Abstract
Epidemiologic investigation has successively defined associations of air pollution exposure with non-malignant and malignant lung disease, cardiovascular disease, cerebrovascular disease, pregnancy outcomes, perinatal effects, and other extra-pulmonary disease including diabetes. Defining these relationships between air pollution exposure and human health closely parallels results of earlier epidemiologic investigation into cigarette smoking and environmental tobacco smoke (ETS), two other particle-related exposures. Humic-like substances (HULIS) have been identified as a chemical component common to cigarette smoke and air pollution particles. Toxicology studies provide evidence that a disruption of iron homeostasis with sequestration of host metal by HULIS is a fundamental mechanistic pathway through which biological effects are initiated by cigarette smoke and air pollution particles. As a result of a common chemical component and a shared mechanistic pathway, it should be possible to extrapolate from the epidemiology of cigarette smoking and ETS to predict associations of air pollution exposure with human disease which are currently unrecognized. Accordingly, it is anticipated that forthcoming epidemiologic investigation will demonstrate relationships of air pollution with COPD causation, peripheral vascular disease, hypertension, renal disease, digestive disease, loss of bone mass/risk of fractures, dental disease, eye disease, fertility problems, and extrapulmonary malignancies.
Keywords: Air pollution, particulate matter, ozone, smoking, tobacco smoke pollution
Introduction
The field of epidemiology identified the relationship between human exposure to air pollution and morbidity and mortality [1,2]. Since that exceptional achievement, epidemiologic investigation has successively defined associations of air pollution exposure with non-malignant lung disease, malignant lung disease, cardiovascular disease, cerebrovascular disease, pregnancy outcomes, perinatal effects, and other extra-pulmonary disease including diabetes.
The development of these breakthroughs into defining the relationships between air pollution exposure and human health closely parallels results of earlier epidemiologic investigation into cigarette smoking and environmental tobacco smoke (ETS), two other particle-related exposures. Humic-like substances (HULIS) have been identified as a chemical component common to cigarette smoke and air pollution particles. Toxicology studies provide evidence that a disruption of iron homeostasis with sequestration of host metal by HULIS is a fundamental mechanistic pathway through which biological effects are initiated by cigarette smoke and air pollution particles. As a result of a common chemical component and a shared mechanistic pathway, it should be possible to extrapolate from the epidemiology of cigarette smoking and ETS to predict associations of air pollution exposure with human disease which are currently unrecognized.
Particle exposures and humic-like substances
Humic substances (HS) are heterogeneous, amorphous organic materials found in all terrestrial and aqueous environments [3]. They include three different fractions: humic acid, fulvic acid, and humin. The humic acid fraction is not soluble in water under acidic conditions (pH<2) but is soluble at higher pH values. Humic acid is the major extractable component of soil HS. Fulvic acid is the fraction of HS which is soluble in water under all pH conditions and remains in solution after removal of humic acid by acidification. Humin is the fraction of HS that is not soluble in water at any pH value.
A substantial mass fraction of tropospheric aerosols (up to 90%) is comprised of natural organic matter which chemically resembles HS with a mixture of aromatic, phenolic, and acidic functional groups [4-6]. This material shares chemical characteristics with HS but differs in having a smaller molecular weight and lower aromaticity; it is designated HULIS [6]. In one study, about 3% of ambient air particulate matter (PM) was estimated to be HULIS [7]. Combustion products such as wood smoke and diesel exhaust particles (i.e. emission air pollution sources) similarly include HULIS at approximately 8% of wood smoke and 5% in diesel exhaust particles [7-9]. HULIS has also been isolated from cigarette smoke particle [8,9]. About 7-10% of tobacco smoke condensate can be characterized as HULIS [8,9].
As a result of having a variety of oxygen-containing functional groups (e.g. carboxylic and phenolic groups), both HS and HULIS complex metal cations [10-13]. The high content of oxygen-containing functional groups in HS and HULIS favors the formation of stable complexes with numerous metals but that with iron is the most favored [14]. The quantity of HULIS isolated from air pollution particles can be correlated with the metal concentration of ambient air PM [10]. Comparable to HS and HULIS, cigarette smoke condensate functions to bind transition metals [15]. The introduction of HULIS, isolated from cigarette smoke condensate, into the lungs of an animal model is followed by its phagocytosis and an intracellular accumulation of iron [9]. Likewise, a material with solubility properties and composition similar to HS can be isolated from smokers’ lungs and the retention of this material is associated with iron accumulation [9]. The sequestration of iron and an associated deficiency of cell metal after exposure to HULIS included in air pollution particles and cigarette smoke can initiate pathways leading to biological effect, injury, and disease [16-23]. The effects of cigarette smoke and air pollution particles on human health can result from an inclusion of HULIS in both.
Interaction of air pollution particles and ozone
Comparable to air pollution particles, exposure to ambient ozone has been associated with increased human mortality (including non-accidental and cardiovascular mortality) [24-27]. This relationship between ozone exposure and human mortality may be non-linear, a threshold is not recognized, and its basis remains unknown.
After reacting with ozone, carbonaceous compounds demonstrate increased surface functionalization (Figure 1A) [28-32]. As indicated by both high-resolution X-ray photoelectron spectroscopy and Fourier transform-infrared spectroscopy, the surface oxygen introduced on these compounds after reaction with ozone is most frequently present in carboxylic acid groups but phenol, lactone, and quinone formation are also observed [33,34]. Soot, a mixture of elemental carbon and organic compounds, is oxidized in the atmosphere leading to the formation of carboxylates [35]. This reaction increases the polarity of soot surfaces and water-solubility of the particles [36-38]. This reaction between ozone and carbon-containing particles appears to generate either HULIS itself or a product which chemically is similar to HULIS; the material includes numerous oxygen-containing functional groups (e.g. carboxylates) and can be water-soluble. Therefore, it can be expected that some portion of the health effects of ozone, including associated mortality, are mediated through its impact on the content of either HULIS itself or a product which chemically is similar to HULIS in air pollution particles. It is possible that other components of air pollution (e.g. nitrogen oxides) also participate in modifying the functional groups at the ambient PM surface and subsequently impact human health through the same pathway [39].
Figures 1A and 1B.
