Abstract
Objective
To determine the prevalence of complications in patients with COVID-19 undergone prone positioning, focusing on the development of prone-related pressure ulcers.
Methods
Cross-sectional study conducted in the hub COVID-19 centre in Milan (Italy), between March and June 2020. All patients with COVID-19 admitted to intensive care unit on invasive mechanical ventilation and treated with prone positioning were included. Association between prone-related pressure ulcers and selected variables was explored by the means of logistic regression.
Results
A total of 219 proning cycles were performed on 63 patients, aged 57.6 (10.8) and predominantly obese males (66.7%). The main complications recorded were: prone-related pressure ulcers (30.2%), bleeding (25.4%) and medical device displacement (12.7%), even if no unplanned extubation was recorded. The majority of patients (17.5%) experienced bleeding of upper airways. Only 15 prone positioning cycles (6.8%) were interrupted, requiring staff to roll the patient back in the supine position. The likelihood of pressure ulcers development was independently associated with the duration of prone positioning, once adjusting for age, hypoxemic level, and nutritional status (OR 1.9, 95%CI 1.04–3.6).
Conclusion
The use of prone positioning in patients with COVID-19 was a safe and feasible treatment, also in obese patients, who might deserve more surveillance and active prevention by intensive care unit staff.
Keywords: COVID-19, Intensive Care Units, Obesity, Pressure Ulcers, Prone Position, Respiratory Distress Syndrome
Implications for clinical practice.
-
•
Patients with severe COVID-19 undergone prone positioning frequently experience complications, in particular pressure ulcers.
-
•
Pressure ulcer development is associated with the duration of prone positioning.
-
•
Obesity is not an obstacle for the use of prone positioning and highly trained staff is the key factor for a safe manoeuver.
Introduction
Coronavirus disease 2019 (COVID-19) is caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), that has spread globally up to pandemic (Huang et al., 2020). SARS-CoV-2 infection affects the respiratory system causing an acute respiratory distress syndrome (ARDS) in 61–81% of patients with COVID‐19 pneumonia requiring intensive care (Wu et al., 2020). In particular, patients with obesity have a higher risk of developing severe COVID-19 (Engin et al., 2020) and obesity is strongly associated with poor outcomes, including an increased need for intensive care and invasive mechanical ventilation support (Chu et al., 2020).
Strategies for treatment of ARDS include therapies like prone ventilation, considered an advanced treatment to consistently improve oxygenation (Koulouras et al., 2016). Prone position has been used at least since 1976 (Piehl and Brown, 1976) and its efficacy on gas exchange improvement and survival benefit have been demonstrated by numerous trials (Gattinoni et al., 2001, Guerin et al., 2004, Taccone et al., 2009) and meta-analyses (Mora-Arteaga et al., 2015, Munshi et al., 2017). However, prone position is not without complications and these could include unplanned extubation, accidental removal of arterial or venous catheters, hemodynamic instability, brachial plexus injury and pressure ulcers in anatomical sites different from those typical of bedridden patients (Jové Ponseti et al., 2017, Labeau et al., 2021).
The extensive use of prone position in a large number of critical patients represented the major challenge for nurses and physicians in intensive care unit (ICU) during the pandemic (Binda et al., 2021). As suggested, using a specific protocol to support ICU staff about prone position-related decisions may limit the occurrence of complications and improve the safety in patients who are not responsive to conventional mechanical ventilation (Carsetti et al., 2020).
The aim of this study was to determine the prevalence of complications in patients with COVID-19 undergoing prone position, particularly addressing the development of pressure ulcers.
Methods
Study design
This is a cross-sectional study conducted at Fondazione IRCCS Ca’ Granda Ospedale Maggiore Policlinico, an academic tertiary-level hospital in Milan (Italy), during the COVID-19 pandemic between March and June 2020. We included all patients with laboratory-confirmed SARS-CoV-2 infection admitted to ICU who were on invasive mechanical ventilation and treated with prone position. Patients were excluded if treated with noninvasive ventilation or intubated but not treated with prone position. The study was approved by the local ethics committee of our Institution (ethics approval number 236/2020).
Prone positioning practice
The proning maneuver was used for all patients as a rescue measure in severe impairment of gas exchanges (PaO2/FiO2 ≤ 100), after having optimized the ventilation in supine position (Grasselli et al., 2020). Because of rapid gas exchange deterioration, patients who did not tolerate ventilation in supine position (useful to easily perform the basic nursing care) were immediately repositioned into the prone position.
