Abstract
The Inflammatory Bowel Diseases (IBD), Ulcerative Colitis (UC) and Crohn’s Disease (CD) are characterised by chronic non-resolving gut mucosal inflammation involving innate and adaptive immune responses. Neutrophils, usually regarded as first responders in inflammation, are a key presence in the gut mucosal inflammatory milieu in IBD. Here, we review the role of neutrophil extracellular trap (NET) formation as a potential effector disease mechanism. NETs are extracellular webs of chromatin, microbicidal proteins and oxidative enzymes that are released by neutrophils to contain pathogens. NETs contribute to the pathogenesis of several immune-mediated diseases such as systemic lupus erythematosus and rheumatoid arthritis; and recently, as a major tissue damaging process involved in the host response to severe acute respiratory syndrome coronavirus 2 infection. NETs are pertinent as a defence mechanism at the gut mucosal interphase exposed to high levels of bacteria, viruses and fungi. On the other hand, NETs can also potentiate and perpetuate gut inflammation. In this review, we discuss the broad protective vs. pathogenic roles of NETs, explanatory factors that could lead to an increase in NET formation in IBD and how NETs may contribute to gut inflammation and IBD-related complications. Finally, we summarise therapeutic opportunities to target NETs in IBD.
Key Words: IBD, UC, CD, Neutrophils, Inflammation, Immunology, Neutrophil Extracellular Traps
Abbreviations used in this paper: AAV, antineutrophil cytoplasmic antibody-associated vasculitis; ANCA, antineutrophil cytoplasmic antibody; CD, Crohn’s disease; DDIT4, DNA damage inducible transcript 4; IBD, inflammatory bowel disease; IL, interleukin; LPS, lipopolysaccharide; MMP, matrix metalloprotease; MPO, myeloperoxidase; mtDNA, mitochondrial DNA; mtNET, mitochondrial neutrophil extracellular trap; NE, neutrophil elastase; NET, neutrophil extracellular trap; PAD4, peptidylarginine deiminase 4; PMA, phorbol-12-myrisate-13-acetate; PR3, proteinase 3; RA, rheumatoid arthritis; ROS, reactive oxygen species; SLE, systemic lupus erythematosus; TLR, Toll-like receptor; TNF, tumor necrosis factor; UC, ulcerative colitis
Summary.
Neutrophils play a key role in gut inflammation. Our review focuses on a distinct effector mechanism, the ability of neutrophils to form extracellular traps as a potential pathogenic factor and a therapeutic target for translation in inflammatory bowel disease.
Ulcerative colitis (UC) and Crohn’s disease (CD) are 2 clinical entities that define the inflammatory bowel diseases (IBD). Both are chronic immune-mediated conditions with rapidly increasing global incidence.1 Although displaying different clinical features, they share a nonresolving pattern of gut mucosal inflammation. Current therapeutic approaches are focused on inhibiting the aberrant gut inflammation and immune response. For example, blocking inflammatory cytokines such as tumor necrosis factor alpha (TNF-α) and interleukin (IL)-23, the migration of leukocytes with anti-α4β7 integrin therapies, T cell responses with thiopurines, and downregulating general inflammation with glucocorticoids. Notwithstanding recent therapeutic advances in IBD, primary treatment failure is common, and complete mucosal healing is achieved in 50% of patients with moderate-to-severe IBD. Hence, a creative appraisal encompassing distinct mechanistic pathways is necessary in the design of future treatment strategies beyond mitigating downstream inflammatory responses.2
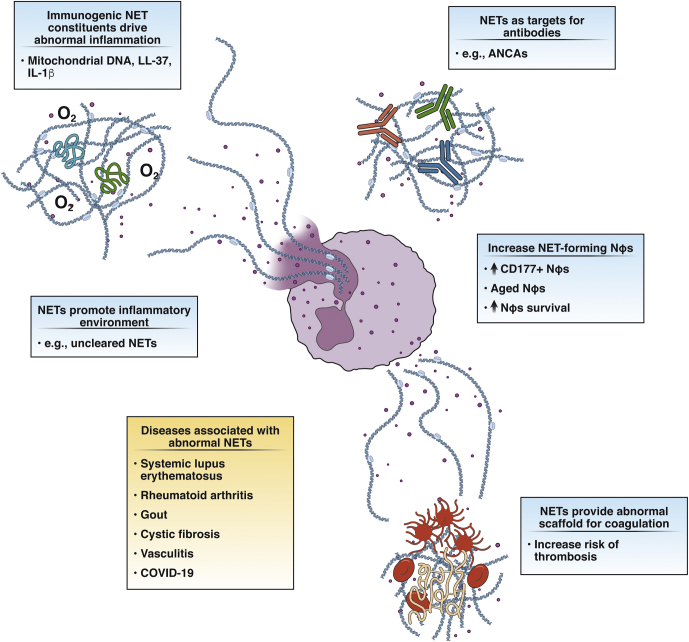
Although prominently featured in the inflamed IBD mucosa, the translational potential of targeting the damaging effects of neutrophils is relatively understudied. A notable inflammatory process driven by neutrophils is mediated via their ability to form neutrophil extracellular traps (NETs). NETs comprise of a scaffold of DNA laced with histones and cytotoxic neutrophil-derived proteins and are released by neutrophils during infection and inflammation to contain invading microbes as a protective response.3, 4, 5 NET components are indiscriminately cytotoxic and proinflammatory and thus can play an active role in a wide range of pathologies involved in autoimmunity, thrombosis, and cancer (Figure 1).6 Here, we focus on the role of the neutrophils and how their ability to form NETs presents an area for clinical translation in IBD.
Figure 1.
Pathogenicprocesses of NETs in human diseases. Nϕs, neutrophils.
The Role of Neutrophils in IBD
Neutrophils are the most abundant immune cell, constituting approximately 70% of leukocytes in human blood and are regarded as first responders of the innate immune system. Neutrophils are best known for their rapid recruitment to sites of infection or tissue damage to contain pathogens.7 Neutrophils undergo apoptosis and efferocytosis upon completion of their tasks to allow the resolution of inflammation, repair, and a return to normal tissue function.8, 9, 10 Persistent activation and overexuberant recruitment of neutrophils are common features in many inflammatory diseases. Neutrophils produce a wide variety of chemokines, cytokines, and leukotrienes, allowing them to recruit and activate a broad spectrum of immune cells.11,12 Neutrophils also directly cause tissue damage by releasing proteases such as matrix metalloproteases and neutrophil elastase (NE),13,14 as well as from oxidative burst which directly disrupts cell membranes.15
Neutrophils play an important role in IBD gut inflammation. They produce high levels of reactive oxygen species (ROS) that cause epithelial barrier damage and can activate redox-sensitive inflammatory pathways.16 They also released a host of proteases, proinflammatory cytokines and mediators such as IL-8, TNF-α, and leukotriene B4 that damage the epithelial barrier and recruit monocytes and more neutrophils to the gut.17,18 Neutrophil infiltration correlates with disease activity in IBD19, 20, 21, 22, 23 and is a widely used and reliable component of UC disease scoring systems.24 Calprotectin (s100A8/9), the most widely used biomarker in IBD, constitutes up to 60% of neutrophil cytosolic proteins.25,26 In addition, many more neutrophil-derived IBD biomarkers have been proposed,27, 28, 29 and there are several examples of neutrophil-targeted therapies. Although a neutrophil response is strongly featured in UC,30 in CD, neutrophil function may be impaired with reduced migration, superoxide production, and phagocytic functions.31,32 In contrast to UC, reduced neutrophil accumulation and delayed bacterial clearance is observed at sites of injury within the gut and systemically in CD.33 This suggests that the development of chronic inflammation and granuloma formation is a consequence of an impaired innate immune response in CD.33,34 In this regard, similar features are seen in chronic granulomatous disease and glycogen storage disease that are characterized by deficient neutrophil responses.32,35
NET Formation
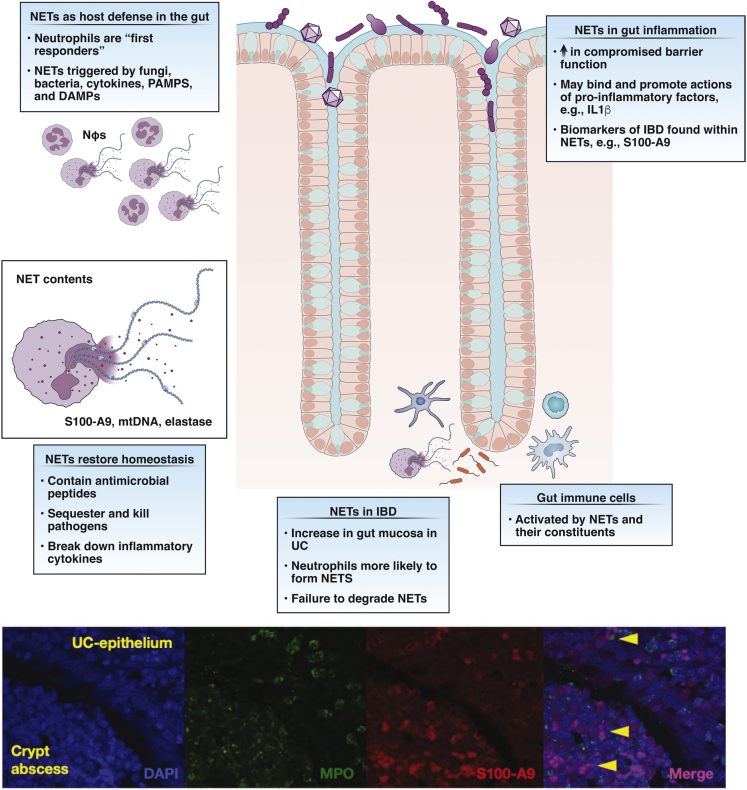
Brinkmann et al3 first discovered NETs upon stimulating neutrophils with IL-8, phorbol-12-myrisate-13-acetate (PMA), or lipopolysaccharide (LPS). NETs prevent the spread of a range of pathogens5 by trapping them in an environment of microbicidal components and prevent fungal growth as has been demonstrated with Candida albicans.4 NETs contain granule proteins, histones, cytoplasmic proteins, and notably, calprotectin, which is important in antifungal defence.4 Extracellular traps are an effective and highly conserved defence mechanism.36 They have been reported in teleosts,37 chickens,38 crabs, and mussels,39 and in plants as part of the root tip resistance to fungal infection,40 and many pathogens have evolved mechanisms to repulse41 or degrade them.42,43 Given the proximity of the gut mucosa to the microbiota, the role of NETs is of particular importance in IBD as an integral component of the host defense (Figure 2).
