Significance
As jails and prisons remain leading sites of COVID-19 outbreaks, mass incarceration poses ongoing health risks for communities. We investigate whether short-term jailing of individuals prior to release may drive COVID-19 spread. We find that cycling individuals through Cook County Jail in March 2020 alone can account for 13% of all COVID-19 cases and 21% of racial COVID-19 disparities in Chicago as of early August. We conclude that detention for alleged offenses that can be safely managed without incarceration is likely harming public safety and driving racial health disparities. These findings reinforce consensus among public health experts that large-scale decarceration should be implemented to protect incarcerated people, mitigate disease spread and racial disparities, and improve biosecurity and pandemic preparedness.
Keywords: carceral-community epidemiology, racial disparities, inequality, public health, mass incarceration
Abstract
Black and Hispanic communities are disproportionately affected by both incarceration and COVID-19. The epidemiological relationship between carceral facilities and community health during the COVID-19 pandemic, however, remains largely unexamined. Using data from Cook County Jail, we examine temporal patterns in the relationship between jail cycling (i.e., arrest and processing of individuals through jails before release) and community cases of COVID-19 in Chicago ZIP codes. We use multivariate regression analyses and a machine-learning tool, elastic regression, with 1,706 demographic control variables. We find that for each arrested individual cycled through Cook County Jail in March 2020, five additional cases of COVID-19 in their ZIP code of residence are independently attributable to the jail as of August. A total 86% of this additional disease burden is borne by majority-Black and/or -Hispanic ZIPs, accounting for 17% of cumulative COVID-19 cases in these ZIPs, 6% in majority-White ZIPs, and 13% across all ZIPs. Jail cycling in March alone can independently account for 21% of racial COVID-19 disparities in Chicago as of August 2020. Relative to all demographic variables in our analysis, jail cycling is the strongest predictor of COVID-19 rates, considerably exceeding poverty, race, and population density, for example. Arrest and incarceration policies appear to be increasing COVID-19 incidence in communities. Our data suggest that jails function as infectious disease multipliers and epidemiological pumps that are especially affecting marginalized communities. Given disproportionate policing and incarceration of racialized residents nationally, the criminal punishment system may explain a large proportion of racial COVID-19 disparities noted across the United States.
High rates of incarceration in crowded detention facilities have been documented as a significant population-level risk factor for the transmission of infectious diseases such as HIV, influenza, tuberculosis, viral hepatitis, and yet other diseases (1–11). Such facilities function as disease incubators, providing sites for easy viral and bacterial replication with a ready supply of tightly packed bodies that are rendered even more vulnerable by inadequate healthcare, poor living conditions, and associated comorbidities (12, 13). As a result, notably overcrowded prisons, jails, and immigrant detention facilities under a system of mass incarceration in the United States effectively constitute infectious disease multipliers (14–21). Given the daily inflow/outflow of staff and detainees, these disease reservoirs—cultivated through disregard for the welfare of incarcerated people — also function as epidemiological pumps that fuel continued disease penetrance in surrounding communities (22–26). We refer to this dynamic as “carceral-community epidemiology” to emphasize that health in carceral facilities is in continuous biosocial interrelation with community health, national public health, and global biosecurity.
During the COVID-19 pandemic, American jails and prisons have predictably emerged as the world’s leading sites of COVID-19 outbreaks. Prior to the resumption of the school year, carceral facilities constituted 90 of the top 100 clusters in the United States as of September 1, 2020 (27). As of March 2021, they featured more than 626,000 publicly documented cases––almost certainly a substantial undercount due to the absence of oversight to ensure adequate testing protocols, data accuracy, and public reporting (27, 28). This crisis was not unanticipated (19, 20, 29, 30). Amid long-standing political acceptance of mass incarceration in the United States, which houses nearly 25% of the world’s incarcerated people despite only representing 4.2% of the global population (31), early warnings from public health experts were followed by delayed and inadequate policy action to alter arrest and incarceration practices in response to pandemic conditions (21, 32) Furthermore, while US jail populations initially declined in late spring and summer months, they have since rebounded toward prepandemic levels, increasing by 10% in the final months of 2020 (33). In this context, it is notable that while a considerable amount of appropriate attention has focused on the risks to which incarcerated individuals are being subjected during COVID-19, comparatively little scientific, media, and policy attention has highlighted the risks that carceral epidemics pose not only to incarcerated people but also to the health of the public at large (34).
It is clear that COVID-19 spreads quickly within US prisons and jails (35), but ascertaining the degree to which cases manifesting in carceral institutions spread to surrounding communities requires more investigation. An early modeling study, which necessarily relied on various assumptions and estimated an eventual total toll of 200,000 deaths from COVID-19, suggested that up to 76,000 deaths in US communities could result from spillover of COVID-19 epidemics in prisons and jails (36, 37). As the number of COVID-19 deaths in the United States now approaches 600,000, it appears likely that a large proportion of total COVID-19 deaths may ultimately be attributable to jail- and prison-linked spread of the novel coronavirus.
As of yet, only one peer-reviewed study has addressed carceral-community epidemiological ties during the COVID-19 pandemic with empirical data analysis based on real-world, rather than projected, dynamics. Controlling for race, poverty, public transit use, and population density, the study’s cross-sectional analysis showed a strong independent association between the arrest and cycling of individuals through Cook County Jail in Chicago before release and COVID-19 case rates in these individuals’ home ZIP codes in Illinois (38).
In addition to this preliminary finding, parallel racial disparities in the American criminal punishment system and COVID-19 cases also suggest a likely epidemiological link between COVID-19 outbreaks in carceral institutions and high case rates in highly policed Black and Hispanic communities (39). American policing and carceral practices disproportionately affect communities of color, who make up only 37% of the general population but 67% of the prison population (40). Communities subjected to high rates of poverty, which often overlap with racialized communities in the United States but also include poor White communities, are also disproportionately affected by policing and incarceration (41, 42) As has been widely noted, COVID-19 cases and deaths in the United States are, like arrest and incarceration, disproportionately affecting communities of color and communities in poverty (43–46). Despite these demographic overlaps and the questions they provoke, little research exists on the relationship between policing and/or incarceration policies and community rates of COVID-19.
The lack of research in this area owes in large part to inadequate data access, low data quality, and obstructive noncooperation from authorities overseeing jails, prisons, and immigration detention facilities (28). The collection and distribution of such data are often controlled, with little to no regulatory oversight, by county sheriffs and related officials whose positions depend upon electoral politics, both directly and indirectly. This may foster a prioritization of anticipated ramifications of negative media coverage rather than a prioritization of effective public health action and facilitation of necessary research (47).
The hazards of this system were confirmed, for example, in an August 2020 Supreme Court case, in which documents revealed that the Orange County Jail deliberately misled a lower court. The dissenting opinion, written by Justices Sotomayor and Ginsberg, affirmed a lower court’s assessment that “the Jail was deliberately indifferent to the health and safety of its inmates.” Furthermore, they noted that “despite knowing the severe threat posed by COVID–19 and contrary to its own apparent policies, the Jail exposed its inmates to significant risks from a highly contagious and potentially deadly disease [… and] has misrepresented its actions to the District Court and failed to safeguard the health of the inmates in its care” (48). Amid widespread legal failures to protect public health, including the Supreme Court’s majority opinion in this case, such abuses and misrepresentations by jail and prison administrators remain difficult to detect, document, and prevent. In this context, recent bicameral legislative efforts in Congress that attempt to force greater data transparency are important for collecting vital public health data and facilitating evidenced-based policymaking (49, 50). Currently proposed legislation does not, however, include adequate provisions to address the problem of data quality, possible data manipulation and misrepresentation, and the associated need for independent oversight to ensure proper COVID-19 testing protocols, accurate data collection, and publicly accessible data infrastructure.
