Abstract
Background:
In the POST SCD study, we autopsied all World Health Organization (WHO) defined sudden cardiac deaths (SCDs) and found only 56% had arrhythmic cause; resuscitated sudden cardiac arrests (SCAs) were excluded because they did not die suddenly. We hypothesized that causes underlying resuscitated SCAs would be similarly heterogeneous.
Objectives:
To determine the causes and outcomes of resuscitated SCAs.
Methods:
We identified all out-of-hospital cardiac arrests (OHCAs) from 2/1/11 to 1/1/15, aged 18–90 years, in San Francisco County. Resuscitated SCAs were OHCAs surviving to hospitalization and meeting WHO criteria for suddenness. Underlying cause was determined by comprehensive record review.
Results:
We identified 734 OHCAs over 48 months; 239 met SCA criteria, 133 (55.6%) were resuscitated to hospitalization and 47 (19.7%) survived to discharge. Arrhythmic causes accounted for significantly more resuscitated SCAs overall (92 of 133 [69.1%]), particularly survivors (43 of 47 [91.5%]), than WHO-defined SCDs in POST SCD (293 of 525 [55.8%], p< 0.004 for both). Among resuscitated SCAs, arrhythmic cause, ventricular tachycardia/fibrillation initial rhythm, and White race were independent predictors of survival. None of the 1 in 5 resuscitated SCAs due to neurologic causes survived.
Conclusions:
In this 4-year countywide study of OHCAs, only one-third were sudden, of which half were resuscitated to hospitalization and 1 in 5 survived to discharge. Arrhythmic cause predicted survival while nearly half of non-survivors had non-arrhythmic causes, suggesting that SCA survivors are not equivalent to SCDs. Early identification of non-arrhythmic SCAs such as neurologic emergencies may be targets to improve OHCA survival.
Keywords: Sudden Cardiac Death, Out of Hospital Cardiac Arrest, Resuscitation
Condensed Abstract:
In the POST SCD study, we autopsied all World Health Organization defined (presumed) SCDs and found that only 56% had arrhythmic cause; resuscitated SCAs were not included because they did not die suddenly. In this study we identified all contemporaneous countywide SCAs resuscitated to hospitalization over 4 years and found that 1 in 5 survived to discharge. Arrhythmic causes were found in 92% of SCA survivors but only 57% of non-survivors, suggesting SCA survivors are distinct from SCDs. Early identification of non-arrhythmic SCAs such as neurologic emergencies (which had 100% mortality) may be targets to improve survival.
Introduction
Despite significant advances in resuscitation science, survival to discharge after out-of-hospital cardiac arrest (OHCA) remains poor at less than 10% (1–3). In 2004, the Centers for Disease Control and Prevention (CDC) established the Cardiac Arrest Registry to Enhance Survival (CARES) to better monitor and study OHCAs. However, despite recognition that OHCAs can be due to non-cardiac causes and that a refined taxonomy of underlying causes may be critical to addressing its high mortality, (4) CARES criteria only require an emergency medical services (EMS) primary impression of cardiac arrest and do not specify suddenness of arrest (5). Moreover, OHCA death is frequently used as a proxy for sudden cardiac death (SCD) (6–8) and many studies equate the outcomes of SCA and SCD.
Recently, we performed a prospective 3-year countywide postmortem study to ascertain the incidence and underlying cause of all CARES-defined OHCA deaths and World Health Organization (WHO)-defined SCDs in San Francisco County POstmortem Systematic InvesTigation of Sudden Cardiac Death [POST SCD] Study (9). We found that 40% of OHCA deaths were not sudden nor unexpected, i.e., did not meet WHO criteria for sudden cardiac arrest (SCA), and only half (55.8%) of WHO-defined SCDs (i.e., those SCAs not resuscitated) were autopsy-defined sudden arrhythmic deaths (SADs) potentially rescuable by a defibrillator; the remainder of these presumed SCDs were due to non-arrhythmic causes (e.g., occult overdose, pulmonary embolism, hemorrhage, tamponade) found on autopsy. Thus, POST SCD demonstrated systematic deficiencies in EMS and conventional definitions of OHCA and SCD.
SCAs resuscitated to hospital admission were tracked but not included in POST SCD because they did not die suddenly. Similar to the SCAs that died in the field (i.e., presumed SCDs) in POST SCD, we hypothesized that the underlying causes of resuscitated SCAs may also be heterogeneous and distinct between SCA survivors and non-survivors, with implications for improving poor survival outcomes and refining resuscitation strategies. Therefore, we sought to determine underlying causes of arrest, survival outcomes, and predictors of survival for SCAs resuscitated to hospitalization in San Francisco County, California during the POST SCD study period via comprehensive review of hospitalization records following resuscitation.
Methods
Setting
The study population included all residents and inhabitants of San Francisco County, California (population: 805,235). Patients were identified through the 3 EMS agencies in San Francisco, California (with the San Francisco Fire Department responding to >85% of all 911 activations). All San Francisco EMS agencies contribute to CARES, and all cases submitted to CARES were reviewed. The study was approved by the University of California, San Francisco Institutional Review Board (IRB) and had additional IRB approval at all 10 San Francisco County adult hospitals and 3 EMS agencies to obtain medical records.
Inclusion Criteria and Case Definitions
All OHCAs aged 18–90 years in San Francisco County between February 1st, 2011 and January 1st, 2015 were included. OHCA was defined by EMS primary impression “cardiac arrest” as per CARES convention (4). OHCAs meeting WHO criteria for suddenness, i.e., cardiac arrest within 1 hour of symptom onset (witnessed), or within 24 hours of having been observed alive and symptom free (unwitnessed) were considered SCAs (10). SCAs that survived to hospital admission were defined as resuscitated SCAs but did not include those dying in the emergency department; the latter were considered SCDs and included in POST SCD. Resuscitated SCAs were further classified by subsequent inpatient death (SCA non-survivor) or survival to hospital discharge (SCA survivor).
The following OHCAs were excluded as they were not considered unexpected: (1) subjects with severe noncardiac chronic and terminal illness in which imminent death was not unexpected, including terminal cancer; (2) end-stage renal disease on dialysis; (3) hospice residents; (4) subjects with an identifiable noncardiac etiology of arrest at presentation, including evidence of drug abuse/overdose at the scene (e.g., intravenous needles, empty pill bottles), clear life-threatening trauma, homicide, or suicide; and (5) subjects who had hospital admission within the prior 30 days for noncardiac illness or surgical procedure.
