Abstract
Objective
To determine whether a healthful plant-based diet is related to lower stroke risk, we examined the associations of plant-based diet quality with risk of total, ischemic, and hemorrhagic stroke.
Methods
The participants were 73,890 women in Nurses' Health Study (NHS; 1984–2016), 92,352 women in NHSII (1991–2017), and 43,266 men in Health Professionals Follow-Up Study (1986–2012) without cardiovascular disease and cancer at baseline. Plant-based diet quality was evaluated by the overall plant-based diet index (PDI), the healthful PDI (hPDI), and the unhealthful PDI (uPDI). Participants who reported that their meat and/or fish intakes were 0 or <1 serving per month were categorized as vegetarians, and others were classified as nonvegetarians. Strokes with available medical records were subtyped as ischemic or hemorrhagic.
Results
During the follow-up, 6,241 total stroke cases (including 3,015 ischemic and 853 hemorrhagic strokes) were documented. Compared to participants with the lowest PDIs, among participants with the highest PDIs, the hazard ratios (HRs) for total stroke were 0.94 (95% confidence interval 0.86–1.03) for PDI, 0.90 (0.83–0.98) for hPDI, and 1.05 (0.96–1.15) for uPDI. Participants in the highest hPDI showed marginally lower HR for ischemic stroke (0.92 [0.82–1.04]) and no consistent associations for hemorrhagic stroke. We observed no association between a vegetarian diet and total stroke (1.00 [0.76–1.32]), although the number of cases was small.
Conclusion
Lower risk of total stroke was observed by those who adhered to a healthful plant-based diet.
Plant-based diets have been reported to lower the risk of diabetes and cardiovascular disease (CVD).1–4 However, few studies examined whether plant-based diets were related to the risk of stroke, particularly different types of stroke, and the results of previous studies were inconsistent. Although our previous study reported an inverse association between a healthful plant-based diet and the risk of CVD, including total stroke,5 a recent article from the European Prospective Investigation Into Cancer and Nutrition (EPIC)–Oxford study showed the higher risk of total and hemorrhagic stroke among vegetarians.6
Previous research on plant-based diets was somewhat limited because most studies focused on vegetarian diets, without differentiation for the quality of plant-based foods. Therefore, we developed 3 plant-based diet indices—the overall plant-based diet index (PDI), the healthful PDI (hPDI), and the unhealthful PDI (uPDI)—to evaluate the quality of plant foods intake without excluding all animal foods.7,8 In this study, we conducted a comprehensive analysis on the each association of PDI, hPDI, and uPDI with the risk of total, ischemic, and hemorrhagic stroke among participants in 3 large US cohorts: the Nurses' Health Study (NHS), the NHSII, and the Health Professionals Follow-Up Study (HPFS), hypothesizing that hPDI would be related to the lower risk of stroke. We also categorized participants with vegetarian diets and assessed whether vegetarians have the higher risk of stroke. To the best of our knowledge, the current study is the first study to evaluate the associations between the plant-based diet quality and risk of different types of stroke.
Methods
Study Population and Design
The NHS started with 121,700 female married nurses who were 30 to 55 years old in 1976. The NHSII started with 116,429 female nurses who were 25 to 42 years old in 1989. The HPFS began among 51,529 male health professionals in the United States who were 40 to 75 years old in 1986. Questionnaires are mailed to participants every 2 years to request information on lifestyle factors and medical history during the most recent follow-up period, with follow-up rates exceeding 90%.9,10
Exclusion criteria for the current study included a history of CVD or cancer at baseline, missing dietary data, or implausible dietary energy intakes (<800 or >4,200 kcal/d in HPFS and <600 or >3,500 kcal/d in NHS and NHS11). A total of 73,890 women in the NHS (baseline 1984), 92,352 women in the NHSII (baseline 1991), and 43,266 men in the HPFS (baseline: 1986) were included in our analyses.
Standard Protocol Approvals, Registrations, and Patient Consents
All research described was approved by the institutional review boards of the Brigham and Women's Hospital and the Harvard T. H. Chan School of Public Health. The return of the questionnaires was regarded as implying informed consent.
