Abstract
An ectopic pregnancy carries the potential for disastrous maternal complications. Early first trimester pelvic ultrasound examinations are frequently obtained in cases of pelvic pain and vaginal bleeding to assess for such diagnoses. The “bagel sign” and the “blob sign” described two sonographic appearances of tubal ectopic pregnancy with positive predictive values of > 95%. Current ectopic pregnancy consensus statements differ in the interpretation of these findings; however, radiologists should have familiarity with the appearances of these findings so as to best educate ordering providers on the potential for presence of a tubal ectopic pregnancy and need for very close patient surveillance.
Keywords: Ectopic pregnancy, Pregnancy, Obstetrics, Gynecology
Introduction
Sonographic evaluation for ectopic pregnancy is not an infrequent indication in both the emergent and outpatient setting. Radiologists’ reporting in these cases may vary based on experience and group practice consensus. Regardless of the classification system utilized, recognizing signs of ectopic pregnancy is imperative so that patients can receive the appropriate medical and surgical care. We herein discuss a case that demonstrate two such signs: the “bagel sign” and the “blob sign.”
Case report
A 32-year-old gravida 2, para 1 female patient that was at 6 weeks gestational age by last menstrual period presented to the emergency with pelvic pain and vaginal bleeding. The beta-hCG was 225 mIU/mL. On physical examination, the patient was in apparent distress but otherwise the vitals were normal, the abdominal examination was benign, and no findings of pelvic infection were identified. A pelvic ultrasound was performed to evaluate for possible ectopic pregnancy. The ultrasound did not reveal an intrauterine or definite ectopic pregnancy and the ovaries were normal without evidence of torsion. An indeterminate, small-sized, solid-appearing para-ovarian structure was noted on the ultrasound and recommendation for close follow-up was advised (Fig. 1). The patient was discharged given clinical stability but presented to the emergency department 3 days later with continued pelvic pain. The repeat beta-hCG was 1657 mIU/mL and a repeat pelvic ultrasound was performed that demonstrated interval cystic change in the previously solid para-ovarian structure, which was suggested to reflect a “bagel sign.” No intrauterine pregnancy was identified; however, the obstetric service deemed the para-ovarian structure to be of high concern for a potential tubal ectopic pregnancy. The patient underwent surgical excision of the structure which was pathologically confirmed to be a tubal ectopic pregnancy.
Fig. 1.
The “blob sign.” A 32-year-old pregnant patient (6 weeks gestational age based on last menstrual period) presented with pelvic pain and vaginal bleeding. Beta-hCG measured 225 mIU/mL. Grayscale pelvic ultrasound of the left adnexa demonstrated a nodule or “blob” like structure (arrow) abutting the ovary (arrowhead).
Discussion
The correlation of a ring-like adnexal structure on ultrasonography (Fig. 2a) to a tubal ectopic pregnancy dates back to at least 1978 [1]. The first description of this ring-like structure as a “bagel” appears to have occurred in 1995 during a personal communication between Drs. S. Goldstein and S. Rottem [2]. Sonographically, the centrally hypoechoic hole of the bagel represents the gestational sac and the thick surrounding echogenic dough of the bagel represents the trophoblastic tissue (Fig. 2b). A fetal pole would not be present as this would be confirmatory of an ectopic pregnancy.
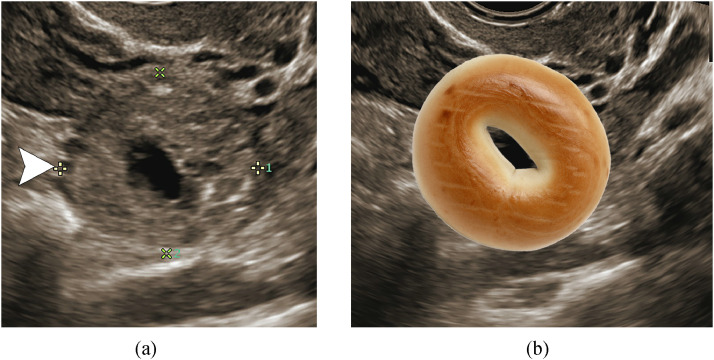
Fig. 2.
The “bagel sign.” A 32-year-old pregnant patient (6 weeks gestational age based on last menstrual period) re-presented with pelvic pain and vaginal bleeding. Beta-hCG measured 1657 mIU/mL compared to 225 mIU/mL 3 days prior. (a) Grayscale pelvic ultrasound of the left adnexa demonstrates a ring-like structure with a thick, solid, hyperechoic periphery and fluid centrally: the “bagel sign” (arrowhead) (calipers along the periphery were placed to measure the size of the structure). (b) Bagel animation overlaid on top of the sonographic finding. Ectopic pregnancy was confirmed clinically.
