Abstract
Due to the evolving nature of injuries caused by high-speed motor vehicle accidents, the incidence rate of blunt chest trauma is continuously increasing. Blunt cardiac injury (BCI) is a potentially lethal entity as a result of trauma to the chest. Due to its indistinct clinical presentation and heterogeneous definition, BCI might be missed during the initial survey of trauma patients in the acute care setting. Additionally, unnecessary operation in hemodynamically stable patients in whom the extent of cardiac injury has not been thoroughly evaluated might result in adverse clinical outcome. Due to ongoing advances in the diagnostic modalities and minimally invasive procedures in the acute care and trauma setting, patients with blunt trauma to the chest, who are also suspected of having a BCI, can be monitored with more confidence and managed accordingly as the clinical scenario evolves. While low-yield diagnostics such as chest X ray, electrocardiogram, and a bedside ultrasonography are still routinely performed in patients with suspected BCI, high-yield modalities such as computed tomography, highly sensitive cardiac biomarkers, and transesophageal echocardiography are all a next step in the management approach. In either case, the clinical judgment of the medical team plays a pivotal role in transition to the next step with adequate resuscitation remaining an inevitable part.
Keywords: Blunt cardiac injury, blunt chest trauma, transesophageal echocardiography, transthoracic echocardiography, electrocardiography, chest X ray
Introduction
Defined as a cardiac injury sustained due to a blunt trauma to the rib cage [1], blunt cardiac injury (BCI) continues to be a diagnostic challenge in the emergency trauma setting [2]. The incidence of BCI has been increasing due to a shift in the pattern of motor vehicle accidents and other collisions [3]. The reported incidence of BCI ranges from 10% in general trauma cases to > 70% of all the patients with high-impact trauma to the chest [1,4,5]. A 15-year review of medical history of patients admitted to a specialized trauma center in China determined BCI to be present in 18.3% of all cases with a documented blunt chest trauma [6].
Patients with BCI can present with a wide variety of signs and symptoms depending on the angle that the trauma is introduced to the mediastinum [7-9]. These include being asymptomatic to developing arrhythmia, a new-onset murmur, myocardial contusion, papillary muscle rupture, or valvular injury, which can lead to acute heart failure, compromised coronary artery flow, and subsequent myocardial ischemia [1].
In parallel with recent advance in radiologic and ultrasonographic technology [10-12], the diagnostic approach to the patients, who are suspicious of contracting BCI has been evolving [7,8]. As the initial manifestation of patients with a potential BCI can widely vary [7,9], a high clinical suspicion is required to prompt the diagnosis and transition of the patient to a higher level of care [8]. This is especially crucial knowing that a high-yield cardiac diagnostic test is not a routine part of the current practice in the trauma setting [10]. Although an unwritten rule necessitates initial cardiac workup in all the patients with an anterior chest trauma [2,13], there is no universally-accepted guideline to systematically direct the trauma team in this setting. If missed, BCI can result in significant morbidity and mortality [8,14,15].
Due to the ambiguous definition of BCI, uncertain diagnostic criteria, and invariable management guidelines for this clinically important entity, we prompted to conduct this review to summarize the current heterogeneous literature into a practical guide.
Mechanism of injury
The mechanism of trauma leading to BCI can be divided into the following categories [1,6,15,16]: 1) direct insult to the chest such as steering wheel trauma; 2) sternal fracture leading to compression of the heart against the vertebral column; 3) acceleration-deceleration impact leading to a torsion at the fixation sites such as the pulmonary trunk; 4) hydraulic effect transmitting the increased intra-abdominal pressure to the right atrium via the draining inferior vena cava (IVC); and 5) blast injury. It remains unclear if a cardiac injury due to a displaced sternal fracture or a dislocated rib segment should be considered a blunt trauma. Regardless of the mechanism of injury, the heart can be afflicted from pericardium, through myocardium, to the endocardium.
Due to its anterior location, the right side of the heart is more susceptible to be impacted by the trauma than the left heart [1,15]. However, concomitant injuries at two or more sites within the heart are also possible, as observed in high-impact accidents [1,12,14,15,17]. In a series of 546 deceased cases due to BCI, who underwent autopsy, Parmley et al. observed the rupture of the right ventricle (RV) in 10.2% of the patients followed by left ventricular (LV) and right atrial (RA) rupture in 8.4% and 6.4% of the patients, respectively [15]. Additionally, rupture of multiple chambers was observed in > 12% of the cases as was concomitant chamber and aortic rupture in > 6% of them. Injuries to other anatomical structures was also observed with variable depth but with less frequency.
Clinical presentation
In trauma setting, patients who sustain an insult to the chest can present with varying manifestations, which might raise a suspicion for BCI if interpreted based on the mechanism of injury and through highly sensitive diagnostic work-up. The mechanism of injury can be depicted via a thorough history, either from the patient or a bystander. Patient history can also reveal underlying comorbidities, risk factors, and concomitant medications.
Physical findings, which might strengthen the suspicion for BCI include Beck’s triad (hypotension, distant/muffled heart sounds, and distended jugular venous pressure), signs of hemothorax such as impending shock following positional change (especially decubitus), and a refractory hypotension, which cannot be explained only by internal bleeding.
