Abstract
Background
Coronavirus disease 2019 (COVID-19) can cause serious complications such as multiorgan failure and death which are difficult to predict. We conducted this retrospective case-control observational study with the hypothesis that low serum albumin at presentation can predict serious outcomes in COVID-19 infection.
Methods
We included severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) reverse transcriptase-polymerase chain reaction (RT-PCR) confirmed, hospitalized patients from March to July 2020 in a tertiary care hospital in the USA. Patients were followed for 21 days for the development of the primary endpoint defined as the composite outcome which included acute encephalopathy, acute kidney injury, the requirement of new renal replacement therapy, acute hypercoagulability, acute circulatory failure, new-onset heart failure, acute cardiac injury, acute arrhythmia, acute respiratory distress syndrome (ARDS), high flow oxygen support, intensive care unit (ICU) stay, mechanical ventilation or death; and the secondary endpoint of death only. Univariate and multivariate logistic regression analyses were performed to study the effect of albumin level and outcomes.
Results
The mean age was 56.76 years vs. 55.67 years (P = 0.68) in the normal albumin vs. the low albumin group. We noticed an inverse relationship between serum albumin at presentation and serious outcomes. The low albumin group had a higher composite outcome (93.88% vs. 6.12%, P < 0.05) and higher mortality (13.87% vs. 2.38%, P < 0.05) in comparison to the normal albumin group. The multivariate logistic regression analysis revealed higher odds of having composite outcomes with lower albumin group (odds ratio (OR) 10.88, 95% confidence interval (CI) 4.74 - 24.97, P < 0.05). In the subgroup analysis, the multivariate logistic regression analysis revealed higher odds of having composite outcomes with the very low albumin group (OR 7.94, 95% CI 1.70 - 37.14, P < 0.05).
Conclusions
Low serum albumin on presentation in COVID-19 infection is associated with serious outcomes not limited to mortality. The therapeutic option of albumin infusion should be investigated.
Keywords: COVID-19, SARS-CoV-2, Hypoalbuminemia, Serious outcomes, Mortality, Albumin, ARDS, Hypercoagulopathy
Introduction
Coronavirus disease 2019 (COVID-19), caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), is a novel viral disease first discovered in December 2019 in Wuhan, China. Within 1 month, it was confirmed in 19 countries [1] and the World Health Organization declared it a pandemic shortly thereafter [2]. As of now, it has been established as a highly contagious viral disease, primarily affecting the respiratory system but with complications including kidney injury, liver injury, cardiac injury, stroke, encephalopathy, post-viral debility, coagulopathy, long hospital stay, and significant risk of mortality [3-12]. The majority of the patients survive the infection without complications, but a notable proportion of patients develop serious complications. Since the beginning, high levels of acute inflammatory markers were observed in the patients who had poor outcomes but the factors that lead to serious complications remain inadequately understood [3-5].
Albumin serves as a major anti-inflammatory agent in our body [13, 14], and one of the lesser discussed properties in the literature are its anti-oxidative and anti-thrombotic property [15, 16]. Albumin is a major defense that protects the host cells from the oxidative burst that occurs against the infection or inflammation [17-19]. Albumin has a long half-life (3 weeks) and 90% of it is in plasma [20]. The level of plasma is dropped rapidly during acute inflammation due to transcapillary leakage, consumption, and other mechanisms [13, 19, 21, 22].
As of now, we lack proven and effective therapeutic options to treat serious complications of COVID-19 infection. We also lack the ability to predict the serious outcomes of COVID-19 infection. In many studies, low levels of albumin, in addition to high inflammatory markers had been observed with those patients that had poor outcomes. Some studies have suggested that low serum albumin can predict mortality in COVID-19 infection [23-27].
We conducted this study to explore this relationship further with the hypothesis that low serum albumin at presentation can predict serious outcomes in COVID-19 infection.
Materials and Methods
The study was approved by Cape Fear Valley Medical Center’s Institutional Review Board (IRB ID number 319-20). This study was conducted in compliance with the ethical standards of the IRB on human subjects.
Study design and population
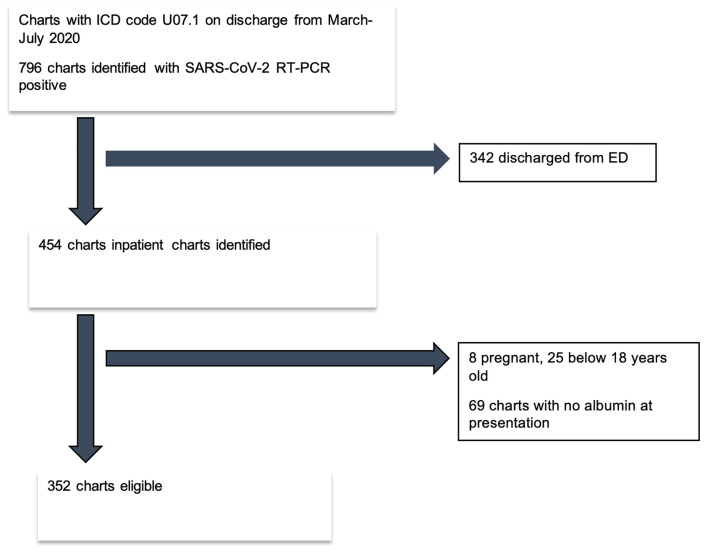
The study was a single-center retrospective case-control study. We reviewed the charts of patients with the discharge diagnosis of “COVID-19, virus identified” (ICD code U07.1) from March 1 to July 31, 2020 in a tertiary care center in North Carolina, United States of America (USA). We identified 796 charts that had confirmed SARS-CoV-2 reverse transcriptase-polymerase chain reaction (RT-PCR) results of nasopharyngeal swab. After exclusions, a total of 352 charts of unique patients were included in the study (Fig. 1). Inclusion criteria included: 1) patients with SARS-CoV-2 detected using the RT-PCR method, 2) age 18 and above, and 3) admission date between March 1, 2020 and July 31, 2020. Patients with 1) emergency department (ED) visits only, 2) less than 18 years of age, 3) pregnancy, and 4) no serum albumin available at presentation in the ED were excluded (Fig. 1).
Figure 1.
Flow diagram of eligible patient selection. RT-PCR: reverse transcriptase polymerase chain reaction; SARS-CoV-2: severe respiratory syndrome coronavirus 2.
