Abstract
Background:
The purpose of this study was to evaluate the incidence of lower extremity compartment syndrome in National Football League (NFL) athletes and report the mechanisms of injury, methods of treatment, and subsequent days missed. We review the existing literature on lower extremity compartment syndrome in athletic populations.
Hypothesis:
Lower extremity compartment syndrome occurs with a low incidence in NFL athletes, and there is a high return-to-play rate after surgical management of acute compartment syndrome.
Study Design:
Case series.
Level of Evidence:
Level 4.
Methods:
A retrospective review of recorded cases of lower extremity compartment syndrome from 2000 to 2017 was performed using the NFL Injury Surveillance System and electronic medical record system. Epidemiological data, injury mechanism, rates of surgery, and days missed due to injury were recorded.
Results:
During the study period, 22 cases of leg compartment syndrome in 21 athletes were recorded. Of these injuries, 50% occurred in games and 73% were the result of a direct impact to the leg. Concomitant tibial fracture was noted in only 2 cases (9.1%) and there was only 1 reported case of chronic exertional compartment syndrome. Surgery was documented in 15 of 22 cases (68.2%). For acute nonfracture cases, the average time missed due to injury was 24.2 days (range, 5-54 days), and all were able to return to full participation within the same season.
Conclusion:
NFL athletes with acute leg compartment syndrome treated with surgery exhibited a high rate of return to play within the same season.
Clinical Relevance:
Although compartment syndrome is a relatively rare diagnosis among NFL players, team physicians and athletic trainers must maintain a high index of suspicion to expediently diagnose and treat this potentially limb-threatening condition.
Keywords: compartment syndrome, National Football League, NFL, fasciotomy
Lower extremity compartment syndrome is a relatively rare but potentially limb-threatening condition, which most commonly affects the leg below the level of the knee.1 Other less commonly affected areas include the thigh, foot, and gluteal region.12 Acute compartment syndrome (ACS) can result from direct impact injuries to soft tissue structures, ischemia related to vascular injury, extremity fractures, or more rarely, overexertion.12,15,24 Acute exertional compartment syndrome (AECS) is a rare subset of ACS, characterized by an increase in intracompartmental pressure without a specific traumatic event.15,24 The lower leg is composed of 4 compartments: anterior, lateral, superficial posterior, and deep posterior.8 Pain with passive stretch of the muscles within the affected compartment(s) is a hallmark of early clinical diagnosis prior to the onset of sensory or motor changes.6,19,26 The anterior compartment, which contains the tibialis anterior, toe extensors, tibial artery, and deep peroneal nerve, is the most common location for lower leg compartment syndrome and may manifest as altered sensation in the first webspace and weakness with ankle dorsiflexion. Lateral compartment involvement may manifest as altered sensation and diminished motor function in the distribution of the superficial peroneal nerve. Because the proximal portion of the deep peroneal neve is contained within the lateral compartment, weakness in dorsiflexion may also be observed in the setting of lateral compartment syndrome. The superficial posterior compartment, containing the gastrocnemius and soleus, is least likely to develop compartment syndrome and usually manifests as a palpably tense and tender compartment. The deep posterior compartment, containing the posterior tibialis, toe flexors, peroneal artery, and tibial nerve, can manifest in plantar dysesthesias and weakness in the toe flexors. ACS results when increased intracompartmental pressure exceeds capillary perfusion pressure, thereby reducing extremity perfusion and causing a marked increase in pain.25 Prolonged decreased tissue perfusion leads to soft tissue ischemia and, without prompt treatment, cell death.9,34 Therefore, early diagnosis and treatment is imperative to prevent irreversible muscle damage. In chronic exertional compartment syndrome (CECS), prompt diagnosis is less critical in preventing irreversible muscle damage, but expeditious treatment of symptomatic elite athletes with CECS may facilitate an earlier return to the athlete’s previous level of performance.7
There are few studies to date reporting on compartment syndrome in athletes, and most existing publications are case reports.2,7,13,17,18,21,23,27,28,33-37 Furthermore, to our knowledge, there is only 1 published case report of compartment syndrome in a National Football League (NFL) player, with this case occurring in an athlete after a fracture of a tibiofibular shaft synostosis.14 As such, the epidemiology of lower extremity compartment syndrome among NFL players is yet to be described. Therefore, the purpose of this study was to evaluate the incidence of lower extremity compartment syndrome in NFL athletes and report the mechanisms of injury, methods of treatment, and subsequent days missed due to injury.
