Abstract
Throughout the years, elbow arthroscopy has advanced tremendously due to improvements in technology and surgical techniques. It is now considered a safe and effective treatment for a variety of elbow disorders. Due to the small working space and nearby neurovascular structures, it is a technically challenging procedure. It can be used to successfully treat complaints caused by loose bodies, osteoarthritis, arthrofibrosis, OCD, lateral epicondylitis, VEOS and fractures. The most devastating complication of elbow arthroscopy is (permanent) nerve injury. Therefore, distortion of the anatomy of the elbow joint and transposition of the ulnar nerve can be a contra-indication for elbow arthroscopy due to the higher risk of postoperative complications. The results of the arthroscopy depend on the experience, knowledge, technique and expertise of the performing surgeon.
Keywords: Elbow, Elbow arthroscopy, Elbow disorders, Treatment elbow
1. Introduction
An arthroscopy of the elbow joint is a technically challenging surgical procedure due to the confined working space and the close proximity of neurovascular structures.1, 2, 3, 4 The first reports in 1931 even described that elbow arthroscopy was an unsafe procedure for those reasons.2,4,5However, increased knowledge of the anatomy of the elbow joint and tremendous advances in technology and surgical technique throughout the past decades, have made it a safe and effective treatment modality for various elbow disorders.2, 3, 4,6, 7, 8 Currently, elbow arthroscopy is being performed more frequently and for an increasing range of elbow pathologies.1,2,5, 6, 7,9,10
Compared to open elbow surgery, advantages of arthroscopy are: less scarring, decreased risk of infection, reduced postoperative pain and swelling, faster return to work and sports and improved visualization of the elbow joint.1,3,4,10 Nevertheless complications may still occur, due to the technical demands of the procedure.1, 2, 3, 4, 5, 6, 7, 8, 9, 10 Therefore a detailed patient history, physical examination and additional imaging studies are necessary for best possible outcomes.1,2,4,5
2. Indications
2.1. Loose bodies
Removal of loose bodies is the most common indication for arthroscopic intervention of the elbow.2,4,5 Loose bodies can be the result of trauma, degeneration or conditions such as osteochondritis dissecans and synovial chondromatosis, and are often chondral or osteochondral fragments.2,5 They can lead to locking symptoms when relatively small bodies temporarily slip into the joint; they can also cause a decreased end range of motion when relatively large.2,5 Not all loose bodies are symptomatic, so a thorough assessment is required to ascertain whether loose bodies that appear on imaging (see Fig. 1) are the cause of the patient's presenting problem. If so, removal is warranted. Arthroscopy is the preferred method as it is less invasive, but still allows a full and detailed assessment of the joint. This is necessary, as loose bodies can migrate through compartments of the elbow.2,5,11Additional procedures may also be needed as described below, depending on the underlying pathology causing the loose bodies.5,6
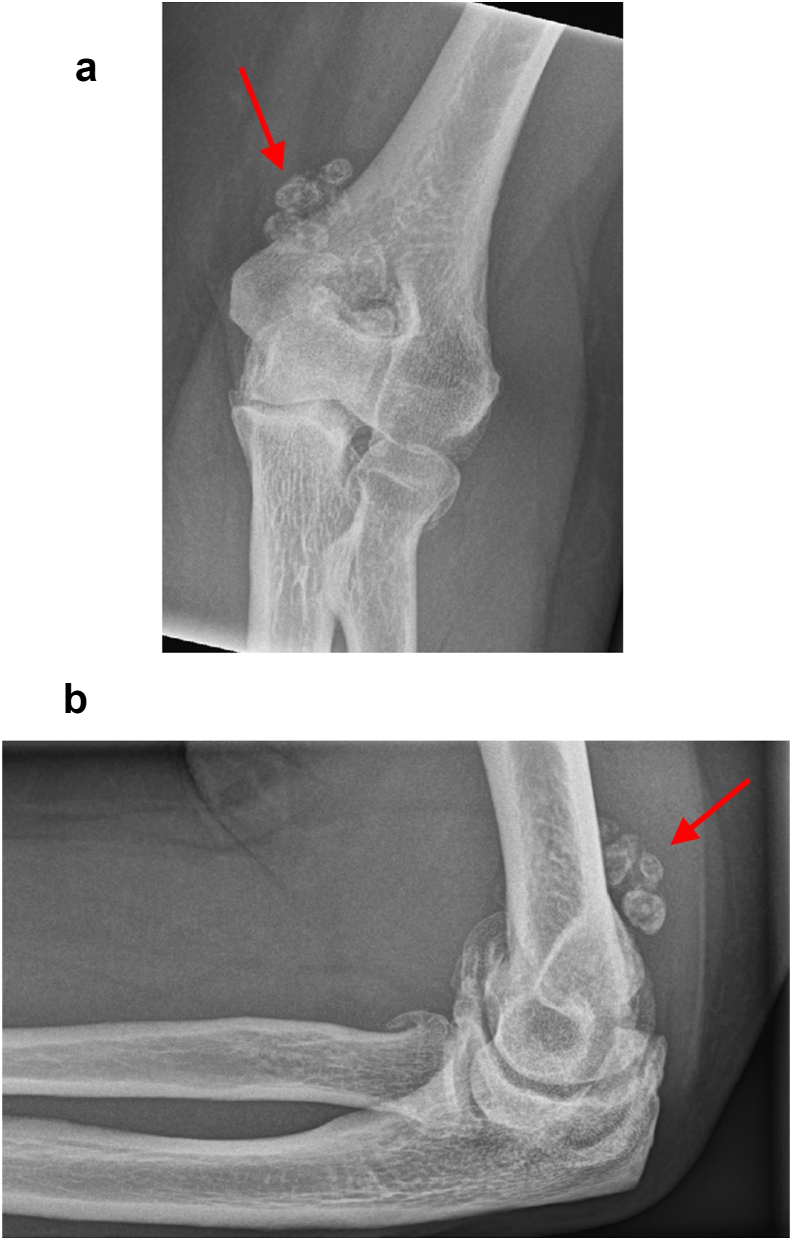
Fig. 1.