Included patients were classified into two groups based on serum albumin at presentation: normal serum albumin (NSA) group with a value of ≥ 3.5 g/dL, and low serum albumin (LSA) group < 3.5 g/dL. The low albumin group was further sub-grouped as mild low albumin (MLA) group with a value of 2.5 - 3.4 g/dL and very low albumin (VLA) group with a value of < 2.5 g/dL for subgroup analysis. The patients were followed up for 21 days or until death if it happened sooner.
Outcomes
The primary outcome was defined as a composite outcome of death or any serious complications. The variables of serious complications were death, acute encephalopathy, acute kidney injury, the requirement of new renal replacement therapy, acute hypercoagulability, acute circulatory failure, new-onset heart failure, acute cardiac injury, acute arrhythmia, acute respiratory distress syndrome (ARDS), high flow oxygen support, intensive care unit (ICU) stay, and mechanical ventilation. The study definitions and definitions of serious complications are outlined in Table 1. The secondary outcome was death due to any cause during the 21 days follow-up period. The abbreviations, normal ranges, and units of variables are outlined in Table 2.
Table 1. Study Definition.
| Study variables | Definitions |
|---|---|
| Coronavirus disease 2019 (COVID-19) patients | Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) detected on reverse transcriptase-polymerase chain reaction (RT-PCR) of nasopharyngeal swab |
| Hypoalbuminemia (low albumin) | Serum albumin less than 3.5 g/dL |
| Mild low albumin | Serum albumin 2.5 - 3.4 g/dL |
| Very low albumin | Serum albumin less than 2.5 g/dL |
| Composite outcome (at least one of the following complications | Death, acute encephalopathy, acute kidney injury, the requirement of new renal replacement therapy, acute hypercoagulability, acute circulatory failure, new-onset heart failure, acute cardiac injury, acute arrhythmia, ARDS, high flow oxygen support, intensive care unit (ICU) stay, mechanical ventilation. |
| Death | Death due to any cause within 21 days |
| Chronic kidney disease (CKD) | Glomerular filtration rate < 60 mL/min (CKD 3-5) |
| Smoking | Active smoker with > 100 cigarettes smoking in lifetime |
| Alcohol dependency | Men ≥ 15 drinks/week; female ≥ 8 drinks/week |
| Malignancy | Cancer patient getting active treatment or finished treatment within 6 months |
| Onset of symptoms | First day of onset of symptoms to presentation to hospital in days |
| Use of one of the following medicines | Tocilizumab, remdesivir, dexamethasone and/or convalescent plasma |
| Secondary infection (one of the following) | Procalcitonin level > 0.5; lactic acid > 2.0; positive blood; urine; body fluid; respiratory secretion culture |
| Quick sequential organ failure assessment (qSOFA) | Altered mental status, respiratory rate ≥ 22/min, systolic blood pressure ≤ 100 mm Hg |
| Acute kidney injury | Increase in serum creatinine by 0.3 mg/dL or more within 48 h or increase in serum creatinine to 1.5 times baseline or more within the last 7 days |
| New renal replacement therapy (RRT) | The requirement of new RRT within 21 days in patients who were not dialysis-dependent |
| Acute encephalopathy | Worsening of alertness and awareness compared to baseline, and/or change in mental status |
| Acute liver injury | Development of severe acute liver injury (aspartate aminotransferase (AST) or alanine aminotransferase (ALT) > 5 times normal) with encephalopathy and impaired synthetic function (INR of ≥ 1.5) in a patient without cirrhosis or preexisting liver disease |
| Acute hypercoagulability | D-dimer level > 0.5 ng/mL |
| Stroke | New focal neurological deficit and/or radiological evidence in computed tomography (CT) or magnetic resonance imaging (MRI) |
| Acute circulatory failure | Systolic blood pressure (SBP) less than 90 mm Hg and/or requiring pressure support |
| Acute cardiac injury | Increase in serum troponin value of > 0.015 in two occasions 6 h apart, and or ST-segment elevation or depression in electrocardiogram (EKG) |
| Arrhythmia | New-onset rhythm disorder proven on 12-lead EKG on two separate occasions |
| New-onset heart failure | New-onset systolic or diastolic heart failure on echocardiogram |
| Acute respiratory distress syndrome (ARDS) | The PaO2/FiO2 ≤ 300 mm Hg, on ventilator settings that include positive end-expiratory pressure (PEEP) or continuous positive airway pressure (CPAP) ≥ 5 cm H2O. |
| High flow oxygen support | Requiring high flow oxygen of 15 L or more to maintain an oxygen saturation of 92% or more |
| New-onset oxygen dependency | Any amount of supplemental oxygen required to maintain an oxygen saturation of 92% and above on discharge |
| Physical debility | Discharge to a skilled nursing facility or rehabilitation center |
| Obesity | Body mass index (BMI) of 30.0 or higher |
Table 2. Abbreviations, Normal Ranges and Units.
| Abbreviations | Full forms | Normal ranges and units (where applicable) |
|---|---|---|
| AKI | Acute kidney injury | |
| Albumin | 3.5 - 5.0 g/dL | |
| ALT | Alanine aminotransferase | 12 - 78 U/L |
| AMS | Altered mental status | |
| AST | Aspartate aminotransferase | 15 - 37 U/L |
| CAD | Coronary artery disease | |
| CHF | Congestive heart failure | |
| CKD | Chronic kidney disease | |
| COPD | Chronic obstructive pulmonary disease | |
| COVID-19 | Coronavirus disease 2019 | |
| CRP | C-reactive protein | < 3 mg/L |
| D-dimer | 0.9 - 0.5 mg/dL | |
| DM | Diabetes mellitus | |
| ESR | Erythrocyte sedimentation rate | 0 - 15 mm/h |
| ESRD on HD | End-stage renal disease on hemodialysis | |
| Ferritin | 26 - 388 ng/mL | |
| HIV | Human immunodeficiency virus | |
| HTN | Hypertension | |
| IL-6 | Interleukin-6 | 0 - 13 pg/mL |
| INR | International normalized ratio | |
| Lactic acid | 0.4 - 2 mmol/L | |
| LDH | Lactate dehydrogenase | 87 - 241 U/L |
| LO | Length of | |
| Lymphocyte | 0.9 - 2.9 × 103/µL | |
| Neutrophil | 1.7 - 7 × 103/µL | |
| NL ratio | Neutrophil to lymphocyte ratio | |
| Platelets | 150 - 450 × 103/µL | |
| Procalcitonin | 0.07 - 0.5 ng/mL | |
| qSOFA | Quick sequential organ failure assessment | |
| RT-PCR | Reverse transcriptase-polymerase chain reaction | |
| SARS-CoV-2 | Severe acute respiratory syndrome coronavirus 2 | |
| SOB | Shortness of breath |
Statistical analysis
A formal sample size calculation was not carried out as all patients meeting criteria in the pre-specified timeframe were included. The differences in categorical variables were analyzed using a Chi-square test, or Fisher’s exact test as appropriate. A Student’s t-test was utilized to evaluate differences in continuous variables that were normally distributed, and a Wilcoxon rank sum test was utilized if the data were not normally distributed. Continuous variables were expressed as mean ± SD and categorical variables were expressed as the frequency with percentages. The association of albumin level category and outcome was estimated in univariate and multivariate logistic regression analyses in terms of odds ratio (OR). Multivariate analyses were adjusted for age, sex, race, diabetes mellitus (DM), hypertension (HTN), chronic kidney disease (CKD), end-stage renal disease on hemodialysis (ESRD on HD), chronic obstructive pulmonary disease (COPD), other lung diseases, congestive heart failure (CHF), coronary artery disease (CAD), human immunodeficiency virus (HIV) infection, malignancy, smoking, alcohol dependency, obesity, and cirrhosis. A P-value of < 0.05 was considered significant. Data analysis was performed using STATA 13.1 (Stata Corp., College Station, TX).