Figure 2.
NETs in the gut and IBD. Inflamed UC gut mucosa and the presence of NETs (colocalization of MPO and s100a9 in crypt abscesses and subepithelium [arrowheads]). s100a9 is part of the calprotectin molecule. DAMPs, damage-associated molecular patterns; NΦs, neutrophils; PAMPs, pathogen-associated molecular patterns.
Although interest in NETs grows, a refined consensus on NET mechanisms and classification is lacking.44,45 From a recent expert review,44 a few aspects are noteworthy; first NETosis does not cover all forms of NET release and the term NET formation is preferred. Second, there are many in vivo NET stimulants including bacteria, fungal hyphae, cytokines, immune complexes, and activated platelets. Third, there are 2 broad mechanistic pathways for NET formation: late lytic, occurring 2–4 hours poststimulus, which is most commonly induced by PMA and results in neutrophil death, and early nonlytic, which occurs 5–60 minutes poststimulus induced by, for example, Toll-like receptors (TLRs) responding to pathogen associated molecular patterns and not resulting in neutrophil death. However, the mechanisms underlying NET formation differ considerably within these general pathways, depending on stimulant.46,47 For instance, PMA-induced NET formation requires protein kinase C activation, calcium flux, ROS, myeloperoxidase (MPO) and NE but bacteria-derived ionophore-induced NET formation can work independently of protein kinase C activation, ROS, MPO, or NE.46 Because NETs with a similar makeup can be induced by very different stimuli, pinpointing what triggers increased NET formation in a pathogenic manner is challenging in gut inflammation and IBD. For instance, disparate factors such as C albicans and PMA can both stimulate the release of NETs containing calprotectin, a known biomarker in IBD.4 However, there may be other ways to pinpoint stimulants. Bacterial factors (eg, N-formylated peptides) may induce the release of different granule types and measuring the levels of primary vs secondary granule proteins such as the ratio of myeloperoxidase to lactoferrin in IBD, may provide insights into the types of neutrophil stimulants in general and therefore NET stimulants.48
NETS as a Pathological Factor in Human Disease
As with many host protective mechanisms, the deployment of NETs can be a double-edged sword.6,49 NETs can promote or prolong both innate and adaptive immune responses in a wide variety of diseases (Figure 1). In cystic fibrosis, NETs directly induce IL-8 and TNF-α production by monocyte-derived macrophages,50 and in atherosclerosis, NETs augment IL-1β and IL-6 production by monocytes stimulated with cholesterol crystals.51 In rheumatoid arthritis (RA), NETs provide a scaffold for autoantibodies against citrullinated histones,52 and in systemic lupus erythematosus (SLE), NETs containing LL-37 and high-mobility group box 1 can trigger plasmacytoid dendritic cell production of interferon alfa.53 NETs can also facilitate thrombosis in vasculitis by providing a framework for platelet and tissue factor adhesion.54 NETs augment cancer progression by trapping and spreading cancerous cells and polarizing neutrophils toward an immunosuppressive N2-like population.55,56 Finally, NETs contribute to sustained proinflammatory cytokine production, mucous secretion, and thrombosis in COVID-19 (coronavirus disease 2019).57,58
Box 1. NETs in IBD: Experimental Considerations.
To achieve better clarity in future work, several experimental considerations are noteworthy.
-
1.
Multiple characterization of NET components beyond the use of single NET markers such as PAD4 are needed. Ideal methodology would combine the use of sandwich enzyme-linked immunosorbent assays for blood work, targeting DNA-MPO/citH3/NE complexes,59 colocalization studies in tissue using immunohistochemistry,60 intravital microscopy, and live cell imaging.61,62
-
2.
For NET formation studies, neutrophils must be isolated with an appreciation of the ability of calcium, magnesium, and chelators to alter NET formation capacity.44,63
-
3.
As for stimulants, PMA should ideally only be used as a positive control44 and more physiologically relevant stimuli such as patient sera,64 cultured medium from inflamed tissue cultures,65 and combinations of IBD relevant cytokines66 should be used.
-
4.
Additionally, previous and current treatment regimens within patient cohorts should be stated in detail because several widely used IBD treatments such as infliximab66,67 and mesalamine68 have been shown to directly inhibit NET formation.
NETS in IBD
Increased NET Formation in IBD
To date, 8 studies (Table 1) have demonstrated an increased presence of NETs in the inflamed gut mucosa, stool, or blood in IBD, 4 of which stipulate that NET abundance is positively correlated with active disease.64,66,69,70 Liquid chromatography-mass spectrometry–based IBD proteomics studies reveal an increase in key NET proteins such as myeloperoxidase (MPO) and NE, both of which are highly specific to neutrophils and involved in chromatin decondensation during NET formation,71 as well as increased calprotectin and cathepsin G, both of which have been found in NETs4 in both intestinal biopsies72 and fecal samples.73 Increased levels of NET-associated proteins in IBD have also been demonstrated by immunofluorescence, immunohistochemistry, or Western blot in intestinal biopsies60,65,66,69 as well as in the colonic mucosa of experimental colitis in mice.70 Using Western blot, these increased NET-specific proteins included NE, MPO, and citrullinated histone H3, another widely used NET biomarker,66,74 and using immunofluorescence, NETs have been found as DNA complexed with NE, MPO, and histones.60,65,66,69 Additionally, increased NET components have been found in the circulation of IBD patients69,70 by capture enzyme-linked immunosorbent assay that measured DNA bound to MPO as a surrogate marker of a NET. Although these findings are important, colocalization or correlation of DNA with NET-implicated proteins is not outright evidence of NET formation because DNA of any source can bind proteins released from neutrophils through several processes including apoptosis and degranulation, and more rigorous qualification and quantification is suggested in Box 1.
Table 1.
A Summary of NET Studies in IBD
| Reference | Methods | Key findings |
|---|---|---|
| Bennike et al72 | Liquid chromatography-mass spectrometry (UC = 10 vs controls = 10). |
|
| Lehmann et al73 | Liquid chromatography-mass spectrometry (UC = 14, CD = 11, other = 29, controls = 17) |
|
| Dinallo et al66 | Immunohistochemistry, immunofluorescence, Western blot; in vitro NET induction, DSS-induced colitis (UC = 9, CD = 9, controls = 12). |
|
| Li et al69 | Immunofluorescence, ELISA, in vitro NET induction; DSS-induced colitis (UC = 24, CD = 24, controls = 10). |
|
| Angelidou et al65 | Immunofluorescence, Western blot; ELISA, in vitro NET induction (UC = 23, CD = 11, other = 15, controls = 25) |
|
| Gottlieb et al60 | Immunofluorescence (UC = 6, CD = 6, control = 2) |
|
| Cao et al70 | Immunofluorescence, ELISA, in vitro NET induction, DSS colitis (UC/CD = 51). |
|
| He et al64 | In vitro NET induction (UC = 28, CD = 23, controls = 12) |
|
ANCA, antineutrophil cytoplasmic antibody; CD, Crohn’s disease; DSS, dextran sulfate sodium; ELISA, enzyme-linked immunosorbent assay; IBD, inflammatory bowel disease; MPO, myeloperoxidase; NET, neutrophil extracellular trap; PAD4, peptidylarginine deiminase 4; PR3, proteinase 3; UC, ulcerative colitis.
Is increased NET formation a shared phenomenon in UC and CD? Several studies have reported this in both entities,60,64,69,70,73 while others found no evidence in CD.65,66 Different experimental methods and patient cohorts may explain some of the discrepancies. For instance, Dinallo et al66 ruled out an increase in NETs in CD intestinal biopsies based on the absence of increased expression of peptidylarginine deiminase 4 (PAD4), a nuclear citrullinating enzyme classically believed to be essential for NET formation. However, it has been proven that PAD4 is not required for all forms of NET release, as shown with C albicans and group B Streptococcus–mediated NET formation.44,46 However, as UC is typically associated with higher neutrophil recruitment,30,33 if true, the finding of increased NETs in UC relative to CD is perhaps not unexpected.
Increased NET abundance is also not unique or specific to IBD and is likely present in any situation in which there is significant neutrophil involvement and gut microbial exposure. For instance, in necrotizing enterocolitis, in which gut barrier defense is markedly compromised by inflammation, high levels of NETs can be found in gut tissue.75 However, higher levels of proteins associated with NETs including MPO, NE, and calprotectin can differentiate individuals with IBD from those with noninflammatory conditions such as irritable bowel syndrome in fecal metaproteomic studies,73 suggesting that increased NET production in the IBD is related to gut inflammation.
Are Neutrophils in IBD More Likely to Form NETs?
