Abstract
Injury to the distal biceps occurs in certain high risk groups. Anatomical continuity of the lacertus fibrosus has bearing on the extent of retraction of the torn tendon stump. The objective of clinical and imaging evaluation is to discriminate between tendinosis, partial tear, acute complete tear and chronic complete tear. A complete tear of the distal biceps tendon can be diagnosed clinically with the Hook test. The traditional Hook test and the resisted Hook test are useful clinical tests. Though x-rays are routinely done, MRI remains the investigation of choice. Non-operative treatment has a role in selected patients with partial tear or patients with complete tear who have low functional demands. Operative treatment is the recommended treatment for complete tear of the distal biceps and is associated with good functional outcome and patient satisfaction.
Keywords: Distal biceps, Rupture, Tear, Repair, Reconstruction
Karthik VishwanathanKrishna Soni
1. Biceps anatomy
The lacertus fibrosus is a fascial thickening that connects the distal biceps superolaterally to the fascia over the forearm flexor muscles in the inferomedial direction. Anatomical continuity of the lacertus fibrosus prevents retraction of the torn distal biceps tendon whereas complete transection of the lacertus fibrosus would lead to significant retraction of the torn biceps tendon.
The biceps tendon at the elbow is a powerful forearm supinator and also contributes to flexion at the elbow. Hence, rupture of the distal biceps leads to weakness of forearm supination which makes it difficult to do tasks requiring powerful supination such as using a screwdriver or turning the key.
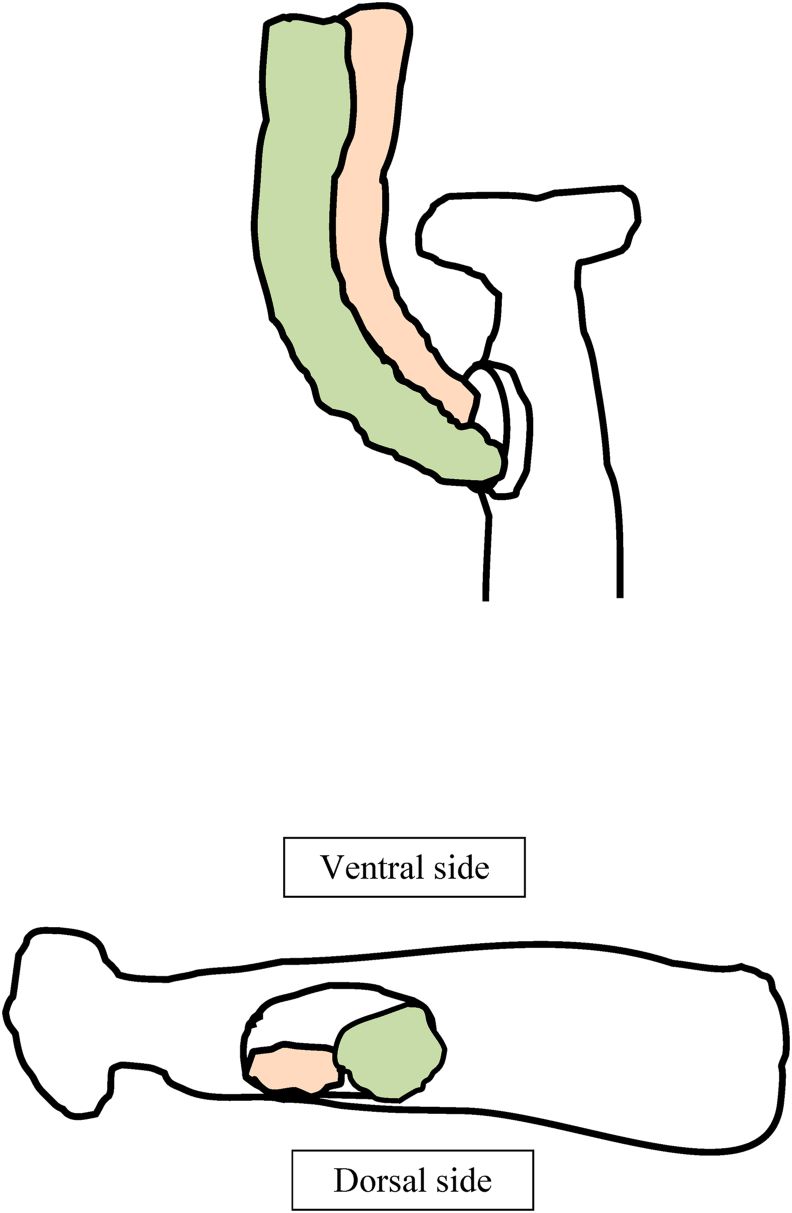
The long head of the biceps inserts on the proximal and slightly posterior aspect of the radial tuberosity and thereby acts as a chief supinator. The short head of the biceps inserts acts as a principal elbow flexor and both the long and the short heads insert posteriorly on the radial tuberosity.1,2 Recreation of the anatomic footprint is paramount to regain satisfactory flexion and supination [Fig. 1].
