ABSTRACT
Nutrient profiling (NP) models aim to assess the nutritional quality of individual foods, according to their energy content and nutrient composition. NP models, initially created to prevent obesity in high-income countries, have tended to penalize dietary energy by giving lower ratings to foods containing excessive calories, fat, sugar, and salt. Energy-driven NP models may need to be reconceptualized for use in low- and middle-income countries (LMIC) where hunger, undernutrition, and micronutrient deficiencies continue to be issues of public health concern. Consistent with the position of the WHO that the purpose of NP methods is to address an identified public health problem, NP models intended for use in LMIC ought to address inadequate intakes of vitamin A, B vitamins, folate, calcium, iron, iodine, and zinc and the frequent lack of high-quality protein. Those models of nutrient density that feature beneficial nutrients (high-quality protein, vitamins, minerals, and trace elements) may be better suited to LMIC needs than are some current NP models that are wholly based around nutrients to limit. NP models intended for LMIC and global use will also need to take food fortification into account. The challenge for LMIC public health agencies is how to balance the future risk of excess “empty” calories against the continuing danger of inadequate nutrients and micronutrient deficiencies that persist at the population level.
Keywords: nutrient profiling, Nutrient Rich Food index, Nutri-Score, Choices International, nutrient inadequacies, affordable nutrition, maternal and child health, fortified foods, cereal, OBAASIMA
Introduction
Nutrition security requires both dietary energy and nutrients (1, 2). The global food supply produces dietary energy from refined grains, vegetable oils, and added sugars at a relatively low cost (3–5). In high-income countries, lower-cost energy-dense diets have been associated with a higher risk of obesity and diet-related noncommunicable diseases (NCDs) (6, 7). As a dietary prevention measure, public health agencies recommend limiting dietary calories and replacing foods containing excess amounts of solid fats, added sugars, and salt with more healthful options (8–11).
Nutrient profiling (NP) models, designed to assess nutritional value of foods, have become an important public policy tool (12, 13). In general, energy density of foods and their nutrient density are inversely linked (13). The goal of NP models is to identify healthful nutrient-rich foods and rank them above foods of lower nutritional value (13). In high-income countries, NP models have provided the scientific rationale for numerous educational, labeling, regulatory, and tax initiatives (12, 13). NP models are the basis of multiple front-of-pack symbols and logos that communicate a given food's nutritional value to the consumer (14, 15). NP models have also provided the necessary benchmarks for product reformulation by the food industry (16, 17).
In its 2010 technical report (18), the WHO stated that the purpose of NP models was to promote the implementation of dietary guidelines by addressing a public health problem. Among high-income countries, the main health problem was the rising prevalence of obesity and diet-related NCD (7, 8). Early NP models, implemented in US supermarkets (19), were primarily intended to steer consumers away from excess dietary energy, fat, sugar, and salt (12).
The Dietary Guidelines for Americans (DGA) (9–11) defined nutrient-dense forms of foods as those that contained little or no added sugar or saturated fat. The concept of nutrient density has evolved along those lines. The 2005 DGA (9) introduced the concept of discretionary calories from SoFAAS (solid fats, alcohol, and added sugars). This was later changed to “empty” calories to reflect only dietary energy from solid fats and added sugars (SoFAS) (10, 20). Consistent with this approach, many NP models also defined nutrient density as the relative absence of dietary energy, sugar, and fat (21). The British Office of Communications (Ofcom) score (22) and its French derivation, Nutri-Score (23) penalized foods for excess dietary energy, sodium, total sugar, and saturated fat. Elsewhere, front-of-pack warning labels alerted consumers to excess energy calories, fat, sugar, and salt (14, 15). In this way, the nutritional value of foods came to be equated with the absence of problematic nutrients rather than with the presence of nutrients that a given food might actually contain (21).
The WHO technical report (18) noted that an internationally recognized NP methodology could have a wide range of global applications. However, that report (18) also cautioned that NP models developed to address a particular dietary or health problem in a given population might not readily be transferred to another. Among the LMIC, obesity prevalence is indeed on the rise (24, 25). However, hunger, undernutrition, and micronutrient deficiencies are still common and represent a continuing danger to population health (26–28).
Among the LMIC, dietary insufficiencies represent a major public health challenge, along with sanitation, clean water, and access to healthcare (2). First, dietary energy can itself be viewed as a shortfall nutrient among some population groups. Second, population diets can be deficient in selected micronutrients: vitamin A, thiamin, vitamin B-12 and calcium, iron, iodine, and zinc (26). Protein quality, never a component of NP models in high-income countries, can also be a problem across the LMIC, depending on the composition of the population diet (29, 30). In much of sub-Saharan Africa, the main protein source is still cassava, known to be deficient in essential amino acids (29, 30). LMIC public health agencies will need to balance the future risk of excess “empty calories” against the continuing danger of insufficient dietary energy, vitamins, minerals, and high-quality protein.
In light of the WHO caution (18), NP models designed to address dietary excesses, may not readily transfer to lower-income countries where dietary deficiencies are still the norm. The following principles should be followed. First, the new nutrient-density metrics need to address inadequate energy intakes, potential protein undernutrition, and still prevalent micronutrient deficiencies (26). Second, the new NP models will need to evaluate nutrient density of multiply fortified foods (31, 32). Third, affordable nutrient density needs to be addressed with reference to local food prices and to the local food supply (33).
The development of NP models ought to be transparent, using open-source nutrient composition databases and published nutrient standards (34, 35). The underlying nutrient-density algorithm ought to be made public, open to inspection and comment, and placed in the public domain (34, 35). Showing how some existing NP models may need to be adapted to the needs of LMIC is the purpose of this review.
How to Develop an NP Model
The need for electronic nutrient composition databases
High-quality local nutrient composition data in electronic format are the first prerequisite for developing NP models (see Box 1). The International Network of Food Data Systems (INFOODS) (36) maintained by the FAO is particularly useful. So is the high-quality SMILING database that covers Cambodia, Indonesia, Laos, Thailand, and Vietnam (37). Some of the databases are available in English and/or in languages other than English. The World Nutrient Databases for Dietary Studies (WNDDS) portal maintained by the Agriculture and Food Systems Institute (AFSI) shows where local data can be found (38). In some cases, access to such data is granted only on application to local agencies.
In the USA, USDA nutrient composition data are available for foods as purchased and for foods as consumed. The Standard Release SR-28 provides rich data on energy and nutrients for >7000 foods as purchased (39). The Food and Nutrient Database for Dietary Studies (FNDDS) (40) provides energy and nutrient data on foods as consumed in the NHANES. Preparation methods are included as well. Data are available on energy, macronutrient content, and a wide range (>50) of vitamins, minerals, trace elements, and other dietary constituents, including flavonoids (41). Amino acid profiles, useful for calculating protein quality, are available for some foods. Added sugar content is missing but can be obtained from other USDA data sources.
The USDA Branded Food Products Database (BFPDB) (42) lists 239,069 branded foods as purchased but only lists those nutrients that appear on the Nutrition Facts Panel or for which a nutrient content claim is made. The BFPDB also includes an electronic ingredient list, never previously captured by the USDA. Fortification patterns in the BFPDB (42) can be inferred through a machine scan of the ingredient list.
The USDA nutrient composition data, available on FoodData Central (39), have served to populate many regional databases, especially when it comes to raw, unprocessed foods. However, it must be noted that the composition of branded processed foods sold in the USA may not be the same as that of seemingly equivalent foods sold in the LMIC. In those cases, USDA food composition data may not be suitable for the LMIC and alternative data sources will need to be found.
Ultimately, the nature of NP models will depend on the extent and quality of the available nutrient composition data. Given lack of such data, it will be necessary to scan food company websites and product labels. Small and mid-size food enterprises may not have detailed information available. Fortification patterns for processed foods may vary from one region to another, even for products from the same manufacturer. Developing nutrient composition databases for branded food products ought to be a priority of LMIC public health research.
A choice between across-the-board and category-specific NP models
Decision steps to developing an NP model are summerized in Box 2. Across-the-board NP models apply the same standards across all food groups (34, 35). As a result, some food groups score low, even if they are an integral component of a healthy diet. Vegetables and fruit generally score high, especially in their unprocessed nutrient-dense forms, that is without the addition of either sugar or fat. By contrast, foods that are high in energy tend to score poorly. Nuts and seeds score low in several NP models because of their high energy density and high fat content. Many cheeses score low because of high sodium and saturated fat content. Arguably, NP ought to do more than emphasize the well-known differences in the nutritional value across different food groups.
Favored by the food industry, category-specific NP models help identify “best of class” items within a given food group (43). Category-specific models apply different nutrition standards to different food groups (44). NP models that follow product lines (cereals, yogurts, snacks) have provided useful benchmarks for innovation and product (re)formulation. However, assigning foods into groups, subgroups, and categories can be a challenge in itself. Multiple ways to aggregate individual foods into food groups have been tried, often based on the contribution of the food group(s) to the total diet.
