Abstract
The popularity of yoga and the prevalence of total hip arthroplasty (THA) have simultaneously increased in the United States. Accordingly, one can assume that the number of THA patients practicing yoga has increased. Certain yoga poses reach the extremes of hip range of motion, potentially leaving patients vulnerable to dislocation. To date, 2 cases of late posterior prosthetic hip dislocations during yoga have been reported; however, there have been no reports of anterior prosthetic hip dislocations. We present one case of late anterior prosthetic hip dislocation during yoga in a patient who underwent THA via the direct anterior approach. Prosthetic hip dislocation during yoga may be a growing concern. We provide additional evidence in support of recommendations for THA patients to safely practice yoga.
Keywords: Total hip arthroplasty, Total hip replacement, Direct anterior approach, Complication, Hip dislocation, Yoga
Introduction
The incidence and prevalence of total hip arthroplasty (THA) in the United States is increasing [1,2]. There were an estimated 2.5 million individuals living with THA in 2010, and projections predict this number may increase to 4 million individuals by 2030 [1]. Furthermore, surgical indications for THA have expanded to include younger, more active patients. Amid this growth in THA, there has been a simultaneous increase in the number of Americans practicing yoga [3]. A study from 2016 demonstrated that there were 36 million yoga practitioners in the United States, which was a 50% growth over the course of 4 years. Seventy percent of yoga practitioners are women, while 62% are below the age of 50 years. While no epidemiologic data link THA patients and yoga practitioners, it has been postulated that the incidence of THA patients practicing yoga is increasing [4]. Our anecdotal experience has been that increasing numbers of patients, particularly young women, are practicing yoga after undergoing THA.
Dislocation is among the most common complications after THA and is the most frequently reported reason for early hip revision [5]. Risk factors for dislocation are multifactorial and include both patient variables such as increased age, female gender, and history of neuromuscular disorders and surgery-related factors such as surgical technique, implant malposition, and implant choice [5,6]. Postoperatively, extreme motion of the hip may also lead to prosthetic hip dislocation, which can be a difficult problem to treat, especially in cases requiring revision surgery.
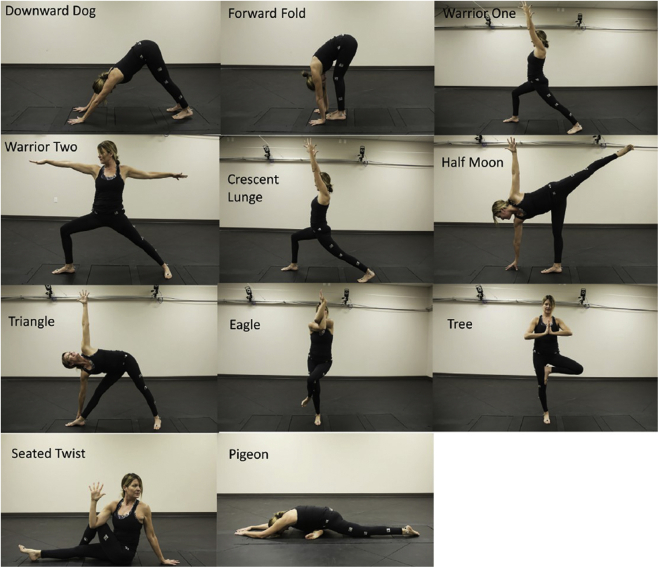
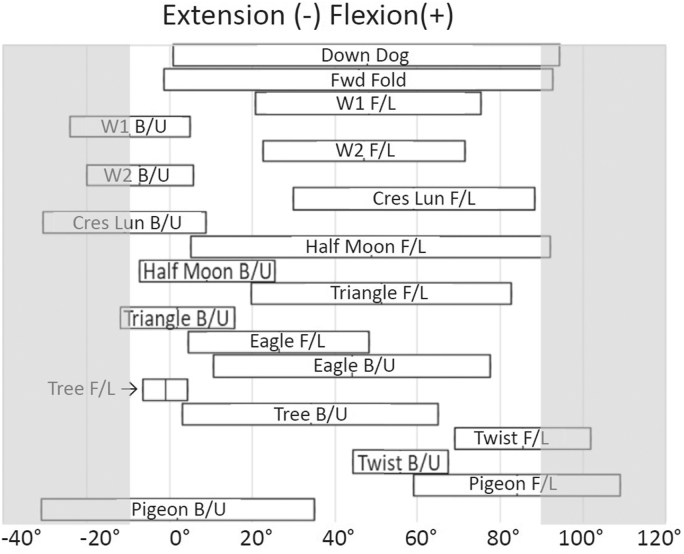
Standard advice after THA is to avoid extremes of motion to reduce the risk of impingement and dislocation. Yoga however places patient’s hips at or beyond these extremes of motion. Mears et al. and analyzed hip position during common yoga poses (Figure 1, Figure 2) and found that poses that put more anterior dislocation forces on the hip include warrior one, warrior 2, crescent lunge, and pigeon (for the backwards/unloaded limb) [6]. In addition, increased posterior forces are seen with downward dog, forward fold, half moon, seated twist, and pigeon (for the forward/loaded limb) [6]. Despite this finding, no specific guidelines exist for arthroplasty patients to safely practice yoga and minimize their dislocation risk. Prosthetic hip dislocation during yoga may be a growing concern as younger patients are undergoing arthroplasty and rates of yoga participation are increasing. Two cases of late posterior prosthetic hip dislocation during yoga have been reported in the literature [4]. However, to our knowledge, there are no reports of anterior hip dislocations during yoga. In this article, we present a case of late anterior THA dislocation that occurred during yoga. The patient underwent THA via the direct anterior approach (DAA) and experienced 2 anterior prosthetic hip dislocations 16 months postoperatively. In addition, we discuss potential activity modifications and precautions which can be implemented during yoga to decrease dislocation risk. The patient was informed that data concerning the case would be submitted for publication, and she provided consent.