In this setting of minimal high-quality data access and correspondingly few peer-reviewed studies, researchers have suspected that the constant circulation of staff and detainees between jails and communities—a weekly flow of 200,000 jail detainees (51) alongside daily movement of over 420,000 jail and prison guards (52)—poses considerable risk for the broader transmission of COVID-19 in communities. Although prisons, which house those who have been convicted of crimes and are serving sentences typically longer than one year, are also porous institutions in constant biosocial interrelation with surrounding communities, the degree of daily inflow/outflow of jails is notably higher. While prisons release ∼600,000 people annually, jails cycle through nearly 11 million admissions each year (41, 53). It is also important to note that jails primarily house pretrial detainees who have not been convicted of a crime and most of whom remain in jails for only a matter of hours, days, or weeks before being released to their communities. Pretrial detainees make up 74% of the typical daily population in US jails (and 43% of this daily population is comprised of Black individuals, who constitute only 13% of the overall national population) alongside a minority of jail detainees who have been convicted of low-level offenses and are serving sentences of less than one year (41). Highly dynamic jail populations with constant flow of new immunologically naïve individuals suggests that jails are an especially important nexus for spread of COVID-19 in US communities.
Against this backdrop, this study improves upon our previously published cross-sectional analysis of the relationship between incarceration and community spread of COVID-19 (38). With new access to longitudinal COVID-19 data that corresponds with jail release data at the ZIP code level, we are able to further characterize our previous study’s observed correlation between jail cycling and COVID-19 case rates in Illinois ZIP codes by including analyses over time to better inform an evaluation of possible causal relationships between jail cycling and COVID-19 spread in surrounding communities. We also more closely analyze the relationship between jail-linked coronavirus spread and racial health inequities as a mechanism of structural racism (39, 54). Our previous study’s single cross-sectional analysis added preliminary quantitative evidence to anecdotal observations, but it could not assess temporal patterns, the plausibility of reverse causality (i.e., that higher preexisting COVID-19 case rates in ZIP codes with high rates of jail cycling––not jail cycling itself––account for the observed relationship), nor the longer-term epidemiological dynamics associated with jail cycling. We now use repeated cross-sectional analyses to examine temporal dynamics in the relationship between jail cycling and community COVID-19 spread.
Data and Methods
We correlate jail cycling and community COVID-19 rates at the ZIP code level using booking, release, and COVID-19 data obtained via a Freedom of Information Act request fulfilled by Cook County Jail and COVID-19 data reported by the City of Chicago (55). Our analysis is restricted to Chicago ZIP codes rather than all Illinois ZIP codes as in our prior analysis (38), due to lack of access to longitudinal COVID-19 data for the entire state at the ZIP code level. To further evaluate and build upon prior preliminary findings, we again focus on jail releases in March 2020 and the same likely confounding demographic variables previously included. We draw data for our controls from the 2018 American Community Survey (ACS) 5 y estimates (56).
Replicating our prior primary specifications, we ran repeated cross-sectional multivariate regressions between the weekly COVID-19 case rate and cumulative case rate from March 1 to August 8 together with the following control variables by ZIP code: jail detainees released in March per capita, proportion of Black residents, proportion of Hispanic residents, poverty rate, public transit utilization rate, population density, and cumulative COVID-19 case rates as of the week beginning on March 29. Notably, these specifications include the addition of two more variables to those included in our prior study: proportion of Hispanic residents and COVID-19 case rates as of the week beginning on March 29. These were selected in light of high rates of COVID-19 observed among Hispanic residents since the date of our earlier study and to control for already-extant COVID-19 infections that preceded the effects of March 2020 jail cycling.
In robustness checks, we implement an elastic regression using 1,706 variables from the 2018 ACS 5-Year Data—all the variables that have no missing values for Chicago ZIP codes. This machine-learning model reduces the size of coefficients to zero when they do not explain much variance, allowing the consideration of a wide range of potential confounding variables so as to address concerns of possible omitted variable bias (57–59). We also use principal components analysis (PCA), a technique for reducing dimensionality of datasets by creating uncorrelated variables that successively maximize variance and minimize information loss. We use PCA on all of the above variables from the ACS. We then run a multivariate regression that includes jail cycling and only the principal components selected by elastic regression. We also control for jail release rates in adjacent ZIP codes in a “donut” spatial analysis to consider possible spillover and diffusion effects and also for the testing rate in each ZIP code as perturbations of the main model.
Limitations.
Our prior study on the relationship between incarceration and community COVID-19 spread did not have access to longitudinal data with which to examine the plausibility of reverse causality as an account for the observed association between jail cycling and COVID-19 in communities. This study now includes such data and is thus better positioned to examine likely casual pathways. Nonetheless, while longitudinal data are helpful to ameliorate concerns of reverse causality, causality still cannot be definitively established without a randomized controlled trial, which, for logistical and ethical reasons, is not a possibility in this case.
As shown below, reverse causality does not appear to be driving the phenomena we observe in our results. Additionally, on this point, it is important to consider that the mechanism of reverse causality would not operate in a straightforward manner in relation to the community spread of COVID-19 attributable to jail cycling in any case. If there are more cases in communities subject to higher rates of arrest prior to any contribution to case rates from jail cycling, then upon arrest and jailing, detainees from these communities would pose a higher risk of inadvertently spreading COVID-19 in the densely populated processing and detention spaces of the jail. This increased exposure risk in the jail would, in turn, lead to yet more released individuals returning to already high-risk ZIP codes with potential to infect others. Incoming individuals who bring severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infections with them into the jail—the direction of flow posited by a theory of reverse causality—would thus nonetheless contribute to higher numbers of released detainees carrying SARS-CoV-2 with them back to their communities, which would in turn be subject to increased exposure in proportion to incarceration rates in a given community.
In such a scenario, the processing spaces involved in arrest, transportation, and jail booking would operate as a multiplier for incoming SARS-CoV-2 from the community, exacerbating existing infectious disease in highly policed communities that, in many cases, are also subject to increased SARS-CoV-2 risk for reasons associated with housing conditions, poverty, type of employment, healthcare access, transport options, and other structural determinants of health. This multiplying function of jail cycling opens what could be regarded as a second causal pathway that would be synergistic with the abovementioned possible “reverse causality” dynamic, ultimately resulting in augmented community spread of SARS-CoV-2 due to jail cycling. What might be characterized here as “forward” and “reverse” causality would thus function to compound one another.
In addition to our present study’s limits with respect to casual inference in the absence of randomization, we also cannot rule out omitted variables as possible contributors to the dynamic observed. However, to mitigate this concern, we control for several likely causal factors behind COVID-19 case rates by using demographic variables in our main specifications that have been shown to be associated with SARS-CoV-2 spread. We found these controls did not account for the association we observe between jail cycling and COVID-19. Additionally, if omitted variables associated with jail cycling are correlated with COVID-19, we might expect jail cycling to be equally correlated with COVID-19 for every week for which we have data. We found, however, that weekly COVID-19 case rates in March were not correlated with jail detainees released in March. This alleviates but does not altogether eliminate concerns regarding missing variables. To further address such concerns, we use elastic regression—a machine-learning tool that allows us to consider a broad range of potential confounding variables. For this robustness check, we use 1,706 variables in the 2018 5 y estimates from the ACS. As reported below in more detail, our results are robust to this measure and allow contextualization of the relative strength of association between jail cycling and community COVID-19 rates.
Notably, the associations we observe grow consistently in the weeks following the month of March, which alleviates possible concerns that statistical noise may be driving the associations we report.
An additional limitation follows from our lack of access to data on jail staff. It is likely that the large number of staff, who move in/out of jails on a daily basis, further contribute to jail-community spread of COVID-19. We have been unable to evaluate this dynamic here and suspect that the contribution of the jail to community spread is likely to be higher than captured by analysis of the cycling of arrested individuals alone.