For example, in a well-balanced diet of high-income nations, certain food groups are sources of specific nutrients (9–11). Milk is a major food source of riboflavin, vitamin B-12, calcium, and phosphorus, whereas meat is a major food source of protein, vitamins B-6 and B-12, niacin, iron, and zinc. In the USA, milk is fortified with vitamin D. Grains are the main food sources of fiber, thiamin, folate, iron, and magnesium. Vegetables are major food sources of fiber, vitamins A and B-6, potassium, and copper, whereas fruit contributes to vitamin C. Milk, butter, oils, and salad dressings are the food sources of essential fatty acids (linoleic, α-linolenic acids) and vitamin E (9–11).
The USDA FNDDS (40), used in What We Eat in America studies, classifies foods into groups, subgroups, and categories based on their nutrient content. The 1-digit FNDDS codes identify 9 major food groups: milk and milk products; meat, poultry, and fish; eggs, dry beans and legumes, grains, fruits, vegetables, fats and oils, and sugars, sweets, and beverages. The 2-digit FNDDS codes identify 38 food subgroups. The dairy group is now split into milks and yogurts, creams, dairy desserts, and cheeses. The meat group is split into beef, pork, lamb, poultry, organ and processed meats, fish and shellfish, mixed meat dishes, and soups. The 4-digit FNDDS codes identify >100 food categories. The 8-digit codes correspond to the individual foods (N >7000).
Processed foods and beverages can also be significant sources of added fat, sugars, and sodium that are added to foods in the course of transformation or industrial processing. The Choices International NP model (formerly Unilever) has based its food categories on food processing and frequency of food use (44–46). The Choices model separates foods into core foods, nonessential snacks, beverages, and milk replacements (46). Treated as basic food groups are dairy, meat, fish, poultry and eggs, nuts and seeds, complex carbohydrates, fruits and vegetables, fats and oils, and composite meals. Treated as nonessential foods are snacks, fruit and vegetable juices, soups, and beverages. The Nestlé Nutritional Profiling System, used to aid product innovation, is also category specific and to some extent aligned with product lines (47).
Food categories created for educational, research, or administrative purposes in high-income countries may not correspond to perceived food categories in LMIC. Deciding how to categorize foods into groups demands some expert knowledge and may be informed by ethnographic research. Categorization schemes may vary by region and by the characteristics of the population of interest.
How to select NP nutrients to limit
Nutrients to limit in NP models typically include saturated fat, total or added sugar, and sodium (46–48) but can also include energy (22). The UK Ofcom model assigned negative points to food energy, saturated fat, total sugar, and sodium (22). Saturated fat, added sugar, and sodium were the negative elements in the French SAIN, LIM nutrient profiling modelsystem in France (49) and the Nutrient Rich Food (NRF) index in the USA (34, 35, 50).
NP models have also used total, added, and “free” sugar. Total sugars include sugars in milk (lactose) and fruit (sucrose and fructose); added sugars are those used in food preparation and processing (sucrose and high-fructose corn syrup); free sugars are those in fruit juice, honey, and molasses. However, there are potential technical limitations. In the USA, the FDA requires that the amount of and percent daily value for added sugar be declared on the new Nutrition Facts Label. Elsewhere, data on added sugar may not be available and may need to be imputed from a variety of sources including recipes, if needed. For that reason, some NP models applied to processed foods have used total as opposed to added sugar.
By treating dietary energy as another nutrient to limit, along with sugar and fat, both Ofcom and Nutri-Score NP models have effectively penalized energy-dense foods. Given that the fat and sugar content of foods are highly correlated with total energy content, such scores are likely to be colinear with energy density, without capturing the nutrient density of foods. The use of energy-driven NP models can become problematic in the context of hunger, undernutrition, and micronutrient deficiencies that are still prevalent among LMIC.
Those NP models that penalize energy-dense foods were specifically designed for obesity prevention in wealthy societies (18). Adapting such models to the nutrition needs of the LMIC will require more attention to local or regional micronutrient deficiencies and other nutrient needs. In the NP terminology, those nutrients are commonly referred to as “nutrients to encourage.”
How to select nutrients of public health concern
The positive nutrients in NP models have been variously called qualifying nutrients, nutrients of concern, or nutrients to encourage (34, 35, 50). Their selection has been based on local regulatory frameworks and on dietary guidance. Based on analyses of nationally representative data and other sources, the 2005 DGA identified vitamins A, C, and E, and calcium, magnesium, and potassium as nutrients of concern (9). Vitamins B-12 and E, folate, and iron, consumed in inadequate amounts by some population subgroups in the USA, were also identified as nutrients of concern. The 2010 DGA singled out vitamin D, calcium, potassium, and dietary fiber (10). The new Nutrition Facts panel in the USA, regulated by the FDA, lists the amount of energy per serving, and the amounts of total fat, saturated and trans fat, cholesterol, sodium, total carbohydrate, dietary fiber, total sugars (and added sugars), protein, vitamin D, calcium, iron, and potassium (51). Not by coincidence, many of those nutrients are included in current NP models as shown in Table 1.
TABLE 1.
Nutrients to encourage in nutrient profiling models1
| NP model | Macronutrients | Vitamins | Minerals |
|---|---|---|---|
| Nutrient Rich Food NP model | |||
| NR5 | Protein, fiber | Vitamin C | Ca, Fe |
| NR6 | Protein, fiber | Vitamins A, C | Ca, Fe |
| NR7 | Protein, fiber | Vitamins A, C, E | Ca, Fe |
| NR10 | Protein, fiber | Vitamins A, C, E, B-12 | Ca, Fe, Zn, K |
| NR11 | Protein, fiber | Vitamins A, C, E, B-12 | Ca, Fe, Mg, Zn, K |
| NR12 | Protein, fiber | Vitamins A, C, E, thiamin, riboflavin, B-12 | Ca, Fe, Zn, K |
| Naturally Nutrient Rich NP model | |||
| NNR | Protein, MUFA | Vitamins A, C, D, E, thiamin, riboflavin, B-12, folate | Ca, Fe, Zn, K |
| Nutrient Density Score NP model | |||
| NDS16a | Protein, fiber, linolenic acid, DHA | Vitamins C, D, E, thiamin, riboflavin, B-6, folate | Ca, Fe, Mg, Zn, K |
| NDS16b | Protein, fiber | Vitamins A, C, D, E, thiamin, riboflavin, niacin, B-6, B-12, folate, pantothenic acid | Ca, Fe, Mg |
Among the NP nutrients to encourage are protein, fiber, and a variety of vitamins, minerals, and trace elements. The NRF family of scores has used anywhere from 5 to 23 nutrients to encourage (52–54). The NR6 model was based on protein, fiber, vitamin A, vitamin C, calcium, and iron, the same 6 nutrients that the FDA has used to support nutrient content claims (52, 53). The NR9 model added 3 nutrients of concern from the 2005 DGA (vitamin E, magnesium, and potassium). To those, the NR11 model added vitamin B-12 and zinc. The original Naturally Nutrient Rich NP model was based on 14 nutrients to encourage: protein, MUFA, vitamins A, C, D, E, and B-12, thiamin, riboflavin, folate, calcium, iron, potassium, and zinc (21).
First, the pattern of nutrient deficiencies among LMIC may not be comparable to the excesses and deficits observed in wealthy societies (55). Second, food sources of common nutrients can be very different, especially among those countries with the traditional diet of starchy staples (56). Specific nutrient deficiencies in LMIC include but are not limited to vitamin A, vitamin D, riboflavin, folate, iodine, calcium, iron, and zinc (26). Adequate protein quality (from animal or plant sources) is another emerging issue (57, 58).
The colinearity among nutrients from common food sources meant that there was no need to include multiple nutrients in the same model. For example, calcium and phosphorus co-occur in dairy foods and there are strong correlations in animal products between total and saturated fat. However, in some food cultures, most dietary fat comes from plant as opposed to animal sources and the relations among nutrients may no longer be the same.
How to select nutrient standards
The Codex nutrient reference values listed by the FAO (59) are summarized in Table 2. The values are those listed in the WHO/FAO Vitamin and Mineral Requirements in Human Nutrition (60). These can be replaced by local standards when available. Nutrient standards for the US-based scores have used the FDA Reference Daily Values that are posted on the back-of-pack nutrition labels (52). French-based NP models have used the standards for France (50).
TABLE 2.
