Abstract
The datasets summarized in this article include more than 38 million appointment wait times that U.S. military veterans experienced when seeking medical care since January 2014. Our data include both within Veterans Health Administration (VHA) facilities and community medical centers, and wait times are stratified by primary/specialty care type. Deidentified wait time data are reported at the referral-level, at the VHA facility-level, and at the patient's 3-digit ZIP code-level.
As of this writing, no other U.S. health care system has made their wait times publicly available. Our data thus represent the largest, national, and most representative measures of timely access to care for patients of both VHA and community providers. Researchers may use these datasets to identify variations in appointment wait times both longitudinally and cross-sectionally, conduct research on policies and interventions to improve access to care, and to incorporate fine-grained measures of wait times into their analyses.
Keywords: Veterans, Veterans Health Administration, Primary care, Specialty care, Wait times, Access to care, Medical care
Specifications Table
| Subject | Public Health and Health Policy |
| Specific subject area | Geographic variation in appointment wait times for medical care |
| Type of data | Preprocessed Data Files SQL scripts Tables Figures |
| How data were acquired | Monthly data on appointment requests, appointment approvals, and completed appointments for medical care were obtained by querying the VHA Corporate Data Warehouse (CDW). |
| Data format | Preprocessed |
| Parameters for data collection | We collected data on primary and specialty care consultations for all appointment types occurring from January 1, 2014 through December 31st, 2020. New data will be added approximately quarterly. Records with missing values for facility or appointment type were excluded. |
| Description of data collection | All data were accessed directly from the VHA CDW using SQL queries, deidentified, and then reported at either the referral-level or aggregated to the level of the VHA facility or county. |
| Data source location | VHA Corporate Data Warehouse (CDW). https://www.hsrd.research.va.gov/for_researchers/vinci/cdw.cfm |
| Data accessibility | Repository name: Mendeley Data Data identification number: https://data.mendeley.com/datasets/rmk89k4rhb Instructions for accessing these data: Pre-processed data and SQL scripts are publicly-available for direct download. |
| Related research article | K.N. Griffith, N.J. Ndugga, S.D. Pizer, 2020. Appointment Wait Times for Specialty Care in Veterans Health Administration Facilities vs Community Medical Centers. JAMA Network Open. 2020;3(8):e2014313. https://doi.org/10.1001/jamanetworkopen.2020.14313 |
Value of the Data
-
•
There are currently not nationwide, publicly available datasets of appointment wait times within the United States.
-
•
Our data provide a unique opportunity for researchers and data journalists to measure wait times for veterans to access care both within the VHA and in the community, both cross-sectionally and over time.
-
•
Facility, county, and referral-level data describe substantial variation in appointment wait times for VHA and community-based providers across a broad range of specialties.
-
•
The large sample size, nationwide coverage, consistent data collection, and broad range of appointment types provide several advantages over previously-published estimates of wait times.
-
•
Researchers may leverage these and other datasets to study the relationship between health policies, appointment wait times, and a wide variety of health, economic, and social outcomes.
1. Data Description
Prior to 2014, the Veterans Health Administration (VHA) only reimbursed providers in the community who provided medical care to veterans when the VHA was unable to do so (e.g. nearby facilities did not have certain types of specialists) or for emergency care [1]. The 2014 Veteran Health Administration (VHA) wait time scandal prompted a nationwide investigation into the amount of time Veterans spent waiting to receive care, and whether their delayed access contributed to significant adverse health outcomes [2]. Congress responded by passing the Veteran's Access to Care through Choice, Accountability, and Transparency Act of 2014, which authorized $16 billion for the Veterans Choice Program (VCP). Under the VCP, veterans who live more than 40 miles from the nearest VHA facility or could not schedule an appointment within 30 days were now permitted to receive care through community providers who contract with the VHA [3]. Congress expanded VCP eligibility criteria in 2015 to include Veterans with an “unusual and excessive burden for travel to VHA health care facilities,” such as geographic challenges, medical conditions, and environmental conditions like road blockages and traffic [4,5]. The MISSION Act of 2018 further expanded Veterans’ eligibility to access community care options and included additional interventions focused on telehealth and mobile deployment units to expand avenues for Veterans to interact with the health care system [6]. Eligible veterans may now seek VHA-funded care from community providers if their estimated drive time to the nearest VHA facility exceeds 60 min, replacing the VCP's 40 mile eligibility standard.
The VHA Corporate Data Warehouse (CDW) contains a record for every referral to primary or specialty care, regardless of whether patients are seen at a VHA facility or community medical center. We observe dates for when referrals were requested, dates when appointments were schedule, and dates when appointments were completed. A consult status of “completed” indicates an initial encounter the healthcare provider who received the referral; additional follow-up appointments and procedures may occur after this date. We also observe primary/specialty type for each consult. Note that the VHA uses “stop codes” to identify care type; stop codes are 3-digit identifiers used to identify the work group primarily responsible for providing a clinical service, and are used for purposes of workload credit, managerial accounting, and program evaluation (see Table 1 for a list) [7]. These stop codes are unique to the VHA but have been grouped together by researchers to study primary care [8], mental health [9], and other specialties [10,11]. Local VHA facilities must first approve all referrals to community providers; we also observe dates of approval for these requests. Additional details on the consult request process are outlined in VHA Direction 1232(2) [12].