Are neutrophils in IBD more prone to forming NETs? Several angles are noteworthy. First, the local biological microenvironment is crucial. For instance, in diabetes, a hyperglycemic environment primes NET formation by upregulating PAD4,76 and in SLE, circulating microparticles derived from apoptotic cells can increase the potential for NET formation.77 Serum from patients with UC and CD; and media from ex vivo culture of inflamed UC mucosa can stimulate higher spontaneous NET formation.64,65 This suggests the involvement of inflammatory mediators in the circulation and from the mucosa, but triggers by transmigrated gut microbial components such as bacterial DNA78, 79, 80 are also likely stimuli.
Second, are there intrinsically distinct neutrophil phenotypes in IBD that are more prone to NET formation? Disease-specific neutrophil subsets such as type I interferon hyperresponsive neutrophils in SLE81 or low-density neutrophils, implicated in a variety of diseases82,83 that are considered more susceptible to form NETs, have been described. He et al64 found that neutrophils, irrespective of whether they are obtained from UC, CD, or non-IBD subjects, had similar NET formation capacity when stimulated with IBD sera. Dinallo et al66 demonstrated that in vitro NET formation capacity by active UC neutrophils is similar to healthy controls in response to a variety of stimulants including TNF-α, LPS, and PMA. However, 3 studies provided contrary evidence, stating that in vitro, neutrophils from CD and UC70 or from UC alone65,69 have a primed or intrinsically increased NET formation capacity, reported as spontaneous65,70 or PMA induced.69
Of interest, NET-prone CD177+ neutrophils are found in increased proportions in the blood and inflamed intestinal mucosa of both UC and CD patients.22,84 CD177 is a glycoprotein that is exclusively expressed on neutrophils, neutrophilic myelocytes, and metamyelocytes. CD177 is involved in neutrophil transmigration and is upregulated upon acute bacterial infection.85 CD177+ neutrophils have a higher expression of granule protein genes86 and are an activated or primed subset in several diseases including antineutrophil cytoplasmic antibody (ANCA)–associated vasculitis (AAV), SLE, and asthma.87,88 In IBD, CD177+ neutrophils have a shifted gene expression profile toward microbial defense and release more ROS, MPO, and calprotectin, and produce more NETs than CD177– neutrophils.22 Notably CD177+ neutrophils in inflamed mucosa of CD and UC patients positively correlate with Crohn’s Disease Activity Index and UC Mayo Score.22
Third, are there increased numbers of aged neutrophils in IBD that are more likely to form NETs? Neutrophil lifespan can be prolonged by growth factors, cytokines, and microbial products during infection and inflammation.89,90 Delayed apoptosis leads to the persistence of autoantigens in RA and AAV,8 enhanced risk of tissue damage in acute coronary syndromes,91 and enhanced NET formation capacity in cystic fibrosis.50 In IBD, spontaneous neutrophil apoptosis is delayed by IL-8 and granulocyte colony-stimulating factor.92,93 With relevance to IBD, it has been reported that a systemic, aged, proinflammatory neutrophil population with higher NET formation capacity, defined as a CD62Llo CXCR4hi subset, can be driven by the gut microbiota via TLRs and myeloid differentiation factor 88–mediated pathways in mice.94 This population is diminished upon depletion of the microbiota with antibiotics.94
Proinflammatory actions of NETs in IBD: Abundance vs Composition
The composition of NETs and their specific effects is a further factor to consider above abundance alone. For instance, in psoriasis, NETs containing proinflammatory LL-37-DNA complexes activate plasmacytoid dendritic cells, leading to increased interferon alfa production.49 In RA, autoantibodies against NET components such as citrullinated vimentin are found in the circulation leading to augmentation of IL-6 and IL-8 inflammatory responses52 and in SLE, NETs are embedded with highly proinflammatory oxidized mitochondrial DNA (mtDNA), which stimulates type I interferon signaling through the DNA sensor stimulator of interferon genes.95
In 2018, Angelidou et al65 described bioactive IL-1β-decorated NETs in UC but not in CD. These IL-1β-containing NETs formed through an autophagy-dependent mechanism that facilitates the extrusion of NET contents.44 Here, they showed that IL-1β–decorated NET production was linked to the expression of DNA damage inducible transcript 4 (DDIT4) in UC.65 DDIT4 is an important, ubiquitously expressed stress-response mammalian target of rapamycin inhibitor linking cellular stress to autophagy-mediated NET-associated IL-1β responses in familial Mediterranean fever.96 DDIT4 expression was higher in UC neutrophils and in control neutrophils stimulated with UC colon tissue culture media.65 It was proposed that this DDIT4/NET/IL-1β pathway may be specific to UC (not CD) as a form of IL-1β autoinflammatory disease. Angelidou et al96 previously described that in familial Mediterranean fever, neutrophils undergo autophagy-mediated NET formation via the DDIT4 pathway through stress mediators such as epinephrine. Studying the effects of similar stress mediators on NET formation may also be relevant in UC.
ANCAs may play a role in NET-mediated IBD pathology. ANCAs drive the development of AAV in which they target proteinase 3 (PR3) or MPO97 and initiate neutrophil-rich necrotizing inflammation, causing organ damage.98 In UC, the perinuclear type, pANCA, is found in up to 80% of UC patients,99,100 with a distinct subset of UC-specific ANCAs, DNase I–sensitive ANCAs, known for targeting only nuclear-protein complexes.99,101 This UC-derived DNase I–sensitive ANCA can bind to antigens present on NETs.102 In 2016, He et al64 showed that NET formation is amplified when neutrophils were incubated with ANCA-IgG isolated from active PR3-ANCA-positive IBD patients. In addition, Li et al69 proposed a further mechanism, in which ANCAs decreased the breakdown of NETs, by attenuating DNase I activity particularly during active IBD. Finally, ANCAs in IBD might activate neutrophils through Fc receptor stimulation when binding granule components such as PR3 or MPO, which have been translocated to their outer membrane during activation, as described with AAV.101,103
Are There Proinflammatory Mitochondrial NETs in IBD?
Another area of significant interest in NET-driven pathology is the existence of NETs embedded with mitochondrial DNA (mtNETs). This is relevant as an association of increased mtDNA levels with active UC and CD have been reported.104 mtNET formation has been described as early, nonlytic, and ROS dependent and was originally demonstrated with neutrophils primed by granulocyte-macrophage colony-stimulating factor followed by TLR4 or complement receptor activation.105 Here, NETs were found to contain mitochondrial DNA and the granule proteins NE and MPO but, interestingly, not genomic DNA. Yousefi et al55 recently proposed mtNETs are an active, proinflammatory, antimicrobial tool that utilize mtDNA fragments no longer needed within the cell in combination with granule proteins, suggesting that they are true nonlytic NETs. Although the mechanisms remain unknown, mtNETs are now supported by many as an alternative form of NET release,5 although they should be carefully differentiated from incomplete mitophagy, which can lead to the release of oxidized nucleoids containing mitochondrial components following cell damage.106 Their similarities with bacteria point to mitochondrial components within mtNETs as potent inflammatory mediators107,108 and oxidized mtDNA and mtNETs have now been implicated in a range of diseases, including SLE and chronic granulomatous disease95 and in sterile injury, surgery,109 and cancer.110
NETs and Thrombotic Tendencies in IBD
One potential implication of increased circulating NETs in IBD is an increased thrombotic risk. Both UC and CD patients have an increased (3-fold) risk of thromboembolic events compared with the general population.111 Although abnormalities in coagulation and fibrinolytic systems such as elevated circulating fibrinogen, prothrombin, and microparticles have been found, these abnormalities are insufficient to explain the increased thromboembolic risk in IBD.111 Recently, 3 separate studies have linked NETs to increased thrombotic tendency in IBD.64,69,70 In 2016, He et al64 found that NETs contributed to increased coagulation, which could be counteracted by DNase I. Here, they highlighted that NET NE can inactivate tissue factor inhibitor and that NETs provide a scaffold for platelet and erythrocyte adhesion. The same group went on to demonstrate that incubating normal platelets with NETs from active IBD patients enhanced procoagulant activity by 32% and the ability to support fibrin formation by 42%.70 Recently, they reported the treatment of a dextran sulfate sodium–induced mouse colitis model with DNase I led to lower disease activity and a decrease in prothrombotic effects.69 Intriguingly, they also found ANCA-IgG to have a role, inducing NET formation as well as microparticle shedding by cultured endothelial cells, which accelerated coagulation.8 The effect of NETs on prothrombotic tendencies in IBD is a novel area and may have similarities to other diseases such as vasculitis.54,112
Beneficial Roles of NETs in IBD
NETs have been shown to play a beneficial role in downregulating inflammation in several conditions. In RA, NETs can downregulate IL-6 and upregulate IL-10 secretion in LPS-activated macrophages.113 In gout, NETs contribute to the resolution of inflammation directly by degrading cytokines and chemokines via serine proteases and when NET formation is impaired, the propensity of monosodium urate crystals, the trigger for gout, to activate neutrophils is amplified.114 Proteases within NETs have been shown to be efficient regulators of cytokine activity in vitro and in vivo and will also play a role in regulating a large number of cytokines in IBD.115 Finally, circulating NETs may have a role in clearing damage-associated molecular patterns such as transmigrated bacterial components,78, 79, 80 a mechanism proven in murine sepsis.62 Thus, some care must be taken in targeting NETs as a therapy in IBD.
Conclusion
The knowledge of NET biology has allowed new insights into the inflammatory processes of many diseases. Although NET formation is a relatively unexplored area in IBD, it presents an excellent opportunity to understand the potential contribution of a major immune cell, the neutrophil, in the pathogenic and nonresolving gut inflammation in IBD. Importantly, the development of NET-targeted therapies in IBD can draw on lessons from other diseases (summarized in Table 2). Targeting NETs may form a novel treatment approach to achieving complete mucosal healing in IBD.