Fig. 1.
Shows long head of biceps (orange colour) and short head of biceps (green colour) inserting on the footprint of left side radial tuberosity.
2. Biceps rupture etiopathology
The distal biceps tendon inserts onto the ulnar aspect of the bicipital tuberosity (also called radial tuberosity). The likely pathophysiological mechanism predisposing the distal biceps to rupture is a compromised zone of hypovascularity due to watershed zone of arterial blood supply and reduced distance between the upper parts of radius and the ulna during pronation.2
3. Epidemiology
The incidence of distal biceps tearis approximately 5.4 cases per 1,00,000 patients per year.3 This condition is most commonly seen in two diverse age groups: the young, active, elite sportsmen and in the middle age group people from fourth to sixth decades.4 Various tendinopathies are commonly observed from fourth to sixth decades of life and hence it is postulated that tendinopathy might be a causative factor for biceps rupture in elderly people.
The incidence of biceps rupture is higher in individuals participating in contact sports, and those consuming anabolic steroids. Pushing or lifting heavy objects, tobacco smoking and raised body mass index are considered predisposing factors for distal biceps rupture.3 Whether distal biceps tears are more frequent in the dominant or non-dominant extremity has also been a subject of debate.3 In a recent study, majority of the individuals with distal biceps rupture were involved in non-heavy, low demand occupations such as office work.4 The possible reasons may be a proportionately greater extension load applied to a flexing elbow leading to rupture of the distal biceps. Cadaver studies have reported that the distal biceps tendon tends to fail at a mean tensile load of 204 N.5Another in vitro cadaver study has reported an increase of the ultimate failure load of the distal biceps as the extension of the elbow increased from the 90° flexed position although the difference was not statistically significant.6
The specific flexion angle of elbow, most prone to the rupture of distal biceps remains unknown.
4. Clinical features
4.1. Symptoms
Prodromal symptom such as aching sensation in the anterior elbow is seen in 10% of the patients. Majority of the patients with a full thickness distal biceps rupture reports a painful “pop” sensation. Anterior elbow pain, anterior arm and elbow swelling and weakness of elbow flexion and forearm supination are commonly reported symptoms. Activities such as operating a manual screw driver or opening jars are difficult to perform by involved arm.
4.2. Signs
The normal biceps contour is seen in Fig. 2. In a torn distal biceps there would be anterior ecchymosis, swelling and a prominent biceps bulge atthe anterior mid-arm level (Popeye the sailor sign) [Fig. 3].
Fig. 2.
Shows the normal contour and shape of the biceps brachii when seen from the front.
Fig. 3.
Shows the abnormal contour of the biceps brachii and Popeye the sailor sign.
Palpation would reveal tenderness and defect in the anterior part of the cubital fossa in case of complete tear. The amount of proximal retraction would depends on the partial or complete rupture of distal biceps and the integrity of the lacertus fibrosus.
4.3. Special tests
4.3.1. Hook test
The Hook test is useful to diagnose acute complete rupture and to evaluate postoperative recovery of the distal biceps tendon.
The Hook test was initially described with the arm positioned by the side of the body and the elbow in 90° flexion. The integrity of biceps tendon is ascertained by hooking it with examiner's finger inserted from the lateral side of the tendon. Repeating the same manoeuvre from the medial side would give information about the anatomical continuity of the lacertus fibrosus.7 With this test, it is difficult to separately ascertain the structural integrity of biceps brachii and the brachialis.7
In the modified Hook test the patients positions the forearm in complete supination so the palm faces inwards with the shoulder in 90° abduction and elbow in 90° flexion. Examiner performs the hook test with patient actively resisting the pronation of the forearm. The advantage of this method is its ability to selectively tighten the distal biceps.8
The interpretation of the findings of the hook test and the resisted hook test are described in Table 1.
Table 1.
