Case
A single, 48-year-old white woman visits a new family physician to seek advice about the prevention of osteoporosis, because she thinks she is entering the menopause. She is confused about the causes of osteoporosis and whether she should make changes to her diet or lifestyle in order to prevent a hip fracture. She is particularly concerned, because her 70-year-old mother recently suffered a hip fracture when she slipped on a stair. A diet history reveals a long-standing intolerance to lactose, resulting in the exclusion of dairy products since the patient was a teenager. She has not consistently taken supplemental calcium, although she recently tried drinking lactase-treated milk and calcium-fortified soy drink or orange juice. She is not a smoker but drinks 1–2 glasses of wine at least 4 days a week. A physical examination reveals a healthy-seeming woman of normal weight for height whose only complaint is occasional back pain when standing for a long time.
Osteoporosis is a costly and debilitating disease that is associated with significant morbidity and mortality. In Canada, the prevalence of osteoporosis among women aged 50 years or more is 15.8%.1 A 50-year-old woman has a 40% chance of experiencing a fragility fracture due to a low bone mass during her remaining lifetime.2 Of patients with hip fractures, 50% experience long-term disability, and up to 20% die within one year of fracture.3 The risk of death from osteoporosis-related fracture exceeds the mortality rates from breast and ovarian cancer combined.4 Osteoporosis is also a significant burden to the health care system in Canada, with an estimated cost of $1.3 billion per year to treat osteoporosis and related fractures. Consequently, there is an urgent need to develop effective strategies that prevent or manage osteoporosis and, ultimately, reduce the risk of osteoporosis-related fragility fracture among Canadians.
Does nutrition have a role in the achievement of peak bone mass?
Genetics is the most important contributor (up to 80%) to the set point for peak bone mass in early life (by late adolescence or early in the third decade). Thus, a family history of osteoporosis is a flag for osteoporosis risk. Nondietary factors that contribute to the causes of adult-onset osteoporosis include a sedentary lifestyle (lack of weight-bearing activity), a small body frame and use of medications such as steroid drugs. Nutrition also has a unique role in the maintenance of bone status and, thereby, may be a factor in optimizing bone health from childhood through late adulthood. Although studies that link diet and bone mass have focused primarily on calcium and vitamin D intake, other nutrients such as magnesium, fluoride, phosphorus and zinc are also important for their specific role in bone composition.
Retrospective and longitudinal studies provide conflicting evidence about the association of calcium intake in childhood, adult bone mass and risk of osteoporosis in later life.5 The current dietary reference intakes (DRIs)6 for calcium, phosphorus and vitamin D for adolescents and adults were based on an approximation of the intake that would maintain desirable rates of calcium retention, factorial estimates of requirements based on the accretion of calcium in bone during growth, and clinical trials in which bone mineral content was measured in response to varying calcium intake.6 In clinical trials involving children and adolescents, those with the lowest habitual calcium intake (< 880 mg/d in one study)7 before entering the study achieved the greatest increase in bone mineral density, with a larger increase occurring in cortical bone sites (radius and femoral shaft) rather than in trabecular bone.5 In addition, prepubertal children, as compared with pubertal children, had a greater increase in bone density from a higher calcium intake.5
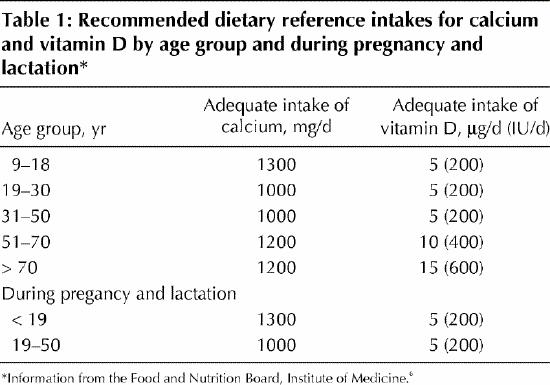
In light of this, it may be important to target dietary advice to promote bone health to those groups at greatest risk and with the greatest potential to respond to diet, namely, children in the premenarcheal and perimenarcheal periods when a major proportion of bone mass is acquired. The DRIs for adequate intake for calcium, phosphorus and vitamin D are summarized in Table 1. How do the current intakes of Canadian children measure up? Unfortunately, no national dietary survey has been conducted since 1970. A recent independent survey of the eating habits of Canadians8 reported mean daily calcium intakes in the 13–17-year age group of 1407 mg for males (n = 84) and 1004 mg for females (n = 94). Because an adequate intake forms the basis of the DRI, it is not possible to determine whether mean intakes below the adequate intake represent any risk of nutritional inadequacy.9 Clinically, children and adolescents who avoid dairy products and take no appropriate nutrient supplementation, who have malabsorptive disorders or who follow very low-energy diets (such as elite female athletes or those with anorexia) should be target groups for dietary counselling.