In general, clinical presentation is not a very sensitive tool for diagnosing BCI but is an appropriate step in triaging the patient. This should be followed by further diagnostic tests regardless of the level of suspicion [6,8,18]. If BCI is highly suspected, a high-yield diagnostic can be pursued, otherwise a lower-yield diagnostic test of screening value would be the next step.
Diagnostic tests
Diagnostic modalities, common findings suggesting BCI, practical advantage or technical disadvantage, and level of evidence supporting their use are summarized in Table 1.
Table 1.
The utility of diagnostic modalities for blunt cardiac injury
| Diagnostic modality | Findings suggesting BCI | Sensitivity | Specificity | References | Pros | Cons | Level of Evidence |
|---|---|---|---|---|---|---|---|
| Chest X ray | Widen mediastinum, haemo/pneumomediastinum | 57%-100% | 33%-90.2% | [46,47] | Simple, fast, and low radiation | Non-specific and variable sensitivity | Level 4 (case series) |
| Electrocardiography | Unspecific ST-T changes; tachycardia; atrial fibrillation; bradycardia | 50%-89% | 23%-67% | [23,48,49] | Simple, available, and inexpensive | Insensitive and nonspecific | Level 4 (case series) |
| Highly sensitive troponin | An increase of 20% from baseline or > 14 ng/L | 23%-100% | 21%-97% | [5,27,48,50] | Sensitive | Not available in every setting; variable specificity | Level 4 (case series) |
| Focused assessment with sonography for trauma | Pericardial effusion; hemopericardium | 83.3%-100% | 99.7% | [51,52] | Feasibly done at the bedside, moderately specific, accuracy dependent on training | Operator dependent, variable sensitivity, requires training and practice | Level 2-4 (prospective cohort, case series) |
| Transthoracic echocardiography | Pericardial effusion; valvular regurgitation; abnormal regional wall motion | Up to 100% | N/A | [4,29,30,53] | Feasibly done at the bedside and specific | Operator dependent and variable sensitivity | Level 4 (case series) |
| Transesophageal echocardiography | Pericardial effusion; valvular regurgitation; abnormal regional wall motion | Up to 100% | N/A | [8,45,54] | Higher specificity than TTE | Challenging in cervical spine traumas and technically demanding | Level 4 (case series) |
| Computed tomography | Pericardial effusion, epicardial fat stranding, abnormal heart (defined by the radiologist) | 22%-78% | 55%-95% | [45,55,56] | Highly sensitive, fast and specific | High-dose radiation | Level 2-4 (prospective cohort, case series) |
| Magnetic resonance imaging | Myocardial edema, haemorrhage , or inflammation, and regional wall motion abnormalities | 60% | 81% | [8,35,50] | Moderate sensitivity but high accuracy and specificity | Time-consuming in trauma setting; the field is evolving. | Level 4 (case series) |
Chest X-ray
Plain radiography of the chest is one of the first step in the initial survey of patients with blunt chest trauma. In a retrospective review of 374 trauma patients evaluated with a chest X-ray (CXR) and abdominal computed tomography (CT) scan, Barrios Jr. et al. showed that addition of thoracic CT scan did not add to the sensitivity of the CXR in the detection of occult intrathoracic injury nor did it change the management of blunt traumatic injury of the chest [19]. Another case series of 174 children with blunt chest trauma, who underwent CT scan and CXR showed that clinically relevant findings on chest CT scan have a good correlation with the radiologic findings of CXR but at the cost of significantly higher radiation dosage [20]. Considering the evolving anatomy of the rib cage and intrathoracic organs in pediatric population, the utility of chest CT versus CXR might be interpreted differently compared to that in adult trauma patients. Nonetheless, in the current era of modern medicine, a routine CXR in lieu of a far advanced rapid focused echocardiography or spiral CT scan seems to be an outdated approach [21].
Electrocardiogram
In hemodynamically stable patients with blunt trauma to the chest, an initial 12-lead electrocardiogram (EKG) is well accepted [7,13,22,23]. However, a normal EKG does not exclude a BCI even in stable patients and cardiac enzymes should also be evaluated if clinically indicated [7,24]. In hemodynamically unstable cases, resuscitation to stabilize the hemodynamic status should precede all diagnostic tests including an EKG.
Cardiac biomarkers
A prospective study of 72 trauma patients with a suspected BCI showed that out of 10 patients with elevated cardiac troponin I 4 to 6 hours after admission, one developed severe LV dysfunction and one died [22]. However, the remaining 8 patients (80%) could be discharged home with no cardiovascular sequel. In another prospective study of 71 consecutive patients with BCI at a level I trauma center, abnormal EKG at admission and a troponin T level > 0.20 µg/L were the only predictors of clinically adverse events [24]. Interestingly, 41% of the patients with a normal EKG at admission later developed a clinically significant EKG abnormality during their course of hospital stay.
