Abstract
Objective
Lamotrigine is one of the most widely used antiepileptic drugs, but it has a critical issue of a skin rash if the starting dose is too high or the escalation rate is too rapid. We investigated the efficacy and safety of a novel and rapid titration protocol for lamotrigine that takes only 11 days to reach a daily dose of 200 mg.
Methods
We prospectively enrolled 33 adult patients (age 18‐85) who were diagnosed with epilepsy and started lamotrigine administration for the first time at a single tertiary hospital. Our new protocol starts with a subthreshold dose of the drug and then administers a stepwise‐incremental dose until reaching the full therapeutic dose within 11 days.
Results
Of 29 patients analyzed, only two (6.9%) experienced idiosyncratic skin rash before the first follow‐up visit at 2 weeks (±3 days). In addition, a therapeutic concentration was reached in more than 75% of studied patients after 2 weeks of lamotrigine administration.
Significance
These findings demonstrate the value of the novel tolerance induction protocol for lamotrigine, which could widen the available application of lamotrigine in various situations. However, this study is a preliminary study limited by a small number of patients and its nonrandomized and open‐label design, so the current protocol needs more rigorous clinical evaluations before the application to the real clinical setting.
Keywords: idiosyncratic skin rash, lamotrigine, rapid titration, skin rash, titration protocol
Key Points.
Lamotrigine has a high risk of cutaneous adverse reactions if the starting dose is too high or if the escalation is made too rapidly.
Thus, the conventional titration protocol recommends to be slower to be safer, taking more than 8 weeks to reach the usual maintenance dose.
We introduce a new lamotrigine titration protocol that takes only eleven days to reach the usual maintenance dose without increasing the risk of skin rash.
By reducing the titration duration, this protocol can lead to an increase in lamotrigine prescription for various indications including frequent seizures and psychiatric diseases.
1. INTRODUCTION
Lamotrigine is a widely used first‐line antiepileptic drug (AED) in both adults and children with epilepsy. 1 , 2 In particular, in elderly epilepsy patients, it is the drug of choice and has the highest retention rate. 3 Moreover, lamotrigine is also a useful option for psychiatric disorders such as bipolar disorder. 4 , 5 However, the major hindrance of lamotrigine administration has been the potentially life‐threatening skin rash. 6 , 7 As an aromatic AED, lamotrigine has a high risk of inducing an idiosyncratic adverse reaction. 8 The risk of lamotrigine‐induced skin rashes increases if the starting dose is too high or if the escalation is made too rapidly. 9 , 10 Thus, the conventional titration protocol has recommended to be slower to be safer, taking more than 8 weeks to reach the usual maintenance dose. 9 , 11 , 12
Tolerance induction of a drug in patients who have drug allergies can be achieved by administration protocol adjustment. 13 The main strategy is to start with the administration of a suboptimal dose of the drug antigen and then to administer a stepwise‐incremental dose until the full therapeutic dose is reached. 14 Various AEDs that are prone to skin rashes, including carbamazepine, oxcarbazepine, valproic acids, phenytoin, and phenobarbital, have been proven to be safely desensitized. 15 , 16 , 17 , 18 , 19 , 20 , 21 Moreover, even in chemotherapy, rituximab was also successfully desensitized by a stepwise‐incremental protocol via the intravenous or intraperitoneal route. 22 , 23 Likewise, with the same concept, tolerance to a certain drug has been successfully achieved even in drug‐naïve patients who were at high risk but never experienced drug rashes before. 24 Jung and the colleagues classified patients according to the presence of a certain type of human leukocyte antigen (HLA), which is strongly associated with allopurinol‐induced severe cutaneous reactions. The slow oral tolerance induction protocol of allopurinol was then applied to the high‐risk drug‐naïve patients, showing a significant reduction in the skin rash.
We hypothesized that the idiosyncratic skin rash in response to lamotrigine could be prevented with the rapid tolerance induction protocol, which would consequently shorten the duration of the titration. Here, we introduce a new lamotrigine titration protocol that takes only eleven days to reach the usual maintenance dose without increasing the risk of skin rash.