The “blob sign” has historically been described as an indication for ectopic pregnancy and, according to Barnhart consensus statement, also evidence of a probable ectopic pregnancy [3]. On transvaginal sonography, the “blob sign” is described as an inhomogeneous adnexal mass [4]. Similar to the “bagel sign,” the likelihood of an ectopic pregnancy in the presence of a “blob sign” was shown to be high in the study done by Nadim et. al (positive predicative value > 96%) [4].
Currently, in the absence of a confirmed intrauterine gestation, identification of the “bagel sign” and “blob sign” are classified as a “probable ectopic pregnancy” based on the Barnhart consensus statement [3] and “pregnancy of unknown location” based on the Society of Radiologists in Ultrasound criteria [5]. However, there is increasing evidence that in the clinical scenario of a positive beta-hCG and absence of an intrauterine pregnancy, identifying the “bagel sign” has a very high likelihood of representing a tubal ectopic pregnancy (positive predictive value > 95%) [4]. Therefore, the patient could potentially be considered for treatment of ectopic pregnancy, thereby reducing patient morbidity and potential mortality. A significant diagnostic pitfall in the same clinical scenario would be mistaking the corpus luteum of a viable intrauterine pregnancy for the “bagel sign.” The tubal ectopic gestation should demonstrate mobility separate from the adjacent ovary. Furthermore, while there may be overlap in other imaging features between the corpus luteum and ectopic pregnancy, a more confident diagnosis of a “bagel sign” can be made when the “bagel dough” is hyperechoic relative to uterine endometrium [6].
If the significance of a “blob” is unrecognized and the patient is imaged multiple times, as in the case reported above, a “blob” may progress to a “bagel” related to the interval development (or sonographer-dependent detection) of a gestation sac. Conversely, the deterioration of a “bagel” into a “blob” could theoretically occur if hemorrhage was to occur within the gestational sac.
Conclusion
An ectopic pregnancy can potentially result in disastrous complications for the mother. Our case highlights two sonographic signs that can be seen in early cases of tubal ectopic pregnancy that radiologists should be familiar with: the “bagel sign” and the “blob sign”. Although there are differences in current consensus statements regarding these signs and how they are reported, given the high positive predictive value of these signs in cases of tubal ectopic pregnancy, radiologists may consider direct communication of the findings with ordering providers to convey the potential significance need for close surveillance.
IRB statement
No IRB approval was required for this manuscript.
Patient consent
Patient and/or next of kin consent could not be obtained due to this being a older examination. All patient identifying information has been stripped from the images and movie files. Additionally, no patient identifying information is used in the case report.
References
- 1.Brown TW, Filly RA, Laing FC, Barton J. Analysis of ultrasonographic criteria in the evaluation for ectopic pregnancy. AJR Am J Roentgenol. 1978;131:967–971. doi: 10.2214/ajr.131.6.967. [DOI] [PubMed] [Google Scholar]
- 2.GSaT-T IE. Ultrasound-Guided Procedures in Gynecology. In: McAteer M, editor. Ultrasound in Gynecology. Churchill Livingstone; New York: 1995. p. 216. [Google Scholar]
- 3.Barnhart K, van Mello NM, Bourne T. Pregnancy of unknown location: a consensus statement of nomenclature, definitions, and outcome. Fertil Steril. 2011;95:857–866. doi: 10.1016/j.fertnstert.2010.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nadim B, Infante F, Lu C, Sathasivam N, Condous G. Morphological ultrasound types known as ‘blob’ and ‘bagel’ signs should be reclassified from suggesting probable to indicating definite tubal ectopic pregnancy. Ultrasound Obstet Gynecol. 2018;51:543–549. doi: 10.1002/uog.17435. [DOI] [PubMed] [Google Scholar]
- 5.Doubilet PM, Benson CB, Bourne T, Blaivas M. Diagnostic criteria for nonviable pregnancy early in the first trimester. N Engl J Med. 2013;369:1443–1451. doi: 10.1056/NEJMra1302417. [DOI] [PubMed] [Google Scholar]
- 6.Stein MW, Ricci ZJ, Novak L, Roberts JH, Koenigsberg M. Sonographic comparison of the tubal ring of ectopic pregnancy with the corpus luteum. Ultrasound Med Biol. 2004;23:57–62. doi: 10.7863/jum.2004.23.1.57. [DOI] [PubMed] [Google Scholar]