Plato, in his Allegory of the Cave, contemplates a group of people who have lived their entire lives facing a wall of a cave and whose impressions of the world are constrained to perceptual experiences of shadows cast on the wall by entities that are never directly observed. Since time immemorial, conscious states of others have been like Platonic shadows, inferred only imperfectly and indirectly through close observation of behaviors. Although for centuries philosophers and neuroscientists have sought to bring us closer to understanding consciousness, an influx of neurotechnologies now enables clinicians and researchers to potentially improve detection of consciousness and prediction of its recovery.1 Innovations in neuroimaging and electrophysiologic techniques now may permit detection of states of consciousness not readily discernible by bedside examination, known as covert consciousness or cognitive motor dissociation.2 The discovery of covert consciousness raises distinctive issues surrounding both the diagnosis and prognosis of persons with disorders of consciousness (DoC), highlighting the need for caution during the acute phase of neuroprognostication and exposing gaps in knowledge about the epidemiology and phenomenology of covert consciousness. These innovations represent a possible step forward from philosophical and scientific traditions that relied on behavioral observations to detect consciousness. In turn, these breakthroughs prompt reconsideration of standard approaches to the evaluation of persons with DoC and necessitate appraisal of how clinicians should communicate results of novel techniques with indeterminate meanings to surrogates. Proactive integration of neuroethical insights in clarifying responsible ends to which these technologies should be directed is essential for addressing these timely challenges. This article proposes an ethical framework to help the clinical and research community consider how to use these emerging neurotechnologies responsibly, calls for careful consideration of the consequences of searching for covert consciousness in practice, and highlights critical avenues for further study of how the finding of covert consciousness might help predict goal-concordant functional recovery.
The advent of novel neurotechnologies in the evaluation of persons with DoC has been motivated by the recognition that persons with DoC may be misclassified as unconscious when standard behavior-based examination is used.3,4 Pitfalls of the behavioral examination in reliably detecting consciousness generate profound ethical dilemmas for clinicians and surrogates who face decisions about continuation of analgesia, life-sustaining therapy, and resource allocation.5 Innovative neuroimaging and electrophysiologic techniques, including functional MRI (fMRI), positron emission tomography, and quantitative electroencephalography (EEG), have demonstrated utility in improving diagnostic and prognostic precision in persons with severe brain injury in both acute and chronic stages; however, these technologies are still far from being used widely, and gaps exist in our knowledge of the phenomenology and functional outcomes associated with patterns of detected brain activity.6–9
Decisions to continue or withdraw life-sustaining treatments and neurorehabilitative services for persons with DoC are typically predicated on clinical judgements regarding the patient's current level of consciousness, the level of consciousness that the patient might recover to, and the likelihood that consciousness will recover to a level that the patient would find acceptable and in a manner that is concordant with what is known about the patient's preferences and goals.10 These assessments have traditionally hinged on a combination of neurobehavioral examination, standard EEG, and neuroimaging (CT or MRI).10 However, these standard measures have proven imperfect, leading to prognostic uncertainty and magnifying the difficulty of goals-of-care decisions.11 Novel neurotechnologies promise to inform these decisions by contributing to more precise measurements of consciousness and reliable markers of recovery.1 In a 2017 study of 16 patients with DoC due to acute traumatic brain injury admitted to the intensive care unit (ICU), covert consciousness was identified in 4 patients using task-based fMRI, including 3 whose behavioral diagnosis suggested a vegetative state.7 Demonstrating the neuroprognostic significance of these findings, a more recent study examined patients in the ICU who were not responsive to verbal commands and performed task-based EEG to detect brain activation.6 EEG detected characteristic brain activation patterns in response to a hand movement task in 15% of those who were behaviorally unresponsive and predicted functional independence at 12 months.6 In the chronic phase, a meta-analysis of 37 studies including more than 1,000 patients found that approximately 20% were misclassified as vegetative when in fact patients displayed covert consciousness by task-based fMRI or EEG,12 findings that may portend a higher chance of functional recovery.8,13 Despite these data, covert consciousness is rarely identified in routine clinical practice at most medical centers; this may either be due to underrecognition, with very few centers equipped to use neurotechnologies enabling detection of covert consciousness, or because of truly low incidence. Further study is thus needed to shed light on the real-world epidemiology of covert consciousness.