2. METHOD
2.1. Patient enrollments
We prospectively enrolled adult patients (age 18‐85) who were diagnosed with epilepsy and started lamotrigine administration for the first time at Seoul National University Hospital from July 2016 to November 2018. Patients who had ever been prescribed enzyme‐inducing AEDs (phenytoin, phenobarbital, carbamazepine, oxcarbazepine), enzyme‐inhibiting AED (valproic acid), or oral contraceptives or had ever experienced drug rashes were excluded.
2.2. Clinical assessment
This study was approved by the Institutional Review Board of the Seoul National University (IRB No 1605‐121‐764) and was registered at ClinicalTrials.gov (NCT 03220256). Written informed consent was obtained from all patients.
Patients were asked to visit the outpatient clinic after two weeks (±3 days) from the protocol onset. When the patient experienced any adverse event before the 1st follow‐up visit, they were informed to report the issue to the researcher by phone. Cutaneous adverse events were evaluated according to the Common Terminology Criteria for Adverse Events (CTCAE), version 4.0. The extent of the skin lesion was calculated using the Lund & Browder body surface chart. The primary outcome was defined as the occurrence of a skin rash until the 1st follow‐up. The secondary outcome was the severity of the skin rash, the lamotrigine serum level, and the occurrence of skin rash beyond 2 weeks of lamotrigine administration. The patients were disqualified from the study when they did not appear to a scheduled visit. Also, patients were dropped out from the study when they omitted three doses of two consecutive doses at their own discretion.
2.3. Lamotrigine rapid tolerance induction protocol
Lamotrigine was prescribed to the patients following an 11‐day schedule for the rapid tolerance induction protocol (Table 1, Figure 1). The protocol started with a dose of 0.1 mg, and the next dose was escalated to 1.5‐2.5 times the previous dose every 12 hours. From day 4, the same dose was given twice a day, and the daily dose of lamotrigine was escalated to 1.5‐2 times the previous dose every day, reaching 100 mg bid on day 11. After the 11th day, the dose was titrated according to the clinician's decision. Doses below 2.5 mg were mixed with lactose additive and prepared as powdered medicine at the hospital pharmacy.
TABLE 1.
Tolerance induction protocol for lamotrigine
| Day | Dose | Total daily dose |
|---|---|---|
| 1 | 0.1‐0.25 mg q12h | 0.35 mg |
| 2 | 0.5‐0.75 mg q12h | 1.25 mg |
| 3 | −1‐1.5 mg q12h | 2.5 mg |
| 4 | 2.5 mg bid | 5 mg |
| 5 | 5 mg bid | 10 mg |
| 6 | 10 mg bid | 20 mg |
| 7 | 15 mg bid | 30 mg |
| 8 | 25 mg bid | 50 mg |
| 9 | 50 mg bid | 100 mg |
| 10 | 75 mg bid | 150 mg |
| 11 | 100 mg bid | 200 mg |
Abbreviations: bid, twice a day; q12h, every 12 h.
FIGURE 1.
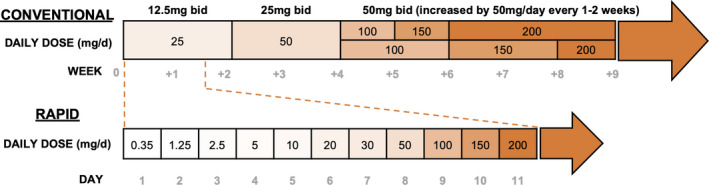
The protocols of lamotrigine titration. Scheme of the conventional and rapid lamotrigine titration protocols. The number inside the box indicates the daily dose of lamotrigine. The conventional protocols start with a dose of 12.5 mg bid for the first and second weeks and double it to 25 mg bid in the third and fourth weeks. From the fifth week, the daily dose is increased by 50 mg every 1‐2 wk, requiring up to 8 wk to reach the maintenance dose of 200 mg/d. This conventional protocol is for patients not taking cytochrome P inducer or inhibitor. Our rapid titration protocol starts with a dose of 0.1 mg, and the next dose is escalated to 1.5‐2.5 times the previous dose every 12 h. From day 4, the same dose is given twice a day, and the daily dose is escalated to 1.5‐2 times the previous dose every day, reaching 100 mg bid on day 11. After day 11, the dose is titrated according to the clinician's decision
2.4. Fluorescence‐activated cell sorting analysis of regulatory T cells before and after the titration protocol
We evaluated fluorescence‐activated cell sorting (FACS) analysis to evaluate the proportion of regulatory T (Treg) cells among CD4+ helper T cells before the lamotrigine rapid titration and after the 2 weeks (±3 days) of the 1st follow‐up visit because former studies have demonstrated the increase in the percentage of the total Treg cells after the tolerance induction of drugs.