Results
Demographic features
Baseline demographic and lab characteristics by albumin level categories are depicted in Table 3. The overall population was predominantly males (n = 184, 52.27%), and African-American (n = 176, 50%). Eighty-one percentage (n = 288) had at least one co-morbidity. Cough (62.78% vs. 73.81%, P = 0.16), fever (58.90% vs. 64.29%, P = 0.5), and shortness of breath (64.08% vs. 59.52%, P = 0.56) were the most common presenting symptoms in the LSA and NSA groups, respectively. The frequency of CKD was higher among the NSA group (35.71% vs. 17.10%, P < 0.05). Among the subgroups of low albumin, the presenting symptoms and co-morbidities were similar between the two groups (Table 3).
Table 3. Baseline Characteristics of Normal and Low Serum Albumin Groups.
| NSA vs. LSA group (primary group) |
MLA vs. VLA group (subgroup) |
|||||
|---|---|---|---|---|---|---|
| NSA (n = 42) | LSA (n = 310) | P-value | MLA (albumin 2.5 - 3.4, n = 249) | VLA (albumin < 2.5, n = 61) | P-value | |
| Age, m (SD) | 56.76 (16.18) | 55.67 (18.23) | 0.68 | 55.91 (18.90) | 54.68 (15.26) | 0.59 |
| Female, n (%) | 18 (42.86) | 150 (48.39) | 0.50 | 109 (43.78) | 41 (67.21) | 0.001* |
| Race | 0.48 | 0.01* | ||||
| White, n (%) | 10 (23.81) | 73 (23.55) | 49 (19.76) | 23 (37.70) | ||
| African American, n (%) | 24 (57.14) | 152 (49.03) | 126 (50.81) | 26 (42.62) | ||
| Others, n (%) | 8 (196.05) | 85 (27.42) | 73 (29.44) | 12 (19.67) | ||
| Comorbid conditions | ||||||
| Diabetes mellitus, n (%) | 20 (47.62) | 111 (35.81) | 0.13 | 95 (38.15) | 16 (26.23) | 0.08 |
| Hypertension, n (%) | 34 (80.95) | 191 (61.61) | 0.014* | 155 (62.25) | 36 (59.02) | 0.64 |
| CKD, n (%) | 15 (35.71) | 53 (17.10) | 0.004* | 41 (16.47) | 12 (19.67) | 0.55 |
| ESRD on HD, n (%) | 5 (11.90) | 21 (6.77) | 0.23 | 18 (7.23) | 3 (4.92) | 0.52 |
| COPD, n (%) | 4 (9.52) | 31 (10) | 0.92 | 25 (10.04) | 6 (9.84) | 0.96 |
| Other lung diseases, n (%) | 5 (11.90) | 47 (15.21) | 0.57 | 36 (14.52) | 11 (18.03) | 0.49 |
| CHF, n (%) | 7 (16.67) | 37 (11.94) | 0.38 | 29 (11.65) | 8 (13.11) | 0.75 |
| CAD, n (%) | 11 (26.19) | 55(17.74) | 0.18 | 45 (18.07) | 10 (16.39) | 0.75 |
| HIV, n (%) | 1 (2.38) | 6 (1.94) | 0.84 | 1 (0.40) | 5 (8.20) | < 0.001* |
| Malignancy, n (%) | 6 (14.29) | 24 (7.74) | 0.15 | 19 (7.63) | 5 (8.20) | 0.88 |
| Smoking, n (%) | 11 (26.19) | 55 (18.52) | 0.24 | 39 (16.53) | 16 (26.23) | 0.082 |
| Alcohol dependency, n (%) | 4 (9.52) | 22 (7.10) | 0.53 | 19 (7.63) | 3 (4.92) | 0.46 |
| Obesity, n (%) | 18 (42.86) | 161 (51.94) | 0.26 | 129 (51.81) | 32 (52.46) | 0.92 |
| Cirrhosis, n (%) | 1 (2.38) | 5 (1.62) | 0.72 | 4 (1.61) | 1 (1.64) | 0.98 |
| Symptoms | ||||||
| Onset of symptoms (days), m (SD) | 4.11 (3.6) | 5.62 (4.97) | 0.018* | 5.52 (5.03) | 5.98 (4.76) | 0.51 |
| Fever, n (%) | 27 (64.29) | 182 (58.90) | 0.50 | 146 (58.63) | 36 (59.02) | 0.95 |
| Cough, n (%) | 31 (73.81) | 194 (62.78) | 0.16 | 150 (60.24) | 44 (72.13) | 0.085 |
| SOB, n (%) | 25 (59.52) | 198 (64.08) | 0.56 | 152 (61.04) | 47 (77.05) | 0.019* |
| Diarrhea, n (%) | 6 (14.29) | 33 (10.68) | 0.48 | 21 (8.43) | 13 (21.31) | 0.004* |
| AMS, n (%) | 6 (14.29) | 35 (11.33) | 0.57 | 31 (12.45) | 4 (6.56) | 0.192 |
| Chest pain, n (%) | 12 (28.57) | 39 (12.66) | 0.006* | 30 (12.10) | 9 (14.75) | 0.57 |
| Others, n (%) | 12 (28.57) | 74 (47.13) | 0.026* | 74 (47.13) | 15 (24.59) | 0.002* |
| Laboratory results | ||||||
| Albumin (g/dL), m (SD) | 3.77 (0.28) | 2.84 (0.41) | < 0.001* | 3.01 (0.24) | 2.15 (0.24) | < 0.001* |
| ESR (mm/h), m (SD) | 24 (15.52) | 57.90 (34.24) | < 0.001* | 53.43 (34.40) | 72.21 (29.30) | 0.010* |
| CRP (mg/L), m (SD) | 35.02 (43.28) | 84.32 (60.49) | < 0.001* | 81.33 (60.62) | 101.21 (64.27) | 0.043* |
| Neutrophil (× 103/µL), m (SD) | 3.65 (2.24) | 5.99 (4.05) | < 0.001* | 5.45 (3.18) | 8.35 (6.87) | 0.005* |
