Abstract
Background
Computed tomography (CT) has traditionally been the first-line imaging method in neck emergencies such as deep neck infections. Due to superior soft-tissue contrast, magnetic resonance imaging (MRI) may be an alternative to CT, also in emergency situations.
Purpose
To characterize the use of routine MRI in neck emergencies, with an emphasis on clinical feasibility and diagnostic accuracy in cases of neck infection.
Material and Methods
We conducted a retrospective cohort study of all primary neck MRI scans performed using a 3-T MRI device during a five-year follow-up period in a tertiary emergency radiology department. Imaging data were compared with final clinical diagnosis and surgical findings as reference standards.
Results
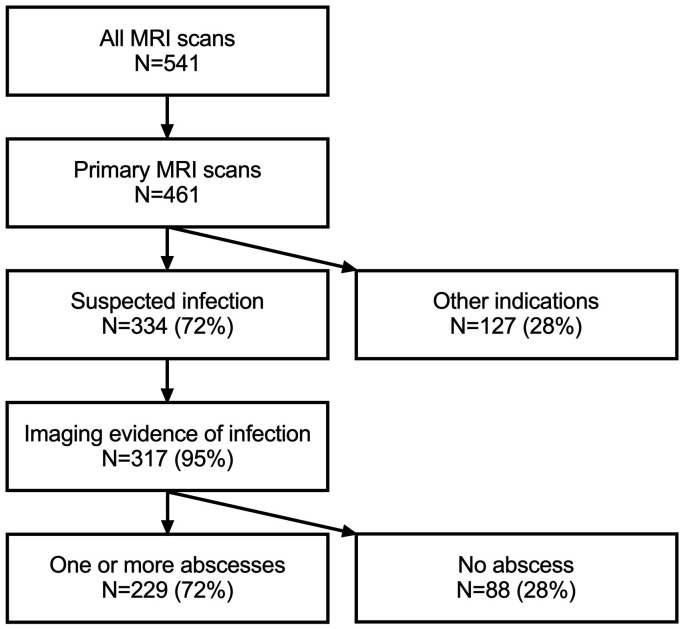
The search identified 461 primary neck MRI scans, of which 334 (72%) were performed on the basis of clinical suspicion of infection. Radiological evidence of infection was observed in 95% of these scans, and at least one abscess was detected in 229 cases (72% of confirmed infection). MRI had an overall technical success rate of 95% and had high positive predictive value for both infection (0.98) and detection of abscess (0.95).
Conclusion
We found that emergency neck MRI can be successfully performed on most patients, and that MRI detects neck infection with a high accuracy. These results suggest that MRI may be an alternative to CT as the first or only imaging modality in neck emergencies.
Keywords: Magnetic resonance imaging, neck, emergency medicine, infection
Introduction
Neck emergencies are medical conditions that require immediate diagnosis and intervention. Common causes include trauma, infection, tumors, and various postoperative complications. Potentially fatal complications include airway compromise, vascular complications, and spread of infection through sepsis. Assessing the compartmental boundaries of the disease is difficult because of the complexity of the neck anatomy. Odontogenic neck infections are typically diagnosed early during clinical examination and panoramic radiographs. Together with clinical examination, cross-sectional radiological imaging aids the diagnostic process when deep neck infection is suspected (1). The exact origin, location, and extent of infection are often difficult to define accurately on clinical grounds because of neck swelling and restricted mouth opening. This information becomes particularly important in the presence of drainable abscesses. Importantly, imaging can help predict the potential spread of the infection into adjacent regions. Finally, imaging may reveal a risk of dangerous airway narrowing or thrombophlebitis.