Considering the critical conditions of patients with COVID-19, at least four healthcare professionals and one experienced team leader were necessary during the maneuver to coordinate each step, as to minimize all possible risks. The prone position maneuver followed a strict protocol and an available decision-making algorithm was used to guide the healthcare professionals through performing a safe procedure, as already reported by our group elsewhere (Binda et al., 2021). Before the procedure, the gastric content was suctioned to avoid inhalation and enteral nutrition was continued, except during the manoeuver (Martindale et al., 2020). Patients were rolled into prone position with face turned on the side toward a flexed arm, with the other arm behind the patient (swimmer position), and repositioned every two hours. As per clinical practice, all patients admitted to ICU were placed on an air loss pressure mattress (TheraKair Visio™ Mattress, ArjoHuntleigh AB, Malmö, Sweden), considering every patient at high risk of pressure ulcers development (Tayyib and Coyer, 2016). No other special measure to prevent pressure ulcers was implemented, such as foam head support or pillows and the use of thoracic pelvic supports was completely avoided (Chiumello et al., 2006). To protect facial anatomical points mostly at risk of pressure ulcers (i.e., forehead, cheekbones) a hydrocolloid dressing (DuoDerm Extra Thin, ConvaTec Inc, Greensboro, USA) was used.
Skin conditions and ocular conjunctiva were assessed before and after pronation to look for any skin damage, presence of infections and vascular or thrombotic complications. Considering the high risk of venous thromboembolism in patients with COVID-19, all of them received an increasing dosage of low-molecular-weight heparin (from 40 mg daily up to 1 mg/kg twice daily), as per medical practice (Martinelli et al., 2021).
Data collection
We collected data on age, sex, body mass index (BMI), presence of comorbidities, Braden scale, ICU length of stay and mortality. Pronation cycle was defined as the period in which the patient is maintained in prone position before returning to supine, and prone position-time as the product between the number of pronation cycles and the mean length of pronation. Every prone position cycle was planned for a minimum of 16 hours. Prone positioning was described both in terms of number of prone position cycles and number of hours spent prone, together with any related complications.
Prone related pressure ulcer was defined as a skin injury resulting from prolonged pressure on the skin during prone position in several anatomical sites: forehead, cheekbone, nasal fold, lip, chin, chest, genitals, knee, leg (pretibial region) and toes. Pressure ulcers related to supine position and reported in the occiput, sacral or heel regions were not considered prone related pressure ulcers, as well as other skin injuries related to the presence of any medical device. All pressure ulcers were evaluated according to the National Pressure Ulcer Advisory Panel (NPUAP) (Edsberg et al., 2016).
Statistical analysis
Data are presented as median and interquartile range (IQR) or counts and percentage. Association between categorical variables was tested by the means of Fisher exact test. Correlation between continuous measures was explored using Spearman correlation coefficient. We hypothesized that the likelihood of developing prone related pressure ulcers was associated to the weight of patients, which is intrinsically related to the causative mechanism of pressure ulcers. Moreover, it was reasonable thinking about an interaction between prone position-time and BMI too. Therefore, a logistic regression model was fitted to test the statistical association between the likelihood of having prone related pressure ulcers and selected variables, namely BMI and prone position-time, adjusting for the level of hypoxemia (PaO2/FiO2 ratio), age and sex. Based on the lowest Akaike information criteria, age and BMI entered in the final model as linear. Hosmer-Lemeshow test was used to test model goodness-of-fit. A likelihood ratio test was used to guide the selecting process towards the best fitting model, which did not include sex. Results are commented as odds ratio and 95% confidence intervals (CI, lower-upper bound). All analyses were performed using R Core Team (version 4.0.3) (R Core Team, 2019), and a P-values <0.05 was considered statistically significant.
Results
As of June 30, 2020, a total of 128 patients with a laboratory-confirmed SARS-CoV-2 infection were admitted to our ICU. Table 1 shows the demographic and clinical characteristics of the 63 patients on invasive mechanical ventilation treated with prone position during the study period. Males with a BMI >25 kg/m2 represented the majority of patients included (66.7%, 42/63). In the present study, presence of comorbidities was associated with patients’ age (P = 0.0299) but not with their nutritional status (P = 0.1572).
Table 1.
General characteristics.
| N = 63 | |
|---|---|
| Demographic characteristics | |
| Age (years) | 59.6 (50.5–65.8) |
| Sex (male) | 51 (81%) |
| Comorbidities | 46 (73%) |
| Pulmonary | 5 (7.9%) |
| Cardiovascular | 44 (69.8%) |
| Diabetes | 11 (17.5%) |
| Others | 8 (12.7%) |
| Body Mass Index | |
| Normal weight (≤24.9) | 13 (20.6%) |
| Overweight (25.0–29.9) | 31 (49.2%) |
| Obesity (≥30.0) | 19 (30.2%) |
| Clinical characteristics | |
| SOFA score | 7.0 (4.0–8.0) |
| Braden scale | 9.0 (8.0–10.0) |
| PaO2/FiO2 ratio before PP | 78.0 (70.0–94.5) |
| Length of IMV (days) | 19.9 (11.0–39.5) |
| V-V ECMO | 6 (9.5%) |
| Length of ICU stay (days) | 19.0 (11.0–45.5) |
| Discharged alive from ICU | 34 (54.0%) |
Data are presented as counts (%) or median (IQR).