The difference in the proportion of the Tregs before and after the lamotrigine rapid titration was analyzed with the Wilcoxon matched‐pairs signed‐rank test. STATA 14 (StataCorp LLC.) was used for analysis, and a P‐value <.05 was considered as statistically significant.
3. RESULT
3.1. Patient characteristics
Of the 33 patients who were enrolled in the current study, four patients (12%) were disqualified; two patients were lost to follow‐up, and two patients omitted lamotrigine more than 3 times without an agreement. Thus, twenty‐nine patients (88%) were ultimately analyzed (Table 2). Thirteen patients were males (44.8%), and the median age was 34 years [interquartile range, 36‐45 years]. Twenty‐four‐hour video electroencephalogram was performed for all patients; temporal lobe epilepsy was the most common diagnosis (15, 51.7%), followed by idiopathic generalized epilepsy (8, 27.6%). Seven patients (24.1%) had taken an AED before lamotrigine administration, with levetiracetam being the most common. None of the patients had taken an aromatic AED, previously.
TABLE 2.
Clinical response of patients with epilepsy after tolerance induction
| ID | Sex/Age | Diagnosis | Combined AED | Idiosyncratic skin rash a (days after LMT) | LMT level at 1st FU | Skin rash beyond 1st FU (days after LMT) | Rash type/BSA(%) b | Potential triggering factor | LMT discontinuation related to rash (daily dose at rash) | Follow‐up with LMT (months) |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | F/45 | Lt. OLE | + (14 d) | 6.9 | − | Maculopapular/18 | (−) | +(100 mg bid) | 0.5 | |
| 2 | M/20 | IGE | + (17 d) | N/A | − | Maculopapular/>95 | Propranolol c | +(100 mg bid) | 0.5 | |
| 3 | F/62 | Rt. TLE | − | 4.2 | + (19 d) | Maculopapular/41 | (−) | +(150 mg bid) | 0.5 | |
| 4 | F/31 | Bilat. TLE | − | 9.4 | + (24 d) | Maculopapular/91 | Roxithromycin d | +(100 mg bid) | 0.5 | |
| 5 | F/44 | Lt. TLE | − | 5.2 | + (37 d) | Maculopapular/6 | Celecoxib e | +(100 mg bid) | 1 | |
| 6 | F/56 | Lt. TLE | − | 5.1 | − | − | 8 | |||
| 7 | F/71 | Lt. TLE | − | 4.1 | − | − | 8 | |||
| 8 | M/31 | Lt. TLE | − | 0.3 | − | − | 8 | |||
| 9 | M/60 | Lt. TLE | − | N/A | − | − | 8 | |||
| 10 | F/36 | Rt. TLE | − | N/A | − | − | 8 | |||
| 11 | F/24 | IGE | LEV | − | N/A | − | − | 8 | ||
| 12 | M/34 | Lt. TLE | − | N/A | − | − | 8 | |||
| 13 | F/23 | Lt. TLE | − | 4.7 | − | − | 9 | |||
| 14 | F/29 | Rt. TLE | − | 4.6 | − | − | 9 | |||
| 15 | M/32 | Lt. FTLE | LEV | − | N/A | − | − | 18 | ||
| 16 | F/59 | Lt. OLE | − | 2.1 | − | − | 19 | |||
| 17 | M/27 | IGE | − | <0.1 | − | − | 20 | |||
| 18 | F/72 | Lt. TLE | − | 3.8 | − | − | 22 | |||
| 19 | F/22 | IGE | − | 3.4 | − | − | 23 | |||
| 20 | M/35 | Bilat. FLE | LEV | − | 2.6 | − | − | 23 | ||
| 21 | M/20 | IGE | LEV | − | 2.6 | − | − | 24 | ||
| 22 | F/49 | JAE | CLZ | − | 3.6 | − | − | 24 | ||
| 23 | M/34 | Rt. TLE | LEV | − | 5.5 | − | − | 25 | ||
| 24 | M/26 | IGE | ETX | − | 4.6 | − | − | 27 | ||
| 25 | M/24 | Lt. TLE | − | N/A | − | − | 27 | |||
| 26 | M/26 | IGE | − | 2.4 | − | − | 29 | |||
| 27 | F/34 | Bilat. TLE | − | 1.6 | − | − | 30 | |||
| 28 | F/18 | Rt. FLE | LEV | − | 4.7 | − | − | 31 | ||
| 29 | M/39 | IGE | − | 3.2 | − | − | 32 |