FAO Codex nutrient reference values1
| Nutrient | Standard | Nutrient | Standard |
|---|---|---|---|
| Protein | 50 g/d | Calcium | 1000 mg/d |
| Fiber | 25 g/d | Magnesium | 310 mg/d |
| Vitamin A | 800 μg RE/d | Iron | 14 mg/d (at 15% absorption)22 mg/d (at 10% absorption) |
| Vitamin D | 5 μg/d; 15 μg/d if no sunlight | Zinc | 11 mg/d (30% mixed diet)14 mg/d (22% cereal-based diet) |
| Vitamin C | 100 mg/d | Iodine | 150 μg/d |
| Vitamin K | 60 μg/d | Copper | 900 μg/d |
| Vitamin E | 9 mg/d | Selenium | 60 μg/d |
| Thiamin | 1.2 mg/d | Phosphorus | 700 mg/d |
| Riboflavin | 1.2 mg/d | Potassium | 3400 mg/d (FDA) 3510 mg/d (WHO) |
| Niacin | 15 mg/d | ||
| Vitamin B-6 | 1.3 mg/d | Saturated fat | 22 g/d |
| Folate | 400 μg/d | Total sugar | 125 g/d (IOM); 90 g NP standard |
| Vitamin B-12 | 2.4 μg/d | Added sugar | 50 g/d (FDA) |
| Pantothenic | 5 mg/d | Sodium | 2000 mg/d (WHO) |
IOM, Institute of Medicine; NP, nutrient profiling; RE, retinol equivalents.
Fortification of foods with vitamins and minerals has emerged as a major nutrition intervention strategy for LMIC (31, 32). However, most nutrient composition databases do not clearly distinguish between foods that are fortified and those that are not. There is an additional distinction to be made between mandatory and voluntary fortification. At this time, many NP models do not award higher scores to fortified foods, effectively not taking vitamin and mineral content of foods into account.
How to determine the basis of calculation: 100 kcal, 100 g, or serving size
The nutrient density of foods is calculated per reference amount, which can be 100 g, 100 kcal, or serving size. The choice of the basis of calculation was most often driven by the local regulatory demands. For example, in the USA, all regulations and food labels are based on serving size (51). The calculations on the Nutrition Facts Panel are based on servings, defined as Reference Amounts Customarily Consumed or RACC (59). The FDA has defined 139 different RACC values for different foods. RACC values are set lower for energy-dense sugar (4 g), fats and oils (15 g), and cheeses (30 g) than for meats (85 g), vegetables and fruit (120 g), or for milk, juices, and other beverages (240 g).
By contrast, dietary information in the EU is provided per 100 g. Models based on the 100 g standard have difficulty handling different serving sizes by food group, given that typical serving sizes run from 15 g for oils to 240 g for beverages. Models whereby saturated fat, added sugar and sodium are calculated per 100 g of food or beverage, tend to penalize energy-dense foods consumed in small quantities (nuts, dried fruit, cheese), while giving favorable scores to sugary beverages of low energy density, unless volume corrections are made. The basis of calculation can also be combined within a single model; for example, the French SAIN, LIM model used 100 kcal as the basis for nutrients to encourage but 100 g for nutrients to limit (49).
How to select the NP algorithm
The calculated NP scores can be continuous (numbers or letter grades) or dichotomous (yes/no). The Nutri-Score and the NRF are both continuous scores whereas Choices uses the pass/fail system.
The Nutri-Score awards “bad” N points based on the food's content of energy, saturated fat, total sugar, and sodium and good C points based on protein, fiber, and the food's percent by weight of vegetables, fruit, nuts, and legumes. For protein, point scores range from 0 to 5 based on total protein content (from any source) per 100 g of food. Foods with total protein content of ≤1.6 g/100 g are given 0 points, whereas those with >8 g/100 g are given full 5 “C” (good) points. By way of comparison, beef sirloin trimmed contains 36.1 g/100 g protein, grilled chicken breast contains 30.9 g/100 g protein, and frozen fish fillet contains 27.2 g/100 g protein. However, the Nutri-Score algorithm counts protein points only if the food contains 80% fruit, vegetables, nuts, or legumes. Otherwise protein content does not contribute to the final score.
The NRF index is based on 2 subscores: NR and LIM. The NRn subscore is based on a variable number n of nutrients to encourage whereas the LIM subscore is based on the same 3 nutrients to limit (saturated fat, total or added sugar, and sodium). The NRn subscore is the sum of percent daily values for n nutrients to encourage. The examples below show how to calculate NRn and LIMt subscores per 100 g. In this formulation, amount i is the amount of nutrient i in 100 g of food and DVi is the reference daily value for that nutrient. The final NRF algorithm is given by NRFn.3 = NRn – LIMt, where
 |
(1) |
 |
(2) |
The amounts were expressed in percentage of DV per 100 g and summed over all nutrients. As in past calculations, percent DVs for nutrients were truncated at 100%. Maximum recommended values (MRVs) for saturated fat, sugar, and sodium were used for nutrients to limit.
How to decide on nutrient balance
Some NP models balance nutrients to limit against nutrients to encourage; other models do not. Noncompensatory NP models are typically based on the food's content of fat, sugar, and salt. Beneficial nutrients (if any) do not affect the final score. This is consistent with the position of the US FDA, which disqualifies foods from posting nutrition and health claims if they contain amounts above the specified limits for fat, saturated fat, trans fat, cholesterol, and sodium per serving. A food cannot claim to be “low in sodium” if it is high in total or saturated fat.
The Nutri-Score can be viewed as partly compensatory because the good scores can be subtracted from the bad scores. However, good protein points are taken into account only when the fruit, vegetables, legume, and nut subscore equals to or exceeds 5 points. For that to occur, the fruit, vegetable, legume, and nut content of foods has to exceed 80%. Otherwise only fiber content is used to arrive at the final score. The NRF is fully compensatory because it is based on the arithmetic difference between the 2 subscores.
How to approach model validation
Developing validation techniques is an essential component of nutrient profiling (34, 35, 50). Approaches to validating NP models have looked for correlations across different models or compared generated scores to professional opinion (50). Models were also tested with respect to energy density and price (52, 53, 61). The goal was to ensure that high scoring foods were not simply those foods that were more expensive (52, 61). Other approaches looked for correlations between nutrient density scores and other independent measures of diet quality such as the Healthy Eating Index (HEI), a measure of compliance with each successive edition of the US Dietary Guidelines (34, 35).
The best correspondence between individual NRF values and HEI-2005 scores for NHANES participants were obtained for an NP model based on 9 nutrients to encourage (protein, fiber, vitamins A, C and E, calcium, iron, potassium, magnesium) and 3 nutrients to limit (saturated fat, added sugar, and sodium) (50). One caution is that the HEI reflects US dietary goals and may not apply to LMIC. Development of LMIC diet quality indices that are not so culture bound would be another requirement.
Even though some models have included as many as 23 or even 40 nutrients (54), in general, NP better correlations with HEI scores, an independent measure of a healthy diet, were obtained with a more restricted number. Published validation studies that compared NP models with an independent measure of a healthy diet pointed to performance optima of ∼9–12 nutrients (50).
Affordable Nutrient Density in NP Models
Affordable nutrient density is the main theme of the 2020 FAO report on transforming food systems for affordable healthy diets (28). Affordable nutrient density in African countries including Ghana is also the main theme of the CANDASA project funded by the Bill and Melinda Gates Foundation (BMGF) and conducted by the Friedman School, IFPRI, and local partners (62). An earlier project on Indicators of Affordability of Nutritious Diets in Africa (IANDA) was funded by the BMGF and the UK Department for International Development (62). The importance of collecting prices for nutrient-rich foods is also noted in a recent IFPRI report on the cost of a nutritious diet in Myanmar that examines the cost of nutrient-rich foods relative to starchy staples (63).
Food affordability is one measure of food access in any society. One problem with NP models is that they generally tend to award more favorable scores to more costly foods (34). Assuring access to affordable nutrient-dense foods across the LMIC can be a particular challenge. First, food affordability continues to be framed as the cost of dietary energy, that is to say calories per unit cost. The FAO report (28) stressed that healthy diets may be, on average, 5 times more expensive than diets that only meet energy needs through a starchy staple. Cost analyses of the EAT Lancet report (64) showed that the recommended diets were not, in fact, affordable to the global poor. The FAO concluded that for consumers to switch to healthier options, the cost of nutritious foods must come down (34). When it comes to dietary energy, healthy nutrient-rich foods that are low in energy tend to cost more (61). There is ongoing work on the cost of nutrient density, that is to say nutrients per unit cost. Here, NP models can provide a common denominator for new metrics of affordable nutrient density that are well suited to the LMIC (61, 64). Other measures of food access can also be critical in a specific LMIC context.
Assessing affordable nutrient density ought to be a key component of NP models intended for LMIC and for global use (62, 63). The point of NP modeling is to identify healthier foods and not necessarily those foods that are more expensive (52). To test for this, it will be necessary to join nutrient composition data with a national food prices database (62, 63, 65) or with locally sought retail prices (66). One question of interest is whether product fortification with protein, vitamins, and minerals is a cost-effective way to improve the nutrients-to-calorie ratio of common foods.