There is another reason why our estimates may be underestimates of the true effects. To the extent that ZIP codes with high levels of jail cycling are affecting COVID-19 rates in neighboring ZIP codes with relatively lower levels of jail cycling, this would bias our estimates downward. We address this concern in a robustness check by calculating jail cycling in a “donut” (analyzing each ZIP code in relation to adjacent ZIP codes), which, when added as a control, increases the effect sizes of jail cycling (60). Ideally, the inclusion of a spatial network analysis would require a randomized controlled trial of peer ZIP codes to estimate peer spillover across ZIP codes (e.g., randomization of whether transportation networks facilitate connections between one peer ZIP code and another) (61). Because such data remains unavailable to us, we have elected to include our spatial analysis as a robustness check rather than incorporate it into the main specifications.
Another potential concern is that documented COVID-19 rates may be in part driven by differential testing rates across neighborhoods; we therefore control for testing rates. There remains the possibility, however, that testing rates are endogenous—that is, a higher or lower index of suspicion for COVID-19 spread in a given area, such as in disproportionately affected minoritized neighborhoods in Chicago, in turn drives changes in testing rates (62). For this reason, we include this control as a robustness check only.
In terms of generalizability, we have been limited to data from only the City of Chicago and a single county jail, Cook County Jail—the nation’s largest single-site jail and third largest jail system (63). Chicago is the third largest city in the United States, and Cook County is the second most populous county in the United States, which makes the activities we observe in this study relevant even if they are not representative of other cities and counties.
Results
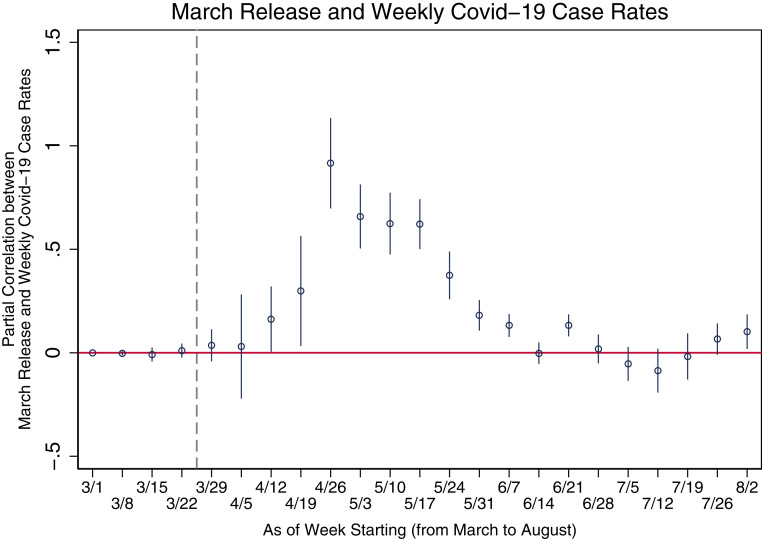
Table 1 provides details on the variables included in our analysis of ZIP codes in Chicago along with summary statistics. In repeated multivariate linear regressions, the significant positive associations with released detainees in March are significant at the 5% level for eight weeks after March (Fig. 1). More specifically, we find that March releases from Cook County Jail are not significantly correlated with COVID-19 case rates in Chicago by ZIP code until the week starting April 19. After that date, the significant positive association becomes largest the week starting April 26 and then gradually declines while remaining significant until the week starting June 14 (SI Appendix, Table S1). When evaluated in terms of cumulative case rates (rather than weekly), the growth in positive significant correlation on multivariate regression analysis continues to increase up to June 14 and remains roughly constant thereafter. These temporal characteristics of our findings suggest that reverse causality is not a likely explanation of the jail community epidemiological dynamic.
Table 1.
Summary statistics
| Mean | SD | |
| COVID case rates per capita in week starting Mar 1 | 0 | 0 |
| COVID case rates per capita in week starting Mar 15 | 0.0000173 | 0.0000457 |
| COVID case rates per capita in week starting Mar 8 | 0.0003007 | 0.0002134 |
| COVID case rates per capita in week starting Mar 22 | 0.0007786 | 0.0004753 |
| COVID case rates per capita in week starting Mar 29 | 0.0009782 | 0.0006099 |
| COVID case rates per capita in week starting Apr 5 | 0.0012338 | 0.000985 |
| COVID case rates per capita in week starting Apr 12 | 0.0013874 | 0.0008094 |
| COVID case rates per capita in week starting Apr 19 | 0.0019778 | 0.0013518 |
| COVID case rates per capita in week starting Apr 26 | 0.0021068 | 0.0017897 |
| COVID case rates per capita in week starting May 3 | 0.0018014 | 0.0013612 |
| COVID case rates per capita in week starting May 10 | 0.0016438 | 0.0012104 |
| COVID case rates per capita in week starting May 17 | 0.0014635 | 0.0010867 |
| COVID case rates per capita in week starting May 24 | 0.0009514 | 0.0007112 |
| COVID case rates per capita in week starting May 31 | 0.0005536 | 0.0003729 |
| COVID case rates per capita in week starting Jun 7 | 0.0004376 | 0.0002927 |
| COVID case rates per capita in week starting Jun 14 | 0.0004021 | 0.0002237 |
| COVID case rates per capita in week starting Jun 21 | 0.000491 | 0.0002194 |
| COVID case rates per capita in week starting Jun 28 | 0.0004883 | 0.0002349 |
| COVID case rates per capita in week starting Jul 5 | 0.0006455 | 0.0002758 |
| COVID case rates per capita in week starting Jul 12 | 0.0006296 | 0.0003715 |
| COVID case rates per capita in week starting Jul 19 | 0.0007078 | 0.0003792 |
| COVID case rates per capita in week starting Jul 26 | 0.00068 | 0.0003452 |
| COVID case rates per capita in seek starting Aug 2 | 0.0007172 | 0.0003691 |
| Cumulative COVID case rates per capita by Aug 2 | 0.0206492 | 0.0093657 |
| Cumulative COVID case rates per capita by Apr 4 | 1,628.979 | 879.4884 |
| Inmates released in March per capita | 0.0010966 | 0.0006232 |
| Poverty rate | 0.0008113 | 0.0010938 |
| Public transit utilization rate | 0.2389 | 0.1636867 |
| Proportion of Black residents | 0.2683241 | 0.1094167 |
| Proportion of Hispanic residents | 0.299919 | 0.3411399 |
| Population density | 0.2141293 | 0.2154392 |
| 16,001.39 | 9,375.842 |
Fig. 1.
Estimated relationships between SARS-CoV-2 case rates and detainees released per capita from multivariate regression analysis including controls––proportion of black residents, proportion of Hispanic residents, poverty rate, public transit utilization rate, population density, and cumulative SARS-CoV-2 case rates as of the week starting March 29. Source: authors’ analysis of data from Cook County Jail, City of Chicago (55), 2018 ACS (56). Whiskers present 95% CIs of the association between COVID-19 case rates and detainees released per capita from multivariate regression analyses.