Patient with osteoarthritis. X-rays show osteophytes and loose bodies (arrow) in the elbow joint.
Removal of isolated loose bodies is the most successful arthroscopic intervention of the elbow with a success rate of 89%.2,5,9,11
2.2. Osteoarthritis
Although debridement of a degenerative joint surface per se is not indicated, it has been proven that removal of symptomatic osteophytes and loose bodies in the degenerative elbow (see Fig. 1) is an effective method to improve patient satisfaction and decrease pain at end range of motion for both flexion and extension.2,5, 6, 7,12,13 If there are capsular contractures, a release should be considered.5, 6, 7,12,13
In the early stages of osteoarthritis, arthroscopy can be especially successful, while its effectiveness is less predictable in advanced osteoarthritis.2,5 This appertains to both younger patients in which this condition can arise due to excessive use in sports (e.g. the boxer's elbow) and posttraumatic degeneration, and in elderly patients with posttraumatic or primary osteoarthritis.12,13 Desmoineaux et al. reported that 93.5% of patients with osteoarthritis were satisfied with the results of their arthroscopic surgery.12 This highlights an important difference in usefulness of arthroscopy of the elbow compared to other joints such as the knee, where it has been proven that debridement of a degenerate joint is generally ineffective.
2.3. Arthrolysis
Stiffness of the elbow has a variety of causes and can be divided in two main groups: post-traumatic (e.g. fractures, dislocations, burns) and non-traumatic (e.g. osteoarthritis, inflammatory arthritis, loose bodies, heterotopic ossifications and synovitis).5,14,15 Stiffness of the elbow can be a very debilitating condition, whereby the patient is no longer able to reach his own mouth or face, or when the elbow cannot be sufficiently extended for the completion of daily tasks such as riding a bike or reaching for objects. The inability to pronate can be a hindrance to activities of daily living such as using a keyboard, writing and other similar tasks, although some people can compensate for a mild protonation impairment by abducting and internally rotating their shoulder. This method of compensation is not possible for a supination deficit, which can cause problems when trying to touch the face or carrying a plate. The general agreement that an indication for surgery arises when there is an extension deficit of more than 30° or the inability to flex the elbow to at least 120°, or smaller deficiencies impairing a patient's lifestyle.14,15 However, this should not be used as a strict guideline: a thorough individual assessment of the presenting problems and the potential benefits of intervention should be done.14,15
When addressing a symptomatic stiff elbow joint, most can be treated arthroscopically by releasing the capsule, removing osteophytes when present and possibly remodeling parts of the joint that contribute to impingement in end range of motion.5,14
Although some authors have shown success with arthroscopic release of complex stiff elbows,5 a low threshold for an open arthrolysis is advised when dealing with extensive heterotopic ossifications, gross (posttraumatic) anatomic deformations or conditions where the ulnar nerve needs to be released. The latter specifically applies when treating a longstanding severe impairment where flexion is limited to 100° or less. While this condition could benefit from an open release of the posterior band of medial collateral ligament anyway, this would also allow for a release of the ulnar nerve ensuring safe tracking without traction injury due to scarring in the cubital tunnel. Extensive rotatory stiffness is also a relative indication for an open arthrolysis.15
2.4. Osteochondritis dissecans
Osteochondritis dissecans (OCD) is a condition which occurs when a segment of articular cartilage separates from the subchondral bone due to repetitive microtrauma to the epiphysis, which leads to local avascular necrosis.2,5,16, 17, 18 OCD typically presents in young patients engaged in overhead or upper extremity weight-bearing activities (e.g. baseball, weightlifting, gymnastics).2,5,16, 17, 18 Patients with OCD have complaints of pain, swelling, loss of extension or a locking sensation in the affected elbow.2,5,16, 17, 18
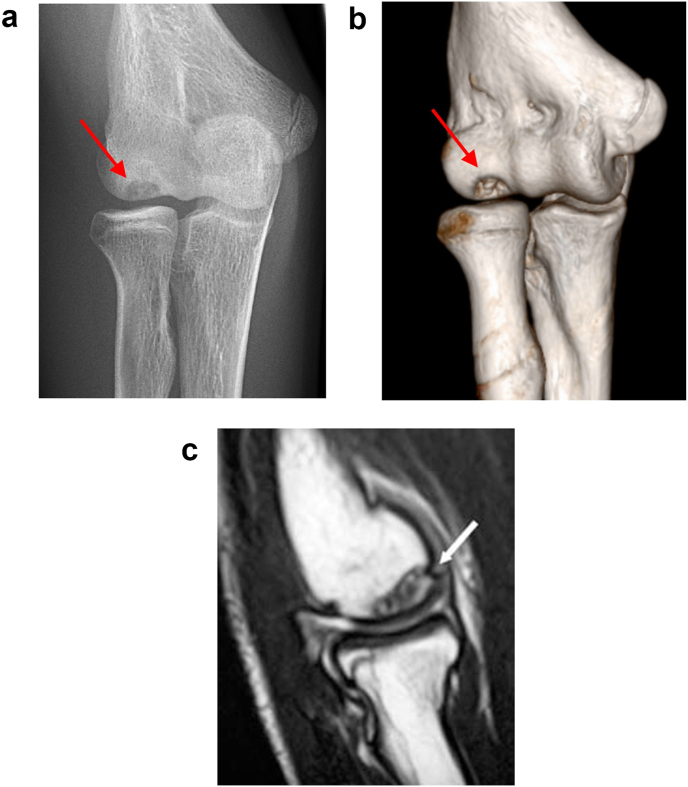
For the treatment of OCD, it is important to differentiate between stable and unstable lesions. A minority of patients present with a stable lesion that can heal with nonoperative treatment. These are characterized by a (near) normal range of motion, a capitellum with an open growth plate and only flattening or radiolucency of the subchondral bone on imaging. Patients with unstable OCD lesions have a decreased range of motion by 20° or more and a capitellum with a closed growth plate and fragmentation on MRI or CT scan (see Fig. 2a).16,17 Arthroscopic surgery is indicated when nonoperative treatment for a stable lesion has failed and for unstable lesions.2,5,16,17 The goal of the surgery is to remove the loose bodies and to perform a debridement on loose cartilage flaps (see Fig. 2b) with optional bone marrow stimulation. Large lesions and lesions with breaching of the lateral wall of the capitellum may warrant other forms of surgery such as (open) osteochondral autografting.2,4,5,16,17 Arthroscopic treatment has shown encouraging results with 80–90% of the patients returning to sports at their pre-injury level.16,18
Fig. 2.