Shows various components, findings and interpretation of hook test and resisted hook test.
| Components of Hook test and resisted Hook test | Clinical findings | Interpretation |
|---|---|---|
| Hook test | Normal intact tendon | |
|
|
|
|
|
|
| Resisted hook test | Taut painless tendon | |
| Hook test | Distal biceps tendinosis or partial rupture of distal biceps | |
|
Taut painless/painful tendon | |
|
Taut painful tendon | |
| Resisted hook test | Taut painful tendon | |
| Hook test | Partial rupture of distal biceps | |
|
No taut, cord like structure | |
|
No taut, cord like structure | |
| Resisted hook test | Taut painful/painless tendon | |
| Hook test | Complete rupture of distal biceps | |
|
No taut, cord like structure | |
|
No taut, cord like structure | |
| Resisted hook test | No taut, cord like structure |
The Hook test cannot be reliably performed and interpreted in the presence of heterotopic ossification in the anterior aspect of the elbow. In chronic cases of distal biceps tear, the formation of large amount of scar tissue may lead to false positive hook test.9
After repair of the torn distal biceps tendon, Hook test should reveal normal taut distal biceps tendon after four months of surgery. A negative Hook test at this stage indicates a failed or failing repair.8
The hook test is a highly sensitive and specific test for diagnosis of distal biceps rupture however both studies on the hook test are retrospective studies and are prone to various types of bias.
4.3.2. Biceps squeeze test
The Biceps squeeze test is useful for both preoperative confirmation of diagnosis of a complete distal biceps rupture and for confirmation of healing of a repaired biceps tendon.
In this test, the patient is made to sit with the elbow in about 70° - 90° flexion and arms by the side of the body with the forearm pronated. Compression of the bulky part of the biceps muscle at the level of mid-arm by the examiner would lead to supination of the forearm if the distal biceps tendon is intact. Lack of supination of the forearm is suggestive of complete rupture of the biceps tendon.10
Limitation of the biceps squeeze test includes its inability to discriminate between partial rupture and intact tendon because squeezing of biceps elicits forearm supination in both conditions. The patient should be relaxed during the squeeze test because guarding due to pain in acute trauma might lead to a false positive result.10
4.3.3. Biceps aponeurosis flex test
This objective of this crucial test is to ascertain the anatomical integrity of the bicipital aponeurosis or the lacertus fibrosus. The patient is asked to clench the fist, palmar flex the wrist, and supinate the forearm with elbow in 75° flexion. The well defined, taut, medial borders of the lacertus fibrosus would be felt if it is intact.11
4.3.4. Supination pronation test
In this test, the patient is asked to alternately supinate and pronate the forearm while the evaluator observes the contour of the biceps muscle. If the distal biceps is intact, the contour of the biceps brachii would become prominent with forearm supination. It would remain unchanged in complete disruption of the distal biceps.12
4.3.5. Biceps crease interval (BCI)
The Biceps Crease Interval (BCI) is an indicator of proximal retraction of the torn distal biceps tendon. The BCI is the vertical distance between the most prominent cubital fossa crease and the point on the arm at which the biceps muscle bulk acutely begins to narrow distally. BCI value greater than 6 cm is indicative of full thickness rupture of the distal biceps tendon.13 The role of BCI in diagnostic confirmation of partial disruption of distal biceps is not known.
4.3.6. Distal biceps provocation test
A clinical test described by Caekebeke et al.14 has been reported to be useful to diagnose partial rupture of the distal biceps. The examiner supports the patients's elbow in 70° flexion and the patient is asked to perform resisted elbow flexion with forearm fully supinated and then maintaining the forearm in full pronation. Aggravation of elbow pain in resisted elbow flexion with the forearm in full pronation is strongly suggestive of distal biceps tendinitis or partial rupture of the distal biceps. This clinical test has 100% sensitivity and 100% specificity.
Our recommendation is to use a combination of these tests. The Hook test has 100% specificity and 80–100% sensitivity.7,9 The Biceps squeeze test and the supination pronation test also have 100% sensitivity. Distal biceps provocation test appears superior as it has 100% sensitivity and 100% specificity to detect partial tears of the distal biceps. Integrity of the lacertus fibrosus can be evaluated using the bicipital aponeurosis flex test.
5. Imaging
5.1. Radiograph
X-ray of the elbow would rule out any bony injuries such as coronoid fracture which can mimic distal biceps rupture. It would also help to rule out bony avulsion of the radial tuberosity which can be associated, although uncommonly, with distal biceps rupture.15
5.2. MRI
MRI is considered the gold standard for distal biceps pathologies. It should be able to diagnose partial tears, accurately measure the extent of tendon retraction in acute or chronic tears and visualise the lacertus fibrosus.16 An intact lacertus fibrosus would prevent significant retraction of the torn tendon. MRI is also useful to diagnose tendinosis which can be treated non-operatively.