Acknowledging the clinical value of these novel paradigms, a 2018 practice guideline on the management of patients with DoC issued jointly by the American Academy of Neurology, American College of Rehabilitation Medicine, and National Institute on Disability, Independent Living, and Rehabilitation Research specifies that “clinicians may use multimodal evaluations incorporating specialized functional imaging or electrophysiologic studies to assess for evidence of awareness not identified on neurobehavioral assessment that might prompt consideration of an alternate diagnosis” and in some circumstances “may assess for the presence of higher level activation of the auditory association cortex using blood-oxygen-level-dependent (BOLD) fMRI in response to a familiar voice speaking the patient's name.”10 More recently, a 2020 European Academy of Neurology (EAN) guideline on the diagnosis of coma and other DoC similarly emphasized that clinicians should “whenever feasible, consider positron emission tomography, resting state functional magnetic resonance imaging (fMRI), active fMRI or EEG paradigms and quantitative analysis of high-density EEG to complement behavioral assessment in patients without command following at the bedside.”14 In even stronger terms, the EAN guideline concludes that “[s]tandardized clinical evaluation, EEG-based techniques, and functional neuroimaging should be integrated for multimodal evaluation of patients with DoC,” and in situations where there is discordance between approaches, the “state of consciousness should be classified according to the highest level revealed by any of these 3 approaches.”14 Building on these sentiments, an August 2020 International Federation of Clinical Neurophysiology Expert Group opinion statement details efforts to integrate novel electrophysiologic measures into assessments of patients with DoC and outlines a plan for stepwise deployment.15 Despite these notable recommendations, how to responsibly assimilate these tools into clinical protocols remains unclear; little is known about ethical concerns surrounding these techniques, the phenomenology of the disordered states of consciousness they reveal, or attitudes of clinicians, patients, and surrogates regarding their optimal implementation.
Recognizing the exigencies that these novel neurotechnologies respond to and the epistemic gap that they aim to fill, an ethical framework that carefully balances benefits and prospects for unintended harm is imperative to ensure responsible translation. We propose 4 guiding neuroethical principles to aid clinicians and researchers in this pressing undertaking.
Communicate Uncertainty
Clinical use of novel neuroimaging and electrophysiologic techniques to aid in the detection of consciousness raises numerous questions surrounding how to meaningfully and reliably share information yielded by these techniques with surrogate decision-makers. In counseling surrogates about the meaning of advanced neuroimaging or neurophysiologic results, especially when results run contrary to countervailing clinical information, the tendency to issue definite or conclusive statements should be avoided. Instead, clinicians should be transparent about the novelty of these techniques and the fundamental uncertainties that remain in their interpretation.
To illustrate these uncertainties, consider the hypothetical case of a patient who sustained severe traumatic brain injury after a motor vehicle accident who remains intubated 2 weeks into the ICU admission, and when sedation is weaned, she is behaviorally unresponsive with eyes closed. However, fMRI reveals intact functional network connectivity, increased BOLD signal in the auditory cortex when a familiar song is played, and increased BOLD signal in the premotor cortices when instructed to imagine playing a sport. What is the meaning of intact functional network connectivity detected by fMRI in the context of a poor bedside neurologic examination, and what is the phenomenological significance of these fMRI responses? Do these findings imply that the patient is aware, or merely suggest that there is some degree of intact rudimentary cognitive processing? Although recent evidence suggests that covert consciousness portends improved prognosis compared with coma or vegetative state (i.e., unresponsive wakefulness syndrome),6 the potential for false-positive or false-negative results also exists and should be recognized.6–8 Furthermore, there is a paucity of data on the degree of long-term recovery and quality-of-life measures among patients within or emerged from covert consciousness during the subacute and chronic phases of care. However, this information is often what matters most to surrogates when deciding on goals of care.16,17
Recognizing these uncertainties, the clinical and phenomenological indeterminacy of these findings should be clearly explained and intelligibly quantified when possible. Further study is needed to clarify best practices in disclosing information of this kind to surrogates, who, already potentially overwhelmed by the critical illness of a loved one, may be distinctively prone to misinterpret the meaning of an advanced data point with unfamiliar referents or to form unrealistic expectations.