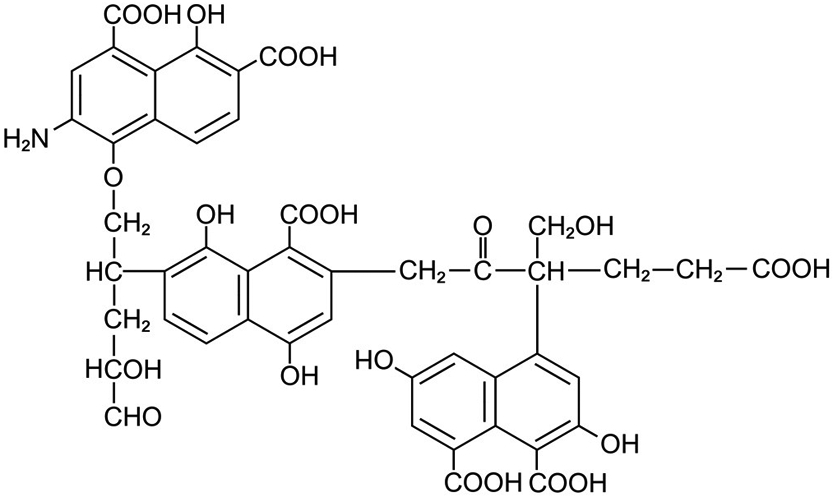
Numerous different sources contribute to the release of carbonaceous particles into the atmosphere (designated by black and brown particles) (Figure 1A). Some of the carbonaceous particles can include HULIS, a polycarboxylic, polyaromatic material (designated by brown particles). Exposure of the ambient air PM to ozone results in additional functionalization of the particle surface with introduction of more phenol, lactone, and quinone groups but especially further carboxylation. The formation of these products increases solubility of components of the PM with systemic distribution following (Figure 1B). Respiratory disease, cardiovascular disease, non-malignant extrapulmonary disease, fertility problems, changes in pregnancy outcomes, effects on the newborn, and extrapulmonary diseases result from the impact of exposure of the tissues to this component of ambient air pollution particle.
Mechanism of biological effect after particle exposure
In the respiratory tract, PM has consistently demonstrated a capacity to accumulate iron from available cell sources reflecting the particle surface’s ability to complex host iron [40,41]. Following exposure to PM containing carbonaceous compounds, this response will also be observed in the lungs [9,42]. Endogenous iron, essential for host function, is complexed by the polyanionic particle surface including both carboxylic and phenolic functional groups [43]. Comparable to other compounds with a capacity to appropriate cell iron, the response to the functional metal deficiency associated with particle exposure will include oxidative stress, activation of cell signaling and transcription factors, and release of pro-inflammatory mediators prior to apoptosis [44-52]. This eventually culminates in the development of tissue inflammation and fibrosis [43,53]. Exposure to other xenobiotic agents with an equivalent capacity to coordinate metal cations impacts comparable inflammatory and fibrotic injuries in humans [54-56].
Interaction between air pollution particles and ozone is suggested to impact human health effects (Figure 1A). Air pollution particles can include a significant concentration of HULIS (i.e. polycarboxylates), and investigation predicts further carboxylation of this PM following ozone exposure. This results in a particle with a greater capacity to impact 1) iron sequestration resulting in an increased disruption in metal homeostasis and 2) subsequent inflammation and fibrosis. Such interaction between particles and ozone is supported by epidemiological, controlled exposure, animal, and in vitro investigation [57-64].
HULIS in the atmosphere has a significant overlap with water-soluble organic compounds (WSOC) [6]. This soluble component of ambient air PM contains compounds more similar to fulvic acid than humic acid and includes many lower molecular weight organic and inorganic species. As a result of their solubility, these compounds can permeate the blood vessels to be distributed systemically (Figure 1B). The capacity to initiate iron sequestration will impact oxidative stress, cell signaling, transcription factor activation, release of pro-inflammatory mediators, apoptosis, inflammation, and fibrosis in exposed cells and tissues predicting a capacity of cigarette smoking, ETS, and air pollution in initiating extra-pulmonary disease.
Predicting the epidemiology of air pollution particles
Particles in cigarette smoke, ETS, and air pollution have a common chemical component (i.e. HULIS) and a shared mechanistic pathway (i.e. disruption of iron homeostasis). The common chemical component and shared mechanistic pathway predict comparable consequences of exposure including biological effects, tissue injuries, and disease. Accordingly, investigation of one of these particles is applicable to the others; morbidity and mortality after cigarette smoking and ETS exposure is expected to be relevant to the impact of air pollution particle exposure on human health.
Epidemiological studies have more thoroughly described the relationships between cigarette smoking and ETS with respiratory morbidity and mortality, relative to air pollution [65-85] (Table 1). Cigarette smoking and ETS are frequently associated with respiratory symptoms (e.g. cough and phlegm) and individuals exposed to ambient air pollution levels can present with these same complaints. Cigarette smoking and exposures to ETS and ambient air pollution particles are all associated with loss of lung function. Cigarette smoking, ETS and air pollution have recurrently been demonstrated to cause asthma and precipitate its exacerbations. While smoking causes chronic obstructive pulmonary disease (COPD) and exacerbates its course, ETS and air pollution can precipitate aggravations; ETS and air pollution have not yet been strongly associated with COPD causation. Smoking, ETS, and air pollution all elevate the risk for both infections and lung cancers.
Table 1.
Respiratory morbidity and mortality associated with cigarette smoking, ETS, and air pollution particles
| Smoking | ETS | Air pollution | |
|---|---|---|---|
| Respiratory symptoms | Yes [77] | Yes [65,77] | Yes [70] |
| Lung function decline | Yes [77] | Yes [65,77] | Yes [70] |
| Asthma – causation | Yes [77] | Yes [65,77] | Yes [70] |
| Asthma - exacerbation | Yes [77] | Yes [65,77] | Yes [70] |
| COPD – causation | Yes [77] | No | No |
| COPD - exacerbation | Yes [77] | Yes [65,77] | Yes [70] |
| Infections | Yes [77] | Yes [65,77] | Yes [70] |
| Lung cancer | Yes [77] | Yes [65,77] | Yes [70] |
Systemic distribution of the water-soluble HULIS component in cigarette smoke will disrupt iron homeostasis at extrapulmonary sites and initiate pathways of inflammation and fibrosis. Accordingly, cigarette smoking influences cardiovascular disease (Table 2), non-malignant extrapulmonary disease (Table 3), fertility problems, pregnancy outcomes, effects on the newborn (Table 4), and malignant diseases outside the respiratory tract (Table 5). ETS similarly will impact cardiovascular disease, non-malignant extrapulmonary disease, pregnancy outcomes, and effects on the newborn (e.g. low birth weight). Differences between cigarette smoking and ETS in associations with these diseases likely reflect the lower dose of particle exposure following the latter (15 to 40 mg per cigarette smoked vs. hundreds to approximately 1000 μg/m3 respectively).
Table 2.
Cardiovascular disease associated with cigarette smoking, ETS, and air pollution particles
| Smoking | ETS | Air pollution | |
|---|---|---|---|
| Atherosclerosis | Yes [77] | Yes [65,77] | Yes [70,95,96] |
| Ischemic/coronary heart disease | Yes [77] | Yes [65,77] | Yes [70,97,98] |
| Cerebrovascular disease | Yes [77] | Yes [99,100] | Yes [101,102] |
| Peripheral vascular disease | Yes [77] | No | No |
| Hypertension | Yes [77] | No | No |
| Other heart disease | Yes [77] | Yes [65,77] | Yes [103,104] |
Table 3.