It is recommended that the MRI of the elbow be performed with the elbow in flexion, shoulder in abduction and forearm in supination position (FABS protocol) for a better view of the distal biceps and other suspected abnormalities.16
MRI has better diagnostic accuracy than USG for diagnosing complete tear of the distal biceps whereas both MRI and USG have similar diagnostic accuracy for incomplete tear of the distal biceps. 17
5.3. Ultrasonography (USG)
USG is a reliable investigation to diagnose various pathologies of the distal biceps. However it is operator dependant. The distal biceps and lacertus fibrosis can be observed dynamically while stressing them with various provocative manoeuvres.16 USG is less expensive than MRI. USG is indicated in patients unable to have MRI either due to claustrophobia or any other contraindications.
USG can also be useful to diagnose any postoperative complications 2.
6. Natural history
Complete tear of the distal biceps results in weakness of the forearm supination, if not treated. Complete tear of the biceps associated with concomitant lacertus fibrosus tear leads to a significant proximal retraction of the torn tendon and might preclude primary repair after 4 weeks. However; primary repair may still be feasible at 3 months if the lacertus fibrosus is intact and there is no significant proximal retraction of the torn tendon. Delayed presentation or neglected chronic complete rupture of the distal biceps usually requires reconstructive procedure.
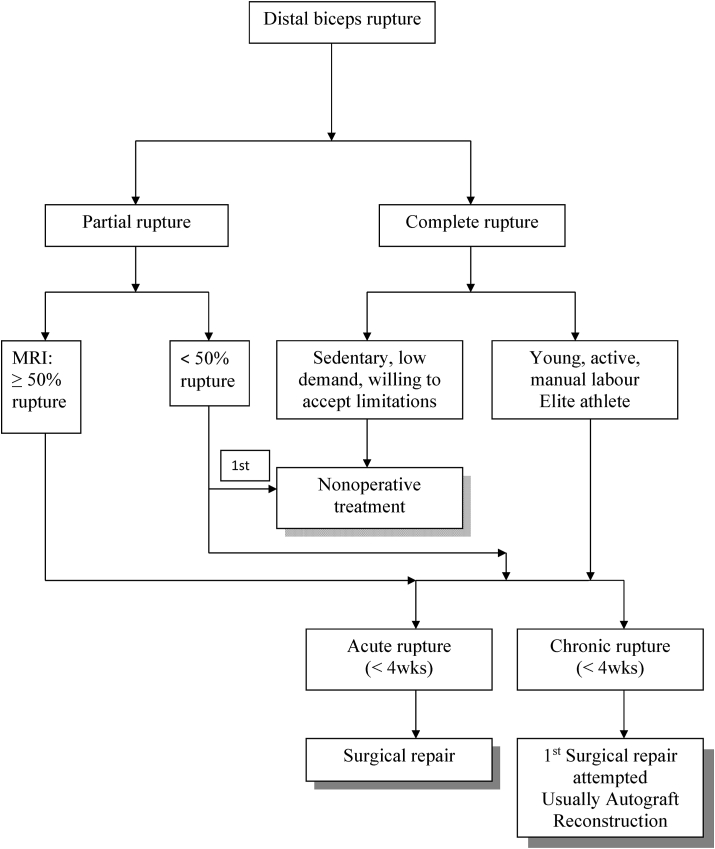
7. Treatment [Fig. 4]
Fig. 4.
Shows the treatment algorithm for management of distal biceps tendon ruptures.
7.1. Partial tears
7.1.1. Non-operative treatment
Non-operative treatment is recommended for incomplete ruptures affecting less than 50% of the biceps tendon.
7.1.2. Operative treatment
The indications for operative intervention are symptomatic partial tears of the distal biceps affecting >50% of the biceps tendon thickness 18 and failure of non-operative treatment for partial tears of <50% of the tendon thickness.
Operative techniques include tendon debridement leading to complete transection of the distal biceps insertion followed by internal fixation of the biceps to its native footprint.
A systematic review reported consistent good outcome after fixation for incomplete transection of distal biceps tendon19 but the evidence is of low quality because included studies were either case reports or case series.
7.2. Acute complete tears
Less than 4 weeks old tears are considered acute tears. 20
7.2.1. Non-operative treatment
Non-operative treatment for complete tears is recommended for elderly patients (>65 years) with low functional demand, for younger patients who are medically unfit or patients unwilling to have surgery. Patients should be informed of the likely weakness of supination causing limitation in recreational and occupational activities if the tear is not repaired.