Capture and Integrate Stakeholder Perspectives
Diverse perspectives of key stakeholders affected by these technologies, including patients, surrogates, and clinicians, ought to be widely elicited and captured in detail to help guide the development and deployment of a neuroethical framework governing their use. Insights from patients who have recovered from covertly conscious states should be evaluated to elucidate the phenomenology of this poorly understood condition and associated quality of life measures. Potential impact on surrogates, including possible prolongation of psychosocial distress and delayed closure, should be anticipated and studied. Such insights from the lived-experiences of key stakeholders can provide evidential grounding for the construction of a neuroethics framework to guide responsible clinical translation.
Optimize DoC Nosology and Diagnostic Criteria
To the extent that advanced neurotechnologies may yield diagnostic information that is tantamount or paramount to information derived by behavioral evaluation, the prevailing taxonomy of DoC and their diagnostic criteria, which are currently formulated solely in behavioral elements, are rendered incomplete, if not obsolete. It is therefore crucial that DoC nosology and diagnostic criteria be modernized to incorporate advanced neuroimaging and electrophysiologic elements and thus better align with recent society guidelines.10,14 Beyond safeguarding the descriptive veracity and consistency of shared nomenclature, a more precise DoC taxonomy can improve the efficiency and integrity of patient-family communication, of inter-clinician communication, and of ongoing research and quality-improvement efforts.
Promote Equity in Neurotechnology Access
Currently, the availability of most advanced neurotechnologies to aid in the detection of consciousness is limited to a few academic centers across the world. However, an implication of recent society guidelines is that the workup of persons with DoC without behavioral evidence of awareness may remain incomplete without advanced data points. A daunting ethical challenge will therefore be how to ensure equitable access to advanced neurotechnologies when demand may far exceed availability, especially in underserved and remote areas. Well-coordinated systems of implementation and policy redesign that prioritize fair access and equity are critical to ensuring long-term success without magnifying pre-existing disparities. These efforts must be coupled with further critical study to shed light on how the finding of covert consciousness might predict acceptable functional recovery and how to ensure goal-concordant care during the process of emerging consciousness and quality of life in such states.
These suggested guiding principles are by no means exhaustive; rather, they are intended to serve as a starting point for the development of a neuroethical framework and to catalyze multidisciplinary dialogue on how to ensure clinically appropriate and ethically resilient use before these techniques are widely implemented at the bedside.
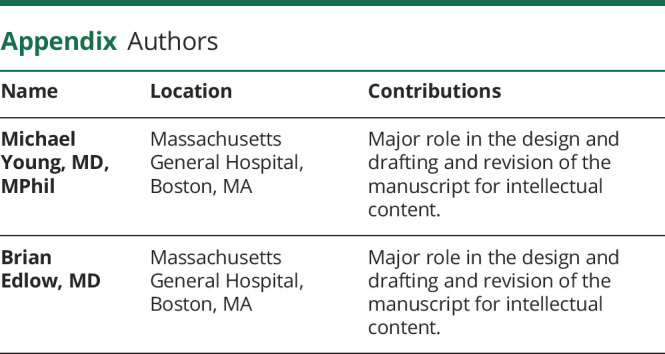
Appendix. Authors
Study Funding
This work was supported by the NIH BRAIN Initiative (F32MH123001), the NIH National Institute of Neurological Disorders and Stroke (R21NS109627, RF1NS115268), NIH Director's Office (DP2HD101400), Henry and Allison McCance Center for Brain Health / Mass General Neuroscience SPARC Award, James S. McDonnell Foundation, and Tiny Blue Dot Foundation.
