Cancer classification using the immunoscore: a worldwide task force. J Transl Med. 2012;10:205. doi: 10.1186/1479-5876-10-205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhang Y, Li M, Gao X, Chen Y, Liu T. Nanotechnology in cancer diagnosis: progress, challenges and opportunities. J Hematol Oncol. 2019;12(1):137. doi: 10.1186/s13045-019-0833-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cryer AM, Thorley AJ. Nanotechnology in the diagnosis and treatment of lung cancer. Pharmacol Ther. 2019;198:189–205. doi: 10.1016/j.pharmthera.2019.02.010. [DOI] [PubMed] [Google Scholar]
- 10.Chen Q, Ke H, Dai Z, Liu Z. Nanoscale theranostics for physical stimulus-responsive cancer therapies. Biomaterials. 2015;73:214–230. doi: 10.1016/j.biomaterials.2015.09.018. [DOI] [PubMed] [Google Scholar]
- 11.Jardim GAM, Lima DJB, Valenca WO, Lima DJB, Cavalcanti BC, Pessoa C, Rafique J, Braga AL, Jacob C, da Silva Junior EN, da Cruz EHG. Synthesis of selenium-quinone hybrid compounds with potential antitumor activity via Rh-catalyzed C–H bond activation and click reactions. Molecules. 2017;23(1):83. doi: 10.3390/molecules23010083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Arruebo M, Vilaboa N, Saez-Gutierrez B, Lambea J, Tres A, Valladares M, Gonzalez-Fernandez A. Assessment of the evolution of cancer treatment therapies. Cancers (Basel) 2011;3(3):3279–3330. doi: 10.3390/cancers3033279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wu Q, Yang Z, Nie Y, Shi Y, Fan D. Multi-drug resistance in cancer chemotherapeutics: mechanisms and lab approaches. Cancer Lett. 2014;347(2):159–166. doi: 10.1016/j.canlet.2014.03.013. [DOI] [PubMed] [Google Scholar]
- 14.Perez-Herrero E, Fernandez-Medarde A. Advanced targeted therapies in cancer: drug nanocarriers, the future of chemotherapy. Eur J Pharm Biopharm. 2015;93:52–79. doi: 10.1016/j.ejpb.2015.03.018. [DOI] [PubMed] [Google Scholar]
- 15.Zhao CY, Cheng R, Yang Z, Tian ZM. Nanotechnology for cancer therapy based on chemotherapy. Molecules. 2018;23(4):826. doi: 10.3390/molecules23040826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lee YT, Tan YJ, Oon CE. Molecular targeted therapy: treating cancer with specificity. Eur J Pharmacol. 2018;834:188–196. doi: 10.1016/j.ejphar.2018.07.034. [DOI] [PubMed] [Google Scholar]
- 17.Wilkes GM. Targeted therapy: attacking cancer with molecular and immunological targeted agents. Asia Pac J Oncol Nurs. 2018;5(2):137–155. doi: 10.4103/apjon.apjon_79_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Islam MT, Ali ES, Uddin SJ, Islam MA, Shaw S, Khan IN, Saravi SSS, Ahmad S, Rehman S, Gupta VK, Gaman MA, Gaman AM, Yele S, Das AK, de Castro ESJM, de Moura Dantas SMM, Rolim HML, de Carvalho Melo-Cavalcante AA, Mubarak MS, Yarla NS, Shilpi JA, Mishra SK, Atanasov AG, Kamal MA. Andrographolide, a diterpene lactone from Andrographis paniculata and its therapeutic promises in cancer. Cancer Lett. 2018;420:129–145. doi: 10.1016/j.canlet.2018.01.074. [DOI] [PubMed] [Google Scholar]
- 19.Ali ES, Sharker SM, Islam MT, Khan IN, Shaw S, Rahman MA, Uddin SJ, Shill MC, Rehman S, Das N, Ahmad S, Shilpi JA, Tripathi S, Mishra SK, Mubarak MS. Targeting cancer cells with nanotherapeutics and nanodiagnostics: current status and future perspectives. Semin Cancer Biol 2020;69:52–68. [DOI] [PubMed]
- 20.Sharma P, Bhargava M. Applications and characteristics of nanomaterials in industrial environment. Res Dev (IJCSEIERD) 2013;3(4):63–72. [Google Scholar]
- 21.Song S, Qin Y, He Y, Huang Q, Fan C, Chen HY. Functional nanoprobes for ultrasensitive detection of biomolecules. Chem Soc Rev. 2010;39(11):4234–4243. doi: 10.1039/c000682n. [DOI] [PubMed] [Google Scholar]
- 22.Osaki T, Yokoe I, Sunden Y, Ota U, Ichikawa T, Imazato H, Ishii T, Takahashi K, Ishizuka M, Tanaka T, Li L, Yamashita M, Murahata Y, Tsuka T, Azuma K, Ito N, Imagawa T, Okamoto Y. Efficacy of 5-aminolevulinic acid in photodynamic detection and photodynamic therapy in veterinary medicine. Cancers (Basel) 2019;11(4):495. doi: 10.3390/cancers11040495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gao W, Wang Z, Lv L, Yin D, Chen D, Han Z, Ma Y, Zhang M, Yang M, Gu Y. Photodynamic therapy induced enhancement of tumor vasculature permeability using an upconversion nanoconstruct for improved intratumoral nanoparticle delivery in deep tissues. Theranostics. 2016;6(8):1131–1144. doi: 10.7150/thno.15262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Horst MF, Coral DF, Fernandez van Raap MB, Alvarez M, Lassalle V. Hybrid nanomaterials based on gum Arabic and magnetite for hyperthermia treatments. Mater Sci Eng C Mater Biol Appl. 2017;74:443–450. doi: 10.1016/j.msec.2016.12.035. [DOI] [PubMed] [Google Scholar]
- 25.Rosenblum D, Joshi N, Tao W, Karp JM, Peer D. Progress and challenges towards targeted delivery of cancer therapeutics. Nat Commun. 2018;9(1):1410. doi: 10.1038/s41467-018-03705-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Masood F. Polymeric nanoparticles for targeted drug delivery system for cancer therapy. Mater Sci Eng C Mater Biol Appl. 2016;60:569–578. doi: 10.1016/j.msec.2015.11.067. [DOI] [PubMed] [Google Scholar]
- 27.Vijayan V, Reddy KR, Sakthivel S, Swetha C. Optimization and charaterization of repaglinide biodegradable polymeric nanoparticle loaded transdermal patchs: in vitro and in vivo studies. Colloids Surf B Biointerfaces. 2013;111:150–155. doi: 10.1016/j.colsurfb.2013.05.020. [DOI] [PubMed] [Google Scholar]
- 28.Shastri VP. Non-degradable biocompatible polymers in medicine: past, present and future. Curr Pharm Biotechnol. 2003;4(5):331–337. doi: 10.2174/1389201033489694. [DOI] [PubMed] [Google Scholar]
- 29.Elsabahy M, Wooley KL. Design of polymeric nanoparticles for biomedical delivery applications. Chem Soc Rev. 2012;41(7):2545–2561. doi: 10.1039/c2cs15327k. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Martín-Saldaña S, Palao-Suay R, Aguilar MR, Ramírez-Camacho R, San Román J. Polymeric nanoparticles loaded with dexamethasone or α-tocopheryl succinate to prevent cisplatin-induced ototoxicity. Acta Biomater. 2017;53:199–210. doi: 10.1016/j.actbio.2017.02.019. [DOI] [PubMed] [Google Scholar]
- 31.Le Broc-Ryckewaert D, Carpentier R, Lipka E, Daher S, Vaccher C, Betbeder D, Furman C. Development of innovative paclitaxel-loaded small PLGA nanoparticles: study of their antiproliferative activity and their molecular interactions on prostatic cancer cells. Int J Pharm. 2013;454(2):712–719. doi: 10.1016/j.ijpharm.2013.05.018. [DOI] [PubMed] [Google Scholar]
- 32.Bellocq NC, Pun SH, Jensen GS, Davis ME. Transferrin-containing, cyclodextrin polymer-based particles for tumor-targeted gene delivery. Bioconjug Chem. 2003;14(6):1122–1132. doi: 10.1021/bc034125f. [DOI] [PubMed] [Google Scholar]
- 33.Zhang X, Liu J, Li X, Li F, Lee RJ, Sun F, Li Y, Liu Z, Teng L. Trastuzumab-coated nanoparticles loaded with docetaxel for breast cancer therapy. Dose Response. 2019;17(3):1559325819872583. doi: 10.1177/1559325819872583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Abedin MR, Powers K, Aiardo R, Barua D, Barua S. Antibody-drug nanoparticle induces synergistic treatment efficacies in HER2 positive breast cancer cells. Sci Rep. 2021;11(1):7347. doi: 10.1038/s41598-021-86762-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bao S, Zheng H, Ye J, Huang H, Zhou B, Yao Q, Lin G, Zhang H, Kou L, Chen R. Dual targeting EGFR and STAT3 with Erlotinib and Alantolactone co-loaded PLGA nanoparticles for pancreatic cancer treatment. Front Pharmacol. 2021;12:625084. doi: 10.3389/fphar.2021.625084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hadla M, Palazzolo S, Corona G, Caligiuri I, Canzonieri V, Toffoli G, Rizzolio F. Exosomes increase the therapeutic index of doxorubicin in breast and ovarian cancer mouse models. Nanomedicine (Lond) 2016;11(18):2431–2441. doi: 10.2217/nnm-2016-0154. [DOI] [PubMed] [Google Scholar]
- 37.Lin AY, Young JK, Nixon AV, Drezek RA. Encapsulated Fe3O4/Ag complexed cores in hollow gold nanoshells for enhanced theranostic magnetic resonance imaging and photothermal therapy. Small. 2014;10(16):3246–3251. doi: 10.1002/smll.201303593. [DOI] [PubMed] [Google Scholar]
- 38.Liu Y, Zhen W, Wang Y, Liu J, Jin L, Zhang T, Zhang S, Zhao Y, Song S, Li C, Zhu J, Yang Y, Zhang H. One-dimensional Fe(2) P acts as a Fenton agent in response to NIR II light and ultrasound for deep tumor synergetic theranostics. Angew Chem Int Ed Engl. 2019;58(8):2407–2412. doi: 10.1002/anie.201813702. [DOI] [PubMed] [Google Scholar]
- 39.Bernier-Latmani J, Petrova TV. Intestinal lymphatic vasculature: structure, mechanisms and functions. Nat Rev Gastroenterol Hepatol. 2017;14(9):510–526. doi: 10.1038/nrgastro.2017.79. [DOI] [PubMed] [Google Scholar]
- 40.Maeda H, Wu J, Sawa T, Matsumura Y, Hori K. Tumor vascular permeability and the EPR effect in macromolecular therapeutics: a review. J Control Release. 2000;65(1–2):271–284. doi: 10.1016/S0168-3659(99)00248-5. [DOI] [PubMed] [Google Scholar]
- 41.Singh N, Joshi A, Toor AP, Verma G. Drug delivery: advancements and challenges. In: Andronescu E, Grumezescu A, editors. Nanostructures for drug delivery. Elsevier; 2017. p. 865–886.