Ghana—a Case Study
Ghana is one country with a double burden of malnutrition. The Ghana Demographic and Health Survey (67) reported that nearly 22% of nonpregnant women were anemic, linked to deficiencies in dietary iron and provitamin A. Folate deficiency was high (>50%) and vitamin B-12 deficiency was reported in 6.9%. Mandatory fortification policies in Ghana apply to vitamin A in vegetable oil (≥10 mg/kg for vitamin A) and to iron, zinc, B vitamins, and vitamin A in wheat flour (68). In the 2017 Ghana micronutrient survey (69), no significant micronutrient differences across socioeconomic strata were observed. However, nearly one-quarter of women were overweight, and nearly 15% were obese.
Micronutrient deficiencies across LMIC are remedied by mandatory or voluntary fortification of food products. One approach to food fortification in Ghana is provided by the OBAASIMA campaign (70, 71). Launched in February 2017, OBAASIMA is a market-based health promotion scheme addressing micronutrient deficiencies across the food chain, from production to supply to demand creation. The OBAASIMA scheme is regulated by the Ghana Standards Authority and co-ordinated by the Association of Ghana Industries. The OBAASIMA fortified foods for women and children (71) are fortified with 18 vitamins and minerals. Included are water-soluble vitamins (riboflavin, thiamin, niacin, vitamins B-6 and B-12, vitamin C, folic acid), fat-soluble vitamins (vitamin A, vitamin D-3, vitamin E, vitamin K), minerals (calcium, magnesium), and trace elements (iron, zinc, iodine, copper, selenium). OBAASIMA-fortified products included in the present analyses were porridge mixes, enriched shortcake, and beverages. OBAASIMA is a trusted consumer symbol for fortified foods which is aimed at increasing the availability of and access to affordable, safe, and nutritious foods in Ghana.
NP of selected foods in Ghana
The present goal was to assess nutrient density of selected foods sold in Ghana, with special attention to fortified products. Foods for nutrient density evaluation were selected from 4 categories: porridges, cereals, biscuits, and beverages (both reconstituted and dry mix). Among these were fortified foods consumed by young children and women of childbearing age. Relevant to NP methodology, the foods were mostly cereal based and did not contain significant amounts of fruit, vegetables, legumes (other than soy protein), nuts, or seeds.
There was no central repository of nutrient composition for commercially sold foods in Ghana. The FAO/INFOODS Food Composition Table for Western Africa (72) was mostly composed of raw unprocessed foods, did not list any branded foods, and was unsuited for the present purpose.
As a result, nutrient composition data for selected foods had to be collected during store visits or came from photographed nutrient content labels from the internet and company websites. For example, data for Cerelac, a dry cereal, came from product nutrition fact panels that were photographed and posted online. For verification purposes, those nutrient values were compared to comparable products listed on company websites and to the USDA Branded Food Products and SR-28 Legacy databases. One caution is that the composition of infant cereals sold in the USA is not necessarily the same as in Ghana.
The final demonstration database of 43 foods had some gaps that needed to be addressed. Nutrient composition data for vitamins, minerals, and trace elements were largely incomplete. Vitamins and minerals were listed on back or pack labels and/or among product ingredients only in those cases when fortified porridges and cereals made nutrition content claims. For many nutrients, no data were available. There were no reliable data on potassium and very limited data for magnesium. Copper and selenium data were not available. Saturated fat data were not always provided and had to be imputed based on comparisons with similar products. Total sugar data were provided but added sugar data were not. As a result, the LIM subscore of the NRF nutrient density score had to be based on total as opposed to added sugar.
The present goal was to assess the performance of Choices and Nutri-Score nutrient density scores relative to the Nutrient Rich approach. Both Choices and Nutri-Score penalize dietary energy, fat, sugar, and salt and do not take fortification with vitamins and minerals into account. As a result, neither score was affected by the missing data on vitamins and minerals. However, incomplete nutrient composition data meant that the NRF score had to be adapted to capture the nutrient density of foods using the data at hand. Potassium and magnesium had to be dropped, given lack of data. So was vitamin C, not usually found in porridges and cereals.
Choices International, Nutri-Score, and NRF models
The Choices model (21) provides dichotomous scores (yes/no) that are category specific. The scoring criteria for the product categories selected were based on energy, saturated fat, total or added sugar, and sodium. Fiber was the positive nutrient. Only Incaparina, the standard corn and soy cereal mix, met the Choices standards, whereas all other products failed. With the exception of the OBAASIMA LolaMilk shortcake, all snacks exceeded energy limits, set at 110 kcal/portion or (∼) 363 kcal/100 g and all sweet snacks exceeded the allowed total sugar content. All reconstituted beverages failed the calorie limitation of <10 kcal/100 g. All beverage dry mixes, assigned to the other products category, failed the total sugar criterion.
The final Nutri-Score was determined by negative (N) score points minus fiber points (73). None of the products tested contained a minimum of 80% by weight of fruit, vegetables, legumes, nuts, or healthy oils so that component of Nutri-Score was set to zero.
Figure 1 shows a scatterplot of Nutri-Score values plotted against the LIMt subscore. In both cases, higher values denote lower nutritional value. Nutri-Score grades are as follows: –1 or less = A; 0 to 2 points = B; 3 to 10 points = C; 11 to 18 points = D; and >19 points = E. The LIMt subscore, based on saturated fat, total sugar, and sodium, was calculated per 100 g (Figure 1A) and per 100 kcal (Figure 1B). First, Nutri-Score was colinear with the LIMt component of the NRF nutrient density score (correlation coefficient was 0.93). Second, Nutri-Score separated foods into 2 groups, largely based on their total sugar content (r = 0.82), saturated fat (r = 0.73), and overall energy density (r = 0.51) but did not capture the higher nutrient content of multiply fortified foods. It would appear that Nutri-Score may not be the NP system that is best suited to address micronutrient inadequacies across LMIC. The content of vitamins and minerals in the healthy group (which included OBAASIMA products) was not the main discriminating factor.
FIGURE 1.
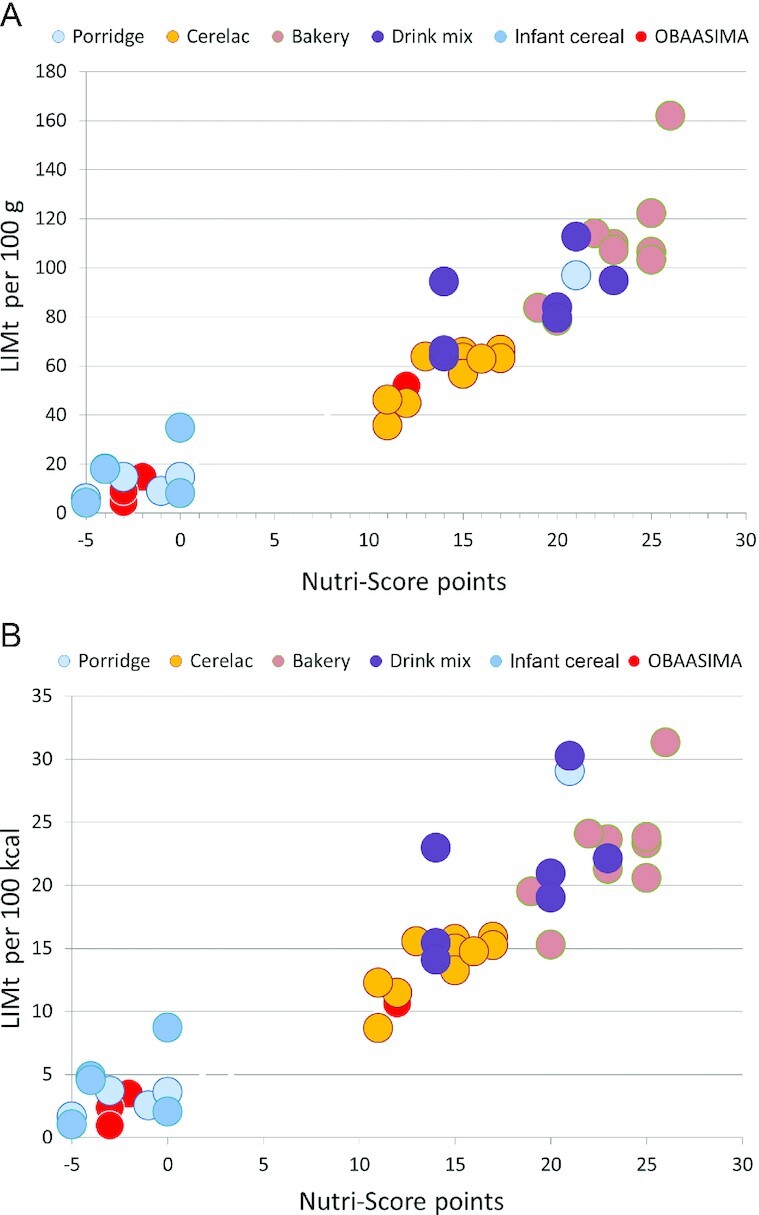
Scatterplot of Nutri-Score plotted against LIMt subscore of the Nutrient Rich Food (NRF) index by product type. LIMt per 100 g (A); LIMt per 100 kcal (B). LIMt, limiting subscore of the NRF index based on added sugar; OBAASIMA.