Figure 1.
Eleven common yoga poses that stress the hip.
Reprinted from J Arthroplasty, 33(7); Mears SC, Wilson MR, Mannen EM, Tackett SA, Barnes CL. Position of the Hip in Yoga, 2306-2311, © 2018, with permission from Elsevier [6].
Figure 2.
Mean hip range-of-motion for each pose in flexion/extension. Hip range-of motion in common yoga poses for the forward/loaded limb (F/L) and the backward/unloaded limb (B/U): downward dog (Down Dog), forward fold (Fwd Fold), warrior 1 (W1), warrior 2 (W2), crescent lunge (Cres Lun), half moon, triangle, eagle, tree, seated twist (Twist), and pigeon.
Reprinted from J Arthroplasty, 33(7); Mears SC, Wilson MR, Mannen EM, Tackett SA, Barnes CL. Position of the Hip in Yoga, 2306-2311, © 2018, with permission from Elsevier [6].
Case history
A 40-year-old woman with a history of bilateral hip osteoarthritis underwent a staged bilateral THA (Fig. 3). Her medical history included only gastroesophageal reflex disease and depression, and her body mass index was 19.1 kg/m2. She had no spinopelvic abnormalities and no history of spinal fusion, deformity, or degeneration. Preoperatively, her hip flexion and extension was 0-90 degrees, and her hip internal and external rotation were 5 and 10 degrees, respectively. She practiced yoga preoperatively to the best of her ability; however, this activity was significantly limited because of pain and poor range of motion. The bilateral THA procedures were performed on consecutive days via the DAA by a high-volume DAA surgeon with utilization of a traction table (Fig. 4). Her left hip used a DePuy Pinnacle Gription coated 54-mm acetabular cup, ceramic 36 × 54-mm liner, and 36 plus 1.5 Biolox ceramic head (CeramTec, Plochingen, Germany), with a size 6 standard-offset active ACTIS femoral stem (DePuy Synthes, Warsaw, IN). Her right hip used all the same components with the exception of a 36 plus 5 Biolox ceramic head. The left acetabular component was well positioned measuring 34 degrees of abduction and 21 degrees of anteversion. Postoperatively, her hip flexion and extension was 0-90 degrees, and her hip internal and external rotation were 10 and 20 degrees, respectively. The authors do not routinely recommend hip precautions for patients after primary anterior THA; accordingly, no postoperative functional restrictions were advised.
Figure 3.
Preoperative anteroposterior pelvis radiograph demonstrating bilateral hip osteoarthritis.
Figure 4.
Postoperative anteroposterior pelvis radiograph after bilateral total hip arthroplasty.
Sixteen months postoperatively, she was practicing yoga when she experienced an anterior hip dislocation. She was performing the warrior one pose, hyperextending and externally rotating her hip in a standing position with her contralateral hip and knee both flexed. She felt a sudden pop to her left hip and immediately fell. She was taken to the emergency department where a left prosthetic anterior hip dislocation was diagnosed (Fig. 5a and b). A closed reduction was performed (Fig. 6a and b). She was discharged to follow-up as an outpatient with her surgeon and instructed on anterior hip precautions and refraining from extremes of hip range of motion, especially hyperextension and external rotation. Before this incident, the patient reported no hip pain and had resumed an active lifestyle. She performed weighted lunges and yoga regularly but however had never experienced hip instability during these movements before this episode.