It is important that patients making an informed choice regarding long term implications of non-operative treatment of distal biceps tear. Morrey and Nesterenko have reported that in patients not undergoing surgical intervention, the mean loss of maximal supination strength was 40–50% and the mean loss of maximal elbow flexion strength was 30% compared to the opposite normal extremity.21,22 It may appear significant loss of strength. However Freeman et al. found that in spite of loss of strength, patients treated non-operatively have satisfactory functional outcome with slight weakness in supination but insignificant weakness of elbow flexion.23
The first phase of conservative treatment is the phase of immobilization using either shoulder arm immobilizer or above elbow plaster slab for three to six weeks depending on the severity of pain. Shoulder arm immobilizer is preferred because it allows ice application in case of severe swelling and ecchymosis. Non Steroidal Anti-Inflammatory Drugs (NSAIDs) are given during the initial weeks of immobilization. Once pain and swelling settles, gentle active elbow flexion and extension exercises are commenced in supine position to reduce the effect of gravity. Active elbow flexion against gravity in sitting and standing position are commenced after three months. Active lifting of heavy weight will need to be delayed for six months after the commencement of treatment.
7.2.2. Operative treatment
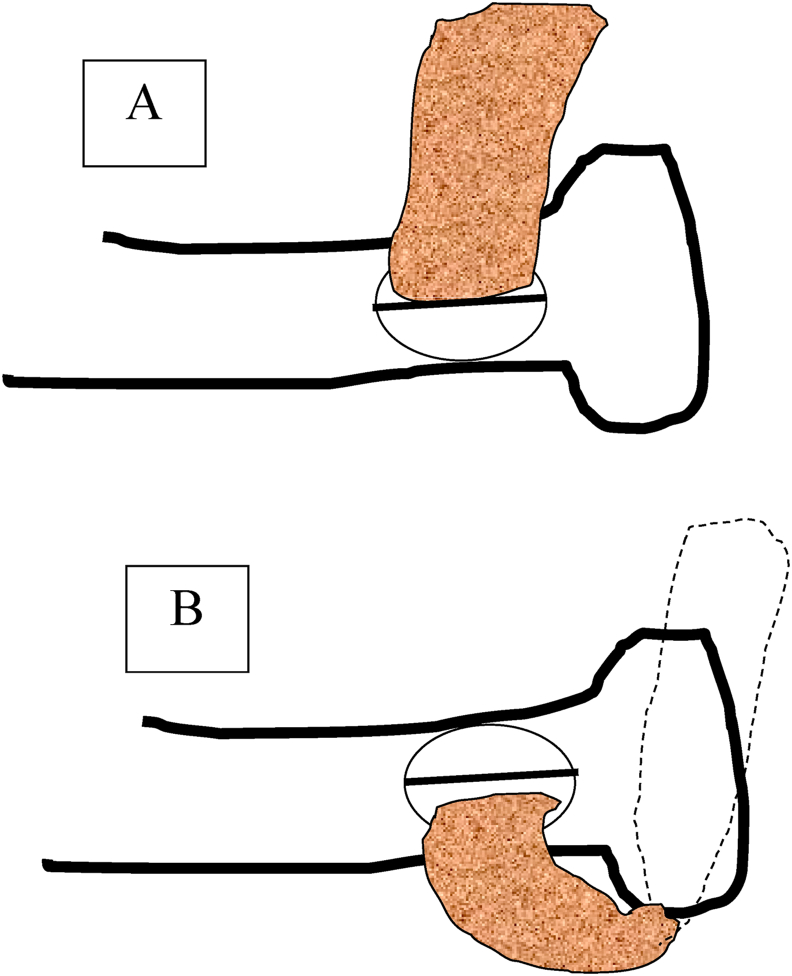
Operative treatment is recommended for acute complete tear in the young, medically fit patients. It aims to internally fix the torn tendon to its anatomical footprint, posterior to the apex of the radial tuberosity [Fig. 5]. This can be achieved either by a single anterior incision or two incisions.
Fig. 5.
Shows schematic diagram of non-anatomic repair (A) and anatomic repair (B).
Single incision technique is easier to perform but is likely to lead to a non-anatomical repair of the tendon, slightly anterior to its footprint on the radial tuberosity [Fig. 5]. There are reports that non-anatomical repair reduces the force of supination as demonstrated in cadaver biomechanical studies.24,25The single incision approach is performed using either a limited anterior approach or an extensile anterior approach. The limited anterior approach involves making a single transverse incision traversing between the pronator teres and brachioradialis. The extensile anterior approach entails using the lazy S incision over the cubital fossa.