The newly developed NR9 subscore shown in Figure 2 was based on 9 positive nutrients: protein, fiber, vitamin A, thiamin, vitamin D, folate, calcium, iron, and iodine. All nutrients were calculated as percent daily values per 100 g (Figure 2A) or per 100 kcal (Figure 2B). For Nutri-Score, lower values denote higher nutrient density; the opposite is true of NRF index scores. Both scatterplots show that the Nutri-Score discriminated on the basis of energy density, giving lower (i.e. better) scores to foods that were lower in energy, total sugar, and saturated fat. The higher nutrient content of fortified infant cereals was reflected by the Nutrient Rich NR9 subscore but not by Nutri-Score.
FIGURE 2.
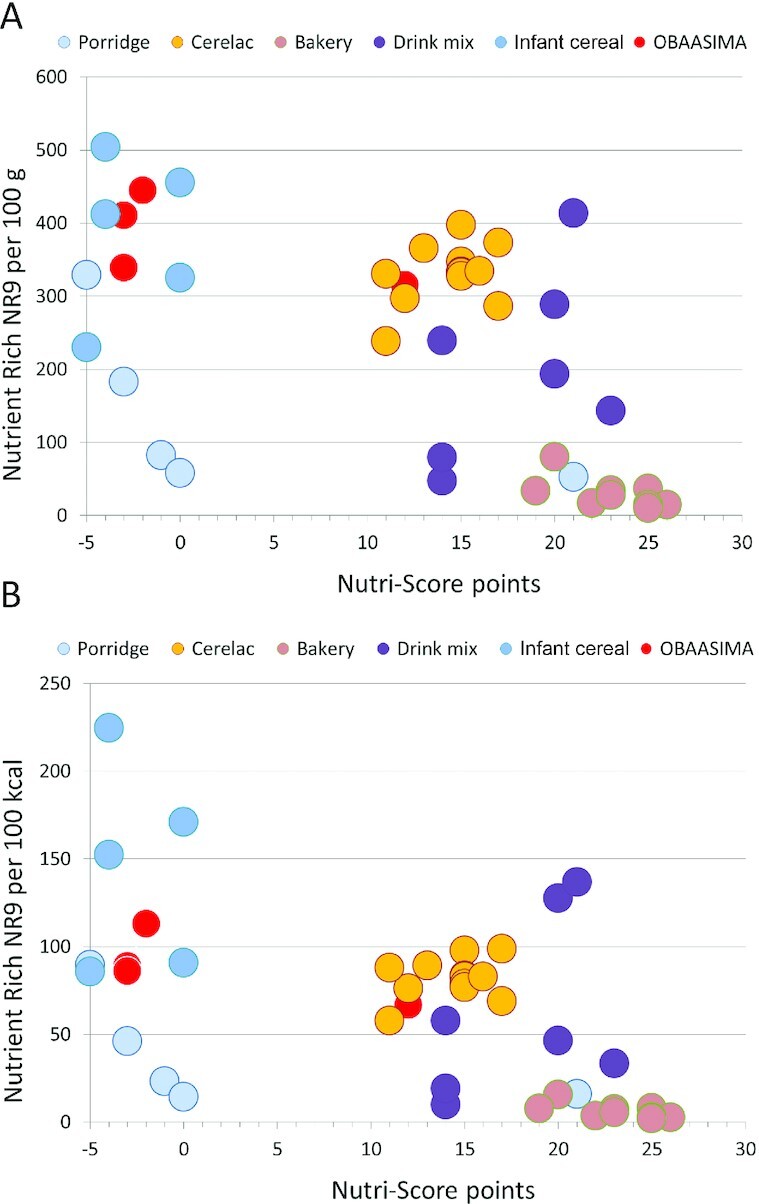
Scatterplot of Nutri-Score plotted against NR9 subscore of the Nutrient Rich Food (NRF) index by product type. NR9 per 100 g (A); NR9 per 100 kcal (B). OBAASIMA.
Figure 3 shows the relation between Nutri-Score and the newly developed NRF9.3 index by product type. All nutrients were calculated as percent daily values per 100 g (Figure 3A) or per 100 kcal (Figure 3B). The scatterplots below show how the NRFn.3 can separate products that are fortified and enriched from those that are not. At the same time, the NRF9.3 algorithm does take saturated fat, total sugar, and sodium into account.
FIGURE 3.
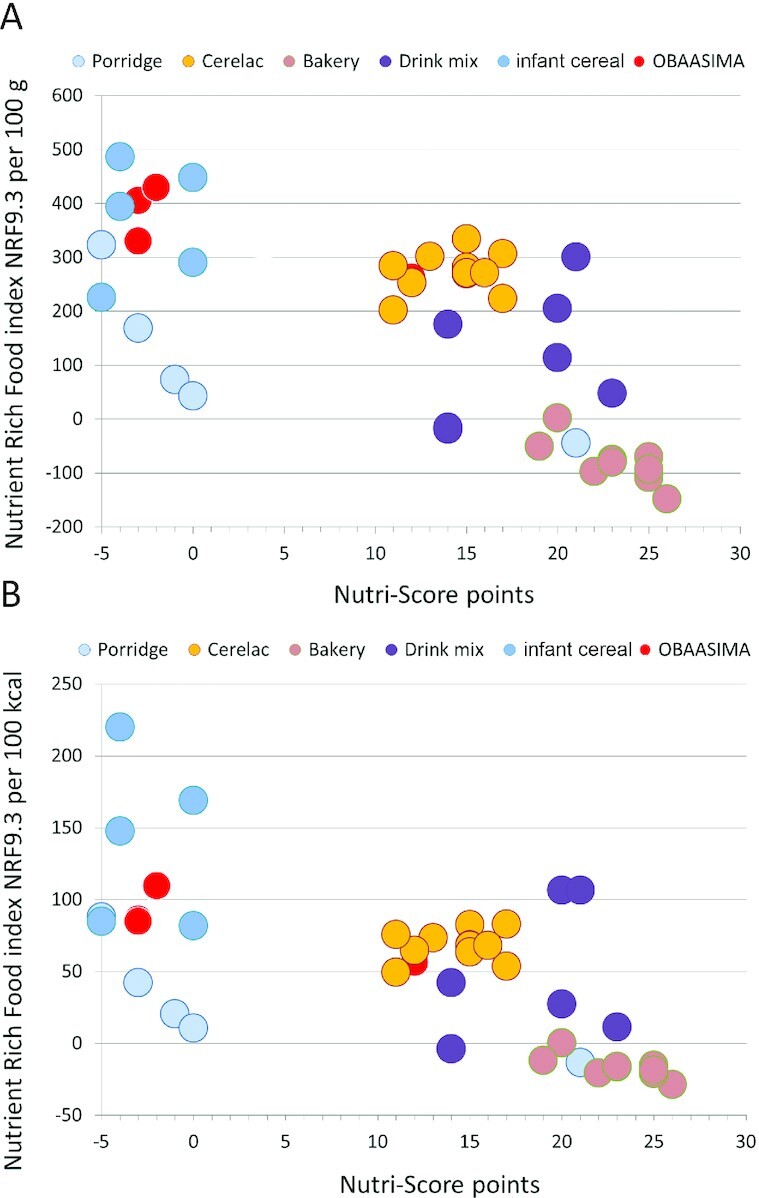
Scatterplot of Nutri-Score plotted against NRF9.3 index scores by product type. NRF9.3 per 100 g (A); NRF9.3 per 100 kcal (B). OBAASIMA.
Limitations of applying NP models to foods in Ghana
Any potential NP models intended for use in Ghana or across the LMIC will be limited by the availability and quality of local nutrient composition, prices, and health data. Extrapolating from other nutrient databases, including those from the USDA may not fill all the gaps. Some considerable investment in maintaining INFOODS and in developing local nutrient composition databases will be required. Whereas large companies have the resources to screen the quality of their product portfolios using NP methods, small and midsize enterprises in Ghana and elsewhere may not. There are multiple opportunities for monitoring and improving nutrient density of the LMIC food supply.
Second, the still prevalent energy and micronutrient deficiencies across the LMIC pose a challenge to the standard concept of nutrient density. The WHO suggested that the main purpose of NP models was to address an identified public health problem (18). For high-income societies, that problem was preventing obesity and NCD risk, most prevalent among lower-income groups. For LMIC, the identified public health problem is preventing undernutrition and micronutrient deficiencies, also most prevalent among lower-income groups. In LMIC, persistent undernutrition and child stunting now coexist with the rising prevalence of adult overweight. There is an unfinished agenda for food fortification (63) in the LMIC that has brought about improved micronutrient status and better health outcomes. There is a need for NP models that capture the nutrient density of foods, and especially fortified foods, as opposed to energy density alone.
