Abstract
Background
Young gay, bisexual, and other men who have sex with men (YMSM) are vulnerable to the risks associated with sexualized substance use. This is a novel study in Singapore that aims to classify patterns of sexualized substance use among YMSM, and investigate its association with sexual and mental health outcomes.
Methods
In this cross-sectional study among 570 YMSM aged 18 to 25 years old, latent class analysis (LCA) conducted to identify classes with similar patterns of sexualized substance use, across which measures of inconsistent condom use, recent STI diagnoses, past suicide ideation and depression severity were compared.
Results
LCA revealed three classes of YMSM based on types of substances ever used in sexualized contexts, which we labelled as ‘substance-naive’, ‘substance-novice’, and ‘chemsex’. Substance-naive participants (n = 404) had only ever used alcohol, while substance-novice participants (n = 143) were primarily amyl nitrite users with a small proportion who reported using chemsex-related drugs. Chemsex participants (n = 23) comprised individuals who had mostly used such drugs. Those in the chemsex group were more likely to report recent unprotected anal sex with casual partners (aPR = 3.28, 95%CI [1.85, 5.79]), depression severity (aβ = 3.69, 95%CI [0.87, 6.51]) and a history of suicide ideation (aPR = 1.64, 95%CI [1.33, 2.03]).
Conclusions
Findings of this study highlight how the use of varying substances in sexualized contexts may be classified and characterized by different sexual and mental health outcomes. Health promotion efforts should be differentiated accordingly to address the risks associated with sexualized substance use among YMSM.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12889-021-11056-5.
Keywords: Chemsex, Alcohol, Poppers, MSM, Singapore
Background
Approximately 38.0 million people globally were estimated to be living with HIV in 2019 [1]. Gay, bisexual, and other men who have sex with men (GBMSM) constitute a key population that continues to be disproportionately affected by HIV on a global scale [2]. Greater vulnerability of GBMSM to HIV may be attributable to physiological, psychosocial, and institutional factors [3, 4]. For example, past research have shown how measures of sexual orientation concealment, internalized homophobia, as well as experienced homophobia have been associated with greater risks of HIV and other sexually transmitted infections acquisition among GBMSM [5–7].
Past studies have shown that the prevalence of drug use is higher among GBMSM, compared to the general heterosexual male population, and is often used in sexualized contexts [8–10]. Sexualized substance use has also been referred to by other terms such as ‘chill fun’, ‘chemsex’, ‘party and play’ and ‘wired sex’, which vary by country setting. These terms typically denote the use of substances such as mephedrone, amyl nitrites (poppers), gamma-hydroxybutyrate/gamma-butyrolactone (GHB/GBL), crystal methamphetamine (meth), as well as drugs usually prescribed for erectile dysfunction (ED) before or during sexual activity [11–13].
Chemsex has been associated with several health implications among GBMSM. With regards to sexual health, studies have found that GBMSM who have engaged in chemsex were more likely to report HIV and other STI risk-related behaviors, as well as the incidence of HIV and sexually transmitted infections (STIs) [14, 15]. With regard to mental health, GBMSM who engage in chemsex have also reported correspondingly poorer mental health outcomes, such as greater depression severity, poorer general mental well-being, and internalized homophobia [13, 16, 17]. Heavy alcohol use has also been found to be common among GBMSM in developed country settings [9, 18, 19], and that sexual minorities such as GBMSM reported a lower age of alcohol use debut compared to their heterosexual counterparts [20, 21]. Such early onset of alcohol use was associated with increase sexual and mental health risks among GBMSM surveyed [22]. The use of alcohol in a sexual context has also been found to be associated with behaviors associated with HIV acquisition risk [23–25].
Within communities of GBMSM, young gay, bisexual, and other men who have sex with men (YMSM) experience a greater burden of HIV and other sexually transmitted infections (STI) risk compared to their older counterparts, which may be attributed to a higher incidence of risky sexual behaviors, the lack of help-seeking behaviors, and sexualized substance use [26, 27]. YMSM are also especially vulnerable to substance use disorders and the risks associated with them [28–30]. A study among YMSM aged 12 to 24 years in eight United States cities found that 10.8% of participants had reported using methamphetamine in the past 3 months [28], while studies in other settings similarly illustrate that YMSM already report using illicit substances at a young age [13, 31], and those who report an earlier age of sexual debut or who are exposed to sexual networks earlier are more likely to initiate chemsex [32].
Past studies employing latent class analysis have found that substance use patterns may not be homogenous among GBMSM, and these classes are characterized by a range of substance use-related behaviors, from GBMSM who do not use substances in sexualized contexts, to those who engage in polydrug use during sex. These studies also find that these classes may be associated with varying sexual risk behaviors [14, 33]. Similarly, the present study will conduct latent class analysis on observational, cross-sectional data from the baseline analysis of the Pink Carpet Y Cohort Study (PCYCS), Singapore’s first prospective cohort study among YMSM, to explore classes of sexualized substance use and its association with other sexual and mental health outcomes. This study is noteworthy as it is novel in the present setting, and allows us to better understand the risk factors that may be associated with substance use initiation among YMSM.
Methods
Country setting
GBMSM are disproportionately represented in prevalent cases of HIV in Singapore. As of 2019, a total of 8295 incident HIV infections among Singapore residents have been notified to the Singapore ministry of health (MOH). In 2011, yearly incident cases of HIV transmitted through male ‘homosexual or bisexual’ modes exceeded that of ‘heterosexual’ modes for the first time, and that trend has persisted since [34]. With regard to GBMSM in Singapore, the general public still holds conservative and largely negative views towards the community. Specifically, most people have indicated in recent surveys that they had perceived same-sex relationships as being wrong, and are also not in favor of the repeal of Section 377A of the Singapore Penal Code, the law that criminalizes sexual relations between men [35, 36]. Past studies have also established the negative impact and trickle-down effects that such stigma has on HIV prevention efforts among GBMSM in Singapore [37–39]. With regard to substance use, a qualitative study conducted on chemsex among GBMSM in Singapore highlight how institutionalized and societal stigma contributed to internalized homophobia that drive chemsex as a coping mechanism, as well as barriers to accessing substance use recovery and care services [13].