Identification of SCAs and Underlying Causes of Arrest
OHCAs were evaluated for WHO criteria for SCA by review of EMS and hospitalization records. San Francisco Fire Department (SFFD) CARES cases and EMS records were obtained between February 1st, 2011 to January 1st, 2013. All CARES cases and EMS records were obtained from the two other private EMS agencies between February 1st, 2011 to January 1st, 2015. San Francisco County transitioned to a dual response system whereby both private EMS agencies and SFFD responded to all emergency calls in the latter years of the study. EMS response time was defined as the time from initial call to scene arrival. We also obtained comprehensive medical records of CARES identified cases from all San Francisco County adult hospitals (96% of cases had records available for review). Underlying cause of SCA was determined by comprehensive review of hospitalization records following resuscitation by two physicians (Z.H.T and S.R.). This review considered inpatient workup that included electrocardiograms, imaging data (echocardiograms, computed tomography scans, magnetic resonance scans), catheterization data, laboratory testing, microbiology data, and autopsy when performed. Arrhythmic cause was an arrest for which no identifiable non-arrhythmic cause was found (e.g., acute cerebrovascular accident, pulmonary embolism, hemorrhage, overdose) thus potentially rescuable with an ICD, but may have had underlying or associated cardiac disease such as acute or chronic coronary artery disease (CAD). Arrhythmic cause did not require ventricular tachycardia/fibrillation (VT/VF) as initial rhythm given the possibility that it may have degenerated to asystole by time of EMS arrival or have a precipitating rhythm of heart block. Notably, arrhythmic causes are distinct from non-arrhythmic, cardiac causes of SCA (e.g., tamponade, acute heart failure with pulmonary edema) which would not be rescuable with a defibrillator. Neurologic cause was defined as stroke, intracranial hemorrhage, or seizure.
Statistical Analysis
The characteristics of the study sample were summarized using means and proportions. For between-group comparisons, we used χ2, Fisher’s exact, analysis of variance, and two tailed t-tests as appropriate. Characteristics of the 133 resuscitated SCAs, including demographics, comorbidities, health related behaviors, medication use, resuscitation variables, were compared between survivors and non-survivors using unadjusted logistic models (Table 1). We used iterative chained equations to multiply impute missing data for multivariate analysis, combining results across the twenty completed datasets using standard methods to account for imputation error (11) (Supplemental Table 1). The final adjusted logistic model for survival was selected using backwards deletion, beginning with the subset of covariates with P≤ 0.1 in Table 1.
Table 1.
Case Characteristics by Survival to Hospital Discharge
| Resuscitated SCA |
||||
|---|---|---|---|---|
| Case Characteristics | Total (n=133) | SCA Non-survivor (n=86) | SCA Survivor (n=47) | P-Value (Non-survivor vs Survivor) |
| Age (years), mean (SD) | 67.4 (16.3) | 70.5 (16.1) | 60.3 (15.9) | <0.01 |
| Male, no. (%) | 87 (65.4) | 53 (61.6) | 34 (72.3) | 0.21 |
| Race / Ethnicity no. (%) | ||||
| Asian | 42 (31.6) | 30 (34.9) | 12 (25.5) | 0.27 |
| Black | 17 (12.8) | 12 (14) | 5 (10.6) | 0.58 |
| Hispanic | 12 (9) | 8 (9.3) | 4 (8.5) | 0.88 |
| White | 43 (32.3) | 21 (24.4) | 22 (46.8) | 0.01 |
| Other | 16 (12) | 12 (14) | 4 (8.5) | 0.42 |
| EMS Response Time (minutes), mean (SD) | 5.5 (3.6) | 5.9 (3.4) | 5 (3.7) | 0.23 |
| Cooling, no. (%) | 48 (36.1) | 25 (29.1) | 23 (49) | 0.02 |
| Witnessed, no. (%) | 81 (60.9) | 47 (54.7) | 34 (71.7) | 0.05 |
| Initial Rhythm, no. (%) | ||||
| Agonal/idioventricular | 3 (2.3) | 4 (4.6) | 1 (2.1) | 0.66 |
| Asystole | 22 (16.5) | 24 (27.9) | 3 (6.4) | <0.01 |
| NSR | 11 (8.3) | 9 (10.5) | 2 (4.3) | 0.33 |
| PEA | 13 (12.8) | 12 (13.9) | 1 (2.1) | 0.03 |
| VT/VF | 55 (41.4) | 18 (20.9) | 37 (78.7) | <0.01 |
| Other | 4 (3) | 4 (4.7) | 0 | |
| History of, no. (%) | ||||