Exposure Assessment
Every 2 to 4 years, dietary information was collected with a semiquantitative food frequency questionnaire (FFQ) containing >110 food items that have been highly validated.11,12 The FFQ asks participants to report how frequently, on average, they had eaten a specified portion of each food during the past year. Detailed methods to create the PDIs were previously reported.7,8,13 In brief, all food items were first divided into 18 food groups. Then, these groups were classified into 3 classes: healthy plant foods, less healthy plant foods, and animal foods.7,8,13 The food groups in each category are shown in table 1. Several foods that crossed categories (e.g., pizza and chowder) were categorized into the animal food group because they contain a substantial amount of animal products. Intake of the 18 food groups (measured in servings per day) was categorized into quintiles (Qs), and each was given a scored from 1 to 5. To create the PDI, both the healthy and the less healthy plant groups were scored positively (Q1 = 1, Q5 = 5), and the animal group was scored inversely (Q5 = 1, Q1 = 5). For calculating the hPDI, positive scores (Q5 = 5) were assigned to the healthy plant group, and inverse scores (Q5 = 1) were given to the less healthy plant foods and animal foods. For developing uPDI, the less healthy plant group was scored positively (Q5 = 5), and the healthy plant and the animal groups were scored inversely (Q5 = 1).7,8,13 Because of the different associations between alcohol intake and health outcomes, alcohol was not included in the food groups but was included as a covariate. Similarly, because the composition of fatty acids in margarine changed over time, we included margarine intake as a covariate. Last, we added the scores of the 18 food groups to calculate the 3 plant-based diet indices (range 18–90).13
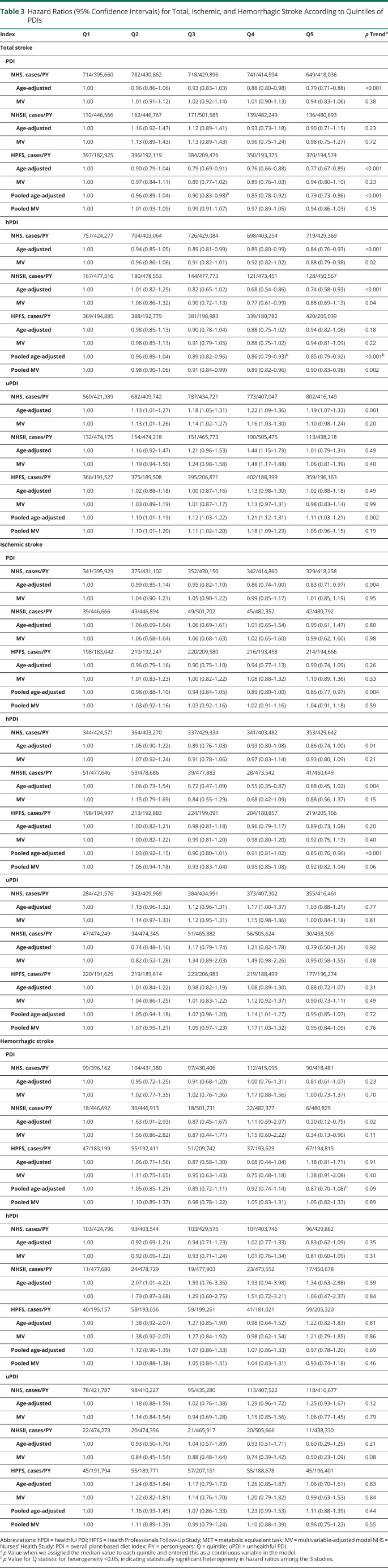
Table 3.
Hazard Ratios (95% Confidence Intervals) for Total, Ischemic, and Hemorrhagic Stroke According to Quintiles of PDIs
In addition, we determined vegetarians and nonvegetarians on the basis of the FFQ information from every dietary assessment. Specifically, we defined vegetarians as participants who consumed plant foods or other animal foods such as butter, dairy, or eggs but reported that their meat and/or fish intakes were 0 or <1 serving per month (the lowest category available in the FFQ response options). Thus, the definition of vegetarians in our cohorts was essentially lacto-ovo-vegetarians. Other participants were defined as nonvegetarians. To check misclassification, we confirmed that the total energy intakes in vegetarians were plausible on each dietary assessment in all cohorts (600–3,500 kcal/d in women and 800–4,200 kcal/d in men).
Ascertainment of Stroke
Stroke was classified as total stroke, ischemic stroke (including thrombotic, embolic, or unspecified nonhemorrhagic stroke), or hemorrhagic stroke (containing subarachnoid or intraparenchymal stroke) according to criteria in the National Survey of Stroke.14 Participants who reported an incident stroke were asked to provide additional detail by letter/interview and were asked for permission to obtain medical records to confirm their diagnosis of stroke by study physicians. The nonfatal stroke cases that were substantiated by letter/interview and but lacked adequate medical documentation were considered probable cases. Fatal events were recognized by reports from family, by the US Postal Service, or by search of the National Death Index, and 98% of the deaths in each cohort were ascertained.15 Confirmation of fatal stroke cases relied on death certificates, medical records during hospitalization, or autopsy records. Both confirmed stroke cases and probable stroke cases were included.