One study has shown that a concordantly abnormal or normal EKG and cardiac troponin I is associated with a positive and negative predictive values of 62% and 100%, respectively [23]. However, the study measurements were performed up to 8 hours after admission. Another study elucidated the alteration pattern of cardiac troponins and creatine kinase membrane-based (CK-MB) at admission and 24 hours later in patients with blunt trauma with (38 cases) and without (51 cases) thoracic injuries [25]. An elevated serum level of cardiac troponins was initially observed in 8-10%, and 24 hours later, in 20% of the patients with thoracic injury. A similar but smaller change was also observed in trauma patients without thoracic injury showing an abnormal serum level of troponin in 2% of the patients after 24 hours of admission.
Elevated levels of highly sensitive cardiac troponin T (hs-cTnT) have shown good correlation with the severity of the BCI, adverse clinical outcome, and poor mid-term (3-year) survival in patients with blunt chest trauma [26,27]. However, the specificity of this correlation has been stronger when the trend of hs-CTnT has been considered in evaluating the patients with a suspected BCI. Unfortunately, the clinical utility of this cardiac biomarker has not been evaluated in large cohorts and not incorporated into the latest guideline of the Eastern Association for the Surgery of Trauma practice management [7].
Focused assessment with sonography for trauma/echocardiography
Although in a patient with high clinical, laboratory, and radiologic evidence for BCI, a focused cardiac ultrasound (FoCUS) seems an appropriate next step, its accuracy in early detection of BCI might be suboptimal due to its operator-dependency and technical challenges in the emergency trauma setting [7,28,29]. However, with adequate training the accuracy of this modality can be improved [30]. Hence, echocardiography can be a complementary diagnostic modality to the routine diagnostic approach in suspicious cases of BCI but its accuracy should be continuously measured against other modalities as the medical staff follow the learning curve [28,29]. In a systematic review of 50 patients with BCI, Ali et al. found that cardiac dysrhythmia occurs in up to 80% of the patients of whom only a third developed relevant echocardiographic abnormality [31]. However, the mortality in this population of patients was 20% and mostly occurred in the first few days following the insult. In a prospective study, Karalis et al. complemented the utility of transthoracic echocardiography (TTE) with transesophageal echocardiography (TEE) when the quality of TTE was determined to be suboptimal [29]. Of 105 patients with severe blunt chest trauma, only 20 patients (19%) had a suboptimal TTE and underwent complementary TEE. Examination with a TEE could detect an additional 9 cases of myocardial contusion, 4 cases of focal aortic intimal injury, and one case of aortic transection. Overall, evaluation with echocardiography rarely changed the management of the trauma patients, a fact that was further highlighted by other studies [28,32].
Computed tomography
Computed tomography (CT) has been established as the modality of choice in early evaluation of patients with blunt chest trauma [33-35]. Apart from the feasibility of rapid acquisition and accurate diagnostic value, the additional capability of contrast enhancement and 3D volumetric measurement of the obtained images can expedite the learning process of the medical team about the trauma case [35,36]. In a prospective study of 110 consecutive patients with blunt chest trauma, Vignon et al. compared the utility of multiplane TEE and contrast-enhanced spiral CT in the diagnosis of cardiovascular injuries in patients with severe blunt trauma to the chest [37]. While both modalities revealed similar diagnostic accuracy, TEE was more sensitive than CT in the diagnosis of the thoracic aorta’s intimal and medial lesions. On the other hand, there are reports of post-traumatic abnormalities, which have been missed or misdiagnosed by TTE but detected with a cardiac CT with or without contrast [38-40]. In either case, it is the medical knowledge of the clinicians, accumulated upon acquired initial diagnostic modalities and clinical investigation, which will guide their next step in diagnostic approach to patients with suspected BCI.
Magnetic resonance imaging
Magnetic resonance imaging (MRI) has a limited role in the initial evaluation of patients with suspected BCI. Although the Eastern Association for the Surgery of Trauma practice management guideline has recommended MRI as a tool to differentiate acute myocardial infarction from BCI [7], limited evidence exists to support the feasibility of such modality in acute care and trauma setting owing to its time consuming nature. This was also emphasized by the recent American College of Radiology Appropriateness Criteria for Blunt Chest Trauma-Suspected Cardiac Injury [35]. Considering great advance in the rapid acquisition and highly-accurate reconstruction of CT images, there is very limited role for a cardiac MRI in the trauma setting at this time.
Treatment
Resuscitation
Due to its high morbidity and mortality rate, timely identification of patients with a possible BCI is of a lifesaving importance. Depending on the level of trauma center at which the patient with a suspected BCI arrives first, the initial workup might vary. However, resuscitation and hemodynamic stabilization of the patients is the priority as it is in every trauma and acute care setting. A hypotensive shock, which cannot be solely explained by hemorrhage in the setting of a blunt chest trauma should raise the suspicion for cardiac injury. Securing the airway, effective circulation, and rhythm control in patients with BCI must be ascertained by any available measures. No need to mention that securing two large-bore venous access is the first and the most important step.
Watchful waiting
In hemodynamically stable patients in whom both echocardiography and chest CT has been negative, close monitoring with serial EKG and cardiac enzymes might be sufficient up to the time of discharge from the hospital or transfer to the next level of care. However, some patients need further in-depth evaluation, such as repeat chest CT with contrast, or observation for a longer period of time. In either case, there is a tradeoff between longer observation and repeating diagnostic procedures.