| Hypertension | 74 (55.6) | 53 (61.6) | 21 (44.6) | 0.06 |
| Diabetes Mellitus | 35 (26.3) | 23 (26.7) | 12 (25.5) | 0.88 |
| Dyslipidemia | 44 (33.1) | 29 (33.7) | 15 (31.9) | 0.83 |
| Myocardial Infarction | 14 (10.5) | 7 (8.1) | 7 (14.9) | 0.23 |
| Congestive Heart Failure | 24 (18) | 19 (22.1) | 5 (10.6) | 0.10 |
| Atrial Fibrillation/Flutter | 21 (15.8) | 16 (18.6) | 5 (10.6) | 0.23 |
| Aortic Stenosis | 7 (5.3) | 6 (7) | 1 (2.1) | 0.42 |
| HIV | 4 (3) | 2 (2.3) | 2 (4.3) | 0.61 |
| Chronic Kidney Disease | 11 (8.3) | 9 (10.5) | 2 (4.3) | 0.33 |
| Seizure | 1 (0.8) | 1 (1.2) | 0 | |
| Psychiatric Illness | 14 (10.5) | 10 (11.6) | 4 (8.5) | 0.77 |
| COPD | 6 (4.5) | 4 (4.7) | 2 (4.3) | 0.92 |
| Non-metastatic Cancer | 12 (9) | 9 (10.5) | 3 (6.4) | 0.54 |
| Prior Stroke | 19 (14.3) | 18 (20.9) | 1 (2.1) | <0.01 |
| Migraines | 3 (2.3) | 1 (1.2) | 2 (4.3) | 0.25 |
| Alcohol Use, no. (%) | 26 (19.5) | 15 (17.4) | 11 (23.4) | 0.41 |
| Tobacco Use, no. (%) | 27 (20.3) | 19 (22.1) | 8 (17) | 0.49 |
| Illicit Drug Use, no. (%) | 3 (2.3) | 1 (1.2) | 2 (4.3) | 0.25 |
| Medications, no. (%) | ||||
| Anticoagulation | 21 (15.8) | 16 (18.6) | 5 (10.6) | 0.23 |
| Anti-platelet | 26 (19.5) | 15 (17.4) | 11 (23.4) | 0.41 |
| ACE/ARB | 32 (24.1) | 19 (22.1) | 13 (27.7) | 0.47 |
| Diuretic | 18 (13.5) | 11 (12.8) | 7 (14.9) | 0.73 |
| Beta Blocker | 32 (24.1) | 21 (24.4) | 11 (23.4) | 0.90 |
| Statin | 33 (24.8) | 20 (23.3) | 13 (27.7) | 0.57 |
| CCB | 13 (9.8) | 12 (14) | 1 (2.1) | 0.03 |
| Amlodipine | 9 (6.8) | 9 (10.5) | 0 | |
| Nifedipine | 1 (0.8) | 1 (1.2) | 0 | |
| Diltiazem | 2(1.5) | 1 (1.2) | 1 (2.1) | |
| Metformin | 10 (7.5) | 5 (5.8) | 5 (10.6) | 0.32 |
| PPI | 13 (9.8) | 8 (9.3) | 5 (10.6) | 0.77 |
| SSRI | 8 (6) | 8 (9.3) | 0 | 0.05 |
| Insulin | 4 (3) | 4 (4.7) | 0 | 0.30 |
| Anti-epileptic | 2 (1.5) | 2 (2.3) | 0 | 0.54 |
| Bronchodilator | 4 (3) | 3 (3.5) | 1 (2.1) | 0.66 |
| Methadone/opiate | 5 (3.8) | 4 (4.7) | 1 (2.1) | 0.46 |
| ARV | 4 (3) | 1 (1.2) | 3 (6.4) | 0.13 |
A Bolded P-values are less than or equal to 0.05. ACE= Angiotensin Converting Enzyme Inhibitor, ARB= Angiotensin Receptor Blocker, ARV= Antiretroviral, CCB=Calcium Channel Blocker, COPD= Chronic Obstructive Pulmonary Disease, HIV= Human Immunodeficiency Virus, NSR= Normal Sinus Rhythm, PEA= Pulseless Electrical Activity, PPI= Proton Pump Inhibitor, SSRI=Selective Serotonin Reuptake Inhibitor, VT/VF= Ventricular Tachycardia/Ventricular Fibrillation.
Results
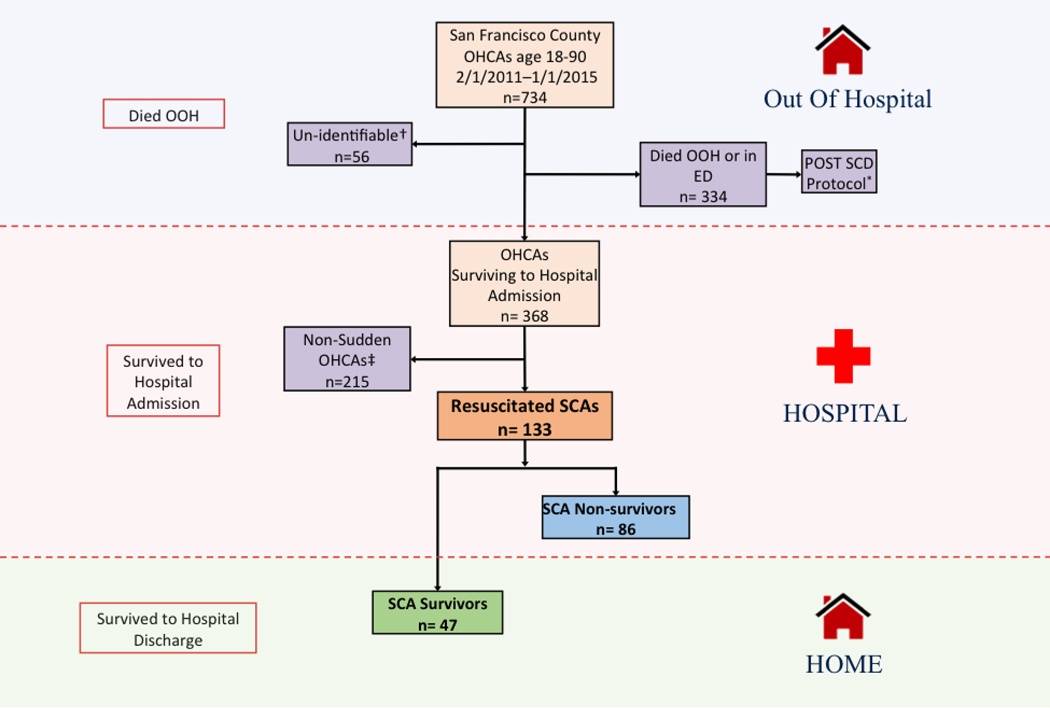
We identified 734 incident, countywide OHCAs over 48 months (Figure 1). Of these, 239 (32.4%) were sudden, i.e., met WHO SCA criteria, approximately half of which were resuscitated to hospitalization (133 of 239, 55.6%). Of the 133 SCAs resuscitated to hospitalization (resuscitated SCAs), 86 (64.7%) died during hospitalization (SCA non-survivors) and 47 (35.3%) survived to hospital discharge (SCA survivors). In sum, 19.7% (47 of 239) of all incident SCAs countywide survived to hospital discharge.
Figure 1. Identification of Resuscitated Sudden Cardiac Arrests.
SCAs aged 18–90 resuscitated to hospitalization in San Francisco County, CA were identified from 2/1/2011 to 1/1/2015. OHCAs dying in the field/ED were excluded but analyzed in the POST SCD Study. Non-sudden OHCAs were excluded. Of the 734 OHCAs analyzed, 133 met SCA criteria and were resuscitated to hospitalization (resuscitated SCAs), of which 86 died during hospitalization and 47 survived to hospital discharge. *Cases included in the POST SCD Study, but do not reflect the entirety of POST SCD cases because additional unwitnessed cases meeting WHO definition were included in the POST SCD protocol. † Unidentifiable cases (e.g., “John Doe”). ‡ Non-Sudden (n=107): end stage disease (n=53), skilled nursing facility (n=23), hospice (n=10), do not resuscitate (DNR) status (n=10), recent serious diagnosis (n=11). Not unexpected (n=108): symptoms > 1hr (n= 63), or suicide/trauma/overdose (n=45). OOH = Out of hospital, OHCA = Out of hospital cardiac arrest, POST SCD = POstmortem Systematic InvesTigation of Sudden Cardiac Death (POST SCD) Study, SCA = Sudden cardiac arrest.