Ascertainment of Covariates
We collected data on weight, smoking, physical activity, the use of aspirin and multivitamin, physician diagnosis of chronic diseases, and medication through the biennial self-reported questionnaires. For female participants, information was queried on their menopausal status, the use of postmenopausal hormone therapy, and oral contraceptives (NHSII only). The validity for collecting the information on body weight and physical activity was described in detail in the previous publications.16,17
Statistical Analysis
We categorized PDI, hPDI, and uPDI into quintiles from the lowest score (Q1) to the highest score (Q5) for each of the dietary assessments conducted every 2 to 4 years. For each 2-year follow-up time period, the most recent assessment was used (simple update method). By using age-adjusted Cox proportional hazards regression, we estimated the associations between PDI, hPDI, uPDI, and stroke risk, updated with information from the most recent FFQ. Person-time was determined from the questionnaire return date to the diagnosis of stroke, death, or the end of follow-up (June 30, 2016, in the NHS; June 30, 2017, in the NHSII; and January 1, 2012, in the HPFS), whichever occurred first. In the multivariable-adjusted model, we adjusted for race (self-reported) and time-varying covariates such as physical activity, alcohol consumption, margarine, total energy intake, smoking, aspirin use, multivitamin use, body mass index (BMI), postmenopausal hormone therapy (for women), oral contraceptives (NHSII), time-varying information on hypertension, hypercholesterolemia, diabetes, antihypertensive use, and anticholesterol medication use. The median value for each quintile was used to test for trends across quintiles. We estimated the risk of stroke per 10-point increase in PDIs by handling the scores as continuous variables. We also evaluated the risk of stroke in vegetarians compared to nonvegetarians.
Several sensitivity analyses were performed to assess the stability of our findings. First, we performed 4-year lag analyses to minimize reverse causation due to existing diseases. Second, we conducted subgroup analyses and assessed statistical interactions according to several potential effect modifiers (age, sex, BMI, smoking, hypertension, and hypercholesterolemia). Third, we examined the associations between food categories (healthy plant food group, less healthy plant food group, and animal food group) and stroke risk by entering the 3 food groups simultaneously into models instead of PDIs. Last, we further adjusted for hypoglycemic medication use, although the information was limited (the assessment was started in 1988 for the NHS and 1989 for the NHSII and was available only in 2008 for the HPFS).
Analyses were executed separately for each cohort (NHS, NHSII, and HPFS), and fixed-effects meta-analysis with inverse variance weighting was used to estimated total associations. However, we pooled the data for the subgroup analysis for sex. SAS for UNIX version 9.4 (SAS Institute Inc, Cary, NC) was used for all analyses. Statistical testing was 2 sided, and values of p < 0.05 were considered statistically significant.
Data Availability
The dataset analyzed in this study is not publicly available, but further information about the dataset can be obtained from the NHS; formal review processes exist for request of datasets.
Results
Participant Characteristics
The baseline attributes of participants and their intakes of each food group with the lowest and highest quintiles of PDI, hPDI, and uPDI are shown in table 2. In all cohorts, participants with the highest PDI had lower BMI, had higher physical activity, were less likely to smoke, had higher healthy and less healthy plant foods intake, and had lower animal foods intake compared to participants with the lowest PDI scores (table 1). Participants with the highest quintile of hPDI scores were older; had lower BMI, higher physical activity, and a higher prevalence of comorbid conditions (elevated cholesterol, diabetes, and hypertension); were less likely to smoke; had higher healthy plant foods intake; and had lower less healthy plant foods and animal foods intake compared to participants with the lowest hPDI scores (table 2). Participants with the highest uPDI scores were younger, had lower physical activity, were more likely to smoke, had higher less healthy plant foods intake, and had lower healthy plant foods and animal foods intake compared to participants with the lowest uPDI scores (table 2).