Table 1
Is nutrition important in the prevention and treatment of osteoporosis in adult life?
In adults, before menopause, maintenance of peak bone mass is probably achieved with calcium intakes of 1000 mg/day.6 In contrast to previous nutrient-based recommendations, the new DRIs for calcium and vitamin D during pregnancy and lactation are not higher than the recommendation for age.6 The demands for fetal accretion of calcium and output in milk are met by physiological changes in calcium metabolism that occur independently of calcium intake and presumably in response to hormonal changes during pregnancy and lactation.10 A combination of elevated calcium absorption in pregnancy mediated by increased production of the active vitamin D metabolite, and renal conservation of calcium and bone resorption during lactation,10,11 supply the necessary calcium for the fetus and milk. The bone loss that occurs (up to 6% or more at some bone sites) is transient, being restored after the return of menses.11 This phenomenon is supported by epidemiological studies that found no negative associations between number of pregnancies or lactations and bone mass or fracture risk.6
Attenuation of the bone loss associated with estrogen withdrawal after menopause most often involves hormone replacement therapy, or other novel therapies. Nutrition, specifically calcium and vitamin D, also has a role at these later stages of the life cycle to be used alone or in combination with traditional therapies to maintain bone mass and prevent fragility fracture. In addition, the identification of phytoestrogens, plant-derived compounds with estrogen-like activity, may be of benefit to bone health. Nutritional strategies that are effective at preventing and managing osteoporosis are particularly important, because rates of acceptance of and compliance with hormone replacement therapy and bisphosphonates are often low due to the potentially adverse side effects associated with these therapies and an overall reluctance of women to take medications to prevent “silent diseases.”12,13,14
In addition to achieving adequate intakes (Table 1) of nutrients associated with bone health through diet and fortified foods or supplements, or both, the following dietary advice might assist in optimizing nutritional balance to support maintenance of bone mass.
Calcium
Although milk and dairy food products are the most concentrated source of dietary calcium, calcium-fortified foods such as orange juice (300 mg per serving) and soy drinks are now available in Canada. In one study, Canadian women (n = 181) aged 50–65 years consumed a daily average of 777 mg of calcium.8 If adults do not consume some combination of these foods, then supplements to provide 1000 mg/day of elemental calcium are advised. To maximize absorption of calcium from supplements and minimize side effects, supplements should be consumed in doses of not more than 500 mg, taken either with meals (calcium carbonate or phosphate) or on an empty stomach (calcium citrate), and taken at a different time from iron supplements and also from drugs such as bisphosphonates or the antibiotic tetracycline.15
Vitamin D
Although adequate exposure to the sun should provide all humans with sufficient vitamin D, many populations require exogenous vitamin D, particularly if they have pigmented skin or live in the extremes of the hemisphere where the ultraviolet energy is not adequate in winter months or is absorbed by clouds, ozone or other atmospheric pollution. Reports of rickets caused by vitamin D deficiency in specific groups of infants and children in Canada16 supports this approach. Clinical trials involving elderly people who are prone to developing vitamin D deficiency have provided evidence of a positive benefit of vitamin D supplementation (with calcium) in reducing fracture risk.17 The adequate intake of vitamin D (Table 1) assumes that no vitamin D is derived by sun-mediated skin synthesis. Food sources of vitamin D include cod-liver oil, fatty fish or fortified foods such as milk and cereal.
Protein, sodium and caffeine
Specific dietary components can influence both the amount of absorbed calcium available for deposition in bone and bone resorption. An adequate amount of dietary protein is essential to maintain production of hormones and growth factors that modulate bone synthesis.18 This is especially important for elderly people who tend to have low protein intakes. At any age, the balance of the total dietary acid and alkaline load is critical to the excretion of calcium, especially if the calcium intake is marginal. This is achieved with a diet balanced in protein foods that generate acid and fruits and vegetables that provide the alkali to neutralize the acid.19,20 In theory, if alkali-producing foods spare bone calcium from being mobilized to serve as a source of labile base to neutralize blood pH, less skeletal mass will be lost over time.
A high intake of salt leads to increased sodium excretion and with it an obligatory loss of urinary calcium because of the solvent drag effect of sodium.21 A high dietary intake of caffeine induces a short-term increase in urinary calcium loss.6 Although the interactive effects of dietary protein, sodium and caffeine on overall calcium retention are recognized, there is no substantive evidence that this contributes to bone loss if the recommended calcium intake for age is achieved. The best advice for all ages is to consume protein to meet needs, but not to excess, and to avoid excessive amounts of sodium and caffeine to minimize any negative effect on urinary calcium loss.