Conservative management/pericardiocentesis
In patients with clinical, laboratory, and radiological findings pointing out to the acute cardiac tamponade, cardiovascular surgery consult should be prompted as the next step (Figure 1). However, the invasiveness of the next step can vary from pericardiocentesis to subxiphoid pericardiotomy and emergent resuscitative thoracotomy [41-43]. A case series of 11 patients with pericardial effusion after blunt chest trauma showed that pericardiocentesis or subxiphoid pericardial window is feasible in patients with BCI even in hemodynamically unstable ones, who arrive alive at the ER [44]. Due to its less invasive nature, non-operative management of blunt pericardial effusion (BPE) leading to acute cardiac tamponade seem a clinically beneficial option. However, non-operative management of patients with BPE should be routinely considered in subspecialized centers with highly-trained critical team. Nonetheless, our knowledge is still evolving on the incidence rate, clinical course, and standard of care for patients with BPE.
Figure 1.
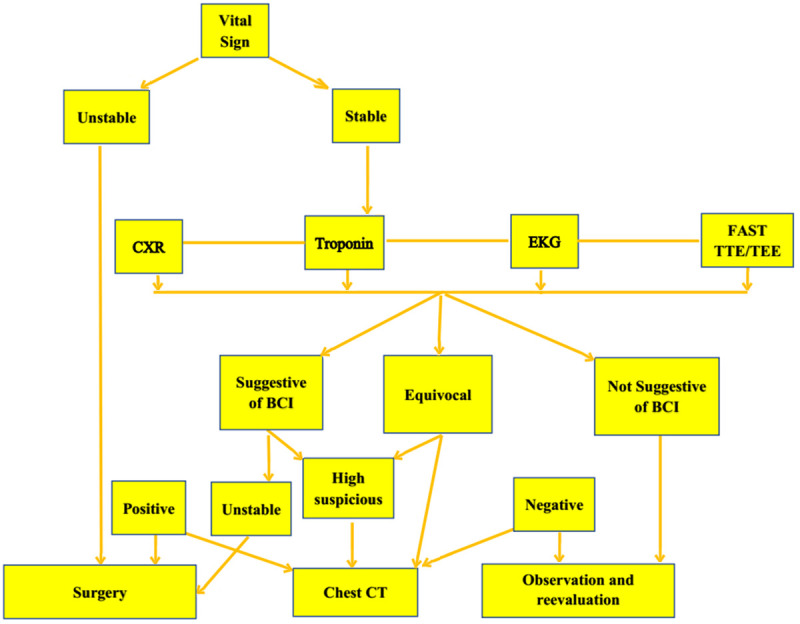
A proposed algorithm to the management of a patient with blunt chest trauma and suspected blunt cardiac injury.
Surgical management/thoracotomy
The absolute indication for surgical management of patients with BCI remains controversial. Hemodynamic instability suggestive of cardiac injuries or surrounding vasculatures continue to be the most common indications for emergent cardiothoracic surgery in patients with BCI [41,43,44]. In a retrospective review of 30 patients with blunt pericardial effusion presenting at a level I trauma center, Huang et al. compared the perioperative parameters of hemodynamically stable patients with and without cardiovascular injuries who were initially managed non-operatively [41]. Of these series, 11 patients underwent emergent surgery while 19 patients were initially managed non-operatively. Twelve out of 19 patients were later operated on due to a refractory hypotension (6 patients, 63%), abnormal echocardiography (4 patients, 21%), persistent cardiovascular abnormality in CT scan (1 patient, 8%), and clinical judgment of the surgeon (1 patient, 8%). However, cardiovascular injuries were found intraoperatively only in four patients (21%). Another study by Witt et al. also compared the clinical outcome of patients with BPE who were managed surgically or non-surgically [43]. Of 75 patients with BCI and pericardial effusion detected by CT scan, 32 patients had minimal pericardial effusion (3% underwent surgery), 20 patients had small effusion (10% underwent surgery), 8 patients had moderate amount of pericardial fluid (13% were managed surgically), and 5 patients developed large pericardial effusion (60% operation rate). Of the seven patients, who were managed operatively, a pericardial window was created in 4 patients. As the mortality rate in hemodynamically unstable patients with severe BPE was none, the authors voted for surgical management of unstable patients with BCI. However, due to invariable outcome measures reported by other studies [19,41,43-45] and technical advances in performing a bedside pericardiotomy, the cost-effectiveness of surgery in the setting of BPE remains unclear.
Limitations
There is a controversy in the literature in recommending EKG [2,22], echocardiography [4,29,35], or chest CT [35,45] as the initial diagnostic modality of choice in detecting subtle cardiac injuries. However, a growing body of knowledge is forming on the clinical utility of serial or delayed measurement of high-sensitive cardiac troponin levels in the trauma setting [5,7,13,22-25]. Nonetheless, with the literature still evolving around the modern CT techniques and high-sensitive cardiac biomarkers in detecting BCI, the pivotal role of the clinical judgment of the medical team in the management of these patients cannot be overlooked.