Non-malignant extrapulmonary disease associated with cigarette smoking, ETS, and air pollution particles
| Smoking | ETS | Air pollution | |
|---|---|---|---|
| Infections | Yes [77] | Yes [65,77] | Yes [105] |
| Diabetes | Yes [77] | Yes [65,77] | Yes [106,107] |
| Renal disease | Yes [77] | No | No |
| Ischemic diseases of the intestines | Yes [77] | No | No |
| Liver cirrhosis | Yes [77] | No | No |
| Other digestive disease | Yes [77] | No | No |
| Loss of bone mass/risk of fractures | Yes [77] | No | No |
| Dental disease | Yes [77] | No | No |
| Eye disease | Yes [77] | No | No |
| Immunologically mediated disease | Yes [77] | No | No |
Table 4.
Fertility problems, changes in pregnancy outcomes, and effects on the newborn associated with cigarette smoking, ETS, and air pollution particles
Table 5.
Extrapulmonary malignant diseases associated with cigarette smoking, ETS, and air pollution particles
| Smoking | ETS | Air pollution | |
|---|---|---|---|
| Laryngeal/lip/pharyngeal cancer | Yes [77] | No | No |
| Esophageal cancer | Yes [77] | No | No |
| Stomach cancer | Yes [77] | No | No |
| Colon cancer | Yes [77] | No | No |
| Liver cancer | Yes [77] | No | No |
| Pancreatic cancer | Yes [77] | No | No |
| Kidney and bladder cancer | Yes [77] | No | No |
| Leukemia/lymphoma | Yes [77] | No | No |
| Breast cancer | Yes [77] | No | No |
| Cervical cancer | Yes [77] | No | No |
| Endometrial cancer | Yes [77] | No | No |
| Rare cancers | Yes [77] | No | No |
| Cancers of unknown site | Yes [77] | No | No |
Comparable to cigarette smoking and ETS, air pollution particles include HULIS, some of which is water-soluble, with a capacity to disrupt metal homeostasis and initiate inflammatory and fibrotic pathways. While the actual mass of particle air pollution a human is exposed to does not approach that of cigarette smoking (~1/100th or less) presumably resulting in less PM dose, the former may demonstrate a greater potential for impacting biological effect following interaction with ozone. Accordingly, investigations with air pollution exposure have demonstrated increases in cardiovascular disease (Table 2), non-malignant extrapulmonary disease (Table 3), pregnancy outcomes, and effects on the newborn (Table 4) comparable to cigarette smoking and ETS exposure. The range of diseases which develops after air pollution closely approximates that observed after ETS exposure. The two cardiovascular diseases which epidemiological investigation has not yet associated with air pollution exposure are peripheral vascular disease and hypertension. The same is true with studies into relationships of air pollution exposure with non-malignant extrapulmonary disease, pregnancy outcomes, and effects on the newborn which parallel results after ETS exposure. Neither ETS nor air pollution exposures have convincingly been demonstrated to increase extrapulmonary malignancies.
As a result of a common chemical component and a shared mechanistic pathway, it should be possible to extrapolate from the epidemiology of cigarette smoking and ETS to predict associations of air pollution particle with human morbidity and mortality. While the total mass of air pollution particle a human will be exposed to will be lower than that of a cigarette smoker, the interactions with other oxidant components (e.g. ozone) will increase the impact. Accordingly, the range of human disease following air pollution potentially is predicted to approach that of a cigarette smoker. It is anticipated that forthcoming epidemiologic investigation will demonstrate a relationship of exposure to air pollution with:
COPD causation
Peripheral vascular disease
Hypertension
Renal disease
Digestive disease
Loss of bone mass/risk of fractures
Dental disease
Eye disease
Fertility problems
Extrapulmonary malignancies including breast cancer and leukemias
Epidemiologic research has already suggested associations of air pollution with several of these endpoints including COPD causation, peripheral vascular disease, hypertension, renal disease, digestive diseases, loss of bone, eye disease, breast cancer, and leukemias [86-94].
Conclusions
Cigarette smoke, ETS, and air pollution have a common chemical component and a shared mechanistic pathway. A common chemical component and share mechanistic pathway allow an extrapolation of the results of the epidemiology of cigarette smoking to predict associations of air pollution exposure with human disease.
Footnotes
Disclaimer: This report has been reviewed by the National Health and Environmental Effects Research Laboratory, United States Environmental Protection Agency, and approved for publication. Approval does not signify that the contents necessarily reflect the views and policies of the Agency, nor does mention of trade names or commercial products constitute endorsement or recommendations for use.
References
- 1.Schwartz J, Marcus A (1990) Mortality and air pollution in London: a time series analysis. Am J Epidemiol 131 (1):185–194 [DOI] [PubMed] [Google Scholar]
- 2.Dockery DW, Pope CA 3rd, Xu X, Spengler JD, Ware JH, Fay ME, Ferris BG Jr., Speizer FE (1993) An association between air pollution and mortality in six U.S. cities. N Engl J Med 329 (24):1753–1759. doi: 10.1056/NEJM199312093292401 [DOI] [PubMed] [Google Scholar]
- 3.Stevenson FJ (1985) Geochemistry of soil humic substances. In: Humic Substances in Soil, Sediment, and Water, edited by Aiken GR, McKnight DM, Wershaw RL, and MacCarthy P. New York: Wiley-Interscience: p. 13–52. [Google Scholar]
- 4.Jacobson MC H H, Noone KJ, Charlson RJ (2000) Organic atmospheric aerosols: review and state of the science. Reviews of Geophysics 38:267–294 [Google Scholar]
- 5.Dinar E M T, Rudich Y (2006) The density of humic acids and humic like substances (HULIS) from fresh and aged wood burning and pollution aerosol particles. Atmos Chem Phys 6:5213–5224 [Google Scholar]