Osteochondritis dissecans. A) x-ray showing an OCD lesion of the capitellum, marked by arrow. B) CT-scan with 3D reconstruction shows an OCD lesion of the capitellum, marked by arrow. C) MRI showing an OCD lesion in the capitellum with cartilage flap and subchondral bone.
2.5. Lateral epicondylitis
In lateral epicondylitis the tendon of the extensor carpi radialis brevis (ECRB) is damaged through repetitive microtrauma, leading to chronic inflammation, tears and eventually a rupture of the tendon, causing pain on the lateral aspect of the elbow.2,5,19Although this condition is usually treated nonoperatively, some patients can be considered for surgical intervention when nonoperative measures have failed.2,5,7,19 Both open and arthroscopic techniques to release the ECRB and removal of the diseased portion of the tendon have been used with high rates of success.2,5, 6, 7 Arthroscopic release preserves the common extensor origin, permits a shorter rehabilitation program and faster return to work or sports compared to open release.2,5,7 Another advantage over open release is that arthroscopy allows further intra-articular examination of other pathology.2,5 Relative contra-indications for an arthroscopic release include elbow instability or radial nerve syndrome. These patients are more effectively treated with open surgery to stabilize the elbow or decompression of the nerve in the same session.19 The long-term results of open treatment of epicondylitis lateralis are comparable to arthroscopic debridement with a success rate of approximately 70%.19
2.6. Valgus extension overload syndrome
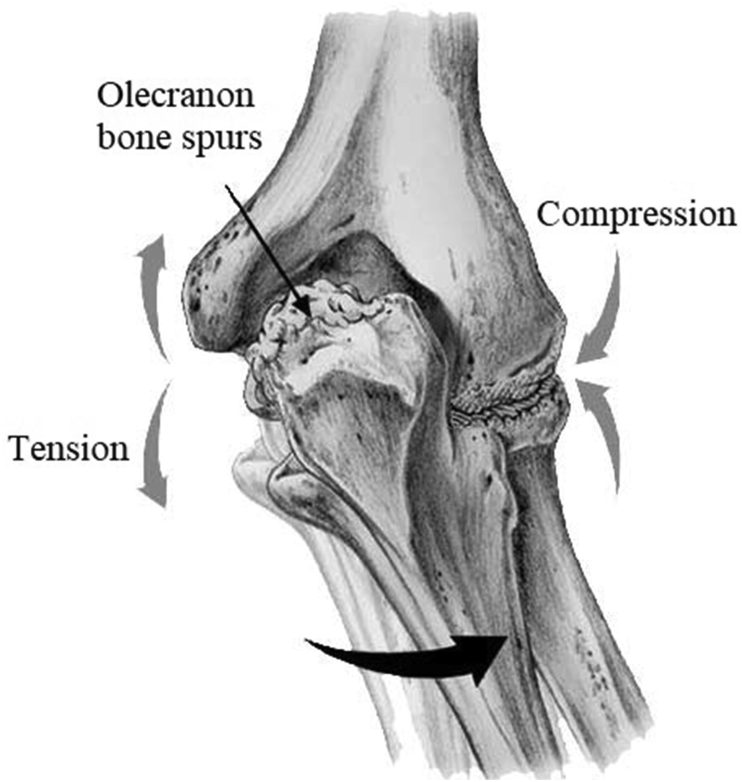
Valgus extension overload syndrome (VEOS) occurs mostly in the overhead throwing athletes and is also named ‘Pitcher's elbow’.2,20-22Laxity of the ulnar collateral ligament (UCL) leads to valgus instability of the elbow, ulnar nerve inflammation, tendinitis of the flexor pronator mass, apophysitis, OCD of the capitellum, trochlear chondromalacia, stress fractures of the olecranon and/or osteophyte formation and loose bodies in the posterior compartment of the elbow.2,5,20, 21, 22 Osteophytes and loose bodies in the posterior compartment of the elbow may lead to posteromedial impingement (see Fig. 3).20 Patients will complain of pain posterior or posteromedial, a feeling of instability on the medial side of the elbow during a throw, loss of extension and locking or catching.20, 21, 22
Fig. 3.
Valgus extension overload syndrome can lead to chondromalacia of the trochlea, stress fractures of the olecranon and osteophyte formation and eventually to loose bodies when it fractures.
