Abstract
Objective
To examine the efficacy and safety of Ilizarov bone transport in the treatment of infected nonunion of long bones.
Methods
Patients who underwent Ilizarov bone transport for treatment of bone nonunion with chronic osteomyelitis in the three largest regional orthopedic trauma centers in China from July 2013 to July 2018 were retrospectively examined. Treatment results were evaluated with Paley’s criteria for bone healing and functional assessment.
Results
In total, 189 patients were treated during the study period. The study population comprised 135 male and 54 female patients with an average age of 37.5 years (range, 11–61 years). The patients were followed up for at least 24 months. According to Paley’s criteria for bone healing and functional assessment, the bone healing results were excellent in 115 (61%) patients, good in 31 (16%), fair in 21 (11%), and poor in 22 (12%). The functional evaluation results were excellent in 76 (40%) patients, good in 65 (34%), fair in 22 (11%), poor in 26 (14%).
Conclusion
Infected nonunion of long bones can be effectively and safely treated with Ilizarov bone transport.
Keywords: Trauma, infected nonunion, Ilizarov bone transport, distraction osteogenesis, long bones, bone nonunion
Introduction
With the rapid industrialization and increased application of heavy machinery in recent decades, the incidence of high-energy injuries from traffic and sports accidents, falls, industrial injuries, and war has been steadily on the rise. This has in turn increased the prevalence of severe soft tissue injury and open bone fracture that can develop into infectious bone nonunion.1–4 Because of the complexity of these types of trauma, infected nonunion of long bones remains a great challenge for orthopedic surgeons. The literature to date shows that 5% to 10% of fractures will eventually progress to bone nonunion.5 With the development of external fixation techniques represented by the Ilizarov technique, the treatment effect of bone nonunion has been greatly improved.6–8 From January 2013 to January 2019, 189 patients (194 limbs; five cases of bilateral tibial nonunion) were treated by Ilizarov bone transport in the authors’ medical centers. Despite the requirements for stable long-term psychological and economic support for limb salvage surgery, most patients in this case series chose limb salvage over amputation. In some cases, the components of the external fixator were maintained and recycled to increase economic sufficiency; additionally, most patients were treated in outpatient clinics after external fixation, greatly reducing the cost of hospitalization. In this study, we retrospectively analyzed the clinical efficacy of Ilizarov bone transport for the treatment of infected nonunion of long bones.
Methods
General information
All the experimental procedures were approved by the ethics committee of the First and Sixth Affiliated Hospitals of Xinjiang Medical University and The First People’s Hospital of Kashgar Area (approval number: K201902-03). All included patients provided written informed consent before the treatment, agreeing to the publication of their clinical materials provided that their identity was not revealed. All the procedures were carried out in accordance with the Declaration of Helsinki. Patients who underwent Ilizarov bone transport for treatment of infected nonunion of long bones in the three largest regional orthopedic trauma centers in China from July 2013 to July 2018 were retrospectively included in the current study.
Preoperative preparation
After admission, each patient underwent relevant routine examinations. If sinus tract secretions were present, they were collected and sent out for bacterial culture and combined drug sensitivity testing. If external fixation had been performed, the external fixation device was removed first, and antibiotics were applied empirically while waiting for the culture and drug sensitivity results. According to the results of the combined drug sensitivity test, relatively sensitive antibiotics were used to replace the previous antibiotic treatment regimen. The preoperative treatment lasted for 5 to 7 days.
Radiographs of the affected limb and healthy limb (1:1 ratio) were acquired preoperatively for surgical planning. Magnetic resonance imaging of the affected side was carried out to determine the extent of osteonecrosis and the quality of bone and soft tissues in the surgical region. An annular external fixator was used for defects of >6 cm after osteotomy, and a single-arm external fixator was used for defects of <6 cm.
Surgical procedures
Wound debridement and cleaning
After establishment of epidural anesthesia, an incision was made along the previous surgical scar and the original implants were removed. Extensive debridement was performed to remove all the necrotic bone and inflammatory tissue, which were sent out for pathological examination. The necrotic bone was excised until fresh blood at the bone end and fresh bone marrow in the medullary cavity were seen. The wounds and medullary cavity were washed with 0.02% iodophor, soaked in 0.02% iodophor for 10 to 15 minutes, and then washed repeatedly with a large amount of sterile normal saline and hydrogen peroxide.