- 6.Graber ER, Rudich Y (2006) Atmospheric HULIS: How humic-like are they? A comprehensive and critical review. Atmos Chem Phys 6:729–753 [Google Scholar]
- 7.Ghio AJ, Stonehuerner J, Pritchard RJ, Piantadosi CA, Quigley DR, Dreher KL, Costa DL (1996) Humic-like substances in air pollution particulates correlate with concentrations of transition metals and oxidant generation. Inhalation Toxicology 8:479–494 [Google Scholar]
- 8.Stedman RL, Chamberlain WJ, Miller RL (1966) High molecular weight pigment in cigarette smoke. Chemistry & Industry 37:1560–1562 [PubMed] [Google Scholar]
- 9.Ghio AJ, Stonehuerner J, Quigley DR (1994) Humic-like substances in cigarette condensate and lung tissue of smokers. Am J Physiol 266:L382–L388 [DOI] [PubMed] [Google Scholar]
- 10.Ghio A, Stonehuerner J, Pritchard RJ, Piantadosi CA, Quigley DR, Dreher KL, and Costa DL (1996) Humic-like substances in air pollution particulates correlate with concentrations of transition metals and oxidant generation. Inhalation Toxicology 8:479–494 [Google Scholar]
- 11.Yang R, Van den Berg CM (2009) Metal complexation by humic substances in seawater. Environ Sci Technol 43 (19):7192–7197 [DOI] [PubMed] [Google Scholar]
- 12.Yamamoto M, Nishida A, Otsuka K, Komai T, Fukushima M (2010) Evaluation of the binding of iron(II) to humic substances derived from a compost sample by a colorimetric method using ferrozine. Bioresour Technol 101 (12):4456–4460. doi: 10.1016/j.biortech.2010.01.050 [DOI] [PubMed] [Google Scholar]
- 13.Town RM, Duval JF, Buffle J, van Leeuwen HP (2012) Chemodynamics of metal complexation by natural soft colloids: Cu(II) binding by humic acid. Journal of Physical Chemistry A 116 (25):6489–6496. doi: 10.1021/jp212226j [DOI] [PubMed] [Google Scholar]
- 14.Erdogan S, Baysal A, Akba O, Hamamci C (2007) Interaction of metals with humic acid isolated from oxidized coal. Polish J Environ Stud 16:671–675 [Google Scholar]
- 15.Qian MW, Eaton JW (1989) Tobacco-borne siderophoric activity. Arch Biochem Biophys 275 (1):280–288 [DOI] [PubMed] [Google Scholar]
- 16.Gau RJ, Yang HL, Suen JL, Lu FJ (2001) Induction of oxidative stress by humic acid through increasing intracellular iron: a possible mechanism leading to atherothrombotic vascular disorder in blackfoot disease. Biochem Biophys Res Commun 283 (4):743–749. doi: 10.1006/bbrc.2001.4832 [DOI] [PubMed] [Google Scholar]
- 17.Hseu YC, Huang HW, Wang SY, Chen HY, Lu FJ, Gau RJ, Yang HL (2002) Humic acid induces apoptosis in human endothelial cells. Toxicol Appl Pharmacol 182 (1):34–43 [DOI] [PubMed] [Google Scholar]
- 18.Cheng ML, Ho HY, Huang YW, Lu FJ, Chiu DT (2003) Humic acid induces oxidative DNA damage, growth retardation, and apoptosis in human primary fibroblasts. Exp Biol Med (Maywood) 228 (4):413–423 [DOI] [PubMed] [Google Scholar]
- 19.Yang HL, Hseu YC, Hseu YT, Lu FJ, Lin E, Lai JS (2004) Humic acid induces apoptosis in human premyelocytic leukemia HL-60 cells. Life Sci 75 (15):1817–1831. doi: 10.1016/j.lfs.2004.02.033 [DOI] [PubMed] [Google Scholar]
- 20.Hseu YC, Lin E, Chen JY, Liua YR, Huang CY, Lu FJ, Liao JW, Chen SC, Yang HL (2009) Humic acid induces G1 phase arrest and apoptosis in cultured vascular smooth muscle cells. Environ Toxicol 24 (3):243–258. doi: 10.1002/tox.20426 [DOI] [PubMed] [Google Scholar]
- 21.van Eijl S, Mortaz E, Ferreira AF, Kuper F, Nijkamp FP, Folkerts G, Bloksma N (2011) Humic acid enhances cigarette smoke-induced lung emphysema in mice and IL-8 release of human monocytes. Pulm Pharmacol Ther 24 (6):682–689. doi: 10.1016/j.pupt.2011.07.001 [DOI] [PubMed] [Google Scholar]
- 22.Hseu YC, Senthil Kumar KJ, Chen CS, Cho HJ, Lin SW, Shen PC, Lin CW, Lu FJ, Yang HL (2014) Humic acid in drinking well water induces inflammation through reactive oxygen species generation and activation of nuclear factor-kappaB/activator protein-1 signaling pathways: a possible role in atherosclerosis. Toxicol Appl Pharmacol 274 (2):249–262. doi: 10.1016/j.taap.2013.11.002 [DOI] [PubMed] [Google Scholar]
- 23.Ghio AJ, Soukup JM, Dailey LA, Tong H, Kesic MJ, Budinger GR, Mutlu GM (2015) Wood Smoke Particle Sequesters Cell Iron to Impact a Biological Effect. Chem Res Toxicol 28 (11):2104–2111. doi: 10.1021/acs.chemrestox.5b00270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bae S, Lim YH, Kashima S, Yorifuji T, Honda Y, Kim H, Hong YC (2015) Non-Linear Concentration-Response Relationships between Ambient Ozone and Daily Mortality. PLoS One 10 (6):e0129423. doi: 10.1371/journal.pone.0129423 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Crouse DL, Peters PA, Hystad P, Brook JR, van Donkelaar A, Martin RV, Villeneuve PJ, Jerrett M, Goldberg MS, Pope CA 3rd, Brauer M, Brook RD, Robichaud A, Menard R, Burnett RT (2015) Ambient PM2.5, O(3), and NO(2) Exposures and Associations with Mortality over 16 Years of Follow-Up in the Canadian Census Health and Environment Cohort (CanCHEC). Environ Health Perspect 123 (11):1180–1186. doi: 10.1289/ehp.1409276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Di Q, Wang Y, Zanobetti A, Wang Y, Koutrakis P, Choirat C, Dominici F, Schwartz JD (2017) Air Pollution and Mortality in the Medicare Population. N Engl J Med 376 (26):2513–2522. doi: 10.1056/NEJMoa1702747 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yin P, Chen R, Wang L, Meng X, Liu C, Niu Y, Lin Z, Liu Y, Liu J, Qi J, You J, Zhou M, Kan H (2017) Ambient Ozone Pollution and Daily Mortality: A Nationwide Study in 272 Chinese Cities. Environ Health Perspect 125 (11):117006. doi: 10.1289/EHP1849 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cataldo F (2007) Ozone reaction with carbon nanostructures 1: Reaction between solid C-60 and C-70 fullerenes and ozone. J Nanosci Nanotechno 7 (4-5):1439–1445. doi: 10.1166/jnn.2007.326 [DOI] [PubMed] [Google Scholar]