Methods
Express written consent to use data from the NFL Injury Surveillance System (ISS) and electronic medical record (EMR) for this study was obtained through the Medical Research Approval Protocol, the NFL Players Association, and the Mount Sinai Institutional Review Board.22 This study was also approved by the Hospital for Special Surgery Institutional Review Board. Patients were identified using the NFL ISS database (IQVIA). A retrospective review of all recorded cases of lower extremity compartment syndrome in the NFL from 2000 to 2017 was performed. Data collection and analytics of all NFL-wide data are led by the IQVIA Injury Surveillance and Analytics Team and used by the NFL, its medical committees, and individual teams to provide aggregate information about injury occurrence and patterns.5
Both injury-specific and athlete-specific data were compiled.3 For injury-specific data, the incidence of lower extremity compartment syndrome, timing of injury (offseason, preseason, regular season, postseason, game, practice), anatomic location of compartment syndrome, chronicity (acute vs chronic), laterality, mechanism of injury (contact vs noncontact), and team activity during which injury occurred was recorded. Athlete-specific data included roster position, height, weight, and body mass index. The number of days from symptom onset or injury to surgery was reported. With regard to return to play, return to full participation and the number of days missed due to injury was retrieved. Time lost due to injury was defined by the NFL ISS as number of days missed from date of removal from participation due to the injury until the player was cleared for full participation in practice or games.3
All cases of lower extremity compartment syndrome as identified by the NFL ISS were included in the study, as well as any injury treated with a decompression fasciotomy (Current Procedural Terminology [CPT] 27600-02, 27892-94). The type of compartment syndrome (ACS, AECS, CECS) was not defined within the ISS or EMR. Rather, data were interpreted by 2 authors who determined in each case the type of compartment syndrome based on mechanism of injury, player activity at time of injury, team activity at time of injury, number of days from injury onset to surgery (if performed), and additional clinical impression codes associated with the injury. In each case, a consensus on clinical diagnosis was clearly reached without dispute. A case was considered CECS if it was documented as insidious and not having an acute player activity, team activity, or injury mechanism reported as the cause of the injury, which would otherwise suggest ACS. From 2000 to 2013, surgeries (classified as Yes/Unknown) and surgery dates were entered into the NFL ISS. From 2014 to 2017, entry of CPT codes was required for documentation of surgeries along with surgery date. Bilateral compartment syndrome occurring in the same patient was considered as 2 separate cases for data analysis. All analyses were conducted using Microsoft Excel. Figures are reported as a proportion of the total number of cases or as mean ± SD.
Results
From 2000 to 2017, 22 cases of leg compartment syndrome in 21 athletes were identified. All cases of compartment syndrome involved the lower leg, and there were no reported cases of thigh, foot, or gluteal compartment syndrome. The mechanism of injury was direct impact in 16 cases (72.7%) (Figure 1). There was only 1 case of bilateral compartment syndrome in a linebacker, which occurred during a regular season practice; this injury was characterized as AECS and did not result from a direct impact. There was a total of 3 cases of AECS and only 1 case of CECS. Surgery was documented in 15 of 22 cases (68.2%). A total of 50% of the cases occurred during regular season games (Figure 2). One-third of cases occurred in offensive or defensive linemen, with another third of cases occurring in defensive secondary players (Figure 3). Concomitant tibia fracture occurred in only 2 cases (9.1%). One tibial fracture was a plateau fracture with an associated knee dislocation and multiligamentous knee injury, and that player’s return to full participation was not documented. The other player with a tibial shaft fracture returned to full participation 89 days after surgery. All nonfracture cases of ACS resulting from a direct impact were treated acutely with surgery at an average of 1 ± 0.6 days after injury (range, 0-2 days), and the average number of days missed due to injury was 24.2 ± 15.5 days (range, 5-54 days). All these athletes were able to return to full participation within the same season. Overall, all players with known return dates returned within the same season.