Using contrast-enhanced computed tomography (CT) for emergency neck imaging is currently routine because it is fast, readily available, and relatively inexpensive (2–4). However, limited soft-tissue contrast and artifacts from bone and dental implants may compromise accurate delineation of neck disease (5). The diagnostic accuracy of CT in the detection of neck abscesses is limited, and about 20% have been false positives in larger studies using surgical findings as a reference standard (6–8). In addition, ionizing radiation from CT is a potential concern in younger age groups. Magnetic resonance imaging (MRI) provides superior soft-tissue characterization to CT (5). A previous comparative head-to-head comparison within the same patients with neck infection between these modalities suggested that MRI was superior to CT in terms of lesion conspicuity and number of affected spaces (9). Nevertheless, MRI is currently less often used in emergency settings as the first or only imaging modality, most likely due to its lack of availability, longer scanning time, reporting difficulty, and higher cost. The feasibility and diagnostic accuracy of MRI as the first or only modality in neck emergencies are unknown.
In this retrospective cohort study, we systematically reviewed imaging and clinical data from a five-year time period during which patients were scanned using 3-T MRI for suspected neck emergency in a tertiary care center. We sought to characterize the clinical use of emergency neck MRI as a first-line imaging method, especially for patients with suspected deep neck infection. To assess the diagnostic accuracy of the neck infections, we compared the MRI findings with the clinical diagnosis of infection and surgical findings as a reference standard.
Material and Methods
Turku University Hospital (Turku, Finland) is an academic tertiary care referral center with an approximate patient catchment area of 480,000, constituting the third largest hospital district in Finland. The emergency radiology department has attending radiologists between 08:00 and 22:00 on weekdays (12:00 to 20:00 on weekends). Between 22:00 and 08:00, one radiologist (resident or attending) is on duty, with possible back-up consultation by a specialist. MRI cases read outside 08:00 to 22:00 and/or by resident radiologists are currently second-read by a specialist the next day at the latest (either generalists, emergency radiologists, or neuroradiologists), although this process was not yet systematic during the study interval. The MRI device is located in the emergency radiology department.
In the present study, we retrospectively reviewed patients who had received an MRI of the neck soft tissues between 1 April 2013 and 30 April 2018. We obtained permission from the hospital district board. Written patient consent was waived due to the retrospective nature of the study. Cases were identified from picture archiving and communication systems (PACS) and radiological information systems (RIS) using standard neck MRI codes, and data were cross-referenced with patient medical files. We considered only primary scans (first emergency MRI). No follow-up scans on the same MRI device or follow-up scans after surgical treatment (when primary scanning had been performed elsewhere) were further examined. However, MRI scans were considered primary scans if a recent CT scan was deemed inadequate and a follow-up MRI was performed to gain more specific information. To examine whether MRI immediately replaced CT as the primary modality in emergency neck imaging, we also reviewed primary neck CT scans from the same time period.
MRI was performed on a Philips Ingenia 3-T system using dS HeadNeckSpine coil configuration (Philips Healthcare, Best, Netherlands). Details of the MRI protocol can be found in Supplemental material. These protocols were carried out in approximately 30 min of scanner time. Absolute MRI contraindications included an unknown magnetizing foreign object and high fever (>38°C or 100°F). We routinely administered gadolinium to all except three adult patients, due to kidney failure, denial of intravenous access, and pregnancy. For these patients, we acquired MR images without gadolinium.
We reviewed the relevant imaging findings from primary radiological reports. In addition, all suspected infections were retrospectively reviewed by a fellowship-trained neuroradiologist (either J.Hi. or J.He.). Discrepancies between primary/secondary readings and retrospective reviews were recorded. To assess the inter-observer agreement on MRI diagnosis of an abscess, a third neuroradiologist (M.N.) independently read a random sample of 50 patients with an infection and rated the images for the presence or absence of an abscess, blind to the primary report and final clinical diagnosis. To assess the diagnostic accuracy of the MRI findings, we used the following clinical reference standards: For infection, we used the final clinical diagnosis from the medical record; for abscesses, we used the presence or absence of purulence or abscess cavity in surgery, if carried out within 48 h of MRI. Surgical information was available for all but one patient. Methods of surgical proof included open surgery, drainage, or puncture of pus. Because patients without abscesses are much less likely to undergo surgery than patients with an abscess (partial verification bias), we considered patients with no abscesses who recovered uneventfully following conservative treatment (including intravenous antibiotics) as representing true negatives, as has been done previously with CT (6).