| Lymphocyte (× 103/µL), m (SD) | 1.38 (0.91) | 1.14 (0.70) | 0.21 | 1.21 (0.74) | 0.89 (0.45) | < 0.001* |
| NL ratio, m (SD) | 3.94 (3.68) | 6.88 (6.74) | 0.001* | 6.28 (6.75) | 8.87 (6.23) | 0.011* |
| Platelets (× 103/µL), m (SD) | 220.90 (73.77) | 233.51 (90.11) | 0.83 | 217.86 (82.40) | 245.48 (114.16) | 0.07 |
| Ferritin (ng/mL), m (SD) | 571.83 (961.77) | 925.69 (2,012.85) | 0.14 | 744.46 (1,150.94) | 1,650.90 (3,696.46) | 0.073 |
| IL-6 (pg/mL), m (SD) | 92.87 (161.77) | 244.18 (533.03) | 0.032* | 200 (433.68) | 352.87 (601.61) | 0.20 |
| LDH (U/L), m (SD) | 287.85 (148.17) | 398.79 (377.32) | 0.007* | 367.92 (166.65) | 515.76 (752.83) | 0.16 |
*Significant P-values. NSA: normal serum albumin; LSA: low serum albumin; MLA: medium low albumin; VLA: very low albumin; m: mean; SD: standard deviation; n: number; CKD: chronic kidney disease; ESRD: end-stage renal disease; HD: hemodialysis; COPD: chronic obstructive pulmonary disease; CHF: congestive heart disease; CAD: coronary artery disease; HIV: human immunodeficiency virus; SOB: shortness of breath; AMS: altered mental status; ESR: erythrocyte sedimentation rate; CRP: C-reactive protein; NL: neutrophil to lymphocyte; IL-6: interleukin-6; LDH: lactate dehydrogenase.
Primary outcome
The LSA group had a significantly higher proportion of composite outcome compared to the NSA group (93.88% vs. 6.12%, P < 0.05). This difference was true in between the subgroups of only low albumin as well, where 96.72% of the VLA group had composite outcome as compared to 81.12% in the MLA group (P < 0.05) (Table 4).
Table 4. In-Hospital Complications and Duration of Stays in Normal and Low Serum Albumin Groups.
| NSA vs. LSA group (primary group) |
MLA vs. VLA group (subgroup) |
|||||
|---|---|---|---|---|---|---|
| NSA (n = 42) | LSA (n = 310) | P-value | MLA (albumin 2.5 - 3.4, n = 249) | VLA (albumin < 2.5, n = 61) | P-value | |
| Composite outcome, n (%) | 17 (6.12) | 261 (93.88) | < 0.001* | 202 (81.12) | 59 (96.72) | 0.003* |
| Death, n (%) | 1 (2.38) | 43 (13.87) | 0.035* | 24 (9.64) | 19 (31.15) | < 0.001* |
| Tocilizumab, n (%) | 4 (9.52) | 73 (23.62) | 0.038* | 51 (20.48) | 22 (36.07) | 0.010* |
| Remdesivir, n (%) | 1 (2.38) | 71 (22.98) | 0.002* | 54 (21.69) | 17 (27.87) | 0.30 |
| Dexamethasone, n (%) | 10 (23.81) | 106 (34.30) | 0.17 | 87 (34.94) | 19 (31.67) | 0.63 |
| Convalescent plasma, n (%) | 2 (4.76) | 35 (11.33) | 0.194 | 22 (8.84) | 13 (21.31) | 0.006* |
| qSOFA 2-3, n (%) | 3 (7.14) | 68 (21.94) | 0.025* | 50 (20.08) | 18 (29.51) | 0.11 |
| Acute circulatory failure, n (%) | 1 (2.38) | 64 (20.65) | 0.004* | 43 (17.27) | 21 (34.43) | 0.003* |
| Secondary infection | ||||||
| Procalcitonin > 0.5 ng/mL, n (%) | 3 (9.09) | 96 (35.29) | 0.002* | 62 (28.57) | 35 (63.64) | < 0.001* |
| Lactic acid > 2 mmol/L, n (%) | 4 (15.38) | 53 (20.08) | 0.56 | 38 (17.92) | 16 (30.77) | 0.04* |
| Blood culture, n (%) | 0 (0) | 19 (7.12) | 0.138 | 12 (5.53) | 8 (16) | 0.011* |
| Urine culture, n (%) | 0 (0) | 16 (9.25) | 0.146 | 13 (8.97) | 4 (14.29) | 0.38 |
| Body fluid culture, n (%) | 1 (4.55) | 6 (6.41) | 0.97 | 5 (4.39) | 1 (4.55) | 0.97 |
| Respiratory secretion culture, n (%) | 7 (26.92) | 47 (24.35) | 0.77 | 38 (23.75) | 9 (27.27) | 0.66 |
| AKI, n (%) | 6 (14.28) | 133 (43.36) | 0.004* | 95 (38.30) | 38 (62.29) | 0.002* |
| Requiring new HD, n (%) | 1 (2.38) | 17 (5.52) | 0.38 | 5 (2.02) | 12 (19.67) | < 0.001* |
| INR > 1.5 | 0 (0) | 22 (8.83) | 0.34 | 13 (6.63) | 9 (16.98) | 0.071 |
| AST or ALT > 5 times normal | 2 (4.76) | 32 (10.49) | 0.24 | 19 (7.79) | 13 13 (21.31) | 0.002* |
| Acute hypercoagulability | < 0.001* | < 0.001* | ||||
| D-dimer > 1 mg/dL, n (%) | 7 (21.21) | 132 (50.96) | 92 (44.66) | 40 (75.47) | ||
| D-dimer 0.5 - 1 mg/dL, n (%) | 3 (9.09) | 62 (23.90) | 55 (26.70) | 7 (13.21) | ||
| Acute encephalopathy, n (%) | 3 (7.14) | 71 (22.90) | 0.019* | 48 (19.28) | 23 (37.70) | 0.002* |