Failure of nonoperative treatment for VEOS is an indication for arthroscopic surgery. The corner stone of surgery is debridement of pathologic osteophytes and removal of symptomatic loose bodies. During arthroscopy, the UCL should also be evaluated for insufficiency and repaired if indicated.2,5,20,22 After an intensive rehabilitation program, the return to sports at the same level in the motivated athlete is about 85%.20
2.7. Fractures
Arthroscopic surgery can be used for the debridement of small coronoid fractures to prevent loose body formation and malunion. Larger fracture fragment in one piece can be fixed with one or two screws, but these are rarely required as the trauma causing a coronoid fracture also tears the UCL which requires repair - under most circumstances with an open surgery.6
Minimally displaced radial head fractures with a single large fragment can be treated with arthroscopic surgery, however, good long-term results can also be achieved with nonoperative treatment in these situations.5,6
2.8. Contra-indications
A deformed elbow after trauma, skin grafts, burns, severe rheumatoid arthritis, previous elbow surgery or congenital deformities will make an elbow arthroscopy more challenging with a higher risk of postoperative complications.1,2,5,7,8 Therefore a detailed physical examination of the patient is required and any changes in anatomy must be noted.1 Due to the higher risk of complications, changes in the elbow anatomy are relative contra-indications for performing an elbow arthroscopy.1,2,5
Arthroscopic surgery should be avoided if the patient has a (sub)luxing ulnar nerve or a history of ulnar nerve transposition,1,2,5,8 unless the nerve can be easily identified during physical examination.7,8 Uncertainty concerning the exact anatomy of the ulnar nerve may lead to iatrogenic nerve injuries.1Alternatively, surgery should begin with an open approach to identify the ulnar nerve before proceeding with the arthroscopy.1
Lastly, the presence of soft tissue infection in the elbow and adjacent area is a contra-indication for elbow arthroscopy.2,5
3. Surgical techniques
An arthroscopy of the elbow is performed under general anesthesia. The advantage of general anesthesia over local anesthesia is the total muscle relaxation, patient comfort1,2,4, 5, 6,8,9 and the ability to perform neurological examination immediately after the procedure.2,4, 5, 6 We prefer to position the patient in a lateral decubitus position with the elbow in 90° flexion, but other possible positions are supine, suspended supine or prone position.1, 2, 3, 4, 5, 6, 7, 8, 9, 10
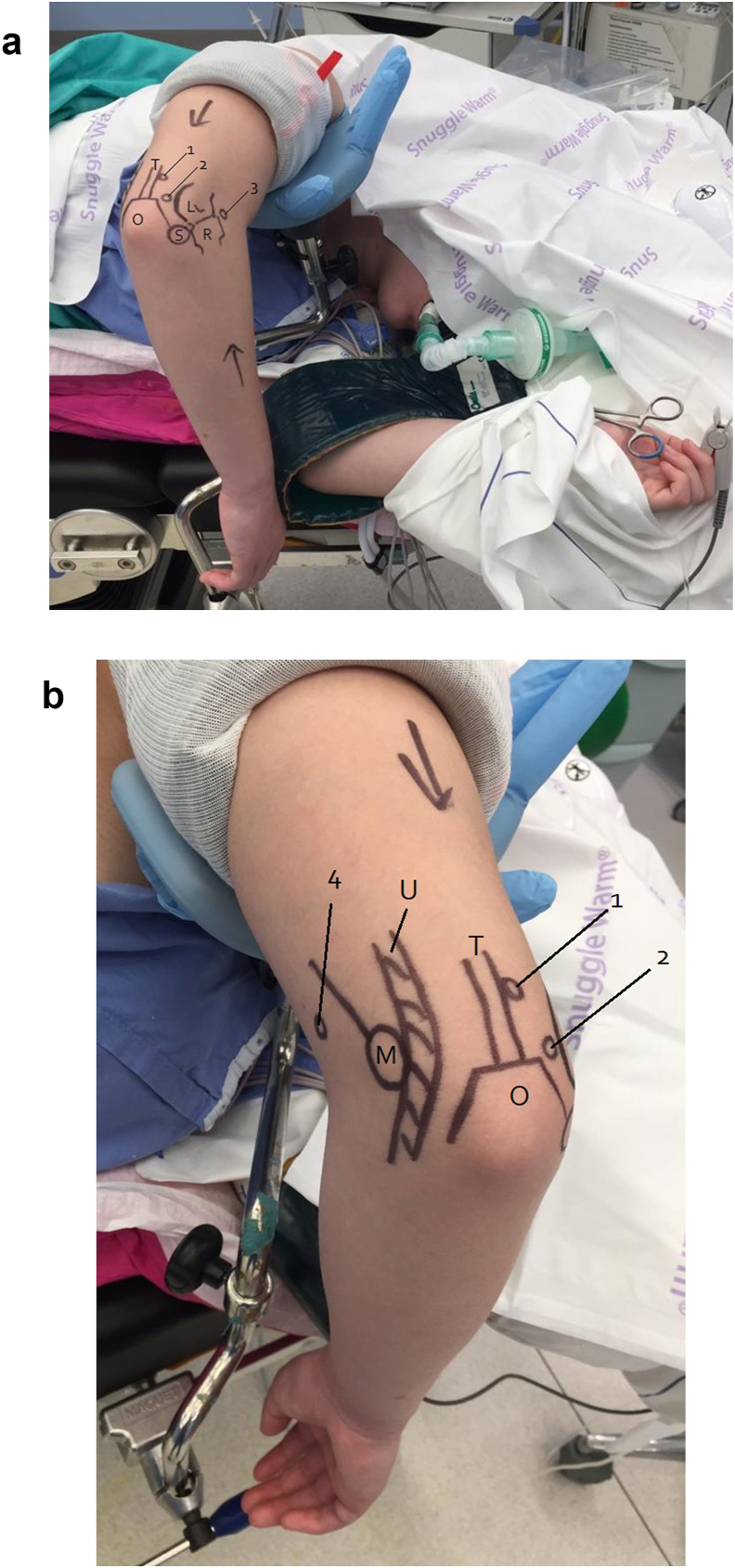
In the lateral decubitus position, the patient must have the upper arm of the affected side on a support small enough to leave the elbow itself completely free, thus avoiding external pressure on the anterior capsule, with the elbow in 90° flexion, allowing a full range of motion of the elbow. The shoulder should be forward elevated to 90°, allowing enough space for the arthroscope, even when visualising the ulnar side of the anterior compartment.1, 2, 3,5 A stable and comfortable patient position can be achieved with the use of a vacuum beanbag immobilizer.1 (see Fig. 4a and b).