Table 2.
Summary of NET-targeted Therapies in IBD and Other Diseases
| Targeted NET component | Inhibitors | IBD Studies | Non-IBD Studies |
|---|---|---|---|
| Peptidylarginine deiminase, a nuclear citrullinating enzyme essential for some forms of NET formation | Chloramidine, BB-Cl-amidine, neonatal inhibitory factor, streptonigrin | Chloramidine—Reduced clinical signs and symptoms in DSS-induced colitis.116,117 Streptonigrin—Reduced colonic inflammation, weight loss, and diarrhea; improved histological scoring in DSS-induced colitis.11 |
Murine models of lupus and MPO-ANCA–associated vasculitis.118, 119, 120 |
| Neutrophil elastase—involved in chromatin decondensation during NET formation | Prolastin, elaspol, range of low-molecular-weight HNE inhibitors | Elaspol—Reduced weight loss and histological score in DSS-induced colitis, reduced IL-17–based inflammation121,122 | Non-IBD—various including (cardio)pulmonary inflammatory diseases, RA, and cancer123 |
| NET DNA | Recombinant human DNase, DNase I | DNase I—Reduced weight loss; lower disease activity index; lower histological score; reduced thrombotic tendencies; reduced IL-1β, IL-6, and TNF-α69,70 | Non-IBD—good safety profile in cystic fibrosis, moderately efficacious124 |
| IL-1β–decorated NETs | Anakinra, rilonacept, canakinumab | Anakinra (ongoing)—IASO phase II trial for ASUC. Question: Does antagonism of IL-1 signaling in addition to intravenous corticosteroid treatment improve outcomes in ASUC patients?125 | Various including RA, FMF, and hyperimmunoglobulinemia D syndrome126,127 |
| Other approaches | - Antibody-mediated targeting of NETs for macrophage degradation.128 Not only breaks down DNA but also proinflammatory/destructive NET proteins. - Cross-linking of NET-inhibitory receptors such as signal inhibitory receptor on leukocytes-1.129 Inhibits NETs but preserves intracellular bacterial killing. |
||
ANCA, antineutrophil cytoplasmic antibody; ASUC, acute severe ulcerative colitis; DSS, dextran sulfate sodium; FMF, familial Mediterranean fever; IASO, Interleukin 1 blockade in Acute Severe Colitis; IBD, inflammatory bowel disease; IL, interleukin; MPO, myeloperoxidase; NET, neutrophil extracellular trap; RA, rheumatoid arthritis; TNF-α, tumor necrosis factor alpha.
Footnotes
Conflicts of interest The authors disclose no conflicts.
Funding Broc Drury and Gwo-tzer Ho are funded by the Leona M. and Harry B. Helmsley Charitable Trust; Gareth Hardisty and Robert D. Gray are funded by an NRS Senior Clinical Fellowship (SCAF/16/02).
References
- 1.Ng S.C., Shi H.Y., Hamidi N., Underwood F.E., Tang W., Benchimol E.I., Panaccione R., Ghosh S., Wu J.C.Y., Chan F.K.L., Sung J.J.Y., Kaplan G.G. Worldwide incidence and prevalence of inflammatory bowel disease in the 21st century: a systematic review of population-based studies. Lancet. 2018;390:2769–2778. doi: 10.1016/S0140-6736(17)32448-0. [DOI] [PubMed] [Google Scholar]
- 2.Ho G.T., Cartwright J.A., Thompson E.J., Bain C.C., Rossi A.G. Resolution of inflammation and gut repair in IBD: translational steps towards complete mucosal healing. Inflamm Bowel Dis. 2020;26:1131–1143. doi: 10.1093/ibd/izaa045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brinkmann V., Reichard U., Goosmann C., Fauler B., Uhlemann Y., Weiss D.S., Weinrauch Y., Zychlinsky A. Neutrophil extracellular traps kill bacteria. Science. 2004;303:1532–1535. doi: 10.1126/science.1092385. [DOI] [PubMed] [Google Scholar]
- 4.Urban C.F., Ermert D., Schmid M., Abu-Abed U., Goosmann C., Nacken W., Brinkmann V., Jungblut P.R., Zychlinsky A. Neutrophil extracellular traps contain calprotectin, a cytosolic protein complex involved in host defense against Candida albicans. PLoS Pathog. 2009;5 doi: 10.1371/journal.ppat.1000639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Menegazzi R., Decleva E., Dri P. Killing by neutrophil extracellular traps: fact or folklore? Blood. 2012;119:1214–1216. doi: 10.1182/blood-2011-07-364604. [DOI] [PubMed] [Google Scholar]
- 6.Jorch S.K., Kubes P. An emerging role for neutrophil extracellular traps in noninfectious disease. Nat Med. 2017;23:279–287. doi: 10.1038/nm.4294. [DOI] [PubMed] [Google Scholar]
- 7.Ley K., Laudanna C., Cybulsky M.I., Nourshargh S. Getting to the site of inflammation: the leukocyte adhesion cascade updated. Nat Rev Immunol. 2007;7:678–689. doi: 10.1038/nri2156. [DOI] [PubMed] [Google Scholar]
- 8.McCracken J.M., Allen L.A. Regulation of human neutrophil apoptosis and lifespan in health and disease. J Cell Death. 2014;7:15–23. doi: 10.4137/JCD.S11038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Scannell M., Flanagan M.B., deStefani A., Wynne K.J., Cagney G., Godson C., Maderna P. Annexin-1 and peptide derivatives are released by apoptotic cells and stimulate phagocytosis of apoptotic neutrophils by macrophages. J Immunol. 2007;178:4595–4605. doi: 10.4049/jimmunol.178.7.4595. [DOI] [PubMed] [Google Scholar]
- 10.Watanabe S., Alexander M., Misharin A.V., Budinger G.R.S. The role of macrophages in the resolution of inflammation. J Clin Invest. 2019;129:2619–2628. doi: 10.1172/JCI124615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fujishima S., Hoffman A.R., Vu T., Kim K.J., Zheng H., Daniel D., Kim Y., Wallace E.F., Larrick J.W., Raffin T.A. Regulation of neutrophil interleukin 8 gene expression and protein secretion by LPS, TNF-alpha, and IL-1 beta. J Cell Physiol. 1993;154:478–485. doi: 10.1002/jcp.1041540305. [DOI] [PubMed] [Google Scholar]
- 12.Scapini P., Nardelli B., Nadali G., Calzetti F., Pizzolo G., Montecucco C., Cassatella M.A. G-CSF-stimulated neutrophils are a prominent source of functional BLyS. J Exp Med. 2003;197:297–302. doi: 10.1084/jem.20021343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.O'Reilly P., Jackson P.L., Noerager B., Parker S., Dransfield M., Gaggar A., Blalock J.E. N-alpha-PGP and PGP, potential biomarkers and therapeutic targets for COPD. Respir Res. 2009;10:38. doi: 10.1186/1465-9921-10-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Carter R.I., Ungurs M.J., Mumford R.A., Stockley R.A. Aalpha-Val360: a marker of neutrophil elastase and COPD disease activity. Eur Respir J. 2013;41:31–38. doi: 10.1183/09031936.00197411. [DOI] [PubMed] [Google Scholar]
- 15.Wright H.L., Moots R.J., Edwards S.W. The multifactorial role of neutrophils in rheumatoid arthritis. Nat Rev Rheumatol. 2014;10:593–601. doi: 10.1038/nrrheum.2014.80. [DOI] [PubMed] [Google Scholar]
- 16.Biasi F., Leonarduzzi G., Oteiza P.I., Poli G. Inflammatory bowel disease: mechanisms, redox considerations, and therapeutic targets. Antioxid Redox Signal. 2013;19:1711–1747. doi: 10.1089/ars.2012.4530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wera O., Lancellotti P., Oury C. The dual role of neutrophils in inflammatory bowel diseases. J Clin Med. 2016;5:118. doi: 10.3390/jcm5120118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhou G.X., Liu Z.J. Potential roles of neutrophils in regulating intestinal mucosal inflammation of inflammatory bowel disease. J Dig Dis. 2017;18:495–503. doi: 10.1111/1751-2980.12540. [DOI] [PubMed] [Google Scholar]
- 19.Akpinar M.Y., Ozin Y.O., Kaplan M., Ates I., Kalkan I.H., Kilic Z.M.Y., Yuksel M., Kayacetin E. Platelet-to-lymphocyte ratio and neutrophil-to-lymphocyte ratio predict mucosal disease severity in ulcerative colitis. J Med Biochem. 2018;37:155–162. doi: 10.1515/jomb-2017-0050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Aydemir Y., Pınar A., Hızal G., Demir H., Saltık Temizel İ.N., Özen H., Akbıyık F., Yüce A. Neutrophil volume distribution width as a new marker in detecting inflammatory bowel disease activation. Int J Lab Hematol. 2017;39:51–57. doi: 10.1111/ijlh.12574. [DOI] [PubMed] [Google Scholar]
- 21.Minar P., Jackson K., Tsai Y.T., Sucharew H., Rosen M.J., Denson L.A. Validation of neutrophil CD64 blood biomarkers to detect mucosal inflammation in pediatric Crohn's disease. Inflamm Bowel Dis. 2017;24:198–208. doi: 10.1093/ibd/izx022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhou G., Yu L., Fang L., Yang W., Yu T., Miao Y., Chen M., Wu K., Chen F., Cong Y., Liu Z. CD177+ neutrophils as functionally activated neutrophils negatively regulate IBD. Gut. 2018;67:1052–1063. doi: 10.1136/gutjnl-2016-313535. [DOI] [PubMed] [Google Scholar]