Table 1.
VHA stop code list (attached as separate file).
| Stop Code | Stop Code Description |
|---|---|
| 524 | ACTIVE DUTY SEXUAL TRAUMA |
| 674 | ADMIN PATIENT ACTIVITIES (Non-Count CBO) |
| 102 | ADMITTING/SCREENING |
| 190 | ADULT DAY HEALTH CARE |
| 302 | ALLERGY IMMUNOLOGY |
| 320 | ALZHEIMER'S AND DEMENTIA CLINIC |
| 418 | AMPUTATION CLINIC |
| 419 | ANESTHESIA PRE-OPERATION (OP) and/or POST-OP CONSULTATION |
| 317 | ANTI-COAGULATION CLINIC |
| 602 | ASSISTED HEMODIALYSIS |
| 203 | AUDIOLOGY |
| 217 | BLIND REHAB OUTPATIENT SPECIALIST (BROS) |
| 481 | BRONCHOSCOPY |
| 333 | CARDIAC CATHETERIZATION |
| 334 | CARDIAC STRESS TEST/EXERCISE TOLERANCE TEST (ETT) |
| 402 | CARDIAC SURGERY |
| 303 | CARDIOLOGY |
| 685 | CARE OF CCHT PROGRAM PATIENTS |
| 422 | CAST CLINIC |
| 683 | CCHT NON-VIDEO MONITORING |
| 168 | CHAPLAIN SERVICE-COLLATERAL |
| 167 | CHAPLAIN SERVICE-GROUP |
| 166 | CHAPLAIN SERVICE-INDIVIDUAL |
| 697 | CHART CONSULT |
| 330 | CHEMOTHERAPY PROCEDURES UNIT MEDICINE |
| 436 | CHIROPRACTIC CARE |
| 160 | CLINICAL PHARMACY |
| 119 | COMMUNITY NURSING HOME FOLLOW-UP |
| 450 | COMPENSATION AND PENSION (C&P) EXAM |
| 159 | COMPLEMENTARY & ALTERNATIVE THERAPIES |
| 322 | COMPREHENSIVE WOMEN'S PRIMARY CARE |
| 218 | COMPUTER ASSISTED TRAINING BLIND REHAB |
| 150 | COMPUTERIZED TOMOGRAPHY (CT) |
| 606 | CONTINUOUS AMBULATORY PERITONEAL DIALYSIS (CAPD) |
| 610 | CONTRACT DIALYSIS |
| 430 | CYSTO ROOM IN UROLOGY CLINIC |
| 554 | DAY HOSPITAL-GROUP |
| 506 | DAY HOSPITAL-INDIVIDUAL |
| 553 | DAY TREATMENT-GROUP |
| 505 | DAY TREATMENT-INDIVIDUAL |
| 180 | DENTAL |
| 656 | DEPARTMENT OF DEFENSE (DOD) NON VA CARE |
| 522 | Department of Housing and Urban Development (HUD)- VA Shared Housing (VASH) |
| 304 | DERMATOLOGY |
| 306 | DIABETES |
| 718 | DIABETIC RETINAL SCREENING |
| 403 | EAR, NOSE, AND THROAT (ENT) |
| 107 | ELECTROCARDIOGRAM (EKG) |
| 106 | ELECTROCEPHALOGRAM (EEG) |
| 369 | ELECTROPHYSIOLOGY LABORATORY |
| 130 | EMERGENCY DEPARTMENT |
| 212 | EMG-ELECTROMYOGRAM |
| 999 | EMPLOYEE HEALTH |
| 305 | ENDO METAB (EXCEPT DIABETES) |
| 142 | ENTEROSTOMAL TX, WOUND OR SKIN CARE |
| 345 | EPILEPSY CENTER OF EXCELLENCE |
| 126 | EVOKED POTENTIAL |
| 449 | FITTINGS & ADJUSTMENTS |
| 307 | GASTROENTEROLOGY |
| 321 | GASTROINTESTINAL (GI) ENDOSCOPY |
| 301 | GENERAL INTERNAL MEDICINE |
| 401 | GENERAL SURGERY |
| 318 | GERIATRIC CLINIC |
| 319 | GERIATRIC EVALUATION AND MANAGEMENT (GEM) |
| 350 | GERIATRIC PRIMARY CARE |
| 511 | GRANT AND PER DIEM |
| 352 | GRECC CLINICAL DEMONSTRATION |
| 404 | GYNECOLOGY |
| 405 | HAND SURGERY |
| 176 | HBPC-CLINICAL PHARMACIST |
| 175 | HBPC-DIETITIAN |
| 177 | HBPC-OTHER |
| 172 | HBPC-PHYSICIAN EXTENDER (NP, CNS, PA) |
| 171 | HBPC-RN AND LPN |
| 173 | HBPC-SOCIAL WORKER |
| 174 | HBPC-THERAPIST |
| 178 | HBPC/TELEPHONE |
| 156 | HBPC-PSYCHOLOGIST |
| 680 | HCBC ASSESSMENT |
| 529 | HCHV/HCMI |
| 120 | HEALTH SCREENING |
| 308 | HEMATOLOGY |
| 337 | HEPATOLOGY CLINIC |
| 170 | HOME BASED PRIMARY CARE (HBPC) – PHYSICIAN |
| 118 | HOME TREATMENT SERVICES |
| 608 | HOME/SELF CONTINUOUS AMBULATORY PERITONEAL DIALYSIS (CAPD) TRAINING |
