Abstract
Objective
To evaluate the clinical efficacy of free flap transplantation combined with Ilizarov bone transport in the treatment of severe composite tibial and soft tissue defects.
Methods
We retrospectively analyzed the clinical data of 40 patients with severe composite tibial and soft tissue defects who underwent free flap transplantation combined with Ilizarov bone transport. The clinical efficacy was evaluated according to the following criteria: success rate of wound repair by free flap transplantation, incidence or recurrence rate of deep infection, healing rate of bone defects and external fixation index, incidence of complications, and functional score of affected extremities.
Results
All infections were generally well controlled by radical debridement and negative-pressure therapy, and all 40 patients’ wounds healed after repair and reconstruction of the tibia and soft tissues. Postoperative complications were alleviated by active treatment. The mean external fixation time was 12.83 ± 2.85 months, and the external fixation index was 1.55 m/cm. According to the Association for the Study and Application of Methods of Ilizarov (ASAMI) score, an excellent or good functional outcome was attained in 85% of patients.
Conclusion
Free flap transplantation combined with Ilizarov bone transport is an effective treatment for severe composite tibial and soft tissue defects.
Keywords: Free flap transplantation, Ilizarov bone transport, soft tissue defect, open fracture, clinical efficacy, functional outcome
Introduction
Open and comminuted fractures of the lower extremities caused by high-energy injury are commonly accompanied by severe injuries or defects of the surrounding soft tissues as well as necrosis and infection of the bone and soft tissues. Large residual tibial (or fibular) and soft tissue defects often remain after debridement in these patients. Such cases are challenging to treat, and severe defects may even require amputation.1 Effective repair of tissue defects, reconstruction of extremity function, and infection control have always been difficult in clinical orthopedics.2,3 Early coverage of the wound refers to covering the wound as soon as possible after the necrotic tissue has been cleaned. The vitality of the damaged tissue is difficult to estimate, especially for war-related firearm injuries, introducing further treatment difficulties.4
Multiple methods have been adopted to repair tissue defects. Among them, Ilizarov bone transport (distraction osteogenesis) and free tissue transplantation (vascularized bone and soft tissue transplantation) are considered effective and have been applied to treat composite bone and soft tissue defects in clinical practice. Zhen et al.5 and Rozbruch et al.6 applied free tissue transplantation and bone transport, respectively, to achieve reconstruction of tibial bone and surrounding soft tissue defects. However, the combination of free tissue transplantation and Ilizarov bone transport can be used to more effectively treat severe composite tibial and soft tissue defects, making this technique a hot topic in the field of extremity repair and reconstruction.
With the recent developments of surgical flap techniques, particularly perforator flap surgery, the damage to the donor site has been significantly reduced and the range of application has become wider.7,8 Free flaps can be used not only to repair the wound and prevent deep tissues necrosis but also to mitigate local infection and enhance patients’ comfort, providing an excellent soft tissue environment for subsequent surgery. Consequently, we prefer to use free flaps to repair the wounds following debridement during treatment of composite bone and soft tissue defects. In this study, we reviewed the data of patients with severe composite tibial bone and soft tissue defects treated in our department from July 2012 to December 2018. Specifically, we evaluated the clinical efficacy of free flap transplantation combined with Ilizarov bone transport.
Materials and methods
Baseline data
In this retrospective study, we reviewed the records of 40 patients with severe composite tibial bone and soft tissue defects who had complete follow-up data. The injuries involved 18 left and 22 right legs, and the study population comprised 27 male and 13 female patients ranging in age from 16 to 65 years. The injuries were caused by vehicle accidents in 26 patients, a fall from a height in 9 patients, and crushing injuries in 5 patients. Among the 40 patients, 25 had undergone preliminary debridement in local hospitals. Injuries were found in the middle tibia in 18 patients, in the distal tibia in 12, and in the proximal tibia in 10; additionally, 15 patients’ injuries were complicated with fibular fractures. All injuries were categorized as Gustilo type IIIB according to their severity. The length of the tibial defects ranged from 4 to 18 cm (average, 8.25 cm). The size of the soft tissue defects ranged from 7.5 × 5.0 cm to 35.0 × 30.0 cm (measured after thorough debridement); the defects could not be repaired by local flap transfer even after limb shortening. Six patients had complicated ipsilateral extremity fractures, 10 had fractures in other sites, and 6 had other injuries.