The double incision approach entails the use of both anterior approach and the posterolateral approaches. The ruptured distal biceps is reattached to its native footprint using suture passage through tunnels in the bone, cortical endobuttons, interference screw or suture anchors.
Functional outcome is similar while using either single or double incision technique.26
There was no difference in the elbow range of motion using any of the surgical approaches or any of fixation methods.27
The overall incidence of complications including major complications after surgical repair based on pooled estimate is 25% and 5% respectively.28 Lateral Ante Brachial cutaneous nerve (LABC nerve) injury was most commonly observed with the limited anterior approach and extensile anterior approach most commonly led to superficial branch of the radial nerve injury.28 Synostosis between the proximal radius and ulna occurs with the double incision approach.28 Fortunately, majority of the injuries to the LABC nerve are neuropraxia and spontaneously recovered1. A systematic review reported significantly higher incidence of failure of primary repair and neural injury with the anterior incision approach whereas heterotopic ossification was most commonly reported from double incision approach.29
Patients are able to return to work between 3 and 4 months after surgical repair.30
A feasibility study on cadavers using endoscopic technique for biceps repair was reported using three portals (parabiceps, mid-biceps and distal anterior) and suture anchors for footprint fixation31 but clinical studies are lacking.
7.3. Chronic complete tear
Injuries longer than 4 weeks duration are considered chronic tears.32
7.3.1. Conservative treatment
Non-operative treatment is recommended for non-compliant or unwilling patients. They should be informed of the possible functional deficit of leaving the tendon unrepaired.
7.3.2. Operative treatment
Primary repair may not be possible in the cases of chronic rupture due to tendon retraction and scarring of the ruptured tendon to the surrounding tissues. Though primary repair should be attempted, significant tendon retraction would necessitate reconstructive procedures. Options for reconstruction include the use of autograft (Palmaris longus, flexor carpi radialis, semitendinosus, latissimus dorsi tendon transfer, gracilis free functioning muscle transfer) or the use of allograft (tendoachilles).33
Studies comparing reconstruction procedures with primary repair have remained inconclusive with few authors suggesting better outcomes with primary repair34 and others reporting equivalent outcome and morbidity with repair and reconstruction. 35
8. Conclusion
High index of suspicion is needed to diagnose this significant soft tissue injury because initial radiographs would be normal. Thorough clinical examination using a combination of clinical tests would point to the diagnosis of full or partial thickness biceps tear. The resisted hook test and the newly described distal biceps provocation test are helpful clinical tests to diagnose partial thickness biceps tear. MRI is the investigation of choice. Operative intervention is indicated for full thickness tears and persistently symptomatic partial tears in spite of non-operative treatment. Unwilling or unsuitable patients should be offered non-operative treatment. Although it is unlikely to restore the strength of biceps, its functional outcome is reasonable.
Funding source
Nil
Distal biceps injuries
Evaluation and management
Declaration of competing interest
None declared.
References
- 1.Garon M.T., Greenberg J.A. Complications of distal biceps repair. Orthop Clin N Am. 2016;47(2):435–444. doi: 10.1016/j.ocl.2015.10.003. [DOI] [PubMed] [Google Scholar]
- 2.Créteur V., Madani A., Sattari A., El Kazzi W., Bianchi S. Ultrasonography of complications in surgical repair of the distal biceps brachii tendon. J Ultrasound Med. 2019;38(2):499–512. doi: 10.1002/jum.14707. [DOI] [PubMed] [Google Scholar]