Figure 5.
(a) AP and (b) lateral hip radiographs demonstrating an anterior prosthetic hip dislocation.
Figure 6.
(a) AP and (b) frog leg lateral hip radiographs after successful closed reduction of anterior prosthetic hip dislocation.
Unfortunately, 9 days after her closed reduction, she tripped and fell, hyperextending her left hip. She sustained a second anterior hip dislocation and was again close reduced in the emergency department. Inflammatory markers were within normal limits. Owing to her recurrent instability, a lengthy discussion was held with the patient. She preferred to pursue observational management and continue guided physical therapy with strict adherence to activity modification. While performing her activities of daily living, she was advised restrictions on hip extension beyond 0 degrees, walking backwards, and hip external rotation. During yoga, she was advised to avoid positions involving excessive hip hyperextension and external rotation, such as warrior one, warrior two, crescent lunge, and pigeon. At 1-year follow-up, she had been compliant with activity restrictions and has not experienced further dislocations. She continues to participate in yoga but however avoids positions of hip hyperextension and external rotation.
Discussion
Adding to the cases presented by Adrados et al. [4], we present a case of late THA dislocation during yoga. Similar to their cases, after an uncomplicated postoperative course, our patient experienced a late prosthetic hip dislocation while performing a standard yoga pose. However, in our case, the prosthesis dislocated anteriorly. Interestingly, the 2 cases they reported were performed through 2 different approaches, the DAA and the posterior approach, and yet both dislocated posteriorly, whereas our case was performed through the DAA and dislocated anteriorly. In addition, the dislocations they observed occurred 17 and 9 years after the index procedure, while our patient's prosthetic hip dislocated 16 months after THA. This variability underlines the challenge orthopedic surgeons may face in counseling THA patients wishing to practice yoga, regarding range-of-motion restrictions. Classic postoperative patient care is focused on avoiding extremes of range of motion that may place the hip at risk for anterior or posterior dislocation. However, yoga is carried out through a series of poses that focus on strengthening, conditioning, and stretching, where motion of the hip is often beyond the range that would normally be advised after THA [6].
Dislocation after THA remains a major complication that can become challenging to treat. The postoperative dislocation rate after THA through the DAA has been reported to be around 0.6-1.5% [7]. Most prosthetic hip dislocations occur within the first postoperative year, and the majority of dislocations can be managed conservatively. However, late dislocations are associated with recurrent instability which causes substantial disability in the daily life of patients and frequently requires surgical intervention [8]. Risk factors for dislocation include patient variables such as age, sex, avascular necrosis of the femoral head, weak abductor muscles, inflammatory arthritis, history of neuromuscular conditions, and previous revision, in addition to surgery-related factors such as implant malposition and implant-related factors including head size and modularity [5,6,8].
Several studies suggest that the type of approach used to perform THA affects the risk of dislocation as well, with the DAA providing an advantage over the posterior approach. One study directly comparing the dislocation rates between THA performed via the DAA and the posterior approach found the dislocation rate to be significantly less in the DAA group [9]. Similarly, 2 meta-analyses comparing outcomes after THA via these 2 approaches suggest that dislocation rates are lower with the DAA [10,11]. Soft tissue tension is one of the factors which predict postoperative dislocation [9], and the DAA allows implantation of the total hip component while relatively minimizing the detachment of muscles and tendons around the hip joint, thereby maintaining soft tissue tension. Preserving muscle may potentially contribute to dynamic stabilization of the hip, thus reducing the incidence of dislocation after THA via the DAA [7]. Lower postoperative dislocation rates with the DAA have also been attributed to the use of supine patient positioning, intraoperative use of fluoroscopy, and more accurate implant positioning [12]. It is important to note however that literature to support the contrary also exists, with studies reporting equivalent dislocation rates between the DAA and the posterior approach [[12], [13], [14], [15], [16]].
Anecdotally, instability is less of a concern, and therefore, most DAA surgeons do not prescribe hip precautions after THA. Barrett et al. reported that with the DAA, the use of intraoperative fluoroscopy aids with precise component positioning which, in addition to preserving posterior soft tissue structures, allows patients to avoid range-of-motion restrictions [14]. Recently, a survey of the American Association of Hip and Knee Surgeons and Canadian Arthroplasty Society members was conducted to determine how often precautions and equipment were prescribed after THA [17]. The results illustrated the relative consensus among North American DAA surgeons that postoperative precautions are routinely not necessary after DAA, with DAA surgeons significantly applying fewer precautions. However, when precautions were taught by DAA surgeons, there was less consensus among responding DAA surgeons for which motions to restrict. The authors note that this is understandable given the paucity of data regarding effective precautions. The majority of the respondents who prescribed hip precautions restricted hip extension, external rotation, and hip flexion. The authors of this case report do not routinely advise postoperative restrictions for patients after primary direct anterior THA.