- 42.Krishnaswamy K, Orsat V. Sustainable delivery systems through green nanotechnology. In: Grumezescu A, editor. Nano-and microscale drug delivery systems. Elsevier; 2017. p. 17–32.
- 43.Andreiuk B, Reisch A, Lindecker M, Follain G, Peyriéras N, Goetz JG, Klymchenko AS. Fluorescent polymer nanoparticles for cell barcoding in vitro and in vivo. Small. 2017;13(38):1701582. doi: 10.1002/smll.201701582. [DOI] [PubMed] [Google Scholar]
- 44.Kang EB, Lee JE, Mazrad ZAI, In I, Jeong JH, Park SY. pH-Responsible fluorescent carbon nanoparticles for tumor selective theranostics via pH-turn on/off fluorescence and photothermal effect in vivo and in vitro. Nanoscale. 2018;10(5):2512–2523. doi: 10.1039/C7NR07900A. [DOI] [PubMed] [Google Scholar]
- 45.Subhan MA, Torchilin VP. Efficient nanocarriers of siRNA therapeutics for cancer treatment. Transl Res. 2019;214:62–91. doi: 10.1016/j.trsl.2019.07.006. [DOI] [PubMed] [Google Scholar]
- 46.Bartlett DW, Davis ME. Insights into the kinetics of siRNA-mediated gene silencing from live-cell and live-animal bioluminescent imaging. Nucleic Acids Res. 2006;34(1):322–333. doi: 10.1093/nar/gkj439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Tang C, Edelstein J, Mikitsh JL, Xiao E, Hemphill AH, 2nd, Pagels R, Chacko AM, Prud'homme R. Biodistribution and fate of core-labeled (125)I polymeric nanocarriers prepared by Flash NanoPrecipitation (FNP) J Mater Chem B. 2016;4(14):2428–2434. doi: 10.1039/C5TB02172C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Peltek OO, Muslimov AR, Zyuzin MV, Timin AS. Current outlook on radionuclide delivery systems: from design consideration to translation into clinics. J Nanobiotechnol. 2019;17(1):90. doi: 10.1186/s12951-019-0524-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Dey R, Xia Y, Nieh MP, Burkhard P. Molecular design of a minimal peptide nanoparticle. ACS Biomater Sci Eng. 2017;3(5):724–732. doi: 10.1021/acsbiomaterials.6b00243. [DOI] [PubMed] [Google Scholar]
- 50.Thakkar D, Gupta R, Mohan P, Monson K, Rapoport N. Overcoming biological barriers with ultrasound. AIP Conf Proc. 2012;1481:381–387. doi: 10.1063/1.4757365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Barua S, Mitragotri S. Challenges associated with penetration of nanoparticles across cell and tissue barriers: a review of current status and future prospects. Nano Today. 2014;9(2):223–243. doi: 10.1016/j.nantod.2014.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Zhou Y, Peng Z, Seven ES, Leblanc RM. Crossing the blood-brain barrier with nanoparticles. J Control Release. 2018;270:290–303. doi: 10.1016/j.jconrel.2017.12.015. [DOI] [PubMed] [Google Scholar]
- 53.Tharkar P, Varanasi R, Wong WSF, Jin CT, Chrzanowski W. Nano-enhanced drug delivery and therapeutic ultrasound for cancer treatment and beyond. Front Bioeng Biotechnol. 2019;7:324. doi: 10.3389/fbioe.2019.00324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lockman PR, Mumper RJ, Khan MA, Allen DD. Nanoparticle technology for drug delivery across the blood-brain barrier. Drug Dev Ind Pharm. 2002;28(1):1–13. doi: 10.1081/DDC-120001481. [DOI] [PubMed] [Google Scholar]
- 55.Sievers EL, Senter PD. Antibody-drug conjugates in cancer therapy. Annu Rev Med. 2013;64:15–29. doi: 10.1146/annurev-med-050311-201823. [DOI] [PubMed] [Google Scholar]
- 56.Nieto C, Vega MA, Martín Del Valle EM. Trastuzumab: more than a guide in HER2-positive cancer nanomedicine. Nanomaterials (Basel) 2020;10(9):1674. doi: 10.3390/nano10091674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Xu P, Wang R, Yang W, Liu Y, He D, Ye Z, Chen D, Ding Y, Tu J, Shen Y. A DM1-doped porous gold nanoshell system for NIR accelerated redox-responsive release and triple modal imaging guided photothermal synergistic chemotherapy. J Nanobiotechnol. 2021;19(1):77. doi: 10.1186/s12951-021-00824-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Fu Q, Wang J, Liu H. Chemo-immune synergetic therapy of esophageal carcinoma: trastuzumab modified, cisplatin and fluorouracil co-delivered lipid-polymer hybrid nanoparticles. Drug Deliv. 2020;27(1):1535–1543. doi: 10.1080/10717544.2020.1837294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Liang S, Sun M, Lu Y, Shi S, Yang Y, Lin Y, Feng C, Liu J, Dong C. Cytokine-induced killer cells-assisted tumor-targeting delivery of Her-2 monoclonal antibody-conjugated gold nanostars with NIR photosensitizer for enhanced therapy of cancer. J Mater Chem B. 2020;8(36):8368–8382. doi: 10.1039/D0TB01391A. [DOI] [PubMed] [Google Scholar]
- 60.György B, Szabó TG, Pásztói M, Pál Z, Misják P, Aradi B, László V, Pállinger E, Pap E, Kittel A, Nagy G, Falus A, Buzás EI. Membrane vesicles, current state-of-the-art: emerging role of extracellular vesicles. Cell Mol Life Sci. 2011;68(16):2667–2688. doi: 10.1007/s00018-011-0689-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Raposo G, Stoorvogel W. Extracellular vesicles: exosomes, microvesicles, and friends. J Cell Biol. 2013;200(4):373–383. doi: 10.1083/jcb.201211138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Colombo M, Raposo G, Théry C. Biogenesis, secretion, and intercellular interactions of exosomes and other extracellular vesicles. Annu Rev Cell Dev Biol. 2014;30:255–289. doi: 10.1146/annurev-cellbio-101512-122326. [DOI] [PubMed] [Google Scholar]
- 63.Batrakova EV, Kim MS. Using exosomes, naturally-equipped nanocarriers, for drug delivery. J Control Release. 2015;219:396–405. doi: 10.1016/j.jconrel.2015.07.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Zhang WW, Li L, Li D, Liu J, Li X, Li W, Xu X, Zhang MJ, Chandler LA, Lin H, Hu A, Xu W, Lam DM. The first approved gene therapy product for cancer Ad-p53 (gendicine): 12 years in the clinic. Hum Gene Ther. 2018;29(2):160–179. doi: 10.1089/hum.2017.218. [DOI] [PubMed] [Google Scholar]
- 65.Zhang H, Zhou X, Xu C, Yang J, Xiang J, Tao M, Xie Y. Synergistic tumor suppression by adenovirus-mediated ING4/PTEN double gene therapy for gastric cancer. Cancer Gene Ther. 2016;23(1):13–23. doi: 10.1038/cgt.2015.59. [DOI] [PubMed] [Google Scholar]
- 66.Phelps MP, Yang H, Patel S, Rahman MM, McFadden G, Chen E. Oncolytic virus-mediated RAS targeting in rhabdomyosarcoma. Mol Ther Oncolytics. 2018;11:52–61. doi: 10.1016/j.omto.2018.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Yoon AR, Jung BK, Choi E, Chung E, Hong J, Kim JS, Koo T, Yun CO. CRISPR-Cas12a with an oAd induces precise and cancer-specific genomic reprogramming of EGFR and efficient tumor regression. Mol Ther. 2020;28(10):2286–2296. doi: 10.1016/j.ymthe.2020.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Moss KH, Popova P, Hadrup SR, Astakhova K, Taskova M. Lipid nanoparticles for delivery of therapeutic RNA oligonucleotides. Mol Pharm. 2019;16(6):2265–2277. doi: 10.1021/acs.molpharmaceut.8b01290. [DOI] [PubMed] [Google Scholar]
- 69.Briolay T, Petithomme T, Fouet M, Nguyen-Pham N, Blanquart C, Boisgerault N. Delivery of cancer therapies by synthetic and bio-inspired nanovectors. Mol Cancer. 2021;20(1):55. doi: 10.1186/s12943-021-01346-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Alvarez-Erviti L, Seow Y, Yin H, Betts C, Lakhal S, Wood MJ. Delivery of siRNA to the mouse brain by systemic injection of targeted exosomes. Nat Biotechnol. 2011;29(4):341–345. doi: 10.1038/nbt.1807. [DOI] [PubMed] [Google Scholar]