- 23.Therrien A., Chapuy L., Bsat M., Rubio M., Bernard G., Arslanian E., Orlicka K., Weber A., Panzini B.P., Dorais J., Bernard E.J., Soucy G., Bouin M., Sarfati M. Recruitment of activated neutrophils correlates with disease severity in adult Crohn's disease. Clin Exp Immunol. 2019;195:251–264. doi: 10.1111/cei.13226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jairath V., Peyrin-Biroulet L., Zou G., Mosli M., Vande Casteele N., Pai R.K., Valasek M.A., Marchal-Bressenot A., Stitt L.W., Shackelton L.M., Khanna R., D'Haens G.R., Sandborn W.J., Olson A., Feagan B.G., Pai R.K. Responsiveness of histological disease activity indices in ulcerative colitis: a post hoc analysis using data from the TOUCHSTONE randomised controlled trial. Gut. 2019;68:1162–1168. doi: 10.1136/gutjnl-2018-316702. [DOI] [PubMed] [Google Scholar]
- 25.Fukunaga S., Kuwaki K., Mitsuyama K., Takedatsu H., Yoshioka S., Yamasaki H., Yamauchi R., Mori A., Kakuma T., Tsuruta O., Torimura T. Detection of calprotectin in inflammatory bowel disease: Fecal and serum levels and immunohistochemical localization. Int J Mol Med. 2018;41:107–118. doi: 10.3892/ijmm.2017.3244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Valenzuela J.E., Rodenas G.A., Martinez A.S. Use of biomarkers in inflammatory bowel disease. Med Clin (Barc) 2019;152:310–316. doi: 10.1016/j.medcli.2018.10.010. [DOI] [PubMed] [Google Scholar]
- 27.Muthas D., Reznichenko A., Balendran C.A., Bottcher G., Clausen G., Mardh C.K. Neutrophils in ulcerative colitis: a review of selected biomarkers and their potential therapeutic implications. Scand J Gastroenterol. 2016;52:125–135. doi: 10.1080/00365521.2016.1235224. [DOI] [PubMed] [Google Scholar]
- 28.Barry R., Ruano-Gallego D., Radhakrishnan S.T., Lovell S., Yu L., Kotik O., Glegola-Madejska I., Tate E.W., Choudhary J.S., Williams H.R.T., Frankel G. Faecal neutrophil elastase-antiprotease balance reflects colitis severity. Mucosal Immunol. 2020;13:322–333. doi: 10.1038/s41385-019-0235-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jablaoui A., Kriaa A., Mkaouar H., Akermi N., Soussou S., Wysocka M., Woloszyn D., Amouri A., Gargouri A., Maguin E., Lesner A., Rhimi M. Fecal serine protease profiling in inflammatory bowel diseases. Front Cell Infect Microbiol. 2020;10:21. doi: 10.3389/fcimb.2020.00021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wysoczanski R., Kendall A.C., Motwani M., Vega R., Rahman F.Z., McCartney S., Bloom S.L., Nicolaou A., Gilroy D.W., Segal A.W., Marks D.J.B. Ulcerative colitis is characterized by amplified acute inflammation with delayed resolution. bioRxiv. 2019 doi: 10.1101/870139. [DOI] [Google Scholar]
- 31.Hayee B., Rahman F.Z., Tempero J., McCartney S., Bloom S.L., Segal A.W., Smith A.M. The neutrophil respiratory burst and bacterial digestion in Crohn's disease. Dig Dis Sci. 2011;56:1482–1488. doi: 10.1007/s10620-010-1426-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Korzenik J.R., Dieckgraefe B.K. Is Crohn’s disease an immunodeficiency? A hypothesis suggesting possible early events in the pathogenisis of Crohn's disease. Dig Dis Sci. 2000;45:1121–1129. doi: 10.1023/a:1005541700805. [DOI] [PubMed] [Google Scholar]
- 33.Segal A.W. Studies on patients establish Crohn's disease as a manifestation of impaired innate immunity. J Intern Med. 2019;286:373–388. doi: 10.1111/joim.12945. [DOI] [PubMed] [Google Scholar]
- 34.Smith A.M., Sewell G.W., Levine A.P., Chew T.S., Dunne J., O'Shea N.R., Smith P.J., Harrison P.J., Macdonald C.M., Bloom S.L., Segal A.W. Disruption of macrophage pro-inflammatory cytokine release in Crohn's disease is associated with reduced optineurin expression in a subset of patients. Immunology. 2015;144:45–55. doi: 10.1111/imm.12338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Marks D., Miyagi K., Rahman F., Novelli M., Bloom S., Segal A. Inflammatory bowel disease in CGD reproduces the clinicopathological features of Crohn's disease. Am J Gastroenterol. 2009;104:117–124. doi: 10.1038/ajg.2008.72. [DOI] [PubMed] [Google Scholar]
- 36.Neumann A., Brogden G., von Kockritz-Blickwede M. Extracellular traps: an ancient weapon of multiple kingdoms. Biology (Basel) 2020;9:34. doi: 10.3390/biology9020034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Palic D., Andreasen C.B., Ostojic J., Tell R.M., Roth J.A. Zebrafish (Danio rerio) whole kidney assays to measure neutrophil extracellular trap release and degranulation of primary granules. J Immunol Methods. 2007;319:87–97. doi: 10.1016/j.jim.2006.11.003. [DOI] [PubMed] [Google Scholar]
- 38.Chuammitri P., Ostojic J., Andreasen C.B., Redmond S.B., Lamont S.J., Palic D. Chicken heterophil extracellular traps (HETs): Novel defense mechanism of chicken heterophils. Vet Immunol Immunopathol. 2009;129:126–131. doi: 10.1016/j.vetimm.2008.12.013. [DOI] [PubMed] [Google Scholar]
- 39.Robb C.T., Dyrynda E.A., Gray R.D., Rossi A., Smith V.J. Invertebrate extracellular phagocyte traps show that chromatin is an ancient defence weapon. Nat Commun. 2014;5:4627. doi: 10.1038/ncomms5627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wen F., White G.J., VanEtten H.D., Xiong Z., Hawes M.C. Extracellular DNA is required for root tip resistance to fungal infection. Plant Physiol. 2009;151:820–829. doi: 10.1104/pp.109.142067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wartha F., Beiter K., Albiger B., Fernebro J., Zychlinsky A., Normark S., Henriques-Normark B. Capsule and D-alanylated lipoteichoic acids protect Streptococcus pneumoniae against neutrophil extracellular traps. Cell Microbiol. 2007;9:1162–1171. doi: 10.1111/j.1462-5822.2006.00857.x. [DOI] [PubMed] [Google Scholar]
- 42.Buchanan J.T., Simpson A.J., Aziz R.K., Liu G.Y., Kristian S.A., Kotb M., Feramisco J., Nizet V. DNase expression allows the pathogen group A Streptococcus to escape killing in neutrophil extracellular traps. Curr Biol. 2006;16:396–400. doi: 10.1016/j.cub.2005.12.039. [DOI] [PubMed] [Google Scholar]
- 43.Berends E.T., Horswill A.R., Haste N.M., Monestier M., Nizet V., von Kockritz-Blickwede M. Nuclease expression by Staphylococcus aureus facilitates escape from neutrophil extracellular traps. J Innate Immun. 2010;2:576–586. doi: 10.1159/000319909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Boeltz S., Amini P., Anders H.-J., Andrade F., Bilyy R., Chatfield S. To NET or not to NET: current opinions and state of the science regarding the formation of neutrophil extracellular traps. Cell Death Differ. 2019;26:395–408. doi: 10.1038/s41418-018-0261-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Yousefi S., Stojkov D., Germic N., Simon D., Wang X., Benarafa C., Simon H.U. Untangling “NETosis” from NETs. Eur J Immunol. 2019;49:221–227. doi: 10.1002/eji.201747053. [DOI] [PubMed] [Google Scholar]
- 46.Kenny E.F., Herzig A., Kruger R., Muth A., Mondal S., Thompson P.R., Brinkmann V., Bernuth H.V., Zychlinsky A. Diverse stimuli engage different neutrophil extracellular trap pathways. Elife. 2017;6 doi: 10.7554/eLife.24437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hoppenbrouwers T., Autar A.S.A., Sultan A.R., Abraham T.E., van Cappellen W.A., Houtsmuller A.B., van Wamel W.J.B., van Beusekom H.M.M., van Neck J.W., de Maat M.P.M. In vitro induction of NETosis: comprehensive live imaging comparison and systematic review. PLoS One. 2017;12 doi: 10.1371/journal.pone.0176472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Dwarakanath A.D., Finnie I.A., Beesley C.M., O'Dowd G.M., Nash J., Tsai H.H., Parker N., Rhodes J.M. Differential excretion of leucocyte granule components in inflammatory bowel disease: implications for pathogenesis. Clin Sci (Lond) 1997;92:307–313. doi: 10.1042/cs0920307. [DOI] [PubMed] [Google Scholar]