| 604 | HOME/SELF HEMODIALYSIS TRAINING |
| 351 | HOSPICE CARE |
| 309 | HYPERTENSION |
| 591 | INCARCERATED VETERANS RE-ENTRY |
| 310 | INFECTIOUS DISEASE |
| 155 | INFO ASSISTS TECHNOLOGY |
| 547 | INTENSIVE SUBSTANCE USE DISORDER-GROUP |
| 548 | INTENSIVE SUBSTANCE USE DISORDER- IND |
| 438 | INTERMEDIATE LOW VISION CARE |
| 153 | INTERVENTIONAL RADIOGRAPHY |
| 214 | KINESIOTHERAPY (KT) |
| 108 | LABORATORY |
| 607 | LIMITED SELF CARE CONTINUOUS AMBULATORY PERITONEAL DIALYSIS (CAPD) |
| 451 | LOCALLY DEFINED CREDIT PAIR |
| 452 | LOCALLY DEFINED CREDIT PAIR |
| 453 | LOCALLY DEFINED CREDIT PAIR |
| 463 | LOCALLY DEFINED CREDIT PAIR |
| 468 | LOCALLY DEFINED CREDIT PAIR |
| 471 | LOCALLY DEFINED CREDIT PAIR |
| 477 | LOCALLY DEFINED CREDIT PAIR |
| 478 | LOCALLY DEFINED CREDIT PAIR |
| 485 | LOCALLY DEFINED CREDIT PAIR |
| 439 | LOW VISION CARE |
| 151 | MAGNETIC RESONANCE IMAGING (MRI) |
| 703 | MAMMOGRAM |
| 327 | MED PHYSICIAN (MD) PERFORM INVASIVE OPERATING ROOM(OR) PROCEDURE (PROC) |
| 336 | MEDICAL PRE-PROCEDURE EVALUATION |
| 329 | MEDICAL PROCEDURE UNIT |
| 394 | MEDICAL SPECIALTY SHARED APPOINTMENT |
| 328 | MEDICAL SURGICAL DAY UNIT (MSDU) |
| 550 | MENTAL HEALTH CLINIC (GROUP) |
| 502 | MENTAL HEALTH CLINIC INDIVIDUAL |
| 568 | MENTAL HEALTH COMPENSATED WORK THERAPY/SUPPORTED EMPLOYMENT (CWT/SE) FACE TO FACE |
| 574 | MENTAL HEALTH COMPENSATED WORK THERAPY/TRANSITIONAL WORK EXPERIENCE (CWT/TWE) FACE-TO-FACE |
| 512 | MENTAL HEALTH CONSULTATION |
| 539 | MENTAL HEALTH INTEGRATED CARE – GROUP |
| 534 | MENTAL HEALTH INTEGRATED CARE INDIVIDUAL |
| 552 | MENTAL HEALTH INTENSIVE CASE MANAGEMENT (MHICM) |
| 503 | MENTAL HEALTH RESIDENTIAL CARE INDIVIDUAL |
| 527 | MENTAL HEALTH TELEPHONE |
| 573 | MH INCENTIVE THERAPY FACE-TO-FACE |
| 567 | MH INTENSIVE CASE MANAGEMENT (MHICM) GROUP |
| 565 | MH INTERVENTION BIOMED CARE GROUP |
| 533 | MH INTERVENTION BIOMEDICAL CARE INDIVIDUAL |
| 566 | MH RISK-FACTOR-REDUCTION ED GROUP |
| 564 | MH TEAM CASE MANAGEMENT |
| 535 | MH VOCATIONAL ASSISTANCE – INDIVIDUAL |
| 575 | MH VOCATIONAL ASSISTANCE Group |
| 315 | NEUROLOGY |
| 406 | NEUROSURGERY |
| 434 | NON-OR ANESTHESIA PROCEDURES |
| 109 | NUCLEAR MEDICINE |
| 117 | NURSING |
| 124 | NUTRITION/DIETETICS/GROUP |
| 123 | NUTRITION/DIETETICS/INDIVIDUAL |
| 292 | OBSERVATION PSYCHIATRY |
| 206 | OCCUPATIONAL THERAPY |
| 316 | ONCOLOGY/TUMOR |
| 407 | OPHTHALMOLOGY |
| 523 | OPIOID SUBSTITUTION |
| 408 | OPTOMETRY |
| 409 | ORTHOPEDICS |
| 429 | OUTPATIENT CARE IN THE OPERATING ROOM |
| 311 | PACEMAKER |
| 335 | PADRECC (PARKINSON'S DISEASE RECC) |
| 420 | PAIN CLINIC |
| 353 | PALLIATIVE CARE |
| 561 | PCT-POST TRAUMATIC STRESS GROUP |
| 145 | PHARMACOLOGY or PHYSIOLOGIC NUCLEAR MYOCARDIAL PERFUSION STUDIES |
| 583 | PHYCHOSOCIAL REHABILITATION AND RECOVERY (PRRC), GROUP |
| 205 | PHYSICAL THERAPY |
| 410 | PLASTIC SURGERY |
| 201 | PM & RS |
| 211 | PM&RS AMPUTATION CLINIC |
| 222 | PM&RS COMPENSATED WORK THERAPY/SUPPORTED EMPLOYMENT (PM&RS CWT/SE) FACE TO FACE |
| 208 | PM&RS COMPENSATED WORK THERAPY/TRANSITIONAL WORK EXPERIENCE (PM&RS CWT/TWE) FACE- TO-FACE |
| 230 | PM&RS DRIVER TRAINING |