- 71.Kim MS, Haney MJ, Zhao Y, Yuan D, Deygen I, Klyachko NL, Kabanov AV, Batrakova EV. Engineering macrophage-derived exosomes for targeted paclitaxel delivery to pulmonary metastases: in vitro and in vivo evaluations. Nanomedicine. 2018;14(1):195–204. doi: 10.1016/j.nano.2017.09.011. [DOI] [PubMed] [Google Scholar]
- 72.Jeong K, Yu YJ, You JY, Rhee WJ, Kim JA. Exosome-mediated microRNA-497 delivery for anti-cancer therapy in a microfluidic 3D lung cancer model. Lab Chip. 2020;20(3):548–557. doi: 10.1039/C9LC00958B. [DOI] [PubMed] [Google Scholar]
- 73.Wei W, Ao Q, Wang X, Cao Y, Liu Y, Zheng SG, Tian X. Mesenchymal stem cell-derived exosomes: a promising biological tool in nanomedicine. Front Pharmacol. 2020;11:590470. doi: 10.3389/fphar.2020.590470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Pegtel DM, Gould SJ. Exosomes. Annu Rev Biochem. 2019;88:487–514. doi: 10.1146/annurev-biochem-013118-111902. [DOI] [PubMed] [Google Scholar]
- 75.Jeyaram A, Jay SM. Preservation and storage stability of extracellular vesicles for therapeutic applications. Aaps J. 2017;20(1):1. doi: 10.1208/s12248-017-0160-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Wei H, Chen J, Wang S, Fu F, Zhu X, Wu C, Liu Z, Zhong G, Lin J. A nanodrug consisting of doxorubicin and exosome derived from mesenchymal stem cells for osteosarcoma treatment in vitro. Int J Nanomed. 2019;14:8603–8610. doi: 10.2147/IJN.S218988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Mizrak A, Bolukbasi MF, Ozdener GB, Brenner GJ, Madlener S, Erkan EP, Ströbel T, Breakefield XO, Saydam O. Genetically engineered microvesicles carrying suicide mRNA/protein inhibit schwannoma tumor growth. Mol Ther. 2013;21(1):101–108. doi: 10.1038/mt.2012.161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Zhang K, Dong C, Chen M, Yang T, Wang X, Gao Y, Wang L, Wen Y, Chen G, Wang X, Yu X, Zhang Y, Wang P, Shang M, Han K, Zhou Y. Extracellular vesicle-mediated delivery of miR-101 inhibits lung metastasis in osteosarcoma. Theranostics. 2020;10(1):411–425. doi: 10.7150/thno.33482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Lin Y, Wu J, Gu W, Huang Y, Tong Z, Huang L, Tan J. Exosome-liposome hybrid nanoparticles deliver CRISPR/Cas9 system in MSCs. Adv Sci (Weinh) 2018;5(4):1700611. doi: 10.1002/advs.201700611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Shi X, Sun J, Li H, Lin H, Xie W, Li J, Tan W. Antitumor efficacy of interferon-γ-modified exosomal vaccine in prostate cancer. Prostate. 2020;80(11):811–823. doi: 10.1002/pros.23996. [DOI] [PubMed] [Google Scholar]
- 81.Allen TM, Cullis PR. Liposomal drug delivery systems: from concept to clinical applications. Adv Drug Deliv Rev. 2013;65(1):36–48. doi: 10.1016/j.addr.2012.09.037. [DOI] [PubMed] [Google Scholar]
- 82.Samad A, Sultana Y, Aqil M. Liposomal drug delivery systems: an update review. Curr Drug Deliv. 2007;4(4):297–305. doi: 10.2174/156720107782151269. [DOI] [PubMed] [Google Scholar]
- 83.Torchilin VP. Recent advances with liposomes as pharmaceutical carriers. Nat Rev Drug Discov. 2005;4(2):145–160. doi: 10.1038/nrd1632. [DOI] [PubMed] [Google Scholar]
- 84.Zhang L, Gu FX, Chan JM, Wang AZ, Langer RS, Farokhzad OC. Nanoparticles in medicine: therapeutic applications and developments. Clin Pharmacol Ther. 2008;83(5):761–769. doi: 10.1038/sj.clpt.6100400. [DOI] [PubMed] [Google Scholar]
- 85.Portney NG, Ozkan M. Nano-oncology: drug delivery, imaging, and sensing. Anal Bioanal Chem. 2006;384(3):620–630. doi: 10.1007/s00216-005-0247-7. [DOI] [PubMed] [Google Scholar]
- 86.Akbarzadeh A, Rezaei-Sadabady R, Davaran S, Joo SW, Zarghami N, Hanifehpour Y, Samiei M, Kouhi M, Nejati-Koshki K. Liposome: classification, preparation, and applications. Nanoscale Res Lett. 2013;8(1):102. doi: 10.1186/1556-276X-8-102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Cattel L, Ceruti M, Dosio F. From conventional to stealth liposomes: a new frontier in cancer chemotherapy. Tumori. 2003;89(3):237–249. doi: 10.1177/030089160308900302. [DOI] [PubMed] [Google Scholar]
- 88.James ND, Coker RJ, Tomlinson D, Harris JR, Gompels M, Pinching AJ, Stewart JS. Liposomal doxorubicin (Doxil): an effective new treatment for Kaposi's sarcoma in AIDS. Clin Oncol (R Coll Radiol) 1994;6(5):294–296. doi: 10.1016/S0936-6555(05)80269-9. [DOI] [PubMed] [Google Scholar]
- 89.Laginha KM, Verwoert S, Charrois GJ, Allen TM. Determination of doxorubicin levels in whole tumor and tumor nuclei in murine breast cancer tumors. Clin Cancer Res. 2005;11(19 Pt 1):6944–6949. doi: 10.1158/1078-0432.CCR-05-0343. [DOI] [PubMed] [Google Scholar]
- 90.Sriraman SK, Geraldo V, Luther E, Degterev A, Torchilin V. Cytotoxicity of PEGylated liposomes co-loaded with novel pro-apoptotic drug NCL-240 and the MEK inhibitor cobimetinib against colon carcinoma in vitro. J Control Release. 2015;220(Pt A):160–168. doi: 10.1016/j.jconrel.2015.10.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Batist G, Gelmon KA, Chi KN, Miller WH, Jr, Chia SK, Mayer LD, Swenson CE, Janoff AS, Louie AC. Safety, pharmacokinetics, and efficacy of CPX-1 liposome injection in patients with advanced solid tumors. Clin Cancer Res. 2009;15(2):692–700. doi: 10.1158/1078-0432.CCR-08-0515. [DOI] [PubMed] [Google Scholar]
- 92.Deng ZJ, Morton SW, Ben-Akiva E, Dreaden EC, Shopsowitz KE, Hammond PT. Layer-by-layer nanoparticles for systemic codelivery of an anticancer drug and siRNA for potential triple-negative breast cancer treatment. ACS Nano. 2013;7(11):9571–9584. doi: 10.1021/nn4047925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Zhang H, Li RY, Lu X, Mou ZZ, Lin GM. Docetaxel-loaded liposomes: preparation, pH sensitivity, pharmacokinetics, and tissue distribution. J Zhejiang Univ Sci B. 2012;13(12):981–989. doi: 10.1631/jzus.B1200098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Yao Y, Su Z, Liang Y, Zhang N. pH-Sensitive carboxymethyl chitosan-modified cationic liposomes for sorafenib and siRNA co-delivery. Int J Nanomed. 2015;10:6185–6197. doi: 10.2147/IJN.S90524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Lee Y, Thompson DH. Stimuli-responsive liposomes for drug delivery. Wiley Interdiscip Rev Nanomed Nanobiotechnol. 2017;9(5):e1450. doi: 10.1002/wnan.1450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Hui L, Chen Y. Tumor microenvironment: sanctuary of the devil. Cancer Lett. 2015;368(1):7–13. doi: 10.1016/j.canlet.2015.07.039. [DOI] [PubMed] [Google Scholar]
- 97.Sun Y. Translational horizons in the tumor microenvironment: harnessing breakthroughs and targeting cures. Med Res Rev. 2015;35(2):408–436. doi: 10.1002/med.21338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Wang M, Zhao J, Zhang L, Wei F, Lian Y, Wu Y, Gong Z, Zhang S, Zhou J, Cao K, Li X, Xiong W, Li G, Zeng Z, Guo C. Role of tumor microenvironment in tumorigenesis. J Cancer. 2017;8(5):761–773. doi: 10.7150/jca.17648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Naseri N, Valizadeh H, Zakeri-Milani P. Solid lipid nanoparticles and nanostructured lipid carriers: structure, preparation and application. Adv Pharm Bull. 2015;5(3):305–313. doi: 10.15171/apb.2015.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Kraft JC, Freeling JP, Wang Z, Ho RJ. Emerging research and clinical development trends of liposome and lipid nanoparticle drug delivery systems. J Pharm Sci. 2014;103(1):29–52. doi: 10.1002/jps.23773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Das S, Chaudhury A. Recent advances in lipid nanoparticle formulations with solid matrix for oral drug delivery. AAPS PharmSciTech. 2011;12(1):62–76. doi: 10.1208/s12249-010-9563-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Iqbal MA, Md S, Sahni JK, Baboota S, Dang S, Ali J. Nanostructured lipid carriers system: recent advances in drug delivery. J Drug Target. 2012;20(10):813–830. doi: 10.3109/1061186X.2012.716845. [DOI] [PubMed] [Google Scholar]