Generally, we defined imaging evidence of infection as any significant high signal of fat-suppressed T2-weighted Dixon images consistent with edema, as well as a high signal of fat-suppressed post-gadolinium T1-weighted Dixon images consistent with abnormal tissue enhancement. Abscess was defined as an abnormal non-enhancing, T2-hyperintense collection with a low apparent diffusion coefficient (ADC) surrounded by abnormal tissue enhancement. Suppurative lymphadenitis was considered an intranodal abscess, and infected cystic masses were considered abscessed if they included purulent fluid as indicated by low ADC.
Results are expressed as percentages, means and standard deviation (SD). For assessing the diagnostic accuracy of detecting abscesses, we formulated 2 × 2 tables (MRI vs. surgery) for true positives (TP), false positives (FP), true negatives (TN), and false negatives (FN); and calculated sensitivity (TP/[TP+FN]), specificity (TN/[TN+FP]), positive predictive value (PPV; TP/[TP+FP]), negative predictive value (NPV; TN/[TN+FN]), and accuracy ([TP+TN]/[TP+FP+TN+FN]). For diagnosing infection, we only used the PPV, because we did not have enough patients without signs of infection to calculate a 2 × 2 table. We assessed inter-observer agreement using Kappa values and percent agreement. The data were analyzed using IBM SPSS Statistics for Mac (version 26, copyright IBM Corporation 2019). P values < 0.05 were considered statistically significant.
Results
Patient population, feasibility, and comparison with CT
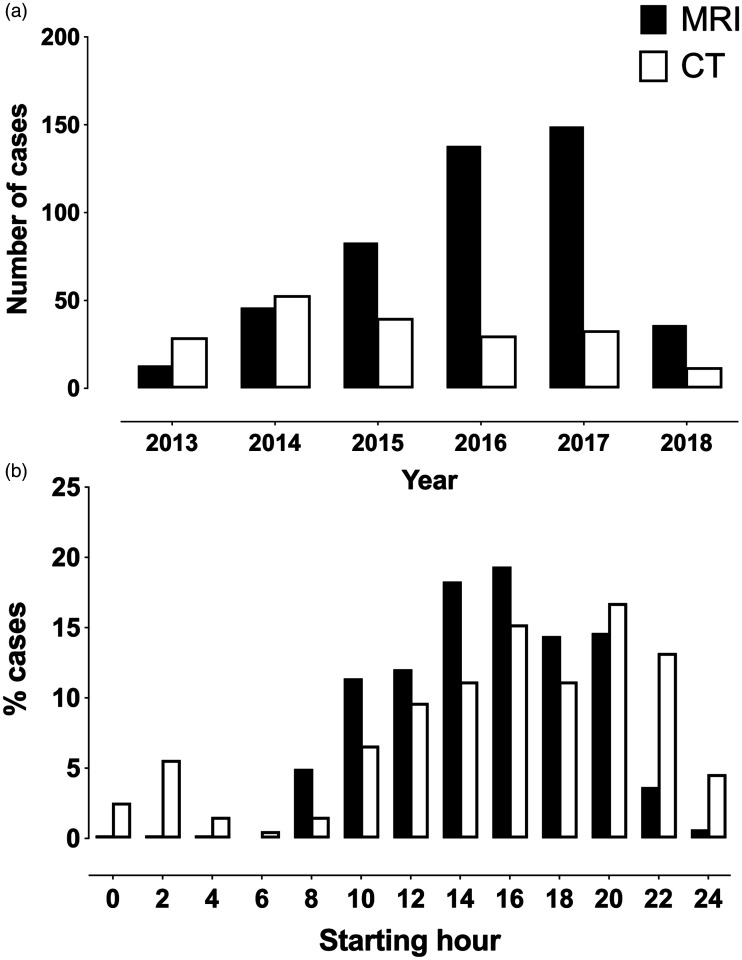
The search identified 461 primary neck MRI scans among a total of 541 neck scans (Fig. 1, Table 1). Of the primary neck MRI scans, 334 (72%) were performed due to suspected infection. Other indications (28%) included postoperative spine imaging, suspected head and neck tumor, neck trauma, and dyspnea. Only five MRI scans (1% of the 461 primary scans) were deemed non-diagnostic due to patient restlessness and resulting image quality deterioration. Two of these patients required follow-up imaging with contrast-enhanced CT on clinical grounds to assess the extent of odontogenic deep neck infection, while no further imaging was considered for the remaining three non-diagnostic MRI patients. Thus, the attempted emergency MRI scans had a technical success rate of 99%. Most primary neck MRI scans were performed between 08:00 and 22:00, and only 11 (2%) scans were performed during the night despite scanner availability (Fig. 2). The total number of primarily requested MRI scans was 485. The number of unsuccessful MRI cases, consisting of both non-diagnostic attempted MRI scans and failures to execute planned MRI scans, was 25. Thus, the overall success rate of emergency neck MRI was 95%. Of the unsuccessful 25 cases, 12 patients were already prepared for the scanner before the process was aborted, and in 13 cases, MRI was canceled before the patient was put in the scanner.