Advocacy and health promotion efforts for GBMSM in Singapore have largely stemmed from community-based efforts, given the presence of Section 377A, which precludes the development and implementation of wider programs such as comprehensive sexuality education and GBMSM-specific healthcare services, or the censorship of positive portrayals of LGBT individuals in the general media [40]. Such community-based efforts include the implementation of community-based anonymous testing sites for HIV and other STIs, as well as HIV and other STIs prevention efforts around education, promoting sexual health-seeking behaviors, and the uptake of novel HIV prevention technologies such as HIV pre-exposure prophylaxis and post-exposure prophylaxis in key populations at risk of acquiring HIV and other STIs [41].
Participants and recruitment
The PCYCS is a prospective cohort study exploring the syndemic risks associated with HIV and other sexually transmitted infections (STI) acquisition among YMSM in Singapore. However, this study presents analysis from observational, cross-sectional data obtained from the baseline survey of the PCYCS. This study was a partnership between Action for AIDS Singapore (AFA), an organization serving the sexual health needs of GBMSM, and the National University of Singapore (NUS). To be eligible for this cohort, participants had to be HIV-negative or unsure of their HIV status, between the ages of 18 to 25 years old, Singapore citizens or permanent residents, and identify as gay, bisexual, or queer (sexual orientation) men at the point of recruitment, which spanned across May to September 2019. Participants were asked to self-report these attributes. With regard to sample size calculation, we targeted recruitment of at least 384 participants. This sample size was obtained to achieve a 95% confidence level and 5% margin of error, assuming a population of 210,000 GBMSM in Singapore [42]. However, 600 participants were targeted for recruitment to account for potential attrition at each follow-up for this cohort study.
Participants were invited to participate in this study through a recruitment flyer that was disseminated through both online (e.g. social media) and offline (e.g. at the organization’s office or outreach activities) channels by a network of community-based organizations in Singapore who are engaged in health advocacy-related activities for GBMSM. Participants who were interested in participating and were eligible for the study signed up through an enrolment link with their self-reported alias, contact details, date of birth, gender, HIV status, sexual orientation, and their residence status. An AFA staff member subsequently verified the eligibility of participants who had signed up prior to sending them a unique identifier, and a link for the baseline survey.
It was imperative for the team to ensure that participants’ identities their data would remain confidential, as drug use and sexual relations between men are criminalized in Singapore. To do so, the researchers ensured that no staff member from AFA or NUS had full access to either the enrolment details held by AFA which contained aliases and contact details of participants, and the baseline survey results held by NUS. Both sets of data were only linked by the unique identifier which participants entered at the beginning of the survey. Upon completion of the survey, a NUS staff member provided AFA with the unique identifiers who had completed the baseline survey, and an SGD20.00 (approximately USD15.00) cash reimbursement was given to the participant. A total of 570 participants were recruited at the baseline of the cohort; the response rate could not be established as it was not possible to ascertain the total number of eligible participants that the recruitment flyers had reached. Participants could also refer their friends to participate in the survey and be reimbursed SGD5.00 (approximately USD3.75) for each eligible individual successfully referred and who had completed the baseline survey; a total of 171 (30.0%) of participants were recruited through referrals.
Ethics declaration
Ethics approval was obtained from the institutional review board at the National University of Singapore (NUS-IRB Reference Code S-19-007) prior to data collection.
Variable measures
A copy of the survey questionnaire developed for this study has been published elsewhere [43]. The survey collected sociodemographic information from respondents, including age, ethnicity, gender, sexual orientation, and monthly household income. Participants were asked if they had ever used a series of substances in sexual contexts, including alcohol, poppers, meth, GHB/GBL as well as other erectile dysfunction (ED) medication or drugs (e.g. Viagra, Cialis, ‘black ants’). For sexual health outcomes, participants were asked about their patterns of unprotected anal sex, as well as STI diagnoses in the last 6 months. Unprotected anal sex with casual partners in the last 6 months was coded as a binary variable (yes vs no), and was derived from a series of questions that solicited frequency of self-reported condom use through a five-point Likert scale from 1 to 5, with 1 being that they did not use condoms and 5 being that they had always used condoms; this question was repeated for permutations of oral and anal sex with regular, casual, and sex worker partners in the last 6 months. Participants who had not used condoms all the time with casual and sex worker partners in the last 6 months were coded as ‘yes’ under this variable. Participants who also reported being tested positive for either gonorrhoea, syphilis, chlamydia, genital herpes, genital warts or hepatitis C were assigned as having been diagnosed with an STI in the past 6 months through a binary (yes vs no) variable.
For mental health outcomes, both depression severity and past suicide ideation were measured. Depression severity, which was measured through the well-established, nine-item patient health questionnaire-9 (PHQ-9) validated by Kroenke and colleagues [44, 45]. Participants were asked “over the last 2 weeks, how often have you been bothered by any of the following problems?” to a total of nine statements, to which they could respond to four possible answers on a Likert scale; 1 being not at all and 4 being nearly every day. Depression severity was measured as an index that was the sum score of all nine items, with a minimum score of 0 and a maximum score of 27. A score of 20 or higher indicates severe depression, 15 to 19 suggests moderately severe depression, 10 to 14 suggests moderate depression, while a score between 5 to 9 indicates mild symptoms of depression. Cronbach’s alpha of the scale was reported as 0.92. Participants were also asked about their suicide-related behaviors, including if they had ever contemplated suicide by responding to three possible answers: yes, no, or prefer not to say.
Statistical analysis
Statistical analysis was carried out using the statistical software STATA version 15 (Stata Corp, College Station, TX, USA). We employed descriptive statistics to identify trends in sample characteristics. Details on the latent class analysis employed has been published elsewhere [32], where the chosen variables included a history of using alcohol, poppers, meth, GHB/GBL as well as other ED medication or drugs (e.g. Viagra, Cialis, ‘black ants’) in sexualized contexts. Given that the three-class model had the lowest AIC and BIC values, it was thus reported in this study, which we labelled post hoc as ‘substance-naïve’, ‘substance-novice’ and ‘chemsex’. A summary of goodness-of-fit statistics are provided in Supplementary Table S1. Following identification of latent classes, we sought to determine the association between varying classes with outcome variables of unprotected anal sex, STI diagnoses, depression severity and past suicide ideation while adjusting for key sociodemographic covariates. We employed multivariable Poisson regression models with robust sandwich variances to compute the crude prevalence ratio (PR) and adjusted prevalence ratio (aPR) estimating these outcome variables. Statistical significance was set at p < 0.05. Analysis for this study was not pre-registered and the results reported here should be considered exploratory.