Abbreviations: ICU, Intensive Care Unit.
IMV, Invasive Mechanical Ventilation.
PP, Prone Positioning.
SOFA, Sequential Organ Failure Assessment Score.
V-V ECMO, Veno-Venous Extracorporeal Membrane Oxygenation.
Prone position was used as a rescue therapy, extended up to 219 cycles, with a median duration of 18 (IQR 15–20) hours. Details about prone position and related complications are reported in Table 2 . During the study period, 32 patients had at least one complication and 15 prone position cycles (6.8%, 15/219) were interrupted, requiring staff to roll the patient back in the supine position. Episodes of bleeding occurred in 25.4% (16/63) of patients and just one required the interruption of prone position for bleeding control. The majority of patients (17.5%, 11/63) experienced bleeding of upper airways. Rate of displacement of medical devices during prone position occurred in 12.7% (8/63) of patients: we did not record any unplanned extubation nor chest drainage tube accidental removal. Overall, the number of complications, including prone related pressure ulcers, was not statistically associated with the frequency of prone position cycles (P = 0.099).
Table 2.
Description of prone positioning and complications.
| Pronation cycles | |
|---|---|
| 1 cycle | 9 (14.3%) |
| 2 cycles | 21 (33.3%) |
| ≥3 cycles | 33 (52.4%) |
| Prolonged cycle ≥16 h | 38 (60.3%) |
| Complications | |
| Bleeding | 16 (25.4%) |
| Mouth and lips | 8 (12.7%) |
| Nose | 3 (4.8%) |
| Exit-site vascular access | 2 (3.2%) |
| Endobronchial | 2 (3.2%) |
| Eyelid | 1 (1.6%) |
| Medical device displacement | 8 (12.7%) |
| Endotracheal tube | 4 (6.3%) |
| Nasogastric tube | 3 (4.8%) |
| Vascular catheter | 1 (1.6%) |
| Prone positioning interrupted for | 15 (23.8%) |
| Prolonged desaturation | 7 (11.1%) |
| Hemodynamic instability | 6 (9.5%) |
| Pneumothorax | 1 (1.6%) |
| Bleeding | 1 (1.6%) |
Data are presented as counts (%).
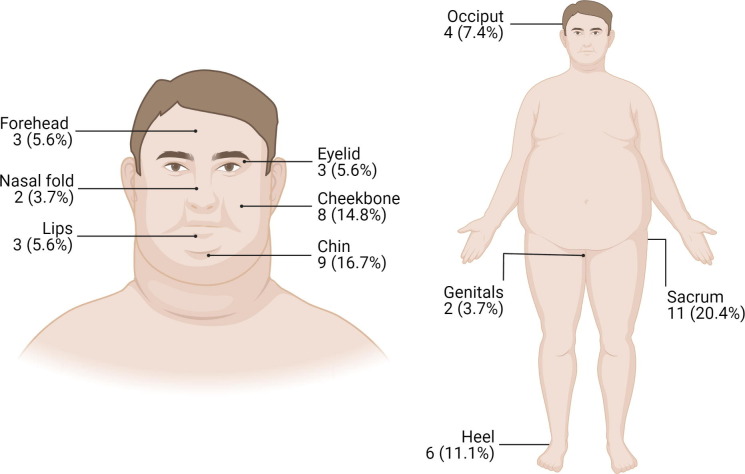
The prevalence of patients with pressure ulcers was 42.9% (95%CI: 30.6–55.1) whereas it was 30.2% (95%CI: 18.8–41.5) when prone related pressure ulcers only were considered. Particularly, patients with pressure ulcers showed a higher level of correlation (ρ = 0.47, P = 0.042) between days of mechanical ventilation and prone position-time, compared to patients without pressure ulcers (ρ = 0.29, P = 0.052). Face was the most affected site and Fig. 1 shows the distribution of pressure ulcers in each anatomical district.
Fig. 1.
Topographic distribution of pressure ulcers in the typical obese male patient with COVID-19 in our study. A total of 54 pressure ulcers were recorded: 59.2% (32/54) were on the head, 35.2% (19/54) were on sacrum, genitals and heels, and 5.6% (3/54) were in other sites. On the head, the most frequent NPUAP stage was stage II (71.9%, 23/32), followed by stage I (28.1%, 9/32). The stage III was recorded only on sacrum (45.4%, 5/11). The figure was created with permission of BioRender.com.