Characteristics of SCA Survivors and Non-survivors
Mean age of the 133 resuscitated SCAs was 67.4 years (SD, 16.3), 66.2% were male, and the racial/ethnic composition reflected the diverse population of San Francisco County (Table 1). The mean age of SCA survivors was more than a decade younger (10.3 years) than SCA non-survivors (95% CI 4.5 to 16 years, P<0.001). SCA non-survivors had significantly higher prevalence of prior stroke (20.9% vs 2.1%, P= 0.003), and were more often prescribed calcium channel blockers (14% vs 2.1%, P=0.03) and selective serotonin reuptake inhibitors (9.3% vs 0%, P= 0.05). Mean EMS response time was similar in SCA survivors and non-survivors (5 minutes vs. 5.9 minutes, P=0.23), and comparable to that for witnessed SCAs resulting in out-of-hospital death included in POST SCD (5.9 minutes). EMS response time was also similar between Whites and Non-Whites (Supplemental Table 2). We observed that more SCA survivors were witnessed than SCA non-survivors (33 of 47 [70.2%] vs 46 of 86 [53.5%], P=0.05). VT/VF was the most common presenting rhythm, found in 55 (41.3%) of resuscitated SCAs, and more common in SCA survivors than non-survivors (78.7% vs 20.9%, P<0.001) despite similar mean EMS response time for VT/VF vs. non-VT/VF rhythms (6 minutes vs. 5.1 minutes, P=0.25). Rates of VT/VF were similar between Whites and Non-Whites (Supplemental Table 2).
Underlying Causes of Arrest
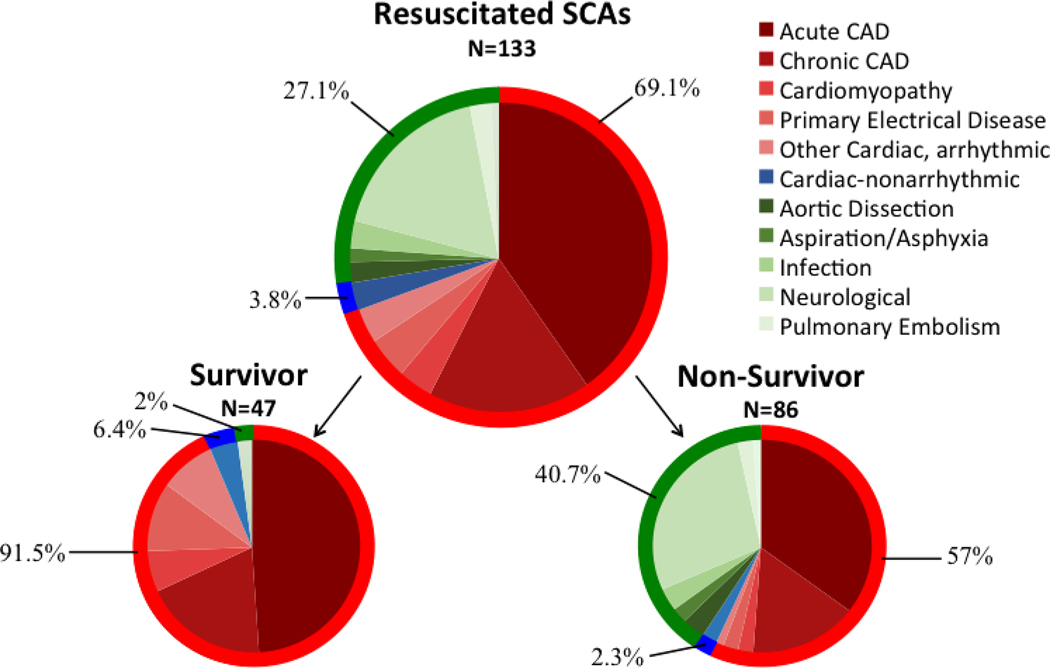
The most common causes of arrest for all resuscitated SCAs were acute coronary artery disease (acute coronary syndrome with or without ST elevation, 39.8%), neurologic (18%), and chronic coronary artery disease (known CAD and no other clear cause, 16.5% [Table 2]). Arrhythmic causes of arrest were found in 69.1% (92 of 133) of resuscitated SCAs, significantly higher than the 55.8% of SCAs resulting in sudden death (i.e., WHO-defined SCD) found by autopsy as reported in POST SCD (P=0.004, Central Illustration). Arrhythmic cause was significantly more common in survivors than non-survivors (92% vs. 57%, P< 0.001; Figure 2).
Table 2.
Adjudicated Etiologies of Resuscitated SCAs by Survival to Discharge Resuscitated SCA.
| Resuscitated SCAs |
||||
|---|---|---|---|---|
| Case of Arrest | Total (n=133) | Non-survivors (n=86) | Survivors (n=47) | P-Value (survivor vs Non-Survivors) |
| Arrhythmic, no. (%) | 92 (69.1) | 49 (57) | 43 (91.5) | <0.01 |
| Acute CAD | 53 (39.8) | 31 (34.9) | 22 (46.8) | 0.11 |
| Chronic CAD | 22 (16.5) | 13 (16.3) | 9 (19.1) | 0.68 |
| Cardiomyopathy | 5 (3.8) | 2 (2.3) | 3 (6.4) | 0.35 |
| Hypertrophy | 0 | 0 | 0 | |
| Primary Electrical Disease | 7 (5.3) | 2 (2.3) | 5 (10.6) | 0.10 |
| Other Cardiac, arrhythmic | 5 (3.8) | 1 (1.2) | 4 (8.5) | 0.05 |
| Non-arrhythmic/Cardiac | 5 (3.8) | 2 (2.3) | 3 (6.4) | 0.61 |
| Non-Cardiac | 36 (27.1) | 35(40.7) | 1 (2) | <0.01 |
| Acute Renal Failure | 0 | 0 | 0 | 0.55 |
| Aortic Dissection | 3 (2.3) | 3 (3.5) | 0 | |
| Aspiration/Asphyxia | 2 (1.5) | 2 (2.3) | 0 | 0.54 |
| Chemical Overdose | 0 | 0 | 0 | |
| GI Hemorrhage/Other GI | 0 | 0 | 0 | |
| Hypo/Hyperglycemia/DKA | 0 | 0 | 0 | |
| Infection | 3 (2.3) | 3 (3.5) | 0 | 0.55 |
| Neurological | 24 (18) | 24 (27.9) | 0 | <0.01 |
| Pulmonary Embolism | 3 (2.3) | 2 (2.3) | 1 (2) | 1 |
| Other Non-Cardiac | 1 (0.8) | 1 (1.2) | 0 | 1 |
Adjudicated etiologies of resuscitated SCAs surviving to hospital admission after review of comprehensive hospitalization records (69.2%=cardiac arrhythmic, 27.1%=Noncardiac, 3%= Cardiac Non-arrhythmic. Non-Survivor. Adjudicated etiologies of resuscitated SCAs who died during initial inpatient hospitalization (55.8%= Cardiac-arrhythmic, 41.9%=Non-cardiac, 2.3%=Cardiac Non-arrhythmic). Survivor.Adjudicated etiologies of resuscitated SCAs who survived to hospital admission (91.5%= Cardiac-arrhythmic, 4.3%=Cardiac Non-arrhythmic, 2%=Non-cardiac). Bolded P-values are less than or equal to 0.05. CAD=Coronary Artery Disease, DKA=Diabetic Ketoacidosis, GI=gastrointestinal, SCA=Sudden Cardiac Arrest.