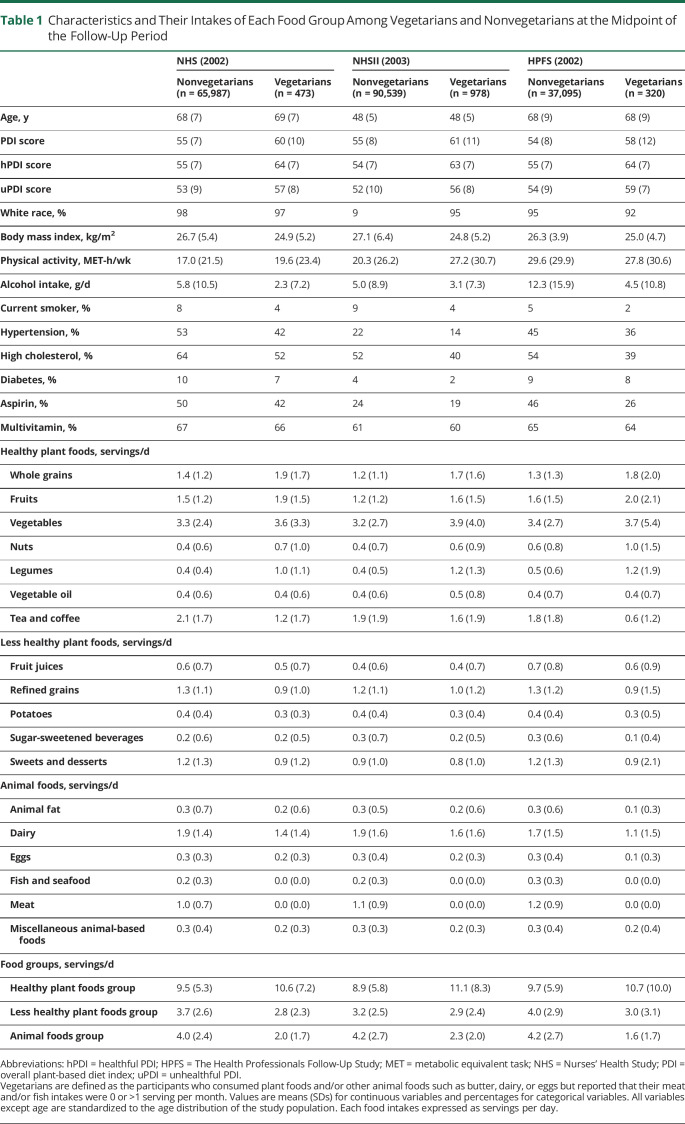
Table 1.
Characteristics and Their Intakes of Each Food Group Among Vegetarians and Nonvegetarians at the Midpoint of the Follow-Up Period
In the NHS, over 2,089,048 person-years of follow-up, 3,604 total strokes (1,739 ischemic and 502 hemorrhagic strokes) were documented. In the NHSII, during 2,357,860 person-years of follow-up, 740 total strokes (218 ischemic and 94 hemorrhagic strokes) were documented. In the HPFS, over 2,357,860 person-years of follow-up, 1,897 total strokes (1,058 ischemic and 257 hemorrhagic strokes) were documented.
Plant-Based Diet Quality and Risk of Stroke
In pooled multivariable analyses, participants with the highest PDI scores (quintile 5) showed a marginally lower hazard ratio (HR) of total stroke (0.94 [95% confidence interval (CI) 0.86–1.03]) compared to those in the lowest quintile (table 3). Participants with the highest hPDI had a significantly lower HR (0.90 [0.83–0.98]) for total stroke, whereas those with the highest uPDI showed a marginally higher HR (1.05 [0.96–1.15]) (table 3). For ischemic stroke, the pooled multivariable HRs comparing the extreme quintiles of diet indices were 1.04 (0.91–1.18) for PDI, 0.92 (0.82–1.04) for hPDI, and 0.96 (0.84–1.09) for uPDI (table 3). No association between PDIs and hemorrhagic stroke was observed (table 3). For 10-point increases in PDI and hPDI, total stroke risk was lower by 4% (0%–7%, p = 0.08) and 5% (2%–9%, p = 0.005), respectively. In contrast, for each 10-point increase in uPDI, the HR for stroke was 3% higher (−1% to 6%, p = 0.12) (figure 1).
Table 2.
Baseline Characteristics of Participants With Lowest and Highest Quintiles of Overall PDI, hPDI, and uPDI Scores
Figure 1. Hazard Ratios for Total and Subtypes of Stroke per 10-Point Increases in PDIs.

Multivariable-adjusted hazard ratios and 95% confidence intervals (CIs) per 10-point increases in the overall plant-based diet index (PDI), healthful PDI (hPDI), and unhealthful PDI (uPDI) were calculated by pooling across the 3 cohorts with a fixed-effects model, adjusted for age, smoking status, alcohol intake, physical activity, multivitamin use, aspirin use, margarine intake, total energy intake, body mass index, postmenopausal hormone use (Nurses' Health Study [NHS] and NHSII), oral contraceptive use (NHSII), hypertension, hypercholesterolemia, diabetes, antihypertensive use, and anticholesterol medication use shown. Error bars represent 95% CIs.