- 103.Jaiswal M, Dudhe R, Sharma PK. Nanoemulsion: an advanced mode of drug delivery system. 3 Biotech. 2015;5(2):123–127. doi: 10.1007/s13205-014-0214-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Gorain B, Choudhury H, Nair AB, Dubey SK, Kesharwani P. Theranostic application of nanoemulsions in chemotherapy. Drug Discov Today. 2020;25(7):1174–1188. doi: 10.1016/j.drudis.2020.04.013. [DOI] [PubMed] [Google Scholar]
- 105.Du M, Yang Z, Lu W, Wang B, Wang Q, Chen Z, Chen L, Han S, Cai T, Cai Y. Design and development of spirulina polysaccharide-loaded nanoemulsions with improved the antitumor effects of paclitaxel. J Microencapsul. 2020;37(6):403–412. doi: 10.1080/02652048.2020.1767224. [DOI] [PubMed] [Google Scholar]
- 106.Dianzani C, Monge C, Miglio G, Serpe L, Martina K, Cangemi L, Ferraris C, Mioletti S, Osella S, Gigliotti CL, Boggio E, Clemente N, Dianzani U, Battaglia L. Nanoemulsions as delivery systems for poly-chemotherapy aiming at melanoma treatment. Cancers (Basel) 2020;12(5):1198. doi: 10.3390/cancers12051198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Ribeiro EB, de Marchi PGF, Honorio-França AC, França EL, Soler MAG. Interferon-gamma carrying nanoemulsion with immunomodulatory and anti-tumor activities. J Biomed Mater Res A. 2020;108(2):234–245. doi: 10.1002/jbm.a.36808. [DOI] [PubMed] [Google Scholar]
- 108.Meng L, Xia X, Yang Y, Ye J, Dong W, Ma P, Jin Y, Liu Y. Co-encapsulation of paclitaxel and baicalein in nanoemulsions to overcome multidrug resistance via oxidative stress augmentation and P-glycoprotein inhibition. Int J Pharm. 2016;513(1–2):8–16. doi: 10.1016/j.ijpharm.2016.09.001. [DOI] [PubMed] [Google Scholar]
- 109.Sanchez-Lopez E, Guerra M, Dias-Ferreira J, Lopez-Machado A, Ettcheto M, Cano A, Espina M, Camins A, Garcia ML, Souto EB. Current applications of nanoemulsions in cancer therapeutics. Nanomaterials (Basel) 2019;9(6):821. doi: 10.3390/nano9060821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Baker JR., Jr Dendrimer-based nanoparticles for cancer therapy. Hematol Am Soc Hematol Educ Program. 2009;209:708–719. doi: 10.1182/asheducation-2009.1.708. [DOI] [PubMed] [Google Scholar]
- 111.Lim J, Kostiainen M, Maly J, da Costa VC, Annunziata O, Pavan GM, Simanek EE. Synthesis of large dendrimers with the dimensions of small viruses. J Am Chem Soc. 2013;135(12):4660–4663. doi: 10.1021/ja400432e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Lo ST, Kumar A, Hsieh JT, Sun X. Dendrimer nanoscaffolds for potential theranostics of prostate cancer with a focus on radiochemistry. Mol Pharm. 2013;10(3):793–812. doi: 10.1021/mp3005325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Li D, Fan Y, Shen M, Bányai I, Shi X. Design of dual drug-loaded dendrimer/carbon dot nanohybrids for fluorescence imaging and enhanced chemotherapy of cancer cells. J Mater Chem B. 2019;7(2):277–285. doi: 10.1039/C8TB02723D. [DOI] [PubMed] [Google Scholar]
- 114.Pishavar E, Ramezani M, Hashemi M. Co-delivery of doxorubicin and TRAIL plasmid by modified PAMAM dendrimer in colon cancer cells, in vitro and in vivo evaluation. Drug Dev Ind Pharm. 2019;45(12):1931–1939. doi: 10.1080/03639045.2019.1680995. [DOI] [PubMed] [Google Scholar]
- 115.Tarach P, Janaszewska A. Recent advances in preclinical research using PAMAM dendrimers for cancer gene therapy. Int J Mol Sci. 2021;22(6):2912. doi: 10.3390/ijms22062912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Jędrzak A, Grześkowiak BF, Coy E, Wojnarowicz J, Szutkowski K, Jurga S, Jesionowski T, Mrówczyński R. Dendrimer based theranostic nanostructures for combined chemo- and photothermal therapy of liver cancer cells in vitro. Colloids Surf B. 2019;173:698–708. doi: 10.1016/j.colsurfb.2018.10.045. [DOI] [PubMed] [Google Scholar]
- 117.Saleem J, Wang L, Chen C. Carbon-based nanomaterials for cancer therapy via targeting tumor microenvironment. Adv Healthc Mater. 2018;7(20):e1800525. doi: 10.1002/adhm.201800525. [DOI] [PubMed] [Google Scholar]
- 118.Fadeel B, Bussy C, Merino S, Vázquez E, Flahaut E, Mouchet F, Evariste L, Gauthier L, Koivisto AJ, Vogel U, Martín C, Delogu LG, Buerki-Thurnherr T, Wick P, Beloin-Saint-Pierre D, Hischier R, Pelin M, Candotto Carniel F, Tretiach M, Cesca F, Benfenati F, Scaini D, Ballerini L, Kostarelos K, Prato M, Bianco A. Safety assessment of graphene-based materials: focus on human health and the environment. ACS Nano. 2018;12(11):10582–10620. doi: 10.1021/acsnano.8b04758. [DOI] [PubMed] [Google Scholar]
- 119.Ou L, Song B, Liang H, Liu J, Feng X, Deng B, Sun T, Shao L. Toxicity of graphene-family nanoparticles: a general review of the origins and mechanisms. Part Fibre Toxicol. 2016;13(1):57. doi: 10.1186/s12989-016-0168-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Krishna KV, Ménard-Moyon C, Verma S, Bianco A. Graphene-based nanomaterials for nanobiotechnology and biomedical applications. Nanomedicine (Lond) 2013;8(10):1669–1688. doi: 10.2217/nnm.13.140. [DOI] [PubMed] [Google Scholar]
- 121.Novoselov KS, Geim AK, Morozov SV, Jiang D, Zhang Y, Dubonos SV, Grigorieva IV, Firsov AA. Electric field effect in atomically thin carbon films. Science. 2004;306(5696):666–669. doi: 10.1126/science.1102896. [DOI] [PubMed] [Google Scholar]
- 122.Liu J, Dong J, Zhang T, Peng Q. Graphene-based nanomaterials and their potentials in advanced drug delivery and cancer therapy. J Control Release. 2018;286:64–73. doi: 10.1016/j.jconrel.2018.07.034. [DOI] [PubMed] [Google Scholar]
- 123.Geim AK, Novoselov KS. The rise of graphene. Nat Mater. 2007;6(3):183–191. doi: 10.1038/nmat1849. [DOI] [PubMed] [Google Scholar]
- 124.Verde V, Longo A, Cucci LM, Sanfilippo V, Magri A, Satriano C, Anfuso CD, Lupo G, La Mendola D. Anti-angiogenic and anti-proliferative graphene oxide nanosheets for tumor cell therapy. Int J Mol Sci. 2020;21(15):5571. doi: 10.3390/ijms21155571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Gao W. The chemistry of graphene oxide. In: Gao W, editor. Graphene oxide. Springer; 2015. p. 61–95
- 126.Balandin AA, Ghosh S, Bao W, Calizo I, Teweldebrhan D, Miao F, Lau CN. Superior thermal conductivity of single-layer graphene. Nano Lett. 2008;8(3):902–907. doi: 10.1021/nl0731872. [DOI] [PubMed] [Google Scholar]
- 127.Kuilla T, Bhadra S, Yao D, Kim NH, Bose S, Lee JH. Recent advances in graphene based polymer composites. Prog Polym Sci. 2010;35(11):1350–1375. doi: 10.1016/j.progpolymsci.2010.07.005. [DOI] [Google Scholar]
- 128.Ema M, Gamo M, Honda K. A review of toxicity studies on graphene-based nanomaterials in laboratory animals. Regul Toxicol Pharmacol. 2017;85:7–24. doi: 10.1016/j.yrtph.2017.01.011. [DOI] [PubMed] [Google Scholar]
- 129.Geim AK. Graphene: status and prospects. Science. 2009;324(5934):1530–1534. doi: 10.1126/science.1158877. [DOI] [PubMed] [Google Scholar]
- 130.Goenka S, Sant V, Sant S. Graphene-based nanomaterials for drug delivery and tissue engineering. J Control Release. 2014;173:75–88. doi: 10.1016/j.jconrel.2013.10.017. [DOI] [PubMed] [Google Scholar]
- 131.Muñoz R, Singh DP, Kumar R, Matsuda A. Graphene oxide for drug delivery and cancer therapy. In: SK Swain, M Jawaid, editors. Nanostructured polymer composites for biomedical applications. Elsevier; 2019. p. 447–488.