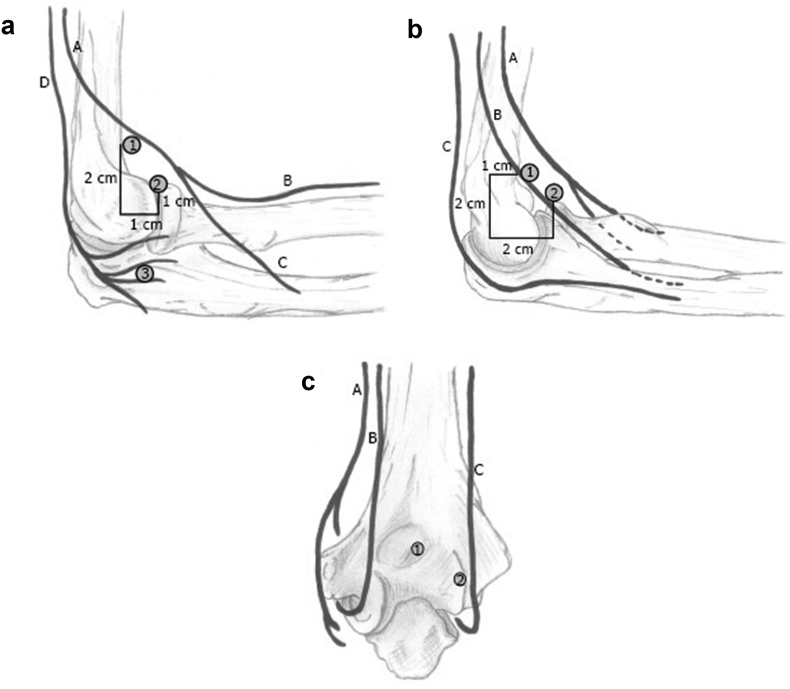
Fig. 4.
Patient lying in lateral decubitus position on a vacuum beanbag (pink) for an arthroscopy of the right elbow. Note that the elbow has a free range of motion and that there is enough space for the arthroscope on the axillary side. A) Anatomical landmarks and portals are shown from lateral view. B) Anatomical landmarks and portals are shown from medial view.
(L = lateral epicondyl, M = medial epicondyl, O = olecranon, R = radial head, S = soft spot,T = triceps, U = Ulnar nerve, 1 = straight posterior portal, 2 = posterolateral portal, 3 = anterolateral portal, 4 = anteromedial portal).
The elbow should then be examined under anesthesia on range of motion, stability and the position of ulnar nerve on both sides. The anatomical landmarks and portals should be marked.1,3,5,8 This includes the central band of the triceps, the medial and lateral epicondyle, radial head and the course of the ulnar nerve (see Fig. 4a and b).1,3
After disinfection and sterile draping, the arm is exsanguinated using an sterile elastic bandage beginning at the hand, up to the level of the tourniquet. The tourniquet is inflated (usually to about 250 mmHg) and the elastic bandage is partly removed, leaving the proximal one third of the forearm free.3,8 The joint is distended by injecting 20–30 mL of saline into the fossa olecrani or the “soft spot”, which is the center of the triangle formed by the lateral epicondyle, olecranon and radial head.1, 2, 3,5,8 Successful injection of the fluid will cause bulging of the posterolateral corner of the elbow, and eventually extend the elbow and move the neurovascular structures together with the anterior capsule away from the joint surface. It should be noted that distention of the elbow does not change the distance between the capsule and nerves.1,2,5,8
3.1. Anterior compartment
A stab incision is made about one cm anterior and two cm proximal of the medial epicondyle. Palpating the medial intermuscular septum should confirm that the portal is indeed anterior to it. A skin-only incision is used to avoid inadvertent damage to the branches of the medial antebrachial cutaneous nerve. A curved clamp with the tip pointing in an anterior direction to locate the distal humerus and achieve a smooth pathway to the anterior side of the joint. It is followed by the insertion of the trocar in the same direction, pointing towards the joint. To achieve penetration of the joint capsule without losing contact with the anterior surface of the humerus, the forearm can be lifted up slightly during this part of the procedure. Arthroscope is inserted through this portal which acts as initial viewing portal.
The next portal can be made under direct arthroscopic vision with a needle inserted from the lateral side to confirm proper placement. If the tip of the needle enters at the level of the radiocapitellar joint, is not too anterior (thus not close to the posterior interosseous nerve) and can easily reach the coronoid, proper portal placement is ensured and the incision is made.
A hooded shaver is then used to perform the synovectomy from the lateral (working) portal, making sure not to use suction at the anterior part of the capsule at the level of the radial head where the posterior interosseous nerve is at risk. Ulnar side of the joint should be thoroughly inspected for loose bodies. Next, the osteophytes at the tip of the coronoid process causing flexion impingement can be removed.
For arthroscopic release of the anterior capsule the classic technique is to use arthroscopic tools to incise the capsule just proximal to the radial head. However, in our institute, we prefer to use an alternative technique: an accessory portal is made at the level of the anterior capsule on the lateral side where it attaches to the distal humerus. Using this portal, the first part of the release is performed using a scalpel and shaver. The release is then completed by tearing the anterior capsule loose, using an introducer or switching stick. After each swiping movement a visual check is performed until no more attachments of the capsule are visible and the brachial muscle is seen across the entire visual field. A gentle manipulation into full extension will complete a full release.2,3,5,7, 8, 9, 10 (See Fig. 6a and b).