Characteristics of a Vegetarian Diet and Risk of Total Stroke
Based on the information on each FFQ (every 2–4 years), the percentages of vegetarians who were classified on the FFQ every 2 to 4 years tended to increase over the follow-up period, from 0.3% (1984) to 0.8% (2014) in the NHS, 0.7% (1991) to 1.6% (2015) in the NHSII, and 0.5% (1986) to 1.2% (2010) in the HPFS. Therefore, we showed the characteristics and intakes of each food groups among vegetarians and nonvegetarians at the midpoint of the follow-up (table 1). In all cohorts, vegetarians tended to have a lower BMI, lower alcohol intake, and lower current smoking prevalence and had a lower prevalence of comorbid conditions. Vegetarians also had higher PDI and hPDI scores; higher consumption of whole grains, fruits, nuts, vegetables, and legumes; and lower consumption of tea/coffee and processed grains than nonvegetarians (table 1). In the pooled multivariable analyses, we did not observe associations between a vegetarian diet (updated at each FFQ) and total stroke risk (HR [95% CI] 1.00 [0.76–1.32), although the estimates were imprecise due to small case numbers (table 4). Given the small number of cases, we did not examine risk of stroke subtypes.
Table 4.
Hazard Ratios (95% Confidence Intervals) for Total Stroke Comparing Vegetariansa and Nonvegetarians

Food Intake and Stroke Risk
When intakes of servings of the 3 food groups (healthy plant foods, less healthy plant foods, and animal foods) were used in placed of PDIs in multivariate models, those in the highest quintile of healthy plant foods showed a marginally lower total stroke risk (HR [95% CI] 0.93 [0.85–1.02]), while participants with the highest animal foods intake had a marginally higher risk (1.07 [0.97–1.18]) compared to participants with the lowest corresponding foods intake (figure 2). We found no associations between less healthy plant food intake and total stroke risk.
Figure 2. HRs (95% Confidence Intervals) for Total Stroke According to Quintiles of the Intakes of Heathy Plant Food, Less Healthy Plant Food, and Animal Food.
Results were pooled across the 3 cohorts using a fixed-effects model. Error bars represent 95% confidence intervals (CIs). HR = hazard ratio; Q = quintile.
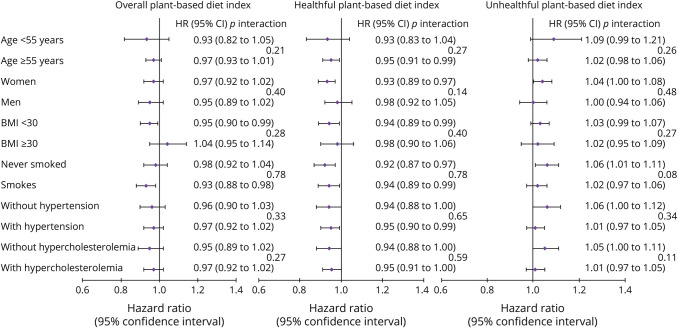
Sensitivity Analyses
The associations between hPDI and stroke risk persisted when we excluded strokes that occurred in the first 4 years (pooled HR corresponding to a 10-point increase in hPDI 0.95 [95% CI 0.91–0.99]) and when we stratified by major confounding factors (age, sex, BMI, smoking status, hypertension, and hypercholesterolemia, figure 3). Although a 10-point hPDI increase was more strongly related to lower stroke risk among female participants (HR [95% CI] 0.93 [0.89–0.97]), participants with BMI <30 kg/m2 (0.94 [0.89–0.99]), and never smokers (0.92 [0.87–0.97]), all p values for interaction were ≥0.14 (figure 3). Furthermore, with additional inclusion of hypoglycemic drug use in the models, the pooled HRs for stroke (comparing the extreme quintiles) remained the same (0.94 [0.86–1.03] for PDI, 0.90 [0.83–0.98] for hPDI, and 1.05 [0.96–1.15] for uPDI).
Figure 3. Subgroup Analyses Between 10-Point Increases in Plant-Based Diet Indices and Risk of Total Stroke.
Error bars represent 95% confidence intervals (CIs). Results were pooled across the 3 cohorts using a fixed-effects model. Error bars represent 95% CIs. BMI = body mass index; HR = hazard ratio.
Discussion
In the 3 US large prospective cohorts, we found that a healthful plant-based diet was significantly associated with a 10% lower total stroke risk (comparing highest and lowest quintiles of hPDI, 95% CI 2%–17%) and marginally lower ischemic stroke risk (HR [95% CI] 0.92 [0.82–1.04]). We did not observe any associations between plant-based indices and hemorrhagic stroke. There was no consistent evidence for an association of vegetarian diet with risk of total stroke, although the case numbers were small.