- 132.Ma J, Liu R, Wang X, Liu Q, Chen Y, Valle RP, Zuo YY, Xia T, Liu S. Crucial role of lateral size for graphene oxide in activating macrophages and stimulating pro-inflammatory responses in cells and animals. ACS Nano. 2015;9(10):10498–10515. doi: 10.1021/acsnano.5b04751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Feito MJ, Vila M, Matesanz MC, Linares J, Gonçalves G, Marques PA, Vallet-Regí M, Rojo JM, Portolés MT. In vitro evaluation of graphene oxide nanosheets on immune function. J Colloid Interface Sci. 2014;432:221–228. doi: 10.1016/j.jcis.2014.07.004. [DOI] [PubMed] [Google Scholar]
- 134.Burnett M, Abuetabh Y, Wronski A, Shen F, Persad S, Leng R, Eisenstat D, Sergi C. Graphene oxide nanoparticles induce apoptosis in wild-type and CRISPR/Cas9-IGF/IGFBP3 knocked-out osteosarcoma cells. J Cancer. 2020;11(17):5007–5023. doi: 10.7150/jca.46464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Najafi M, Mortezaee K, Majidpoor J. Cancer stem cell (CSC) resistance drivers. Life Sci. 2019;234:116781. doi: 10.1016/j.lfs.2019.116781. [DOI] [PubMed] [Google Scholar]
- 136.Fiorillo M, Verre AF, Iliut M, Peiris-Pagés M, Ozsvari B, Gandara R, Cappello AR, Sotgia F, Vijayaraghavan A, Lisanti MP. Graphene oxide selectively targets cancer stem cells, across multiple tumor types: implications for non-toxic cancer treatment, via "differentiation-based nano-therapy". Oncotarget. 2015;6(6):3553–3562. doi: 10.18632/oncotarget.3348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Quagliarini E, Di Santo R, Pozzi D, Tentori P, Cardarelli F, Caracciolo G. Mechanistic insights into the release of doxorubicin from graphene oxide in cancer cells. Nanomaterials (Basel) 2020;10(8):1482. doi: 10.3390/nano10081482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Tao Y, Zhu L, Zhao Y, Yi X, Zhu L, Ge F, Mou X, Chen L, Sun L, Yang K. Nano-graphene oxide-manganese dioxide nanocomposites for overcoming tumor hypoxia and enhancing cancer radioisotope therapy. Nanoscale. 2018;10(11):5114–5123. doi: 10.1039/C7NR08747K. [DOI] [PubMed] [Google Scholar]
- 139.Zhang X, Tian W, Cai X, Wang X, Dang W, Tang H, Cao H, Wang L, Chen T. Hydrazinocurcumin Encapsuled nanoparticles "re-educate" tumor-associated macrophages and exhibit anti-tumor effects on breast cancer following STAT3 suppression. PLoS ONE. 2013;8(6):e65896. doi: 10.1371/journal.pone.0065896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Shi S, Yang K, Hong H, Valdovinos HF, Nayak TR, Zhang Y, Theuer CP, Barnhart TE, Liu Z, Cai W. Tumor vasculature targeting and imaging in living mice with reduced graphene oxide. Biomaterials. 2013;34(12):3002–3009. doi: 10.1016/j.biomaterials.2013.01.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Sahu A, Min K, Jeon J, Yang HS, Tae G. Catalytic nanographene oxide with hemin for enhanced photodynamic therapy. J Control Release. 2020;326:442–454. doi: 10.1016/j.jconrel.2020.07.023. [DOI] [PubMed] [Google Scholar]
- 142.Wu C, Zhu A, Li D, Wang L, Yang H, Zeng H, Liu Y. Photosensitizer-assembled PEGylated graphene-copper sulfide nanohybrids as a synergistic near-infrared phototherapeutic agent. Expert Opin Drug Deliv. 2016;13(1):155–165. doi: 10.1517/17425247.2016.1118049. [DOI] [PubMed] [Google Scholar]
- 143.Ivanovskii A. Graphynes and graphdyines. Prog Solid State Chem. 2013;41(1–2):1–19. doi: 10.1016/j.progsolidstchem.2012.12.001. [DOI] [Google Scholar]
- 144.Min H, Qi Y, Zhang Y, Han X, Cheng K, Liu Y, Liu H, Hu J, Nie G, Li Y. A graphdiyne oxide-based iron sponge with photothermally enhanced tumor-specific fenton chemistry. Adv Mater. 2020;32(31):e2000038. doi: 10.1002/adma.202000038. [DOI] [PubMed] [Google Scholar]
- 145.Fusco L, Gazzi A, Peng G, Shin Y, Vranic S, Bedognetti D, Vitale F, Yilmazer A, Feng X, Fadeel B, Casiraghi C, Delogu LG. Graphene and other 2D materials: a multidisciplinary analysis to uncover the hidden potential as cancer theranostics. Theranostics. 2020;10(12):5435–5488. doi: 10.7150/thno.40068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Li Y, Li X, Meng Y, Hun X. Photoelectrochemical platform for MicroRNA let-7a detection based on graphdiyne loaded with AuNPs modified electrode coupled with alkaline phosphatase. Biosens Bioelectron. 2019;130:269–275. doi: 10.1016/j.bios.2019.02.002. [DOI] [PubMed] [Google Scholar]
- 147.Wang J, Chen C, Li B, Yu H, Zhao Y, Sun J, Li Y, Xing G, Yuan H, Tang J, Chen Z, Meng H, Gao Y, Ye C, Chai Z, Zhu C, Ma B, Fang X, Wan L. Antioxidative function and biodistribution of [Gd@C82(OH)22]n nanoparticles in tumor-bearing mice. Biochem Pharmacol. 2006;71(6):872–881. doi: 10.1016/j.bcp.2005.12.001. [DOI] [PubMed] [Google Scholar]
- 148.Yin JJ, Lao F, Fu PP, Wamer WG, Zhao Y, Wang PC, Qiu Y, Sun B, Xing G, Dong J, Liang XJ, Chen C. The scavenging of reactive oxygen species and the potential for cell protection by functionalized fullerene materials. Biomaterials. 2009;30(4):611–621. doi: 10.1016/j.biomaterials.2008.09.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Chen A, Grobmyer SR, Krishna VB. Photothermal response of polyhydroxy fullerenes. ACS Omega. 2020;5(24):14444–14450. doi: 10.1021/acsomega.0c01018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Grebinyk A, Prylutska S, Chepurna O, Grebinyk S, Prylutskyy Y, Ritter U, Ohulchanskyy TY, Matyshevska O, Dandekar T, Frohme M. Synergy of chemo- and photodynamic therapies with C(60) fullerene-doxorubicin nanocomplex. Nanomaterials (Basel) 2019;9(11):1540. doi: 10.3390/nano9111540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Franskevych D, Prylutska S, Grynyuk I, Pasichnyk G, Drobot L, Matyshevska O, Ritter U. Mode of photoexcited C(60) fullerene involvement in potentiating cisplatin toxicity against drug-resistant L1210 cells. Bioimpacts. 2019;9(4):211–217. doi: 10.15171/bi.2019.26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Meng J, Yang M, Jia F, Kong H, Zhang W, Wang C, Xing J, Xie S, Xu H. Subcutaneous injection of water-soluble multi-walled carbon nanotubes in tumor-bearing mice boosts the host immune activity. Nanotechnology. 2010;21(14):145104. doi: 10.1088/0957-4484/21/14/145104. [DOI] [PubMed] [Google Scholar]
- 153.Meng J, Meng J, Duan J, Kong H, Li L, Wang C, Xie S, Chen S, Gu N, Xu H, Yang XD. Carbon nanotubes conjugated to tumor lysate protein enhance the efficacy of an antitumor immunotherapy. Small. 2008;4(9):1364–1370. doi: 10.1002/smll.200701059. [DOI] [PubMed] [Google Scholar]
- 154.Sundaram P, Abrahamse H. Effective photodynamic therapy for colon cancer cells using chlorin e6 coated hyaluronic acid-based carbon nanotubes. Int J Mol Sci. 2020;21(13):4745. doi: 10.3390/ijms21134745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Neelgund GM, Okolie MC, Williams FK, Oki A. Ag(2)S nanocrystallites deposited over polyamidoamine grafted carbon nanotubes: an efficient NIR active photothermal agent. Mater Chem Phys. 2019;234:32–37. doi: 10.1016/j.matchemphys.2019.05.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Omurtag Ozgen PS, Atasoy S, Zengin Kurt B, Durmus Z, Yigit G, Dag A. Glycopolymer decorated multiwalled carbon nanotubes for dual targeted breast cancer therapy. J Mater Chem B. 2020;8(15):3123–3137. doi: 10.1039/C9TB02711D. [DOI] [PubMed] [Google Scholar]
- 157.Yaghoubi A, Ramazani A. Anticancer DOX delivery system based on CNTs: functionalization, targeting and novel technologies. J Control Release. 2020;327:198–224. doi: 10.1016/j.jconrel.2020.08.001. [DOI] [PubMed] [Google Scholar]
- 158.Al Garalleh H, Algarni A. Modelling of paclitaxel conjugated with carbon nanotubes as an antitumor agent for cancer therapy. J Biomed Nanotechnol. 2020;16(2):224–234. doi: 10.1166/jbn.2020.2886. [DOI] [PubMed] [Google Scholar]
- 159.He Z, Jiang R, Long W, Huang H, Liu M, Chen J, Deng F, Zhou N, Zhang X, Wei Y. The combination of Diels–Alder reaction and redox polymerization for preparation of functionalized CNTs for intracellular controlled drug delivery. Mater Sci Eng C Mater Biol Appl. 2020;109:110442. doi: 10.1016/j.msec.2019.110442. [DOI] [PubMed] [Google Scholar]
- 160.Karousis N, Suarez-Martinez I, Ewels CP, Tagmatarchis N. Structure, properties, functionalization, and applications of carbon nanohorns. Chem Rev. 2016;116(8):4850–4883. doi: 10.1021/acs.chemrev.5b00611. [DOI] [PubMed] [Google Scholar]
- 161.Chronopoulos D, Karousis N, Ichihashi T, Yudasaka M, Iijima S, Tagmatarchis N. Benzyne cycloaddition onto carbon nanohorns. Nanoscale. 2013;5(14):6388–6394. doi: 10.1039/c3nr01755a. [DOI] [PubMed] [Google Scholar]
- 162.Jiang B-P, Hu L-F, Shen X-C, Ji S-C, Shi Z, Liu C-J, Zhang L, Liang H. One-step preparation of a water-soluble carbon nanohorn/phthalocyanine hybrid for dual-modality photothermal and photodynamic therapy. ACS Appl Mater Interfaces. 2014;6(20):18008–18017. doi: 10.1021/am504860c. [DOI] [PubMed] [Google Scholar]