Fig. 1.
Retrospective cohort study flow chart.
Fig. 2.
Comparison of numbers of primary studies of magnetic resonance imaging (black bars) and computed tomography (white bars) as annual totals (a), and in terms of cumulative distributions regarding time of day (b).
We found 196 primary neck CT scans from the same time period (118 suspected infection and 78 other). The pattern of annual CT and MRI scans suggests that MRI had gradually overtaken CT as the preferred imaging method, although emergency neck scanning had clearly increased overall (Fig. 2). Of these CT scans, 22 were performed instead of primarily requested MRI. This change in strategy was mostly due to patient-related contraindications, such as restlessness (n = 4), claustrophobia (n = 3), high fever (n = 3), and dyspnea (n = 2). In four cases, MRI could not be performed due to limited scanner availability. In five cases, we found no specific reason for conversion from MRI to CT.
Imaging outcomes and diagnostic accuracy
Among the patients with suspected infection, 95% of the scans had MRI evidence of infection. The most common main locations for infections were the peritonsillar/parapharyngeal space (43%) and the submandibular/sublingual/oral cavity (20%) (Table 2 and Figs. 3 and 4). As many as 310 of these 317 patients had a final clinical diagnosis of neck infection, suggesting a PPV of 0.98. One or more abscesses were found in 229 (72%) of the patients. A total of 193 (84%) of these patients underwent surgery, and an abscess was surgically confirmed in 183 patients, suggesting a PPV of 0.95. There were 10 FPs, in whom purulence could not be surgically demonstrated (Fig. 5). Twenty-two patients underwent surgery without MRI evidence of abscess (27% of confirmed infections); among these, 20 were TNs and 2 were FNs (Fig. 5). Assuming 59 more TNs (i.e. patients with neck infection but without MRI evidence of abscess, who recovered uneventfully after conservative treatment), we found sensitivity, specificity, and accuracy of 0.99, 0.89, and 0.96, respectively for MRI diagnoses of an abscess (Table 3). Regarding inter-observer agreement on the presence of an abscess, the blind reader agreed with the primary and secondary reads in 45/50 (90%) cases. Kappa was 0.781, indicating substantial agreement.
Table 2.
Main location of neck infection.
| Main location of infection | |
| Peritonsillar, parapharyngeal | 137 (43) |
| Sublingual, submandibular, tongue | 64 (20) |
| Masticator, buccal | 33 (10) |
| Lymph node, cyst, other mass | 27 (9) |
| Retropharyngeal, prevertebral, mediastinal | 22 (7) |
| Superficial | 12 (4) |
| Epiglottis, glottis | 10 (3) |
| Parotid | 10 (3) |
| Ear-related | 3 (1) |
| Paranasal sinuses | 1 (<1) |
Values are given as n (%).