Results
Sociodemographic attributes and description of analytic sample
A total of 570 participants were recruited in this study. Table 1 summarizes the sociodemographic attributes and overall description of the analytic sample. In terms of their sociodemographic attributes, the mean age of the sample was 21.9 years (SD = 2.17). 83.9% of the participants identified as Chinese (n = 478), 92.1% identified as cisgender male (n = 525), 71.6% identified as gay (n = 408), and 35.6% reported a monthly household income of SGD5000 and above (n = 203). A total of 33.5% (n = 189), 28.0% (n = 158), 4.6% (n = 26), 4.6% (n = 26), and 4.6% (n = 26) reported ever using alcohol, poppers, meth, GHB/GBL, and ED medication or drugs in sexual contexts, respectively.
Table 1.
Description of analytic sample (n = 570)
| Variables | n / Mean | % / SD |
|---|---|---|
| Age | 21.9 | 2.17 |
| Chinese ethnicity (Ref = Non-Chinese) | 478 | 83.9% |
| Cisgender male (Ref = Transgender, genderqueer, or others) | 525 | 92.1% |
| Gay (Ref = Bisexual, queer, or others) | 408 | 71.6% |
| Monthly household income ≥ SGD5000 (Ref < SGD5000) | 203 | 35.6% |
| Ever had sexualized substance use with | ||
| Alcohol | 190 | 33.3% |
| Amyl nitrites (Poppers) | 161 | 28.3% |
| Crystal methamphetamine (Meth) | 27 | 4.7% |
| Gamma-hydroxybutyrate/gamma-butyrolactone (GHB/GBL) | 27 | 4.7% |
| Erectile dysfunction drugs (ED) | 26 | 4.6% |
| Ever contemplated suicide | 308 | 54.0% |
| Unprotected anal sex with casual partners in the last 6 months | 96 | 16.8% |
| Tested positive for an STI in the last 6 months | 39 | 6.8% |
| Depression severity (PHQ-9) | 7.9 | 6.79 |
Abbreviation: SD Standard Deviation, STI Sexually Transmitted Infections, GHB/GBL Gamma-Hydroxybutyrate/Gamma-Butyrolactone, PHQ-9 Patient Health Questionnaire-9
With regard to the outcome variables of the study, participants reported a mean score of 7.9 (SD = 6.79) on depression severity, while most participants had ever contemplated suicide (n = 308, 54.1%). A total of 16.8% of participants also reported unprotected anal sex with casual partners in the last 6 months (n = 96), while 6.7% (n = 38) reported testing positive for an STI in the past 6 months.
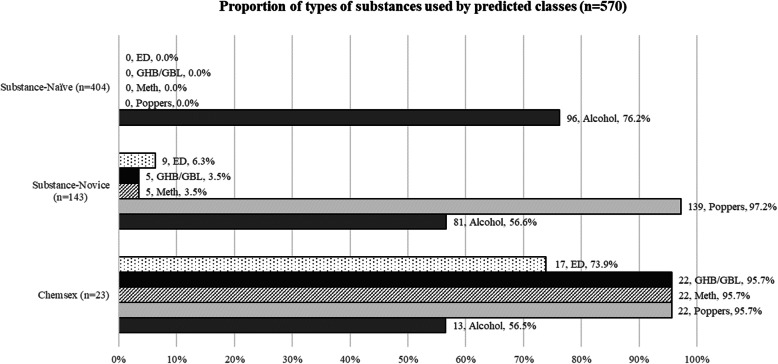
Patterns of sexualized substance use
LCA revealed three classes (AIC = 1743.14; BIC = 1808.33), which we labelled post hoc as ‘Substance-naive’, ‘Substance-novice’, and ‘Chemsex’. Participants in the substance-naive (n = 403) class reported only ever using alcohol (n = 96, 76.2%), and never using any other substances during sex. Participants in the substance-novice class (n = 143) had mostly ever used poppers during sex (n = 139, 97.2%), with some reporting ever using meth (n = 5, 3.9%), GHB/GBL (n = 5, 3.9%), and erectile dysfunction drugs (n = 9, 6.3%) during sex, over and above those who reported ever using alcohol during sex (n = 81, 56.6%). A similar proportion of participants in the chemsex class (n = 23) reported ever using alcohol (n = 13, 56.5%) and poppers during sex (n = 22, 95.7%), but a large proportion reported ever using meth (n = 22, 95.7%), GHB/GBL (n = 22, 95.7%), and erectile dysfunction drugs (n = 17, 73.9%) during sex. Table 2 describes the analytic sample by substance using classes, while Fig. 1 summarizes the proportion of individuals who reported ever using varying substances by substance using classes.
Table 2.
Description of analytic sample by predicted substance-using classes (n = 570)
| Variables | Substance-Naïve (n = 404) | Substance-Novice (n = 143) | Chemsex (n = 23) | Fisher’s Exact Test p-value |
|||
|---|---|---|---|---|---|---|---|
| n/Mean | %/SD | n/Mean | %/SD | n/Mean | %/SD | ||
| Age | 21.7 | 2.18 | 22.4 | 2.11 | 22.3 | 1.77 | 0.001 |
| Chinese ethnicity (Ref = Non-Chinese) | 336 | 83.2% | 124 | 86.7% | 18 | 78.3% | 0.436 |
| Cisgender male (Ref = Transgender, genderqueer, or others) | 365 | 90.4% | 139 | 97.2% | 21 | 91.3% | 0.018 |
| Gay (Ref = Bisexual, queer, or others) | 268 | 66.3% | 122 | 85.3% | 18 | 78.3% | < 0.001 |
| Monthly household income ≥ SGD5000 (Ref < SGD5000) | 131 | 32.4% | 65 | 45.5% | 7 | 30.4% | 0.019 |
| Ever had sexualized substance use with | |||||||
| Alcohol | 96 | 76.2% | 81 | 56.6% | 13 | 56.5% | < 0.001 |
| Amyl nitrites (Poppers) | 0 | 0.0% | 139 | 97.2% | 22 | 95.7% | < 0.001 |
| Crystal methamphetamine (Meth) | 0 | 0.0% | 5 | 3.5% | 22 | 95.7% | < 0.001 |
| Gamma-Hydroxybutyrate/Gamma-Butyrolactone (GHB/GBL) | 0 | 0.0% | 5 | 3.5% | 22 | 95.7% | < 0.001 |
| Erectile dysfunction drugs (ED) | 0 | 0.0% | 9 | 6.3% | 17 | 73.9% | < 0.001 |
| Ever contemplated suicide | 207 | 51.2% | 82 | 57.3% | 19 | 82.6% | 0.007 |
| Unprotected anal sex with casual partners in the last 6 months | 51 | 12.6% | 36 | 25.2% | 9 | 39.1% | < 0.001 |
| Tested positive for an STI in the last 6 months | 22 | 5.5% | 15 | 10.5% | 2 | 8.7% | 0.083 |
| Depression severity (PHQ-9) | 7.9 | 6.69 | 7.4 | 6.60 | 11.4 | 8.87 | 0.030 |
Abbreviation: SD Standard Deviation, STI Sexually Transmitted Infections, GHB/GBL Gamma-Hydroxybutyrate/Gamma-Butyrolactone, PHQ-9 Patient Health Questionnaire-9
Fig. 1.