Figure 2. Adjudicated Causes of Resuscitated SCAs.
Etiologies of resuscitated SCAs as determined by review of EMS runsheets and hospitalization records after admission for resuscitated SCA. Causes of arrest were classified as arrhythmic (red), cardiac-nonarrhythmic (blue), and non-cardiac (green). CAD=Coronary Artery Disease.
Central Illustration. Underlying Causes of SCA By Resuscitation and Survival Status. All OHCAs between 2/1/2011 and 1/1/2015 in San Francisco County, CA were identified through EMS agencies. OHCAs dying in the field/ED (POST SCD cases) or non-sudden were excluded, to arrive at SCAs resuscitated to hospitalization. Causes of resuscitated SCA were determined after review of comprehensive hospital records: arrhythmic (red), cardiac/non-arrhythmic (blue), or non-cardiac causes (green). Arrhythmic causes accounted for 69.1% (92 of 133) of resuscitated SCAs, significantly higher than the 55.8% of SCAs resulting in WHO-defined (presumed) SCDs by autopsy as reported in POST SCD (P=0.004). Arrhythmic cause was significantly more common in survivors than non-survivors (92% vs. 57%, P< 0.001). * N=525 total presumed SCDs as previously reported,9 including 334 OHCAs identified in this study with initial signs of life but dying on scene/ED and an additional 191 EMS-attended cases in POST SCD without signs of life but with primary impression OHCA. † P-value survivors vs. non-survivors.
Neurologic causes of arrest were universally fatal despite initial resuscitation (28% of SCA non-survivors vs. 0% of SCA survivors, P<0.001). Over half of resuscitated SCAs with a prior stroke (10 of 19, 53%) were subsequently found to have a precipitating neurologic cause. The majority (20 of 24, 83.3%) of neurologic SCAs were hemorrhagic strokes, all of which were prescribed anticoagulation or antiplatelet medications at the time of arrest.
Predictors of SCA Survival to Hospital Discharge
In multivariate analysis, White race (adjusted odds ratio [aOR] 4.04, 95% CI 1.21 to 13.56, P=0.02), presenting rhythm of VT/VF (aOR 19.26, 95% CI 5.25 to 70.59, P<0.01), and arrhythmic cause (aOR 5.29, 95% CI 1.38 to 20.34, P=0.02) were statistically significant predictors of survival to hospital discharge after resuscitated SCA (Table 3). Conversely, history of prior stroke was associated with reduced odds of survival (aOR 0.02, 95% CI 0 to 0.45, P=0.01). While no medications were associated with increased odds of survival, calcium channel blockers were independently associated with reduced odds of survival (aOR 0.06, 95% CI 0 to 0.8, P=0.04). Of note, of 12 SCA non-survivors prescribed calcium channel blockers, 7 had underlying arrhythmic cause, 4 neurologic cause, and 1 non-arrhythmic cause. Because neurologic cause of arrest had 100% mortality, this was not included in the multivariate model. Multiply imputed variables used in logistic models were similar to observed case variables (Supplemental Table 1).
Table 3.
Independent Predictors of Survival to Discharge after Admission for Resuscitated SCA
| Predictor | Adjusted Odds Ratio (95% CI) | P-Value |
|---|---|---|
| Race/Ethnicity | ||
| White | 3.6 (1.2–10.5) | 0.02 |
| Presenting Rhythm | ||
| VT/VF | 13.4 (4.4–40.8) | <0.01 |
| History Of | ||
| Stroke | 0.06 (0.01–0.59) | 0.02 |
| Medications | ||
| CCB | 0.08 (0.01–1.01) | 0.05 |
| Arrhythmic Etiology | 4.6 (1.3–16.4) | 0.02 |
CCB= Calcium Channel Blocker, CHF= Congestive Heart Failure, VT/VF= Ventricular Tachycardia/Ventricular Fibrillation.
Discussion
In this 4-year study of all incident OHCAs in San Francisco County, we found that only one-third were sudden; half of these SCAs were resuscitated to hospitalization and 1 in 5 survived to hospital discharge. Underlying arrhythmic cause accounted for 92% of resuscitated SCAs surviving to discharge, significantly higher than the 56% for SCAs dying in the field (i.e., WHO-defined SCDs) as reported in the contemporaneous POST SCD Study (9). Among SCAs surviving to hospitalization, we identified a presenting rhythm of VT/VF, underlying arrhythmic cause, and White race as independent predictors of survival to discharge. Notably, the nearly 1 in 5 SCAs with underlying neurologic catastrophe had a universally fatal outcome with 100% in-hospital mortality despite initial resuscitation. These data suggest that resuscitated SCA, especially the survivor, is a condition distinct from SCD and should not be equated, particularly since EMS response times were similar. Recognition of underlying causes of SCAs is essential to advancing the field and study of resuscitation and may ultimately help guide refinement of resuscitation algorithms and enable treatments more precisely directed towards the underlying cause of arrest.
Studies of OHCAs typically do not distinguish acuity of arrest, i.e., whether an arrest was sudden –not surprising given that first responders are focused on resuscitative efforts. These studies estimate that approximately 80% of OHCAs are due to underlying cardiac causes (12–15). However, OHCA classification criteria such as CARES have significant heterogeneity and presume primary cardiac etiology by requiring only an EMS primary impression of cardiac arrest (5,16,17). Moreover, many SCD studies equate SCA with SCD. However as we reported in POST SCD, presumed SCDs as defined by WHO criteria had only 56% positive predictive value for actual arrhythmic deaths, the only type of sudden death potentially rescuable with a defibrillator, nearly identical to the 57% for SCA non-survivors we found. We found a similar lack of specificity for resuscitated SCAs presumed cardiac by CARES convention since less than 7 in 10 had actual arrhythmic causes after comprehensive review of hospital workup. Our refined population of resuscitated SCAs with confirmed arrhythmic causes had a higher rate of survival to discharge (20%) than in a 2010 meta-analysis of international OHCAs (7.6%) (1) and in a more recent report after incorporation of updated 2010 resuscitation guidelines (16%) (18), likely due in part to a substantial proportion of non-sudden and non-cardiac cases misclassified as OHCAs in those studies. Thus resuscitated SCAs are a distinct phenotype from SCAs that result in death out-of-hospital (i.e., presumed SCDs) or death in-hospital after resuscitation (i.e., SCA non-survivors). Indeed the common practice of mixing these phenotypes may contribute to negative findings in recent large genetic association studies of SCA/SCD (19).