Previous reports that analyzed the association of plant-based diets with stroke have been inconclusive.5,6,18–20 Two previous studies including EPIC-Oxford data found no association between the intake of vegetarian diets and risk of stroke mortality, which is consistent with our previous study of changes in PDIs and total and cause-specific mortality.13,18,19 In contrast, a recent article from the EPIC-Oxford study reported that individuals with vegetarian diets had higher HRs of total and hemorrhagic stroke (1.20 [95% CI 1.02–1.40] and 1.43 [1.08–1.90], respectively),6 whereas the prospective cohort studies in Taiwan showed inverse associations between vegetarian diets and lower ischemic and hemorrhagic stroke risk.20 Our recent study that included the NHS, NHSII, and HPFS also reported the association of a healthful plant-based diet with lower total stroke risk.5
Therefore, in this study, we comprehensively analyzed the associations of 3 plant-based diet indices with the risk of total, ischemic, and hemorrhagic stroke and additionally tested the association of a vegetarian diet with stroke risk. A healthful plant-based diet was significantly associated with lower total stroke risk and was not associated with hemorrhagic stroke, and a vegetarian diet was not associated with risk of total stroke. These discrepancies may be attributed to differences in the quality of plant-based foods that the participants consumed. A vegetarian diet with higher intakes of unhealthy plant-based foods (such as refined grains and added sugars and fats) than intakes of whole foods would be unlikely to yield maximal health benefit; this difference in the plant food quality may explain the prior inconsistent results.5,6,18–20 In line with the finding of a lower stroke risk with a higher hPDI, a meta-analyses using 20 prospective cohort studies showed a 21% lower stroke risk (95% CI 16%–25%) comparing the highest and lowest consumption of fruits and vegetables.21 Another recent meta-analysis of carbohydrate quality found that intake of carbohydrates with a lower glycemic index such as whole grains and dietary fibers was related to a 33% lower stroke mortality and 26% lower total stroke incidence compared with carbohydrates with a higher glycemic index (high intakes of refined grains and sugars).22 The consistent opposite associations of hPDI and uPDI in our analyses also highlight the importance of considering plant-based dietary quality and should focus attention on increasing healthy plant foods consumption and decreasing the unhealthy plant foods intake. Our findings have important public health implications in that future nutrition policies to lower stroke risk should consider the plant-based foods quality.
Another advantage of hPDI, which is different from a vegetarian diet, is that our hPDI represents a diet without entire exclusion of animal-based foods intake. For example, our previous study showed that a 10-point increase in hPDI can be achieved by increasing intakes of fruits, vegetables, or whole grains by 3 servings per day and decreasing intakes of refined grains, added sugars, or red meats by 2 servings per day.13 Such an approach is desirable because of the flexibility and because individuals are allowed to change their diets gradually. In addition, excluding all animal foods might not be appropriate for all populations because some animal foods intake such as fish and dairy were reported to be associated with lower stroke risk.23,24 Furthermore, diets based entirely on plant foods may lead to deficiencies in nutrients such as vitamin B12 that might negate the benefits of a vegetarian diet.25,26 In our analyses, we classified vegetarians as participants whose meat/fish intake was >1 serving per month based on the lowest intake category on our FFQ and data was updated every 2 to 4 years, while the EPIC-Oxford study identified meat eaters, fish eaters, and vegetarians directly on a its questionnaire by asking whether they ate any meat and/or fish at baseline and assessed this again ≈10 years later.6 In addition to the small number of vegetarians in the current study, there is a possibility that vegetarians in our study consumed a small amount of meat and/or fish (<1 serving per month). These differences might partly explain the differences in the associations of a vegetarian diet with stroke risk between the previous study and our study.
We previously reported that several dietary patterns such as the prudent pattern, the Dietary Approaches to Stop Hypertension, and the Alternate Mediterranean Diet were associated with a lower stroke risk.27–29 Although a healthful plant-based diet is close to these diets, our PDIs differ from other diets by the focus on the quality of plant-based foods. Because the PDI, hPDI, and uPDI all assign negative scores to animal-based foods, hPDI reflects the effect of high plant-based diet quality (higher consumption of healthy plant foods), while uPDI reflects the impact of low plant-based diet quality (high intakes of less healthy plant foods). Examining how the plant-based dietary quality is related to stroke risk is essential, especially given the increasing interest in plant-based diets for both health outcomes and environmental sustainability.30
This study has several strengths, including the prospective study design with long-term follow-up, the large size of the cohorts, the robust number of stroke cases, the high rate of follow-up, repeated dietary measurements, and the evaluation of quality of plant-based foods. However, several limitations should be noted. First, all participants in this study were health professionals and were predominantly non-Hispanic White, limiting generalizability. Second, although many lifestyle factors were controlled for and participants with CVD, cancer, or implausible energy intakes were excluded, residual confounding cannot be completely excluded. Third, the indices were based on self-reported dietary intake, which may produce measurement errors. Therefore, misclassification may have underestimated the true strength of the associations; however, the FFQs have been highly validated.11,12 Fourth, although we have adjusted for the development of hypertension, hypercholesterolemia, and diabetes and the use of medications for these conditions, we did not adjust for systolic blood pressure, lipid levels, or glucose levels because we do not have these available in most of the participants. Fifth, because of the low prevalence of vegetarians, the statistical power for the analysis of vegetarian diets was low. Last, the 38% of patients with stroke in this study had no information of stroke subtypes, which limited the precision of associations with ischemic and hemorrhagic stroke risk. Because the number of cases in each quintile differed between the dietary patterns, statistical variation might explain why the point estimates of HRs for ischemic stroke subtypes were slightly higher in participants with the highest PDI than in those with the highest uPDI in this study; all of these associations were nonsignificant with wide CIs.
