Abstract
Despite theadvancements in surgical reconstructive techniques for bladder exstrophy-epispadias complex, urinary incontinence represents a major problem that affects the quality of life. Bladder augmentation associated to Mitrofanoff external continent urinary diversion (ECUD) constitute for some surgeon the best solution for the management of bladder exstrophyallowing to achieve continence and to preserve renal function.
Keywords: Mitrofanoff, Appendix, Diversion
Introduction
Despite theadvancements in surgical reconstructive techniques for bladder exstrophy-epispadias complex, urinary incontinence represents a major problem that affects the quality of life.Achieving a capacitating and continent urinary reservoir in patients with bladder exstrophyare the main therapeutic goals. Presentation in adolescence and adulthood due to failure of anterior surgical procedures or to delayed presentation explained by a lack of awareness is very rare. At this age bony fusion has already occurred and bladder capacity is very low which constitute a surgical challenge.1Bladder augmentation associated to Mitrofanoff external continent urinary diversion (ECUD) constitute for some surgeon the best solution for the management of bladder exstrophyallowing to achieve continence and to preserve renal function.
Observation
Our patient is a 16 years-old-boy without antenatal diagnosis of malformations. He was operated at the age of three months and six months for primary closure of his extrophied bladder without concomitant osteotomy complicated by failure for both surgeries. He presented to our department forextrophy-epispadias complex. At examination we found an abdominal wall defect with completely exposed and everted bladder below umbilical stump, a complete dorsally opened urethral plate, corpora cavernosa were clearly visible beneath and alongside the urethral plate and the scrotum was normally developed, with descended testes which reached puberty (Fig. 1). It was responsible for significant social and psychological repercussions: He dropped out of school at the age of eightand had general behavioral problems.No psychological supportwas provided due to the low-socioeconomic status.On peroperatory, the bladder template was too small to be closed (Fig. 2a), we liberated the dome and lateral walls of the bladder, ileocystoplasty was performed using 30 cm of ileum, the bladder neck was completely closed and a right sided continent urinary diversion, Mitrofanoff, was perfomed using the appendix(Fig. 2b). The patient had undergone simultaneous epispadias repair. lntermittent catheterization of the bladder via appendicocutaneostomy was started on the 21st postoperative day (Fig. 3) and it was easily learned and performed by the patient. There were no complications related to Mitrofanoff procedure. The ultimate bladder capacity was 300 ml. The patient was continent and on clean intermittent catheterization per stoma every 3 hours.psychological care has been initiated in this patient.
Fig. 1.
Abdominal defect and epispadias.
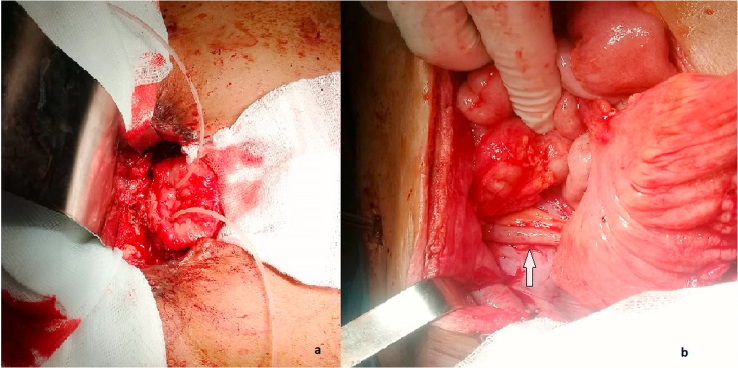
Fig. 2.
Preoperative aspect
a: bladder template
b: final aspect of the mitrofanoff urinary diversion
white arrow: appendix used as cutaneostomy.
Fig. 3.
Catheterization of the Mitrofanoff appendicocutaneostomy.