- 49.Delgado-Rizo V., Martinez-Guzman M.A., Iniguez-Gutierrez L., Garcia-Orozco A., Alvarado-Navarro A., Fafutis-Morris M. Neutrophil extracellular traps and its implications in inflammation: an overview. Front Immunol. 2017;8:81. doi: 10.3389/fimmu.2017.00081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Gray R.D., Hardisty G., Regan K.H., Smith M., Robb C.T., Duffin R., Mackellar A., Felton J.M., Paemka L., McCullagh B.N., Lucas C.D., Dorward D.A., McKone E.F., Cooke G., Donnelly S.C., Singh P.K., Stoltz D.A., Haslett C., McCray P.B., Whyte M.K.B., Rossi A.G., Davidson D.J. Delayed neutrophil apoptosis enhances NET formation in cystic fibrosis. Thorax. 2018;73:134–144. doi: 10.1136/thoraxjnl-2017-210134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Warnatsch A., Ioannou M., Wang Q., Papayannopoulos V. Neutrophil extracellular traps license macrophages and Th17 cells for cytokine production in atherosclerosis. Science. 2015;349:316–320. doi: 10.1126/science.aaa8064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Khandpur R., Carmona-Rivera C., Vivekanandan-Giri A., Gizinski A., Yalavarthi S., Knight J.S., Friday S., Li S., Patel R.M., Subramanian V., Thompson P., Chen P., Fox D.A., Pennathur S., Kaplan M.J. NETs are a source of citrullinated autoantigens and stimulate inflammatory responses in rheumatoid arthritis. Sci Transl Med. 2013;5:178ra40. doi: 10.1126/scitranslmed.3005580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Garcia-Romo G.S., Caielli S., Vega B., Connolly J., Allantaz F., Xu Z., Punaro M., Baisch J., Guiducci C., Coffman R.L., Barrat F.J., Banchereau J., Pascual V. Netting neutrophils are major inducers of type I IFN production in pediatric systemic lupus erythematosus. Sci Transl Med. 2011;3 doi: 10.1126/scitranslmed.3001201. 73ra20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Huang Y.M., Wang H., Wang C., Chen M., Zhao M.H. Promotion of hypercoagulability in antineutrophil cytoplasmic antibody-associated vasculitis by C5a-induced tissue factor-expressing microparticles and neutrophil extracellular traps. Arthritis Rheumatol. 2015;67:2780–2790. doi: 10.1002/art.39239. [DOI] [PubMed] [Google Scholar]
- 55.Guglietta S., Chiavelli A., Zagato E., Krieg C., Gandini S., Ravenda P.S., Bazolli B., Lu B., Penna G., Rescigno M. Coagulation induced by C3aR-dependent NETosis drives protumorigenic neutrophils during small intestinal tumorigenesis. Nat Commun. 2016;7:11037. doi: 10.1038/ncomms11037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Cools-Lartigue J., Spicer J., McDonald B., Gowing S., Chow S., Giannias B., Bourdeau F., Kubes P., Ferri L. Neutrophil extracellular traps sequester circulating tumor cells and promote metastasis. J Clin Invest. 2013;123:3446–3458. doi: 10.1172/JCI67484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Barnes B.J., Adrover J.M., Baxter-Stoltzfus A., Borczuk A., Cools-Lartigue J., Crawford J.M., Daßler-Plenker J., Guerci P., Huynh C., Knight J.S., Loda M., Looney M.R., McAllister F., Rayes R., Renaud S., Rousseau S., Salvatore S., Schwartz R.E., Spicer J.D., Yost C.C., Weber A., Zuo Y., Egeblad M. Targeting potential drivers of COVID-19: neutrophil extracellular traps. J Exp Med. 2020;217 doi: 10.1084/jem.20200652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Middleton E.A., He X.Y., Denorme F., Campbell R.A., Ng D., Salvatore S.P., Mostyka M., Baxter-Stoltzfus A., Borczuk A.C., Loda M., Cody M.J., Manne B.K., Portier I., Harris E.S., Petrey A.C., Beswick E.J., Caulin A.F., Iovino A., Abegglen L.M., Weyrich A.S., Rondina M.T., Egeblad M., Schiffman J.D., Yost C.C. Neutrophil extracellular traps contribute to immunothrombosis in COVID-19 acute respiratory distress syndrome. Blood. 2020;136:1169–1179. doi: 10.1182/blood.2020007008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Lachowicz-Scroggins M.E., Dunican E.M., Charbit A.R., Raymond W., Looney M.R., Peters M.C., Gordon E.D., Woodruff P.G., Lefrançais E., Phillips B.R., Mauger D.T., Comhair S.A., Erzurum S.C., Johansson M.W., Jarjour N.N., Coverstone A.M., Castro M., Hastie A.T., Bleecker E.R., Fajt M.L., Wenzel S.E., Israel E., Levy B.D., Fahy J.V. Extracellular DNA, neutrophil extracellular traps, and inflammasome activation in severe asthma. Am J Respir Crit Care Med. 2019;199:1076–1085. doi: 10.1164/rccm.201810-1869OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Gottlieb Y., Elhasid R., Berger-Achituv S., Brazowski E., Yerushalmy-Feler A., Cohen S. Neutrophil extracellular traps in pediatric inflammatory bowel disease. Pathol Int. 2018;68:517–523. doi: 10.1111/pin.12715. [DOI] [PubMed] [Google Scholar]
- 61.Alasmari S.Z. In vivo imaging of neutrophil extracellular traps (NETs): visualization methods and outcomes. Biomed Res Int. 2020;2020:4192745. doi: 10.1155/2020/4192745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.McDonald B., Urrutia R., Yipp B.G., Jenne C.N., Kubes P. Intravascular neutrophil extracellular traps capture bacteria from the bloodstream during sepsis. Cell Host Microbe. 2012;12:324–333. doi: 10.1016/j.chom.2012.06.011. [DOI] [PubMed] [Google Scholar]
- 63.Manfredi A.A., Rovere-Querini P., D'Angelo A., Maugeri N. Low molecular weight heparins prevent the induction of autophagy of activated neutrophils and the formation of neutrophil extracellular traps. Pharmacol Res. 2017;123:146–156. doi: 10.1016/j.phrs.2016.08.008. [DOI] [PubMed] [Google Scholar]
- 64.He Z., Si Y., Jiang T., Ma R., Zhang Y., Cao M. Phosphotidylserine exposure and neutrophil extracellular traps enhance procoagulant activity in patients with inflammatory bowel disease. Thromb Haemost. 2016;115:738–751. doi: 10.1160/TH15-09-0710. [DOI] [PubMed] [Google Scholar]
- 65.Angelidou I., Chrysanthopoulou A., Mitsios A., Arelaki S., Arampatzioglou A., Kambas K., Ritis D., Tsironidou V., Moschos I., Dalla V., Stakos D., Kouklakis G., Mitroulis I., Ritis K., Skendros P. REDD1/autophagy pathway is associated with neutrophil-driven IL-1β inflammatory response in active ulcerative colitis. J Immunol. 2018;200:3950–3961. doi: 10.4049/jimmunol.1701643. [DOI] [PubMed] [Google Scholar]
- 66.Dinallo V., Marafini I., Di Fusco D., Laudisi F., Franze E., Di Grazia A., Figliuzzi M.M., Caprioli F., Stolfi C., Monteleone I., Monteleone G. Neutrophil extracellular traps sustain inflammatory signals in ulcerative colitis. J Crohns Colitis. 2019;13:772–784. doi: 10.1093/ecco-jcc/jjy215. [DOI] [PubMed] [Google Scholar]
- 67.Zhang C., Shu W., Zhou G., Lin J., Chu F., Wu H., Liu Z. Anti-TNF-alpha therapy suppresses proinflammatory activities of mucosal neutrophils in inflammatory bowel disease. Mediators Inflamm. 2018;2018:3021863. doi: 10.1155/2018/3021863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Kirchner T., Hermann E., Moller S., Klinger M., Solbach W., Laskay T., Behnen M. Flavonoids and 5-aminosalicylic acid inhibit the formation of neutrophil extracellular traps. Mediators Inflamm. 2013;2013:710239. doi: 10.1155/2013/710239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Li T., Wang C., Liu Y., Li B., Zhang W., Wang L., Yu M., Zhao X., Du J., Zhang J., Dong Z., Jiang T., Xie R., Ma R., Fang S., Zhou J., Shi J. Neutrophil extracellular traps induce intestinal damage and thrombotic tendency in inflammatory bowel disease. J Crohn's Colitis. 2019;14:240–253. doi: 10.1093/ecco-jcc/jjz132. [DOI] [PubMed] [Google Scholar]
- 70.Cao M., Yu M., Zhang Y., Tong D., Guo L., Wang C., Li T., Yang X., Zhang C., Kou J., Bi Y., Zhou J., Shi J. Neutrophil extracellular traps exacerbate inflammatory responses and thrombotic tendency in both a murine colitis model and patients with inflammatory bowel disease. Blood. 2017;130 994–994. [Google Scholar]
- 71.Papayannopoulos V., Metzler K.D., Hakkim A., Zychlinsky A. Neutrophil elastase and myeloperoxidase regulate the formation of neutrophil extracellular traps. J Cell Biol. 2010;191:677–691. doi: 10.1083/jcb.201006052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Bennike T.B., Carlsen T.G., Ellingsen T., Bonderup O.K., Glerup H., Bogsted M., Christiansen G., Birkelund S., Stensballe A., Andersen V. Neutrophil extracellular traps in ulcerative colitis: a proteome analysis of intestinal biopsies. Inflamm Bowel Dis. 2015;21:2052–2067. doi: 10.1097/MIB.0000000000000460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Lehmann T., Schallert K., Vilchez-Vargas R., Benndorf D., Puttker S., Sydor S., Schulz C., Bechmann L., Canbay A., Heidrich B., Reichl U., Link A., Heyer R. Metaproteomics of fecal samples of Crohn's disease and ulcerative colitis. J Proteomics. 2019;201:93–103. doi: 10.1016/j.jprot.2019.04.009. [DOI] [PubMed] [Google Scholar]