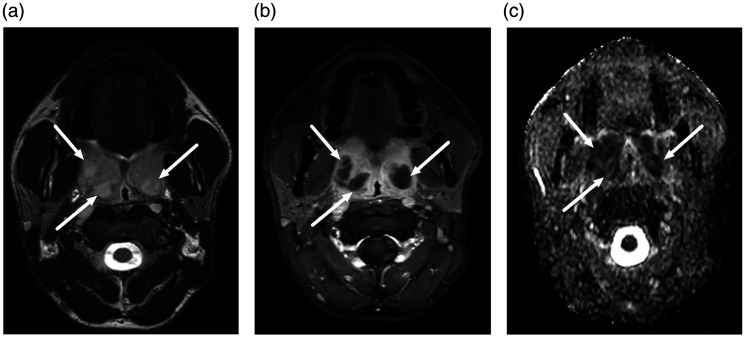
Fig. 3.
Bilateral peritonsillar abscesses. A 25-year-old male presented with a sore throat that did not respond to oral antibiotics. Axial MRI slices (a, T2-weighted Dixon in-phase; b, gadolinium-enhanced T1-weighted Dixon water; c, apparent diffusion coefficient from diffusion-weighted imaging) demonstrated bilateral non-enhancing collections with restricted diffusion surrounded by abnormal tissue enhancement (arrows).
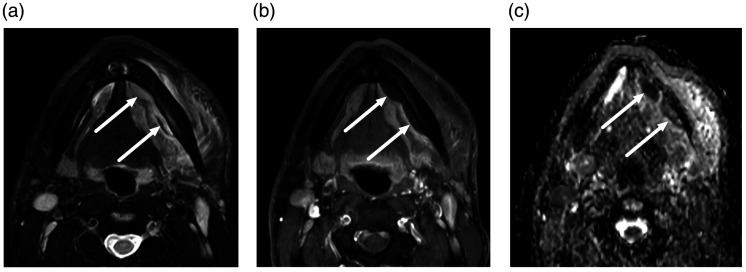
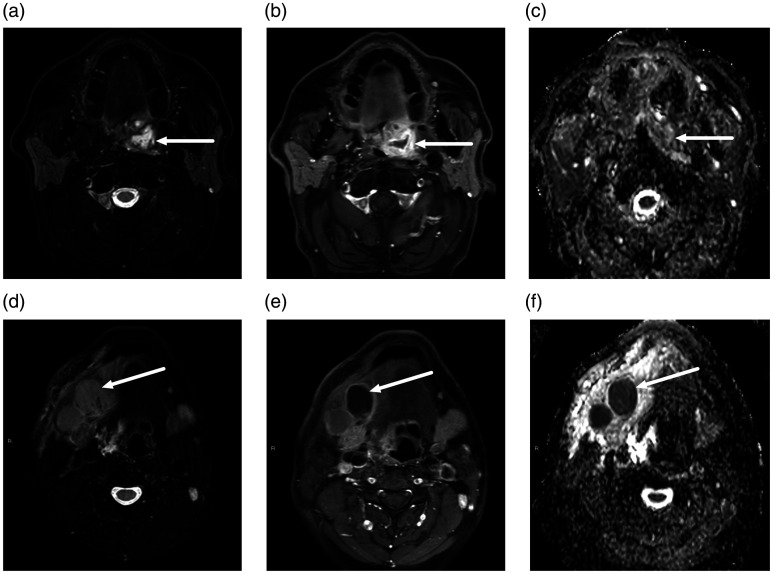
Fig. 4.
Submandibular space subperiosteal abscesses. A 32-year-old man presented with left submandibular space swelling and subsequent dental extraction. Axial MRI slices (a, T2-weighted Dixon water; b, gadolinium-enhanced T1-weighted Dixon water; c, apparent diffusion coefficient from diffusion-weighted imaging) demonstrated non-enhancing collections with restricted diffusion surrounded by abnormal tissue enhancement (arrows) on the medial aspect of the body of the mandible, consistent with subperiosteal abscesses.
Fig. 5.