We found that underlying arrhythmic cause was an independent predictor of survival to hospital discharge after admission for resuscitated SCA. This is not surprising as current resuscitation algorithms and automated external defibrillators are designed to treat these etiologies, thus enriching survivors for treatable arrhythmic causes. Arrhythmic cases are likely more survivable than non-arrhythmic cases as they often are more readily reversed. Our finding of improved outcomes among Whites is consistent with prior studies demonstrating lower rates of cardiac arrest survival in minority populations which have longer EMS response times, lower rates of bystander CPR, and less frequently present with VT/VF (20–22). However, EMS response times and prevalence of VT/VF were similar for all races, therefore other unmeasured factors, such as socioeconomic status, may account for the racial differences in SCA survival we observed. Future research may be directed at these disparities to improve minority survival after SCA.
The presenting rhythm in 80% of survivors was VT/VF, consistent with prior studies which have consistently demonstrated that VT/VF is an independent predictor of survival (1,5,23–25). In our study, presenting rhythm of VT/VF was not a function of EMS response time as this was similar for non-VT/VF rhythms. Notably, only 1 of 13 (8%) of PEA arrests survived to hospital discharge. This reinforces the prognostic importance of presenting rhythm. While some events that are not cardiac may be addressed by defibrillation and advanced cardiac life support, and indeed our population of SCAs had all been initially successfully resuscitated, we discovered an array of non-arrhythmic causes after initial successful resuscitation that are not addressed by current resuscitation protocols, which likely contributed to the 80% mortality in this countywide population of resuscitated SCAs. This is consistent with our observations in POST SCD that despite successful defibrillator shocks for VF or continuous rhythm monitoring that documented complete heart block, some out-of-hospital SCD victims still died suddenly of non-cardiac causes (26,27). Thus, extending the examination of SCAs beyond the lens of rhythms treatable or not treatable by defibrillators to identify and address their diverse underlying causes may help effect the next leap in resuscitation science.
Neurologic catastrophes, chiefly intracranial hemorrhage, accounted for almost 1 in 5 SCAs and were 100% fatal despite resuscitation to hospitalization. This observation extends our prior findings of unrecognized sudden neurologic death among presumed SCDs (27) to resuscitated SCAs and confirms that underlying neurologic catastrophes may be inherently less survivable. Neurologic cause of arrest was not included in the multivariate analysis because it was fully predictive of mortality, yet we found that history of prior stroke, present in over half of neurologic SCAs, was an independent negative predictor of survival. Notably, therapeutic hypothermia was used significantly more commonly in SCA survivors but was not independently associated with survival, likely due to selection criteria for therapeutic hypothermia.
The majority (20 of 24, 83.3%) of neurologic SCAs were hemorrhagic strokes, all of which were prescribed anticoagulation or antiplatelet medications at the time of arrest. Therefore SCAs due to neurologic cause may represent a high-impact target to improve survival as any improvement in outcomes would represent an improvement over the 100% mortality we found. Strategies may include early EMS screening for history of prior stroke to identify cases for early triage to a specialized stroke center (over half of resuscitated SCAs with a prior stroke in this study were found to have a repeat neurologic catastrophe) or rapid assessment on scene for anticoagulant or antiplatelet prescription to allow for expedited, targeted therapy such as reversal of anticoagulation or neurosurgical intervention. Notably, antiplatelet and anticoagulant trials (28,29) may have missed intracranial hemorrhages presenting as OHCAs or SCD, therefore the risk associated with these medications may be underestimated.
We found that prescription for calcium channel blockers was a negative predictor of survival to discharge after resuscitated SCA. Previous studies show that the dihydropyridine calcium channel blocker nifedipine is associated with increased risk of OHCA (30), therefore our findings may extend the risk to lower survival after resuscitated OHCA. This may be due to increased sympathetic tone following rapid reduction in blood pressure with dihydropyridine calcium channel blockers or coronary steal from collateral arteries, however, this finding may not extend to other calcium channel blockers. We also found that a prescription for SSRIs was found exclusively in SCA non-survivors; half of SCAs in our study who were on SSRIs had intracranial hemorrhages. While this finding may be due to chance, it is also consistent with prior reports of the association of SSRIs with platelet dysfunction and increased risk of hemorrhagic stroke, especially in those taking anticoagulant or antiplatelet medications (31,32).
Limitations
A major strength of our study is the high capture rate of countywide SCAs over the 4-year study period, but some limitations are worth noting. First, SFFD records were unavailable for the later period of the study; however, in the latter years of the study San Francisco County transitioned to a dual response system, therefore we have captured the vast majority of cases during the study period. Second, some OHCA victims were not identifiable (e.g., homeless status), though these cases accounted for only 7.6% of the original sample. Third, only one autopsy record was available for the SCA non-survivors, consistent with low prevailing autopsy rates for in-hospital deaths. However, SCA victims resuscitated to hospitalization in this study generally had hospital workup more than sufficient to adjudicate underlying cause. Thus, while very few cases underwent autopsy, postmortem investigation would be of less yield than for out-of-hospital SCDs who (outside of the POST SCD Study) typically receive no investigation after the event and thus cardiac cause is presumed. Fourth, although our study was performed in a single metro area, the diverse nature of San Francisco County is an advantage, allowing us to report these outcomes in minority populations underrepresented in SCA and SCD databases. Generalizability is a concern of any study, yet clinically useful risk score and prediction models are often generalized beyond their source populations (e.g., Framingham, Oregon Sudden Unexplained Death Study) (33,34). Moreover, we are reassured that some of the factors identified in our study (e.g., higher survival with VT/VF) replicate those identified in previous studies, suggesting that the San Francisco SCA population is similar to other SCA cohorts thus our other novel findings may be generalizable to SCA as a whole. Fifth, we were limited by the variable degree of hospital evaluation after admission for resuscitated SCA to determine the underlying cause. However, the large majority of cases had an easily identifiable and often unequivocal cause of arrest (e.g., acute plaque rupture, massive subarachnoid hemorrhage, etc.), therefore our resuscitated SCAs refined for underlying causes represents a significant improvement over prior studies based entirely on EMS initial impression. Moreover, because we found that SCA non-survivors and SCAs dying in the field, i.e., presumed SCDs in POST SCD, had a nearly identical proportion of arrhythmic cause (57% vs. 56%), SCAs causing death likely represent a phenotypically distinct population than the small minority that ultimately survive to discharge and clinical follow-up.