- 29.Cataldo F (2007) Ozone reaction with carbon nanostructures 2: The reaction of ozone with milled graphite and different carbon black grades. J Nanosci Nanotechno 7 (4-5):1446–1454. doi: 10.1166/jnn.2007.327 [DOI] [PubMed] [Google Scholar]
- 30.Chapleski RC, Morris JR, Troya D (2014) A theoretical study of the ozonolysis of C60: primary ozonide formation, dissociation, and multiple ozone additions. Phys Chem Chem Phys 16 (13):5977–5986. doi: 10.1039/c3cp55212h [DOI] [PubMed] [Google Scholar]
- 31.Tiwari AJ, Morris JR, Vejerano EP, Hochella MF, Marr LC (2014) Oxidation of C-60 Aerosols by Atmospherically Relevant Levels of O-3. Environmental Science & Technology 48 (5):2706–2714. doi: 10.1021/es4045693 [DOI] [PubMed] [Google Scholar]
- 32.Liu YC, Liggio J, Li SM, Breznan D, Vincent R, Thomson EM, Kumarathasan P, Das D, Abbatt J, Antinolo M, Russell L (2015) Chemical and Toxicological Evolution of Carbon Nanotubes During Atmospherically Relevant Aging Processes. Environmental Science & Technology 49 (5):2806–2814. doi: 10.1021/es505298d [DOI] [PubMed] [Google Scholar]
- 33.Sutherland I, Sheng E, Bradley RH, Freakley PK (1996) Effects of ozone oxidation on carbon black surfaces. J Mater Sci 31 (21):5651–5655. doi:Doi 10.1007/Bf01160810 [DOI] [Google Scholar]
- 34.Ciobanu M LA, Asaftei S. (2016) Chemical and electrochemical studies of carbon black surface by treatment with ozone and nitrogen oxide. . Materials Today – Proceedings 3 (Supplement 2):S252–S257 [Google Scholar]
- 35.Smith DM, Chughtai AR (1995) The Surface-Structure and Reactivity of Black Carbon. Colloid Surface A 105 (1):47–77. doi:Doi 10.1016/0927-7757(95)03337-1 [DOI] [Google Scholar]
- 36.Chughtai AR, Jassim JA, Peterson JH, Stedman DH, Smith DM (1991) Spectroscopic and Solubility Characteristics of Oxidized Soots. Aerosol Sci Tech 15 (2):112–126. doi:Doi 10.1080/02786829108959518 [DOI] [Google Scholar]
- 37.Chughtai AR, Brooks ME, Smith DM (1996) Hydration of black carbon. J Geophys Res-Atmos 101 (D14):19505–19514. doi:Doi 10.1029/95jd01882 [DOI] [Google Scholar]
- 38.Chughtai AR, Miller NJ, Smith DM, Pitts JR (1999) Carbonaceous particle hydration III. J Atmos Chem 34 (2):259–279. doi:Doi 10.1023/A:1006221326060 [DOI] [Google Scholar]
- 39.Ciobanu M, Lepadatu AM, Asaftei S (2016) Chemical and electrochemical studies of carbon black surface by treatment with ozone and nitrogen oxide. Mater Today-Proc 3:S252–S257. doi: 10.1016/j.matpr.2016.02.042 [DOI] [Google Scholar]
- 40.Koerten HK, Brederoo P, Ginsel LA, Daems WT (1986) The endocytosis of asbestos by mouse peritoneal macrophages and its long-term effect on iron accumulation and labyrinth formation. Eur J Cell Biol 40 (1):25–36 [PubMed] [Google Scholar]
- 41.Ghio AJ, Jaskot RH, Hatch GE (1994) Lung injury after silica instillation is associated with an accumulation of iron in rats. Am J Physiol 267 (6 Pt 1):L686–692 [DOI] [PubMed] [Google Scholar]
- 42.Sporn TA, Roggli VL (2008) Pneumoconioses, Mineral and Vegetable. In: Tomashefski JFJ, Cagle PT, Farver CF, Fraire AE (Editors) Dail and Hammar's Pulmonary Pathology. Volume I. Nonneoplastic Lung Disease 3rd edn. Springer, p 933 [Google Scholar]
- 43.Ghio AJ, Tong H, Soukup JM, Dailey LA, Cheng WY, Samet JM, Kesic MJ, Bromberg PA, Turi JL, Upadhyay D, Scott Budinger GR, Mutlu GM (2013) Sequestration of mitochondrial iron by silica particle initiates a biological effect. Am J Physiol Lung Cell Mol Physiol 305 (10):L712–724. doi: 10.1152/ajplung.00099.2013 [DOI] [PubMed] [Google Scholar]
- 44.Laughton MJ, Moroney MA, Hoult JR, Halliwell B (1989) Effects of desferrioxamine on eicosanoid production in two intact cell systems. Biochem Pharmacol 38 (1):189–193 [DOI] [PubMed] [Google Scholar]
- 45.Hileti D, Panayiotidis P, Hoffbrand AV (1995) Iron chelators induce apoptosis in proliferating cells. Br J Haematol 89 (1):181–187 [DOI] [PubMed] [Google Scholar]
- 46.Tanji K, Imaizumi T, Matsumiya T, Itaya H, Fujimoto K, Cui X, Toki T, Ito E, Yoshida H, Wakabayashi K, Satoh K (2001) Desferrioxamine, an iron chelator, upregulates cyclooxygenase-2 expression and prostaglandin production in a human macrophage cell line. Biochim Biophys Acta 1530 (2-3):227–235 [DOI] [PubMed] [Google Scholar]
- 47.Kim BS, Yoon KH, Oh HM, Choi EY, Kim SW, Han WC, Kim EA, Choi SC, Kim TH, Yun KJ, Kim EC, Lyou JH, Nah YH, Chung HT, Cha YN, Jun CD (2002) Involvement of p38 MAP kinase during iron chelator-mediated apoptotic cell death. Cell Immunol 220 (2):96–106 [DOI] [PubMed] [Google Scholar]
- 48.Lee SK, Jang HJ, Lee HJ, Lee J, Jeon BH, Jun CD, Lee SK, Kim EC (2006) p38 and ERK MAP kinase mediates iron chelator-induced apoptosis and -suppressed differentiation of immortalized and malignant human oral keratinocytes. Life Sci 79 (15):1419–1427. doi: 10.1016/j.lfs.2006.04.011 [DOI] [PubMed] [Google Scholar]
- 49.Huang X, Dai J, Huang C, Zhang Q, Bhanot O, Pelle E (2007) Deferoxamine synergistically enhances iron-mediated AP-1 activation: a showcase of the interplay between extracellular-signal-regulated kinase and tyrosine phosphatase. Free Radic Res 41 (10):1135–1142. doi: 10.1080/10715760701609061 [DOI] [PubMed] [Google Scholar]
- 50.Markel TA, Crisostomo PR, Wang M, Herring CM, Lahm T, Meldrum KK, Lillemoe KD, Rescorla FJ, Meldrum DR (2007) Iron chelation acutely stimulates fetal human intestinal cell production of IL-6 and VEGF while decreasing HGF: the roles of p38, ERK, and JNK MAPK signaling. Am J Physiol Gastrointest Liver Physiol 292 (4):G958–963. doi: 10.1152/ajpgi.00502.2006 [DOI] [PubMed] [Google Scholar]
- 51.Liu Y, Cui Y, Shi M, Zhang Q, Wang Q, Chen X (2014) Deferoxamine promotes MDA-MB-231 cell migration and invasion through increased ROS-dependent HIF-1alpha accumulation. Cell Physiol Biochem 33 (4):1036–1046. doi: 10.1159/000358674 [DOI] [PubMed] [Google Scholar]