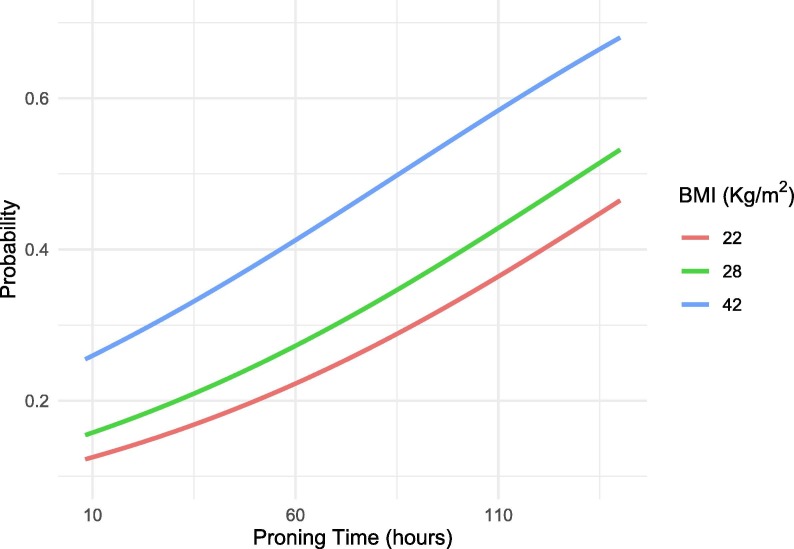
From the fitted model, the interaction between BMI and prone position-time was not statistically significant and prone position-time was the only significant predictor for prone related pressure ulcers (P = 0.039). The effect of increasing mean prone position-time from 24 to 48 hours was to increase the odds by a factor of 1.4 (95%CI: 1.02 to 1.91). Although not statistically significant, a clinical important effect of BMI is worth to be acknowledged, as represented in the marginal effect in Fig. 2 . Remarkably, increasing weight from 22 to 28 kg/m2 increased the odds by a factor of 1.3 (95%CI 0.6–2.8, P = 0.498). Although not meant for prediction, discriminative ability of the model was 0.68 (adjusted C-index), where 0.5 means that the model is not better than assigning observations randomly.
Fig. 2.
Probability of developing prone related pressure ulcers as a function of the time spent prone, holding age constant at the mean sample value (i.e., 58 years), PaO2/FiO2 ratio at mean sample value (i.e., 85) of three patients at different BMI (min, median and max sample values). The fitted model explained the 20% of the total variance.
Discussion
During the COVID-19 pandemic, the number of patients with moderate-to-severe ARDS has increased considerably and prone position has gained importance as an adjunctive treatment of severe hypoxemia (Qadri et al., 2020). Prone position maneuver during mechanically ventilation is reported as safe and feasible, even though the incidence of several complications (including pressure ulcers) is higher for patients prone than those treated in supine position (Girard et al., 2014).
A broad prevalence of prone position complications is reported in literature (Guérin et al., 2018, Martínez Campayo et al., 2020, Taito et al., 2018). Several studies have reported a higher frequency of pressure ulcers in patients kept prone for long sessions (Beuret et al., 2002, Girard et al., 2014, Voggenreiter et al., 2005) and one meta-analysis of 366 patients found that pressure ulcers of any grade were 37% more common when adopting prone compared to supine position (relative risk 1.37; 95%CI, 1.05–1.79) (Bloomfield et al., 2015).
Differently from one study that did not include patients with COVID-19, prevalence of prone related pressure ulcers in our sample was higher, (30.2% versus 13.5%), although the most commonly affected anatomical sites by prone related pressure ulcers were the same, specifically cheekbones and chin (Lucchini et al., 2020). Comparison to other studies that report data on COVID-19 yields to a prevalence of pressure ulcers in the head and neck area varying from 30.2% (19/63) in our study to 44.3% (27/61) (Douglas et al., 2021), 47.6% (68/143) (Shearer et al., 2021) and 77.0% (57/74) (Ibarra et al., 2020). In patients with COVID-19, the prolonged skin pressure on the face together with the severe hypoxemia, the microvascular injury and thrombosis could explain the high risk of facial prone related pressure ulcers. In particular, severe hypoxemia causes a decrease in peripheral perfusion (including skin perfusion) and promotes the occurrence of ischemic skin lesions (Perrillat et al., 2020). In addition to this pathophysiologic mechanism, it is worth noting that the face has little muscle mass to provide blood supply to the skin and to subcutaneous facial tissues under the sustained deformations caused by the weight of the head. On the whole, this could promote the development of facial pressure ulcers, particularly at the pressure points of the prone head, namely forehead, cheekbones and chin (Grisell and Place, 2008). Using a low air loss pressure mattress without other pillows or thoraco-pelvic supports might ensure the reduction of the contact pressure at the skin-mattress interface by increasing the surface area. In principle, this mechanism permits to prevent the skin breakdown as well as to distribute pressure by conforming to bony prominences and minimizing tissue deformation.
Pressure ulcers prevention involves skin assessments and frequent off‐loading of pressure points, and repositioning (Boyko et al., 2018). However, these recommendations are not always feasible in patients who are mechanically ventilated in prone position and connected to a variety of monitors, probes, and tube systems. Under this scenario, the risk of tubes and devices dislodgement is increased at every intervention on patient, thus requiring multiple highly trained nurses to coordinate the positioning safely (Peko et al., 2020).