Such NP models can contribute to assessments of nutrition security across the LMIC. There are strong associations between nutritional status, infectious diseases, and other indicators of health including child growth and maternal mortality (74). In particular, further validation work will be needed in order to link NP models of food or dietary nutrient density with objectively assessed health outcomes (75, 76). For example, the UK Food Standards Agency nutrient profiling system (FSAm-NPS) awards higher scores to foods containing more added sugar and saturated fat. In 10 European countries, mostly high income, consuming higher-scoring foods (i.e. lower quality diets) was associated with a higher mortality for all causes and for cancer and diseases of the circulatory, respiratory, and digestive systems (77). However, linking NP models with health outcomes is region or population specific and depends on the leading causes of a health burden in a given society. In LMIC, that would include an association between NP models and the prevalence or risks of micronutrient deficiencies or other objectively assessed health outcomes. Such work in the LMIC will require access to additional databases that may not be available at this time.
Finally, NP models intended to improve diet quality of the global poor ought to take food prices and likely diet costs into account (62, 63). The relative caloric prices for “empty” calories and for healthy foods differ systematically across countries and income levels (62, 63). This is the outcome of deliberate agricultural policies that have for years promoted the production of low-cost dietary energy, sometimes at the expense of more nutrient-dense specialty crops. There is an economic gap between the low-cost diets of minimal nutritional value and the higher-cost more "prudent", and more nutrient-rich diets. NP models, when used as an evaluation metric, should not become the tool that aggravates the existing social disparities in food access and contributes to inequities in diets and health (78).
Summary and Conclusion
The initial goal of most NP models was to prevent obesity in high-income countries by penalizing energy-dense foods. Many such NP models are unable to track nutrient density of fortified foods and cannot assist in efforts to improve nutrient density of the food supply in Ghana and across the LMIC (31). New NP models intended for LMIC use need to address the still prevalent vitamin and mineral deficiencies. Assuming access to nutrient composition data, the development of such models can follow already established principles and guidelines.
Box 1: Nutrient composition and other data needs.
• Nutrient composition database in electronic format that lists energy and nutrient content of foods in standard units (g, mg, μg, or IU) per 100 g edible portion.
• Branded product databases are useful for screening nutrient density of manufacturers’ product lines.
• Many NP models require data on protein, fiber, total fat, saturated fat, total sugar, and sodium. Data on added sugars may not be available.
• Protein quality is an emerging issue. Separation of protein content by source (meat, dairy, plant) will be useful.
• Locally important nutrients need to be included. Vitamins and minerals ought to include vitamin A, riboflavin, thiamin, niacin, vitamins B-6 and B-12, calcium, iron, zinc, potassium, and sodium. Data on folate and iodine should be included if available.
• The WHO/FAO Vitamin and Mineral Requirements in Human Nutrition Codex standards may be used when local standards are not available.
• A regional food prices database (cost per 100 g edible portion) will be essential for any future assessments of affordable nutrient density.
• Electronic ingredient lists (if available) will be useful for identifying fortified foods.
• Recommended portion size in grams is useful as a potential base of calculations.
Box 2: Decision steps to developing an NP model.
• Decide on the nutrient composition data that you want to use. Does it include branded foods?
• Decide whether the model should be across-the-board (all foods) or category specific (“best of class”). Are there clear ways to assign foods into groups or categories?
• Select nutrients to limit. Is the usual choice of dietary energy, saturated fat, total or added sugar, and sodium suitable to local needs? Should dietary energy be penalized?
• Select nutrients of public health concern. Decide whether the model includes vitamin A, calcium, iron, and zinc. What about vitamins B-6, B-12, and vitamin D? Are there other regional needs?
• Address protein quality. Decide whether animal proteins should be scored higher than some plant proteins.
• Select nutrient standards. If no local recommendations exist, use WHO/FAO standards.
• Decide on the basis of calculation: 100 g, per 100 kcal, or serving size.
• Decide whether the NP models should be compensatory. Should NP scores balance beneficial nutrients against nutrients to limit?
• Formulate the NP algorithm. Do you want a continuous score (letter or number) or a simple yes/no?
• Compare with other NP models using the same database.
Acknowledgments
The authors’ responsibilities were as follows—BG-S and AD conceptualized the study. DA led the development of the Ghana database; AD took the lead on data analysis and the writing of manuscript; all authors contributed to the writing and revisions and read and approved the final manuscript.
Notes
This study was supported by the Sight and Life Foundation. DA collected nutrient composition data for Ghana foods, including OBAASIMA products. The funders were not involved in the development of nutrient profiling models or data analysis and interpretation. The funders were involved in manuscript preparation and the decision to submit the manuscript for publication.
Author disclosures: AD is the developer of the Nutrient Rich Food (NRF) index, a nutrient profiling model, and has received grants, contracts, and honoraria from entities, both public and private, with an interest in nutrient density of foods, complex meals, and the total diet. DA and BG-S are with the Sight and Life Foundation. DA and BG-S report no conflicts of interest.
Perspective articles allow authors to take a position on a topic of current major importance or controversy in the field of nutrition. As such, these articles could include statements based on author opinions or point of view. Opinions expressed in Perspective articles are those of the author and are not attributable to the funder(s) or the sponsor(s) or the publisher, Editor, or Editorial Board of Advances in Nutrition. Individuals with different positions on the topic of a Perspective are invited to submit their comments in the form of a Perspectives article or in a Letter to the Editor.
Abbreviations used: AFSi, Agriculture and Food Systems Institute; BFPDB, USDA Branded Food Products Database; BMGF, Bill and Melinda Gates Foundation; DGA, Dietary Guidelines for Americans; DV, daily value; HEI, Healthy Eating Index; IFPRI, International Food Policy Research Institute; INFOODS, International Network of Food Data Systems; LIM, limiting nutrient subscore of the NRF index based on added sugar; LIMt, limiting nutrient subscore of the NRF index based on total sugar; LMIC, Low- and middle-income countries; MUFA, monounsaturated fatty acids; NCD, noncommunicable disease; NDS, Nutrient Density Score; NP, nutrient profiling; NR, Nutrient rich subscore of the NRF index; NRF, Nutrient Rich Food index; Ofcom, Office of Communications (UK); RACC, Reference Amounts Customarily Consumed; SAIN, LIM French nutrient profiling model; WNDDS. World Nutrient Datanase for Dietary Studies.
Contributor Information
Adam Drewnowski, Center for Public Health Nutrition, University of Washington, Seattle, WA, USA.
Daniel Amanquah, Sight and Life Foundation, Accra, Ghana.
Breda Gavin-Smith, Sight and Life Foundation, Accra, Ghana; Sight and Life Foundation, Wurmisweg, Kaiseraugst, Switzerland.