- 163.Pagona G, Sandanayaka AS, Araki Y, Fan J, Tagmatarchis N, Yudasaka M, Iijima S, Ito O. Electronic interplay on illuminated aqueous carbon nanohorn− porphyrin ensembles. J Phys Chem B. 2006;110(42):20729–20732. doi: 10.1021/jp064685m. [DOI] [PubMed] [Google Scholar]
- 164.Yang J, Su H, Sun W, Cai J, Liu S, Chai Y, Zhang C. Dual chemodrug-loaded single-walled carbon nanohorns for multimodal imaging-guided chemo-photothermal therapy of tumors and lung metastases. Theranostics. 2018;8(7):1966–1984. doi: 10.7150/thno.23848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Lucío MI, Opri R, Pinto M, Scarsi A, Fierro JLG, Meneghetti M, Fracasso G, Prato M, Vázquez E, Herrero MA. Targeted killing of prostate cancer cells using antibody-drug conjugated carbon nanohorns. J Mater Chem B. 2017;5(44):8821–8832. doi: 10.1039/C7TB02464A. [DOI] [PubMed] [Google Scholar]
- 166.Liu Y, Zhong H, Qin Y, Zhang Y, Zhang T. Non-covalent hydrophilization of reduced graphene oxide used as a paclitaxel vehicle. RSC Adv. 2016;6(36):30184–30193. doi: 10.1039/C6RA04349F. [DOI] [Google Scholar]
- 167.Park YH, Park SY, In I. Direct noncovalent conjugation of folic acid on reduced graphene oxide as anticancer drug carrier. J Ind Eng Chem. 2015;30:190–196. doi: 10.1016/j.jiec.2015.05.021. [DOI] [Google Scholar]
- 168.Jafarizad A, Aghanejad A, Sevim M, Metin N, Barar J, Omidi Y, Ekinci D. Gold nanoparticles and reduced graphene oxide-gold nanoparticle composite materials as covalent drug delivery systems for breast cancer treatment. ChemistrySelect. 2017;2(23):6663–6672. doi: 10.1002/slct.201701178. [DOI] [Google Scholar]
- 169.Masoudipour E, Kashanian S, Maleki N. A targeted drug delivery system based on dopamine functionalized nano graphene oxide. Chem Phys Lett. 2017;668:56–63. doi: 10.1016/j.cplett.2016.12.019. [DOI] [Google Scholar]
- 170.Rao Z, Ge H, Liu L, Zhu C, Min L, Liu M, Fan L, Li D. Carboxymethyl cellulose modified graphene oxide as pH-sensitive drug delivery system. Int J Biol Macromol. 2018;107(Pt A):1184–1192. doi: 10.1016/j.ijbiomac.2017.09.096. [DOI] [PubMed] [Google Scholar]
- 171.Nie X, Tang J, Liu Y, Cai R, Miao Q, Zhao Y, Chen C. Fullerenol inhibits the cross-talk between bone marrow-derived mesenchymal stem cells and tumor cells by regulating MAPK signaling. Nanomed Nanotechnol Biol Med. 2017;13:1879–1890. doi: 10.1016/j.nano.2017.03.013. [DOI] [PubMed] [Google Scholar]
- 172.Meng H, Xing G, Sun B, Zhao F, Lei H, Li W, Song Y, Chen Z, Yuan H, Wang X, Long J, Chen C, Liang X, Zhang N, Chai Z, Zhao Y. Potent angiogenesis inhibition by the particulate form of fullerene derivatives. ACS Nano. 2010;4(5):2773–2783. doi: 10.1021/nn100448z. [DOI] [PubMed] [Google Scholar]
- 173.Gu YJ, Cheng J, Jin J, Cheng SH, Wong WT. Development and evaluation of pH-responsive single-walled carbon nanotube-doxorubicin complexes in cancer cells. Int J Nanomed. 2011;6:2889–2898. doi: 10.2147/IJN.S25162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Dong X, Sun Z, Wang X, Leng X. An innovative MWCNTs/DOX/TC nanosystem for chemo-photothermal combination therapy of cancer. Nanomedicine. 2017;13(7):2271–2280. doi: 10.1016/j.nano.2017.07.002. [DOI] [PubMed] [Google Scholar]
- 175.Zhou L, Li Z, Liu Z, Ren J, Qu X. Luminescent carbon dot-gated nanovehicles for pH-triggered intracellular controlled release and imaging. Langmuir. 2013;29(21):6396–6403. doi: 10.1021/la400479n. [DOI] [PubMed] [Google Scholar]
- 176.Chong Y, Ge C, Yang Z, Garate JA, Gu Z, Weber JK, Liu J, Zhou R. Reduced cytotoxicity of graphene nanosheets mediated by blood-protein coating. ACS Nano. 2015;9(6):5713–5724. doi: 10.1021/nn5066606. [DOI] [PubMed] [Google Scholar]
- 177.Kenry LKP, Lim CT. Molecular interactions of graphene oxide with human blood plasma proteins. Nanoscale. 2016;8(17):9425–9441. doi: 10.1039/C6NR01697A. [DOI] [PubMed] [Google Scholar]
- 178.Liao KH, Lin YS, Macosko CW, Haynes CL. Cytotoxicity of graphene oxide and graphene in human erythrocytes and skin fibroblasts. ACS Appl Mater Interfaces. 2011;3(7):2607–2615. doi: 10.1021/am200428v. [DOI] [PubMed] [Google Scholar]
- 179.Sasidharan A, Panchakarla LS, Chandran P, Menon D, Nair S, Rao CN, Koyakutty M. Differential nano-bio interactions and toxicity effects of pristine versus functionalized graphene. Nanoscale. 2011;3(6):2461–2464. doi: 10.1039/c1nr10172b. [DOI] [PubMed] [Google Scholar]
- 180.van Zandwijk N, Frank AL. Awareness: potential toxicities of carbon nanotubes. Transl Lung Cancer Res. 2019;8(Suppl 4):S471–S472. doi: 10.21037/tlcr.2019.12.05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Yan H, Xue Z, Xie J, Dong Y, Ma Z, Sun X, Kebebe Borga D, Liu Z, Li J. Toxicity of carbon nanotubes as anti-tumor drug carriers. Int J Nanomed. 2019;14:10179–10194. doi: 10.2147/IJN.S220087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Yuan X, Zhang X, Sun L, Wei Y, Wei X. Cellular toxicity and immunological effects of carbon-based nanomaterials. Part Fibre Toxicol. 2019;16(1):18. doi: 10.1186/s12989-019-0299-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Dubertret B, Skourides P, Norris DJ, Noireaux V, Brivanlou AH, Libchaber A. In vivo imaging of quantum dots encapsulated in phospholipid micelles. Science. 2002;298(5599):1759–1762. doi: 10.1126/science.1077194. [DOI] [PubMed] [Google Scholar]
- 184.Gao X, Cui Y, Levenson RM, Chung LW, Nie S. In vivo cancer targeting and imaging with semiconductor quantum dots. Nat Biotechnol. 2004;22(8):969–976. doi: 10.1038/nbt994. [DOI] [PubMed] [Google Scholar]
- 185.Pooresmaeil M, Namazi H, Salehi R. Synthesis of photoluminescent glycodendrimer with terminal beta-cyclodextrin molecules as a biocompatible pH-sensitive carrier for doxorubicin delivery. Carbohydr Polym. 2020;246:116658. doi: 10.1016/j.carbpol.2020.116658. [DOI] [PubMed] [Google Scholar]
- 186.Liu H, Li C, Qian Y, Hu L, Fang J, Tong W, Nie R, Chen Q, Wang H. Magnetic-induced graphene quantum dots for imaging-guided photothermal therapy in the second near-infrared window. Biomaterials. 2020;232:119700. doi: 10.1016/j.biomaterials.2019.119700. [DOI] [PubMed] [Google Scholar]
- 187.Li X, Vinothini K, Ramesh T, Rajan M, Ramu A. Combined photodynamic-chemotherapy investigation of cancer cells using carbon quantum dot-based drug carrier system. Drug Deliv. 2020;27(1):791–804. doi: 10.1080/10717544.2020.1765431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Wang S, Chen L, Wang J, Du J, Li Q, Gao Y, Yu S, Yang Y. Enhanced-fluorescent imaging and targeted therapy of liver cancer using highly luminescent carbon dots-conjugated foliate. Mater Sci Eng C Mater Biol Appl. 2020;116:111233. doi: 10.1016/j.msec.2020.111233. [DOI] [PubMed] [Google Scholar]
- 189.Chen W, Li J, Xing Y, Wang X, Zhang H, Xia M, Wang D. Dual-pH sensitive charge-reversal drug delivery system for highly precise and penetrative chemotherapy. Pharm Res. 2020;37(7):134. doi: 10.1007/s11095-020-02852-6. [DOI] [PubMed] [Google Scholar]
- 190.Li H, Ma M, Zhang J, Hou W, Chen H, Zeng D, Wang Z. Ultrasound-enhanced delivery of doxorubicin-loaded nanodiamonds from pullulan-all-trans-retinal nanoparticles for effective cancer therapy. ACS Appl Mater Interfaces. 2019;11(22):20341–20349. doi: 10.1021/acsami.9b03559. [DOI] [PubMed] [Google Scholar]
- 191.Wen Y, Jia Q, Nan F, Zheng X, Liu W, Wu J, Ren H, Ge J, Wang P. Pheophytin derived near-infrared-light responsive carbon dot assembly as a new phototheranotic agent for bioimaging and photodynamic therapy. Chem Asian J. 2019;14(12):2162–2168. doi: 10.1002/asia.201900416. [DOI] [PubMed] [Google Scholar]
- 192.Zhang M, Wang W, Wu F, Zheng T, Ashley J, Mohammadniaei M, Zhang Q, Wang M, Li L, Shen J, Sun Y. Biodegradable Poly(γ-glutamic acid)@glucose oxidase@carbon dot nanoparticles for simultaneous multimodal imaging and synergetic cancer therapy. Biomaterials. 2020;252:120106. doi: 10.1016/j.biomaterials.2020.120106. [DOI] [PubMed] [Google Scholar]
- 193.Kim DH, Seo J, Na K. pH-Sensitive carbon dots for enhancing photomediated antitumor immunity. Mol Pharm. 2020;17(7):2532–2545. doi: 10.1021/acs.molpharmaceut.0c00227. [DOI] [PubMed] [Google Scholar]
- 194.Chen Z, Wang C, Li TF, Li K, Yue Y, Liu X, Xu HZ, Wen Y, Zhang Q, Han M, Komatsu N, Xu YH, Zhao L, Chen X. Doxorubicin conjugated with nanodiamonds and in free form commit glioblastoma cells to heterodromous fates. Nanomedicine (Lond) 2019;14(3):335–351. doi: 10.2217/nnm-2018-0330. [DOI] [PubMed] [Google Scholar]
- 195.Liu J, Li R, Yang B. Carbon dots: a new type of carbon-based nanomaterial with wide applications. ACS Cent Sci. 2020;6(12):2179–2195. doi: 10.1021/acscentsci.0c01306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Zhu L, Ma J, Jia N, Zhao Y, Shen H. Chitosan-coated magnetic nanoparticles as carriers of 5-fluorouracil: preparation, characterization and cytotoxicity studies. Colloids Surf B Biointerfaces. 2009;68(1):1–6. doi: 10.1016/j.colsurfb.2008.07.020. [DOI] [PubMed] [Google Scholar]
- 197.Lin H, Chen Y, Shi J. Nanoparticle-triggered in situ catalytic chemical reactions for tumour-specific therapy. Chem Soc Rev. 2018;47(6):1938–1958. doi: 10.1039/C7CS00471K. [DOI] [PubMed] [Google Scholar]