FN (a–c) and FP (D–F) abscesses on MRI in two different patients. Axial MRI slices (a, d, T2-weighted Dixon water; b, e, gadolinium-enhanced T1-weighted Dixon water; c, f, ADC from DWI). FN abscess, top row (a–c): a 62-year-old man presented with a sore throat. MRI demonstrated an abnormal collection with enhancing rim and non-enhancing center superior to the left palatine tonsil (arrows). ADC values were high rather than low in the non-enhancing part, and therefore, an abscess was not diagnosed. However, subsequent surgery found an abscess. FP abscess, bottom row (d–f): A 43-year-old man with neck swelling. MRI showed lymphadenitis and tissue edema on the right suprahyoid neck, and one enlarged submandibular space lymph node with no enhancement and low ADC values (arrows). Suppurative lymphadenitis (intranodal abscess) was diagnosed based on these MRI findings. However, surgery demonstrated necrotic lymphadenitis, but no purulence. ADC, apparent diffusion coefficient; DWI, diffusion-weighted imaging; FN, false negative; FP, false positive; MRI, magnetic resonance imaging.
Table 3.
Diagnostic accuracy of MRI in detection of abscesses, using surgical findings as reference standard.*
| Surgery |
|||
|---|---|---|---|
| Yes | No | ||
| MRI | Yes | 183 | 10 |
| No | 2 | 79† | |
Values are given as n.
*Sensitivity = 0.99, specificity = 0.89, PPV = 0.95, NPV = 0.98, accuracy = 0.96.
†20 patients surgically confirmed, 59 patients based on clinical assessment.
MRI, magnetic resonance imaging; NPV, negative predictive value; PPV, positive predictive value.
Discussion
In this retrospective analysis, we demonstrate the feasibility of neck MRI in an emergency care setting and a 99% technical success rate. Taking into account both non-diagnostic MRI studies and failures to execute MRI, we found an overall technical success rate of 95%. Only a few MRI scans among these acutely ill patients were non-diagnostic, and only a few patients were primarily excluded from MRI. Furthermore, we found that MRI had very high diagnostic accuracy and predictive value for both infection and abscess. From a clinical perspective, emergency MRI altered patient management, because the patients with MRI evidence of an abscess were over three times more likely to undergo surgery than the patients without abscesses. These results suggest that MRI could be an alternative to CT as the first or only modality in neck emergencies.
The detection of abscesses, the most crucial finding guiding treatment in deep neck infections, was much more accurate with MRI than has previously been reported with CT. For example, the PPV for the detection of an abscess using MRI was 0.95, whereas that reported for CT was about 0.80 (6,7). Common CT criteria for abscesses include low-density core and rim enhancement, but these signs are often unreliable (6,8). Thus, differentiating phlegmon and abscess using CT may be difficult, especially in early abscess formation. MRI has several advantages over CT for diagnosing abscesses, such as superior soft-tissue discrimination and detection of purulent fluid with DWI. The FPs that we noted were mostly very small abscesses, or poorly enhancing infected lymph nodes misdiagnosed as abscesses. However, the reference standard of surgical outcome may also not always be correct, because small or deep abscesses may be missed in surgery.
Only a few previously published studies have directly compared CT and MRI of the neck in an emergency setting. One such study prospectively assessed 47 patients with clinical suspicion of acute neck infection and found that MRI revealed more infected neck spaces and delineated more abscesses than CT, while CT more readily indicated the presence of gas and calcifications in soft tissue (9). Another study reported 10 patients with deep neck infections scanned using both CT and MRI but did not report on direct comparisons between the two modalities (10). More recently, MRI was found to be more accurate than CT in the prospective evaluation of maxillofacial space infections among 15 patients (11). We did not compare MRI and CT of the same patients.
Most of the infections in the current study were seen in the peritonsillar/parapharyngeal space (43%) and the sublingual/submandibular/oral cavity (20%) (Table 2 and Figs. 3 and 4). These consisted mainly of throat and odontogenic infections, respectively. We found a smaller proportion of odontogenic infections than previous studies of deep neck infections (30%–50%) (12–15). A likely explanation is that in addition to true deep neck infections, we found many throat infections that did extend to deep neck spaces (e.g. peritonsillar infections, not routinely considered to require imaging). Further analyses of the current data will allow a more thorough analysis of the predictive value of various MRI characteristics in both major types of neck infections.
Table 1.