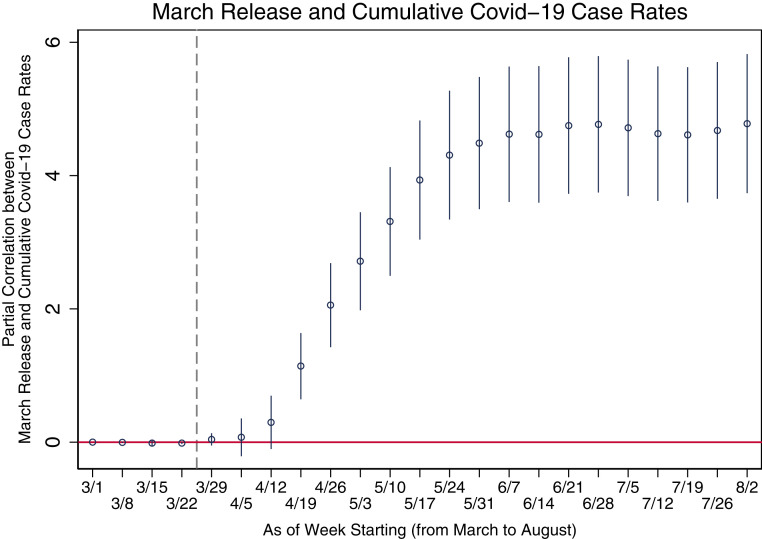
Fig. 2 shows the multiplier effect of detainees released in March on cumulative COVID-19 cases. The final bar indicates a COVID-19 multiplier effect of 4.78 per detainee cycled through the jail in March—that is, for each person cycled through the jail in March, nearly five additional cases are observed in their ZIP code of residence by the week of August 2. Rendered in population terms, our findings suggest that 8,468 (13%) of the total 64,080 cumulative COVID-19 cases documented in Chicago ZIP codes as of August 8 can be attributed to March jail cycling. We have arrived at this number by multiplying the jail detainees released in March per capita in each ZIP code by the coefficient (4.78) reported in the final bar of Fig. 2 (SI Appendix, Table S2) and then multiplying this number by population for each ZIP code.
Fig. 2.
Estimated relationships between cumulative SARS-CoV-2 case rates and detainees released per capita from multivariate regression analysis including controls––proportion of black residents, proportion of Hispanic residents, poverty rate, public transit utilization rate, population density, and cumulative SARS-CoV-2 case rates as of the week starting March 29. Source: authors’ analysis of data from Cook County Jail, City of Chicago (55), 2018 ACS (56). Whiskers present 95% CIs of the association between cumulative COVID-19 case rates and detainees released per capita from multivariate regression analyses.
When examining the distribution of COVID-19 cases attributable to March jail cycling in relation to the demographic characteristics of each ZIP code, 86% (7,303/8,468) of all additional cases appear in ZIP codes in which more than 50% of residents are Black and/or Hispanic while only 8.5% appear in majority-White ZIP codes. A total of 17% of all cases in Black and/or Hispanic-majority ZIP codes are attributable to March jail cycling, while only 6% of cumulative cases in White-majority ZIP codes are attributable to March jail cycling. This corresponds with broader racial disparities observed in our data. Notably, the average cumulative COVID-19 case rate in Black-/Hispanic-majority ZIP codes is 2.6% compared with 1.6% in all other ZIP codes (and 1.5% in White-majority ZIP codes). Furthermore, 44,246 (69%) of 64,080 total COVID-19 cases appear in majority-Black and -Hispanic ZIP codes. March jail cycling alone independently accounts for 21% of the racial disparity in COVID-19 cases across ZIP codes in Chicago, as inferred from ZIP code demographics and relative to an even distribution of case rates across all ZIP codes, as of August 8.
Poverty in Chicago ZIP codes is highly correlated with race; when considered alone, however, poverty is also strongly correlated with COVID-19 cases and particularly with COVID-19 cases attributable to jail cycling. While 45% of all COVID-19 cases as of August 8 appear in ZIP codes in which more than one-third of residents live in poverty, 74% of cases attributable to jail cycling appear in these same ZIP codes. The cumulative case rate in such high-poverty ZIP codes is 2.6% while it is 1.8% in all other ZIP codes.
To address concerns for omitted variable bias, we use an elastic regression model as a robustness check in which we include all 1,706 variables from the US Census and ACS—all those that had no missing values for Chicago ZIP codes. The detailed set of observables we have for this test include statistics on the demographic composition of the population rendered in percent terms for gender, age, household status, ethnicity (20+ categories), type of housing (e.g., residents per household; resident age ranges; multiunit buildings; and renter versus owner), child age range, employment (25+ categories), household income (10 categories), manner of transportation to work (8 categories), ancestry (100+ categories), foreign-born, education (10+ categories), and intersections of the aforementioned categories.
To aid interpretability, we first use PCA on all ACS variables. We then include only the principal components selected by elastic regression (SI Appendix, Table S3); this renders a multiplier effect of 4.4—a result slightly lower than in our main specifications. This assuages concerns for omitted variable bias. The data, while inadequate to definitively infer causality, indicate that arrest and subsequent jail cycling is a strong predictor of COVID-19 spread in Chicago ZIP codes.
When we control for March jail releases in adjacent ZIP codes, the COVID-19 multiplier effect per arrested individual cycled through the jail in March grows slightly to 4.8 (SI Appendix, Table S4), consistent with the hypothesis that incorporation of spatial network spillover effects produces effect sizes larger than the baseline estimates. This is because spillovers in our study context—in which “control” ZIP codes are contaminated by “treatment” ZIP codes—are likely to dampen the contrasts between ZIP codes with high and low release numbers. When we also control for the cumulative testing rate in each ZIP code, the coefficient is reduced to 4.0 (SI Appendix, Table S5), consistent with potential endogeneity of testing in the phenomena being studied.
Discussion and Conclusions
Our analysis of carceral-community epidemiology in Chicago indicates that for each arrested individual cycled through Cook County Jail in March 2020, approximately five additional cases of COVID-19 in their ZIP code of residence are independently attributable to jail cycling as of August 8. A total of 86% of this additional disease burden is borne by Black and/or Hispanic-majority ZIP codes, accounting for 17% of cumulative COVID-19 cases in these ZIP codes, 6% in White-majority ZIP codes, and 13% across all Chicago ZIP codes. Jail cycling in March 2020 alone can independently account for 21% of racial disparities in COVID-19 in Chicago as of August 8. Additionally, jail cycling remains by far the strongest predictor of COVID-19 rates when controlling for all other demographic variables, including poverty, racial demographics, education, and population density. These findings suggest that arrest and incarceration policies are substantially increasing COVID-19 incidence in communities, with especially severe consequences for marginalized communities of color.
Our data suggest that the cycling of individuals through Cook County Jail in March 2020 effectively functioned to seed the virus in disproportionately criminalized Black and Hispanic communities early in the COVID-19 pandemic at a time when relatively few cases had yet been documented in Chicago. This appears to have provided an initial epidemiological stimulus behind uneven racial distribution of COVID-19, driving inequalities that have subsequently compounded over time as jail cycling has continued to pump SARS-CoV-2 into marginalized communities while the virus has simultaneously most quickly multiplied in the very same areas due to the synergistic consequences of health, workplace, housing, and economic vulnerabilities accumulated through long-standing structural racism (55, 64).
These findings already indicate the serious consequences of carceral-community epidemiology, but it is important to note that they reflect only jail-linked SARS-CoV-2 spread associated with jail releases during the single month of March 2020. Additional research should evaluate the effects of subsequent months’ releases as well as those of jail staff’s daily circulation between the high-risk spaces of the jail and community contexts, which have almost certainly further added to the jail-linked burden of disease such that the cumulative proportion of cases and racial COVID-19 disparities attributable to jail cycling is likely considerably higher than demonstrated in this study.
As in Chicago, racial and class disparities in COVID-19 case rates and outcomes have been noted across the United States (65–67). Although it is clear that these disparities reflect structural racism and economic inequality, more closely examining mechanisms behind them is vital in order to guide effective health policy. Mutually reinforcing factors such as racial inequalities in housing conditions and security (68, 69), employment type and access to remote work options (70), minimal wealth and access to financial supports allowing for work stoppage and sick leave (71), school conditions, cumulative health disadvantages and comorbidities (72), and healthcare access and quality, among other considerations, are likely important drivers of observed COVID-19 inequities and broad health disparities (54). Although the US systems of policing and mass incarceration are also widely recognized as key vehicles of structural racism (64), there has been little evidence available with which to evaluate their role in the generation of disproportionately high COVID-19 case and death rates observed in many Black and Hispanic communities (39, 44, 73, 74).