Installation of external fixator
After thorough debridement, a circular external fixator was installed if the bone defect was >6 cm. After satisfactory adjustment of the limb force line, the circular external fixator was fixed with three to five 2.5-mm-diameter pins and two or three 4.5-mm-diameter half pins under C-arm fluoroscopy. When the bone defect was <6 cm, an Orthofix External Fixator (Orthofix, Lewisville, TX, USA) was installed with a 4.5-mm-diameter half pin. In patients with severe osteoporosis, the external fixator was fixed with a 4.5-mm hydroxyapatite half pin. During the operation, needle puncture was performed in strict accordance with the safe passage technique, and the limb force line was confirmed by C-arm fluoroscopy.
Corticotomy
The corticotomy site was decided according to the size of the bone defect, location of the lesion, and preoperative surgical design; it was located in the metaphysis in most cases. The surrounding blood vessels, nerves, and soft tissues were protected during corticotomy, which was performed with a minimally invasive drilling osteotomy device. Patients underwent single-segment (n = 63), double-segment (n = 121), or triple-segment (n = 5) corticotomy with the minimally invasive drilling osteotomy device.
Wound treatment
In 83 patients, the surgical wounds had no soft tissue defects and were sutured directly, and the negative-pressure drainage tube was removed after <5 mL of drainage per day was attained. In 106 patients, the surgical wounds had soft tissue defects and could not be directly sutured; 64 of these patients underwent open dressing changes, and 42 underwent vacuum sealing drainage. When the patient’s condition allowed, a skin flap was transferred to close the open wound.
Postoperative treatment and bone transport
Postoperative antibiotic therapy was continued for 2 to 3 weeks. The pins were disinfected with 75% alcohol twice a day until no obvious exudation was found, after which this regimen was changed to once a day or once every other day. Isometric contraction joint activity and partial weight-bearing exercises were started from the second postoperative day. Bone transfer was started an average of 10 days (range, 8–14 days) after osteotomy. The rate of bone transfer was 0.25 mm every 6 hours, which was slowed when the patient expressed discomfort. During the extension period, the general condition of the limbs was closely observed. The bone transfer was paused in cases of abnormal sensation and rapid reduction in the blood supply. A radiograph of the affected limb was reviewed once a week to observe the limb alignment and the mineralization process of the moving bone section.
Outcome assessment
According to the classification of bone healing and functioning established by Paley et al.,9 the specific evaluation criteria for bone healing were no infection, deformity of <7 degrees, and limb length discrepancy of <25 mm. According to this standard, bone union without relapsed infection, deformity of <7 degrees, and limb shortening of <25 mm was rated as excellent. Bone healing with satisfaction of any two of the three criteria was rated as good. If one of the Paley classification criteria was met, bone healing was considered acceptable; if no criteria were met, the results were considered poor. The functional evaluation criteria included five indexes: (1) obvious claudication or limb deformity, (2) stiffness of adjacent joints, (3) dystrophic soft tissue, (4) limb pain affecting activity and sleep, and (5) limb motor dysfunction. Patients who had good physical activity and none of the above five conditions were considered to have excellent function, those who had good physical activity and conditions (1) and (2) had good function, those who had good physical activity and conditions (3) and (4) had average function, and those who had serious hindrance of physical activity had poor function.
Statistical analysis
IBM SPSS Statistics for Windows, Version ≥24.0 (IBM Corp., Armonk, NY, USA) was used to analyze the correlations among the extent of lengthening, external fixation time, bone healing, and functional recovery by Spearman’s test. Differences were considered statistically significant at P < 0.05.
Results
In total, 189 patients were included in the final analysis. They comprised 135 male and 54 female patients ranging in age from 11 to 61 years, with an average age of 37.5 years (range, 11–61 years). The sites of nonunion were the femur in 41 patients, humerus in 8, and tibia in 140. The cause of the initial injury was a traffic accident in 95 cases, crush injury in 43, and falling injury in 51. The fracture type was an open fracture in 117 cases and a closed fracture in 72. The initial surgery was internal fixation in 128 cases and external fixation in 61. Ninety-three patients had a lower limb deformity and 96 had bone defects, including 76 patients with tibial bone defects and 20 patients with femoral bone defects; the mean length of the bone defects in these 96 patients was 6.1 ± 1.5 cm. The patients underwent a mean of 3.3 ± 1.2 (range, 1–6) surgeries before receiving bone transport treatment in our centers. The disease course ranged from 5 to 32 months (mean, 16.3 ± 5.5 months). A total of 105 patients had sinus tract and secretion outflow, and 84 patients had no sinus formation. The cause of infection was Staphylococcus aureus in 57 patients, Klebsiella in 13, Escherichia coli in 19, mixed bacterial infection in 20, and negative bacterial infection in 80. There were 52 smokers and 6 patients with diabetes (Table 1).