Future research
As the majority of our knowledge in the management of patients with BCI comes from retrospective studies or case reports, prospective cohorts are required on this topic, especially measuring the revolutionary role of multidetector CT scans, high-sensitive troponins, and highly-efficient fast cardiac ultrasound. Also, an updated expert panel is required to systematically review the current data on the management of BCI, fill the gaps due to a lack of evidence with consensus, and draw a step-by-step approach.
Conclusion
The approach to a patient with suspected BCI is still guided by the clinical judgment of the medical team and must include adequate stabilization and close monitoring of the patient’s hemodynamic status. While CXR, EKG, and basic cardiovascular panels are not of a high diagnostic value compared to the more advanced modalities such as multi-detector CT scan, fast cardiac sonography, and serial high-sensitive troponins, they still constitute the initial steps of the diagnostic approach to the patients with BCI. Nonetheless, BCI continues to account for a significant morbidity and mortality in the trauma setting and an approach to its diagnosis and management bears uncertainty.
Disclosure of conflict of interest
None.
References
- 1.Schultz JM, Trunkey DD. Blunt cardiac injury. Crit Care Clin. 2004;20:57–70. doi: 10.1016/s0749-0704(03)00092-7. [DOI] [PubMed] [Google Scholar]
- 2.Nagy KK, Krosner SM, Roberts RR, Joseph KT, Smith RF, Barrett J. Determining which patients require evaluation for blunt cardiac injury following blunt chest trauma. World J Surg. 2001;25:108–111. doi: 10.1007/s002680020372. [DOI] [PubMed] [Google Scholar]
- 3.Matsuyama T, Kitamura T, Katayama Y, Hirose T, Kiguchi T, Sado J, Kiyohara K, Izawa J, Okada N, Takebe K, Watanabe M, Miyamoto Y, Yamahata Y, Ohta B. Motor vehicle accident mortality by elderly drivers in the super-aging era: a nationwide hospital-based registry in Japan. Medicine (Baltimore) 2018;97:e12350. doi: 10.1097/MD.0000000000012350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bahar AM, Nouri M, Alizadeh L, Namvar F, Asadi M. Estimated incidence of cardiac contusion using transthoracic echocardiography in patients suffering from severe blunt trauma to the chest. Acta Chir Belg. 2014;114:105–109. [PubMed] [Google Scholar]
- 5.Bertinchant JP, Polge A, Mohty D, Nguyen-Ngoc-Lam R, Estorc J, Cohendy R, Joubert P, Poupard P, Fabbro-Peray P, Monpeyroux F, Poirey S, Ledermann B, Raczka F, Brunet J, Nigond J, de la Coussaye JE. Evaluation of incidence, clinical significance, and prognostic value of circulating cardiac troponin I and T elevation in hemodynamically stable patients with suspected myocardial contusion after blunt chest trauma. J Trauma. 2000;48:924–931. doi: 10.1097/00005373-200005000-00018. [DOI] [PubMed] [Google Scholar]
- 6.Gao JM, Du DY, Kong LW, Yang J, Li H, Wei GB, Li CH, Liu CP. Emergency surgery for blunt cardiac injury: experience in 43 cases. World J Surg. 2020;44:1666–1672. doi: 10.1007/s00268-020-05369-6. [DOI] [PubMed] [Google Scholar]
- 7.Clancy K, Velopulos C, Bilaniuk JW, Collier B, Crowley W, Kurek S, Lui F, Nayduch D, Sangosanya A, Tucker B, Haut ER Eastern Association for the Surgery of Trauma. Screening for blunt cardiac injury: an Eastern Association for the Surgery of Trauma practice management guideline. J Trauma Acute Care Surg. 2012;73:S301–306. doi: 10.1097/TA.0b013e318270193a. [DOI] [PubMed] [Google Scholar]
- 8.Gao JM, Li H, Wei GB, Liu CP, Du DY, Kong LW, Li CH, Yang J, Yang Q. Blunt cardiac injury: a single-center 15-year experience. Am Surg. 2020;86:354–361. [PubMed] [Google Scholar]
- 9.Heidelberg L, Uhlich R, Bosarge P, Kerby J, Hu P. The depth of sternal fracture displacement is not associated with blunt cardiac injury. J Surg Res. 2019;235:322–328. doi: 10.1016/j.jss.2018.08.051. [DOI] [PubMed] [Google Scholar]
- 10.Dancer SC, Le Roux C, Fosgate GT, Kirberger RM. Radiography is less sensitive relative to CT for detecting thoracic radiographic changes in dogs affected by blunt trauma secondary to a motor vehicle accident. Vet Radiol Ultrasound. 2019;60:648–658. doi: 10.1111/vru.12795. [DOI] [PubMed] [Google Scholar]