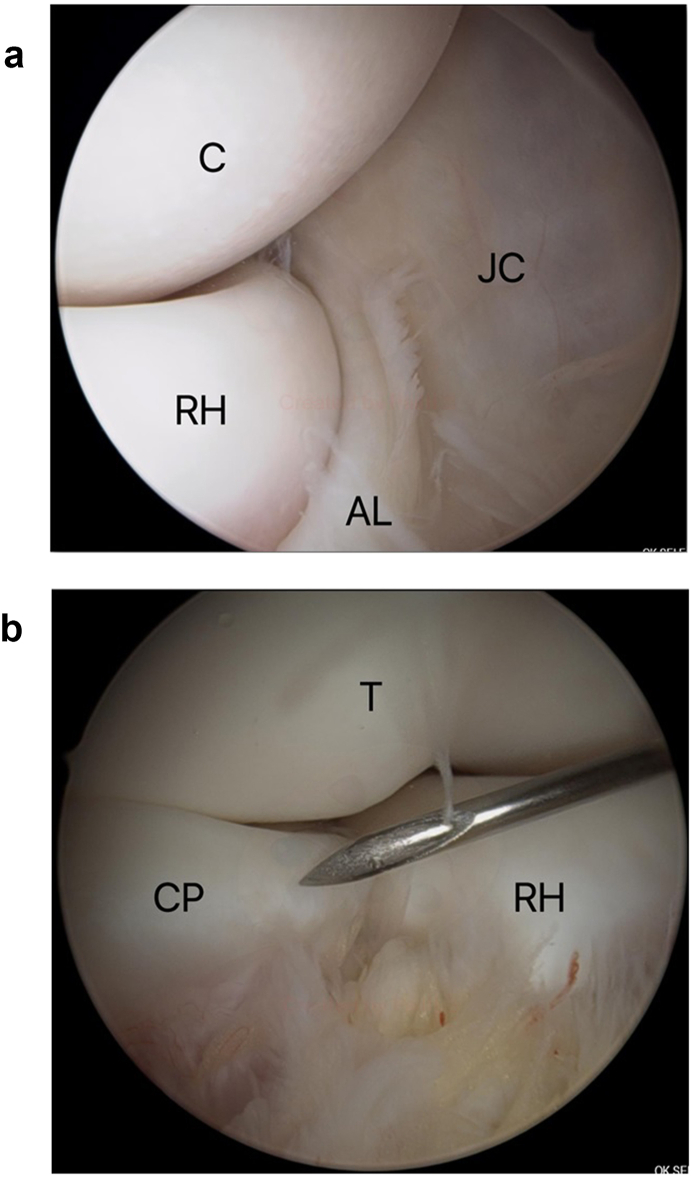
Fig. 6.
Arthroscopic view of the anterior compartment of the elbow. A) View from the anteromedial portal. (AL = Annular ligament, C = Capitellum, JC = Joint capsule, RH = Radial head). B) View from the anteromedial portal. (CP = Coronoid process, RH = Radial head, T = Trochlea).
3.2. Posterior compartment
For the posterior central portal, an incision is made over the fossa olecrani, 3 cms proximal to the tip of olecranon while avoiding damage to the central band of the triceps. Posterior lateral portal is created by making an incision at the radial side of the tip of the olecranon in such a way that both the fossa olecrani and the posterolateral space (at a later stage) can be reached from this portal.
The arthroscope is introduced from the posterior central portal, while the shaver is introduced from the posterolateral portal. After clearing the fossa from tissue to establish a good view, loose bodies can be removed. Working distally the tip of the olecranon is then visualized (see Fig. 7). If indicated osteophytes are removed. It is worthwhile to note that posterior impingement is caused not just by the osteophytes at the tip but mostly by a posteromedial and posterolateral osteophytic facet. Observing the distal humerus and tip of olecranon for impingement in extension would clarify which parts of the distal humerus should be debrided with a burr to ensure optimal extension of the joint. Quite often, loose bodies are hidden in the medial and lateral gutter so they must be checked. It usually helps to use an instrument such as a tissue retractor when performing this step.2,3,5,7, 8, 9, 10
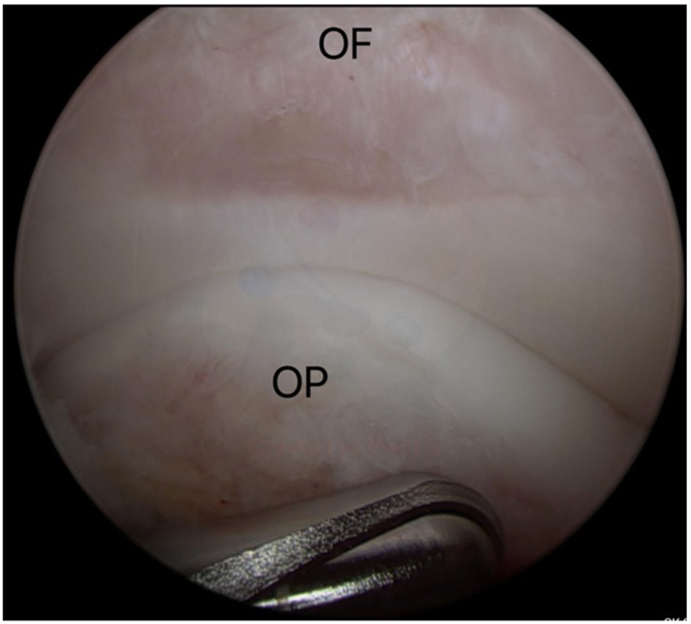
Fig. 7.
Posterior compartment of the elbow through arthroscopic view. (OF = Olecranonfossa, OP = Olecranon process).
3.3. Posterolateral compartment
The posterior lateral portal is used as a viewing portal and arthroscope is inserted in a blind fashion. It is usually helpful to slightly extend the elbow during this step so as to prevent the arthroscope ending up in the subcutaneous layer. The posterolateral compartment is sometimes immediately visible, but in other cases abundant synovial tissue may obscure a clear view. The working portal is then established at the soft spot. The blade must be aimed at a 45° angle with respect to the posterior plane of the olecranon to minimise the risk of damaging the joint surface. A curved clamp can then be used to penetrate the capsule, which is confirmed by a popping sensation and the outflow of joint fluid. Next the shaver is used to establish a clear view.