Figure 1.

Mechanism of injury resulting in lower extremity compartment syndrome.
Figure 2.
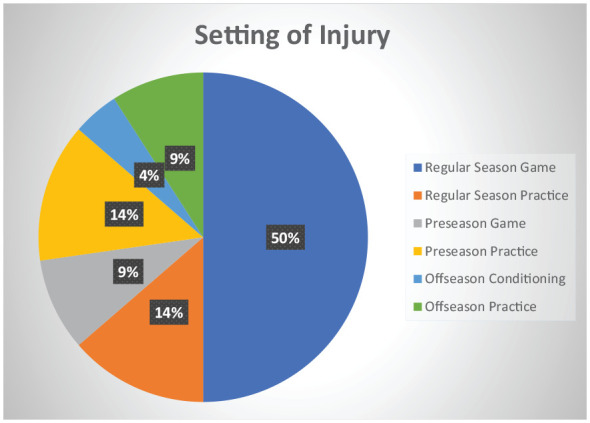
Setting in which lower extremity compartment syndrome occurred.
Figure 3.

Position among players who developed lower extremity compartment syndrome.
Discussion
Over an 18-year period, we report 22 cases of lower extremity compartment syndrome among NFL players. All cases involved the leg, all but 1 case was unilateral, and the mechanism of injury was most commonly a direct impact to the leg without associated fracture. Interestingly, only 2 cases were associated with fracture. Half of the injuries occurred in a regular season game, and there was a similar incidence of injury among linemen, skill players, offensive players, and defensive players. Among athletes diagnosed with ACS without an associated fracture, all returned to play within the same season and missed an average of 3.5 weeks due to injury. To our knowledge, this is the first case series of lower extremity compartment syndrome in NFL players.
These findings will be useful in several ways for physicians treating football athletes. First, to our knowledge, ACS of the leg secondary to a direct impact has not been described in an athletic population and comprised the majority of cases in this series. As such, athletic trainers and team physicians must maintain a high index of suspicion for this injury in players presenting with signs and symptoms of compartment syndrome even in the absence of a fracture. Second, players diagnosed with ACS and treated operatively in an expeditious manner can be counseled that a full return to participation is very likely, often within the same season, and most likely within approximately 3 to 4 weeks postoperatively.
One prior study described a case of recurrent compartment syndrome in an NFL player who fractured a previously unrecognized synostosis of the tibial and fibular shafts.14 This player developed anterior compartment syndrome requiring fasciotomy at the time of synostosis fracture and recurrent compartment syndrome after a direct impact injury in which he was kicked in the leg during a blocking drill. He was able to return to full activity by 6 months after his repeat fasciotomy but was not offered a subsequent contract. Starr et al33 reported a case of anterior leg compartment syndrome after a bimalleolar equivalent ankle fracture in a collegiate football player who was injured playing recreational touch football. In the present series, 1 NFL player with ACS and an associated tibial shaft fracture sustained during a preseason practice returned to full participation 89 days postoperatively. A second player with an associated multiligamentous knee injury and tibial plateau fracture sustained during a regular season game did not return to full participation during the same season, and return to full participation was not documented but is unlikely given the extensive nature of his injuries. While it is expected that patients with leg compartment syndrome and an associated fracture would have a prolonged recovery period prior to return to full participation, all NFL players with ACS without an associated fracture were able to return to full participation within the same season.
In this study, we report 2 cases of AECS in 2 patients. The athlete with bilateral AECS returned to participation after 14 missed days, and the other player did not have a documented return to participation. AECS is a rare and uncommonly reported condition that can present a diagnostic dilemma among athletes presenting with leg pain associated with activity without a direct impact injury.31 The diagnosis in these cases is often made in a delayed fashion, possibly resulting in progressive myonecrosis and nerve injury as has been described in 2 previous case reports of football players.18,34 With potentially devastating consequences if not expediently diagnosed and treated, AECS must be considered in the differential diagnosis of an athlete presenting with leg pain along with conditions such as CECS, medial tibial stress syndrome, and stress fracture, especially if no specific trauma has occurred.34 An index of suspicion should also be maintained in athletes with sickle cell trait or a bleeding diathesis. A prompt diagnosis and appropriate treatment of AECS is paramount because of the potentially catastrophic sequelae of this condition.