- 11.Kettunen P, Nieminen M. Creatine kinase MB and M-mode echocardiographic changes in cardiac contusion. Ann Clin Res. 1985;17:292–298. [PubMed] [Google Scholar]
- 12.Rosenbaum RC, Johnston GS. Posttraumatic cardiac dysfunction: assessment with radionuclide ventriculography. Radiology. 1986;160:91–94. doi: 10.1148/radiology.160.1.3012633. [DOI] [PubMed] [Google Scholar]
- 13.Joseph B, Jokar TO, Khalil M, Haider AA, Kulvatunyou N, Zangbar B, Tang A, Zeeshan M, O’Keeffe T, Abbas D, Latifi R, Rhee P. Identifying the broken heart: predictors of mortality and morbidity in suspected blunt cardiac injury. Am J Surg. 2016;211:982–988. doi: 10.1016/j.amjsurg.2015.10.027. [DOI] [PubMed] [Google Scholar]
- 14.Kato K, Kushimoto S, Mashiko K, Henmi H, Yamamoto Y, Otsuka T. Blunt traumatic rupture of the heart: an experience in Tokyo. J Trauma. 1994;36:859–863. doi: 10.1097/00005373-199406000-00017. discussion 863-854. [DOI] [PubMed] [Google Scholar]
- 15.Parmley LF, Manion WC, Mattingly TW. Nonpenetrating traumatic injury of the heart. Circulation. 1958;18:371–396. doi: 10.1161/01.cir.18.3.371. [DOI] [PubMed] [Google Scholar]
- 16.Fulda G, Brathwaite CE, Rodriguez A, Turney SZ, Dunham CM, Cowley RA. Blunt traumatic rupture of the heart and pericardium: a ten-year experience (1979-1989) J Trauma. 1991;31:167–172. discussion 172-163. [PubMed] [Google Scholar]
- 17.Beck CS. The management of wounds of the heart. Surg Clin North Am. 1958;38:1557–1568. doi: 10.1016/s0039-6109(16)35636-5. [DOI] [PubMed] [Google Scholar]
- 18.Shorr RM, Crittenden M, Indeck M, Hartunian SL, Rodriguez A. Blunt thoracic trauma. Analysis of 515 patients. Ann Surg. 1987;206:200–205. doi: 10.1097/00000658-198708000-00013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Barrios C Jr, Pham J, Malinoski D, Dolich M, Lekawa M, Cinat M. Ability of a chest X-ray and an abdominal computed tomography scan to identify traumatic thoracic injury. Am J Surg. 2010;200:741–744. doi: 10.1016/j.amjsurg.2010.08.004. discussion 744-745. [DOI] [PubMed] [Google Scholar]
- 20.Holscher CM, Faulk LW, Moore EE, Cothren Burlew C, Moore HB, Stewart CL, Pieracci FM, Barnett CC, Bensard DD. Chest computed tomography imaging for blunt pediatric trauma: not worth the radiation risk. J Surg Res. 2013;184:352–357. doi: 10.1016/j.jss.2013.04.044. [DOI] [PubMed] [Google Scholar]
- 21.Choi J, Forrester JD, Spain DA. Necessity of routine chest radiograph in blunt trauma resuscitation: time to evaluate dogma with evidence. J Trauma Acute Care Surg. 2020;89:e69–e70. doi: 10.1097/TA.0000000000002793. [DOI] [PubMed] [Google Scholar]
- 22.Collins JN, Cole FJ, Weireter LJ, Riblet JL, Britt LD. The usefulness of serum troponin levels in evaluating cardiac injury. Am Surg. 2001;67:821–825. discussion 825-826. [PubMed] [Google Scholar]
- 23.Salim A, Velmahos GC, Jindal A, Chan L, Vassiliu P, Belzberg H, Asensio J, Demetriades D. Clinically significant blunt cardiac trauma: role of serum troponin levels combined with electrocardiographic findings. J Trauma. 2001;50:237–243. doi: 10.1097/00005373-200102000-00008. [DOI] [PubMed] [Google Scholar]
- 24.Fulda GJ, Giberson F, Hailstone D, Law A, Stillabower M. An evaluation of serum troponin T and signal-averaged electrocardiography in predicting electrocardiographic abnormalities after blunt chest trauma. J Trauma. 1997;43:304–310. doi: 10.1097/00005373-199708000-00016. discussion 310-302. [DOI] [PubMed] [Google Scholar]
- 25.Swaanenburg JC, Klaase JM, DeJongste MJ, Zimmerman KW, ten Duis HJ. Troponin I, troponin T, CKMB-activity and CKMB-mass as markers for the detection of myocardial contusion in patients who experienced blunt trauma. Clin Chim Acta. 1998;272:171–181. doi: 10.1016/s0009-8981(98)00014-x. [DOI] [PubMed] [Google Scholar]
- 26.Keskpaik T, Starkopf J, Kirsimagi U, Mihnovits V, Lomp A, Raamat EM, Saar S, Talving P. The role of elevated high-sensitivity cardiac troponin on outcomes following severe blunt chest trauma. Injury. 2020;51:1177–1182. doi: 10.1016/j.injury.2019.12.037. [DOI] [PubMed] [Google Scholar]