Phytoestrogens
Phytoestrogens are plant-derived compounds (i.e., isoflavones) that have a similar chemical structure to endogenous estrogen with the potential to act like estrogen on bone tissue.22 Soy protein and flaxseed are the most common sources of phytoestrogens in the Canadian diet. The protective effects of phytoestrogens on bone loss have been reported from only 2 human feeding trials.23,24 In postmenopausal women who consumed no isoflavones or 56 mg or 90 mg of isoflavones per day for 6 months, the higher dose of isoflavones produced a higher bone mineral content (2.4%) and bone mineral density (2.2%) at the lumbar spine compared with baseline values.23 Among perimenopausal women, lumbar bone mineral content and bone mineral density were preserved in the group who consumed the high dose of isoflavones (80 mg), whereas women who consumed no isoflavones experienced a significant loss in lumbar spine bone mineral content and bone mineral density compared with baseline values over the 6 months of the intervention.24 However, prospective randomized trials of longer duration (>> 2 years) with larger sample sizes are required to establish whether consuming a diet rich in phytoestrogens prevents bone loss and reduces fracture risk.
Treatment for the patient
The family physician first took the new patient's history to determine whether she had any particular risk factors for developing postmenopausal osteoporosis. The mother's hip fracture, which was related to a fall down some stairs, may or may not be indicative of a genetic predisposition to osteoporosis. The physician suggested that both the patient and her mother have a bone density measurement done by dual energy x-ray absorptiometry. This method is considered to be the “gold standard” of measures of bone mass25 and allows the evaluation of a subject's bone density in relation to age-related and sex-related references, as well as providing a basis for the diagnosis of osteoporosis.26 Knowledge of their bone density measures influences womens' decisions about the use of drug therapies or adoption of life-style habits that promote bone health.27 The lifelong avoidance of calcium-rich foods by the patient, without the use of supplemental calcium, and extended exposure to only winter sunlight (which is known not to generate synthesis of cholecalciferol [vitamin D] in skin) may represent risk factors for the patient not to have achieved her genetic potential for peak bone mass. Because the patient is approaching menopause, the physician advised her to optimize her intake of calcium and vitamin D through the consumption of lactase-treated milk, calcium-fortified soy drinks or orange juice, or calcium supplements, or some combination of these. Based on the current DRIs, she should aim for 1000 mg of calcium per day (1200 mg after she enters the menopause) and 5 μg vitamin D per day (10 μg after the menopause). The physician recommended that the patient consume adequate amounts of protein, moderate amounts of salt and caffeine, and a variety of vegetables and fruit and to engage in weight-bearing activity in order to minimize the excessive bone loss usually associated with estrogen withdrawal. Once the physician has obtained the results of the bone density scans, he will be able to tell the patient if more aggressive intervention is warranted such as with bone antiresorption drugs or hormone replacement therapy.
Articles to date in this series .
Hoffer LJ. Clinical nutrition: 1. Protein–energy malnutrition in the inpatient. CMAJ 2001;165(10):1345-9.
Footnotes
This series is supported, in part, by an unrestricted educational grant from the Danone Institute of Canada.
This article has been peer reviewed.
Competing interests: None declared.
Correspondence to: Dr. Stephanie Atkinson, Department of Pediatrics, McMaster University Health Sciences Centre, Rm. 3V42, 1200 Main St. W, Hamilton ON L8N 3Z5; fax 905 521-1703; satkins@mcmaster.ca
References
- 1.Tenenhouse A, Joseph L, Kreiger N, Poliquin S, Murray TM, Blondeau L, et al. Estimation of the prevalence of low bone density in Canadian women and men using a population-specific DXA reference standard: the Canadian Multicentre Osteoporosis Study (CaMos). Osteoporos Int 2000;11(10):897-904. [DOI] [PubMed]
- 2.Melton LJD, Chrischilles EA, Cooper C, Lane AW, Riggs BL. Perspective. How many women have osteoporosis? J Bone Miner Res 1992;7:1005-10. [DOI] [PubMed]
- 3.Cummings SR, Kelsey JL, Nevitt MC, O'Dowd KJ. Epidemiology of osteoporosis and osteoporotic fractures. Epidemiol Rev 1985;7:178-208. [DOI] [PubMed]
- 4.Canada yearbook. Ottawa: Statistics Canada; 1994.
- 5.Wosje KS, Specker BL. Role of calcium in bone health during childhood. Nutr Rev 2000;58:253-68. [DOI] [PubMed]
- 6.Food and Nutrition Board, Institute of Medicine. Dietary reference intakes for calcium, magnesium, phosphorus, vitamin D and fluoride. Washington: National Academy Press; 1997.