A healthful plant-based diet was significantly associated with a lower total stroke risk, and we found no stroke-related harm from a vegetarian diet. Our results support dietary guidelines that emphasize increasing consumption of healthy plant-based foods for cardiometabolic health outcomes.
Glossary
- BMI
body mass index
- CI
confidence interval
- CVD
cardiovascular disease
- EPIC
European Prospective Investigation Into Cancer and Nutrition
- FFQ
food frequency questionnaire
- hPDI
healthful PDI
- HPFS
Health Professionals Follow-Up Study
- HR
hazard ratio
- NHS
Nurses' Health Study
- PDI
plant-based diet index
- Q
quintile
- uPDI
unhealthful PDI
Appendix. Authors

Study Funding
Funded by grants UM1 CA186107, U01 CA176726, U01 CA167552, R01 HL034594, R01 HL088521, and R01 HL35464 from the NIH. M.Y.B. was supported by a fellowship from the Manpei Suzuki Diabetes Foundation. F.B.H. was supported by grants HL60712, HL118264, and DK112940 from the NIH.
Disclosure
Megu Y. Baden, Zhilei Shan, and Fenglei Wang report no disclosures. Yanping Li reports research support from the California Walnut Commission, outside the submitted manuscript. JoAnn E. Manson, Eric B. Rimm, and Walter C Willett report no disclosures. Frank B. Hu reports research support from the California Walnut Commission, honorariums from Diet Quality Photo Navigation, and honorariums for lectures from Metagenics and Standard Process, outside the submitted manuscript. Kathryn M. Rexrode reports no disclosures. Go to Neurology.org/N for full disclosures.
References
- 1.Huang T, Yang B, Zheng J, Li G, Wahlqvist ML, Li D. Cardiovascular disease mortality and cancer incidence in vegetarians: a meta-analysis and systematic review. Ann Nutr Metab 2012;60:233–240. [DOI] [PubMed] [Google Scholar]
- 2.Kwok CS, Umar S, Myint PK, Mamas MA, Loke YK. Vegetarian diet, Seventh Day Adventists and risk of cardiovascular mortality: a systematic review and meta-analysis. Int J Cardiol 2014;176:680–686. [DOI] [PubMed] [Google Scholar]
- 3.Tonstad S, Stewart K, Oda K, Batech M, Herring RP, Fraser GE. Vegetarian diets and incidence of diabetes in the Adventist Health Study-2: nutrition, metabolism, and cardiovascular diseases. Nutr Metab Cardiovasc Dis 2013;23:292–299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yokoyama Y, Nishimura K, Barnard ND, et al. Vegetarian diets and blood pressure: a meta-analysis. JAMA Intern Med 2014;174:577–587. [DOI] [PubMed] [Google Scholar]
- 5.Shan Z, Li Y, Baden MY, et al. Association between healthy eating patterns and risk of cardiovascular disease. JAMA Intern Med 2020;180:1090–1100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tong TYN, Appleby PN, Bradbury KE, et al. Risks of ischaemic heart disease and stroke in meat eaters, fish eaters, and vegetarians over 18 years of follow-up: results from the prospective EPIC-Oxford study. BMJ 2019;366:l4897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Satija A, Bhupathiraju SN, Rimm EB, et al. Plant-based dietary patterns and incidence of type 2 diabetes in US men and women: results from three prospective cohort studies. PLoS Med 2016;13:e1002039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Satija A, Bhupathiraju SN, Spiegelman D, et al. Healthful and unhealthful plant-based diets and the risk of coronary heart disease in U.S. adults. J Am Coll Cardiol 2017;70:411–422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Colditz GA, Manson JE, Hankinson SE. The Nurses' Health Study: 20-year contribution to the understanding of health among women. J Womens Health 1997;6:49–62. [DOI] [PubMed] [Google Scholar]
- 10.Rimm EB, Giovannucci EL, Willett WC, et al. Prospective study of alcohol consumption and risk of coronary disease in men. Lancet 1991;338:464–468. [DOI] [PubMed] [Google Scholar]
- 11.Willett WC, Sampson L, Stampfer MJ, et al. Reproducibility and validity of a semiquantitative food frequency questionnaire. Am J Epidemiol 1985;122:51–65. [DOI] [PubMed] [Google Scholar]