- 27.Pfortmueller CA, Lindner G, Leichtle AB, Fiedler GM, Exadaktylos AK. Diagnostic significance of high sensitivity troponin in diagnosis of blunt cardiac injury. Intensive Care Med. 2014;40:623–624. doi: 10.1007/s00134-013-3204-5. [DOI] [PubMed] [Google Scholar]
- 28.Helling TS, Duke P, Beggs CW, Crouse LJ. A prospective evaluation of 68 patients suffering blunt chest trauma for evidence of cardiac injury. J Trauma. 1989;29:961–965. doi: 10.1097/00005373-198907000-00009. discussion 965-966. [DOI] [PubMed] [Google Scholar]
- 29.Karalis DG, Victor MF, Davis GA, McAllister MP, Covalesky VA, Ross JJ Jr, Foley RV, Kerstein MD, Chandrasekaran K. The role of echocardiography in blunt chest trauma: a transthoracic and transesophageal echocardiographic study. J Trauma. 1994;36:53–58. doi: 10.1097/00005373-199401000-00008. [DOI] [PubMed] [Google Scholar]
- 30.Manasia AR, Nagaraj HM, Kodali RB, Croft LB, Oropello JM, Kohli-Seth R, Leibowitz AB, DelGiudice R, Hufanda JF, Benjamin E, Goldman ME. Feasibility and potential clinical utility of goal-directed transthoracic echocardiography performed by noncardiologist intensivists using a small hand-carried device (SonoHeart) in critically ill patients. J Cardiothorac Vasc Anesth. 2005;19:155–159. doi: 10.1053/j.jvca.2005.01.023. [DOI] [PubMed] [Google Scholar]
- 31.Ali H, Furlanello F, Lupo P, Foresti S, De Ambroggi G, Epicoco G, Semprini L, Fundaliotis A, Cappato R. Clinical and electrocardiographic features of complete heart block after blunt cardiac injury: a systematic review of the literature. Heart Rhythm. 2017;14:1561–1569. doi: 10.1016/j.hrthm.2017.05.040. [DOI] [PubMed] [Google Scholar]
- 32.Emet M, Akoz A, Aslan S, Saritas A, Cakir Z, Acemoglu H. Assessment of cardiac injury in patients with blunt chest trauma. Eur J Trauma Emerg Surg. 2010;36:441–447. doi: 10.1007/s00068-010-0005-1. [DOI] [PubMed] [Google Scholar]
- 33.Baxi AJ, Restrepo C, Mumbower A, McCarthy M, Rashmi K. Cardiac injuries: a review of multidetector computed tomography findings. Trauma Mon. 2015;20:e19086. doi: 10.5812/traumamon.19086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Terry NL, Watts JR Jr, Sonavane SK, Beasley TM, Munden R, Nath PH, Singh SP. Improved identification of sternal injuries with multidetector computed tomography (MDCT): sagittal reconstructions. Clin Imaging. 2016;40:739–744. doi: 10.1016/j.clinimag.2016.02.021. [DOI] [PubMed] [Google Scholar]
- 35.Expert Panels on Cardiac Imaging and Thoracic Imaging. Stojanovska J, Hurwitz Koweek LM, Chung JH, Ghoshhajra BB, Walker CM, Beache GM, Berry MF, Colletti PM, Davis AM, Hsu JY, Khosa F, Kicska GA, Kligerman SJ, Litmanovich D, Maroules CD, Meyersohn N, Syed MA, Tong BC, Villines TC, Wann S, Wolf SJ, Kanne JP, Abbara S. ACR appropriateness criteria(R) blunt chest trauma-suspected cardiac injury. J Am Coll Radiol. 2020;17:S380–S390. doi: 10.1016/j.jacr.2020.09.012. [DOI] [PubMed] [Google Scholar]
- 36.Kaewlai R, Avery LL, Asrani AV, Novelline RA. Multidetector CT of blunt thoracic trauma. Radiographics. 2008;28:1555–1570. doi: 10.1148/rg.286085510. [DOI] [PubMed] [Google Scholar]
- 37.Vignon P, Boncoeur MP, Francois B, Rambaud G, Maubon A, Gastinne H. Comparison of multiplane transesophageal echocardiography and contrast-enhanced helical CT in the diagnosis of blunt traumatic cardiovascular injuries. Anesthesiology. 2001;94:615–622. doi: 10.1097/00000542-200104000-00015. discussion 615A. [DOI] [PubMed] [Google Scholar]
- 38.Nabeel M, Williams KA Sr. A broken heart: right ventricular rupture after blunt cardiac injury. J Cardiovasc Comput Tomogr. 2013;7:133–135. doi: 10.1016/j.jcct.2013.01.015. [DOI] [PubMed] [Google Scholar]
- 39.Park MR, Min MK, Ryu JH, Lee DS, Lee KH. Extension of a coronary intramural hematoma after blunt chest trauma. Ulus Travma Acil Cerrahi Derg. 2018;24:78–81. doi: 10.5505/tjtes.2017.72393. [DOI] [PubMed] [Google Scholar]
- 40.Sadr-Ameli MA, Amiri E, Pouraliakbar H, Heidarali M. Left anterior descending coronary artery dissection after blunt chest trauma. Arch Iran Med. 2014;17:86–90. [PubMed] [Google Scholar]
- 41.Huang JF, Hsieh FJ, Fu CY, Liao CH. Non-operative management is feasible for selected blunt trauma patients with pericardial effusion. Injury. 2018;49:20–26. doi: 10.1016/j.injury.2017.11.034. [DOI] [PubMed] [Google Scholar]