- 74.Mauracher L.M., Posch F., Martinod K., Grilz E., Daullary T., Hell L., Brostjan C., Zielinski C., Ay C., Wagner D.D., Pabinger I., Thaler J. Citrullinated histone H3, a biomarker of neutrophil extracellular trap formation, predicts the risk of venous thromboembolism in cancer patients. J Thromb Haemost. 2018;16:508–518. doi: 10.1111/jth.13951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.MacQueen B.C., Christensen R.D., Yost C.C., Lambert D.K., Baer V.L., Sheffield M.J., Gordon P.V., Cody M.J., Gerday E., Schlaberg R., Lowe J., Shepherd J.G. Elevated fecal calprotectin levels during necrotizing enterocolitis are associated with activated neutrophils extruding neutrophil extracellular traps. J Perinatol. 2016;36:862–869. doi: 10.1038/jp.2016.105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Wong S.L., Demers M., Martinod K., Gallant M., Wang Y., Goldfine A.B. Diabetes primes neutrophils to undergo NETosis, which impairs wound healing. Nature Medicine. 2015;21:815–819. doi: 10.1038/nm.3887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Dieker J., Tel J., Pieterse E., Thielen A., Rother N., Bakker M., Fransen J., Dijkman H.B., Berden J.H., de Vries J.M., Hilbrands L.B., van der Vlag J. Circulating apoptotic microparticles in systemic lupus erythematosus patients drive the activation of dendritic cell subsets and prime neutrophils for NETosis. Arthritis Rheumatol. 2016;68:462–472. doi: 10.1002/art.39417. [DOI] [PubMed] [Google Scholar]
- 78.Gutierrez A., Frances R., Amoros A., Zapater P., Garmendia M., Ndongo M., Cano R., Jover R., Such J., Perez-Mateo M. Cytokine association with bacterial DNA in serum of patients with inflammatory bowel disease. Inflamm Bowel Dis. 2009;15:508–514. doi: 10.1002/ibd.20806. [DOI] [PubMed] [Google Scholar]
- 79.Gutiérrez A., Zapater P., Juanola O., Sempere L., García M., Laveda R., Martínez A., Scharl M., González-Navajas J.M., Such J., Wiest R., Rogler G., Francés R. Gut bacterial DNA translocation is an independent risk factor of flare at short term in patients with Crohn’s disease. American Journal of Gastroenterology. 2016;111:529–540. doi: 10.1038/ajg.2016.8. [DOI] [PubMed] [Google Scholar]
- 80.Vrakas S., Mountzouris K.C., Michalopoulos G., Karamanolis G., Papatheodoridis G., Tzathas C., Gazouli M. Intestinal bacteria composition and translocation of bacteria in inflammatory bowel disease. PLoS One. 2017;12 doi: 10.1371/journal.pone.0170034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Coit P., Yalavarthi S., Ognenovski M., Zhao W., Hasni S., Wren J.D., Kaplan M.J., Sawalha A.H. Epigenome profiling reveals significant DNA demethylation of interferon signature genes in lupus neutrophils. J Autoimmun. 2015;58:59–66. doi: 10.1016/j.jaut.2015.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Hassani M., Hellebrekers P., Chen N., Cv Aalst, Bongers S., Hietbrink F., Koenderman L., Vrisekoop N. On the origin of low-density neutrophils. Journal of Leukocyte Biology. 2020;107:809–818. doi: 10.1002/JLB.5HR0120-459R. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Hardisty G.R., Lanwarne F.L., Minns D., Gillan J.L., Davidson D.J., Findlay E.G., Gray R.D. Ultra-pure isolation of low density neutrophils casts doubt on their exceptionality in health and disease. bioRxiv. 2020 doi: 10.1101/2020.06.17.156588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Song Y., Yang W., Zhou G., Liu Z. CD177+ neutrophils and its correlation with mucosal impairment in patients with inflammatory bowel disease. Chinese J Dig Endosc. 2016;33:178–182. [Google Scholar]
- 85.Stroncek D.F., Shankar R.A., Noren P.A., Herr G.P., Clement L.T. Analysis of the expression of NB1 antigen using two monoclonal antibodies. Transfusion. 1996;36:168–174. doi: 10.1046/j.1537-2995.1996.36296181931.x. [DOI] [PubMed] [Google Scholar]
- 86.Hu N., Mora-Jensen H., Theilgaard-Monch K., Doornbos-van der Meer B., Huitema M.G., Stegeman C.A., Heeringa P., Kallenberg C.G., Westra J. Differential expression of granulopoiesis related genes in neutrophil subsets distinguished by membrane expression of CD177. PLoS One. 2014;9 doi: 10.1371/journal.pone.0099671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Abdgawad M., Gunnarsson L., Bengtsson A.A., Geborek P., Nilsson L., Segelmark M. Elevated neutrophil membrane expression of proteinase 3 is dependent upon CD177 expression. Clin Exp Immunol. 2010;161:89–97. doi: 10.1111/j.1365-2249.2010.04154.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Ramirez-Velazquez C., Castillo E.C., Guido-Bayardo L., Ortiz-Navarette V. IL-17-producing peripheral blood CD177+ neutrophils increase in allergic asthmatic subjects. Allergy Asthma Clin Immunol. 2013;9:23. doi: 10.1186/1710-1492-9-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Lee A., Whyte M.K., Haslett C. Inhibition of apoptosis and prolongation of neutrophil functional longevity by inflammatory mediators. J Leukoc Biol. 1993;54:283–288. [PubMed] [Google Scholar]
- 90.Pocock J.M., Storisteanu D.M.L., Reeves M.B., Juss J.K., Wills M.R., Cowburn A.S., Chilvers E.R. Human cytomegalovirus delays neutrophil apoptosis and stimulates the release of a prosurvival secretome. Front Immunol. 2017;8:1185. doi: 10.3389/fimmu.2017.01185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Garlichs C.D., Eskafi S., Cicha I., Schmeisser A., Walzog B., Raaz D., Stumpf C., Yilmaz A., Bremer J., Ludwig J., Daniel W.G. Delay of neutrophil apoptosis in acute coronary syndromes. J Leukoc Biol. 2004;75:828–835. doi: 10.1189/jlb.0703358. [DOI] [PubMed] [Google Scholar]
- 92.Brannigan A., O-Connell P.R., Hurley H., O'Neill A., Brady H.R., Fitzpatrick J.M. Neutrophil apoptosis is delayed in patients with inflammatory bowel disease. Shock. 2000;13:361–366. doi: 10.1097/00024382-200005000-00003. [DOI] [PubMed] [Google Scholar]
- 93.Ina K., Kusugami K., Hosokawa T., Imada A., Shimizu T., Yamaguchi T., Ohsuga M., Kyokane K. Increased mucosal production of granulocyte colony-stimulating factor is related to a delay in neutrophil apoptosis in Inflammatory Bowel disease. J Gastroenterol Hepatol. 2002;14:46–53. doi: 10.1046/j.1440-1746.1999.01807.x. [DOI] [PubMed] [Google Scholar]
- 94.Zhang D., Chen G., Manwani D., Mortha A., Xu C., Faith J.J. Neutrophil ageing is regulated by the microbiome. Nature. 2016;525:528–532. doi: 10.1038/nature15367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Lood C., Blanco L.P., Purmalek M.M., Carmona-Rivera C., De Ravin S.S., Smith C.K., Malech H.L., Ledbetter J.A., Elkon K.B., Kaplan M.J. Neutrophil extracellular traps enriched in oxidized mitochondrial DNA are interferogenic and contribute to lupus-like disease. Nat Med. 2016;22:146–153. doi: 10.1038/nm.4027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Skendros P., Chrysanthopoulou A., Rousset F., Kambas K., Arampatzioglou A., Mitsios A. Regulated in development and DNA damage responses 1 (REDD1) links stress with IL-1β-mediated familial Mediterranean fever attack through autophagy-driven neutrophil extracellular traps. J Allergy Clin Immunol. 2017;140:1378–1387. doi: 10.1016/j.jaci.2017.02.021. [DOI] [PubMed] [Google Scholar]
- 97.Kallenberg C.G. Key advances in the clinical approach to ANCA-associated vasculitis. Nat Rev Rheumatol. 2014;10:484–493. doi: 10.1038/nrrheum.2014.104. [DOI] [PubMed] [Google Scholar]
- 98.Jennette J.C., Falk R.J. Pathogenesis of antineutrophil cytoplasmic autoantibody-mediated disease. Nat Rev Rheumatol. 2014;10:463–473. doi: 10.1038/nrrheum.2014.103. [DOI] [PubMed] [Google Scholar]
- 99.Kuna A.T. Serological markers of inflammatory bowel disease. Biochem Med (Zagreb) 2013;23:28–42. doi: 10.11613/BM.2013.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Wang Z.Z., Shi K., Peng J. Serologic testing of a panel of five antibodies in inflammatory bowel diseases: Diagnostic value and correlation with disease phenotype. Biomed Rep. 2017;6:401–410. doi: 10.3892/br.2017.860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Jennette J.C., Falk R.J., Gasim A.H. Pathogenesis of ANCA vasculitis. Curr Opin Nephrol Hypertens. 2011;20:263–270. doi: 10.1097/MNH.0b013e3283456731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Roitsch S., Gosswein S., Neurath M.F., Leppkes M. Detection by flow cytometry of anti-neutrophil cytoplasmic antibodies in a novel approach based on neutrophil extracellular traps. Autoimmunity. 2018;51:288–296. doi: 10.1080/08916934.2018.1527317. [DOI] [PubMed] [Google Scholar]
- 103.Porges A.J., Redecha P.B., Kimberly W.T., Csernok E., Gross W.L., Kimberly R.P. Anti-neutrophil cytoplasmic antibodies engage and activate human neutrophils via Fc gamma RIIa. J Immunol. 1994;153:1271–1280. [PubMed] [Google Scholar]