Table 1.
Patients’ basic characteristics.
| Demographics | |
|---|---|
| Male | 135 (71) |
| Age, years | 37.5 ± 13.2 |
| Site of nonunion | |
| Femur | 41 (22) |
| Humerus | 8 (4) |
| Tibia | 140 (74) |
| Primary injury | |
| Traffic accidents | 95 (50) |
| Falls | 51 (27) |
| Other crush injuries | 43 (23) |
| Type of initial fracture | |
| Open | 105 (56) |
| Closed | 72 (38) |
| Combined | 12 (6) |
| Primary fixation | |
| External fixation | 61 (32) |
| Internal fixation | 128 (68) |
| Type of bacteria | |
| Staphylococcus aureus | 57 (30) |
| Klebsiella | 13 (7) |
| Escherichia coli | 19 (10) |
| Mixed | 20 (11) |
| Negative | 80 (42) |
| Length of bone defect, cm | 6.1 ± 1.5 |
| Number of surgeries | 3.3 ± 1.2 |
| Smoker | 52 (28) |
| Diabetes | 6 (3) |
Data are presented as n (%) or mean ± standard deviation.
After the surgery, the mean duration of external fixation was 142 ± 65 days and the mean follow-up duration was 28.6 ± 7.6 months. All deformities were corrected at the time of bone healing. There were 635 pin tract infections in 84 patients, among which 140 pins in 32 patients were replaced after failure of conservative anti-bacterial treatment and dressing changes. Seventeen patients developed recurrent infection, which occurred at a mean of 3.2 ± 1.2 months after removal of the external fixator. The infection was effectively controlled by the application of antibiotics, dressing changes, or sinus removal. Seven patients had a limb length discrepancy of >2.5 cm, and no patients had residual deformity of >7 degrees. The external fixator required adjustment because of axial displacement in 15 patients. Poor distraction osteogenesis was observed in 23 patients; this was treated by slowing the speed of bone transport and encouraging the patients to perform partial weight-bearing exercises with the protection of crutches. Ninety-two patients had varying degrees of knee and ankle stiffness caused by multiple surgical scar contractures. Among the 135 male patients, 87 (54%) remained engaged in their original work, 54 (34%) needed to change their jobs, and 16 (12%) could not engage in paid work. Among the 54 female patients, 37 (71%) could normally engage in housework and 17 (29%) had difficulty in doing so. Ninety-two patients had obvious claudication, 106 had ankle or knee stiffness, and 42 had continuous pain that reduced their activity or affected their quality of sleep. Twelve patients developed a second fracture due to high-energy injury after removal of the external fixator, and they were retreated with external fixation.
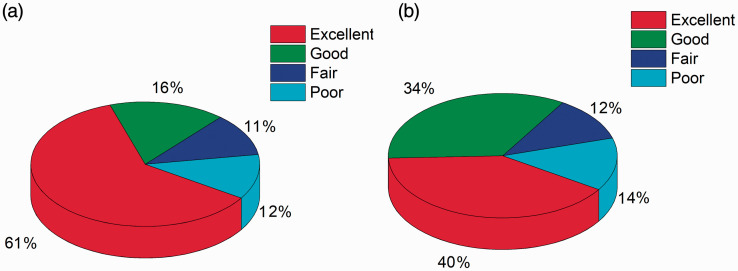
According to the bone healing evaluation criteria, the results were excellent in 115 (61%) cases, good in 31 (16%), fair in 21 (11%), and poor in 22 (12%). According to the functional evaluation criteria, the results were excellent in 76 (40%) cases, good in 65 (34%), fair in 22 (12%), and poor in 26 (14%) (Figures 1 and 2).
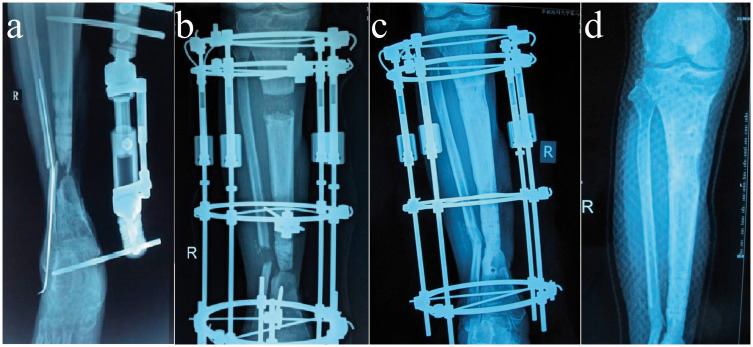
Figure 1.