- 42.Thorson CM, Namias N, Van Haren RM, Guarch GA, Ginzburg E, Salerno TA, Schulman CI, Livingstone AS, Proctor KG. Does hemopericardium after chest trauma mandate sternotomy? J Trauma Acute Care Surg. 2012;72:1518–1524. doi: 10.1097/TA.0b013e318254306e. discussion 1524-1515. [DOI] [PubMed] [Google Scholar]
- 43.Witt CE, Linnau KF, Maier RV, Rivara FP, Vavilala MS, Bulger EM, Arbabi S. Management of pericardial fluid in blunt trauma: variability in practice and predictors of operative outcome in patients with computed tomography evidence of pericardial fluid. J Trauma Acute Care Surg. 2017;82:733–741. doi: 10.1097/TA.0000000000001386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Tanizaki S, Nishida S, Maeda S, Ishida H. Non-surgical management in hemodynamically unstable blunt traumatic pericardial effusion: a feasible option for treatment. Am J Emerg Med. 2018;36:1655–1658. doi: 10.1016/j.ajem.2018.06.066. [DOI] [PubMed] [Google Scholar]
- 45.Hammer MM, Raptis DA, Cummings KW, Mellnick VM, Bhalla S, Schuerer DJ, Raptis CA. Imaging in blunt cardiac injury: computed tomographic findings in cardiac contusion and associated injuries. Injury. 2016;47:1025–1030. doi: 10.1016/j.injury.2015.11.008. [DOI] [PubMed] [Google Scholar]
- 46.Vasileiou G, Qian S, Al-Ghamdi H, Pace D, Rattan R, Mulder M, Namias N, Dante Yeh D. Blunt trauma: what is behind the widened mediastinum on chest X-ray (CXR)? J Surg Res. 2019;243:23–26. doi: 10.1016/j.jss.2019.04.079. [DOI] [PubMed] [Google Scholar]
- 47.Ugalde IT, Prater S, Cardenas-Turanzas M, Sanghani N, Mendez D, Peacock J, Guvernator G, Koerner C, Allukian M 3rd. Chest x-ray vs. computed tomography of the chest in pediatric blunt trauma. J Pediatr Surg. 2020 doi: 10.1016/j.jpedsurg.2020.09.003. [DOI] [PubMed] [Google Scholar]
- 48.Velmahos GC, Karaiskakis M, Salim A, Toutouzas KG, Murray J, Asensio J, Demetriades D. Normal electrocardiography and serum troponin I levels preclude the presence of clinically significant blunt cardiac injury. J Trauma. 2003;54:45–50. doi: 10.1097/00005373-200301000-00006. discussion 50-41. [DOI] [PubMed] [Google Scholar]
- 49.Bayer MJ, Burdick D. Diagnosis of myocardial contusion in blunt chest trauma. JACEP. 1977;6:238–242. doi: 10.1016/s0361-1124(77)80460-7. [DOI] [PubMed] [Google Scholar]
- 50.Burrell AJ, Kaye DM, Fitzgerald MC, Cooper DJ, Hare JL, Costello BT, Taylor AJ. Cardiac magnetic resonance imaging in suspected blunt cardiac injury: a prospective, pilot, cohort study. Injury. 2017;48:1013–1019. doi: 10.1016/j.injury.2017.02.025. [DOI] [PubMed] [Google Scholar]
- 51.Rozycki GS, Ballard RB, Feliciano DV, Schmidt JA, Pennington SD. Surgeon-performed ultrasound for the assessment of truncal injuries: lessons learned from 1540 patients. Ann Surg. 1998;228:557–567. doi: 10.1097/00000658-199810000-00012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Rozycki GS, Ochsner MG, Jaffin JH, Champion HR. Prospective evaluation of surgeons’ use of ultrasound in the evaluation of trauma patients. J Trauma. 1993;34:516–526. doi: 10.1097/00005373-199304000-00008. discussion 526-517. [DOI] [PubMed] [Google Scholar]
- 53.Shimbo M, Watanabe H, Watanabe K, Yamaura G, Ito H. Blunt traumatic rupture of the right ventricle: visualization of spurting blood using transthoracic echocardiography. Eur Heart J Cardiovasc Imaging. 2016;17:1258. doi: 10.1093/ehjci/jew129. [DOI] [PubMed] [Google Scholar]
- 54.Smith DC, Bansal RC. Transesophageal echocardiography in the diagnosis of traumatic rupture of the aorta. N Engl J Med. 1995;333:457–458. [PubMed] [Google Scholar]
- 55.Qamar SR, Wu Y, Nicolaou S, Murray N. State of the art imaging review of blunt and penetrating cardiac trauma. Can Assoc Radiol J. 2020;71:301–312. doi: 10.1177/0846537119899200. [DOI] [PubMed] [Google Scholar]
- 56.Benjamin E, Cho J, Recinos G, Dilektasli E, Lam L, Brunner J, Inaba K, Demetriades D. Negative computed tomography can safely rule out clinically significant intra-abdominal injury in the asymptomatic patient after blunt trauma: prospective evaluation of 1193 patients. J Trauma Acute Care Surg. 2018;84:128–132. doi: 10.1097/TA.0000000000001705. [DOI] [PubMed] [Google Scholar]