Numerous consensus articles have been published regarding return to athletic activity after THA [[18], [19], [20], [21], [22]]. A 2020 survey among members of the European Hip Society, which is the first and only article to reference yoga specifically, recommends allowing return to yoga 6 weeks after THA [21]. This represents a greater tolerance by surveyed surgeons to allow return to activity than consensus guidelines from 2007 which recommended allowing return to pilates, a similar activity, only to those with previous experience [22]. Authors have also divided sporting activities into 3 broad categories based on impact level—“high impact,” “intermediate impact,” and “low impact”—and base their recommendations accordingly. Although yoga had not been distinctly referenced before the recommendations from Thaler et al. [21], other authors do however mention activities, such as martial arts, which require hip motion beyond the range that would normally be advised with THA. Furthermore, in discussing the likelihood of dislocation, they note that there is no evidence to suggest an increased dislocation rate in THA patients involved in sports and that surgeons can reduce risk by using larger femoral heads, up to 36 mm [19,20].
Yoga would be classified as a “low-impact” activity; however, the concern with yoga is not how much load the prosthesis may have to bear but rather how much motion the hip will be ranged through. Mears et al. identified hip poses that place the hip in higher ranges of motion [6]. The poses of warrior one, warrior two, crescent lunge, and pigeon resulted in hyperextension of more than 10 degrees on average, increasing the risk of an anterior dislocation. Similarly, certain poses increase the risk of a posterior dislocation [6]. As evident in our case, and in prior cases of THA dislocation during yoga, these poses may lead to dislocation of the prosthesis regardless of how long ago the index procedure was performed. While the authors do not routinely advise postoperative restrictions for all patients after primary direct anterior THA, for patients who practice yoga, we are now advising them to exercise caution when practicing poses that may put their hip in extreme positions, such as warrior one, warrior two, crescent lunge, and pigeon.
Ultimately, it is important that surgeons provide patients with realistic expectations about activity after a THA. Counseling the patient on postoperative ways to avoid possible dislocation and about yoga positions that may be safely practiced after THA is paramount to protect and maintain the longevity of the hip prosthesis. Furthermore, surgical modifications to add additional stability for patients who practice yoga, such as use of dual-mobility implants, might be considered; however, this may be controversial given the current evolving indications for these prostheses.
Summary
Our study adds to the growing field of evidence that hip dislocation during yoga is a true phenomenon. Prosthetic hip dislocation during yoga may be a growing concern as younger patients are undergoing arthroplasty and rates of yoga participation are increasing. Patients who practice yoga after undergoing THA should be cautioned, both in the early and late postoperative periods, to avoid extremes in hip range of motion to decrease their risk of prosthetic hip dislocation.
Conflict of interests
The authors declare there are no conflicts of interest.
Supplementary data
References
- 1.Kremers H.M., Larson D.R., Crowson C.S. Prevalence of total hip and knee replacement in the United States. J Bone Joint Surg Am. 2014;97(17):1386. doi: 10.2106/JBJS.N.01141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kurtz S., Ong K., Lau E., Mowat F., Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89(4):780. doi: 10.2106/JBJS.F.00222. [DOI] [PubMed] [Google Scholar]
- 3.Yoga Alliance The 2016 yoga in America - study conducted by yoga journal and yoga alliance. Yoga J. 2016. https://www.yogaalliance.org/Portals/0/2016 Yoga in America Study RESULTS.pdf
- 4.Adrados M., Myhre L.A., Rubin L.E. Late total hip arthroplasty dislocation due to yoga. Arthroplast Today. 2018;4(2):180. doi: 10.1016/j.artd.2018.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zahar A., Rastogi A., Kendoff D. Dislocation after total hip arthroplasty. Curr Rev Musculoskelet Med. 2013;6(4):350. doi: 10.1007/s12178-013-9187-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mears S.C., Wilson M.R., Mannen E.M., Tackett S.A., Barnes C.L. Position of the hip in yoga. J Arthroplasty. 2018;33(7):2306. doi: 10.1016/j.arth.2018.02.070. [DOI] [PubMed] [Google Scholar]