Proportion of types of substances used by predicted classes (n=570)
Association between substance use class membership and sexual health outcomes
Table 3 summarizes the associations between substance use class membership and sexual health outcomes. At the bivariate level, participants who were in the substance-novice (PR = 1.99, 95%CI [1.36, 2.92]) and chemsex (PR = 3.10, 95%CI [1.75, 5.49]) classes were more likely than substance-naive participants to have reported engaging in unprotected anal sex with a casual partner in the last 6 months. Participants who were in the substance-novice class were also more likely that those in the substance-naive class to have reported a diagnosis for any STI in the last 6 months (PR = 1.93, 95%CI [1.03, 3.61]). At the multivariable level, analyses revealed that an increasing age was negatively associated with unprotected anal sex with casual partners in the last 6 months (aPR = 0.91, 95%CI [0.84, 0.99]), while participants who were in the substance-novice (aPR = 2.24, 95%CI [1.51, 3.33]) and chemsex (aPR = 3.28, 95%CI [1.85, 5.79]) classes were more likely than substance-naive participants to have reported engaging in unprotected anal sex with a casual partner in the last 6 months. Participants who were in the substance-novice class were also more likely that those in the substance-naive class to have reported a diagnosis for any STI in the last 6 months (aPR = 2.01, 95%CI [1.05, 3.85]).
Table 3.
Multivariable Poisson regression for sexual health outcomes and its association with substance using classes
| Unprotected anal sex with casual partners in the last six months (n = 96) | STI diagnoses in the last six months (n = 39) | |||||||
|---|---|---|---|---|---|---|---|---|
| PR | 95% CI | aPR | 95% CI | PR | 95% CI | aPR | 95% CI | |
| Age | 0.94 | (0.87, 1.02) | 0.91 | (0.84, 0.99) | 0.95 | (0.83, 1.08) | 0.92 | (0.80, 1.06) |
| Chinese ethnicity (Ref = Non-Chinese) | 0.83 | (0.53, 1.32) | 0.85 | (0.53, 1.36) | 0.75 | (0.35, 1.57) | 0.72 | (0.35, 1.51) |
| Cisgender male (Ref = Transgender, genderqueer, or others) | 0.83 | (0.45, 1.53) | 0.77 | (0.43, 1.37) | 1.59 | (0.39, 6.37) | 1.42 | (0.36, 5.63) |
| Gay (Ref = Bisexual, queer, or others) | 1.13 | (0.74, 1.71) | 1.04 | (0.67, 1.60) | 1.32 | (0.64, 2.73) | 1.19 | (0.57, 2.46) |
| Monthly household income ≥ SGD5000 (Ref < SGD5000) | 0.82 | (0.55, 1.22) | 0.79 | (0.52, 1.19) | 0.90 | (0.47, 1.72) | 0.88 | (0.46, 1.67) |
| Classes | ||||||||
| Substance-naïve | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref |
| Substance-novice | 1.99 | (1.36, 2.92) | 2.24 | (1.51, 3.33) | 1.93 | (1.03, 3.61) | 2.01 | (1.05, 3.85) |
| Chemsex | 3.10 | (1.75, 5.49) | 3.28 | (1.85, 5.79) | 1.60 | (0.40, 6.39) | 1.64 | (0.42, 6.38) |
Notes
Abbreviations: CI Confidence Interval, PR Prevalence Ratio, aPR Adjusted Prevalence Ratio
Statistically significant (p < 0.05) are highlighted in bold font
Association between substance use class membership and mental health outcomes
Table 4 summarizes the associations between substance use class membership and mental health outcomes. At the bivariate level, increasing age was positively associated with ever contemplating suicide (PR = 0.96, 95%CI [0.93, 1.00]). Participants who were in the chemsex class (PR = 1.61, 95%CI [1.31, 1.99]) were more likely than substance-naive participants to have reported ever contemplating suicide. Increasing age (β = − 0.41, 95%CI [− 0.66, − 0.15]), being of Chinese ethnicity (β = − 1.92, 95%CI [− 3.43, − 0.40]), and identifying as a cisgender male (β = − 2.48, 95%CI [− 4.55, − 0.42]) were negatively associated with depression severity. Participants who were in the chemsex class were also more likely that those in the substance-naive class to have reported higher scores for depression severity (β = 3.51, 95%CI [0.66, 6.36]). All factors that were statistically significant at the bivariate level remain significant at the multivariable level. Increasing age was positively associated with ever contemplating suicide (aPR = 0.96, 95%CI [0.93, 0.99]). Participants who were in the chemsex class (aPR = 1.64, 95%CI [1.33, 2.03]) were more likely than substance-naive participants to have reported ever contemplating suicide. Increasing age (aβ = − 0.39, 95%CI [− 0.65, − 0.14]), being of Chinese ethnicity (aβ = − 1.86, 95%CI [− 3.37, − 0.34]), and identifying as a cisgender male (a β = − 2.13, 95%CI [− 4.22, − 0.04]) were negatively associated with depression severity. Participants who were in the chemsex class were also more likely that those in the substance-naive class to have reported higher scores for depression severity (aβ = 3.69, 95%CI [0.87, 6.51]).