Characteristics of patients who underwent primary MRI scanning.
| Characteristics | |
| Age overall (years) | 46 ± 21 |
| Female | 47 ± 21 |
| Male | 45 ± 21 |
| Subgroups | |
| Pediatric/adolescent (age 0–21 years) | 65 (14) |
| Elderly adults (age > 65 years) | 97 (21) |
Values are given as n (%) or mean ± SD.
MRI, magnetic resonance imaging.
Some limitations and precautions need to be addressed. First, MRI may not be suitable for every patient with a neck emergency, such as those at a high risk of airway compromise, for whom CT, with its shorter examination time, may be preferred. Our analysis did not exclude potential patients for whom emergency MRI was deemed contraindicated in the first place due to, for example, severe dyspnea or restlessness, and who were thus managed without MRI scanning. Although we found only a few such patients, we are unsure about the true proportion of these patients, since incompatibility with MRI may not always have been explicitly mentioned in the CT referrals. Second, we did not include inpatients on whom MRI may have been performed in another MRI unit in the same hospital. However, these patients would unlikely represent true emergency imaging cases. Third, we only retrieved cases on whom a neck MRI protocol was performed. Therefore, we may have missed cases labeled under head and neck emergencies, on whom head MRI protocol had been performed instead, although this would likely only apply to a local spread of disease in sinonasal and ear infections, and not suspected deep neck infections. We also intentionally excluded cervical spine infections, as they are typically scanned according to spine MRI protocol. Fourth, MRI may be more complex and time-consuming to read than CT, which may limit the generalizability of the current results to other emergency radiology departments. We are also unsure whether abscesses can reliably be excluded without gadolinium-based contrast agents, because we administered contrast in almost all cases. Fifth, whether MRI can reliably indicate the tooth/teeth responsible for odontogenic infections is currently unknown and should be properly established in future studies. Sixth, the estimation of diagnostic accuracy was limited by partial verification bias, which resulted from the fact that patients with an abscess are much more likely to undergo surgery (reference standard) than patients without abscesses. Because the proportions of TNs and FNs are uncertain, sensitivity was overestimated and specificity underestimated (16). This limitation also applies to previous studies using CT (6,7). Yet, we can assume that patients who recover uneventfully following conservative treatment represent true negatives, at least from a practical perspective. In addition, PPV is unaffected by partial verification bias and can thus modalities can be compared. Finally, MRI scans cost more than CT scans, and we did not perform cost-effectiveness analyses. However, by way of improved PPV, MRI may prevent unnecessary surgery.
In conclusion, our retrospective analysis of 461 emergency neck MRI scans revealed: (i) good feasibility indicated by a high technical success rate (99%); (ii) that MRI confirms suspected neck infection in the majority of patients (>95%); and (iii) that MRI has very high diagnostic accuracy and predictive value for both infections and abscesses. These findings suggest that MRI may be a feasible alternative to CT in emergency neck imaging, especially during daytime hours and among younger patients.
Supplemental Material
Supplemental material, sj-pdf-1-acr-10.1177_0284185120940242 for Emergency neck MRI: feasibility and diagnostic accuracy in cases of neck infection by Janne Nurminen, Jarno Velhonoja, Jaakko Heikkinen, Tatu Happonen, Mikko Nyman, Heikki Irjala, Tero Soukka, Kimmo Mattila and Jussi Hirvonen in Acta Radiologica
Acknowledgements
The authors thank the staff of the Radiology Department of Turku University Hospital for their assistance in emergency neck imaging, and for retrieving image data from electronic archives.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received the following financial support for the research, authorship, and/or publication of this article: This work was supported by the Sigrid Jusélius Foundation, Turku University Foundation, and Turku University Hospital (grant nos. K3904 and K4804).
Supplemental material : Supplemental material for this article is available online.