Abbreviations: AED, antiepileptic drug; Bilat., bilateral; BSA, body surface area; CLZ, clonazepam; ETX, ethosuximide; FLE, frontal lobe epilepsy; FTLE, frontotemporal epilepsy; FU, follow‐up; IGE, idiopathic generalized epilepsy; JAE, juvenile absence epilepsy; LEV, levetiracetam; LMT, lamotrigine; Lt., left; OLE, occipital epilepsy; Rt., right; TLE, temporal lobe epilepsy.
Idiosyncratic skin rash was defined as the incidence of rash within 2 wk (14 d ± 3) of lamotrigine onset.
The extent of skin rash was calculated using the Lung & Browder body surface chart.
Propranolol was coadministered for one day before the rash.
Codeine, bromhexine, chlorpheniramine, and roxithromycin were coadministered for 3 d before the rash.
Celecoxib was coadministered for 9 d before the rash.
3.2. Idiosyncratic skin rash occurrence after lamotrigine rapid titration
Two patients (2 of 29, 6.9%) experienced idiosyncratic skin rash before the 1st follow‐up visit (Table 2). One patient (Patient ID 1) had a relatively mild rash on the arms and one leg (BSA 18%) on day 14 (on lamotrigine dose 100 mg bid). The skin lesion disappeared after changing the AED to levetiracetam. The other patient (Patient ID 2) experienced acute‐onset maculopapular rash on the whole body (BSA > 95%) on day 17 (on lamotrigine dose 100 mg bid) just after the administration of propranolol due to newly diagnosed postural tachycardia syndrome. The rash subsided the next day after withholding lamotrigine and propranolol.
3.3. Serum lamotrigine level and long‐term assessment
At the 1st follow‐up visit, the serum lamotrigine level was checked in 22 patients (75.9%) (Table 2). The mean value of the serum lamotrigine level was 3.85 μg/mL (SD 2.07). Among them, 17 patients (77.2%) successfully reached the therapeutic serum level (2.5‐15 μg/mL) 25 within 2 weeks.
Beyond the 1st follow‐up visit at 2 weeks (±3 days), a delayed‐onset skin rash appeared in three patients (Patient ID 3, 4, and 5, 10.3%). One patient (Patient ID 3) had a maculopapular rash on the neck, body, arms, and legs (BSA 41%) on day 19 just after increasing the dose of lamotrigine to 150 mg twice a day. One patient (Patient ID 4) experienced a maculopapular rash on almost the whole body below the neck (BSA 91%) on day 24 (on lamotrigine 100 mg bid), but it was unclear whether the rash was induced by lamotrigine. While the dosage of lamotrigine was maintained at 100 mg twice a day for nearly 2 weeks, common cold drugs (codeine, bromhexine, chlorpheniramine, and roxithromycin) were given to the patient since 3 days before the rash occurrence. After withholding the cold medications and lamotrigine, the rash subsided. The other patient (Patient ID 5) reported a very mild skin rash on the thigh on day 28; therefore, the lamotrigine was prescribed continuously (on 100 mg bid). Afterward, celecoxib was added as the painkiller for an orthopedic reason. After 9 days, the skin rash on the hand and thigh (BSA 6%) flared up; therefore, lamotrigine and celecoxib were stopped. The rash disappeared soon after the discontinuation. However, none of the patients experienced Stevens‐Johnson syndrome or toxic epidermal necrosis.