- 12.Yuan C, Spiegelman D, Rimm EB, et al. Relative validity of nutrient intakes assessed by questionnaire, 24-hour recalls, and diet records as compared with urinary recovery and plasma concentration biomarkers: findings for women. Am J Epidemiol 2018;187:1051–1063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Baden MY, Liu G, Satija A, et al. Changes in plant-based diet quality and total and cause-specific mortality. Circulation 2019;140:979–991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Walker AE, Robins M, Weinfeld FD. The National Survey of Stroke: clinical findings. Stroke 1981;12:I13–I44. [PubMed] [Google Scholar]
- 15.Rich-Edwards JW, Corsano KA, Stampfer MJ. Test of the National Death Index and Equifax Nationwide Death Search. Am J Epidemiol 1994;140:1016–1019. [DOI] [PubMed] [Google Scholar]
- 16.Rimm EB, Stampfer MJ, Colditz GA, Chute CG, Litin LB, Willett WC. Validity of self-reported waist and hip circumferences in men and women. Epidemiology 1990;1:466–473. [DOI] [PubMed] [Google Scholar]
- 17.Chasan-Taber S, Rimm EB, Stampfer MJ, et al. Reproducibility and validity of a self-administered physical activity questionnaire for male health professionals. Epidemiology 1996;7:81–86. [DOI] [PubMed] [Google Scholar]
- 18.Key TJ, Fraser GE, Thorogood M, et al. Mortality in vegetarians and nonvegetarians: detailed findings from a collaborative analysis of 5 prospective studies. Am J Clin Nutr 1999;70:516s–524s. [DOI] [PubMed] [Google Scholar]
- 19.Orlich MJ, Singh PN, Sabaté J, et al. Vegetarian dietary patterns and mortality in Adventist Health Study 2. JAMA Intern Med 2013;173:1230–1238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chiu THT, Chang HR, Wang LY, Chang CC, Lin MN, Lin CL. Vegetarian diet and incidence of total, ischemic, and hemorrhagic stroke in 2 cohorts in Taiwan. Neurology 2020;94:e1112–e1121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hu D, Huang J, Wang Y, Zhang D, Qu Y. Fruits and vegetables consumption and risk of stroke: a meta-analysis of prospective cohort studies. Stroke 2014;45:1613–1619. [DOI] [PubMed] [Google Scholar]
- 22.Reynolds A, Mann J, Cummings J, Winter N, Mete E, Te Morenga L. Carbohydrate quality and human health: a series of systematic reviews and meta-analyses. Lancet 2019;393:434–445. [DOI] [PubMed] [Google Scholar]
- 23.Larsson SC, Orsini N. Fish consumption and the risk of stroke: a dose-response meta-analysis. Stroke 2011;42:3621–3623. [DOI] [PubMed] [Google Scholar]
- 24.Alexander DD, Bylsma LC, Vargas AJ, et al. Dairy consumption and CVD: a systematic review and meta-analysis. Br J Nutr 2016;115:737–750. [DOI] [PubMed] [Google Scholar]
- 25.Rizzo G, Laganà AS, Rapisarda AM, et al. Vitamin B12 among vegetarians: status, assessment and supplementation. Nutrients 2016;8:767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pawlak R. Is vitamin B12 deficiency a risk factor for cardiovascular disease in vegetarians?. Am J Prev Med 2015;48:e11–e26. [DOI] [PubMed] [Google Scholar]
- 27.Fung TT, Stampfer MJ, Manson JE, Rexrode KM, Willett WC, Hu FB. Prospective study of major dietary patterns and stroke risk in women. Stroke 2004;35:2014–2019. [DOI] [PubMed] [Google Scholar]
- 28.Fung TT, Chiuve SE, McCullough ML, Rexrode KM, Logroscino G, Hu FB. Adherence to a DASH-style diet and risk of coronary heart disease and stroke in women. Arch Intern Med 2008;168:713–720. [DOI] [PubMed] [Google Scholar]
- 29.Fung TT, Rexrode KM, Mantzoros CS, Manson JE, Willett WC, Hu FB. Mediterranean diet and incidence of and mortality from coronary heart disease and stroke in women. Circulation 2009;119:1093–1100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Willett W, Rockström J, Loken B, et al. Food in the Anthropocene: the EAT-Lancet Commission on Healthy Diets From Sustainable Food Systems. Lancet 2019;393:447–492. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The dataset analyzed in this study is not publicly available, but further information about the dataset can be obtained from the NHS; formal review processes exist for request of datasets.