The current literature describes the risk of pressure ulcers development as related also to nutritional status (Hyun et al., 2014). Indeed, BMI is associated with occurrence of pressure ulcers in ICU setting and obese patients have higher rates of pressure ulcers compared to patients with normal weight. A link between obesity and SARS-CoV-2 infection has been already documented, and these patients are mostly obese and have a higher need of invasive mechanical ventilation (Simonnet et al., 2020), as reported also in our study. Although the present results did not find evidence of association between pressure ulcers and BMI, the effect of BMI on the likelihood of developing pressure ulcers is not negligible. As reported from an ancillary analysis of a large prospective multicentre trial on early application of prone position (Guérin et al., 2013), BMI, male sex and age were significant covariates for the risk of developing pressure ulcers during ICU stay (Girard et al., 2014). Altogether, these findings are really important, helping nurses and physicians to better identify patients who require additional care. For instance, the widely used Braden scale to assess the risk for pressure ulcers (which takes into account sensory perception, skin moisture, activity, mobility, nutrition, friction and shear) has poor predictive value for patients in ICU (Cox, 2012, Deschepper et al., 2021, Zhang et al., 2021). For this reason, in addition to standard tools, BMI should be considered when evaluating the risk for pressure ulcers development.
A further novel finding of our study is the reported prevalence of bleeding complications. Mouth and nose were the most common bleeding sites associated to the presence of medical devices, like orotracheal and nasogastric tube. The occurrence of this complication could be explained by the antithrombotic prophylaxis with augmented dosage of low-molecular-weight heparin or unfractionated heparin to counter the hypercoagulability (Panigada et al., 2020). Indeed, pulmonary embolism was a frequent fatal event in patients with COVID-19 (Wichmann et al., 2020) and the active administration of anticoagulants seems to be associated with better prognosis (Tang et al., 2020). These medical-device-related complications, once summed to the facial oedema and the high prevalence of pressure ulcers on the chin, cheekbones and forehead, put the face at the greatest risk of pressure ulcers and thus requires special care from nursing staff.
Among the other complications of prone position described in the literature (Galazzi et al., 2019, Guérin et al., 2020, Sanghi et al., 2021), we also recorded medical devices displacement, severe hemodynamic instability and prolonged desaturation, which required the interruption of prone position. The peculiar situation of hospitals during the pandemic, characterized by an increased number of ICU beds with new undertrained staff not familiar with nursing in critical care (Grasselli et al., 2020), could partially explain the increased prevalence of such complications related to the extensive use of prone position, even if lower compared to other study (Rodríguez-Huerta et al., 2021). In this context, using protocols, including algorithmic approach to evaluation, was helpful to guide the staff members with less experience through the advanced clinical management of the most critical patients (Oliveira et al., 2017).
Strengths and limitations
To our knowledge, this is the largest cross-sectional study describing complications related to prone positioning in patients with severe COVID-19. During the pandemic, our hospital has been designated as coordinator hub of the ICUs in Lombardy region, therefore the worst critically ill patients were transferred to our Institution. This could be commented as a selection bias towards the most compromised patients. Nevertheless, the low prevalence of prone related pressure ulcers and the lack of serious complications may be reported as another strength of our study, potentially due to procedures performed or supervised by expert ICU staff. As a matter of fact, experience and specific training are the key factors of our ICU. Among the limitations, we acknowledge that data regarding postural changes are missing. These were supposed to occur every 2 h according to internal protocol but they were not recorded on a routine basis, making impossible to determine when the patients’ head and arms were not moved or the maneuvers were not recorded.
Conclusion
Considering the large number of pronation cycles performed in our hub COVID-19 centre, prone related pressure ulcers affected a smaller number of patients compared to other similar studies. In particular, obesity was not an obstacle for the use of prone positioning, but the ICU staff should be aware that obese patients may require more surveillance and active prevention.
Funding Source
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Ethical Approval
The study was approved by ethical committee of Foundation IRCCS Ca’ Granda Ospedale Maggiore Policlinico - Milano, Italy (approval no. 236/2020).