- 52.Zhang W, Wu Y, Yan Q, Ma F, Shi X, Zhao Y, Peng Y, Wang J, Jiang B (2014) Deferoxamine enhances cell migration and invasion through promotion of HIF-1alpha expression and epithelial-mesenchymal transition in colorectal cancer. Oncol Rep 31 (1):111–116. doi: 10.3892/or.2013.2828 [DOI] [PubMed] [Google Scholar]
- 53.Ghio AJ, Soukup JM, Dailey LA (2016) Air pollution particles and iron homeostasis. Biochim Biophys Acta. doi: 10.1016/j.bbagen.2016.05.026 [DOI] [PubMed] [Google Scholar]
- 54.Lovstad RA (1991) The reaction of ferric- and ferrous salts with bleomycin. Int J Biochem 23 (2):235–238 [DOI] [PubMed] [Google Scholar]
- 55.Ueda N, Guidet B, Shah SV (1993) Gentamicin-induced mobilization of iron from renal cortical mitochondria. Am J Physiol 265 (3 Pt 2):F435–439 [DOI] [PubMed] [Google Scholar]
- 56.Elias Z, Poirot O, Daniere MC, Terzetti F, Binet S, Tomatis M, Fubini B (2002) Surface reactivity, cytotoxicity, and transforming potency of iron-covered compared to untreated refractory ceramic fibers. J Toxicol Environ Health A 65 (23):2007–2027. doi: 10.1080/00984100290071360 [DOI] [PubMed] [Google Scholar]
- 57.Jakab GJ, Hemenway DR (1994) Concomitant exposure to carbon black particulates enhances ozone-induced lung inflammation and suppression of alveolar macrophage phagocytosis. J Toxicol Environ Health 41 (2):221–231. doi: 10.1080/15287399409531838 [DOI] [PubMed] [Google Scholar]
- 58.Madden MC, Richards JH, Dailey LA, Hatch GE, Ghio AJ (2000) Effect of ozone on diesel exhaust particle toxicity in rat lung. Toxicol Appl Pharmacol 168 (2):140–148. doi: 10.1006/taap.2000.9024 [DOI] [PubMed] [Google Scholar]
- 59.Kafoury RM, Kelley J (2005) Ozone enhances diesel exhaust particles (DEP)-induced interleukin-8 (IL-8) gene expression in human airway epithelial cells through activation of nuclear factors- kappaB (NF-kappaB) and IL-6 (NF-IL6). Int J Environ Res Public Health 2 (3-4):403–410 [DOI] [PubMed] [Google Scholar]
- 60.Molhave L, Kjaergaard SK, Sigsgaard T, Lebowitz M (2005) Interaction between ozone and airborne particulate matter in office air. Indoor Air 15 (6):383–392. doi: 10.1111/j.1600-0668.2005.00366.x [DOI] [PubMed] [Google Scholar]
- 61.Chen GH, Song GX, Jiang LL, Zhang YH, Zhao NQ, Chen BH, Kan HD (2007) Interaction between ambient particles and ozone and its effect on daily mortality. Biomed Environ Sci 20 (6):502–505 [PubMed] [Google Scholar]
- 62.Bosson J, Barath S, Pourazar J, Behndig AF, Sandstrom T, Blomberg A, Adelroth E (2008) Diesel exhaust exposure enhances the ozone-induced airway inflammation in healthy humans. Eur Respir J 31 (6):1234–1240. doi: 10.1183/09031936.00078407 [DOI] [PubMed] [Google Scholar]
- 63.Madden MC, Stevens T, Case M, Schmitt M, Diaz-Sanchez D, Bassett M, Montilla TS, Berntsen J, Devlin RB. Diesel Exhaust Modulates Ozone-induced Lung Function Decrements in Healthy Human Volunteers. doi: 10.1186/s12989-014-0037-5. Particle and Fibre Toxicology. 2014. 11(1):37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Stiegel MA, Pleil JD, Sobus JR, Madden MC (2016) Inflammatory Cytokines and White Blood Cell Counts Response to Environmental Levels of Diesel Exhaust and Ozone Inhalation Exposures. PLoS One 11 (4):e0152458. doi: 10.1371/journal.pone.0152458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.U.S. Department of Health and Human Services, Centers for Disease Control, Coordinating Center for Health Promotion, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health (2006) The Health Consequences of Involuntary Exposure to Tobacco Smoke: A Report of the Surgeon General. U.S. Department of Health and Human Services, Atlanta, Georgia: [PubMed] [Google Scholar]
- 66.Ciencewicki J, Jaspers I (2007) Air pollution and respiratory viral infection. Inhal Toxicol 19 (14):1135–1146. doi: 10.1080/08958370701665434 [DOI] [PubMed] [Google Scholar]
- 67.Leonardi-Bee J, Smyth A, Britton J, Coleman T (2008) Environmental tobacco smoke and fetal health: systematic review and meta-analysis. Arch Dis Child Fetal Neonatal Ed 93 (5):F351–361. doi: 10.1136/adc.2007.133553 [DOI] [PubMed] [Google Scholar]
- 68.Stillerman KP, Mattison DR, Giudice LC, Woodruff TJ (2008) Environmental exposures and adverse pregnancy outcomes: a review of the science. Reprod Sci 15 (7):631–650. doi: 10.1177/1933719108322436 [DOI] [PubMed] [Google Scholar]
- 69.Chang JS (2009) Parental smoking and childhood leukemia. Methods Mol Biol 472:103–137. doi: 10.1007/978-1-60327-492-0_5 [DOI] [PubMed] [Google Scholar]
- 70.National Center for Environmental Assessment (2009) Integrated Science Assessment (ISA) for Particulate Matter. US Environmental Protection Agency., Research Triangle Park, North Carolina [Google Scholar]
- 71.Pate Capps N, Stewart A, Burns C (2009) The interplay between secondhand cigarette smoke, genetics, and cervical cancer: a review of the literature. Biol Res Nurs 10 (4):392–399. doi: 10.1177/1099800408330849 [DOI] [PubMed] [Google Scholar]
- 72.Franchini M, Mannucci PM (2011) Thrombogenicity and cardiovascular effects of ambient air pollution. Blood 118 (9):2405–2412. doi: 10.1182/blood-2011-04-343111 [DOI] [PubMed] [Google Scholar]
- 73.Johnson KC, Miller AB, Collishaw NE, Palmer JR, Hammond SK, Salmon AG, Cantor KP, Miller MD, Boyd NF, Millar J, Turcotte F (2011) Active smoking and secondhand smoke increase breast cancer risk: the report of the Canadian Expert Panel on Tobacco Smoke and Breast Cancer Risk (2009). Tobacco control 20 (1):e2. doi: 10.1136/tc.2010.035931 [DOI] [PubMed] [Google Scholar]
- 74.Bentayeb M, Simoni M, Norback D, Baldacci S, Maio S, Viegi G, Annesi-Maesano I (2013) Indoor air pollution and respiratory health in the elderly. J Environ Sci Health A Tox Hazard Subst Environ Eng 48 (14):1783–1789. doi: 10.1080/10934529.2013.826052 [DOI] [PubMed] [Google Scholar]