Disclosure
None reported. Go to Neurology.org/N for full disclosures.
References
- 1.Edlow BL, Claassen J, Schiff ND, Greer DM. Recovery from disorders of consciousness: mechanisms, prognosis, and emerging therapies. Nat Rev Neurol 2021;17:135–156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schiff ND. Cognitive motor dissociation following severe brain injuries. JAMA Neurol 2015;72:1413–1415. [DOI] [PubMed] [Google Scholar]
- 3.Schnakers C, Vanhaudenhuyse A, Giacino J, et al. Diagnostic accuracy of the vegetative and minimally conscious state: clinical consensus versus standardized neurobehavioral assessment. BMC Neurol 2009;9:35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fins JJ. When No one notices: disorders of consciousness and the chronic vegetative state. Hastings Cent Rep 2019;49:14–17. [DOI] [PubMed] [Google Scholar]
- 5.Fins JJ, Bernat JL. Ethical, palliative, and policy considerations in disorders of consciousness. Neurology 2018;91:471–475. [DOI] [PubMed] [Google Scholar]
- 6.Claassen J, Doyle K, Matory A, et al. Detection of brain activation in unresponsive patients with acute brain injury. N Engl J Med 2019;380:2497–2505. [DOI] [PubMed] [Google Scholar]
- 7.Edlow BL, Chatelle C, Spencer CA, et al. Early detection of consciousness in patients with acute severe traumatic brain injury. Brain 2017;140:2399–2414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stender J, Gosseries O, Bruno MA, et al. Diagnostic precision of PET imaging and functional MRI in disorders of consciousness: a clinical validation study. Lancet 2014;384:514–522. [DOI] [PubMed] [Google Scholar]
- 9.Monti MM, Vanhaudenhuyse A, Coleman MR, et al. Willful modulation of brain activity in disorders of consciousness. N Engl J Med 2010;362:579–589. [DOI] [PubMed] [Google Scholar]
- 10.Giacino JT, Katz DI, Schiff ND, et al. Practice guideline update recommendations summary: disorders of consciousness: report of the guideline development, dissemination, and implementation subcommittee of the American Academy of Neurology; the American Congress of Rehabilitation Medicine; and the National Institute on Disability, Independent Living, and Rehabilitation Research. Neurology 2018;91:450–460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bernat JL. Prognostic limitations of syndromic diagnosis in disorders of consciousness. AJOB Neurosci 2016;7:46–48. [Google Scholar]
- 12.Kondziella D, Friberg CK, Frokjaer VG, Fabricius M, Møller K. Preserved consciousness in vegetative and minimal conscious states: systematic review and meta-analysis. J Neurol Neurosurg Psychiatry 2016;87:485–492. [DOI] [PubMed] [Google Scholar]
- 13.Pan J, Xie Q, Qin P, et al. Prognosis for patients with cognitive motor dissociation identified by brain-computer interface. Brain 2020;143:1177–1189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kondziella D, Bender A, Diserens K, et al. European Academy of Neurology guideline on the diagnosis of coma and other disorders of consciousness. Eur J Neurol 2020;27:741–756. [DOI] [PubMed] [Google Scholar]
- 15.Comanducci A, Boly M, Claassen J, et al. Basic and advanced neurophysiology in the prognostic and diagnostic evaluation of disorders of consciousness: review of an IFCN-endorsed expert group. Clin Neurophysiol 2020;131:2736–2765. [DOI] [PubMed] [Google Scholar]
- 16.Fins JJ. Rights Come to Mind: Brain Injury, Ethics, and the Struggle for Consciousness. Cambridge University Press; Cambridge, UK: 2015. [Google Scholar]
- 17.Young MJ. “Consciousness” as a vague predicate. AJOB Neurosci 2017;8:157–159. [Google Scholar]