Table 4.
Multivariable Poisson regression for mental health outcomes and its association with substance using classes
| Ever contemplated suicide (n = 308) | Depression severity | |||||||
|---|---|---|---|---|---|---|---|---|
| PR | 95% CI | aPR | 95% CI | β | 95% CI | aβ | 95% CI | |
| Age | 0.96 | (0.93, 1.00) | 0.96 | (0.93, 0.99) | −0.41 | (−0.66, −0.15) | −0.39 | (−0.65, −0.14) |
| Chinese ethnicity (Ref = Non-Chinese) | 0.87 | (0.72, 1.04) | 0.87 | (0.72, 1.04) | −1.92 | (−3.43, − 0.40) | −1.86 | (−3.37, − 0.34) |
| Cisgender male (Ref = Transgender, genderqueer, or others) | 0.89 | (0.69, 1.15) | 0.88 | (0.69, 1.14) | −2.48 | (−4.55, − 0.42) | −2.13 | (−4.22, − 0.04) |
| Gay (Ref = Bisexual, queer, or others) | 1.04 | (0.88, 1.24) | 1.06 | (0.89, 1.26) | −0.55 | (−1.7, − 0.69) | 0.04 | (− 1.22, 1.31) |
| Monthly household income ≥ SGD5000 (Ref < SGD5000) | 1.00 | (0.86, 1.18) | 1.02 | (0.87, 1.20) | 0.33 | (− 0.83, 1.50) | 0.69 | (− 0.48, 1.86) |
| Classes | ||||||||
| Substance-naïve | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref |
| Substance-novice | 1.12 | (0.94, 1.33) | 1.16 | (0.97, 1.38) | −0.52 | (−1.81, 0.78) | − 0.11 | (− 1.43, 1.21) |
| Chemsex | 1.61 | (1.31, 1.99) | 1.64 | (1.33, 2.03) | 3.51 | (0.66, 6.36) | 3.69 | (0.87, 6.51) |
Notes
Abbreviations: CI Confidence Interval, PR Prevalence Ratio, aPR Adjusted Prevalence Ratio, β Unadjusted Coefficient, aβ Adjusted Coefficient
Statistically significant (p < 0.05) are highlighted in bold font
Discussion
This study sought to identify classes of YMSM based on the substances that they had ever used in sexualized contexts. We explored the sociodemographic and substance use patterns across each of the different classes, and how these classes differed based on their associations with a variety of sexual and mental health outcomes, specifically recent unprotected anal sex with casual partners and STI diagnoses, as well as depression severity and ever contemplating suicide. This study is noteworthy in that, to our knowledge, no prior study has sought to delineate classes of substance use specifically in younger samples of MSM, which allows us to better understand the risk factors that may be associated with substance use initiation. Furthermore, no other study had ever sought to investigate such patterns of substance use among GBMSM in Singapore.
Results of latent class analysis revealed three classes of YMSM based on the substances that they had ever used in sexualized contexts, which we labelled post hoc as ‘substance-naive’, ‘substance novice’, and ‘chemsex’. Those in the substance-naive group had only ever used alcohol, while the substance-novice group were primarily poppers users with a small proportion who reported using drugs typically associated with chemsex, including meth, GHB/GBL, as well as erectile dysfunction drugs [13, 46]. The chemsex group comprised individuals who had mostly used such drugs. This finding aligns with that of other studies, which identified classes of GBMSM characterized by those who were negligible or non-users of recreational substances excluding alcohol, those who were ‘soft’ drug users, and those who were ‘hard’ drug or polydrug users [33]. Several studies have also found find greater nuances in such patterns of use, separating those who are polydrug users without meth or mephedrone, and those who do [14, 47].
Controlling for potential confounding variables, we found that being in the substance-novice or chemsex classes were associated with poorer sexual and mental health outcomes, compared to those who were in the substance-naive class. Given that those in the chemsex class reported both historical and recent indicators of poorer mental health, we believe that this may underpin certain mechanisms that lead to both sexual risk and substance use risk-related behaviors. This corroborates the findings of other studies [4, 48]. As we are not able to establish causation due to the study design, an alternative explanation would be that substance use itself may be a factor that may cause poorer mental health, and disinhibition associated with sexual risk-related behaviors, which corroborate the findings of other studies as well [49]. These two may mechanisms may also be working in tandem to exacerbate poorer sexual and mental health outcomes in the chemsex class, compared to the substance-naive class of YMSM. We remain mindful that we cannot draw a direct association between substance use and some of these outcomes as the time frame assessed for both differ.
Our study has several strengths. As it was conducted among self-identified HIV-negative YMSM aged 18 to 25 years old, we may be identifying certain risk factors and substance use patterns that may place them at risk of HIV and other STI acquisition. We may also draw conclusions around factors that may be associated with substance use initiation without stronger confounds of age, as GBMSM are more likely to be exposed to various substances throughout their life course due to its cumulative availability via sexual and social networks [50].
Our study has several limitations. First, we might expect that our study participants comprising HIV-negative GBMSM would report a lower prevalence of substance, given that measures of substance use have been positively associated with an HIV-positive status among GBMSM in past studies [51, 52]. As such, a similar study involving GBMSM living with HIV is warranted. Second, as HIV status was self-reported in this study, there may be misclassification of HIV-positive individuals as HIV-negative participants in our study. As past studies have shown that sexualized substance use is a risk factor for HIV acquisition [53, 54], such misclassification might have led to a higher prevalence of substance use in our sample than should be expected from a sample of HIV-negative GBMSM. Third, the implementation of a referral system to recruit study participants from existing members of the study cohort may have led to selection effects or referral bias. Unfortunately, no reference data on population level characteristics for GBMSM is Singapore are available for the construction of sample weights, and thus such bias could have led to either and underestimation or overestimation of the effects reported in this study. Fourth, drug use carries severe penalties in Singapore under the Misuse of Drugs Act, which criminalizes the possession and use of drugs with penalties that range from fines of up to S$20,000 to a maximum of 10 years in prison, and trafficking of drugs beyond stipulated thresholds with a mandatory death penalty or life imprisonment. As such, participants may not be entirely honest with their answers around drug use, which may have led to an underreporting of substance use in the present sample. This form of non-differential misclassification would have biased our results towards the null, when in fact the associations between substance use and the outcomes of interest would have been stronger.