While several studies have investigated acute leg compartment syndrome in athletic populations, none to our knowledge report a direct blow without fracture as the mechanism of injury.21,23,28,30,31,35 Mendelson et al28 reported a case of acute leg compartment syndrome in a high school football player after an inversion ankle injury resulting in acute peroneus longus rupture. In this study, we report only 1 case of CECS.2,7,11 To our knowledge, there is no previous report of CECS in an NFL player in the existing literature. Goldfarb et al11 reported a case of bilateral AECS of the lateral compartment in the setting of preexisting CECS in a 21-year-old collegiate football player. Over an 18-year period, no cases of thigh compartment syndrome among NFL players were reported to the database. Acknowledging the possibility of underreporting during the early years of this study, this is an interesting and surprising finding, as thigh compartment syndrome has been previously reported in nonprofessional football players4,20,27 and in other contact sports, including rugby29,32,37 and soccer.10,16 This is likely, at least, partially attributable to a league requirement that all players wear anterior thigh pads during contact practices and games. While there have been no reported cases of thigh compartment syndrome among NFL players to date, it must be a consideration for a player presenting with signs and symptoms consistent with this diagnosis after a direct blow to the thigh.
There are multiple limitations to this study. This was a retrospective database study performed using the NFL ISS and EMR. The NFL EMR was introduced in 2014 and implemented throughout the 2015 season, collecting more comprehensive injury information than the IQVIA ISS program, utilized from 2012 to 2013, or the historical injury surveillance system, utilized from 1980 to 2011.5 The EMR was specifically adapted for use in sports, and all complaints evaluated or treated by medical staff throughout the full year, including the offseason, were required to be reported. Therefore, injury incidence between these time periods may not be directly comparable. Prior to 2011, cases were collected using a case report form, with expanded attention to completion and accuracy of reporting in 2011. As such, it is possible that cases of lower extremity compartment syndrome prior to 2000 were underreported. Because an injury without completed surgery information indicates only that the surgery data were not entered, this likely resulted in a considerable underreporting of surgery status. Offseason injuries and injuries related to conditioning were not required to be documented until 2015, which likely resulted in underreporting of these nongame and nonpractice injuries. While return dates are captured for the entire year from 2012-2017, data from 2000 to 2011 may be limited to in-season days lost only. Specific diagnostic criteria used to establish a diagnosis of compartment syndrome (ie, compartment pressure measurements, clinical examination) were not available within the ISS or EMR. The specific procedure(s) performed was not captured by the data collection system in most cases. Starting in 2014, entry of CPT codes was required for documentation of all surgeries in the EMR, but cases reported prior to then were not required to document the specific procedure(s) performed. Because of the deidentified query that was performed to retrieve the data from the NFL ISS and EMR, information regarding player performance after return to play was not available. Finally, the possibility of unreported cases is a limitation of our data set.
In conclusion, NFL players treated with surgery for ACS of the leg exhibited a high rate of return to play within the same season. All documented cases of lower extremity compartment syndrome occurred within the lower leg, and the majority of cases were acute and occurred as a result of a direct impact without associated fracture. Although compartment syndrome is a relatively rare diagnosis among NFL players, team physicians and athletic trainers must maintain a high index of suspicion to expediently diagnose and treat this potentially limb-threatening condition. By better understanding the epidemiology of lower extremity compartment syndrome among NFL players, the mechanisms by which these injuries occur, the settings in which they occur, and the time missed due to these injuries, the findings of this study may be helpful in caring for athletes with this condition.
Footnotes
The following authors declared potential conflicts of interest: D.W. is a paid consultant for Newclip, USA and has stock options from Cartilage, Inc. K.Z. and C.M. are employees of IQVIA, which provides research support to the National Football League under a consultation partnership. R.F.W. reports personal fees and stock options from Orthonet. S.A.R. reports personal fees from Advance Medical and Ortho RTI.