ORCID iDs
Heikki Irjala https://orcid.org/0000-0003-3054-4677
Jussi Hirvonen https://orcid.org/0000-0002-0368-3746
References
- 1.Miller WD, Furst IM, Sàndor GKB, et al. A Prospective, Blinded Comparison of Clinical Examination and Computed Tomography in Deep Neck Infections. Laryngoscope 1999; 109:1873–1879. [DOI] [PubMed] [Google Scholar]
- 2.Kamalian S, Avery L, Lev MH, et al. Nontraumatic Head and Neck Emergencies. RadioGraphics 2019; 39:1808–1823. [DOI] [PubMed] [Google Scholar]
- 3.Pinto A, Scaglione M, Scuderi MG, et al. Infections of the neck leading to descending necrotizing mediastinitis: Role of multi-detector row computed tomography. Eur J Radiol 2008; 65:389–394. [DOI] [PubMed] [Google Scholar]
- 4.Maroldi R, Farina D, Ravanelli M, et al. Emergency Imaging Assessment of Deep Neck Space Infections. Semin Ultrasound CT MRI 2012; 33:432–442. [DOI] [PubMed] [Google Scholar]
- 5.Hurley MC, Heran MKS. Imaging studies for head and neck infections. Infect Dis Clin North Am 2007; 21:305–353. [DOI] [PubMed] [Google Scholar]
- 6.Freling N, Roele E, Schaefer-Prokop C, et al. Prediction of deep neck abscesses by contrast-enhanced computerized tomography in 76 clinically suspect consecutive patients. Laryngoscope 2009; 119:1745–1752. [DOI] [PubMed] [Google Scholar]
- 7.Elden LM, Grundfast KM, Vezina G. Accuracy and usefulness of radiographic assessment of cervical neck infections in children. J Otolaryngol 2001; 30:82–89. [DOI] [PubMed] [Google Scholar]
- 8.Vural C, Gungor A, Comerci S. Accuracy of computerized tomography in deep neck infections in the pediatric population. Am J Otolaryngol 2003; 24:143–148. [DOI] [PubMed] [Google Scholar]
- 9.Muñoz A, Castillo M, Melchor MA, et al. Acute Neck Infections: Prospective Comparison Between CT and MRI in 47 Patients. J Comput Assist Tomogr 2001; 25:733–741. [DOI] [PubMed] [Google Scholar]
- 10.Wang B, Gao B-L, Xu G-P, et al. Images of deep neck space infection and the clinical significance. Acta Radiol 2014; 55:945–951. [DOI] [PubMed] [Google Scholar]
- 11.Babu VR, Ikkurthi S, Perisetty DK, et al. A Prospective Comparison of Computed Tomography and Magnetic Resonance Imaging as a Diagnostic tool for Maxillofacial Space Infections. J Int Soc Prev Community Dent 2018; 8:343–348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Marioni G, Staffieri A, Parisi S, et al. Rational diagnostic and therapeutic management of deep neck infections: analysis of 233 consecutive cases. Ann Otol Rhinol Laryngol 2010; 119:181–187. [DOI] [PubMed] [Google Scholar]
- 13.Bakir S, Tanriverdi MH, Gün R, et al. Deep neck space infections: a retrospective review of 173 cases. Am J Otolaryngol 2012; 33:56–63. [DOI] [PubMed] [Google Scholar]
- 14.Eftekharian A, Roozbahany NA, Vaezeafshar R, et al. Deep neck infections: a retrospective review of 112 cases. Eur Arch Otorhinolaryngol 2009; 266:273–277. [DOI] [PubMed] [Google Scholar]
- 15.Velhonoja J, Lääveri M, Soukka T, et al. Deep neck space infections: an upward trend and changing characteristics. Eur Arch Otorhinolaryngol 2020;277:863–872. [DOI] [PMC free article] [PubMed]
- 16.Whiting P, Rutjes AWS, Reitsma JB, et al. Sources of Variation and Bias in Studies of Diagnostic Accuracy: A Systematic Review. Ann Intern Med 2004; 140:189. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-acr-10.1177_0284185120940242 for Emergency neck MRI: feasibility and diagnostic accuracy in cases of neck infection by Janne Nurminen, Jarno Velhonoja, Jaakko Heikkinen, Tatu Happonen, Mikko Nyman, Heikki Irjala, Tero Soukka, Kimmo Mattila and Jussi Hirvonen in Acta Radiologica