3.4. The proportion of regulatory T cells among the total CD4+ T cells before and after the titration protocol
FACS analysis of the Treg cells was performed before and after the lamotrigine rapid titration in 10 patients. The mean value of the percentage of Treg before the titration was 4.64% (SD 0.64), and that of Treg after the titration was 4.00% (SD 0.93). No statistically significant alteration of the Treg proportion was observed after the lamotrigine tolerance induction (P = .333).
4. DISCUSSION
Here, we demonstrated a new titration protocol for lamotrigine that could be faster and safer than the conventional titration protocol. The conventional protocol starts with a dose of 25 mg per day and doubles it every one to 2weeks, requiring up to 8 weeks to reach the maintenance dose of 200 mg per day. Our rapid protocol dramatically reduces the time required for titration and reaches 200 mg per day in 11 days without severe cutaneous adverse reactions.
The new titration protocol was safer in terms of cutaneous adverse reactions when compared to the conventional titration protocol, at least in the Asian population. Only 6.9% (2/29) of the patients experienced skin rash during rapid titration, which was lower than the rate of cutaneous adverse reactions after lamotrigine in the Korean and Japanese studies, which have been reported to be up to 22.5% (23/102) and 13.1% (130/989), respectively. 26 , 27 Furthermore, one of these patients experienced idiosyncratic skin rash just after the administration of propranolol, suggesting that lamotrigine may not be the true cause of the skin rash. However, in a retrospective study conducted in different ethnic groups, the incidence of the rash was lower in the Northern American (5.7%) than in the Korean studies. 28 Meta‐analysis researches including Asian and European‐Caucasian subjects showed that lamotrigine‐related skin rash was reported as around 10% in prospective studies. 8 , 10 Considering that our study was conducted in a prospective manner in which adverse events are generally reported more, the safety of the rapid titration protocol would not be inferior to the conventional protocol across the geographic difference.
The additional three patients encountered skin rash beyond the 1st follow‐up visit; one patient experienced skin rash after the dose escalation of lamotrigine to 150 mg bid, and two patients experienced skin rash after the administration of a potentially causative drug (roxithromycin and celecoxib, respectively). We think the skin rash could have been preventable by further protocol refinement in the first patient and the lamotrigine was not the culprit drug in the latter two patients.
The new titration protocol allows the lamotrigine serum levels to rise rapidly to the therapeutic range in a fairly short time. At the 1st follow‐up visit, 2 weeks (±3 days) after lamotrigine administration, the therapeutic concentration was reached in more than three‐quarters of the measured patients. Two patients (Patient ID 14 and 23) with frequent seizures at baseline (5 times/wk and 2 times/wk, respectively) experienced significant seizure reduction by reaching the therapeutic concentration (serum lamotrigine level 4.6 and 5.5 μg/mL, respectively) within 2 weeks of lamotrigine administration. Conventionally, patients who start taking lamotrigine would be exposed to sustained risk of seizure for nearly 2 months until the lamotrigine reaches the therapeutic levels. Therefore, combined prescription of other AEDs is often required during the titration period. Thus, the current protocol would be extremely useful in severe epilepsy patients with frequent seizures, and it will shorten the duration of bridging therapy during the conversion from other AEDs to lamotrigine. Moreover, this protocol can be useful in the acute management of psychiatric disorders such as bipolar disorder in an acute stage of a manic state.
Desensitization protocols, originally developed for the prevention of drug allergies, can also be effective when starting a new drug. Desensitization protocols induce temporary tolerance to a drug in patients who have experienced drug hypersensitivity. 29 The protocols start with a suboptimal dose of the drug antigen at fixed time intervals, followed by stepwise increases to full therapeutic doses, and they have been successful at avoiding skin rashes in response to many drugs, including AEDs and antibiotics. 30 , 31 Desensitization protocols can be refined by increasing the step of incremental dose, which normally induces fewer symptoms. 32 The mechanism of desensitization is not fully understood, but it is thought to be achieved by reducing the mast cell and basophil response or by increasing drug‐specific Treg cells, 14 , 32 , 33 so that it could also be effective in drug‐naïve patients. Jung et al 24 demonstrated that the desensitization protocol was useful during the first administration of allopurinol in high‐risk patients. In line with this, our study demonstrates that tolerance to lamotrigine can be achieved by applying the rapid desensitization protocol to patients who start receiving lamotrigine.