References
- 1. Ingram J. Nutrition security is more than food security. Nat Food. 2020;1(1):2. [Google Scholar]
- 2. Development Initiatives . Global Nutrition Report: shining a light to spur action on nutrition. [Internet]. Bristol (UK): Development Initiatives; 2018. [Accessed 2021 Feb 24]. Available from: https://www.who.int/nutrition/globalnutritionreport/2018_Global_Nutrition_Report.pdf?ua=1. [Google Scholar]
- 3. Drewnowski A, Popkin BM. The nutrition transition: new trends in the global diet. Nutr Rev. 2009;55(2):31–43. [DOI] [PubMed] [Google Scholar]
- 4. Drewnowski A, Darmon N. The economics of obesity: dietary energy density and energy cost. Am J Clin Nutr. 2005;82(1 Suppl):265S–73S. [DOI] [PubMed] [Google Scholar]
- 5. Darmon N, Drewnowski A. Contribution of food prices and diet cost to socioeconomic disparities in diet quality and health: a systematic review and analysis. Nutr Rev. 2015;73(10):643–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Drewnowski A, Specter S. Poverty and obesity: the role of energy density and energy costs. Am J Clin Nutr. 2004;79(1):6–16. [DOI] [PubMed] [Google Scholar]
- 7. Loring B, Robertson A. Obesity and inequities: guidance for addressing inequities in overweight and obesity. [Internet]. Copenhagen (Denmark): WHO Regional Office for Europe; 2014. [Accessed 2021 Feb 24]. Available from: https://www.euro.who.int/__data/assets/pdf_file/0003/247638/obesity-090514.pdf?ua=1. [Google Scholar]
- 8. UK Government Office for Science . Foresight Report 2007. Tackling Obesities: Future Choices. [Internet]. 2007; [updated 2020 Oct 17; cited 2020 Dec 21]. Available from: https://www.gov.uk/government/collections/tackling-obesities-future-choices#project-report. [Google Scholar]
- 9. Department of Health and Human Services/Department of Agriculture. Dietary Guidelines for Americans. [Internet]. 2005. [Accessed 2020 Dec 21]. Available from: http://www.health.gov/dietaryguidelines/dga2005/document/default.htm. [Google Scholar]
- 10. United States Department of Health and Human Services/Department of Agriculture . Dietary Guidelines for Americans. [Internet]. 2010. [Accessed 2020 Dec 21]. Available from: http://www.health.gov/dietaryguidelines/dga2010/document/default.htm. [Google Scholar]
- 11. United States Department of Health and Human Services/Department of Agriculture . Dietary Guidelines for Americans, 2015–2020. [Internet]. [Accessed 2020 Dec 21]. Available from: http://www.health.gov/dietaryguidelines/dga2015/document/default.htm. [Google Scholar]
- 12. Labonte M-È, Poon T, Gladanac B, Ahmed M, Franco-Arellano B, Rayner M, L'Abbé MR. Nutrient profile models with applications in government-led nutrition policies aimed at health promotion and noncommunicable disease prevention: a systematic review. Adv Nutr. 2018;9(6):741–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Drewnowski A. Uses of nutrient profiling to address public health needs: from regulation to reformulation. Proc Nutr Soc. 2017;76(3):220–9. [DOI] [PubMed] [Google Scholar]
- 14. UK Food Standards Agency and UK Department of Health . Guide to creating a front of pack (FoP) nutrition label for pre-packed products sold through retail outlets. [Internet]. 2016; Nov. [Accessed 2021 Feb 24]. Available from: https://www.food.gov.uk/sites/default/files/media/document/fop-guidance_0.pdf. [Google Scholar]
- 15. Reyes M, Garmendia ML, Olivares S, Aqueveque C, Zacarías I, Corvalán C. Development of the Chilean front-of-package food warning label. BMC Public Health. 2019;19(1):906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Combet E, Vlassopoulos A, Mölenberg F, Gressier M, Privet L, Wratten C, Sharif S, Vieux F, Lehmann U, Masset G. Testing the capacity of a multi-nutrient profiling system to guide food and beverage reformulation: results from five national food composition databases. Nutrients. 2017;9(4):406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Lehmann U, Charles VR, Vlassopoulos A, Masset G, Spieldenner J. Nutrient profiling for product reformulation: public health impact and benefits for the consumer. Proc Nutr Soc. 2017;76(3):255–64. [DOI] [PubMed] [Google Scholar]
- 18. WHO 2010 . Nutrient profiling: Report of a WHO/IASO Technical Meeting, London, United Kingdom 4–6 October 2010. [Internet]. [Accessed 2021 Feb 24]. Available from: https://www.who.int/nutrition/publications/profiling/WHO_IASO_report2010.pdf?ua=1. [Google Scholar]
- 19. Hannaford supermarkets . Learn about Guiding Stars. [Internet]. [Accessed 2021 Feb 24]. Available from: https://www.hannaford.com/health-wellness/guiding-stars. [Google Scholar]
- 20. Nicklas TA, O'Neil CE. Development of the SoFAS (Solid Fats and Added Sugars) Concept: the 2010 Dietary Guidelines for Americans. Adv Nutr. 2015;6(3):368S–75S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Drewnowski A. Concept of a nutritious food: toward a nutrient density score. Am J Clin Nutr. 2005;82(4):721–32. [DOI] [PubMed] [Google Scholar]
- 22. UK Department of Health and Social Care Food Standards Agency . The Nutrient Profiling Model. [Internet]. [Accessed 2020 Dec 21]. Available from: https://www.gov.uk/government/publications/the-nutrient-profiling-model. [Google Scholar]
- 23. Julia C, Etilé F, Hercberg S. Front-of-pack Nutri-Score labelling in France: an evidence-based policy. The Lancet Public Health. 2018;3(4):e164. [DOI] [PubMed] [Google Scholar]
- 24. Popkin BM, Adair LS, Ng SW. Global nutrition transition and the pandemic of obesity in developing countries. Nutr Rev. 2012;70(1):3–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Popkin BM, Corvalan C, Grummer-Strawn LM. Dynamics of the double burden of malnutrition and the changing nutrition reality. Lancet North Am Ed. 2020;395(10217):65–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Harika R, Faber M, Samuel F, Kimiywe J, Mulugeta A, Eilander A. Micronutrient status and dietary intake of iron, vitamin A, iodine, folate and zinc in women of reproductive age and pregnant women in Ethiopia, Kenya, Nigeria and South Africa: a systematic review of data from 2005 to 2015. Nutrients. 2017;9(10):1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Thow AM, Kadiyala S, Khandelwal S, Menon P, Downs S, Reddy KS. Toward food policy for the dual burden of malnutrition. Food Nutr Bull. 2016;37(3):261–74. [DOI] [PubMed] [Google Scholar]
- 28. FAO, IFAD, UNICEF, WFP, WHO . The state of food security and nutrition in the world 2020: transforming food systems for affordable healthy diets. [Internet]. [Accessed 2021 Feb 24]. Rome: FAO; 2020. Available from: http://www.fao.org/3/ca9692en/online/ca9692en.html. [Google Scholar]
- 29. Ghosh S, Suri D, Uauy R. Assessment of protein adequacy in developing countries: quality matters. Br J Nutr. 2012;108(S2):S77–87. [DOI] [PubMed] [Google Scholar]
- 30. Semba RD. The rise and fall of protein malnutrition in global health. Ann Nutr Metab. 2016;69(2):79–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Mkambula P, Mbuya MNN, Rowe LA, Sablah M, Friesen VM, Chadha M, Osei AK, Ringholz C, Vasta FC, Gorstein J. The unfinished agenda for food fortification in low- and middle-income countries: quantifying progress, gaps and potential opportunities. Nutrients. 2020;12(2):354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Keats EC, Neufeld LM, Garrett GS, Mbuya MNN, Bhutta ZA. Improved micronutrient status and health outcomes in low- and middle-income countries following large-scale fortification: evidence from a systematic review and meta-analysis. Am J Clin Nutr. 2019;109(6):1696–708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Headey DD, Alderman HH. The relative caloric prices of healthy and unhealthy foods differ systematically across income levels and continents. J Nutr. 2019;149(11):2020–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Drewnowski A, Fulgoni V. Nutrient profiling of foods: creating a nutrient-rich food index. Nutr Rev. 2008;66(1):23–39. [DOI] [PubMed] [Google Scholar]
- 35. Drewnowski A, Fulgoni VL. Nutrient density: principles and evaluation tools. Am J Clin Nutr. 2014;99(5):1223S–8S. [DOI] [PubMed] [Google Scholar]
- 36. Food and Agriculture Organization . International Network of Food Data Systems (INFOODS). [Internet]. [Cited 2020 Dec 21]. Available from: http://www.fao.org/infoods/infoods/en/. [Google Scholar]
- 37. Hulshof P, Doets E, Seyha S, Bunthang T, Vonglokham M, Kounnavong S, Famida U, Muslimatun S, Santika O, Prihatini Set al. Food composition tables in Southeast Asia: the contribution of the SMILING Project. Matern Child Health J. 2019;23(S1):46–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. World Nutrient Databases for Dietary Studies (WNDDS). [Internet]. [Cited 2020 Dec 21]. Available from: https://foodsystems.org/resources/wndds/. [Google Scholar]
- 39. United States Department of Agriculture . [Cited 2020 Dec 21].. [Internet]. [Cited 2020 Dec 21].Available from: https://fdc.nal.usda.gov/. [Google Scholar]
- 40. United States Department of Agriculture Food and Nutrient Database for Dietary Studies, 2015–2016. [Internet]. 2018; [updated Jul; cited 2020 Dec 21]. Available from: https://www.ars.usda.gov/ARSUserFiles/80400530/pdf/fndds/FNDDS_2015_2016_factsheet.pdf. [Google Scholar]