- 3.Kelly M.P., Perkinson S.G., Ablove R.H., Tueting J.L. Distal biceps tendon ruptures: an epidemiological analysis using a large population database. Am J Sports Med. 2015;43(8):2012–2017. doi: 10.1177/0363546515587738. [DOI] [PubMed] [Google Scholar]
- 4.Luokkala T., Sidharthan S.K., Karjalainen T.V., Paloneva J., Watts A.C. Distal biceps tendon repairs and reconstructions-an analysis of demographics, prodromal symptoms and complications. Arch Orthop Trauma Surg. 2021 Jan 23 doi: 10.1007/s00402-021-03750-1. [DOI] [PubMed] [Google Scholar]
- 5.Idler C.S., Montgomery W.H., 3rd, Lindsey D.P., Badua P.A., Wynne G.F., Yerby S.A. Distal biceps tendon repair: a biomechanical comparison of intact tendon and 2 repair techniques. Am J Sports Med. 2006;34(6):968–974. doi: 10.1177/0363546505284185. [DOI] [PubMed] [Google Scholar]
- 6.Shukla D.R., Morrey B.F., Thoreson A.R., An K.N., O'Driscoll S.W. Distal biceps tendon rupture: an in vitro study. Clin Biomech. 2012;27(3):263–267. doi: 10.1016/j.clinbiomech.2011.09.010. [DOI] [PubMed] [Google Scholar]
- 7.O'Driscoll S.W., Goncalves L.B., Dietz P. The hook test for distal biceps tendon avulsion. Am J Sports Med. 2007;35(11):1865–1869. doi: 10.1177/0363546507305016. [DOI] [PubMed] [Google Scholar]
- 8.Pallante G.D., O'Driscoll S.W. Return of an intact hook test result: clinical assessment of biceps tendon integrity after surgical repair. Orthop J Sports Med. 2019;7(2) doi: 10.1177/2325967119827311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Devereaux M.W., El Maraghy A.W. Improving the rapid and reliable diagnosis of complete distal biceps tendon rupture: a nuanced approach to the clinical examination. Am J Sports Med. 2013;41(9):1998–2004. doi: 10.1177/0363546513493383. [DOI] [PubMed] [Google Scholar]
- 10.Ruland R.T., Dunbar R.P., Bowen J.D. The biceps squeeze test for diagnosis of distal biceps tendon ruptures. Clin Orthop Relat Res. 2005;437:128–131. doi: 10.1097/01.blo.0000167668.18444.f5. [DOI] [PubMed] [Google Scholar]
- 11.El Maraghy A., Devereaux M. The "bicipital aponeurosis flex test": evaluating the integrity of the bicipital aponeurosis and its implications for treatment of distal biceps tendon ruptures. J Shoulder Elbow Surg. 2013;22(7):908–914. doi: 10.1016/j.jse.2013.02.005. [DOI] [PubMed] [Google Scholar]
- 12.Metzman L.S., Tivener K.A. The supination-pronation test for distal biceps tendon rupture. Am J Orthop (Belle Mead NJ) 2015;44(10):361–364. [PubMed] [Google Scholar]
- 13.El Maraghy A., Devereaux M., Tsoi K. The biceps crease interval for diagnosing complete distal biceps ruptures. Clin Orthop Relat Res. 2008;466(9):2255–2262. doi: 10.1007/s11999-008-0334-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Caekebeke P., Schenkels E., Bell S.N., van Riet R. Distal biceps provocation test. J Hand Surg Am. 2021 Mar 20;S0363–5023(21) doi: 10.1016/j.jhsa.2020.12.012. 00005-8. [DOI] [PubMed] [Google Scholar]
- 15.Sutton K.M., Dodds S.D., Ahmad C.S., Sethi P.M. Surgical treatment of distal biceps rupture. J Am Acad Orthop Surg. 2010;18(3):139–148. doi: 10.5435/00124635-201003000-00003. [DOI] [PubMed] [Google Scholar]
- 16.Nguyen M.L., Rosenthal J., Karas S. A comprehensive review of the normal, abnormal, and post-operative MRI appearance of the distal biceps brachii. Skeletal Radiol. 2020;49(11):1695–1707. doi: 10.1007/s00256-020-03501-0. [DOI] [PubMed] [Google Scholar]
- 17.Lynch J., Yu C.C., Chen C., Muh S. Magnetic resonance imaging versus ultrasound in diagnosis of distal biceps tendon avulsion. Orthop Traumatol Surg Res. 2019;105(5):861–866. doi: 10.1016/j.otsr.2019.01.021. [DOI] [PubMed] [Google Scholar]
- 18.Bauer T.M., Wong J.C., Lazarus M.D. Is nonoperative management of partial distal biceps tears really successful? J Shoulder Elbow Surg. 2018;27(4):720–725. doi: 10.1016/j.jse.2017.12.010. [DOI] [PubMed] [Google Scholar]
- 19.Behun M.A., Geeslin A.G., O'Hagan E.C., King J.C. Partial tears of the distal biceps brachii tendon: a systematic review of surgical outcomes. J Hand Surg Am. 2016;41(7):175–189. doi: 10.1016/j.jhsa.2016.04.019. [DOI] [PubMed] [Google Scholar]