However, the exact mechanism of tolerance induction is worth being investigated. We assessed the proportion of Treg cells among the total CD4+ T cells before and after the protocol in some patients, which did not demonstrate any meaningful alterations. This shows the different result with other studies of AED desensitization having the increase in the proportion of the total Tregs after the tolerance induction. The discrepancy could come from the fundamental difference in the immune reactions, in that our tolerance induction targets the naive immune cells, but the former studies are the desensitization protocol against the memory T cells, which the patients already had had the immunity against the AEDs. Thus, for the tolerance induction, the percentage of the antigen‐specific Treg cells, not that of the total Treg cells, could have mattered to the tolerance induction. The alteration of drug‐specific T cells and mast cell/basophil functions after titration should be investigated in the future.
This study is limited by a small number of patients and its nonrandomized and open‐label design. Therefore, this is a preliminary study and subsequent studies should be conducted in a larger number of patients with a multicenter randomized control trial including a control group of patients treated with conventional lamotrigine titration protocol. In addition, we excluded patients who were taking enzyme inducers of enzyme inhibitors, so the current protocol needs more rigorous clinical evaluations before the application to the real clinical setting. Further protocol refinement may increase the safety of the protocol, and strategies for increasing lamotrigine to a higher daily dose (beyond 100 mg bid) should be investigated.
In conclusion, our study demonstrated a successful rapid tolerance induction protocol for lamotrigine in patients with epilepsy. It significantly reduced the duration of titration to 11 days with noticeable safety, which will be extremely helpful in patients with frequent seizures who require prompt dose escalation of AEDs. Moreover, this protocol can lead to an increase in lamotrigine prescription for various indications. Thus, additional refinement and validation of the protocol should be investigated in a larger trial in the near future.
CONFLICT OF INTEREST
The authors declare no conflict of interests. We confirm that we have read the Journal's position on issues involved in ethical publication and affirm that this report is consistent with those guidelines.
AUTHOR CONTRIBUTIONS
Y.J and JM wrote and revised the manuscript. Y.J, NK, and JM analyzed the data. Y.J, J.M, T‐J. K, J‐S. J., Y‐W. S, H.C, S‐T. L, K‐I. P, K‐Y. J, K.C, and SKL collected clinical data. J.M, H‐R. K, K.C, and SKL provided study concepts and revised the manuscript. J.M, S‐T. L, K‐H. J, K‐I. P, K‐Y. J, KC and SKL provided materials and funding. KC and SKL supervised the study. All authors reviewed the manuscript.
ACKNOWLEDGEMENTS
This study was supported by the Seoul National University Hospital Research Fund (0420170820) and Samjin Pharmaceutical (0620201110). We appreciate the support of Hong Won Jang and Yoon Sook Cho at the SNUH Clinical Trial Center Pharmacy and the Hospital Pharmacy.
Jang Y, Moon J, Kim N, et al. A new rapid titration protocol for lamotrigine that reduces the risk of skin rash. Epilepsia Open. 2021;6:394–401. 10.1002/epi4.12495
Yoonhyuk Jang and Jangsup Moon contributed equally to this study.
Contributor Information
Kon Chu, Email: stemcell.snu@gmail.com, Email: sangkun2923@gmail.com.
Sang Kun Lee, Email: stemcell.snu@gmail.com, Email: sangkun2923@gmail.com.