Through this portal, the radial head, the proximal radioulnar joint, and the ulnohumeral joint can be assessed (See Fig. 8). Osteochondritis dissecans lesions of the capitellum can also be visualized and treated using these portals.7, 8, 9, 10
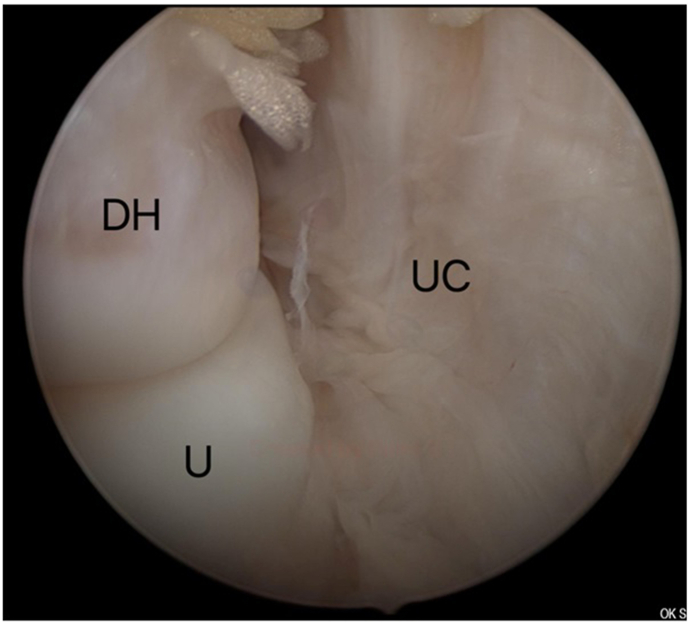
Fig. 8.
Posterolateral compartment of the elbow. (DH = Distal humerus, U = Ulna, UC = Ulnar capsule).
4. Complications
Complications mostly occur in patients with distorted anatomy of the elbow joint.3,7One of the most devastating and commonly occurring complications of elbow arthroscopy is injury to nerves.1, 2, 3, 4, 5,7,8,10 Table 1 and Fig. 5 shows the proximity of nerves to the portals. Fortunately, the majority of such complications are transient neuropraxias.1, 2, 3, 4,8 Injury can be caused by a sharp penetration through the subcutaneous tissue, compression from a cannula, fluid extravasation or the use of local anesthetics.2,5,8 The prevalence of nerve injury in the current literature after arthroscopy is 0–14%,1 which is believed to be understated.1,7
Table 1.
Overview of portal placement in elbow arthroscopy. Different portals are needed depending on the indication and goal of the arthroscopy.2,3,5,7, 8, 9, 10
| Portal | Location | Visualization | Nearby nerves (distance) |
|---|---|---|---|
| Anterolateral | 2 cm anterior and 3 cm proximal to the lateral epicondyle | - Medial capsule - Medial plica - Distal humerus - Coronoid process and fossa - Trochlea |
- Radial nerve (3 mm) - Posterior antebrachial cutaneous nerve (2 mm) - Posterior interosseous nerve (1–13 mm) |
| Anteromedial | 2 cm anterior and 2 cm distal to the medial epicondyle | - Radiocapitellar joint - Ulnohumeral joint - Coronoid fossa - Capitellum - Superior capsule |
- Medial antebrachial cutaneous nerve (6 mm) - Median nerve (7–14 mm) - Ulnar nerve (21 mm) |
| Proximal medial | 2 cm proximal and 1–2 cm anterior to the medial epicondyle | - Anterior compartment - Radiocapitellar joint |
|
| Posterolateral | 3 cm proximal to the tip of the olecranon, near the lateral margin of the triceps | - Olecranon fossa and tip - Posterior trochlea |
- Medial antebrachial cutaneous nerve (25 mm) - Posterior antebrachial cutaneous nerve (25 mm) |
| Straight lateral | Soft spot: center of the triangle formed by the lateral epicondyle, olecranon and radial head | - Posterior capitellum - Radioulnar joint |
- Posterior antebrachial cutaneous nerve (7 mm) |
| Straight posterior | 3 cm proximal to the olecranon tip | - Posterior elbow joint - Olecranon osteophytes |
- Posterior antebrachial cutaneous nerve (23 mm) - Ulnar nerve (25 mm) |
Fig. 5.
Proximity of nerves and portals. A) Lateral view (A. Radial nerve, B. Superficial branch, C. Deep branch, D. Posteriorantebrachial cutaneous nerve, 1. Proximal lateral portal, 2. Anterolateral portal, 3. Midlateral portal). B) Medial view (A. Median nerve, B. Medial antebrachial cutaneous nerve, C. Ulnarnerve, 1. Proximal medial portal, 2. Anteromedial portal). C) Posterior view (A. Medial antebrachial cutaneous nerve, B. Ulnar nerve, C. Posteriorantebrachial cutaneous nerve, 1. Straight posterior portal, 2. Posterolateral portal).
Other complications include wound infection, ganglion formation, heterotopic ossifications, cartilage damage and complex regional pain syndrome.1, 2, 3, 4, 5,8,10 Persistent drainage of synovial fluid from the portals site and the formation of synovial fistula can be prevented by closing the portals with a suture.6,7
Complications can be reduced by careful patient selection, a detailed examination, correct indication, and through the experience, knowledge, technique and expertise of the surgeon.2,5,8
5. Conclusion
Elbow arthroscopy is a technically demanding procedure but is a safe and effective modality to treat various elbow pathologies if performed carefully. A successful surgical outcome and the prevention of complications is dependent upon an thorough understanding of the relevant anatomy and pathology. Although many conditions can be treated with an elbow arthroscopy, the surgeon must keep an open mind for using an open approach, if necessary.
CRediT authorship contribution statement
Chow HY: Writing – original draft, Writing – review & editing, Visualization. Eygendaal D: Supervision, Writing – review & editing, Visualization. The B: Corresponding author, Supervision, Conceptualization, Writing – review & editing, Visualization.
Declaration of competing interest
None.