As researchers have struggled to obtain data on carceral conditions while COVID-19 has spread throughout the United States, widespread protests following George Floyd’s murder have intensified public attention to structural racism in policing and incarceration practices. Our findings show that racial disparities in COVID-19 and criminal punishment directly intersect with one another. The racially uneven incidence of COVID-19 is inseparable from disproportionately high rates of arrest and incarceration in communities of color. For example, in Chicago, 89% of the more than 100,000 individuals cycled through Cook County Jail each year are Black or Hispanic (63, 75). Although data access has limited our analysis to Chicago, given the disparities in criminal punishment and COVID-19 nationally, the health consequences of high rates of arrest and incarceration appear likely to be similar in many other jurisdictions across the nation. COVID-19 is making visible in a new way the long-standing harms—including trauma and psychiatric sequelae (76, 77), family separation (76), long-term economic disadvantage (77–80), infectious disease risk (2, 3, 7), and death (81)—that American policing and mass incarceration policies have inflicted on marginalized communities for decades but that are often difficult to trace and quantify (22, 82–85).
The harmful effects of high rates of arrest and jail cycling arise from preventable conditions that evidence shows can be effectively addressed by implementing changes to policing and incarceration policies to protect public health and improve the safety of all (22, 32, 86–89). Decarceration efforts in the summer months of 2020 in response to COVID-19 temporarily reduced jail populations in some jurisdictions, although jail populations have since begun to return back to prepandemic levels (22, 33, 34, 90, 91). Notably, these early decarceration measures, which reduced jail populations by over 30% in many jurisdictions, have not resulted in higher rearrest rates (86). This is consistent with long-standing evidence that mass incarceration is neither an effective means of criminal deterrence nor of improving public safety and that the United States continues to incarcerate well past the point of diminishing returns for deterrent effects (86, 92–97).
To mitigate jail-linked COVID-19 spread, decarceration should be enacted through multiple mechanisms (21). Early release and lowering overnight jail populations alone does not address the front-end problem of unnecessarily high rates of arrest that continue to subject large numbers of detainees to transit through detention facilities before release back to their communities (14, 98). Infections acquired during this high-risk arrest and processing period will not be detected on testing at time of booking due to the incubation period required following exposure before the SARS-CoV-2infection will appear upon testing. Many of those booked into jails are released before such newly acquired infections would appear on testing even if adequate testing regimens are in place, which, in most facilities, is still not the case. For this reason, decarceration policies must include both front-end diversion away from unnecessary jailing (e.g., via expanded use of citations, summonses, home monitoring, etc.) as well as large-scale releases (21).
Changes to arrest and incarceration policies are not only needed to protect public health during COVID-19 but are also compatible with—even necessary for—protecting public welfare and safety (21). A large majority of the nearly 11 million annual jail admissions in the United States, including in Chicago, do not serve public safety interest and are closely associated with poverty and public underinvestment in communities (53, 99). Nationally, 74% of individuals held in city and county jails are pretrial detainees; many of these individuals remain jailed because of poverty and an associated inability to pay bail, even as most bails are set at amounts less than $10,000 (the median for felony charges) and very often, as in cases of misdemeanors charges, far less (100). Less than 5% of arrests are for serious violent offenses, and the vast majority are for petty alleged crimes associated with poverty and homelessness (101). Nearly 50% of those who are arrested multiple times in a year have incomes below $10,000 (102). In a major study of two of the largest county jails in the United States, 42% of those jailed were not convicted of any charges for which they were detained (78). For at least 39% of those in US prisons, there is no public safety justification for their incarceration (87). This figure is considerably higher in jails in which, unlike in prisons, three quarters of detainees have not yet been convicted of a criminal charge, and the quarter who have are serving short sentences for minor offenses that typically present no ongoing risk to public safety (41). Now, during a pandemic, not only does the excessive investment in punishment that underwrites this American justice system not serve public safety, but it also appears to be inflicting large-scale morbidity and mortality upon the public at large.
As more infectious SARS-CoV-2 variants continue to emerge and become dominant in the United States, large-scale decarceration remains urgently needed to protect public health. While many have anticipated that the arrival of vaccines would obviate the need for substantive policy action to address the public health catastrophe transpiring in and through jails and prisons, vaccines will not be sufficient to solve the ongoing problem. For epidemiological reasons explained at length elsewhere (103), SARS-CoV-2 outbreaks inside carceral facilities appear almost certain to continue to inflict preventable disease and death for the foreseeable future if not addressed with priority vaccination combined with large-scale decarceration. In brief, this is because very high rates of transmission, in combination with pronounced vaccine hesitancy in carceral contexts poorly equipped to earn the trust of incarcerated people (104), will substantially detract from the real-world effectiveness of vaccination, which depends heavily upon the effective transmission rate shaping the context of vaccine use (105).
Fortunately, decarceration has been demonstrated to be extremely effective at reducing transmission rates in US carceral contexts, which feature the highest documented reproduction ratios of any context in the world (35). Using data from a large urban jail, researchers found that decarceration measures, paired with basic Centers for Disease Control and Prevention guideline compliance (e.g., testing, limited visitation), were strikingly effective in achieving reductions in viral transmission: a 9% reduction in the carceral population was associated with a 56% decrease in transmission (14). Further depopulation, ultimately reaching a population decrease of 25%, was associated with ongoing reductions in transmission (14). This study’s conclusion that decarceration should be “a primary strategy for COVID-19 mitigation in jails” is shared by a consensus policy report by The National Academies of Science, Engineering, and Medicine and was further buttressed by a recent study of transmission dynamics in Texas prisons (21, 90). Evidence-based policy should insist that priority vaccination of incarcerated people be paired with large-scale decarceration in order to maximize vaccination effectiveness, disrupt the high risk for the development of new SARS-CoV-2 variants posed by current carceral conditions, and break viral transmission chains extending well beyond carceral facilities (103).
Our findings show that the community spread of COVID-19 as a result of the US criminal punishment system is most affecting economically marginalized communities of color, but the reality of carceral-community epidemiology in the context of a highly infectious respiratory virus means that public health harms due to incarceration are also disseminating into America’s wealthiest communities. Biological networks are such that even distant, segregated bodies are entwined by communicable diseases. This biosocial reality at the intersection of criminal punishment, structural racism, and public health dictates that it is in the interest of all, regardless of socioeconomic position or political commitments, to curtail high rates of arrest and incarceration. To guard public health against COVID-19, future epidemics of novel pathogens, and already well-known infectious diseases like influenza, HIV, and viral hepatitis, large-scale changes to the current system of policing and mass incarceration should be implemented immediately and sustained permanently.
Supplementary Material
Acknowledgments
We thank Viknesh Nagarathinam for his assistance in this research. We also thank Monica Peek and Salmaan Keshavjee for their support. D.L.C. acknowledges support from American Friends of Toulouse Schools of Economics, Toulouse School of Economics, and Institute for Advanced Study in Toulouse, including from the French National Research Agency under the Investments for the Future program (ANR-17-EUR-0010). E.R. acknowledges support from the Bucksbaum Institute for Clinical Excellence at The University of Chicago.
Footnotes
The authors declare no competing interest.
This article is a PNAS Direct Submission.
This article contains supporting information online at https://www.pnas.org/lookup/suppl/doi:10.1073/pnas.2026577118/-/DCSupplemental.
Data Availability
Anonymized jail cycling data by ZIP code (supplied by Freedom of Information Act Request fulfilled by Cook County Jail), COVID-19 case and testing data by ZIP code (already made public by City of Chicago), and all other variables (drawn from public US Census and ACS data) have been deposited in Harvard Dataverse along with code, processed data, and model outputs (https://doi.org/10.7910/DVN/NNBEGK) (106).