| 207 | PM&RS INCENTIVE THERAPY FACE-TO- FACE |
| 213 | PM&RS VOCATIONAL ASSISTANCE |
| 411 | PODIATRY |
| 196 | POLYTRAUMA TRANSITIONAL REHABILITATION PROGRAM GROUP |
| 195 | POLYTRAUMA TRANSITIONAL REHABILITATION PROGRAM INDIVIDUAL |
| 198 | POLYTRAUMA/TRAUMATIC BRAIN INJURY (TBI)-GROUP |
| 197 | POLYTRAUMA/TRAUMATIC BRAIN INJURY (TBI)-INDIVIDUAL |
| 199 | POLYTRAUMA/TRAUMATIC BRAIN INJURY (TBI)-TELEPHONE |
| 146 | POSITRON EMISSION TOMOGRAPHY (PET) |
| 516 | POST TRAUMATIC STRESS DISORDER (PTSD)-GROUP |
| 331 | PRE-BED CARE (MD) (MEDICAL SERVICE) |
| 332 | PRE-BED CARE RN (MEDICAL SERVICE) |
| 432 | PRE-SURGERY EVALUATION BY MD |
| 416 | PRE-SURGERY EVALUATION BY NON-MD |
| 433 | PRE-SURGERY EVALUATION BY NURSING |
| 348 | PRIMARY CARE SHARED APPOINTMENT |
| 323 | PRIMARY CARE/MEDICINE |
| 412 | PROCTOLOGY |
| 128 | PROLONGED VIDEO-EEG MONITORING |
| 423 | PROSTHETIC AND SENSORY AIDS SERVICE |
| 417 | PROSTHETIC, ORTHOTICS |
| 557 | PSYCHIATRY-GROUP |
| 509 | PSYCHIATRY INDIVIDUAL |
| 577 | PSYCHOGERIATRIC CLINIC, GROUP |
| 576 | PSYCHOGERIATRIC CLINIC, INDIVIDUAL |
| 538 | PSYCHOLOGICAL TESTING |
| 558 | PSYCHOLOGY-GROUP |
| 510 | PSYCHOLOGY (PSO)-INDIVIDUAL |
| 559 | PSYCHOSOCIAL REHABILITATION-GROUP |
| 582 | PSYCHOSOCIAL REHABILITATION AND RECOVERY CENTER (PRRC), IND |
| 532 | PSYCHOSOCIAL REHABILITATION- INDIVIDUAL |
| 562 | PTSD-INDIVIDUAL |
| 540 | PTSD CLINICAL TEAM (PCT) POST-TRAUMATIC STRESS-INDIVIDUAL |
| 580 | PTSD DAY HOSPITAL |
| 104 | PULMONARY FUNCTION |
| 312 | PULMONARY/CHEST |
| 149 | RADIATION THERAPY TREATMENT |
| 144 | RADIONUCLIDE THERAPY |
| 179 | REAL TIME CLINICAL VIDEO CARE TO HOME |
| 690 | REAL TIME CLINICAL VIDEO TELEHEALTH-PATIENT SITE |
| 202 | RECREATION THERAPY SERVICE |
| 313 | RENAL/NEPHROL(EXCEPT DIALYSIS) |
| 474 | RESEARCH |
| 121 | RESIDENTIAL CARE [NON-MENTAL HEALTH (MH)] |
| 599 | RESIDENTIAL REHABILITATION TREATMENT PROGRAM (RRTP) PRE- ADMISION - GROUP |
| 598 | RESIDENTIAL REHABILITATION TREATMENT PROGRAM (RRTP) PRE- ADMISSION-INDIVIDUAL |
| 596 | RESIDENTIAL REHABILITATION TREATMENT PROGRAM (RRTP) ADMISSION SCREENING |
| 595 | RESIDENTIAL REHABILITATION TREATMENT PROGRAM (RRTP) AFTERCARE-GROUP |
| 593 | RESIDENTIAL REHABILITATION TREATMENT PROGRAM (RRTP) OUTREACH SERVICES |
| 116 | RESPIRATORY THERAPY |
| 314 | RHEUMATOLOGY/ARTHRITIS |
| 215 | SCI HOME CARE PROGRAM |
| 572 | SeRV-MH (Services for Returning Veterans-Mental Health) GROUP |
| 571 | SeRV-MH (Services for Returning Veterans-Mental Health) INDIVIDUAL |
| 349 | SLEEP MEDICINE |
| 143 | SLEEP STUDY |
| 707 | SMOKING CESSATION |
| 125 | SOCIAL WORK SERVICE |
| 204 | SPEECH PATHOLOGY |
| 210 | SPINAL CORD INJURY |
| 694 | STORE- AND- FORWARD TELEHEALTH – PATIENT SITE |
| 560 | SUBSTANCE USE DISORDER-GROUP |
| 514 | SUBSTANCE USE DISORDER-HOME VISIT |
| 513 | SUBSTANCE USE DISORDER-INDIVIDUAL |
| 519 | SUBSTANCE USE DISORDER/PTSD TEAMS |
| 435 | SURGICAL PROCEDURE UNIT |
| 182 | TELEPHONE CASE MANAGEMENT |
| 686 | TELEPHONE CONTACT BY CARE COORDINATION STAFF |
| 584 | TELEPHONE PSYCHOSOCIAL REHABILITATION AND RECOVERY CENTER (PRRC) |
| 216 | TELEPHONE REHABILITATION (REHAB) AND SUPPORT |
| 103 | TELEPHONE TRIAGE |