- 75.Link MS, Luttmann-Gibson H, Schwartz J, Mittleman MA, Wessler B, Gold DR, Dockery DW, Laden F (2013) Acute exposure to air pollution triggers atrial fibrillation. J Am Coll Cardiol 62 (9):816–825. doi: 10.1016/j.jacc.2013.05.043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Stocks J, Sonnappa S (2013) Early life influences on the development of chronic obstructive pulmonary disease. Ther Adv Respir Dis 7 (3):161–173. doi: 10.1177/1753465813479428 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.U.S. Department of Health and Human Services, Centers for Disease Control, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health (2014) The Health Consequences of Smoking: 50 Years of Progress. A Report of the Surgeon General. U.S. Department of Health and Human Services, Atlanta, Georgia [Google Scholar]
- 78.Wang B, Xu D, Jing Z, Liu D, Yan S, Wang Y (2014) Effect of long-term exposure to air pollution on type 2 diabetes mellitus risk: a systemic review and meta-analysis of cohort studies. Eur J Endocrinol 171 (5):R173–182. doi: 10.1530/EJE-14-0365 [DOI] [PubMed] [Google Scholar]
- 79.Cao S, Yang C, Gan Y, Lu Z (2015) The Health Effects of Passive Smoking: An Overview of Systematic Reviews Based on Observational Epidemiological Evidence. PLoS One 10 (10):e0139907. doi: 10.1371/journal.pone.0139907 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Macacu A, Autier P, Boniol M, Boyle P (2015) Active and passive smoking and risk of breast cancer: a meta-analysis. Breast Cancer Res Treat 154 (2):213–224. doi: 10.1007/s10549-015-3628-4 [DOI] [PubMed] [Google Scholar]
- 81.Wei X, E M, Yu S (2015) A meta-analysis of passive smoking and risk of developing Type 2 Diabetes Mellitus. Diabetes Res Clin Pract 107 (1):9–14. doi: 10.1016/j.diabres.2014.09.019 [DOI] [PubMed] [Google Scholar]
- 82.Dixit S, Pletcher MJ, Vittinghoff E, Imburgia K, Maguire C, Whitman IR, Glantz SA, Olgin JE, Marcus GM (2016) Secondhand smoke and atrial fibrillation: Data from the Health eHeart Study. Heart Rhythm 13 (1):3–9. doi: 10.1016/j.hrthm.2015.08.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Hori M, Tanaka H, Wakai K, Sasazuki S, Katanoda K (2016) Secondhand smoke exposure and risk of lung cancer in Japan: a systematic review and meta-analysis of epidemiologic studies. Jpn J Clin Oncol 46 (10):942–951. doi: 10.1093/jjco/hyw091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Wang F, Jia X, Wang X, Zhao Y, Hao W (2016) Particulate matter and atherosclerosis: a bibliometric analysis of original research articles published in 1973-2014. BMC Public Health 16:348. doi: 10.1186/s12889-016-3015-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Nelson L, Valle J, King G, Mills PK, Richardson MJ, Roberts EM, Smith D, English P (2017) Estimating the Proportion of Childhood Cancer Cases and Costs Attributable to the Environment in California. Am J Public Health 107 (5):756–762. doi: 10.2105/AJPH.2017.303690 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Hoffmann B, Moebus S, Kroger K, Stang A, Mohlenkamp S, Dragano N, Schmermund A, Memmesheimer M, Erbel R, Jockel KH (2009) Residential exposure to urban air pollution, ankle-brachial index, and peripheral arterial disease. Epidemiology 20 (2):280–288. doi: 10.1097/EDE.0b013e3181961ac2 [DOI] [PubMed] [Google Scholar]
- 87.Ananthakrishnan AN, McGinley EL, Binion DG, Saeian K (2011) Ambient air pollution correlates with hospitalizations for inflammatory bowel disease: an ecologic analysis. Inflamm Bowel Dis 17 (5):1138–1145. doi: 10.1002/ibd.21455 [DOI] [PubMed] [Google Scholar]
- 88.Song Q, Christiani DC, Xiaorong Wang, Ren J (2014) The global contribution of outdoor air pollution to the incidence, prevalence, mortality and hospital admission for chronic obstructive pulmonary disease: a systematic review and meta-analysis. Int J Environ Res Public Health 11 (11):11822–11832. doi: 10.3390/ijerph111111822 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Chen Z, Salam MT, Karim R, Toledo-Corral CM, Watanabe RM, Xiang AH, Buchanan TA, Habre R, Bastain TM, Lurmann F, Taher M, Wilson JP, Trigo E, Gilliland FD (2015) Living near a freeway is associated with lower bone mineral density among Mexican Americans. Osteoporos Int 26 (6):1713–1721. doi: 10.1007/s00198-015-3051-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Ravilla TD, Gupta S, Ravindran RD, Vashist P, Krishnan T, Maraini G, Chakravarthy U, Fletcher AE (2016) Use of Cooking Fuels and Cataract in a Population-Based Study: The India Eye Disease Study. Environ Health Perspect 124 (12):1857–1862. doi: 10.1289/EHP193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Magnani C, Ranucci A, Badaloni C, Cesaroni G, Ferrante D, Miligi L, Mattioli S, Rondelli R, Bisanti L, Zambon P, Cannizzaro S, Michelozzi P, Cocco P, Celentano E, Assennato G, Merlo DF, Mosciatti P, Minelli L, Cuttini M, Torregrossa MV, Lagorio S, Haupt R, Forastiere F, Group SW (2016) Road Traffic Pollution and Childhood Leukemia: A Nationwide Case-control Study in Italy. Arch Med Res 47 (8):694–705. doi: 10.1016/j.arcmed.2017.02.001 [DOI] [PubMed] [Google Scholar]
- 92.Andersen ZJ, Stafoggia M, Weinmayr G, Pedersen M, Galassi C, Jorgensen JT, Oudin A, Forsberg B, Olsson D, Oftedal B, Aasvang GM, Aamodt G, Pyko A, Pershagen G, Korek M, De Faire U, Pedersen NL, Ostenson CG, Fratiglioni L, Eriksen KT, Tjonneland A, Peeters PH, Bueno-de-Mesquita B, Plusquin M, Key TJ, Jaensch A, Nagel G, Lang A, Wang M, Tsai MY, Fournier A, Boutron-Ruault MC, Baglietto L, Grioni S, Marcon A, Krogh V, Ricceri F, Sacerdote C, Migliore E, Tamayo-Uria I, Amiano P, Dorronsoro M, Vermeulen R, Sokhi R, Keuken M, de Hoogh K, Beelen R, Vineis P, Cesaroni G, Brunekreef B, Hoek G, Raaschou-Nielsen O (2017) Long-Term Exposure to Ambient Air Pollution and Incidence of Postmenopausal Breast Cancer in 15 European Cohorts within the ESCAPE Project. Environ Health Perspect 125 (10):107005. doi: 10.1289/EHP1742 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Fuks KB, Weinmayr G, Basagana X, Gruzieva O, Hampel R, Oftedal B, Sorensen M, Wolf K, Aamodt G, Aasvang GM, Aguilera I, Becker T, Beelen R, Brunekreef B, Caracciolo B, Cyrys J, Elosua R, Eriksen KT, Foraster M, Fratiglioni L, Hilding A, Houthuijs D, Korek M, Kunzli N, Marrugat J, Nieuwenhuijsen M, Ostenson CG, Penell J, Pershagen G, Raaschou-Nielsen O, Swart WJR, Peters A, Hoffmann B (2017) Long-term exposure to ambient air pollution and traffic noise and incident hypertension in seven cohorts of the European study of cohorts for air pollution effects (ESCAPE). Eur Heart J 38 (13):983–990. doi: 10.1093/eurheartj/ehw413 [DOI] [PubMed] [Google Scholar]