| Cerebrovascular accident, n (%) | 0 (0) | 0 (0) | n/a | 0 (0) | 0 (0) | n/a |
| Acute cardiac injury, n (%) | 3 (7.32) | 89 (29.87) | 0.002* | 67 (28.03) | 22 (37.29) | 0.164 |
| New-onset heart failure, n (%) | 1 (2.44) | 13 (4.22) | 0.58 | 9 (3.63) | 4 (6.67) | 0.29 |
| New-onset arrhythmia, n (%) | 4. (9.76) | 34 (10.97) | 0.81 | 21 (8.43) | 13 (21.31) | 0.004* |
| ARDS, n (%) | 1 (2.27) | 60 (20.98) | 0.008* | 34 (15.04) | 26 (43.33) | < 0.001* |
| Mechanical ventilation, n (%) | 1 (2.38) | 41 (13.27) | 0.041* | 23 (9.27) | 18 (29.51) | < 0.001* |
| Requiring > 3 L O2, n (%) | 8 (19.05) | 166 (53.55) | < 0.001* | 117 (46.99) | 49 (80.33) | < 0.001* |
| Requiring > 15 L high flow O2, n (%) | 4 (9.52) | 88 (28.39) | 0.009* | 57 (22.89) | 31 (50.82) | < 0.001* |
| New-onset oxygen dependency, n (%) | 1 (2.38) | 41 (13.80) | 0.035* | 27 (11.20) | 14 (25) | 0.007* |
| LO stay (days), m (SD) | 4.16 (5.55) | 9.32 (9.70) | < 0.001* | 8.14 (8.53) | 14.18 (12.40) | < 0.001* |
| LO ICU stay (days), m (SD) | 0.24 (1.56) | 1.96 (5.59) | < 0.001* | 1.4 (4.9) | 4.24 (7.44) | 0.005* |
| LO mechanical vent (days), m (SD) | 0.24 (1.56) | 1.60 (4.96) | < 0.001* | 1.13 (4.16) | 3.59 (7.13) | 0.01* |
| Physical debility (days), n (%) | 3 (7.32) | 75 (24.51) | 0.013* | 56 (22.67) | 19 (32.20) | 0.12 |
| Discharged, n (%) | 41 (97.62) | 270 (87.10) | 0.046* | 221 (88.76) | 49 (80.33) | 0.078* |
| Readmission, n (%) | 5 (11.90) | 47 (15.16) | 0.57 | 38 (15.26) | 9 (14.75) | 0.92 |
*Significant P-values. NSA: normal serum albumin; LSA: low serum albumin; MLA: medium low albumin; VLA: very low albumin; m: mean; SD: standard deviation; n: number; qSOFA: quick sequential organ failure assessment; AKI: acute kidney injury; CVA: cerebrovascular accident; HD: hemodialysis; INR: international normalized ratio; AST: aspartate aminotransferase; ALT: alanine aminotransferase; ARDS: acute respiratory distress syndrome; LO: length of; ICU: intensive care unit.
Logistic regression analysis revealed higher odds of having composite outcome with the lower albumin group during univariate (OR 7.83, 95% confidence interval (CI) 3.94 - 15.58, P < 0.05) and multivariate (OR 10.88, 95% CI 4.74 - 24.97, P < 0.05) analyses. Subgroup analysis also revealed a similar relationship (Table 5).
Table 5. Results From Logistic Regression Analyses - Odds of Composite Outcome Based on Albumin Level Category.
| Univariate analysis |
Multivariate analysisa |
|||||
|---|---|---|---|---|---|---|
| Odds ratio | 95% CI | P-value | Odds ratio | 95% CI | P-value | |
| Main group (LSA vs. NSA) | 7.83 | 3.94 - 15.58 | < 0.001* | 10.88 | 4.74 - 24.97 | < 0.001* |
| Subgroup (VLA vs. MLA) | 6.86 | 1.62 - 29.10 | 0.009* | 7.94 | 1.70 - 37.14 | 0.009* |
*Significant P-values. aControlled for age; sex; race; diabetes mellitus; hypertension; chronic kidney disease; end-stage renal disease on hemodialysis; chronic obstructive pulmonary disease; other lung diseases; congestive heart failure; coronary artery disease; human immunodeficiency virus infection; malignancy; smoking; alcohol dependency; obesity; and cirrhosis. NSA: normal serum albumin; LSA: low serum albumin; MLA: medium low albumin; VLA: very low albumin; CI: confidence interval.
In comparison to the NSA group, the LSA group had higher length of stay (9.33 days vs. 4.48 days, P < 0.05), higher incidence of acute kidney injury (AKI) (42.90% vs. 14.29%, P < 0.05), acute encephalopathy (22.90% vs. 7.14%, P < 0.05), mechanical ventilation use (13.23% vs. 2.38%, P < 0.05), development of ARDS (19.35% vs. 2.39%, P < 0.05) and post-viral physical debility (24.19% vs. 3%, P < 0.05). Similar differences were observed between the VLA and MLA groups with a higher incidence among the VLA group (Table 4). Multivariate analysis revealed that malignancy had the strongest influence on the primary outcome (OR 11.34, 95% CI 2.05 - 62.64, P < 0.05) (Table 6).