| 579 | TELEPHONE/ PSYCHOGERIATRICS |
| 147 | TELEPHONE/ANCILLARY |
| 229 | TELEPHONE/BLIND REHAB PROGRAM |
| 169 | TELEPHONE/CHAPLAIN |
| 181 | TELEPHONE/DENTAL |
| 148 | TELEPHONE/DIAGNOSTIC |
| 611 | TELEPHONE/DIALYSIS |
| 326 | TELEPHONE/GERIATRICS |
| 528 | TELEPHONE/HOMELESS CHRONICALLY MENTALLY ILL (HCMI) |
| 530 | TELEPHONE/HUD-VASH |
| 324 | TELEPHONE/MEDICINE |
| 536 | TELEPHONE/MH VOCATIONAL ASSISTANCE |
| 546 | TELEPHONE/MHICM |
| 325 | TELEPHONE/NEUROLOGY |
| 428 | TELEPHONE/OPTOMETRY |
| 425 | TELEPHONE/PROSTHETICS/ORTHOTICS |
| 537 | TELEPHONE/PSYCHOSOCIAL REHABILITATION |
| 542 | TELEPHONE/PTSD |
| 597 | TELEPHONE/RESIDENTIAL REHABILITATION TREATMENT PROGRAM (RRTP) |
| 545 | TELEPHONE/SUBSTANCE USE DISORDER |
| 424 | TELEPHONE/SURGERY |
| 221 | TELEPHONE/VISUAL IMPAIRMENT SERVICE TEAM (VIST) |
| 413 | THORACIC SURGERY |
| 457 | TRANSPLANT |
| 115 | ULTRASOUND |
| 131 | URGENT CARE |
| 414 | UROLOGY CLINIC |
| 421 | VASCULAR LABORATORY |
| 415 | VASCULAR SURGERY |
| 592 | VETERANS JUSTICE OUTREACH |
| 437 | VICTORS & ADVANCED LOW VISION |
| 220 | VISOR and ADVANCED BLIND REHAB |
| 209 | VIST COORDINATOR |
| 373 | WEIGHT MANAGEMENT COUNSELING (MOVE PROGRAM) GROUP |
| 372 | WEIGHT MANAGEMENT COUNSELING (MOVE PROGRAM) INDIVIDUAL |
| 704 | WOMEN'S GENDER- SPECIFIC PREVENTIVE CARE |
| 426 | WOMEN'S SURGERY |
| 525 | WOMEN'S STRESS DISORDER TREATMENT TEAMS |
| 105 | X-RAY |
| 110 | INTERVENTIONAL RADIOLOGY CLINIC |
| 111 | TELE-PATHOLOGY |
| 122 | PUBLIC HEALTH NURSING |
| 132 | MAMMOGRAM |
| 138 | SMOKING CESSATION |
| 139 | HEALTH/WELL BEING SERVICES |
| 192 | CAREGIVER SUPPORT |
| 219 | TRAUMATIC BRAIN INJURY |
| 224 | TELEPHONE SCI |
| 225 | TELEHEALTH VIRTUAL |
| 231 | CARDIO-PULMONARY REHAB |
| 240 | PM&R ASSIST TECH CLINIC |
| 241 | WHEELCHAIR |
| 250 | REHAV SERVICES GROUP |
| 338 | TELEPHONE PRIMARY CARE |
| 339 | OBSTETRICS |
| 340 | GENOMIC CARE |
| 344 | MULTIPLE SCLEROSIS |
| 346 | ALS CENTER |
| 354 | HOSPITAL IN HOME |
| 391 | CARDIAC ECHO |
| 392 | AMBULATORY ECG MONITORING |
| 427 | ANES SPECIAL PROCS |
| 441 | TELEPHONE ANESTHESIA |
| 486 | CARDIOTHORACIC SURGERY |
| 487 | BARIATRIC SURGERY |
| 488 | SURGICAL ONCOLOGY |
| 489 | SPINAL SURGERY |
| 507 | HUND/VASH GROUP |
| 508 | HCHV/HCMI GROUP |
| 531 | PRIMARY CARE FOR PATIENTS WITH SMI |
| 555 | HOMELESS VET SERVICES, INVIDUAL |
| 556 | HOMELESS VET SERVICES, GROUP |
| 563 | MH PRIMARY CARE - GROUP |
| 570 | MH CWT |
| 586 | RRTP INDIVIDUAL |
| 587 | RRTP GROUP |
| 589 | NON-ACTIVE DUTY SEXUAL TRAUMA |
| 642 | BMS CM FEE REQUEST |
| 660 | CHIROPRACTIC CARE OUTSIDE VA |
| 669 | COMMUNITY CARE CONSULT |
| 682 | VA REFER TO HCBC PROVIDER |
| 702 | CHOLESTEROL SCREENING |
| 728 | RRTP ADMISSION SCREENING SERVICES |
| 902 | CT SCANS |
| 903 | RADIATION THERAPY |
| 904 | CHEMOTHERAPY |
| 905 | AMBULATORY SURGERY SERVICES |
| 907 | NUCLEAR MAGNETIC RESONANCE |
Our data source thus incorporates the universe of primary and specialty care appointments paid for by the VHA from January 2014 through April 2021. The associated Mendeley data repository will be updated approximately quarterly with new data as they become available.