- 94.Yang YR, Chen YM, Chen SY, Chan CC (2017) Associations between Long-Term Particulate Matter Exposure and Adult Renal Function in the Taipei Metropolis. Environ Health Persp 125 (4):602–607. doi: 10.1289/Ehp302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Campen MJ, Lund A, Rosenfeld M (2012) Mechanisms linking traffic-related air pollution and atherosclerosis. Curr Opin Pulm Med 18 (2):155–160. doi: 10.1097/MCP.0b013e32834f210a [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Bai Y, Sun Q (2016) Fine particulate matter air pollution and atherosclerosis: Mechanistic insights. Biochim Biophys Acta 1860 (12):2863–2868. doi: 10.1016/j.bbagen.2016.04.030 [DOI] [PubMed] [Google Scholar]
- 97.Ye X, Peng L, Kan H, Wang W, Geng F, Mu Z, Zhou J, Yang D (2016) Acute Effects of Particulate Air Pollution on the Incidence of Coronary Heart Disease in Shanghai, China. PLoS One 11 (3):e0151119. doi: 10.1371/journal.pone.0151119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Hartiala J, Breton CV, Tang WH, Lurmann F, Hazen SL, Gilliland FD, Allayee H (2016) Ambient Air Pollution Is Associated With the Severity of Coronary Atherosclerosis and Incident Myocardial Infarction in Patients Undergoing Elective Cardiac Evaluation. J Am Heart Assoc 5 (8). doi: 10.1161/JAHA.116.003947 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Malek AM, Cushman M, Lackland DT, Howard G, McClure LA (2015) Secondhand Smoke Exposure and Stroke: The Reasons for Geographic and Racial Differences in Stroke (REGARDS) Study. Am J Prev Med 49 (6):e89–97. doi: 10.1016/j.amepre.2015.04.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Fischer F, Kraemer A (2015) Meta-analysis of the association between second-hand smoke exposure and ischaemic heart diseases, COPD and stroke. BMC Public Health 15:1202. doi: 10.1186/s12889-015-2489-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Shah AS, Lee KK, McAllister DA, Hunter A, Nair H, Whiteley W, Langrish JP, Newby DE, Mills NL (2015) Short term exposure to air pollution and stroke: systematic review and meta-analysis. BMJ 350:h1295. doi: 10.1136/bmj.h1295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Ljungman PL, Mittleman MA (2014) Ambient air pollution and stroke. Stroke 45 (12):3734–3741. doi: 10.1161/STROKEAHA.114.003130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Rich DQ, Mittleman MA, Link MS, Schwartz J, Luttmann-Gibson H, Catalano PJ, Speizer FE, Gold DR, Dockery DW (2006) Increased risk of paroxysmal atrial fibrillation episodes associated with acute increases in ambient air pollution. Environ Health Perspect 114 (1):120–123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Monrad M, Sajadieh A, Christensen JS, Ketzel M, Raaschou-Nielsen O, Tjonneland A, Overvad K, Loft S, Sorensen M (2017) Long-Term Exposure to Traffic-Related Air Pollution and Risk of Incident Atrial Fibrillation: A Cohort Study. Environ Health Perspect 125 (3):422–427. doi: 10.1289/EHP392 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Ghio AJ (2014) Particle exposures and infections. Infection 42 (3):459–467. doi: 10.1007/s15010-014-0592-6 [DOI] [PubMed] [Google Scholar]
- 106.Thiering E, Heinrich J (2015) Epidemiology of air pollution and diabetes. Trends Endocrinol Metab 26 (7):384–394. doi: 10.1016/j.tem.2015.05.002 [DOI] [PubMed] [Google Scholar]
- 107.Eze IC, Hemkens LG, Bucher HC, Hoffmann B, Schindler C, Kunzli N, Schikowski T, Probst-Hensch NM (2015) Association between ambient air pollution and diabetes mellitus in Europe and North America: systematic review and meta-analysis. Environ Health Perspect 123 (5):381–389. doi: 10.1289/ehp.1307823 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Pineles BL, Hsu S, Park E, Samet JM (2016) Systematic Review and Meta-Analyses of Perinatal Death and Maternal Exposure to Tobacco Smoke During Pregnancy. Am J Epidemiol 184 (2):87–97. doi: 10.1093/aje/kwv301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Christie B (2015) Smoke-free legislation in England has reduced stillbirths, neonatal mortality, and low birth weight. BMJ 351:h4469. doi: 10.1136/bmj.h4469 [DOI] [PubMed] [Google Scholar]
- 110.Gehring U, Tamburic L, Sbihi H, Davies HW, Brauer M (2014) Impact of noise and air pollution on pregnancy outcomes. Epidemiology 25 (3):351–358. doi: 10.1097/EDE.0000000000000073 [DOI] [PubMed] [Google Scholar]
- 111.Amegah AK, Quansah R, Jaakkola JJ (2014) Household air pollution from solid fuel use and risk of adverse pregnancy outcomes: a systematic review and meta-analysis of the empirical evidence. PLoS One 9 (12):e113920. doi: 10.1371/journal.pone.0113920 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Smith RB, Fecht D, Gulliver J, Beevers SD, Dajnak D, Blangiardo M, Ghosh RE, Hansell AL, Kelly FJ, Anderson HR, Toledano MB (2017) Impact of London's road traffic air and noise pollution on birth weight: retrospective population based cohort study. BMJ 359:j5299. doi: 10.1136/bmj.j5299 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Erickson AC, Ostry A, Chan HM, Arbour L (2016) Air pollution, neighbourhood and maternal-level factors modify the effect of smoking on birth weight: a multilevel analysis in British Columbia, Canada. BMC Public Health 16 (1):585. doi: 10.1186/s12889-016-3273-9 [DOI] [PMC free article] [PubMed] [Google Scholar]