References
- 1. Branco BC, Inaba K, Barmparas G, et al. Incidence and predictors for the need for fasciotomy after extremity trauma: a 10-year review in a mature level I trauma centre. Injury. 2011;42:1157-1163. [DOI] [PubMed] [Google Scholar]
- 2. Cetinus E, Uzel M, Bilgic E, Karaoguz A, Herdem M. Exercise induced compartment syndrome in a professional footballer. Br J Sports Med. 2004;38:227-229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Chang ES, Bishop ME, Dodson CC, et al. Management of elbow dislocations in the National Football League. Orthop J Sports Med. 2018;6:2325967118755451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Colosimo AJ, Ireland ML. Thigh compartment syndrome in a football athlete: a case report and review of the literature. Med Sci Sports Exerc. 1992;24:958-963. [PubMed] [Google Scholar]
- 5. Dreyer NA, Mack CD, Anderson RB, Wojtys EM, Hershman EB, Sills A. Lessons on data collection and curation from the NFL Injury Surveillance Program. Sports Health. 2019;11:440-445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Elliott KG, Johnstone AJ. Diagnosing acute compartment syndrome. J Bone Joint Surg Br. 2003;85:625-632. [PubMed] [Google Scholar]
- 7. Farr D, Selesnick H. Chronic exertional compartment syndrome in a collegiate soccer player: a case report and literature review. Am J Orthop (Belle Mead NJ). 2008;37:374-377. [PubMed] [Google Scholar]
- 8. Frink M, Hildebrand F, Krettek C, Brand J, Hankemeier S. Compartment syndrome of the lower leg and foot. Clin Orthop Relat Res. 2010;468:940-950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Gelberman RH, Garfin SR, Hergenroeder PT, Mubarak SJ, Menon J. Compartment syndromes of the forearm: diagnosis and treatment. Clin Orthop Relat Res. 1981;161:252-261. [PubMed] [Google Scholar]
- 10. Golden DW, Flik KR, Turner DA, Bach BR, Jr, Sawyer JR. Acute compartment syndrome of the thigh in a high school soccer player: indications for expedient action. Phys Sportsmed. 2005;33:19-24. [DOI] [PubMed] [Google Scholar]
- 11. Goldfarb SJ, Kaeding CC. Bilateral acute-on-chronic exertional lateral compartment syndrome of the leg: a case report and review of the literature. Clin J Sport Med. 1997;7:59-61. [DOI] [PubMed] [Google Scholar]
- 12. Guo J, Yin Y, Jin L, Zhang R, Hou Z, Zhang Y. Acute compartment syndrome: cause, diagnosis, and new viewpoint. Medicine (Baltimore). 2019;98:e16260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Haddad FS, Bann S, Hill RA, Jones DH. Displaced stress fracture of the femoral neck in an active amenorrhoeic adolescent. Br J Sports Med. 1997;31:70-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hanypsiak B, Bergfeld JA, Miniaci A, Joyce MJ. Recurrent compartment syndrome after fracture of a tibiofibular synostosis in a National Football League player. Am J Sports Med. 2007;35:127-130. [DOI] [PubMed] [Google Scholar]
- 15. Hope MJ, McQueen MM. Acute compartment syndrome in the absence of fracture. J Orthop Trauma. 2004;18:220-224. [DOI] [PubMed] [Google Scholar]
- 16. How MI, Lee PK, Wei TS, Chong CT. Delayed presentation of compartment syndrome of the thigh secondary to quadriceps trauma and vascular injury in a soccer athlete. Int J Surg Case Rep. 2015;11:56-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Imade S, Takao M, Miyamoto W, Nishi H, Uchio Y. Leg anterior compartment syndrome following ankle arthroscopy after Maisonneuve fracture. Arthroscopy. 2009;25:215-218. [DOI] [PubMed] [Google Scholar]
- 18. Johnson J, Becker J. Bilateral acute compartment syndrome in a football player: a case report. Curr Sports Med Rep. 2012;11:287-289. [DOI] [PubMed] [Google Scholar]
- 19. Köstler W, Strohm PC, Südkamp NP. Acute compartment syndrome of the limb. Injury. 2005;36:992-998. [DOI] [PubMed] [Google Scholar]