Radiographs of patient who underwent Ilizarov bone transport. (a) Preoperative image and (b) 1-month, (c) 6-month, and (d) 24-month postoperative images are shown.
Figure 2.
Results of Paley classification of (a) bone healing and (b) recovery of limb function.
Discussion
This study showed that the Ilizarov bone transport technique can be an effective and safe method to treat patients with infected nonunion of long bones. The basic principles of Ilizarov bone transport include stable external fixation, anatomic realignment, low-energy corticotomy, and gradual controlled mechanical distraction to regenerate new bone/soft tissue as necessary.10,11 Previous studies have clearly shown that autogenous bone grafting after debridement significantly accelerates bone healing,12,13 whereas Ilizarov bone transport achieves osteogenesis through gradual and continuous axial distraction and compression.14–17 In our study, most patients achieved satisfactory osteogenesis after the application of Ilizarov bone transport, confirming that simple distraction provides an effective stimulus for osteogenesis. This is in accordance with the results of previous studies.18,19
The treatment of infected nonunion of long bones is still one of the most challenging problems in orthopedic clinics. However, it is apparent from our patient series that Ilizarov bone transport is an effective method for the treatment of infected nonunion of long bones. In our study, the rate of excellent and good bone healing was 77% and the rate of excellent and good functional recovery was 75%; these rates are not as high as those in previous studies.20–22 Testa et al.20 reported a 96% rate of excellent or good bone healing and an 84% rate of excellent or good functional recovery in their study. Liu et al.21 reported a 94% rate of excellent or good radiologic bone healing and a 79% rate of excellent or good functional results. Tetsworth et al.22 compared bone transport with acute shortening/lengthening in the treatment of infected (36 of 42 at the time of surgery) tibial nonunion and obtained excellent or good radiologic and functional bone healing results in 95% of the patients treated with bone transport. This might have been partly due to surgical handling and postoperative rehabilitation as well as differences in outcome assessment parameters. Notably, in severe cases of osteomyelitis, even when perfect bone healing is achieved, there is no guarantee that patients can achieve good functional recovery, partly because of the deteriorated conditions of nerves, blood vessels, and adjacent joints. However, further systemic rehabilitation treatment and a proper exercise regimen may further improve the functional outcome.
Although the present study provides further evidence of the efficacy of Ilizarov bone transport in the treatment of infected nonunion of long bones with a relatively large patient base, several limitations must be addressed. First, its retrospective nature makes it difficult to obtain more comprehensive information on patient demographics, treatment methods, and outcome assessment parameters. The included patients were treated and evaluated in different medical centers by different surgeons, which likely created inconsistent data regarding similar conditions. Well-coordinated prospective studies with larger numbers of patients are needed to further validate the results of the current study.
Conclusion
The results of our study clearly show that the Ilizarov bone transport technique is effective in treating infected nonunion of long bones.
Footnotes
Declaration of conflicting interest: The authors declare that there is no conflict of interest.
Funding: This work was supported by the Natural Science Foundation of Xinjiang, China (Grant number: 2020D01C195). The ethics approval numbers are: LFYLLSC20191231-03.