References
- 1.Dolan K., et al., Global burden of HIV, viral hepatitis, and tuberculosis in prisoners and detainees. Lancet 388, 1089–1102 (2016). [DOI] [PubMed] [Google Scholar]
- 2.Altice F. L., et al., The perfect storm: Incarceration and the high-risk environment perpetuating transmission of HIV, hepatitis C virus, and tuberculosis in Eastern Europe and central Asia. Lancet 388, 1228–1248 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kamarulzaman A., et al., Prevention of transmission of HIV, hepatitis B virus, hepatitis C virus, and tuberculosis in prisoners. Lancet 388, 1115–1126 (2016). [DOI] [PubMed] [Google Scholar]
- 4.Braun M. M., et al., Increasing incidence of tuberculosis in a prison inmate population. Association with HIV infection. JAMA 261, 393–397 (1989). [PubMed] [Google Scholar]
- 5.Dolan K., Kite B., Black E., Aceijas C., Stimson G. V.; Reference Group on HIV/AIDS Prevention and Care among Injecting Drug Users in Developing and Transitional Countries , HIV in prison in low-income and middle-income countries. Lancet Infect. Dis. 7, 32–41 (2007). [DOI] [PubMed] [Google Scholar]
- 6.Gough E., et al., HIV and hepatitis B and C incidence rates in US correctional populations and high risk groups: A systematic review and meta-analysis. BMC Public Health 10, 777 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Maruschak L. M., Sabol W. J., Potter R. H., Reid L. C., Cramer E. W., Pandemic influenza and jail facilities and populations. Am. J. Public Health 99 (suppl. 2), S339–S344 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bick J. A., Infection control in jails and prisons. Clin. Infect. Dis. 45, 1047–1055 (2007). [DOI] [PubMed] [Google Scholar]
- 9.Hawks L., Woolhandler S., McCormick D., COVID-19 in prisons and jails in the United States. JAMA Intern. Med. 180, 1041–1042 (2020). [DOI] [PubMed] [Google Scholar]
- 10.Stanley L. L., Public health reports (1896-1970): Influenza at San Quentin Prison, California. Vol 43 (1919). https://www.jstor.org/stable/4575142?seq=1#metadata_info_tab_contents. Accessed 24 August 2020.
- 11.Sequera V. G., et al., Increased incarceration rates drive growing tuberculosis burden in prisons and jeopardize overall tuberculosis control in Paraguay. Sci. Rep. 10, 21247 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Maruschak L. M., Berzofsky M., Unangst J., Medical problems of state and federal prisoners and jail inmates, 2011-12. Bureau of Justice Statistics, February 2015. https://www.bjs.gov/content/pub/pdf/mpsfpji1112.pdf. Accessed 24 August 2020.
- 13.Trusts Pew Charitable. Prison Health Care: Costs and Quality. Pew Charitable Trusts, October 2017. https://www.pewtrusts.org/-/media/assets/2017/10/sfh_prison_health_care_costs_and_quality_final.pdf?la=en&hash=C3120E4248708AB27435866F5EEC12AE24F63DFE. Accessed 1 May 2021.
- 14.Malloy G. S., Puglisi L., Brandeau M. L., Harvey T. D., Wang E. A., The effectiveness of interventions to reduce COVID-19 transmission in a large urban jail. MedRxiv [Preprint] (2020). 10.1101/2020.06.16.20133280 (Accessed 18 June 2020).
- 15.Shrage L., African Americans, HIV, and mass incarceration. Lancet 388, e2–e3 (2016). [DOI] [PubMed] [Google Scholar]
- 16.Heard C., Towards a health-informed approach to penal reform? Evidence from ten countries. Institute for Criminal Policy Research June 2019. https://www.prisonstudies.org/sites/default/files/resources/downloads/icpr_prison_health_report.pdf. Accessed 24 August 2020.
- 17.Wurcel A. G., et al., Spotlight on jails: COVID-19 mitigation policies needed now. Clin. Infect. Dis. 71, 891–892 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Akiyama M. J., Spaulding A. C., Rich J. D., Flattening the curve for incarcerated populations - cCOVID-19 in jails and prisons. N. Engl. J. Med. 382, 2075–2077 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nowotny K., Bailey Z., Omori M., Brinkley-Rubinstein L., COVID-19 exposes need for progressive criminal justice reform. Am. J. Public Health 110, 967–968 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Barnert E., Ahalt C., Williams B., Prisons: Amplifiers of the COVID-19 pandemic hiding in plain sight. Am. J. Public Health 110, 964–966 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wang E. A., Western B., Backes E. P., Schuck J., Decarcerating Correctional Facilities during COVID-19: Advancing Health, Equity, and Safety (National Academies Press, Washington, DC, 2020). [PubMed] [Google Scholar]
- 22.Dumont D. M., Brockmann B., Dickman S., Alexander N., Rich J. D., Public health and the epidemic of incarceration. Annu. Rev. Public Health 33, 325–339 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Spaulding A. C., et al., How public health and prisons can partner for pandemic influenza preparedness: A report from Georgia. J. Correct. Health Care 15, 118–128 (2009). [DOI] [PubMed] [Google Scholar]
- 24.Sacchi F. P., et al., Prisons as reservoir for community transmission of tuberculosis, Brazil. Emerg. Infect. Dis. 21, 452–455 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Stuckler D., Basu S., McKee M., King L., Mass incarceration can explain population increases in TB and multidrug-resistant TB in European and central Asian countries. Proc. Natl. Acad. Sci. U.S.A. 105, 13280–13285 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kamarulzaman A., Verster A., Altice F. L., Prisons: Ignore them at our peril. Curr. Opin. HIV AIDS 14, 415–422 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.The New York Times , COVID in the U.S.: Latest Map and Case Count. The New York Times, 20 March 2021. https://www.nytimes.com/interactive/2020/us/coronavirus-us-cases.html. Accessed 1 September 2020.
- 28.Dolovich S., Mass incarceration, meet COVID-19. University of Chicago Law Review Online (16 November 2020). https://lawreviewblog.uchicago.edu/2020/11/16/covid-dolovich/. Accessed 1 May 2021.
- 29.Williams B. A., Ahalt C., Cloud D.et al., Correctional facilities in the shadow Of COVID-19: Unique challenges and proposed solutions. Health Affairs Blog (26 March 2020). 10.1377/hblog20200324.784502.
- 30.Rubin R., The challenge of preventing COVID-19 spread in correctional facilities. JAMA 323, 1760–1761 (2020). [DOI] [PubMed] [Google Scholar]
- 31.Wagner P., Sawyer W., States of Incarceration: The Global Context 2018. Prison Policy Initiative. June 2018. https://www.prisonpolicy.org/global/2018.html. Accessed 22 August 2020.
- 32.Franco-Paredes C., et al., Decarceration and community re-entry in the COVID-19 era. The Lancet Infectious Diseases. 10.1016/S1473-3099(20)30730-1. Accessed 29 September 2020.
- 33.Kang-Brown J., Montagnet C., Heiss J., People in jail and prison in 2020. Vera Institute of Justice. https://www.vera.org/publications/people-in-jail-and-prison-in-2020. Accessed 27 January 2020.
- 34.Servick K., Pandemic inspires new push to shrink jails and prisons. Science. https://www.sciencemag.org/news/2020/09/pandemic-inspires-new-push-shrink-jails-and-prisons. Accessed 18 September 2020.
- 35.Puglisi L. B., Malloy G. S. P., Harvey T. D., Brandeau M. L., Wang E. A., Estimation of COVID-19 basic reproduction ratio in a large urban jail in the United States. Ann. Epidemiol. 53, 103–105 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.American Civil Liberties Union , New Model Shows COVID-19 Death Toll is 100,000 Higher Than Current Projections. American Civil Liberties Union. 2020. https://www.aclu.org/press-releases/new-model-shows-covid-19-death-toll-100000-higher-current-projections. Accessed 1 May 2021.