Discussion
The maingoals of the surgical management of the bladder exstrophy are closing the abdomen and bladder,establishing urinary continence with the preservation of renal function and providing acceptable external genitalia. Neonatalis the best period to perform surgery; actually two main surgical techniques are usedfor closure:
-
1)
The classic staged technique consists on initial closure of the bladder and posterior urethra followed by epispadias repair 6–12 months later and finally bladder-neck reconstruction associated usually with bilateral ureteric reimplantsat a later date, around the age of 4–6; and
-
2)
complete primary repair which consists of repairing the bladder and epispadias at the time of the initial closure, usually shortly after birth.2Late presentation in adolescence adulthood where bony fusion has occurred and the exposed bladder plate wascontracted, therefore constitutedmajor surgical challenge.1In the literature we found that during the last three decades several cases of late presentation of exstrophy have been reported in non-developed countries, surgical techniques have evolved during these years.The first reported case of adult bladder exstrophy was in 1987 by Matsuda et al. who treated two adult female patients with cystectomy, construction of a Kock's continent ileal reservoir, and closure of the abdominal fascial defect using alloplastic material.Ten years later Gulati et al.3 reported two cases of adult females presenting with untreated bladder exstrophy which underwent cystectomy and modified Mainz pouch with primary closure of the abdominal wall defect. Pathak et al. and recentely Jana et al.4 provided their experience with a modified surgical management of bladder exstrophy in adults characterized by a preservation of the bladder template usingileocystoplasty, bladder neck reconstruction, and abdominal wall closure with flaps. Continent urinary diversion with bladder augmentationhas beenrecently considered for patients with epispadias-exstrophy complex who have failed bladder neck repair or whose bladder is not adequate for reconstruction. It can also be considered as primary surgical procedure for patients with delayed presentation of bladder exstrophy in poor resource countries, indeed, it constitutes of an acceptable alternative to the patient allowing achieving dryness without the need forrepeated anti-incontinence procedures.1 In our case, we opted for bladder augmentation associated to Mitrofanoff ECUD since he has already benefited from primary closure of the bladder template complicated by failure twice which resulted in a very small contracted template with poor chances of successful bladder closure and neck reconstruction.
Bladder neck closure in conjunction with a continent cutaneous diversion procedure is a highly effective method of achieving continence in patients with bladder exstrophy-epispadias complex.1 Reports on the functional outcome of achieving continence using intermittent catheterization for patients failing primary reconstreuction exceed 90%. Bladder exstrophy has a dramatic psychological impact in childhood and adolescence.5 The main complaint reported by patients is incontinence which greatly affects the patient's school life and social life. Vajda et al. found an appreciable improvement in quality of life in 90% of 49 patients who undergo bladder augmentation of whom 18 patients for bladder exstrophy. Quality of life was significantly better in those patients who received an abdominal stoma as opposed to clean intermittent catheterization per the native urethra. Kari et al. evaluated the compliance of two groups of children with neurogenic bladder to perform Clean Intermittent Catheterization: voiding through natural orifice versus through appendico-vesocostomy. There was acceptance of catheterization by most children but Mitrofanoff catheterization seemed to have a lower social impact, complications and more adherence to therapy.
Conclusion
Management of bladder exstrophy in adolescence constitutes a major surgical challenge especially in developing countries. We emphasize that bladder neck closure and augmentation in conjunction with Mitrofanoff ECUD is an effective and safe alternative to classic reconstruction techniques allowing toachieve continence and toimprove quality of life.
Contributor Information
Mohamed Amine Mseddi, Email: mseddi_amine@yahoo.fr.
Ahmed Samet, Email: ahmed.samet40@gmail.com.
Mourad Hadjslimene, Email: mourad.hadjslimen@gmail.com.
References
- 1.Mensah J.E., Asante E.K., Appeadu Mensah W., Glover-Addy H. Continent cutaneous diversion for bladder exstrophy in adults. Afr J Urol. 2013;19:94–98. June (2) [Google Scholar]
- 2.Grady R.W., Mitchell M.E. Complete primary repair of exstrophy. J Urol. 1999;162:1415–1420. [PubMed] [Google Scholar]
- 3.Gulati P., Yadav S.P., Sharma U. Management of bladder exstrophy in adulthood: report of 2 cases. J Urol. 1997;157:947–948. [PubMed] [Google Scholar]
- 4.Jana A., Maiti K., Mondal T.K., Majhi T.K. Management of the exstrophy-epispadiascomplex in adolescents and adults. Afr J Urol. June 2017;23(2):100–104. [Google Scholar]
- 5.Stjernqvist K., Kockum C.C. Bladder exstrophy: psychological impact during childhood. J Urol. 1999 Dec;162(6):2125–2129. doi: 10.1016/S0022-5347(05)68139-6. [DOI] [PubMed] [Google Scholar]