- 20. Lee AT, Fanton GS, McAdams TR. Acute compartment syndrome of the thigh in a football athlete: a case report and the role of the vacuum-assisted wound closure dressing. J Orthop Trauma. 2005;19:748-750. [DOI] [PubMed] [Google Scholar]
- 21. Lipscomb AB, Ibrahim AA. Acute peroneal compartment syndrome in a well conditioned athlete: report of a case. Am J Sports Med. 1977;5:154-157. [DOI] [PubMed] [Google Scholar]
- 22. Mack CD, Matava M, Zeidler K, Sills A, Solomon G. Clinical research in the National Football League (NFL): the player scientific and Medical Research Protocol (MRAP). Curr Sports Med Rep. 2020;19:168-174. [DOI] [PubMed] [Google Scholar]
- 23. Marcu D, Dunbar WH, Kaplan LD. Footdrop without significant pain as late presentation of acute peroneal compartment syndrome in an intercollegiate football player. Am J Orthop (Belle Mead NJ). 2009;38:241-244. [PubMed] [Google Scholar]
- 24. McKinney B, Gaunder C, Schumer R. Acute exertional compartment syndrome with rhabdomyolysis: case report and review of literature. Am J Case Rep. 2018;19:145-149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. McLaughlin N, Heard H, Kelham S. Acute and chronic compartment syndromes: know when to act fast. JAAPA. 2014;27:23-26. [DOI] [PubMed] [Google Scholar]
- 26. McQueen MM, Gaston P, Court-Brown CM. Acute compartment syndrome. Who is at risk? J Bone Joint Surg Br. 2000;82:200-203. [PubMed] [Google Scholar]
- 27. McQuerry JL, Burnham JM, Ireland ML, Wright RD. Delayed presentation of compartment syndrome of the thigh in a previously undiagnosed factor VII-deficient high school football athlete: a case report. JBJS Case Connect. 2018;8:e4. [DOI] [PubMed] [Google Scholar]
- 28. Mendelson S, Mendelson A, Holmes J. Compartment syndrome after acute rupture of the peroneus longus in a high school football player: a case report. Am J Orthop (Belle Mead NJ). 2003;32:510-512. [PubMed] [Google Scholar]
- 29. Mithofer K, Lhowe DW, Altman GT. Delayed presentation of acute compartment syndrome after contusion of the thigh. J Orthop Trauma. 2002;16:436-438. [DOI] [PubMed] [Google Scholar]
- 30. Mohanna PN, Haddad FS. Acute compartment syndrome following non-contact football injury. Br J Sports Med. 1997;31:254-255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Moyer RA, Boden BP, Marchetto PA, Kleinbart F, Kelly JD, 4th. Acute compartment syndrome of the lower extremity secondary to noncontact injury. Foot Ankle. 1993;14:534-537. [DOI] [PubMed] [Google Scholar]
- 32. Smith RDJ, Rust-March H, Kluzek S. Acute compartment syndrome of the thigh in a rugby player. BMJ Case Rep. 2015;2015:BCR2015210856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Starr AM, Swan KG, Jr, Swan KG. Isolated anterior compartment syndrome after a bimalleolar-equivalent ankle fracture in a collegiate football player. Sports Health. 2011;3:560-563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Stollsteimer GT, Shelton WR. Acute atraumatic compartment syndrome in an athlete: a case report. J Athl Train. 1997;32:248-250. [PMC free article] [PubMed] [Google Scholar]
- 35. Taxter AJ, Konstantakos EK, Ames DW. Lateral compartment syndrome of the lower extremity in a recreational athlete: a case report. Am J Emerg Med. 2008;26:973.e1-e2. [DOI] [PubMed] [Google Scholar]
- 36. Wind TC, Saunders SM, Barfield WR, Mooney JF, 3rd, Hartsock LA. Compartment syndrome after low-energy tibia fractures sustained during athletic competition. J Orthop Trauma. 2012;26:33-36. [DOI] [PubMed] [Google Scholar]
- 37. Young PS, Middleton RG, Shaw AD. Profunda femoris artery pseudoaneurysm complicating compartment syndrome after blunt trauma. Am J Sports Med. 2011;39:1786-1788. [DOI] [PubMed] [Google Scholar]