- 41. United States Department of Agriculture . USDA's Expanded Flavonoid Database for the Assessment of Dietary Intakes—September 2014. [Internet]. 2015; [updated 21 Apr; cited 21 Dec, 2020]. Available from: https://data.nal.usda.gov/dataset/usdas-expanded-flavonoid-database-assessment-dietary-intakes-september-2014. [Google Scholar]
- 42. United States Department of Agriculture . USDA Branded Food Products Database. [Internet]. 2019; [updated Apr; cited 2020 Dec 21]. Available from: https://data.nal.usda.gov/dataset/usda-branded-food-products-database. [Google Scholar]
- 43. Scarborough P, Arambepola C, Kaur A, Bhatnagar P, Rayner M. Should nutrient profile models be ‘category specific’ or ‘across-the-board’? A comparison of the two systems using diets of British adults. Eur J Clin Nutr. 2010;64(6):553–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Roodenburg AJC, Popkin BM, Seidell JC. Development of international criteria for a front of package food labelling system: the International Choices Programme. Eur J Clin Nutr. 2011;65(11):1190–200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Jansen L, Roodenburg AJC. The use of food composition data in the Choices International Programme. Food Chem. 2016;193:196–202. [DOI] [PubMed] [Google Scholar]
- 46. Choices International Foundation . Nutrition criteria. [Internet]. [Cited 2020 Dec 21]. Available from: https://www.choicesprogramme.org/our-work/nutrition-criteria/. [Google Scholar]
- 47. The Nestlé Nutritional Profiling System, its product categories and sets of criteria. [Internet]. [ Accessed 2021 Feb 24]. Available from: https://www.nestle.com/sites/default/files/asset-library/documents/library/documents/nutrition_health_wellness/nestle-nutritional-profiling-system.pdf. [Google Scholar]
- 48. Government of Australia . Health Star Rating System. [Internet]. [Accessed 2021 Feb 24]. Available from: http://www.healthstarrating.gov.au/internet/healthstarrating/publishing.nsf/content/home. [Google Scholar]
- 49. Tharrey M, Maillot M, Azaïs-Braesco V, Darmon N. From the SAIN, LIM system to the SENS algorithm: a review of a French approach of nutrient profiling. Proc Nutr Soc. 2017;76(3):237–46. [DOI] [PubMed] [Google Scholar]
- 50. Fulgoni VL, Keast DR, Drewnowski A. Development and validation of the Nutrient-Rich Foods Index: a tool to measure nutritional quality of foods. J Nutr. 2009;139(8):1549–54. [DOI] [PubMed] [Google Scholar]
- 51. US Food and Drug Administration . Electronic Code of Federal Regulations. [Internet]. 2020; [updated 2020 Dec 18; cited 2020 Dec 21]. Available from: https://www.ecfr.gov/cgi-bin/text-idx?SID=a94277d83556d01a86b5728b2f66fb7b&mc = true&node = se21.2.101_19&rgn = div8. [Google Scholar]
- 52. Drewnowski A, Maillot M, Darmon N. Testing nutrient profile models in relation to energy density and energy cost. Eur J Clin Nutr. 2009;63(5):674–83. [DOI] [PubMed] [Google Scholar]
- 53. Drewnowski A, Maillot M, Darmon N. Should nutrient profiles be based on 100 g, 100 kcal or serving size?. Eur J Clin Nutr. 2009;63(7):898–904. [DOI] [PubMed] [Google Scholar]
- 54. Fern EB, Watzke H, Barclay DV, Roulin A, Drewnowski A. The nutrient balance concept: a new quality metric for composite meals and diets. PLoS One. 2015;10(7):e0130491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. World Health Organization . Global and regional food consumption patterns and trends. [Internet]. [Cited 2020 Dec 21]. Available from: https://www.who.int/nutrition/topics/3_foodconsumption/en/index4.html. [Google Scholar]
- 56. Trijsburg L, Talsma EF, Vries D, Jeanne HM, Kennedy G, Kuijsten A, Brouwer ID. Diet quality indices for research in low- and middle-income countries: a systematic review. Nutr Rev. 2019;77(8):515–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Dror DK, Allen LH. The importance of milk and other animal-source foods for children in low-income countries. Food Nutr Bull. 2011;32(3):227–43. [DOI] [PubMed] [Google Scholar]
- 58. Drewnowski A. Adjusting for protein quality by food source may affect nutrient density metrics. Nutr Rev. 2020(in press). [DOI] [PubMed] [Google Scholar]
- 59. US Food and Drug Administration . Center for Food Safety and Applied Nutrition. Reference amounts customarily consumed: list of products for each product category: guidance for industry. [Internet]. College Park (MD): U.S. Department of Health and Human Services; 2018; Feb. [Accessed 2021 Feb 24]. Available from: https://www.fda.gov/media/102587/download. [Google Scholar]
- 60. Lewis J. Codex Nutrient Reference Values. Rome: Food and Agriculture Organization of the United Nations. [Internet]. 2019. [Accessed 2021 Feb 24]. Available from: http://www.fao.org/publications/card/en/c/CA6969EN/. [Google Scholar]
- 61. Maillot M, Darmon N, Darmon M, Lafay L, Drewnowski A. Nutrient-dense food groups have high energy costs: an econometric approach to nutrient profiling. J Nutr. 2007;137(7):1815–20. [DOI] [PubMed] [Google Scholar]
- 62. Changing Access to Nutritious Diets in Africa and South Asia: (CANDASA) new price indexes to measure food system change. [Internet]. [Cited 2020 Dec 25]. Available from: http://sites.tufts.edu/candasa/. [Google Scholar]
- 63. Mahrt K, Mather D, Herforth A, Headey D. Household dietary patterns and the cost of a nutritious diet in Myanmar. [Internet]2019; 30 Jun. IFPRI Discussion Paper 1854. [Accessed 2021 Feb 24]. Available from: https://ssrn.com/abstract=3430692. [Google Scholar]
- 64. Hirvonen K, Bai Y, Headey D, Masters WA. Affordability of the EAT–Lancet reference diet: a global analysis. The Lancet Global Health. 2020;8(1):e59–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Fulgoni V, Drewnowski A. An economic gap between the recommended healthy food patterns and existing diets of minority groups in the US National Health and Nutrition Examination Survey 2013–14. Front Nutr. 2019;6:37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Rose CM, Gupta S, Buszkiewicz J, Ko LK, Mou J, Cook A, Moudon AV, Aggarwal A, Drewnowski A. Small increments in diet cost can improve compliance with the Dietary Guidelines for Americans. Soc Sci Med. 2020;266:113359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Ghana Statistical Service (GSS), Ghana Health Service (GHS), and ICF International . Ghana Demographic and Health Survey 2014. Rockville (MD): GSS, GHS, and ICF International; 2015. [Google Scholar]
- 68. Nyumuah RO, Hoang TC, Amoaful EF, Agble R, Meyer M, Wirth JP, Locatelli-Rossi L, Panagides D. Implementing large-scale food fortification in Ghana: lessons learned. Food Nutr Bull. 2012;33(4_suppl3):S293–300. [DOI] [PubMed] [Google Scholar]
- 69. University of Ghana, GroundWork, University of Wisconsin-Madison, KEMRI-Wellcome Trust, UNICEF . Ghana Micronutrient Survey 2017. [Internet]. Accra (Ghana); 2017. [Accessed 2021 Feb 24]. Available from: https://groundworkhealth.org/wp-content/uploads/2018/06/UoG-GroundWork_2017-GHANA-MICRONUTRIENT-SURVEY_Final_180607.pdf. [Google Scholar]
- 70. OBAASIMA. [Internet]. [Accessed 2020 Dec 21]. Available from: http://obaasimaghana.com/home.php.
- 71. Gavin-Smith B, Amanquah D. OBAASIMA. A demand-driven approach to reduce micronutrient malnutrition in Ghana. [Internet]. [Accessed 2021 Feb 24]. Available from: https://sightandlife.org/wp-content/uploads/2018/12/35_SALMZ_0218_FieldReport_03.pdf. [Google Scholar]
- 72. FAO/INFOODS Food Composition Table for Western Africa (2019) / Table de composition des aliments FAO/INFOODS pour l'Afrique de l'Ouest (2019)—User guide (PDF) / Datasheets (Excel). [Internet]. [Accessed 2021 Feb 24]. Available from: http://www.fao.org/infoods/infoods/tables-and-databases/africa/en/.
- 73. Santé Publique France—conditions of use of the Nutri-Score logo. [Internet]. [Accessed 2021 Feb 24]. Available from: file:///C:/Users/Adam/AppData/Local/Temp/20200616RUV21_EN-1.pdf. [Google Scholar]
- 74. DeBoer MD, Lima AA, Oría RB, Scharf RJ, Moore SR, Luna MA, Guerrant RL. Early childhood growth failure and the developmental origins of adult disease: do enteric infections and malnutrition increase risk for the metabolic syndrome?. Nutr Rev. 2012;70(11):642–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Streppel MT, Sluik D, van Yperen JF, Geelen A, Hofman A, Franco OH, Witteman JC, Feskens EJ. Nutrient-rich foods, cardiovascular diseases and all-cause mortality: the Rotterdam study. Eur J Clin Nutr. 2014;68(6):741–7. [DOI] [PubMed] [Google Scholar]
- 76. Mytton OT, Forouhi NG, Scarborough P, Lentjes M, Luben R, Rayner M, Khaw KT, Wareham NJ, Monsivais P. Association between intake of less-healthy foods defined by the United Kingdom's nutrient profile model and cardiovascular disease: a population-based cohort study. PLoS Med. 2018;15:e1002484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Deschasaux M, Huybrechts I, Julia C, Hercberg S, Egnell M, Srour B, Kesse-Guyot E, Latino-Martel P, Biessy C, Casagrande Cet al. Association between nutritional profiles of foods underlying Nutri-Score front-of-pack labels and mortality: EPIC cohort study in 10 European countries. BMJ. 2020;370:m3173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Jones NR, Conklin AI, Suhrcke M, Monsivais P. The growing price gap between more and less healthy foods: analysis of a novel longitudinal UK dataset. PLoS One. 2014;9(10):e109343. [DOI] [PMC free article] [PubMed] [Google Scholar]