Table 6. Results From MV Analysis in Normal and Low Albumin Groups.
| Outcome | Normal vs. low albumin group (primary group) |
Medium low vs. very low albumin group (subgroup) |
||||
|---|---|---|---|---|---|---|
| Odds ratio | 95% CI | P-value | Odds ratio | 95% CI | P-value | |
| Albumin level (lower ref to higher) | 10.88 | 4.74 - 24.97 | < 0.001* | 7.94 | 1.70 - 37.14 | 0.009* |
| Age | 1.00 | 0.98 - 1.02 | 0.56 | 0.99 | 0.91 - 1.02 | 0.81 |
| Sex | 0.77 | 0.41 - 1.47 | 0.44 | 1.5 | 0.71 - 3.18 | 0.27 |
| Race | ||||||
| White | 0.37 | 0.16 - 0.82 | 0.015* | 1.77 | 0.59 - 5.32 | 0.30 |
| Others | 0.73 | 0.33 - 1.63 | 0.45 | 1.16 | 0.49 - 2.71 | 0.72 |
| Smoking | 1.93 | 0.81 - 4.5 | 0.13 | 0.52 | 0.20 - 1.33 | 0.17 |
| DM | 0.61 | 0.32 - 1.19 | 0.15 | 1.12 | 0.52 - 2.40 | 0.76 |
| HTN | 1.04 | 0.46 - 2.36 | 0.91 | 0.38 | 0.14 - 1.04 | 0.06 |
| CKD | 0.54 | 0.22 - 1.32 | 0.18 | 2.04 | 0.66 - 6.32 | 0.21 |
| ESRD on HD | 1.11 | 0.30 - 4.11 | 0.86 | 0.38 | 0.08 - 1.69 | 0.20 |
| COPD | 0.41 | 0.13 - 1.21 | 0.1 | 1.30 | 0.34 - 4.92 | 0.69 |
| CHF | 1.40 | 0.45 - 4.32 | 0.55 | 4.78 | 1.06 - 21.38 | 0.041* |
| CAD | 0.67 | 0.26 - 1.72 | 0.40 | 0.75 | 0.26 - 2.16 | 0.60 |
| HIV | 1.46 | 0.14 - 14.93 | 0.74 | 1 | ||
| Malignancy | 11.34 | 2.05 - 62.64 | 0.005* | 0.78 | 0.20 - 2.99 | 0.72 |
| Alcohol dependency | 1.58 | 0.40 - 6.19 | 0.50 | 3.35 | 0.62 - 17.86 | 0.15 |
| Obesity | 0.66 | 0.35 - 2.14 | 0.22 | 0.66 | 0.31 - 1.39 | 0.28 |
| Other lung disease | 0.87 | 0.35 - 2.14 | 0.77 | 0.31 | 0.12 - 0.78 | 0.014* |
| Cirrhosis | 0.06 | 0.08 - 0.57 | 0.014* | 1.45 | 0.09 - 22.22 | 0.78 |
MV controlled for age; sex; race; diabetes mellitus (DM); hypertension (HTN); chronic kidney disease (CKD); end-stage renal disease (ESRD) on hemodialysis (HD); chronic obstructive pulmonary disease (COPD); other lung diseases; congestive heart failure (CHF); coronary artery disease (CAD); human immunodeficiency virus (HIV) infection; malignancy; smoking; alcohol dependency; obesity; and cirrhosis. *Significant P-values. MV: multivariate; CI: confidence interval.
Secondary outcome
The LSA group was found to have higher mortality within 21 days as compared to the NSA group (13.87% vs. 2.38%, P < 0.05). Subgroup analysis of the low albumin group revealed 31.15% mortality in the VLA group vs. 9.64% in the MLA group (P < 0.05) (Table 4). We were unable to perform the regression analysis on mortality outcomes due to the very low number of mortalities in the normal albumin group.
Discussion
In this single-center study, we found that low serum albumin at the presentation in hospitalized patients with COVID-19 infection predicted higher mortality. Lower serum albumin at presentation was found to be an independent predictor of serious outcomes even after controlling for the multitude of factors such as age, sex, and presence of co-morbid conditions.
Low albumin level has been reported in hospitalized patients with COVID-19 that had poor outcomes from the beginning of the pandemic [3-5, 28]. A similar trend was observed in other studies that were conducted outside of China as well [26, 27, 29]. A few studies that compared low albumin level with mortality concluded that low albumin can predict mortality in COVID-19 patients [23-25]. In addition to low albumin, high levels of inflammatory markers were also noted in those studies. The findings of our study are consistent with these prior findings.
Low albumin has been found to predict higher mortality, a longer length of stay in hospitalized patients, and the general elderly population [30-34]; normalization of albumin prior to discharge was found to lower the mortality [33]. Albumin therapy has been shown to improve the oxygenation in ARDS [35, 36], and improve mortality in spontaneous bacterial peritonitis patients [37]. In the letter to the editor by Wiedermann et al and its response, the authors reported pooled analysis of three large-scale randomized controlled trials on sepsis and found that albumin therapy had a significant reduction in mortality which was attributed partly to albumin’s anti-oxidative and anti-immunosuppressive property [38]. The mechanistic theory for this includes albumin’s ability to bind reactive oxygen and reactive nitrogen species (ROS and RNS) preventing cellular damage and tissue injury during overwhelming inflammatory response [17-19]. These findings have given rise to the concept of the potential therapeutic use of albumin for COVID-19 infection [27, 39].
One of the limitations of our study is being a single-center study. More than 50% of the charts needed to be excluded decreasing the sample size. However, our study sample size was comparable to many similar studies done recently. The population was of mixed races unlike many studies done in China or Europe. We could not do the multivariate analysis of mortality because there was only one death in the normal albumin group.
COVID-19 has been diagnosed in more than 200 countries [40]. In the USA alone more than 30 million people were infected, and 556 thousand had died [41]. So far, there is no effective treatment for COVID-19 infection [40, 42-47], and the success of developed vaccines being unanswered due to emerging new strains of SARS-CoV-2. Due to recurrent waves of infection caused by emerging strains of SARS-CoV-2 the South Asian region, South American, Europe and other parts of the world had been through series of lockdowns. In addition, the vaccines are still out of reach of many low-medium income countries. We believe that this study will help health providers recognize that lower albumin carries a higher risk of severe complications and mortality in COVID-19 infection. It will be interesting to see the studies that utilize albumin as a treatment for serious COVID-19 illness.
Conclusion
Low serum albumin on presentation in COVID-19 infection is associated with a higher incidence of serious outcomes like kidney injury, cardiac injury, hypercoagulability, post-viral physical debility, and encephalopathy; and higher mortality. Further investigation of the utility of albumin replacement as a treatment of COVID-19 infection should be done as soon as possible.
Acknowledgments
None to declare.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Informed Consent
The informed consent was waived by IRB as the study was a retrospective study.
Author Contributions
RA designed the study, portions of statistical analysis, manuscript writing; DP and RB did the statistical analysis and contributed to manuscript writing; RA, AP, ES, MB, RP, SS, MB and SK did the portions of statistical analysis, and contributed to manuscript writing; KL and IL contributed to manuscript writing and supervision of the study. All authors read and approved the final manuscript.