- 37.Lofgren E., Lum K., Horowitz A., Madubuonwu B., Fefferman N., The epidemiological implications of incarceration dynamics in jails for community, corrections officer, and incarcerated population risks from COVID-19. medRXiV [Preprint]. 10.1101/2020.04.08.20058842.
- 38.Reinhart E., Chen D. L., Incarceration and its disseminations: COVID-19 pandemic lessons from Chicago’s Cook County Jail. Health Aff. (Millwood) 39, 1412–1418 (2020). [DOI] [PubMed] [Google Scholar]
- 39.Nowotny K. M., Bailey Z., Brinkley-Rubinstein L., The contribution of prisons and jails to US racial disparities during COVID-19. Am. J. Public Health 111, 197–199 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.The Sentencing Project, Criminal Justice Facts. The Sentencing Project. https://www.sentencingproject.org/criminal-justice-facts/. Accessed 1 May 2021.
- 41.Sawyer W., Wagner P., Mass Incarceration: The Whole Pie 2020. Prison Policy Initiative. March 24, 2020. https://www.prisonpolicy.org/reports/pie2020.html. Accessed 24 August 2020.
- 42.Wacquant L., Punishing the Poor: The Neoliberal Government of Social Insecurity (Duke University Press, Durham, NC, 2009). [Google Scholar]
- 43.Price-Haywood E. G., Burton J., Fort D., Seoane L., Hospitalization and mortality among black patients and white patients with cCOVID-19. N. Engl. J. Med. 382, 2534–2543 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gross C. P., et al., Racial and ethnic disparities in population-level cCOVID-19 mortality. J. Gen. Intern. Med. 35, 3097–3099 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Adhikari S., et al., Assessment of community-level disparities in coronavirus disease 2019 (COVID-19) infections and deaths in large US metropolitan areas. JAMA Netw. Open 3, e2016938 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Muñoz-Price L. S., et al., Racial disparities in incidence and outcomes among patients with COVID-19. JAMA Netw. Open 3, e2021892 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Dolovich S., The regulation and oversight of American prisons. Annu. Rev. Criminol. (2021) in press. [Google Scholar]
- 48.Sotomayor S., 591 U.S. Supreme Court. No. 20A19. Don Barnes, Sheriff, Orange County, California, et al v. Melissa Ahlman, et al. On application for stay. August 5, 2020. https://www.supremecourt.gov/opinions/19pdf/20a19_k537.pdf. Accessed 24 August 2020.
- 49.Pressley A. H. R., 7983–COVID-19 in Corrections Data Transparency Act. 116th United States Congress (2019-2020). Introduced August 7, 2020. https://www.congress.gov/bill/116th-congress/house-bill/7983. Accessed 24 August 2020.
- 50.Warren L., Warren, Barragán, Booker introduce legislation to require weekly COVID-19 testing, data collection, and robust COVID-19 prevention standards in federal prisons. https://www.warren.senate.gov/newsroom/press-releases/warren-barragn-booker-introduce-legislation-to-require-weekly-covid-19-testing-data-collection-and-robust-covid-19-prevention-standards-in-federal-prisons. Accessed 5 October 2020.
- 51.Flagg A., Neff J., Why jails are so important in the fight against coronavirus. The Marshall Project (2020). https://www.themarshallproject.org/2020/03/31/why-jails-are-so-important-in-the-fight-against-coronavirus. Accessed 1 May 2021.
- 52.Occupational Employment and Wages , May 2019: 33-3012 Correctional officers and jailers. US Bureau of Labor Statistics. https://www.bls.gov/oes/current/oes333012.htm. Accessed 25 January 2021.
- 53.Zenh Z., Jail inmates in 2017. Bureau of Justice Statistics, April 2019, NCJ 251774. https://www.bjs.gov/content/pub/pdf/ji17.pdf. Accessed 24 August 2020.
- 54.Bailey Z. D., et al., Structural racism and health inequities in the USA: Evidence and interventions. Lancet 389, 1453–1463 (2017). [DOI] [PubMed] [Google Scholar]
- 55.City of Chicago , COVID-19 cases, tests, and deaths by ZIP code. Chicago Data Portal. https://data.cityofchicago.org/Health-Human-Services/COVID-19-Cases-Tests-and-Deaths-by-ZIP-Code/yhhz-zm2v. Accessed 13 August 2020.
- 56.US Census Bureau , American community survey 5-year data (2009-2018). https://www.census.gov/data/developers/data-sets/acs-5year.html. Accessed 24 August 2020.
- 57.Zou H., Hastie T., Regularization and variable selection via the elastic net. J. R. Stat. Soc. B 67, 301–320 (2005). [Google Scholar]
- 58.Friedman J., Hastie T., Tibshirani R., Regularization paths for generalized linear models via coordinate descent. J. Stat. Softw. 33, 1–22 (2010). [PMC free article] [PubMed] [Google Scholar]
- 59.Milanez-Almeida P., Martins A. J., Germain R. N., Tsang J. S., Cancer prognosis with shallow tumor RNA sequencing. Nat. Med. 26, 188–192 (2020). [DOI] [PubMed] [Google Scholar]
- 60.LeSage J., “Spatial econometrics” in Handbook of Research Methods and Applications in Economic Geography, Karlsson C., Andersson M., Norman T., Eds. (Edward Elgar Publishing, Northampton, MA, 2015). [Google Scholar]
- 61.Manski C. F., Identification of endogenous social effects: The reflection problem. Rev. Econ. Stud. 60, 531–542 (1993). [Google Scholar]
- 62.Angrist J. D., Pischke J. S., The credibility revolution in empirical economics: How better research design is taking the con out of econometrics. J. Econ. Perspect. 24, 3–30 (2010). [Google Scholar]
- 63.Cook County Sheriff’s Office , About the Cook County Department of Corrections. https://www.cookcountysheriff.org/cook-county-department-of-corrections/. Accessed 24 August 2020.
- 64.Wildeman C., Wang E. A., Mass incarceration, public health, and widening inequality in the USA. Lancet 389, 1464–1474 (2017). [DOI] [PubMed] [Google Scholar]
- 65.Andrasfay T., Goldman N., Reductions in 2020 US life expectancy due to COVID-19 and the disproportionate impact on the Black and Latino populations. Proc. Natl. Acad. Sci. U.S.A. 188, e2014746118 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Centers for Disease Control and Prevention , COVID-19 Provisional Counts - Health Disparities 2020. https://www.cdc.gov/nchs/nvss/vsrr/covid19/health_disparities.htm. Accessed 30 September 2020.
- 67.Racial Data Dashboard , The COVID tracking project. 2020. https://covidtracking.com/race/dashboard. Accessed 30 September 2020.
- 68.Jay J., et al., Neighbourhood income and physical distancing during the COVID-19 pandemic in the United States. Nat. Hum. Behav. 4, 1294–1302 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Jowers K., Timmins C., Bhavsar N., Hu Q., Marshall J., Housing Precarity & the COVID-19 Pandemic: Impacts of Utility Disconnection and Eviction Moratoria on Infections and Deaths Across US Counties. NBER Working Paper 28394. January 2021. https://www.nber.org/papers/w28394. Accessed 1 May 2021.
- 70.Chen Y.-H., et al., Excess mortality associated with the COVID-19 pandemic among Californians 18–65 years of age, by occupational sector and occupation: March through October 2020. medRxiv [Preprint]. 10.1101/2021.01.21.21250266. [DOI] [PMC free article] [PubMed]
- 71.Ahmed F., Ahmed N., Pissarides C., Stiglitz J., Why inequality could spread COVID-19. Lancet Public Health 5, e240 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Wiemers E. E., et al., Disparities in Vulnerability to Severe Complications from COVID-19 in the United States. NBER Working Paper 27294. June 2020. https://www.nber.org/papers/w27294. Accessed 1 May 2021.