- 198.Han Y, Gao S, Zhang Y, Ni Q, Li Z, Liang XJ, Zhang J. Metal-based nanocatalyst for combined cancer therapeutics. Bioconjug Chem. 2020;31(5):1247–1258. doi: 10.1021/acs.bioconjchem.0c00194. [DOI] [PubMed] [Google Scholar]
- 199.Tang Z, Zhang H, Liu Y, Ni D, Zhang H, Zhang J, Yao Z, He M, Shi J, Bu W. Antiferromagnetic pyrite as the tumor microenvironment-mediated nanoplatform for self-enhanced tumor imaging and therapy. Adv Mater. 2017;29(47):1701683. doi: 10.1002/adma.201701683. [DOI] [PubMed] [Google Scholar]
- 200.Lee KT, Lu YJ, Mi FL, Burnouf T, Wei YT, Chiu SC, Chuang EY, Lu SY. Catalase-modulated heterogeneous fenton reaction for selective cancer cell eradication: SnFe(2)O(4) nanocrystals as an effective reagent for treating lung cancer cells. ACS Appl Mater Interfaces. 2017;9(2):1273–1279. doi: 10.1021/acsami.6b13529. [DOI] [PubMed] [Google Scholar]
- 201.Dolmans DE, Fukumura D, Jain RK. Photodynamic therapy for cancer. Nat Rev Cancer. 2003;3(5):380–387. doi: 10.1038/nrc1071. [DOI] [PubMed] [Google Scholar]
- 202.Yang Z, Sun Z, Ren Y, Chen X, Zhang W, Zhu X, Mao Z, Shen J, Nie S. Advances in nanomaterials for use in photothermal and photodynamic therapeutics (Review) Mol Med Rep. 2019;20(1):5–15. doi: 10.3892/mmr.2019.10218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Zhou M, Tian M, Li C. Copper-based nanomaterials for cancer imaging and therapy. Bioconjug Chem. 2016;27(5):1188–1199. doi: 10.1021/acs.bioconjchem.6b00156. [DOI] [PubMed] [Google Scholar]
- 204.Eshaghi Malekshah R, Fahimirad B, Khaleghian A. Synthesis, characterization, biomedical application, molecular dynamic simulation and molecular docking of schiff base complex of Cu(II) supported on Fe(3)O(4)/SiO(2)/APTS. Int J Nanomed. 2020;15:2583–2603. doi: 10.2147/IJN.S231062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Attarilar S, Yang J, Ebrahimi M, Wang Q, Liu J, Tang Y, Yang J. The toxicity phenomenon and the related occurrence in metal and metal oxide nanoparticles: a brief review from the biomedical perspective. Front Bioeng Biotechnol. 2020;8:822. doi: 10.3389/fbioe.2020.00822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Zhang X, Zheng Y, Wang Z, Huang S, Chen Y, Jiang W, Zhang H, Ding M, Li Q, Xiao X, Luo X, Wang Z, Qi H. Methotrexate-loaded PLGA nanobubbles for ultrasound imaging and Synergistic Targeted therapy of residual tumor during HIFU ablation. Biomaterials. 2014;35(19):5148–5161. doi: 10.1016/j.biomaterials.2014.02.036. [DOI] [PubMed] [Google Scholar]
- 207.Maghsoudnia N, Baradaran Eftekhari R, Naderi Sohi A, Norouzi P, Akbari H, Ghahremani MH, Soleimani M, Amini M, Samadi H, Dorkoosh FA. Mitochondrial delivery of microRNA mimic let-7b to NSCLC cells by PAMAM-based nanoparticles. J Drug Target. 2020;28:1–13. doi: 10.1080/1061186X.2020.1774594. [DOI] [PubMed] [Google Scholar]
- 208.Roy B, Ghose S, Biswas S. Therapeutic strategies for miRNA delivery to reduce hepatocellular carcinoma. Semin Cell Dev Biol. 2021. 10.1016/j.semcdb.2021.04.006. [DOI] [PubMed]
- 209.Sengupta S, Eavarone D, Capila I, Zhao G, Watson N, Kiziltepe T, Sasisekharan R. Temporal targeting of tumour cells and neovasculature with a nanoscale delivery system. Nature. 2005;436(7050):568–572. doi: 10.1038/nature03794. [DOI] [PubMed] [Google Scholar]
- 210.Trédan O, Galmarini CM, Patel K, Tannock IF. Drug resistance and the solid tumor microenvironment. J Natl Cancer Inst. 2007;99(19):1441–1454. doi: 10.1093/jnci/djm135. [DOI] [PubMed] [Google Scholar]
- 211.Gkretsi V, Stylianou A, Papageorgis P, Polydorou C, Stylianopoulos T. Remodeling components of the tumor microenvironment to enhance cancer therapy. Front Oncol. 2015;5:214. doi: 10.3389/fonc.2015.00214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Klemm F, Joyce JA. Microenvironmental regulation of therapeutic response in cancer. Trends Cell Biol. 2015;25(4):198–213. doi: 10.1016/j.tcb.2014.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Merchant N, Nagaraju GP, Rajitha B, Lammata S, Jella KK, Buchwald ZS, Lakka SS, Ali AN. Matrix metalloproteinases: their functional role in lung cancer. Carcinogenesis. 2017;38(8):766–780. doi: 10.1093/carcin/bgx063. [DOI] [PubMed] [Google Scholar]
- 214.Hingorani SR, Harris WP, Beck JT, Berdov BA, Wagner SA, Pshevlotsky EM, Tjulandin SA, Gladkov OA, Holcombe RF, Korn R, Raghunand N, Dychter S, Jiang P, Shepard HM, Devoe CE. Phase Ib study of PEGylated recombinant human hyaluronidase and gemcitabine in patients with advanced pancreatic cancer. Clin Cancer Res. 2016;22(12):2848–2854. doi: 10.1158/1078-0432.CCR-15-2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Chen E, Han S, Song B, Xu L, Yuan H, Liang M, Sun Y. Mechanism investigation of hyaluronidase-combined multistage nanoparticles for solid tumor penetration and antitumor effect. Int J Nanomed. 2020;15:6311–6324. doi: 10.2147/IJN.S257164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Yan S, Luo Z, Li Z, Wang Y, Tao J, Gong C, Liu X. Improving cancer immunotherapy outcomes using biomaterials. Angew Chem Int Ed Engl. 2020;59(40):17332–17343. doi: 10.1002/anie.202002780. [DOI] [PubMed] [Google Scholar]
- 217.Liu YT, Sun ZJ. Turning cold tumors into hot tumors by improving T-cell infiltration. Theranostics. 2021;11(11):5365–5386. doi: 10.7150/thno.58390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Bu J, Nair A, Iida M, Jeong WJ, Poellmann MJ, Mudd K, Kubiatowicz LJ, Liu EW, Wheeler DL, Hong S. An avidity-based PD-L1 antagonist using nanoparticle-antibody conjugates for enhanced immunotherapy. Nano Lett. 2020;20(7):4901–4909. doi: 10.1021/acs.nanolett.0c00953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Sanaei MJ, Pourbagheri-Sigaroodi A, Kaveh V, Sheikholeslami SA, Salari S, Bashash D. The application of nano-medicine to overcome the challenges related to immune checkpoint blockades in cancer immunotherapy: Recent advances and opportunities. Crit Rev Oncol Hematol. 2021;157:103160. doi: 10.1016/j.critrevonc.2020.103160. [DOI] [PubMed] [Google Scholar]
- 220.Rios-Doria J, Durham N, Wetzel L, Rothstein R, Chesebrough J, Holoweckyj N, Zhao W, Leow CC, Hollingsworth R. Doxil synergizes with cancer immunotherapies to enhance antitumor responses in syngeneic mouse models. Neoplasia. 2015;17(8):661–670. doi: 10.1016/j.neo.2015.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Li SY, Liu Y, Xu CF, Shen S, Sun R, Du XJ, Xia JX, Zhu YH, Wang J. Restoring anti-tumor functions of T cells via nanoparticle-mediated immune checkpoint modulation. J Control Release. 2016;231:17–28. doi: 10.1016/j.jconrel.2016.01.044. [DOI] [PubMed] [Google Scholar]
- 222.Liu L, Wang Y, Miao L, Liu Q, Musetti S, Li J, Huang L. Combination immunotherapy of MUC1 mRNA nano-vaccine and CTLA-4 blockade effectively inhibits growth of triple negative breast cancer. Mol Ther. 2018;26(1):45–55. doi: 10.1016/j.ymthe.2017.10.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Zhou F, Wang M, Luo T, Qu J, Chen WR. Photo-activated chemo-immunotherapy for metastatic cancer using a synergistic graphene nanosystem. Biomaterials. 2021;265:120421. doi: 10.1016/j.biomaterials.2020.120421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Hanahan D, Weinberg RA. The hallmarks of cancer. Cell. 2000;100(1):57–70. doi: 10.1016/S0092-8674(00)81683-9. [DOI] [PubMed] [Google Scholar]
- 225.Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell. 2011;144(5):646–674. doi: 10.1016/j.cell.2011.02.013. [DOI] [PubMed] [Google Scholar]
- 226.Hartshorn CM, Bradbury MS, Lanza GM, Nel AE, Rao J, Wang AZ, Wiesner UB, Yang L, Grodzinski P. Nanotechnology strategies to advance outcomes in clinical cancer care. ACS Nano. 2018;12(1):24–43. doi: 10.1021/acsnano.7b05108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Yona S, Gordon S. From the reticuloendothelial to mononuclear phagocyte system—the unaccounted years. Front Immunol. 2015;6:328. doi: 10.3389/fimmu.2015.00328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Hume DA, Irvine KM, Pridans C. The mononuclear phagocyte system: the relationship between monocytes and macrophages. Trends Immunol. 2019;40(2):98–112. doi: 10.1016/j.it.2018.11.007. [DOI] [PubMed] [Google Scholar]
- 229.Liang T, Zhang R, Liu X, Ding Q, Wu S, Li C, Lin Y, Ye Y, Zhong Z, Zhou M. Recent advances in macrophage-mediated drug delivery systems. Int J Nanomed. 2021;16:2703–2714. doi: 10.2147/IJN.S298159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.von Roemeling C, Jiang W, Chan CK, Weissman IL, Kim BYS. Breaking down the barriers to precision cancer nanomedicine. Trends Biotechnol. 2017;35(2):159–171. doi: 10.1016/j.tibtech.2016.07.006. [DOI] [PubMed] [Google Scholar]