ORCID iDs: Tayierjiang Yasheng https://orcid.org/0000-0002-4868-8807
Aihemaitijiang Yusufu https://orcid.org/0000-0003-4801-3815
References
- 1.Richards RG, Verhofstad MHJ, Borens O, et al. Infection after fracture fixation: current surgical and microbiological concepts. Injury 2018; 49: 511–522. [DOI] [PubMed] [Google Scholar]
- 2.Rollo G, Falzarano G, Ronga M, et al. Challenges in the management of floating knee injuries: results of treatment and outcomes of 224 consecutive cases in 10 years. Injury 2019; 50: S30–S38. [DOI] [PubMed] [Google Scholar]
- 3.Fortina M, Maniscalco P, Carulli C, et al. Jockey injuries during the Siena “Palio.” A 72-year analysis of the oldest horse race in Italy. Injury 2019; 50: S56–S59. [DOI] [PubMed] [Google Scholar]
- 4.Grubor P, Milicevic S, Grubor M, et al. Treatment of bone defects in war wounds: retrospective study. Med Arch 2015; 69: 260–264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ekegren CL, Edwards ER, De Steiger R, et al. Incidence, costs and predictors of non-union, delayed union and mal-union following long bone fracture. Int J Environ Res Public Health 2018; 15: 2845. doi: 10.3390/ijerph15122845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Grubor P, Falzarano G, Grubor M, et al. Treatment of the chronic war tibial osteomyelitis, Gustilo type IIIB and Cierny-Mader IIIB, using various methods. A retrospective study. EMBJ 2014; 9: 7–18. [Google Scholar]
- 7.Grubor P, Mitković M, Grubor M, et al. Biomechanical stability of juvidur and bone models on osteosyntesic materials. Acta Inform Med 2016; 24: 261–265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bisaccia M, Rinonapoli G, Meccariello L, et al . The challenges of monoaxial bone transport in orthopedics and traumatology. Ortop Traumatol Rehabil 2017; 19: 373–378. [DOI] [PubMed] [Google Scholar]
- 9.Paley D, Catagni MA, Argnani F, et al . Ilizarov treatment of tibial nonunions with bone loss. Clin Orthop Relat Res 1989; 241: 146–165. [PubMed] [Google Scholar]
- 10.Ilizarov GA. The principles of the Ilizarov method. Bull Hosp Jt Dis Orthop Inst 1988; 48: 1–11. [PubMed] [Google Scholar]
- 11.Zhang Q, Zhang W, Zhang Z, et al. Femoral nonunion with segmental bone defect treated by distraction osteogenesis with monolateral external fixation. J Orthop Surg Res 2017; 12: 183. doi: 10.1186/s13018-017-0684-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Patzakis MJ, Zalavras CG. Chronic posttraumatic osteomyelitis and infected nonunion of the tibia: current management concepts. J Am Acad Orthop Surg 2005; 13: 417–427. doi: 10.5435/00124635-200510000-00006. [DOI] [PubMed] [Google Scholar]
- 13.Pace F, Randelli F, Ayeni OR, et al. Debridement, internal fixation and staged autogenous bone graft for the management of infected femoral non-union. Injury 2018; 49: S48–S57. [DOI] [PubMed] [Google Scholar]
- 14.Lavini F, Dall’Oca C, Bartolozzi P. Bone transport and compression-distraction in the treatment of bone loss of the lower limbs. Injury 2010; 41: 1191–1195. [DOI] [PubMed] [Google Scholar]
- 15.Krishnan A, Pamecha C, Patwa JJ. Modified Ilizarov technique for infected nonunion of the femur: the principle of distraction-compression osteogenesis. J Orthop Surg (Hong Kong) 2006; 14: 265–272. [DOI] [PubMed] [Google Scholar]
- 16.Rollo G, Luceri F, Falzarano G, et al. Effectiveness of teriparatide combined with the Ilizarov technique in septic tibial non-union. Med Glas (Zenica) 2021; 18. doi: 10.17392/1280-21. [DOI] [PubMed] [Google Scholar]
- 17.Ripani U, Manzarbeitia-Arroba P, Guijarro-Leo S, et al. Vitamin C may help to reduce the knee's arthritic symptoms. Outcomes assessment of nutriceutical therapy. Med Arch 2019; 73: 173–177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Azzam W, El-Sayed M. Ilizarov distraction osteogenesis over the preexisting nail for treatment of nonunited femurs with significant shortening. Eur J Orthop Surg Traumatol 2016; 26: 319–328. [DOI] [PubMed] [Google Scholar]
- 19.Catagni MA, Guerreschi F, Lovisetti L. Distraction osteogenesis for bone repair in the 21st century: lessons learned. Injury 2011; 42: 580–586. [DOI] [PubMed] [Google Scholar]
- 20.Testa G, Vescio A, Aloj DC, et al. Treatment of infected tibial non-unions with Ilizarov technique: a case series. J Clin Med 2020; 9: 1352. doi: 10.3390/jcm9051352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Liu Y, Yushan M, Liu Z, et al. Complications of bone transport technique using the Ilizarov method in the lower extremity: a retrospective analysis of 282 consecutive cases over 10 years. BMC Musculoskelet Disord 2020; 21: 354. doi: 10.1186/s12891-020-03335-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tetsworth K, Paley D, Sen C, et al. Bone transport versus acute shortening for the management of infected tibial non-unions with bone defects. Injury 2017; 48: 2276–2284. [DOI] [PubMed] [Google Scholar]