Conclusions
In this 4-year countywide study of incident OHCAs, only one-third were sudden, of which half were resuscitated to hospitalization and 1 in 5 survived to discharge. Underlying cause had a significant impact on survival - with arrhythmic cause found in 92% of SCAs that survived to hospital discharge but only 57% of non-survivors. These results suggest that conventional definitions of cardiac arrest poorly specify actual arrhythmic cause; specifying suddenness and separating the outcomes of resuscitated SCAs and SCDs may help refine future analyses of OCHAs. Early identification of non-arrhythmic SCAs such as neurologic emergencies may be a target to improve OHCA survival.
Supplementary Material
PERSPECTIVES.
Competency in Medical Knowledge:
Several non-cardiac conditions can predispose to high mortality among both initial survivors of out-of-hospital cardiac arrest, including stroke, sepsis, and pulmonary embolism.
Translational Outlook:
Analysis of systematically collected data on clinical phenotypes, mechanisms and therapies could improve outcomes for victims of cardiac arrest.
Acknowledgements:
We are grateful to all victims of sudden cardiac arrest and their families and for the efforts of all EMS personnel in San Francisco County.
Sources of Funding: This study was funded by NIH R01 HL102090 (NHLBI to ZHT). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH.
Disclosures: Dr. Tseng reports grants from NIH/NHLBI and CDC during the conduct of the study, and personal fees from Biotronik, outside the submitted work. Dr. Salazar reports a grant (Award No. R38HL143581) from the NHLBI. Drs. Ricceri, Vu, Moffatt, and Vittinghoff report no disclosures.
Abbreviations:
- CARES
Cardiac Arrest Registry to Enhance Survival
- CDC
Center for Disease Control
- EMS
Emergency Medical Service
- SCA
Sudden Cardiac Arrest
- SCD
Sudden Cardiac Death
- OHCA
Out of Hospital Cardiac Arrest
- SAD
Sudden Arrhythmic Death
- POST SCD
POstmortem Systematic InvesTigation of Sudden Cardiac Death
- WHO
World Health Organization
- VT/VF
Ventricular Tachycardia/Ventricular Fibrillation
Footnotes
Publisher's Disclaimer: This is a PDF file of an article that has undergone enhancements after acceptance, such as the addition of a cover page and metadata, and formatting for readability, but it is not yet the definitive version of record. This version will undergo additional copyediting, typesetting and review before it is published in its final form, but we are providing this version to give early visibility of the article. Please note that, during the production process, errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Sasson C, Rogers MAM., Dahl J, Kellermann AL. Predictors of Survival From Out-of-Hospital Cardiac Arrest. Circ Cardiovasc Qual Outcomes. 2010;3(1):63–81. doi: 10.1161/CIRCOUTCOMES.109.889576 [DOI] [PubMed] [Google Scholar]
- 2.Chugh SS, Jui J, Gunson K, et al. Current burden of sudden cardiac death: Multiple source surveillance versus retrospective death certificate-based review in a large U.S. community. J Am Coll Cardiol. 2004;44(6):1268–1275. doi: 10.1016/j.jacc.2004.06.029 [DOI] [PubMed] [Google Scholar]
- 3.Nichol G, Rumsfeld J, Eigel B, et al. Essential Features of Designating Out-of-Hospital Cardiac Arrest as a Reportable Event. Circulation. 2008;117(17):2299–2308. doi: 10.1161/CIRCULATIONAHA.107.189472 [DOI] [PubMed] [Google Scholar]
- 4.Narayan SM., Wang PJ., Daubert JP. New Concepts in Sudden Cardiac Arrest to Address an Intractable Epidemic. J Am Coll Cardiol. 2019;73(1):70–88. doi: 10.1016/j.jacc.2018.09.083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McNally B, Stokes A, Crouch A, Kellermann AL. CARES: Cardiac Arrest Registry to Enhance Survival. Ann Emerg Med. 2009;54(5):674–683.e2. doi: 10.1016/j.annemergmed.2009.03.018 [DOI] [PubMed] [Google Scholar]
- 6.Hayashi M, Shimizu W, Albert CM. The Spectrum of Epidemiology Underlying Sudden Cardiac Death. Circ Res. 2015;116(12):1887–1906. doi: 10.1161/CIRCRESAHA.116.304521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rohde LE., Chatterjee NA., Vaduganathan M, et al. Sacubitril/Valsartan and Sudden Cardiac Death According to Implantable Cardioverter-Defibrillator Use and Heart Failure Cause. JACC Heart Fail. 2020;8(10):844–855. doi: 10.1016/j.jchf.2020.06.015 [DOI] [PubMed] [Google Scholar]
- 8.Chatterjee NA, Moorthy MV, Pester J, et al. Sudden Death in Patients With Coronary Heart Disease Without Severe Systolic Dysfunction. JAMA Cardiol. 2018;3(7):591–600. doi: 10.1001/jamacardio.2018.1049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tseng ZH., Olgin JE., Vittinghoff E et al. Prospective Countywide Surveillance and Autopsy Characterization of Sudden Cardiac Death. Circulation. 2018;137(25):2689–2700. doi: 10.1161/CIRCULATIONAHA.117.033427 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.World Health Organization. Sudden Cardiac Death. World Health Organization Technical Report Series, Report 726. 1985. [PubMed] [Google Scholar]
- 11.Barnard J, Meng X-L. Applications of multiple imputation in medical studies: from AIDS to NHANES: Stat Methods Med Res. Published online July 2, 2016. doi: 10.1177/096228029900800103 [DOI] [PubMed] [Google Scholar]
- 12.Fischer M, Fischer NJ, Schüttler J. One-year survival after out-of-hospital cardiac arrest in Bonn city: outcome report according to the ‘Utstein style.’ Resuscitation. 1997;33(3):233–243. doi: 10.1016/S0300-9572(96)01022-2 [DOI] [PubMed] [Google Scholar]