- 231.Tran S, DeGiovanni PJ, Piel B, Rai P. Cancer nanomedicine: a review of recent success in drug delivery. Clin Transl Med. 2017;6(1):44. doi: 10.1186/s40169-017-0175-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Emami J, Yousefian H, Sadeghi H. Targeted nanostructured lipid carrier for brain delivery of artemisinin: design, preparation, characterization, optimization and cell toxicity. J Pharm Pharm Sci. 2018;21(1s):225s–241s. doi: 10.18433/jpps30117. [DOI] [PubMed] [Google Scholar]
- 233.Hu Y, Gaillard PJ, de Lange ECM, Hammarlund-Udenaes M. Targeted brain delivery of methotrexate by glutathione PEGylated liposomes: how can the formulation make a difference? Eur J Pharm Biopharm. 2019;139:197–204. doi: 10.1016/j.ejpb.2019.04.004. [DOI] [PubMed] [Google Scholar]
- 234.Feng Q, Shen Y, Fu Y, Muroski ME, Zhang P, Wang Q, Xu C, Lesniak MS, Li G, Cheng Y. Self-assembly of gold nanoparticles shows microenvironment-mediated dynamic switching and enhanced brain tumor targeting. Theranostics. 2017;7(7):1875–1889. doi: 10.7150/thno.18985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Ruan S, Xiao W, Hu C, Zhang H, Rao J, Wang S, Wang X, He Q, Gao H. Ligand-mediated and enzyme-directed precise targeting and retention for the enhanced treatment of glioblastoma. ACS Appl Mater Interfaces. 2017;9(24):20348–20360. doi: 10.1021/acsami.7b02303. [DOI] [PubMed] [Google Scholar]
- 236.Ohta S, Kikuchi E, Ishijima A, Azuma T, Sakuma I, Ito T. Investigating the optimum size of nanoparticles for their delivery into the brain assisted by focused ultrasound-induced blood-brain barrier opening. Sci Rep. 2020;10(1):18220. doi: 10.1038/s41598-020-75253-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Zhang J, Zhang Z, Jiang M, Li S, Yuan H, Sun H, Yang F, Liang H. Developing a novel gold(III) agent to treat glioma based on the unique properties of apoferritin nanoparticles: inducing lethal autophagy and apoptosis. J Med Chem. 2020;63(22):13695–13708. doi: 10.1021/acs.jmedchem.0c01257. [DOI] [PubMed] [Google Scholar]
- 238.Gao H, Chu C, Cheng Y, Zhang Y, Pang X, Li D, Wang X, Ren E, Xie F, Bai Y, Chen L, Liu G, Wang M. In situ formation of nanotheranostics to overcome the blood-brain barrier and enhance treatment of orthotopic glioma. ACS Appl Mater Interfaces. 2020;12(24):26880–26892. doi: 10.1021/acsami.0c03873. [DOI] [PubMed] [Google Scholar]
- 239.Nicolas J, Mura S, Brambilla D, Mackiewicz N, Couvreur P. Design, functionalization strategies and biomedical applications of targeted biodegradable/biocompatible polymer-based nanocarriers for drug delivery. Chem Soc Rev. 2013;42(3):1147–1235. doi: 10.1039/C2CS35265F. [DOI] [PubMed] [Google Scholar]
- 240.Wang W, Zhou F, Ge L, Liu X, Kong F. Transferrin-PEG-PE modified dexamethasone conjugated cationic lipid carrier mediated gene delivery system for tumor-targeted transfection. Int J Nanomed. 2012;7:2513–2522. doi: 10.2147/IJN.S31915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Markman JL, Rekechenetskiy A, Holler E, Ljubimova JY. Nanomedicine therapeutic approaches to overcome cancer drug resistance. Adv Drug Deliv Rev. 2013;65(13–14):1866–1879. doi: 10.1016/j.addr.2013.09.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Ryman-Rasmussen JP, Riviere JE, Monteiro-Riviere NA. Penetration of intact skin by quantum dots with diverse physicochemical properties. Toxicol Sci. 2006;91(1):159–165. doi: 10.1093/toxsci/kfj122. [DOI] [PubMed] [Google Scholar]
- 243.Xia T, Kovochich M, Brant J, Hotze M, Sempf J, Oberley T, Sioutas C, Yeh JI, Wiesner MR, Nel AE. Comparison of the abilities of ambient and manufactured nanoparticles to induce cellular toxicity according to an oxidative stress paradigm. Nano Lett. 2006;6(8):1794–1807. doi: 10.1021/nl061025k. [DOI] [PubMed] [Google Scholar]
- 244.Penn A, Murphy G, Barker S, Henk W, Penn L. Combustion-derived ultrafine particles transport organic toxicants to target respiratory cells. Environ Health Perspect. 2005;113(8):956–963. doi: 10.1289/ehp.7661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.Vallhov H, Qin J, Johansson SM, Ahlborg N, Muhammed MA, Scheynius A, Gabrielsson S. The importance of an endotoxin-free environment during the production of nanoparticles used in medical applications. Nano Lett. 2006;6(8):1682–1686. doi: 10.1021/nl060860z. [DOI] [PubMed] [Google Scholar]
- 246.Danhier F. To exploit the tumor microenvironment: since the EPR effect fails in the clinic, what is the future of nanomedicine? J Control Release. 2016;244(Pt A):108–121. doi: 10.1016/j.jconrel.2016.11.015. [DOI] [PubMed] [Google Scholar]
- 247.Sindhwani S, Syed AM, Ngai J, Kingston BR, Maiorino L, Rothschild J, MacMillan P, Zhang Y, Rajesh NU, Hoang T, Wu JLY, Wilhelm S, Zilman A, Gadde S, Sulaiman A, Ouyang B, Lin Z, Wang L, Egeblad M, Chan WCW. The entry of nanoparticles into solid tumours. Nat Mater. 2020;19(5):566–575. doi: 10.1038/s41563-019-0566-2. [DOI] [PubMed] [Google Scholar]
- 248.Ramanathan RK, Korn RL, Sachdev JC, Fetterly GJ, Marceau K, Marsh V, Neil JM, Newbold RG, Raghunand N, Prey J. Abstract CT224: Pilot study in patients with advanced solid tumors to evaluate feasibility of ferumoxytol (FMX) as tumor imaging agent prior to MM-398, a nanoliposomal irinotecan (nal-IRI). In: AACR; 2014.
- 249.Shi J, Kantoff PW, Wooster R, Farokhzad OC. Cancer nanomedicine: progress, challenges and opportunities. Nat Rev Cancer. 2017;17(1):20–37. doi: 10.1038/nrc.2016.108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 250.Bertrand N, Wu J, Xu X, Kamaly N, Farokhzad OC. Cancer nanotechnology: the impact of passive and active targeting in the era of modern cancer biology. Adv Drug Deliv Rev. 2014;66:2–25. doi: 10.1016/j.addr.2013.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251.Albanese A, Lam AK, Sykes EA, Rocheleau JV, Chan WC. Tumour-on-a-chip provides an optical window into nanoparticle tissue transport. Nat Commun. 2013;4:2718. doi: 10.1038/ncomms3718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252.Dutta D, Heo I, Clevers H. Disease modeling in stem cell-derived 3D organoid systems. Trends Mol Med. 2017;23(5):393–410. doi: 10.1016/j.molmed.2017.02.007. [DOI] [PubMed] [Google Scholar]
- 253.Bleijs M, van de Wetering M, Clevers H, Drost J. Xenograft and organoid model systems in cancer research. Embo J. 2019;38(15):e101654. doi: 10.15252/embj.2019101654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.Bobo D, Robinson KJ, Islam J, Thurecht KJ, Corrie SR. Nanoparticle-based medicines: a review of FDA-approved materials and clinical trials to date. Pharm Res. 2016;33(10):2373–2387. doi: 10.1007/s11095-016-1958-5. [DOI] [PubMed] [Google Scholar]
- 255.Wicki A, Witzigmann D, Balasubramanian V, Huwyler J. Nanomedicine in cancer therapy: challenges, opportunities, and clinical applications. J Control Release. 2015;200:138–157. doi: 10.1016/j.jconrel.2014.12.030. [DOI] [PubMed] [Google Scholar]
- 256.Sainz V, Conniot J, Matos AI, Peres C, Zupancic E, Moura L, Silva LC, Florindo HF, Gaspar RS. Regulatory aspects on nanomedicines. Biochem Biophys Res Commun. 2015;468(3):504–510. doi: 10.1016/j.bbrc.2015.08.023. [DOI] [PubMed] [Google Scholar]
- 257.van Elk M, Murphy BP, Eufrásio-da-Silva T, O'Reilly DP, Vermonden T, Hennink WE, Duffy GP, Ruiz-Hernández E. Nanomedicines for advanced cancer treatments: transitioning towards responsive systems. Int J Pharm. 2016;515(1–2):132–164. doi: 10.1016/j.ijpharm.2016.10.013. [DOI] [PubMed] [Google Scholar]
- 258.Raj S, Khurana S, Choudhari R, Kesari KK, Kamal MA, Garg N, Ruokolainen J, Das BC, Kumar D. Specific targeting cancer cells with nanoparticles and drug delivery in cancer therapy. Semin Cancer Biol 2019;69:166–77. [DOI] [PubMed]
- 259.US Clinical trials website [http://clinicaltrials.gov/]
- 260.US Food and Drug Administration website [http://www.accessdata.fda.gov/]
- 261.Sebak AA, Gomaa IEO, ElMeshad AN, Farag MH, Breitinger U, Breitinger HG, AbdelKader MH. Distinct proteins in protein corona of nanoparticles represent a promising venue for endogenous targeting—part I: in vitro release and intracellular uptake perspective. Int J Nanomedicine. 2020;15:8845–8862. doi: 10.2147/IJN.S273713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 262.Vroman L, Adams AL, Fischer GC, Munoz PC. Interaction of high molecular weight kininogen, factor XII, and fibrinogen in plasma at interfaces. Blood. 1980;55(1):156–159. doi: 10.1182/blood.V55.1.156.156. [DOI] [PubMed] [Google Scholar]
- 263.Pederzoli F, Tosi G, Vandelli MA, Belletti D, Forni F, Ruozi B. Protein corona and nanoparticles: how can we investigate on? Wiley Interdiscip Rev Nanomed Nanobiotechnol. 2017;9(6):e1467. doi: 10.1002/wnan.1467. [DOI] [PubMed] [Google Scholar]
- 264.Risha Y, Minic Z, Ghobadloo SM, Berezovski MV. The proteomic analysis of breast cell line exosomes reveals disease patterns and potential biomarkers. Sci Rep. 2020;10(1):13572. doi: 10.1038/s41598-020-70393-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 265.Elzek MA, Rodland KD. Proteomics of ovarian cancer: functional insights and clinical applications. Cancer Metastasis Rev. 2015;34(1):83–96. doi: 10.1007/s10555-014-9547-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.