Authors’ contribution
FB, AG and FM designed the study, coordinate data collection, data curation and writing the original draft. SG performed formal analysis of data and reviewed the manuscript. LV and EV made the data collection. IA and DL gave expert content and reviewed the manuscript. DL contributed also to study supervision. All authors read and approved the final manuscript.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- Beuret P., Carton M.-J., Nourdine K., Kaaki M., Tramoni G., Ducreux J.-C. Prone position as prevention of lung injury in comatose patients: a prospective, randomized, controlled study. Intensive Care Med. 2002;28:564–569. doi: 10.1007/s00134-002-1266-x. [DOI] [PubMed] [Google Scholar]
- Binda F., Marelli F., Galazzi A., Pascuzzo R., Adamini I., Laquintana D. Nursing management of prone positioning in patients with COVID-19. Crit. Care Nurse. 2021;41:27–35. doi: 10.4037/ccn2020222. [DOI] [PubMed] [Google Scholar]
- Bloomfield, R., Noble, D.W., Sudlow, A., 2015. Prone position for acute respiratory failure in adults. Cochrane Database Syst. Rev. https://doi.org/10.1002/14651858.CD008095.pub2. [DOI] [PMC free article] [PubMed]
- Boyko T.V., Longaker M.T., Yang G.P. Review of the current management of pressure ulcers. Adv. Wound Care. 2018;7:57–67. doi: 10.1089/wound.2016.0697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carsetti A., Damia Paciarini A., Marini B., Pantanetti S., Adrario E., Donati A. Prolonged prone position ventilation for SARS-CoV-2 patients is feasible and effective. Crit. Care. 2020;24:225. doi: 10.1186/s13054-020-02956-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiumello D., Cressoni M., Racagni M., Landi L., Li Bassi G., Polli F., et al. Effects of thoraco-pelvic supports during prone position in patients with acute lung injury/acute respiratory distress syndrome: a physiological study. Crit. Care. 2006;10:R87. doi: 10.1186/cc4933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chu Y., Yang J., Shi J., Zhang P., Wang X. Obesity is associated with increased severity of disease in COVID-19 pneumonia: a systematic review and meta-analysis. Eur. J. Med. Res. 2020;25:64. doi: 10.1186/s40001-020-00464-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cox J. Predictive power of the Braden scale for pressure sore risk in adult critical care patients. J. Wound Ostomy Cont. Nurs. 2012;39:613–621. doi: 10.1097/WON.0b013e31826a4d83. [DOI] [PubMed] [Google Scholar]
- Deschepper M., Labeau S.O., Waegeman W., Blot S.I. Pressure injury prediction models for critically-ill patients should consider both the case-mix and local factors. Intensive Crit. Care Nurs. 2021 doi: 10.1016/j.iccn.2021.103033. [DOI] [PubMed] [Google Scholar]
- Douglas I.S., Rosenthal C.A., Swanson D.D., Hiller T., Oakes J., Bach J., et al. Safety and outcomes of prolonged usual care prone position mechanical ventilation to treat acute Coronavirus Disease 2019 hypoxemic respiratory failure. Crit. Care Med. 2021;49:490–502. doi: 10.1097/CCM.0000000000004818. [DOI] [PubMed] [Google Scholar]
- Edsberg L.E., Black J.M., Goldberg M., McNichol L., Moore L., Sieggreen M. Revised national pressure ulcer advisory panel pressure injury staging system. J. Wound Ostomy Cont. Nurs. 2016;43:585–597. doi: 10.1097/WON.0000000000000281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Engin A.B., Engin E.D., Engin A. Two important controversial risk factors in SARS-CoV-2 infection: obesity and smoking. Environ. Toxicol. Pharmacol. 2020 doi: 10.1016/j.etap.2020.103411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galazzi A., Adamini I., Consonni D., Roselli P., Rancati D., Ghilardi G., et al. Accidental removal of devices in intensive care unit: an eight-year observational study. Intensive Crit. Care Nurs. 2019;54:34–38. doi: 10.1016/j.iccn.2019.06.002. [DOI] [PubMed] [Google Scholar]
- Gattinoni L., Tognoni G., Pesenti A., Taccone P., Mascheroni D., Labarta V., et al. Effect of prone positioning on the survival of patients with acute respiratory failure. N. Engl. J. Med. 2001;345:568–573. doi: 10.1056/NEJMoa010043. [DOI] [PubMed] [Google Scholar]
- Girard R., Baboi L., Ayzac L., Richard J.-C., Guérin C. The impact of patient positioning on pressure ulcers in patients with severe ARDS: results from a multicentre randomised controlled trial on prone positioning. Intensive Care Med. 2014;40:397–403. doi: 10.1007/s00134-013-3188-1. [DOI] [PubMed] [Google Scholar]
- Grasselli G., Pesenti A., Cecconi M. Critical care utilization for the COVID-19 outbreak in Lombardy, Italy: early experience and forecast during an emergency response. JAMA. 2020;323:1545–1546. doi: 10.1001/jama.2020.4031. [DOI] [PubMed] [Google Scholar]
- Grisell M., Place H.M. Face tissue pressure in prone positioning: a comparison of three face pillows while in the prone position for spinal surgery. Spine (Phila. Pa. 1976) 2008;33:2938–2941. doi: 10.1097/BRS.0b013e31818b9029. [DOI] [PubMed] [Google Scholar]
- Guérin C., Albert R.K., Beitler J., Gattinoni L., Jaber S., Marini J.J., et al. Prone position in ARDS patients: why, when, how and for whom. Intensive Care Med. 2020;46:2385–2396. doi: 10.1007/s00134-020-06306-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guérin C., Beuret P., Constantin J.M., Bellani G., Garcia-Olivares P., Roca O., et al. A prospective international observational prevalence study on prone positioning of ARDS patients: the APRONET (ARDS Prone Position Network) study. Intensive Care Med. 2018;44:22–37. doi: 10.1007/s00134-017-4996-5. [DOI] [PubMed] [Google Scholar]