- 73.Millett G. A., et al., Assessing differential impacts of COVID-19 on black communities. Ann. Epidemiol. 47, 37–44 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Gordon C., Johnson W., Purnell J. Q., Rogers J., COVID-19 and the color line. Boston Review. May 1, 2020. bostonreview.net/race/colin-gordon-walter-johnson-jason-q-purnell-jamala-rogers-covid-19-and-color-line. Accessed 22 August 2020.
- 75.Olson D. E., Taheri S., Population dynamics and the characteristics of inmates in the Cook County Jail. Cook County Sheriff’s Reentry Council Research Bulletin. February 2012. https://ecommons.luc.edu/cgi/viewcontent.cgi?article=1000&context=criminaljustice_facpubs. Accessed 22 August 2020.
- 76.Gifford E. J., et al., Association of parental incarceration with psychiatric and functional outcomes of young Adults. JAMA Netw. Open 2, e1910005 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Hatzenbuehler M. L., Keyes K., Hamilton A., Uddin M., Galea S., The collateral damage of mass incarceration: Risk of psychiatric morbidity among nonincarcerated residents of high-incarceration neighborhoods. Am. J. Public Health 105, 138–143 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Dobbie W., Goldin J., Yang C. S., The effects of pretrial detention on conviction, future crime, and employment: Evidence from randomly Assigned judges. Am. Econ. Rev. 108, 201–240 (2018). [Google Scholar]
- 79.Kirk D. S., Wakefield S., Collateral consequences of punishment: A critical review and path forward. Annu. Rev. Criminol. 1, 171–194 (2018). [Google Scholar]
- 80.Western B., Pettit B., Incarceration and social inequality. Daedalus 139, 8–19 (2010). [DOI] [PubMed] [Google Scholar]
- 81.Binswanger I. A., et al., Release from prison–A high risk of death for former inmates. N. Engl. J. Med. 356, 157–165 (2007). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Travis J., Western B., Redburn S., The Growth of Incarceration in the United States: Exploring Causes and Consequences (National Academies Press, Washington, DC, 2014). [Google Scholar]
- 83.Brinkley-Rubinstein L., Sadacharan R., Macmadu A., Rich J. D., Introduction to the special issue of the Journal of Urban Health on incarceration and health. J. Urban Health 95, 441–443 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Kinner S. A., Young J. T., Understanding and improving the health of people who experience incarceration: An overview and synthesis. Epidemiol. Rev. 40, 4–11 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Brinkley-Rubinstein L., Cloud D. H., Mass incarceration as a social-structural driver of health inequities: A supplement to AJPH. Am. J. Public Health 110 (S1), S14–S15 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Harvey A., Taylor O., Wang A., COVID-19, jails, and public safety: December 2020. update. National Commission on COVID-19 and Criminal Justice. https://cdn.ymaws.com/counciloncj.org/resource/resmgr/covid_commission/covid-19,_jails,_and_public_.pdf. Accessed 1 May 2021.
- 87.Austin J., et al., How many Americans are unnecessarily incarcerated? Fed. Sentencing Report. 29, 140–174 (2017). [Google Scholar]
- 88.Margulies J., Let the people go. Boston review. April 20, 2020. http://bostonreview.net/law-justice/joseph-margulies-prisons-and-pandemics. Accessed 22 August 2020.
- 89.Nowonty K. M., Piquero A. R., The global impact of the pandemic on institutional and community corrections: Assessing short-term crisis management and long-term change strategies. Victims & Offenders 15, 839–847, 10.1080/15564886.2020.1813229 (2020). [DOI] [Google Scholar]
- 90.Vest N. A., Johnson O. D., Nowotny K. M., Brinkley-Rubinstein L., Prison population reductions and COVID-19: A latent profile analysis synthesizing recent evidence from the Texas state prison system. medRxiv [Preprint] 2020. 10.1101/2020.09.08.20190884. [DOI] [PMC free article] [PubMed]
- 91.Geng L., Report: Cook County Jail is filling up again. South Side Weekly (28 September 2020). https://southsideweekly.com/cook-county-jail-filling/. Accessed 29 September 2020.
- 92.Chalfin A., McCrary J., Criminal deterrence: A review of the literature. J. Econ. Lit. 55, 5–48 (2017). [Google Scholar]
- 93.Harding D. J., Do prisons make us safer? Scientific American. June 21, 2019. https://www.scientificamerican.com/article/do-prisons-make-us-safer/. Accessed 22 August 2020.
- 94.Harding D. J., Morenoff J. D., Nguyen A. P., Bushway S. D., Short- and long-term effects of imprisonment on future felony convictions and prison admissions. Proc. Natl. Acad. Sci. U.S.A. 114, 11103–11108 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Tseloni A., Mailley J., Garrell G., Exploring the international decline in crime rates. Eur. J. Criminol. 7, 375–394 (2010). [Google Scholar]
- 96.Harding D. J., Morenoff J. D., Nguyen A. P., Bushway S. D., Binswanger I. A., A natural experiment study of the effects of imprisonment on violence in the community. Nat. Hum. Behav. 3, 671–677 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Mauer M., Ghandnoosh N., Policy brief: Fewer prisoners, less crime. The sentencing project (23 July 2014). https://www.sentencingproject.org/publications/fewer-prisoners-less-crime-a-tale-of-three-states/. Accessed 6 October 2020.
- 98.Jiménez M. C., et al., Epidemiology of COVID-19 among incarcerated individuals and staff in Massachusetts jails and prisons. JAMA Netw. Open 3, e2018851 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Detention P., Prison policy initiative. https://www.prisonpolicy.org/research/pretrial_detention/. Accessed 5 October 2020.
- 100.Rabuy B., Kopf D., Detaining the poor: How money bail perpetuates an endless cycle of poverty and jail time (May 2016). https://www.prisonpolicy.org/reports/incomejails.html. Accessed 5 October 2020.
- 101.Vera Institute for Justice, Arrest Trends, Vera Institute for Justice (2018). https://arresttrends.vera.org/arrests. Accessed 22 August 2020.
- 102.Jones A., Sawyer W., Arrest, release, repeat: How police and jails are misused to respond to social problems. Prison policy initiative. August 2019. https://www.prisonpolicy.org/reports/repeatarrests.html. Accessed 22 August 2020.
- 103.Barsky B.A., Reinhart E., Farmer P. E., Keshavjee S., Vaccination plus decarceration––Stopping COVID-19 in jails and prisons. N. Engl. J. Med. 10.1056/NEJMp2100609 (2021). [DOI] [PubMed] [Google Scholar]
- 104.Press release: Middlesex Sheriff’s Office announces results of baseline vaccination surveys. Middlesex Sheriff’s Office (13 January 2021). https://www.middlesexsheriff.org/press-releases/news/middlesex-sheriff-announces-results-baseline-vaccination-surveys. Accessed 22 January 2021.
- 105.Paltiel A. D., Schwartz J. L., Zheng A., Walensky R. P., Clinical outcomes of a COVID-19 vaccine: Implementation over efficacy: Study examines how definitions and thresholds of vaccine efficacy, coupled with different levels of implementation effectiveness and background epidemic severity, translate into outcomes. Health Aff. 40, 10–377 (2020). [Google Scholar]
- 106.Reinhart E., Chen D. L., DE JURE WBG, Data for Carceral-Community Epidemiology, Structural Racism, and Covid-19 Disparities. Harvard Dataverse. 10.7910/DVN/NNBEGK. Accessed 1 May 2021. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Anonymized jail cycling data by ZIP code (supplied by Freedom of Information Act Request fulfilled by Cook County Jail), COVID-19 case and testing data by ZIP code (already made public by City of Chicago), and all other variables (drawn from public US Census and ACS data) have been deposited in Harvard Dataverse along with code, processed data, and model outputs (https://doi.org/10.7910/DVN/NNBEGK) (106).