We have several recommendations for health promotion and policy interventions. Overall, such health promotion efforts and interventions should acknowledge that substance use-related support needs among YMSM and GBMSM may be heterogenous, and would require a combination of upstream interventions that promote literacy around the risks associated with substance use, and downstream ones that mitigate such risks or promote the well-being of those who require long-term support. For example, policy changes and campaigns should focus on reducing homophobia towards GBMSM and YMSM to improve mental health outcomes, as well as reduce the demand for chemsex as a means of coping with such forms of stigma. Specifically, this may involve the decriminalization of same-sex sexual relations among GBMSM and the implementation of comprehensive sexuality education in schools.
Findings of this study indicate that efforts for early intervention and education for YMSM should focus on reducing the harms associated with engaging in chemsex. Specifically, interventions may be implemented to identify YMSM who may be at risk of the harms associated with chemsex or mental health comorbidities, based on either their substance use patterns or mental health risk, and engage them in holistic care. Engaging such YMSM would provide opportunities for harm reduction efforts around dealing with stigma and poor mental health, alongside HIV and other STIs acquisition as well. Public health communication and campaigns could also work to frame substance use among GBMSM and YMSM as mental health challenges, rather than criminalized and stigmatized behaviors, given its association with stigma and mental health comorbidities.
Supplementary Information
Additional file 1: Table S1. Summary goodness of fit statistics for class membership comparison.
Acknowledgements
The study team would like to thank all the participants who took part in the study. We would like to extend our sincerest thanks to Action for AIDS Singapore and the Pink Carpet Y Team for their collaboration on this project. We would like to extend our sincerest gratitude to all community-based organizations who have helped us in the recruitment of participants.
Abbreviations
- GBMSM
Gay, Bisexual and other Men who have Sex with Men
- YMSM
Young Men who have Sex with Men
- STI
Sexually Transmitted Infections
- GHB/GBL
Gamma-Hydroxybutyrate/Gamma-Butyrolactone
- AFA
Action for AIDS Singapore
- NUS
National University of Singapore
- SGD
Singapore Dollars
- GHB/GBL
Gamma Hydroxybutyrate and Gamma-Butyrolactone
- C
Coefficient
- PR
Prevalence Ratio
Authors’ contributions
RKJT, DL, SB and MLW conceptualized the study; MLW provided supervision for the study; RKJT and MLW acquired the funding for the study; CAO, WLK and RKJT conducted formal analyses; RKJT, DL, AT1, AT2, CT, CK and SB conducted the investigation and curated the data associated with the study; CAO, WLK and RKJT wrote the original draft; All co-authors have reviewed and approved of the manuscript prior to submission.
Funding
This research is supported by the Singapore Ministry of Health’s National Medical Research Council under the Seed Funding Programme by Singapore Population Health Improvement Centre (NMRC/CG/C026/2017_NUHS). The funder had no role in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
Ethics approval was provided by the National University of Singapore Institutional Review Board (Reference Code S-19-007). Participants provided written informed consent to participate.
Consent for publication
Not applicable.
Competing interests
RKJT is an associate editor with BMC Public Health. The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.UNAIDS. Global HIV & AIDS statistics — 2020 fact sheet 2020 [cited 2020 September 17]. Available from: https://www.unaids.org/en/resources/fact-sheet. Accessed 28 Apr 2021.
- 2.Beyrer C, Baral SD, van Griensven F, Goodreau SM, Chariyalertsak S, Wirtz AL, Brookmeyer R. Global epidemiology of HIV infection in men who have sex with men. Lancet. 2012;380(9839):367–377. doi: 10.1016/S0140-6736(12)60821-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Goodreau SM, Golden MR. Biological and demographic causes of high HIV and sexually transmitted disease prevalence in men who have sex with men. Sex Transm Infect. 2007;83(6):458–462. doi: 10.1136/sti.2007.025627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychol Bull. 2003;129(5):674–697. doi: 10.1037/0033-2909.129.5.674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Xu W, Zheng L, Xu Y, Zheng Y. Internalized homophobia, mental health, sexual behaviors, and outness of gay/bisexual men from Southwest China. Int J Equity Health. 2017;16(1):36. doi: 10.1186/s12939-017-0530-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Huebner DM, Davis MC, Nemeroff CJ, Aiken LS. The impact of internalized homophobia on HIV preventive interventions. Am J Community Psychol. 2002;30(3):327–348. doi: 10.1023/A:1015325303002. [DOI] [PubMed] [Google Scholar]
- 7.Pachankis JE, Hatzenbuehler ML, Hickson F, Weatherburn P, Berg RC, Marcus U, et al. Hidden from health: structural stigma, sexual orientation concealment, and HIV across 38 countries in the European MSM Internet Survey. AIDS (London, England) 2015;29(10):1239–1246. doi: 10.1097/QAD.0000000000000724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bourne A. Drug use among men who have sex with men. Implications for harm reduction. In: Stoicescu C, editor. Global State of Health Reduction 2012. London: Harm Reduction International; 2012. pp. 147–155. [Google Scholar]
- 9.McCabe SE, Hughes TL, Bostwick WB, West BT, Boyd CJ. Sexual orientation, substance use behaviors and substance dependence in the United States. Addiction (Abingdon, England) 2009;104(8):1333–1345. doi: 10.1111/j.1360-0443.2009.02596.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hunter LJ, Dargan PI, Benzie A, White JA, Wood DM. Recreational drug use in men who have sex with men (MSM) attending UK sexual health services is significantly higher than in non-MSM. Postgrad Med J. 2014;90(1061):133–138. doi: 10.1136/postgradmedj-2012-131428. [DOI] [PubMed] [Google Scholar]