References
- 1.Hilgersom N.F., Oh L.S., Flipsen M., Eygendaal D., van den Bekerom M.P. Tips to avoid nerve injury in elbow arthroscopy. World J Orthoped. 2017;8(2):99–106. doi: 10.5312/wjo.v8.i2.99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dodson C.C., Nho S.J., Williams R.J., 3rd, Altchek D.W. Elbow arthroscopy. J Am Acad Orthop Surg. 2008;16(10):574–585. doi: 10.5435/00124635-200810000-00003. [DOI] [PubMed] [Google Scholar]
- 3.Elfeddali R., Schreuder M.H., Eygendaal D. Arthroscopic elbow surgery, is it safe? J Shoulder Elbow Surg. 2013;22(5):647–652. doi: 10.1016/j.jse.2013.01.032. [DOI] [PubMed] [Google Scholar]
- 4.Matsuura T., Egawa H., Takahashi M. State of the art: elbow arthroscopy: review of the literature and application for osteochondritis dissecans of the capitellum. J Med Invest. 2014;61(3-4):233–240. doi: 10.2152/jmi.61.233. [DOI] [PubMed] [Google Scholar]
- 5.Baker C.L., Jr., Jones G.L. Arthroscopy of the elbow. Am J Sports Med. 1999;27(2):251–264. doi: 10.1177/03635465990270022401. [DOI] [PubMed] [Google Scholar]
- 6.Steinmann S.P. Elbow arthroscopy: where are we now? Arthroscopy. 2007;23(11):1231–1236. doi: 10.1016/j.arthro.2007.08.008. [DOI] [PubMed] [Google Scholar]
- 7.Adams J.E., King G.J., Steinmann S.P., Cohen M.S. Elbow arthroscopy: indications, techniques, outcomes, and complications. Instr Course Lect. 2015;64:215–224. [PubMed] [Google Scholar]
- 8.Bennett J.M. Elbow arthroscopy: the basics. J Hand Surg Am. 2013;38(1):164–167. doi: 10.1016/j.jhsa.2012.10.023. [DOI] [PubMed] [Google Scholar]
- 9.Andrews J.R., Carson W.G. Arthroscopy of the elbow. Arthroscopy. 1985;1(2):97–107. doi: 10.1016/s0749-8063(85)80038-4. [DOI] [PubMed] [Google Scholar]
- 10.Brach P., Goitz R.J. Elbow arthroscopy: surgical techniques and rehabilitation. J Hand Ther. 2006;19(2):228–236. doi: 10.1197/j.jht.2006.02.013. [DOI] [PubMed] [Google Scholar]
- 11.Ogilvie-Harris D.J., Schemitsch E. Arthroscopy of the elbow for removal of loose bodies. Arthroscopy. 1993;9(1):5–8. doi: 10.1016/s0749-8063(05)80335-4. [DOI] [PubMed] [Google Scholar]
- 12.Desmoineaux P., Carlier Y., Mansat P., Bleton R., Rouleau D.M., Duparc F. Arthroscopic treatment of elbow osteoarthritis. Orthop Traumatol Surg Res. 2019;105(8S):S235–S240. doi: 10.1016/j.otsr.2019.09.003. [DOI] [PubMed] [Google Scholar]
- 13.Sochacki K.R., Jack R.A., 2nd, Hirase T. Arthroscopic debridement for primary degenerative osteoarthritis of the elbow leads to significant improvement in range of motion and clinical outcomes: a systematic review. Arthroscopy. 2017;33(12):2255–2262. doi: 10.1016/j.arthro.2017.08.247. [DOI] [PubMed] [Google Scholar]
- 14.Vieira L.A., Dal Molin F.F., Visco A. Arthroscopic treatment of elbow stiffness. Rev Bras Ortop. 2015;46(4):398–402. doi: 10.1016/S2255-4971(15)30251-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Evans P.J., Nandi S., Maschke S., Hoyen H.A., Lawton J.N. Prevention and treatment of elbow stiffness. J Hand Surg Am. 2009;34(4):769–778. doi: 10.1016/j.jhsa.2009.02.020. [DOI] [PubMed] [Google Scholar]
- 16.van Bergen C.J., van den Ende K.I., Ten Brinke B., Eygendaal D. Osteochondritis dissecans of the capitellum in adolescents. World J Orthoped. 2016;7(2):102–108. doi: 10.5312/wjo.v7.i2.102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lu Y., Li Y.J., Guo S.Y., Zhang H.L. Is there any difference between open and arthroscopic treatment for osteochondritis dissecans (OCD) of the humeral capitellum: a systematic review and meta-analysis. Int Orthop. 2018;42(3):601–607. doi: 10.1007/s00264-018-3768-3. [DOI] [PubMed] [Google Scholar]
- 18.Rahusen F.T., Brinkman J.M., Eygendaal D. Results of arthroscopic debridement for osteochondritis dissecans of the elbow. Br J Sports Med. 2006;40(12):966–969. doi: 10.1136/bjsm.2006.030056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kalainov D.M., Makowiec R.L., Cohen M.S. Arthroscopic tennis elbow release. Tech Hand Up Extrem Surg. 2007;11(1):2–7. doi: 10.1097/01.bth.0000248358.06825.98. [DOI] [PubMed] [Google Scholar]
- 20.Rossy W.H., Oh L.S. Pitcher's elbow: medial elbow pain in the overhead-throwing athlete. Curr Rev Musculoskelet Med. 2016;9(2):207–214. doi: 10.1007/s12178-016-9346-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cain E.L., Dugas J.R., Wolf R.S., Andrews J.R. Elbow injuries in throwing athletes: a current concepts review. Am J Sports Med. 2003;31(4):621–635. doi: 10.1177/03635465030310042601. [DOI] [PubMed] [Google Scholar]
- 22.Ahmad C.S., ElAttrache N.S. Valgus extension overload syndrome and stress injury of the olecranon. Clin Sports Med. 2004;23(4):665–676. doi: 10.1016/j.csm.2004.04.013. [DOI] [PubMed] [Google Scholar]