Data Availability
The database used and/or analyzed during the current study is available from the corresponding author on reasonable request.
References
- 1.Adhikari SP, Meng S, Wu YJ, Mao YP, Ye RX, Wang QZ, Sun C. et al. Epidemiology, causes, clinical manifestation and diagnosis, prevention and control of coronavirus disease (COVID-19) during the early outbreak period: a scoping review. Infect Dis Poverty. 2020;9(1):29. doi: 10.1186/s40249-020-00646-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. WHO Director-General’s opening remarks at the media briefing on COVID-19. March 11, 2020 [Internet]. [cited Oct 9, 2020]. Available from: https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020.
- 3.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L. et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, Xiang J. et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chen T, Wu D, Chen H, Yan W, Yang D, Chen G, Ma K. et al. Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study. BMJ. 2020;368:m1091. doi: 10.1136/bmj.m1091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chen YT, Shao SC, Hsu CK, Wu IW, Hung MJ, Chen YC. Incidence of acute kidney injury in COVID-19 infection: a systematic review and meta-analysis. Crit Care. 2020;24(1):346. doi: 10.1186/s13054-020-03009-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Long B, Brady WJ, Koyfman A, Gottlieb M. Cardiovascular complications in COVID-19. Am J Emerg Med. 2020;38(7):1504–1507. doi: 10.1016/j.ajem.2020.04.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Levi M, Thachil J, Iba T, Levy JH. Coagulation abnormalities and thrombosis in patients with COVID-19. Lancet Haematol. 2020;7(6):e438–e440. doi: 10.1016/S2352-3026(20)30145-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Klok FA, Kruip M, van der Meer NJM, Arbous MS, Gommers D, Kant KM, Kaptein FHJ. et al. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res. 2020;191:145–147. doi: 10.1016/j.thromres.2020.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Middeldorp S, Coppens M, van Haaps TF, Foppen M, Vlaar AP, Muller MCA, Bouman CCS. et al. Incidence of venous thromboembolism in hospitalized patients with COVID-19. J Thromb Haemost. 2020;18(8):1995–2002. doi: 10.1111/jth.14888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mao R, Qiu Y, He JS, Tan JY, Li XH, Liang J, Shen J. et al. Manifestations and prognosis of gastrointestinal and liver involvement in patients with COVID-19: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol. 2020;5(7):667–678. doi: 10.1016/S2468-1253(20)30126-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mao L, Jin H, Wang M, Hu Y, Chen S, He Q, Chang J. et al. Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan, China. JAMA Neurol. 2020;77(6):683–690. doi: 10.1001/jamaneurol.2020.1127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Artigas A, Wernerman J, Arroyo V, Vincent JL, Levy M. Role of albumin in diseases associated with severe systemic inflammation: Pathophysiologic and clinical evidence in sepsis and in decompensated cirrhosis. J Crit Care. 2016;33:62–70. doi: 10.1016/j.jcrc.2015.12.019. [DOI] [PubMed] [Google Scholar]
- 14.Rozga J, Piatek T, Malkowski P. Human albumin: old, new, and emerging applications. Ann Transplant. 2013;18:205–217. doi: 10.12659/AOT.889188. [DOI] [PubMed] [Google Scholar]
- 15.Grigoriadis G, Stewart AG. Albumin inhibits platelet-activating factor (PAF)-induced responses in platelets and macrophages: implications for the biologically active form of PAF. Br J Pharmacol. 1992;107(1):73–77. doi: 10.1111/j.1476-5381.1992.tb14465.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kim SB, Chi HS, Park JS, Hong CD, Yang WS. Effect of increasing serum albumin on plasma D-dimer, von Willebrand factor, and platelet aggregation in CAPD patients. Am J Kidney Dis. 1999;33(2):312–317. doi: 10.1016/S0272-6386(99)70306-9. [DOI] [PubMed] [Google Scholar]
- 17.Rabbani G, Ahn SN. Structure, enzymatic activities, glycation and therapeutic potential of human serum albumin: A natural cargo. Int J Biol Macromol. 2019;123:979–990. doi: 10.1016/j.ijbiomac.2018.11.053. [DOI] [PubMed] [Google Scholar]
- 18.Galley HF. Oxidative stress and mitochondrial dysfunction in sepsis. Br J Anaesth. 2011;107(1):57–64. doi: 10.1093/bja/aer093. [DOI] [PubMed] [Google Scholar]
- 19.Caraceni P, Tufoni M, Bonavita ME. Clinical use of albumin. Blood Transfus. 2013;11(Suppl 4):s18–25. doi: 10.2450/2013.005s. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Garcovich M, Zocco MA, Gasbarrini A. Clinical use of albumin in hepatology. Blood Transfus. 2009;7(4):268–277. doi: 10.2450/2008.0080-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Moshage HJ, Janssen JA, Franssen JH, Hafkenscheid JC, Yap SH. Study of the molecular mechanism of decreased liver synthesis of albumin in inflammation. J Clin Invest. 1987;79(6):1635–1641. doi: 10.1172/JCI113000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Brenner DA, Buck M, Feitelberg SP, Chojkier M. Tumor necrosis factor-alpha inhibits albumin gene expression in a murine model of cachexia. J Clin Invest. 1990;85(1):248–255. doi: 10.1172/JCI114419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Huang J, Cheng A, Kumar R, Fang Y, Chen G, Zhu Y, Lin S. Hypoalbuminemia predicts the outcome of COVID-19 independent of age and co-morbidity. J Med Virol. 2020;92(10):2152–2158. doi: 10.1002/jmv.26003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Violi F, Cangemi R, Romiti GF, Ceccarelli G, Oliva A, Alessandri F, Pirro M, Is Albumin Predictor of Mortality in COVID-19? Antioxid Redox Signal. 2020. [DOI] [PubMed]