- 7.Bonjour JP, Carrie AL, Ferrari S, Clavien H, Slosman D, Theintz G, et al. Calcium-enriched foods and bone mass growth in prepubertal girls: a randomized, double-blind, placebo-controlled trial. J Clin Invest 1997;99:1287-94. [DOI] [PMC free article] [PubMed]
- 8.Starkey LJ, Johnson-Down L, Gary-Donald K. Food habits of Canadians: comparison of intakes in adults and adolescents to the recommendations of Canada's Food Guide to Healthy Eating. Can J Diet Pract Res 2001;62(2):61-9. [PubMed]
- 9.Food and Nutrition Board, Institute of Medicine. Dietary reference intakes: applications in dietary assessment. Washington: National Academy Press; 2001.
- 10.Ritchie LD, Fung EB, Halloran BP, Turnlund JR, Van Loan MD, Cann CE, et al. A longitudinal study of calcium homeostasis during human pregnancy and lactation and after resumption of menses. Am J Clin Nutr 1998;67:693-701. [DOI] [PubMed]
- 11.Kalkwarf HJ, Specker BL, Bianchi DC, Ranz J, Ho M. The effect of calcium supplementation on bone density during lactation and after weaning. N Engl J Med 1997;337;523-8. [DOI] [PubMed]
- 12.den Tonkelaar I, Oddens BJ. Determinants of long-term hormone replacement therapy and reasons for early discontinuation. Obstet Gynecol 2000; 95:507-12. [DOI] [PubMed]
- 13.Groeneveld FP, Bareman FP, Barentsen R, Dokter HJ, Drogendijk AC, Hoes AW. Determinants of first prescription of hormone replacement therapy. A follow-up study among 1689 women aged 45–60 years. Maturitas 1994;20:81-9. [DOI] [PubMed]
- 14.Hill DA, Weiss NS, LaCroix AZ. Adherence to postmenopausal hormone therapy during the year after the initial prescription: a population-based study. Am J Obstet Gynecol 2000;182:270-6. [DOI] [PubMed]
- 15.Dawson-Hughes B. Calcium, vitamin D and risk of osteoporosis in adults: essential information for the clinician. Nutr Clin Care 1998;1(2):63-70.
- 16.Binet A, Kooh SW. Persistence of vitamin D-deficiency rickets in Toronto in the 1990s. Can J Public Health 1996;87:227-30. [PubMed]
- 17.Dawson-Hughes B, Harris SS, Krall EA, Dallal GE. Calcium and vitamin D supplementation on bone density in men and women 65 years of age or older. N Engl J Med 1997;337:670-6. [DOI] [PubMed]
- 18.Heaney RP. Protein intake and bone health: the influence of belief systems on the conduct of nutritional science. Am J Clin Nutr 2001;73:5-6. [DOI] [PubMed]
- 19.Appel LJ, Moore TJ, Obarzanek E, Vollmer WM, Svetkey LP, Sacks FM, et al. A clinical trial of the effects of dietary patterns on blood pressure. N Engl J Med 1997;336:1117-24. [DOI] [PubMed]
- 20.Tucker KL, Hannan MT, Chen H, Cupples LA, Wilson PW, Kiel DP. Potassium, magnesium and fruit and vegetable intakes are associated with greater bone mineral density in elderly men and women. Am J Clin Nutr 1999; 69:727-36. [DOI] [PubMed]
- 21.Cappuccio FP, Blackwood AM, Cook DG, Sagnella GA. Blood pressure and sodium intake as risk factors for high urinary Ca losses in a multi-ethnic population. Osteoporos Int 2000;11(Suppl l2):S91.
- 22.Miksicek RJ. Interaction of naturally occurring nonsteroidal estrogens with expressed recombinant human estrogen receptor. J Steroid Biochem Mol Biol 1994; 49:153-60. [DOI] [PubMed]
- 23.Potter SM, Baum JA, Teng H, Stillman RJ, Shay NF, Erdman JW Jr. Soy protein and isoflavones: their effects on blood lipids and bone density in postmenopausal women. Am J Clin Nutr 1998;68:1375S-9S. [DOI] [PubMed]
- 24.Alekel DL, Germain AS, Peterson CT, Hanson KB, Stewart JW, Toda T. Isoflavone-rich soy protein isolate attenuates bone loss in the lumbar spine of perimenopausal women. Am J Clin Nutr 2000;72:844-52. [DOI] [PubMed]
- 25.Genant HK, Engelke KM, Fuerst T, Gluer CC, Grampf S, Harris ST, et al. Noninvasive assessment of bone mineral and structure: state of the art. J Bone Miner Res 1996;11:707-30. [DOI] [PubMed]
- 26.Lu Y, Genant HK, Shepherd J, Zhao S, Mathur A, Guerst TP, et al. Classification of osteoporosis based on bone mineral densities. J Bone Miner Res 2001;16:901-10. [DOI] [PubMed]
- 27.Marci CD, Viechnicki MB, Greenspan SL. Bone mineral densitometry substantially influences health-related behaviors of postmenopausal women. Calcif Tissue Int 2000;66:113-8. [DOI] [PubMed]