- 13.Pijls RWM, Nelemans PJ, Rahel BM, Gorgels APM. Circumstances and causes of sudden circulatory arrests in the Dutch province of Limburg and the involvement of citizen rescuers. Neth Heart J. 2018;26(1):41–48. doi: 10.1007/s12471-017-1057-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kuisma M, Alaspää A. Out-of-hospital cardiac arrests of non-cardiac originEpidemiology and outcome. Eur Heart J. 1997;18(7):1122–1128. doi: 10.1093/oxfordjournals.eurheartj.a015407 [DOI] [PubMed] [Google Scholar]
- 15.Ro YS, Shin SD, Song KJ, et al. A comparison of outcomes of out-of-hospital cardiac arrest with non-cardiac etiology between emergency departments with low- and high-resuscitation case volume. Resuscitation. 2012;83(7):855–861. doi: 10.1016/j.resuscitation.2012.02.002 [DOI] [PubMed] [Google Scholar]
- 16.Hinkle LE, Thaler HT. Clinical classification of cardiac deaths. Circulation. 1982;65(3):457–464. doi: 10.1161/01.CIR.65.3.457 [DOI] [PubMed] [Google Scholar]
- 17.Perkins GD., Jacobs IG, Nadkarni VM., et al. Cardiac Arrest and Cardiopulmonary Resuscitation Outcome Reports: Update of the Utstein Resuscitation Registry Templates for Out-of-Hospital Cardiac Arrest. Circulation. 2015;132(13):1286–1300. doi: 10.1161/CIR.0000000000000144 [DOI] [PubMed] [Google Scholar]
- 18.Pasupula DK, Bhat A, Siddappa MSK., et al. Impact of Change in 2010 American Heart Association Cardiopulmonary Resuscitation Guidelines on Survival After Out-of-Hospital Cardiac Arrest in the United States. Circ Arrhythm Electrophysiol. 2020;13(2):e007843. doi: 10.1161/CIRCEP.119.007843 [DOI] [PubMed] [Google Scholar]
- 19.Ashar FN, Mitchell RN, Albert CM, et al. A comprehensive evaluation of the genetic architecture of sudden cardiac arrest. Eur Heart J. 2018;39(44):3961–3969. doi: 10.1093/eurheartj/ehy474 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Galea S, Blaney S, Nandi A, et al. Explaining Racial Disparities in Incidence of and Survival from Out-of-Hospital Cardiac Arrest. Am J Epidemiol. 2007;166(5):534–543. doi: 10.1093/aje/kwm102 [DOI] [PubMed] [Google Scholar]
- 21.Becker LB, Han BH, Meyer PM, et al. Racial Differences in the Incidence of Cardiac Arrest and Subsequent Survival. N Engl J Med. 1993;329(9):600–606. doi: 10.1056/NEJM199308263290902 [DOI] [PubMed] [Google Scholar]
- 22.Nichol G, Thomas E, Callaway CW, et al. Regional Variation in Out-of-Hospital Cardiac Arrest Incidence and Outcome. JAMA. 2008;300(12):1423–1431. doi: 10.1001/jama.300.12.1423 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Myat A, Song K-J, Rea T. Out-of-hospital cardiac arrest: current concepts. The Lancet. 2018;391(10124):970–979. doi: 10.1016/S0140-6736(18)30472-0 [DOI] [PubMed] [Google Scholar]
- 24.Lombardi G, Gallagher EJ, Paul. Outcome of Out-of-Hospital Cardiac Arrest in New York City: The Pre-Hospital Arrest Survival Evaluation (PHASE) Study. JAMA. 1994;271(9):678–683. doi: 10.1001/jama.1994.03510330056034 [DOI] [PubMed] [Google Scholar]
- 25.Eid SM, Abougergi MS, Albaeni A, Chandra-Strobos N. Survival, expenditure and disposition in patients following out-of-hospital cardiac arrest: 1995–2013. Resuscitation. 2017;113:13–20. doi: 10.1016/j.resuscitation.2016.12.027 [DOI] [PubMed] [Google Scholar]
- 26.Tseng ZH, Hayward RM, Clark NM, et al. SUdden death in patients with cardiac implantable electronic devices. JAMA Intern Med. 2015;175(8):1342–1350. doi: 10.1001/jamainternmed.2015.2641 [DOI] [PubMed] [Google Scholar]
- 27.Kim AS, Moffatt E, Ursell PC, Devinsky O, Olgin J, Tseng ZH. Sudden neurologic death masquerading as out-of-hospital sudden cardiac death. Neurology. 2016;87(16):1669–1673. doi: 10.1212/WNL.0000000000003238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lopes RD, Heizer G, Aronson R, et al. Antithrombotic Therapy after Acute Coronary Syndrome or PCI in Atrial Fibrillation. N Engl J Med. 2019;380(16):1509–1524. doi: 10.1056/NEJMoa1817083 [DOI] [PubMed] [Google Scholar]
- 29.Yusuf S, Zhao F, Mehta SR, et al. Effects of clopidogrel in addition to aspirin in patients with acute coronary syndromes without ST-segment elevation. N Engl J Med. 2001;345(7):494–502. doi: 10.1056/NEJMoa010746 [DOI] [PubMed] [Google Scholar]
- 30.Eroglu TE, Mohr GH, Blom MT, et al. Differential effects on out-of-hospital cardiac arrest of dihydropyridines: real-world data from population-based cohorts across two European countries. Eur Heart J - Cardiovasc Pharmacother. doi: 10.1093/ehjcvp/pvz038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hackam DG, Mrkobrada M. Selective serotonin reuptake inhibitors and brain hemorrhage: a meta-analysis. Neurology. 2012;79(18):1862–1865. doi: 10.1212/WNL.0b013e318271f848 [DOI] [PubMed] [Google Scholar]
- 32.Renoux C, Vahey S, Dell’Aniello S, Boivin J-F. Association of Selective Serotonin Reuptake Inhibitors With the Risk for Spontaneous Intracranial Hemorrhage. JAMA Neurol. 2017;74(2):173–180. doi: 10.1001/jamaneurol.2016.4529 [DOI] [PubMed] [Google Scholar]
- 33.Chugh SS, Reinier K, Balaji S, et al. Population-Based Analysis of Sudden Death in Children: The Oregon Sudden Unexpected Death Study. Heart Rhythm Off J Heart Rhythm Soc. 2009;6(11):1618–1622. doi: 10.1016/j.hrthm.2009.07.046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wilson PWF., D’Agostino RB, Levy D, Belanger AM, Silbershatz H, Kannel WB. Prediction of Coronary Heart Disease Using Risk Factor Categories. Circulation. 1998;97(18):1837–1847. doi: 10.1161/01.CIR.97.18.1837 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.