We calculated three types of appointment wait times by specialty:
-
(1)
Consult-level wait times wait times which include specialty type, year, whether a VHA or community provider were used, wait times, and patient's 3-digit ZIP Code.
-
(2)
County-level wait times which aggregates all appointment requests by patient's county of residence.
-
(3)
Facility-level wait times which aggregates all appointment requests to the VHA parent facility which provided approval. A parent facility is referred to as a “station” or “STA3N” within the VHA and may also have several subsidiary medical centers or community-based outpatient clinics assigned to it.
These datasets cover 41,249,208 consult requests for both primary and specialty care during the time period from January 1, 2014 through December 31, 2020. We fill an important data gap in U.S. health services research, which until now has lacked a large national dataset on appointment wait times for either primary or specialty care. We provide researchers and journalists with the broadest, most rigorously-collected datasets on wait times that are publicly-available. Data dictionaries for each dataset are available in Table 2, Table 3, Table 4.
Table 2.
Data dictionary: facility-Level.
| Variable Name | Variable Description |
|---|---|
| year | Calendar year |
| month | Calendar month |
| sta3n | VHA facility identifier |
| stopcode | VHA primary/specialty care type designation |
| count | The number of consults in the stop code-year-month-sta3n combination |
| dta | Days to approved |
| dts | Days to schedules |
| dtc | Days to completed |
| dtot | Sum of days to approved and days to completed |
| non_va | Community-based care indicator (1 if community care, 0 if VHA care) |
| address1 | Street address of VHA facility, line 1 |
| address2 | Street address of VHA facility, line 2 |
| city | City of VHA facility |
| state | State of VHA facility |
| zip | ZIP Code of VHA facility |
Table 3.
Data dictionary: ZIP3-level.
| Variable Name | Variable Description |
|---|---|
| year | Calendar year |
| month | Calendar month |
| stopcode | VHA primary/specialty care type designation |
| zip | Three-digit ZIP code |
| count | The number of consults in the stop code-year-month-ZIP3 combination |
| dta | Days to approved |
| dts | Days to schedules |
| dtc | Days to completed |
| dtot | Sum of days to approved and days to completed |
| non_va | Community-based care indicator (1 if community care, 0 if VHA care) |
Table 4.
Data dictionary: consultation-level.
| Variable Name | Variable Description |
|---|---|
| year | Calendar year |
| sta3n | VHA facility identifier |
| stopcode | VHA primary/specialty care type designation |
| dta | Days to approved |
| dts | Days to schedules |
| dtc | Days to completed |
| dtot | Sum of days to approved and days to completed |
| non_va | Community-based care indicator (1 if community care, 0 if VHA care) |
| zip | Patient's ZIP Code of residence (first three digits) |
| disp | Final disposition (i.e. completed, discontinued, or canceled) |
2. Experimental Design, Materials and Methods
We used SQL to query the VHA CDW and calculate wait times for referrals to both VHA and community-based providers. Referrals with completed, discontinued, or canceled status were included for calculations. Discontinued & cancelled appointments accounted for 2.3% and 1.7% of total consult volume respectively, and were included since their exclusion may bias estimates of wait times downwards (e.g. if a Veteran is unsatisfied with the wait and thus cancels their appointment). Referrals were excluded if an appointment was never scheduled, since no wait time was observed. Referrals were also excluded if they were missing information on facility or primary/specialty care type. Note the terms ‘consults’ and ‘referrals’ are used interchangeably within the VHA.