- 104.Boyapati R.K., Dorward D.A., Tamborska A., Kalla R., Ventham N.T., Doherty M.K., Whitfield P.D., Gray M., Loane J., Rossi A.G., Satsangi J., Ho G-t. Mitochondrial DNA is a pro-inflammatory damage-associated molecular pattern released during active IBD. Inflamm Bowel Dis. 2018;24:2113–2122. doi: 10.1093/ibd/izy095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Yousefi S., Mihalache C., Kozlowski E., Schmid I., Simon H.U. Viable neutrophils release mitochondrial DNA to form neutrophil extracellular traps. Cell Death Differ. 2009;16:1438–1444. doi: 10.1038/cdd.2009.96. [DOI] [PubMed] [Google Scholar]
- 106.Caielli S., Athale S., Domic B., Murat E., Chandra M., Banchereau R., Baisch J., Phelps K., Clayton S., Gong M., Wright T., Punaro M., Palucka K., Guiducci C., Banchereau J., Pascual V. Oxidized mitochondrial nucleoids released by neutrophils drive type I interferon production in human lupus. J Exp Med. 2016;213:697–713. doi: 10.1084/jem.20151876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Zhang Q., Raoof M., Chen Y., Sumi Y., Sursal T., Junger W., Brohi K., Itagaki K., Hauser C.J. Circulating mitochondrial DAMPs cause inflammatory responses to injury. Nature. 2010;464:104–107. doi: 10.1038/nature08780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.West A.P., Shadel G.S. Mitochondrial DNA in innate immune responses and inflammatory pathology. Nat Rev Immunol. 2017;17:363–375. doi: 10.1038/nri.2017.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.McIlroy D.J., Jarnicki A.G., Au G.G., Lott N., Smith D.W., Hansbro P.M., Balogh Z.J. Mitochondrial DNA neutrophil extracellular traps are formed after trauma and subsequent surgery. J Crit Care. 2014;29:1133.e1–1133.e5. doi: 10.1016/j.jcrc.2014.07.013. [DOI] [PubMed] [Google Scholar]
- 110.Cristinziano L., Modestino L., Loffredo S., Varricchi G., Braile M., Ferrara A.L., de Paulis A., Antonelli A., Marone G., Galdiero M.R. Anaplastic thyroid cancer cells induce the release of mitochondrial extracellular DNA traps by viable neutrophils. J Immunol. 2020;204:1362–1372. doi: 10.4049/jimmunol.1900543. [DOI] [PubMed] [Google Scholar]
- 111.Giannotta M., Tapete G., Emmi G., Silvestri E., Milla M. Thrombosis in inflammatory bowel diseases: what's the link? Thromb J. 2015;13:14. doi: 10.1186/s12959-015-0044-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Kambas K., Chrysanthopoulou A., Vassilopoulos D., Apostolidou E., Skendros P., Girod A., Arelaki S., Froudarakis M., Nakopoulou L., Giatromanolaki A., Sidiropoulos P., Koffa M., Boumpas D.T., Ritis K., Mitroulis I. Tissue factor expression in neutrophil extracellular traps and neutrophil derived microparticles in antineutrophil cytoplasmic antibody associated vasculitis may promote thromboinflammation and the thrombophilic state associated with the disease. Ann Rheum Dis. 2014;73:1854–1863. doi: 10.1136/annrheumdis-2013-203430. [DOI] [PubMed] [Google Scholar]
- 113.Ribon M., Seninet S., Mussard J., Sebbag M., Clavel C., Serre G. Neutrophil extracellular traps exert both pro- and anti-inflammatory actions in rheumatoid arthritis that are modulated by C1q and LL-37. J Autoimmun. 2019;98:122–131. doi: 10.1016/j.jaut.2019.01.003. [DOI] [PubMed] [Google Scholar]
- 114.Schauer C., Janko C., Munoz L.E., Zhao Y., Kienhofer D., Frey B., Lell M., Manger B., Rech J., Naschberger E., Holmdahl R., Krenn V., Harrer T., Jeremic I., Bilyy R., Schett G., Hoffmann M., Herrmann M. Aggregated neutrophil extracellular traps limit inflammation by degrading cytokines and chemokines. Nat Med. 2014;20:511–517. doi: 10.1038/nm.3547. [DOI] [PubMed] [Google Scholar]
- 115.Clancy D.M., Sullivan G.P., Moran H.B.T., Henry C.M., Reeves E.P., McElvaney N.G., Lavelle E.C., Martin S.J. Extracellular neutrophil proteases are efficient regulators of IL-1, IL-33, and IL-36 cytokine activity but poor effectors of microbial killing. Cell Rep. 2018;22:2937–2950. doi: 10.1016/j.celrep.2018.02.062. [DOI] [PubMed] [Google Scholar]
- 116.Chumanevich A.A., Causey C.P., Knuckley B.A., Jones J.E., Poudyal D., Chumanevich A.P., Davis T., Matesic L.E., Thompson P.R., Hofseth L.J. Suppression of colitis in mice by Cl-amidine: a novel peptidylarginine deiminase inhibitor. Am J Physiol Gastrointest Liver Physiol. 2011;300:G929–G938. doi: 10.1152/ajpgi.00435.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Witalison E.E., Cui X., Causey C.P., Thompson P.R., Hofseth L.J. Molecular targeting of protein arginine deiminases to suppress colitis and prevent colon cancer. Oncotarget. 2015;6:36053–36062. doi: 10.18632/oncotarget.5937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Yost C.C., Schwertz H., Cody M.J., Wallace J.A., Campbell R.A., Vieira-de-Abreu A., Araujo C.V., Schubert S., Harris E.S., Rowley J.W., Rondina M.T., Fulcher J.M., Koening C.L., Weyrich A.S., Zimmerman G.A. Neonatal NET-inhibitory factor and related peptides inhibit neutrophil extracellular trap formation. J Clin Invest. 2016;126:3783–3798. doi: 10.1172/JCI83873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Knight J.S., Subramanian V., O'Dell A.A., Yalavarthi S., Zhao W., Smith C.K., Hodgin J.B., Thompson P.R., Kaplan M.J. Peptidylarginine deiminase inhibition disrupts NET formation and protects against kidney, skin and vascular disease in lupus-prone MRL/lpr mice. Ann Rheum Dis. 2015;74:2199–2206. doi: 10.1136/annrheumdis-2014-205365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Kusunoki Y., Nakazawa D., Shida H., Hattanda F., Miyoshi A., Masuda S., Nishio S., Tomaru U., Atsumi T., Ishizu A. Peptidylarginine deiminase inhibitor suppresses neutrophil extracellular trap formation and MPO-ANCA production. Front Immunol. 2016;7:227. doi: 10.3389/fimmu.2016.00227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Morohoshi Y., Matsuoka K., Chinen H., Kamada N., Sato T., Hisamatsu T., Okamoto S., Inoue N., Takaishi H., Ogata H., Iwao Y., Hibi T. Inhibition of neutrophil elastase prevents the development of murine dextran sulfate sodium-induced colitis. J Gastroenterol. 2006;41:318–324. doi: 10.1007/s00535-005-1768-8. [DOI] [PubMed] [Google Scholar]
- 122.Shioya Y., Katakura K., Ohira H. Neutrophil elastase inhibitor suppresses IL-17 based inflammation of murine experimental colitis. Fukushima J Med Sci. 2014;60:14–21. doi: 10.5387/fms.2013-2. [DOI] [PubMed] [Google Scholar]
- 123.Crocetti L., Quinn M., Schepetkin I., Giovannoni M. A patenting perspective on human neutrophil elastase (HNE) inhibitors (2014-2018) and their therapeutic applications. Expert Opinion o Therapeutic Patents. 2019;29:555–578. doi: 10.1080/13543776.2019.1630379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.INNES J.A. DNase in cystic fibrosis: the challenge of assessing response and maximising benefit. Thorax. 1998;53:1003–1004. doi: 10.1136/thx.53.12.1003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Thomas M.G., Bayliss C., Bond S., Dowling F., Galea J., Jairath V., Lamb C., Probert C., Timperley-Preece E., Watson A., Whitehead L., Williams J.G., Parkes M., Kaser A., Raine T. Trial summary and protocol for a phase II randomised placebo-controlled double-blinded trial of Interleukin 1 blockade in Acute Severe Colitis: the IASO trial. BMJ Open. 2019;9 doi: 10.1136/bmjopen-2018-023765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Dinarello C.A., Simon A., van der Meer J.W. Treating inflammation by blocking interleukin-1 in a broad spectrum of diseases. Nat Rev Drug Discov. 2012;11:633–652. doi: 10.1038/nrd3800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Mertens M., Singh J.A. Anakinra for rheumatoid arthritis: a systematic review. J Rheumatol. 2009;36:1118–1125. doi: 10.3899/jrheum.090074. [DOI] [PubMed] [Google Scholar]
- 128.Chirivi R.G.S., van Rosmalen J.W.G., van der Linden M., Euler M., Schmets G., Bogatkevich G., Kambas K., Hahn J., Braster Q., Soehnlein O., Hoffmann M.H., Es H., Raats J.M.H. Therapeutic ACPA inhibits NET formation: a potential therapy for neutrophil-mediated inflammatory diseases. Cell Mol Immunol. 2020 Mar 20 doi: 10.1038/s41423-020-0381-3. [E-pub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Van Avondt K., van der Linden M., Naccache P.H., Egan D.A., Meyaard L. Signal inhibitory receptor on leukocytes-1 limits the formation of neutrophil extracellular traps, but preserves intracellular bacterial killing. J Immunol. 2016;196:3686–3694. doi: 10.4049/jimmunol.1501650. [DOI] [PubMed] [Google Scholar]