REFERENCES
- 1. Kwan P, Brodie MJ. Effectiveness of first antiepileptic drug. Epilepsia. 2001;42(10):1255–60. [DOI] [PubMed] [Google Scholar]
- 2. Nevitt SJ, Sudell M, Weston J, Tudur Smith C, Marson AG. Antiepileptic drug monotherapy for epilepsy: a network meta‐analysis of individual participant data. Cochrane Database Syst Rev. 2017;12:CD011412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Arif H, Buchsbaum R, Pierro J, Whalen M, Sims J, Resor SR, et al. Comparative effectiveness of 10 antiepileptic drugs in older adults with epilepsy. Arch Neurol. 2010;67(4):408–15. [DOI] [PubMed] [Google Scholar]
- 4. Prabhavalkar KS, Poovanpallil NB, Bhatt LK. Management of bipolar depression with lamotrigine: an antiepileptic mood stabilizer. Front Pharmacol. 2015;6:242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Geddes JR, Calabrese JR, Goodwin GM. Lamotrigine for treatment of bipolar depression: independent meta‐analysis and meta‐regression of individual patient data from five randomised trials. Br J Psychiatry. 2009;194(1):4–9. [DOI] [PubMed] [Google Scholar]
- 6. Moon J, Park HK, Chu K, Sunwoo JS, Byun JI, Lim JA, et al. The HLA‐A* 2402/C w* 0102 haplotype is associated with lamotrigine‐induced maculopapular eruption in the Korean population. Epilepsia. 2015;56(10):e161–e167. [DOI] [PubMed] [Google Scholar]
- 7. Kim B‐K, Jung J‐W, Kim T‐B, Chang Y‐S, Park H‐S, Moon J, et al. HLA‐A* 31: 01 and lamotrigine‐induced severe cutaneous adverse drug reactions in a Korean population. Ann Allergy Asthma Immunol. 2017;118(5):629–30. [DOI] [PubMed] [Google Scholar]
- 8. Wang XQ, Xiong J, Xu WH, Yu SY, Huang XS, Zhang JT, et al. Risk of a lamotrigine‐related skin rash: current meta‐analysis and postmarketing cohort analysis. Seizure. 2015;25:52–61. [DOI] [PubMed] [Google Scholar]
- 9. Wong IC, Mawer GE, Sander JW. Factors influencing the incidence of lamotrigine‐related skin rash. Ann Pharmacother. 1999;33(10):1037–42. [DOI] [PubMed] [Google Scholar]
- 10. Guberman AH, Besag FMC, Brodie MJ, Dooley JM, Duchowny MS, Pellock JM, et al. Lamotrigine‐associated rash: risk/benefit considerations in adults and children. Epilepsia. 1999;40(7):985–91. [DOI] [PubMed] [Google Scholar]
- 11. John AM. Rash in adult and pediatric patients treated with lamotrigine. Can J Neurological Sci. 1998;25(S4):S14–S18. [DOI] [PubMed] [Google Scholar]
- 12. Alan HG, Frank MCB, Martin JB, Joseph MD, Michael SD, John MP, et al. Lamotrigine‐associated rash: risk/benefit considerations in adults and children. Epilepsia. 1999;40(7):985–91. [DOI] [PubMed] [Google Scholar]
- 13. Khan DA, Solensky R. Drug allergy. J Allergy Clin Immunol. 2010;125(2):S126–S137.e121. [DOI] [PubMed] [Google Scholar]
- 14. Akdis CA. Therapies for allergic inflammation: refining strategies to induce tolerance. Nat Med. 2012;18(5):736. [DOI] [PubMed] [Google Scholar]
- 15. Lee B, Yu H, Kang E‐S, Lee M, Lee J. Human leukocyte antigen genotypes and trial of desensitization in patients with oxcarbazepine‐induced skin rash: a pilot study. Pediatr Neurol. 2014;51(2):207–14. [DOI] [PubMed] [Google Scholar]
- 16. Smith H, Newton R. Adverse reactions to carbamazepine managed by desensitisation. Lancet. 1985;325(8431):753. [DOI] [PubMed] [Google Scholar]
- 17. Eames P. Adverse reactions to carbamazepine managed by desensitisation. Lancet. 1989;333(8636):509–10. [DOI] [PubMed] [Google Scholar]
- 18. Toker O, Tal Y, Horev L, Shmoeli D, Gilboa T. Valproic acid hypersensitivity and desensitization. Dev Med Child Neurol. 2015;57(11):1076–8. [DOI] [PubMed] [Google Scholar]