The CDW's Con.Consult table identifies the facility where the consult was created, a unique patient identifier, initial request date, and may be linked to other tables to identify consult type (e.g. cardiology, gastroenterology). The Con.ConsultActivity table tracks changes to the status of a consult and contains individual rows for when a consult is created, approved, scheduled, completed, cancelled, or discontinued. We use the ‘ActivityDateTime’ field to calculate four outcome measures:
-
(1)
Days to Approved, a measure of the difference between dates for when a consult is created and when it has been approved by the local VHA medical center. For community care, this is when the veteran was authorized to seek care in the community. A violin plot of approval wait times for four high-volume medical specialties is contained in Fig. 1. A violin plot is similar to a box plot with the addition of a rotated kernel density plot on each side which shows the distribution of the data.
-
(2)
Days to Scheduled, a measure of the difference between when a consult is approved and when the appointment is scheduled. For community care, this measure represents the date the local VHA medical center followed up with a Veteran and found out they have scheduled the appointment; this is likely several days or weeks after the Veteran actually made the appointment.
-
(3)
Days to Completed, a measure of the difference between when a consult is approved and when it was completed.
-
(4)
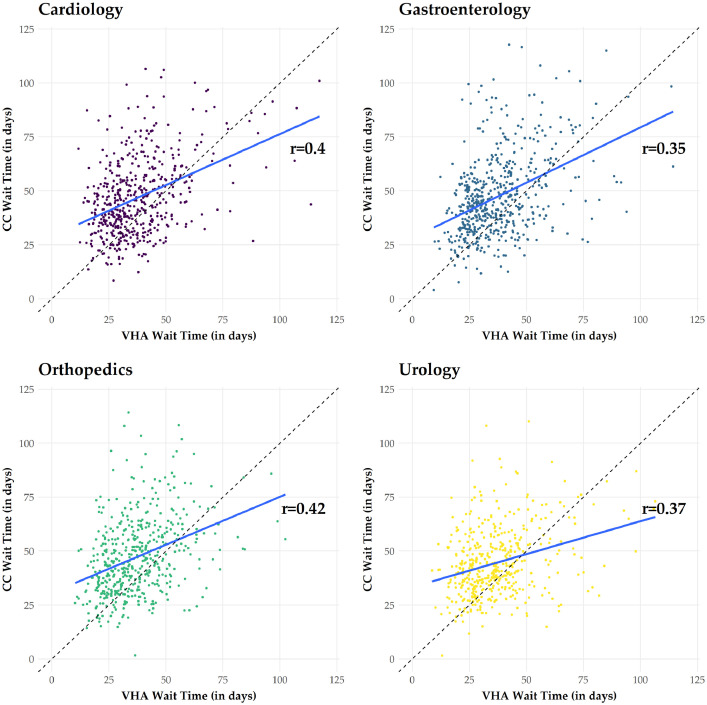
Total Wait Time, a measure of the difference between when a referral was initially requested and when the appointment was completed. For cancelled/discontinued appointments, this is the difference between when a referral was initially requested and the scheduled appointment date. A scatter plot of wait times for VHA and community care at the ZIP-3 is displayed in Fig. 2. On average, the VHA outperformed community medical centers in terms of mean wait times. Further, VHA wait times were positively correlated with wait times at community medical centers.
Fig. 1.
Number of days veterans wait for approval to seek care in the community for four high-volume specialties Notes: The figure displays violin plots of approval wait times during the study period. The white box represents the interquartile range, the black horizontal line represents the median, the black vertical line represents 1.5 times the interquartile range, and on each side is a kernel density estimation which shows the distribution of wait times.
Fig. 2.
Associations between wait times for veterans seeking care within the Veterans Health Administration and the community Notes: The figure displays scatter plots of VHA and community-care wait times for four high-volume specialties. Each dot represents a ZIP3-month. The blue line represents the regression line, and the dashed black line represents a 45-degree angle. Dots above the dashed-black line indicate ZIP3 codes where the wait times at community medical centers exceeded wait times at nearby VHA facilities. Pearson correlations are also displayed. (For interpretation of the references to color in this figure legend, the reader is referred to the web version of this article.)
The consult tables were also linked to the Appt.Appointments table through a unique ConsultSID, which allows us to observe actual appointment dates. These appointment dates were validated by chart reviews. We leveraged the ToRequestServiceName field of the Con.Consult CDW table to identify and exclude consultation types that had average completion times of < = 0.2 days. Chart reviews indicated these are mostly e-consultations (such as email or text messages between providers) that are opened and closed within a few minutes or hours.
Our referral-level wait time dataset indicates appointment year, wait time measures, 3-digit ZIP Code of the veteran's home address (obtained from the SPatient.SPatientAddress table), an indicator for whether the appointment was for a VHA or community provider, and the primary stop code. VHA uses primary stop codes (also known as Decision Support System Identifiers) to identify the main clinical group responsible for a patient's care (see Table 4). We created a facility-level dataset by averaging appointment wait times by each stop code in a given month.
The resulting referral-level dataset was then aggregated to calculate mean average wait times by month at the ZIP code- and VHA facility-level, then deidentified for public release. All data preparation was performed in Microsoft SQL Server Management Studio version 15.10.18206.0 (Redmond, WA). The latest SQL script used to calculate the three wait time datasets, as well as copies of each dataset, are publicly available within our Mendeley Data repository.