- 7.Tamaki T., Oinuma K., Miura Y., Higashi H., Kaneyama R., Shiratsuchi H. Epidemiology of dislocation following direct anterior total hip arthroplasty: a minimum 5-year follow-up study. J Arthroplasty. 2016;31(12):2886. doi: 10.1016/j.arth.2016.05.042. [DOI] [PubMed] [Google Scholar]
- 8.Itokawa T., Nakashima Y., Yamamoto T. Late dislocation is associated with recurrence after total hip arthroplasty. Int Orthop. 2013;37(8):1457. doi: 10.1007/s00264-013-1921-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tsukada S., Wakui M. Lower dislocation rate following total hip arthroplasty via direct anterior approach than via posterior approach: five-year-average follow-up results. Open Orthop J. 2015;9:157. doi: 10.2174/1874325001509010157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Higgins B.T., Barlow D.R., Heagerty N.E., Lin T.J. Anterior vs. posterior approach for total hip arthroplasty, a systematic review and meta-analysis. J Arthroplasty. 2015;30(3):419. doi: 10.1016/j.arth.2014.10.020. [DOI] [PubMed] [Google Scholar]
- 11.Miller L.E., Gondusky J.S., Kamath A.F., Boettner F., Wright J., Bhattacharyya S. Influence of surgical approach on complication risk in primary total hip arthroplasty: systematic review and meta-analysis. Acta Orthop. 2018;89(3):289. doi: 10.1080/17453674.2018.1438694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Barrett W.P., Turner S.E., Murphy J.A., Flener J.L., Alton T.B. Prospective, randomized study of direct anterior approach vs posterolateral approach total hip arthroplasty: a concise 5-year follow-up evaluation. J Arthroplasty. 2019;34(6):1139. doi: 10.1016/j.arth.2019.01.060. [DOI] [PubMed] [Google Scholar]
- 13.Maratt J.D., Gagnier J.J., Butler P.D., Hallstrom B.R., Urquhart A.G., Roberts K.C. No difference in dislocation seen in anterior vs posterior approach total hip arthroplasty. J Arthroplasty. 2016;31(9 Suppl):127. doi: 10.1016/j.arth.2016.02.071. [DOI] [PubMed] [Google Scholar]
- 14.Barrett W.P., Turner S.E., Leopold J.P. Prospective randomized study of direct anterior vs postero-lateral approach for total hip arthroplasty. J Arthroplasty. 2013;28(9):1634. doi: 10.1016/j.arth.2013.01.034. [DOI] [PubMed] [Google Scholar]
- 15.Wang Z., Hou J.Z., Wu C.H. A systematic review and meta-analysis of direct anterior approach versus posterior approach in total hip arthroplasty. J Orthop Surg Res. 2018;13(1):1. doi: 10.1186/s13018-018-0929-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Miller L.E., Gondusky J.S., Bhattacharyya S., Kamath A.F., Boettner F., Wright J. Does surgical approach affect outcomes in total hip arthroplasty through 90 Days of follow-up? A systematic review with meta-analysis. J Arthroplasty. 2018;33(4):1296. doi: 10.1016/j.arth.2017.11.011. [DOI] [PubMed] [Google Scholar]
- 17.Carli A.V., Poitras S., Clohisy J.C., Beaulé P.E. Variation in use of postoperative precautions and equipment following total hip arthroplasty: a survey of the AAHKS and CAS membership. J Arthroplasty. 2018;33(10):3201. doi: 10.1016/j.arth.2018.05.043. [DOI] [PubMed] [Google Scholar]
- 18.Wilson M.J., Villar R.N. Hip replacement in the athlete: is there a role? Knee Surg Sports Traumatol Arthrosc. 2011;19(9):1524. doi: 10.1007/s00167-011-1492-2. [DOI] [PubMed] [Google Scholar]
- 19.Krismer M. Sports activities after total hip arthroplasty. EFORT Open Rev. 2017;2(5):189. doi: 10.1302/2058-5241.2.160059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bradley B.M., Moul S.J., Doyle F.J., Wilson M.J. Return to sporting activity after total hip arthroplasty—a survey of members of the British Hip Society. J Arthroplasty. 2017;32(3):898. doi: 10.1016/j.arth.2016.09.019. [DOI] [PubMed] [Google Scholar]
- 21.Thaler M., Khosravi I., Putzer D., Siebenrock K.A., Zagra L. Return to sports after total hip arthroplasty: a survey among members of the European Hip Society. J Arthroplasty. 2020 doi: 10.1016/j.arth.2020.11.009. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 22.Klein G.R., Levine B.R., Hozack W.J. Return to athletic activity after total hip arthroplasty. Consensus guidelines based on a survey of the Hip Society and American Association of Hip and Knee Surgeons. J Arthroplasty. 2007;22(2):171. doi: 10.1016/j.arth.2006.09.001. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.