- Guerin C., Gaillard S., Lemasson S., Ayzac L., Girard R., Beuret P., et al. Effects of systematic prone positioning in hypoxemic acute respiratory failure. JAMA. 2004;292:2379. doi: 10.1001/jama.292.19.2379. [DOI] [PubMed] [Google Scholar]
- Guérin C., Reignier J., Richard J.-C., Beuret P., Gacouin A., Boulain T., et al. Prone positioning in severe acute respiratory distress syndrome. N. Engl. J. Med. 2013;368:2159–2168. doi: 10.1056/NEJMoa1214103. [DOI] [PubMed] [Google Scholar]
- Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y., et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hyun S., Li X., Vermillion B., Newton C., Fall M., Kaewprag P., et al. Body mass index and pressure ulcers: improved predictability of pressure ulcers in intensive care patients. Am. J. Crit. Care. 2014;23:494–500. doi: 10.4037/ajcc2014535. quiz 501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ibarra G., Rivera A., Fernandez-Ibarburu B., Lorca-García C., Garcia-Ruano A. Prone position pressure sores in the COVID-19 pandemic: the Madrid experience. J. Plast. Reconstr. Aesthet. Surg. 2020 doi: 10.1016/j.bjps.2020.12.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jové Ponseti E., Villarrasa Millán A., Ortiz Chinchilla D. Analysis of complications of prone position in acute respiratory distress syndrome: quality standard, incidence and related factors. Enfermería Intensiva. 2017;28:125–134. doi: 10.1016/j.enfie.2016.12.002. [DOI] [PubMed] [Google Scholar]
- Koulouras V., Papathanakos G., Papathanasiou A., Nakos G. Efficacy of prone position in acute respiratory distress syndrome patients: a pathophysiology-based review. World J. Crit. Care Med. 2016;5:121. doi: 10.5492/wjccm.v5.i2.121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Labeau S.O., Afonso E., Benbenishty J., Blackwood B., Boulanger C., Brett S.J., et al. Prevalence, associated factors and outcomes of pressure injuries in adult intensive care unit patients: the DecubICUs study. Intensive Care Med. 2021;47:160–169. doi: 10.1007/s00134-020-06234-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lucchini A., Bambi S., Mattiussi E., Elli S., Villa L., Bondi H., et al. Prone position in acute respiratory distress syndrome patients: a retrospective analysis of complications. Dimens. Crit. Care Nurs. 2020;39:39–46. doi: 10.1097/DCC.0000000000000393. [DOI] [PubMed] [Google Scholar]
- Martindale R., Patel J.J., Taylor B., Arabi Y.M., Warren M., McClave S.A. Nutrition therapy in critically ill patients with Coronavirus Disease 2019. J. Parenter. Enter. Nutr. 2020;44:1174–1184. doi: 10.1002/jpen.v44.710.1002/jpen.1930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinelli I., Ciavarella A., Abbattista M., Aliberti S., De Zan V., Folli C., et al. Increasing dosages of low-molecular-weight heparin in hospitalized patients with Covid-19. Intern. Emerg. Med. 2021 doi: 10.1007/s11739-020-02585-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martínez Campayo N., Bugallo Sanz J.I., Mosquera Fajardo I. Symmetric chest pressure ulcers, consequence of prone position ventilation in a patient with COVID-19. J. Eur. Acad. Dermatol. Venereol. 2020;34 doi: 10.1111/jdv.v34.1110.1111/jdv.16755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mora-Arteaga J.A., Bernal-Ramírez O.J., Rodríguez S.J. The effects of prone position ventilation in patients with acute respiratory distress syndrome. A systematic review and meta-analysis. Med. Intensiva. 2015;39:352–365. doi: 10.1016/j.medin.2014.11.003. [DOI] [PubMed] [Google Scholar]
- Munshi L., Del Sorbo L., Adhikari N.K.J., Hodgson C.L., Wunsch H., Meade M.O., et al. Prone position for acute respiratory distress syndrome. A systematic review and meta-analysis. Ann. Am. Thorac. Soc. 2017;14:S280–S288. doi: 10.1513/AnnalsATS.201704-343OT. [DOI] [PubMed] [Google Scholar]
- Oliveira V.M., Piekala D.M., Deponti G.N., Batista D.C.R., Minossi S.D., Chisté M., et al. Safe prone checklist: construction and implementation of a tool for performing the prone maneuver. Rev. Bras. Ter. Intensiva. 2017;29:131–141. doi: 10.5935/0103-507X.20170023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Panigada M., Bottino N., Tagliabue P., Grasselli G., Novembrino C., Chantarangkul V., et al. Hypercoagulability of COVID-19 patients in intensive care unit: a report of thromboelastography findings and other parameters of hemostasis. J. Thromb. Haemost. 2020;18:1738–1742. doi: 10.1111/jth.14850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peko L., Barakat‐Johnson M., Gefen A. Protecting prone positioned patients from facial pressure ulcers using prophylactic dressings: a timely biomechanical analysis in the context of the COVID-19 pandemic. Int. Wound J. 2020;17:1595–1606. doi: 10.1111/iwj.13435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perrillat A., Foletti J.-M., Lacagne A.-S., Guyot L., Graillon N. Facial pressure ulcers in COVID-19 patients undergoing prone positioning: how to prevent an underestimated epidemic? J. Stomatol. Oral Maxillofac. Surg. 2020;121:442–444. doi: 10.1016/j.jormas.2020.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piehl M.A., Brown R.S. Use of extreme position changes in acute respiratory failure. Crit. Care Med. 1976;4:13–14. doi: 10.1097/00003246-197601000-00003. [DOI] [PubMed] [Google Scholar]
- Qadri S.K., Ng P., Toh T.S.W., Loh S.W., Tan H.L., Lin C.B., et al. Critically ill patients with COVID-19: a narrative review on prone position. Pulm. Ther. 2020;6:233–246. doi: 10.1007/s41030-020-00135-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- R Core Team, 2019. R: A Language and Environment for Statistical Computing.