- 11.Bourne A, Reid D, Hickson F, Torres-Rueda S, Weatherburn P. Illicit drug use in sexual settings (‘chemsex’) and HIV/STI transmission risk behaviour among gay men in South London: findings from a qualitative study. Sex Transm Infect. 2015;91(8):564–568. doi: 10.1136/sextrans-2015-052052. [DOI] [PubMed] [Google Scholar]
- 12.Race K. ‘Party and play’: online hook-up devices and the emergence of PNP practices among gay men. Sexualities. 2015;18(3):253–275. doi: 10.1177/1363460714550913. [DOI] [Google Scholar]
- 13.Tan RKJ, Wong CM, Chen MIC, Chan YY, Bin Ibrahim MA, Lim OZ, Chio MTW, Wong CS, Chan RKW, Chua LJ, Choong BCH. Chemsex among gay, bisexual, and other men who have sex with men in Singapore and the challenges ahead: a qualitative study. Int J Drug Policy. 2018;61:31–37. doi: 10.1016/j.drugpo.2018.10.002. [DOI] [PubMed] [Google Scholar]
- 14.Achterbergh RCA, de Vries HJC, Boyd A, Davidovich U, Drückler S, Hoornenborg E, et al. Identification and characterization of latent classes based on drug use among men who have sex with men at risk of sexually transmitted infections in Amsterdam, the Netherlands. Addiction. 2020;115(1):121–133. doi: 10.1111/add.14774. [DOI] [PubMed] [Google Scholar]
- 15.Bourne A, Weatherburn P. Substance use among men who have sex with men: patterns, motivations, impacts and intervention development need. Sex Transm Infect. 2017;93(5):342–346. doi: 10.1136/sextrans-2016-052674. [DOI] [PubMed] [Google Scholar]
- 16.Sewell J, Cambiano V, Speakman A, Lampe FC, Phillips A, Stuart D, Gilson R, Asboe D, Nwokolo N, Clarke A, Rodger AJ. Changes in chemsex and sexual behaviour over time, among a cohort of MSM in London and Brighton: findings from the AURAH2 study. Int J Drug Policy. 2019;68:54–61. doi: 10.1016/j.drugpo.2019.03.021. [DOI] [PubMed] [Google Scholar]
- 17.Berg RC, Amundsen E, Haugstvedt Å. Links between chemsex and reduced mental health among Norwegian MSM and other men: results from a cross-sectional clinic survey. BMC Public Health. 2020;20(1):1785. doi: 10.1186/s12889-020-09916-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stall R, Paul JP, Greenwood G, Pollack LM, Bein E, Crosby GM, et al. Alcohol use, drug use and alcohol-related problems among men who have sex with men: the Urban Men's Health Study. Addiction. 2001;96(11):1589–1601. doi: 10.1046/j.1360-0443.2001.961115896.x. [DOI] [PubMed] [Google Scholar]
- 19.Lea T, Ryan D, Prestage G, Zablotska I, Mao L, de Wit J, et al. Alcohol use among a community-based sample of gay men: Correlates of high-risk use and implications for service provision. Drug Alcohol Rev. 2015;34(4):349–357. doi: 10.1111/dar.12234. [DOI] [PubMed] [Google Scholar]
- 20.Corliss HL, Rosario M, Wypij D, Fisher LB, Austin SB. Sexual orientation disparities in longitudinal alcohol use patterns among adolescents: findings from the growing up today study. Arch Pediatr Adolesc Med. 2008;162(11):1071–1078. doi: 10.1001/archpedi.162.11.1071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Garofalo R, Wolf RC, Kessel S, Palfrey J, DuRant RH. The association between health risk behaviors and sexual orientation among a school-based sample of adolescents. Pediatrics. 1998;101(5):895–902. doi: 10.1542/peds.101.5.895. [DOI] [PubMed] [Google Scholar]
- 22.Grosso AL, Downing MJ, Thomann M, Chiasson MA, Schrimshaw EW, Hirshfield S. Age of onset of alcohol consumption and subsequent negative health outcomes in gay and bisexual men who have sex with men. J Homosex. 2019;66(11):1609–1625. doi: 10.1080/00918369.2018.1505757. [DOI] [PubMed] [Google Scholar]
- 23.Washington TA, Patel SN, Meyer-Adams N. Drinking patterns and HIV risk behaviors among black and latino men who have sex within los angeles county. Am J Mens Health. 2017;11(4):834–844. doi: 10.1177/1557988315605894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Li J, McDaid LM. Alcohol and drug use during unprotected anal intercourse among gay and bisexual men in Scotland: what are the implications for HIV prevention? SexTransm Infect. 2014;90(2):125–132. doi: 10.1136/sextrans-2013-051195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bolton R, Vincke J, Mak R, Dennehy E. Alcohol and risky sex: in search of an elusive connection. Med Anthropol. 1992;14(2–4):323–363. doi: 10.1080/01459740.1992.9966077. [DOI] [PubMed] [Google Scholar]
- 26.Qi J, Zhang D, Fu X, Li C, Meng S, Dai M, Liu H, Sun J. High risks of HIV transmission for men who have sex with men — a comparison of risk factors of HIV infection among MSM associated with recruitment channels in 15 cities of China. PLoS One. 2015;10(4):e0121267. doi: 10.1371/journal.pone.0121267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Singh S, Song R, Johnson AS, McCray E, Hall HI. HIV incidence, prevalence, and undiagnosed infections in U.S. men who have sex with MenEstimated HIV incidence, HIV prevalence, and undiagnosed HIV infections. Ann Intern Med. 2018;168(10):685–694. doi: 10.7326/M17-2082. [DOI] [PubMed] [Google Scholar]
- 28.Freeman P, Walker BC, Harris DR, Garofalo R, Willard N, Ellen JM, Adolescent Trials Network for HIV/AIDS Interventions 016b Team Methamphetamine use and risk for HIV among young men who have sex with men in 8 US cities. Arch Pediatr Adolesc Med. 2011;165(8):736–740. doi: 10.1001/archpediatrics.2011.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Clatts MC, Goldsamt LA, Yi H. Club drug use among young men who have sex with men in NYC: a preliminary epidemiological profile. Substance Use Misuse. 2005;40(9–10):1317–1330. doi: 10.1081/JA-200066898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kecojevic A, Silva K, Sell RL, Lankenau SE. Prescription drug misuse and sexual risk behaviors among young men who have sex with men (YMSM) in Philadelphia. AIDS Behav. 2015;19(5):847–856. doi: 10.1007/s10461-014-0898-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gamarel KE, Brown L, Kahler CW, Fernandez MI, Bruce D, Nichols S, Adolescent Medicine Trials Network for HIV/AIDS Intervention Prevalence and correlates of substance use among youth living with HIV in clinical settings. Drug Alcohol Depend. 2016;169:11–18. doi: 10.1016/j.drugalcdep.2016.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.RKJ T, O’Hara CA, Koh WL, Le D, Tan A, Tyler A, et al. Social capital and chemsex initiation in young gay, bisexual, and other men who have sex with men: the pink carpet Y cohort study. Subst Abuse Treat Prev Policy. 2021;16(1):18. doi: 10.1186/s13011-021-00353-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lim SH, Cheung DH, Guadamuz TE, Wei C, Koe S, Altice FL. Latent class analysis of substance use among men who have sex with men in Malaysia: findings from the Asian internet MSM sex survey. Drug Alcohol Depend. 2015;151:31–37. doi: 10.1016/j.drugalcdep.2015.02.040. [DOI] [PubMed] [Google Scholar]