- 20.Ramsey M.L. Distal biceps tendon injuries: diagnosis and management. J Am Acad Orthop Surg. 1999;7(3):199–207. doi: 10.5435/00124635-199905000-00006. [DOI] [PubMed] [Google Scholar]
- 21.Morrey B.F., Askew L.J., An K.N., Dobyns J.H. Rupture of the distal tendon of the biceps brachii. A biomechanical study. J Bone Joint Surg Am. 1985;67(3):418–421. [PubMed] [Google Scholar]
- 22.Nesterenko S., Domire Z.J., Morrey B.F., Sanchez-Sotelo J. Elbow strength and endurance in patients with a ruptured distal biceps tendon. J Shoulder Elbow Surg. 2010;19:184–189. doi: 10.1016/j.jse.2009.06.001. [DOI] [PubMed] [Google Scholar]
- 23.Freeman C.R., McCormick K.R., Mahoney D., Baratz M., Lubahn J.D. Nonoperative treatment of distal biceps tendon ruptures compared with a historical control group. J Bone Joint Surg Am. 2009;91-A:2329–2334. doi: 10.2106/JBJS.H.01150. [DOI] [PubMed] [Google Scholar]
- 24.Hansen G., Smith A., Pollock J.W. Anatomic repair of the distal biceps tendon cannot be consistently performed through a classic single-incision suture anchor technique. J Shoulder Elbow Surg. 2014;23(12):1898–1904. doi: 10.1016/j.jse.2014.06.051. [DOI] [PubMed] [Google Scholar]
- 25.Prud'homme-Foster M., Louati H., Pollock J.W., Papp S. Proper placement of the distal biceps during repair improves supination strength – a biomechanical analysis. J Shoulder Elbow Surg. 2015;24(4):527–532. doi: 10.1016/j.jse.2014.09.039. [DOI] [PubMed] [Google Scholar]
- 26.Castioni D., Mercurio M., Fanelli D., Cosentino O., Gasparini G., Galasso O. Single- versus double-incision technique for the treatment of distal biceps tendon rupture. Bone Joint Lett J. 2020;102(12):1608–1617. doi: 10.1302/0301-620X.102B12.BJJ-2020-0822.R2. [DOI] [PubMed] [Google Scholar]
- 27.Kodde I.F., Baerveldt R.C., Mulder P.G., Eygendaal D., van den Bekerom M.P. Refixation techniques and approaches for distal biceps tendon ruptures: a systematic review of clinical studies. J Shoulder Elbow Surg. 2016;25(2):29–37. doi: 10.1016/j.jse.2015.09.004. [DOI] [PubMed] [Google Scholar]
- 28.Amarasooriya M., Bain G.I., Roper T., Bryant K., Iqbal K., Phadnis J. Complications after distal biceps tendon repair: a systematic review. Am J Sports Med. 2020;48(12):3103–3111. doi: 10.1177/0363546519899933. [DOI] [PubMed] [Google Scholar]
- 29.Amin N.H., Volpi A., Lynch T.S. Complications of distal biceps tendon repair: a meta-analysis of single-incision versus double-incision surgical technique. Orthop J Sports Med. 2016;4(10) doi: 10.1177/2325967116668137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rubinger L., Solow M., Johal H., Al-Asiri J. Return to work following a distal biceps repair: a systematic review of the literature. J Shoulder Elbow Surg. 2020;29(5):1002–1009. doi: 10.1016/j.jse.2019.12.006. [DOI] [PubMed] [Google Scholar]
- 31.Bhatia D.N. Endoscopic repair of acute and chronic retracted distal biceps ruptures. J Hand Surg Am. 2016;41(12):e501–e507. doi: 10.1016/j.jhsa.2016.09.008. [DOI] [PubMed] [Google Scholar]
- 32.Tjoumakaris F.P., Bradley J.P. Distal biceps injuries. Clin Sports Med. 2020;39(3):661–672. doi: 10.1016/j.csm.2020.02.004. [DOI] [PubMed] [Google Scholar]
- 33.Srinivasan R.C., Pederson W.C., Morrey B.F. Distal biceps tendon repair and reconstruction. J Hand Surg Am. 2020;45(1):48–56. doi: 10.1016/j.jhsa.2019.09.014. [DOI] [PubMed] [Google Scholar]
- 34.Frank T., Seltser A., Grewal R., King G.J.W., Athwal G.S. Management of chronic distal biceps tendon ruptures: primary repair vs. Semitendinosus autograft reconstruction. J Shoulder Elbow Surg. 2019;28(6):1104–1110. doi: 10.1016/j.jse.2019.01.006. [DOI] [PubMed] [Google Scholar]
- 35.Hendy B.A., Padegimas E.M., Harper T. Outcomes of chronic distal biceps reconstruction with tendon grafting: a matched comparison with primary repair. JSES Int. 2020;5(2):302–306. doi: 10.1016/j.jseint.2020.10.023. [DOI] [PMC free article] [PubMed] [Google Scholar]