We note several important caveats with these data. Prior to 2018, there was no standardized method for VHA facilities to indicate whether or not a referral was to VHA or community-based providers. We identified referrals to the community by text searches of the ‘ToRequestServiceName’ field of the Con.Consult CDW table (e.g. mentions of ‘community care,’ ‘CHOICE,’ ‘fee basis’). We estimate that approximately 50% to 75% of community-based consultations were misclassified as VHA consultations before May 2018. The number of non-VA consults that we can identify increased sharply starting in 2018 (Fig. 3). This comports with guidance which went out on how to record these consults in the data (e.g. use of stop code 669 and including the phrase ‘COMMUNITY CARE’ in the ‘ToRequestServiceName’ field of the Con.Consult CDW table). The implementation of stop code ‘669’ has enabled better identification of community care consults. Unfortunately, this general stop code has also made it more difficult to identify their specialty. We follow a tiered approach to try and convert these 669 stop codes; in our tests, 87% of stop codes are matched to more informative stop codes.
Fig. 3.
Number of VHA facilities reporting internal and external referrals and referral volume over time Notes: The top-left panel displays monthly frequencies of referrals to community care. The top-right panel displays monthly frequencies of referrals within the VHA system. The bottom-left panel displays the number of VHA facilities that reported any referrals to community care in a given month. The bottom-right panel displays the number of VHA facilities that reported any referrals within the VHA system in a given month.
Lastly, VHA users who would like to run our code are advised not to examine wait times within the previous six months. Appointment information, especially for community care consults, may only appear in the CDW after long and variable lags of several months.
File inventory
-
•
Wait time data at the facility level (processed).
-
•
Wait time data at the county level (processed).
-
•
Wait time data at the consultation level (processed).
-
•
SQL script to calculate wait time datasets.
Ethics Statement
The Privacy Office of the Veterans Affairs Boston Healthcare System have certified these datasets are de-identified and may be publicly-released as part of this publication.
Declaration of Competing Interest
Yevgeniy Feyman, Aaron Legler, and Kevin Griffith are investigators at the VA Boston Healthcare System. The content is solely the responsibility of the authors and does not necessarily represent the views of the VHA, which did not have editorial input or control over this research.
Acknowledgments
None
References
- 1.R. Gidwani, J. Hong, S. Murrell, Fee basis data: a guide for researchers, (2015). https://www.herc.research.va.gov/include/page.asp?id=guidebook-fee-basis. Accessed January 18, 2021.
- 2.G. Lopez, The VA scandal of 2014, explained, vox. (2014). https://www.vox.com/2014/9/26/18080592/va-scandal-explained. Accessed January 18, 2021.
- 3.Stroupe K.T., Martinez R., Hogan T.P., Gordon E.J., Gonzalez B., Kale I., Osteen C., Tarlov E., Weaver F.M., Hynes D.M., Smith B.M. Experiences with the veterans’ choice program. J. Gen. Intern. Med. 2019;34:2141–2149. doi: 10.1007/s11606-019-05224-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.US Department of Veterans Affairs, Summary: veterans access, choice and accountability act of 2014 (“choice act”), (n.d.). https://www.va.gov/opa/choiceact/documents/choice-act-summary.pdf.
- 5.US Department of Veterans Affairs, How to become a veterans choice program and/or patient-centered community care provider, (n.d.). https://www.va.gov/opa/choiceact/documents/FactSheets/VACAA_Provider_Fact_Sheet_Choice_Program_508c_Internet.pdf.
- 6.J. Isakson, VA MISSION act of 2018, 2018. https://www.congress.gov/bill/115th-congress/senate-bill/2372/text. Accessed January 18, 2021.
- 7.Veterans Health Administration, Decision support system outpatient identifiers, (2013).
- 8.Smith V.A., Morgan P.A., Edelman D., Woolson S.L., Berkowitz T.S.Z., Van Houtven C.H., Hendrix C.C., Everett C.M., White B.S., Jackson G.L. Utilization and costs by primary care provider type : are there differences among diabetic patients of physicians, nurse practitioners, and physician assistants? Med. Care. 2020;58:681–688. doi: 10.1097/MLR.0000000000001326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Milicevic A.S., Mitsantisuk K., Tjader A., Vargas D.L., Hubert T.L., Scott B. Modeling patient no-show history and predicting future appointment behavior at the veterans administration's outpatient mental health clinics: NIRMO-2. Milit. Med. 2020;185:e988–e994. doi: 10.1093/milmed/usaa095. [DOI] [PubMed] [Google Scholar]
- 10.Griffith K.N., Ndugga N.J., Pizer S.D. Appointment wait times for specialty care in veterans health administration facilities vs community medical centers. JAMA Netw. Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.14313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Liu C.F., Batten A., Wong E.S., Fihn S.D., Hebert P.L. Fee-for-service medicare-enrolled elderly veterans are increasingly voting with their feet to use more va and less medicare, 2003–2014. Health Serv. Res. 2018;53:5140–5158. doi: 10.1111/1475-6773.13029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Veterans Health Administration, Consult processes and procedures, 2016. https://www.va.gov/vhapublications/ViewPublication.asp?pub_ID=3230. Accessed January 18, 2021.