- 34.Ministry of Health Singapore . Update on the HIV/AIDS Situation in Singapore 2019 (June 2020) 2020. [Google Scholar]
- 35.Chua LJ, Su D, Tan RKJ, Jie KW. Decriminalisation of same-sex relations and social attitudes: an empirical study of Singapore. Hong Kong Law J. 2017;47(3):793–824. [Google Scholar]
- 36.Mathews M, Lim L, Selvarajan S. Religion, morality and conservatism in Singapore. Singapore: Institute of Policy Studies; 2019. [Google Scholar]
- 37.Tan R, Kaur N, Kumar PA, Tay E, Leong A, Chen MI, Wong CS. Clinics as spaces of costly disclosure: HIV/STI testing and anticipated stigma among gay, bisexual and queer men. Cult Health Sex. 2020;22(3):307–20. 10.1080/13691058.2019.1596313. [DOI] [PubMed]
- 38.Tan RKJ, Teo AKJ, Kaur N, Harrison-Quintana J, Chen MI-C, Wong CS. Extent and selectivity of sexual orientation disclosure and its association with HIV and other STI testing patterns among gay, bisexual, and other men who have sex with men. Sex Transm Infect. 2019;95(4):273–278. doi: 10.1136/sextrans-2018-053866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tan R. Internalized homophobia, HIV knowledge, and HIV/AIDS personal responsibility beliefs: correlates of HIV/AIDS discrimination among MSM in the context of institutionalized stigma. J Homosex. 2019;66(8):1082–22. 10.1080/00918369.2018.1491249. [DOI] [PubMed]
- 40.Kher C, Shing L. Saying no: sections 377 and 377A of the Penal Code. Singap J Leg Stud. 2003:209–61. Retrieved May 27, 2021, from http://www.jstor.org/stable/24868200.
- 41.Action for AIDS Singapore. Community Blueprint to End HIV & AIDS. Singapore: Action for AIDS Singapore; 2019.
- 42.Teo AKJ, Prem K, Chen MIC, Roellin A, Wong ML, La HH, et al. Estimating the size of key populations for HIV in Singapore using the network scale-up method. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ong C, Tan RKJ, Le D, Tan A, Tyler A, Tan C, et al. Association between sexual orientation acceptance and suicidal ideation, substance use, and internalised homophobia amongst the Pink Carpet Y Cohort Study of young gay, bisexual, and queer men in Singapore. BMC Public Health. 2021;21(1):971. doi: 10.1186/s12889-021-10992-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Spitzer RL, Kroenke K, Williams JBW, Group atPHQPCS Validation and utility of a self-report version of PRIME-MDThe PHQ primary care study. JAMA. 1999;282(18):1737–1744. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- 46.Bourne A, Reid D, Hickson F, Torres Rueda S, Weatherburn P. The Chemsex study: drug use in sexual settings among gay and bisexual men in Lambeth, Southwark and Lewisham. 2014. [Google Scholar]
- 47.McCarty-Caplan D, Jantz I, Swartz J. MSM and drug use: a latent class analysis of drug use and related sexual risk behaviors. AIDS Behav. 2014;18(7):1339–1351. doi: 10.1007/s10461-013-0622-x. [DOI] [PubMed] [Google Scholar]
- 48.Sewell J, Cambiano V, Miltz A, Speakman A, Lampe FC, Phillips A, Stuart D, Gilson R, Asboe D, Nwokolo N, Clarke A, Hart G, Rodger A. Changes in recreational drug use, drug use associated with chemsex, and HIV-related behaviours, among HIV-negative men who have sex with men in London and Brighton, 2013–2016. Sex Transm Infect. 2018;94(7):494–501. doi: 10.1136/sextrans-2017-053439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Javanbakht M, Shoptaw S, Ragsdale A, Brookmeyer R, Bolan R, Gorbach PM. Depressive symptoms and substance use: changes overtime among a cohort of HIV-positive and HIV-negative MSM. Drug Alcohol Depend. 2020;207:107770. doi: 10.1016/j.drugalcdep.2019.107770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Holloway IW. Substance use homophily among geosocial networking application using gay, bisexual, and other men who have sex with men. Arch Sex Behav. 2015;44(7):1799–1811. doi: 10.1007/s10508-015-0581-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Semple SJ, Strathdee SA, Zians J, Patterson TL. Factors associated with experiences of stigma in a sample of HIV-positive, methamphetamine-using men who have sex with men. Drug Alcohol Depend. 2012;125(1–2):154–159. doi: 10.1016/j.drugalcdep.2012.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Lewis LA, Ross MW. The gay dance party culture in Sydney. J Homosex. 1995;29(1):41–70. doi: 10.1300/J082v29n01_03. [DOI] [PubMed] [Google Scholar]
- 53.Carey JW, Mejia R, Bingham T, Ciesielski C, Gelaude D, Herbst JH, et al. Drug use, high-risk sex behaviors, and increased risk for recent HIV infection among men who have sex with men in Chicago and Los Angeles. AIDS Behav. 2008;13(6):1084. doi: 10.1007/s10461-008-9403-3. [DOI] [PubMed] [Google Scholar]
- 54.Colfax G, Coates TJ, Husnik MJ, Huang Y, Buchbinder S, Koblin B, Chesney M, Vittinghoff E, EXPLORE Study Team Longitudinal patterns of methamphetamine, popper (amyl nitrite), and cocaine use and high-risk sexual behavior among a cohort of San Francisco men who have sex with men. J Urban Health. 2005;82(1 Suppl 1):i62–i70. doi: 10.1093/jurban/jti025. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Table S1. Summary goodness of fit statistics for class membership comparison.
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.