- 25.Li J, Li M, Zheng S, Li M, Zhang M, Sun M, Li X. et al. Plasma albumin levels predict risk for nonsurvivors in critically ill patients with COVID-19. Biomark Med. 2020;14(10):827–837. doi: 10.2217/bmm-2020-0254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.de la Rica R, Borges M, Aranda M, Del Castillo A, Socias A, Payeras A, Rialp G. et al. Low albumin levels are associated with poorer outcomes in a case series of covid-19 patients in Spain: a retrospective cohort study. Microorganisms. 2020;8(8):1106. doi: 10.3390/microorganisms8081106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Herlekar R, Sur Roy A, Matson M. Hypoalbuminaemia in COVID-19 infection: A predictor of severity or a potential therapeutic target? J Med Virol. 2021;93(1):83–84. doi: 10.1002/jmv.26151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zhang Y, Zheng L, Liu L, Zhao M, Xiao J, Zhao Q. Liver impairment in COVID-19 patients: A retrospective analysis of 115 cases from a single centre in Wuhan city, China. Liver Int. 2020;40(9):2095–2103. doi: 10.1111/liv.14455. [DOI] [PubMed] [Google Scholar]
- 29.Li T, Guo Y, Zhuang X, Huang L, Zhang X, Wei F, Yang B. Abnormal liver-related biomarkers in COVID-19 patients and the role of prealbumin. Saudi J Gastroenterol. 2020;26(5):272–278. doi: 10.4103/sjg.SJG_239_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sullivan DH, Roberson PK, Bopp MM. Hypoalbuminemia 3 months after hospital discharge: significance for long-term survival. J Am Geriatr Soc. 2005;53(7):1222–1226. doi: 10.1111/j.1532-5415.2005.53369.x. [DOI] [PubMed] [Google Scholar]
- 31.Reinhardt GF, Myscofski JW, Wilkens DB, Dobrin PB, Mangan JE Jr, Stannard RT. Incidence and mortality of hypoalbuminemic patients in hospitalized veterans. JPEN J Parenter Enteral Nutr. 1980;4(4):357–359. doi: 10.1177/014860718000400404. [DOI] [PubMed] [Google Scholar]
- 32.Sullivan DH, Roberson PK, Johnson LE, Mendiratta P, Bopp MM, Bishara O. Association between inflammation-associated cytokines, serum albumins, and mortality in the elderly. J Am Med Dir Assoc. 2007;8(7):458–463. doi: 10.1016/j.jamda.2007.04.004. [DOI] [PubMed] [Google Scholar]
- 33.Akirov A, Masri-Iraqi H, Atamna A, Shimon I. Low albumin levels are associated with mortality risk in hospitalized patients. Am J Med. 2017;130(12):1465, e1411–1465. doi: 10.1016/j.amjmed.2017.07.020. e1419. [DOI] [PubMed] [Google Scholar]
- 34.Herrmann FR, Safran C, Levkoff SE, Minaker KL. Serum albumin level on admission as a predictor of death, length of stay, and readmission. Arch Intern Med. 1992;152(1):125–130. doi: 10.1001/archinte.152.1.125. [DOI] [PubMed] [Google Scholar]
- 35.Martin GS, Moss M, Wheeler AP, Mealer M, Morris JA, Bernard GR. A randomized, controlled trial of furosemide with or without albumin in hypoproteinemic patients with acute lung injury. Crit Care Med. 2005;33(8):1681–1687. doi: 10.1097/01.CCM.0000171539.47006.02. [DOI] [PubMed] [Google Scholar]
- 36.Uhlig C, Silva PL, Deckert S, Schmitt J, de Abreu MG. Albumin versus crystalloid solutions in patients with the acute respiratory distress syndrome: a systematic review and meta-analysis. Crit Care. 2014;18(1):R10. doi: 10.1186/cc13187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Salerno F, Navickis RJ, Wilkes MM. Albumin infusion improves outcomes of patients with spontaneous bacterial peritonitis: a meta-analysis of randomized trials. Clin Gastroenterol Hepatol. 2013;11(2):123–130. doi: 10.1016/j.cgh.2012.11.007. e121. [DOI] [PubMed] [Google Scholar]
- 38.Wiedermann CJ, Joannidis M. Albumin replacement in severe sepsis or septic shock. N Engl J Med. 2014;371(1):83. doi: 10.1056/NEJMc1405675. [DOI] [PubMed] [Google Scholar]
- 39.Mani Mishra P, Uversky VN, Nandi CK. Serum albumin-mediated strategy for the effective targeting of SARS-CoV-2. Med Hypotheses. 2020;140:109790. doi: 10.1016/j.mehy.2020.109790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wiersinga WJ, Rhodes A, Cheng AC, Peacock SJ, Prescott HC. Pathophysiology, transmission, diagnosis, and treatment of coronavirus disease 2019 (COVID-19): a review. JAMA. 2020;324(8):782–793. doi: 10.1001/jama.2020.12839. [DOI] [PubMed] [Google Scholar]
- 41. CDC. COVID Data Tracker [Internet]. Centers for Disease Control and Prevention. 2020 [cited 2021 Apr 8]. Available from: https://covid.cdc.gov/covid-data-tracker.
- 42.Cavalcanti AB, Zampieri FG, Rosa RG, Azevedo LCP, Veiga VC, Avezum A, Damiani LP. et al. Hydroxychloroquine with or without Azithromycin in Mild-to-Moderate Covid-19. N Engl J Med. 2020;383(21):2041–2052. doi: 10.1056/NEJMx200021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Campochiaro C, Della-Torre E, Cavalli G, De Luca G, Ripa M, Boffini N, Tomelleri A. et al. Efficacy and safety of tocilizumab in severe COVID-19 patients: a single-centre retrospective cohort study. Eur J Intern Med. 2020;76:43–49. doi: 10.1016/j.ejim.2020.05.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Beigel JH, Tomashek KM, Dodd LE, Mehta AK, Zingman BS, Kalil AC, Hohmann E. et al. Remdesivir for the treatment of COVID-19 - final report. N Engl J Med. 2020;383(19):1813–1826. doi: 10.1056/NEJMoa2007764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.RECOVERY Collaborative Group; Horby P, Lim WS, Emberson JR, Mafham M, Bell JL, Linsell L. et al. Dexamethasone in hospitalized patients with COVID-19 - preliminary report. N Engl J Med. 2020 doi: 10.1056/NEJMoa2021436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Rosenberg ES, Dufort EM, Udo T, Wilberschied LA, Kumar J, Tesoriero J, Weinberg P. et al. Association of treatment with hydroxychloroquine or azithromycin with in-hospital mortality in patients with COVID-19 in New York State. JAMA. 2020;323(24):2493–2502. doi: 10.1001/jama.2020.8630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Li L, Zhang W, Hu Y, Tong X, Zheng S, Yang J, Kong Y. et al. Effect of convalescent plasma therapy on time to clinical improvement in patients with severe and life-threatening COVID-19: a randomized clinical trial. JAMA. 2020;324(5):460–470. doi: 10.1001/jama.2020.12607. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The database used and/or analyzed during the current study is available from the corresponding author on reasonable request.