- 19. Okumura A, Tsuge I, Kubota T, Kurahashi H, Natsume J, Negoro T, et al. Phenytoin desensitization monitored by antigen specific T cell response using carboxyfluorescein succinimidyl ester dilution assay. Eur J Paediatr Neurol. 2007;11(6):385–8. [DOI] [PubMed] [Google Scholar]
- 20. Itomi S, Okumura A, Ikuta T, Negoro T, Watanabe K. Phenytoin desensitization in a child with symptomatic localization‐related epilepsy. Brain Develop. 2007;29(2):121–3. [DOI] [PubMed] [Google Scholar]
- 21. Butte MJ, Dodson B, Dioun A. Pentobarbital desensitization in a 3‐month‐old child. Allergy Asthma Proc. 2004;25(4):225–7. [PubMed] [Google Scholar]
- 22. Aydogan M, Yologlu N, Gacar G, Uyan Z, Eser I, Karaoz E. Successful rapid rituximab desensitization in an adolescent patient with nephrotic syndrome: Increase in number of Treg cells after desensitization. J Allergy Clin Immunol. 2013;132(2):478–80. [DOI] [PubMed] [Google Scholar]
- 23. Castells MC, Tennant NM, Sloane DE, Hsu IF, Barrett NA, Hong DI, et al. Hypersensitivity reactions to chemotherapy: outcomes and safety of rapid desensitization in 413 cases. J Allergy Clin Immunol. 2008;122(3):574–80. [DOI] [PubMed] [Google Scholar]
- 24. Jung J‐W, Kim D‐K, Park H‐W, Oh K‐H, Joo K‐W, Kim Y‐S, et al. An effective strategy to prevent allopurinol‐induced hypersensitivity by HLA typing. Genet Med. 2015;17(10):807. [DOI] [PubMed] [Google Scholar]
- 25. Johannessen SI, Battino D, Berry DJ, Bialer M, Krämer G, Tomson T, et al. Therapeutic drug monitoring of the newer antiepileptic drugs. Ther Drug Monit. 2003;25(3):347–63. [DOI] [PubMed] [Google Scholar]
- 26. Tak H‐J, Ahn J‐H, Kim K‐W, Kim Y, Choi S‐W, Lee K‐Y, et al. Rash in psychiatric and nonpsychiatric adolescent patients receiving lamotrigine in Korea: a retrospective cohort study. Psychiatry Investig. 2012;9(2):174–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Terao T, Ishida A, Kimura T, Yoshida M, Hara T. Assessment of safety and efficacy of lamotrigine over the course of 1‐year observation in Japanese patients with bipolar disorder: post‐marketing surveillance study report. Neuropsychiatr Dis Treat. 2017;13:1441–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Hirsch LJ, Weintraub DB, Buchsbaum R, Spencer HT, Straka T, Hager M, et al. Predictors of lamotrigine‐associated rash. Epilepsia. 2006;47(2):318–22. [DOI] [PubMed] [Google Scholar]
- 29. Castells M. Desensitization for drug allergy. Curr Opin Allergy Clin Immunol. 2006;6(6):476–81. [DOI] [PubMed] [Google Scholar]
- 30. Legendre DP, Muzny CA, Marshall GD, Swiatlo E. Antibiotic hypersensitivity reactions and approaches to desensitization. Clin Infect Dis. 2013;58(8):1140–8. [DOI] [PubMed] [Google Scholar]
- 31. Mani R, Monteleone C, Schalock PC, Truong T, Zhang XB, Wagner ML. Rashes and other hypersensitivity reactions associated with antiepileptic drugs: a review of current literature. Seizure. 2019;71:270–8. [DOI] [PubMed] [Google Scholar]
- 32. Liu A, Fanning L, Chong H, Fernandez J, Sloane D, Sancho‐Serra M, et al. Desensitization regimens for drug allergy: state of the art in the 21st century. Clin Exp Allergy. 2011;41(12):1679–89. [DOI] [PubMed] [Google Scholar]
- 33. Scherer K, Brockow K, Aberer W, Gooi JHC, Demoly P, Romano A, et al. Desensitization in delayed drug hypersensitivity reactions – an EAACI position paper of the Drug Allergy Interest Group. Allergy. 2013;68(7):844–52. [DOI] [PubMed] [Google Scholar]