- Rodríguez-Huerta M.D., Díez-Fernández A., Rodríguez-Alonso M.J., Robles-González M., Martín-Rodríguez M., González-García A. Nursing care and prevalence of adverse events in prone position: characteristics of mechanically ventilated patients with severe SARS-CoV-2 pulmonary infection. Nurs. Crit. Care. 2021 doi: 10.1111/nicc.12606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanghi P., Malik M., Hossain I.T., Manzouri B. Ocular complications in the prone position in the critical care setting: the COVID-19 pandemic. J. Intensive Care Med. 2021;36:361–372. doi: 10.1177/0885066620959031. [DOI] [PubMed] [Google Scholar]
- Shearer S.C., Parsa K.M., Newark A., Peesay T., Walsh A.R., Fernandez S., et al. Facial pressure injuries from prone positioning in the COVID-19 era. Laryngoscope. 2021 doi: 10.1002/lary.29374. [DOI] [PubMed] [Google Scholar]
- Simonnet A., Chetboun M., Poissy J., Raverdy V., Noulette J., Duhamel A., et al. High prevalence of obesity in severe acute respiratory syndrome Coronavirus-2 (SARS-CoV-2) requiring invasive mechanical ventilation. Obesity. 2020;28:1195–1199. doi: 10.1002/oby.22831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taccone P., Pesenti A., Latini R., Polli F., Vagginelli F., Mietto C., et al. Prone positioning in patients with moderate and severe acute respiratory distress syndrome. JAMA. 2009;302:1977. doi: 10.1001/jama.2009.1614. [DOI] [PubMed] [Google Scholar]
- Taito S., Sarada K., Guérin C. Prevalence of prone position use and complications among ventilated ARDS patients. Intensive Care Med. 2018;44:397–398. doi: 10.1007/s00134-018-5065-4. [DOI] [PubMed] [Google Scholar]
- Tang N., Bai H., Chen X., Gong J., Li D., Sun Z. Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy. J. Thromb. Haemost. 2020;18:1094–1099. doi: 10.1111/jth.14817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tayyib N., Coyer F. Effectiveness of pressure ulcer prevention strategies for adult patients in intensive care units: a systematic review. Worldviews Evidence-Based Nurs. 2016;13:432–444. doi: 10.1111/wvn.12177. [DOI] [PubMed] [Google Scholar]
- Voggenreiter G., Aufmkolk M., Stiletto R.J., Baacke M.G., Waydhas C., Ose C., et al. Prone positioning improves oxygenation in post-traumatic lung injury—a prospective randomized trial. J. Trauma Inj. Infect. Crit. Care. 2005;59:333–343. doi: 10.1097/01.ta.0000179952.95921.49. [DOI] [PubMed] [Google Scholar]
- Wichmann D., Sperhake J.-P., Lütgehetmann M., Steurer S., Edler C., Heinemann A., et al. Autopsy findings and venous thromboembolism in patients with COVID-19. Ann. Intern. Med. 2020;173:268–277. doi: 10.7326/M20-2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu C., Chen X., Cai Y., Xia J., Zhou X., Xu S., Huang H., et al. Risk factors associated with acute respiratory distress syndrome and death in patients with Coronavirus Disease 2019 pneumonia in Wuhan, China. JAMA Intern. Med. 2020;180:934. doi: 10.1001/jamainternmed.2020.0994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y., Zhuang Y., Shen J., Chen X., Wen Q., Jiang Q., et al. Value of pressure injury assessment scales for patients in the intensive care unit: systematic review and diagnostic test accuracy meta-analysis. Intensive Crit. Care Nurs. 2021;64 doi: 10.1016/j.iccn.2020.103009. [DOI] [PubMed] [Google Scholar]