Surgical procedures
According to our previously described methods,7,8 debridement was carried out in the early stage. A simple external fixator was used to fix the fracture on an emergency basis following the principle of “damage control.” A vacuum sealing drainage tube or negative-pressure sponge (KCI Technologies, San Antonio, TX, USA) was used to temporarily cover the wounds. In the second stage of repair and reconstruction surgery, the simple external fixator was replaced by a transportable external fixator (Orthofix Medical Inc., Lewisville, TX, USA or Tianjin Xinzhong Medical Devices Co., Ltd., Tianjin, China) as described by Nayagam,9 and tibial osteotomy (transport) and free flap transplantation were performed simultaneously or consecutively. Following free flap transplantation, conventional microsurgical treatments were provided, such as anti-infection, anti-spasm, and anti-coagulation interventions with real-time observation of the flap blood supply to assess survival of the free flap and the occurrence of serious complications after the operation. Vascular crises and other postoperative complications were treated timely and effectively. According to the classic method proposed by Ilizarov,10 bone sliding was performed at a speed of 0.5 to 1.0 mm/day two to four times a day beginning 1 week postoperatively and was continued until the bilateral fractured ends contacted each other. If the contact area between the bilateral fractured ends was too small, bone grafting was performed in a timely manner. If the contact area was adequately large, compression and the “accordion” maneuver were adopted to accelerate bone healing.11,12 The external fixator was removed if X-ray examination demonstrated cortex continuity at least on three sides of the fractured bone, the density of the new bone transported by osteotomy close to that of the normal bone, or no significant discomfort after 1 week of walking with a loose external fixation pin.13
Evaluation of clinical efficacy
Clinical efficacy was evaluated using the following criteria: the success rate of wound repair by the skin flap, the healing rate of the bone defects and the external fixator index (external fixation time/length of tibial bone defect), the incidence or recurrence rate of deep infection, the incidence of complications, and the Association for the Study and Application of Methods of Ilizarov (ASAMI) score of the lower extremity.14
Results
No obvious infection occurred in any of the 40 patients after thorough debridement and one to three negative-pressure treatments; thus, all wounds were ready for subsequent repair and reconstruction. The postoperative follow-up time was 18 to 60 months (average, 28.2 months). A unilateral external fixator was used in 28 patients, an annular external fixator in nine, and a unilateral–annular combined external fixator in three. The wounds healed well in all 40 patients after flap transplantation, including anterolateral femoral flaps (n = 33), latissimus dorsi flaps (n = 5), and thoraco-umbilical flaps (n = 2). The postoperative complications and treatments are shown in Table 1. The mean time interval from bone transport to removal of the external fixator was 12.83 ± 2.85 months (range, 10–24 months). The mean external fixation index was 1.55 m/cm. According to the ASAMI functional scores, excellent functional outcomes were obtained in 24 (60%) patients, good in 10 (25%), moderate in 4 (10%), and poor in 2 (5%). A representative case is shown in Figure 1.
Table 1.
Incidence and management of postoperative complications.
| Complication | Number of patients (n = 40) | Management | Outcome |
|---|---|---|---|
| Flap crisis | 3 | Vascular exploration | Survived completely (n = 1); slight flap necrosis healed after debridement, grafting, or dressing change (n = 2) |
| Developed hydrops or fat liquefaction surrounding the flap | 5 | Dressing change | Healed |
| Nonunion of bone defect | 8 | Iliac bone graft | Healed |
| Deep infection | 0 | / | / |
| Refracture | 2 | External fixation for another 6 months | Bone union |
| Severe nail tunnel reaction or mechanical axis deviation | 10 | Nail/needle replacement, mechanical axis adjustment | Improved |
| Joint stiffness (ankle joint stiffness, foot drop, claw toe) | 8 | Release and decompression operation, foot ring | Improved |
| Limb shortening (<2 cm) | 4 | Wearing of elevated insoles | Improved |
| Limb shortening (>3 cm) | 1 | Re-osteotomy and lengthening | Healed |
Note: The number of complications refers to the number of patients presenting with complications. One patient may have successively or simultaneously had different complications, and patients may have simultaneously undergone one or more procedures during surgical treatment.
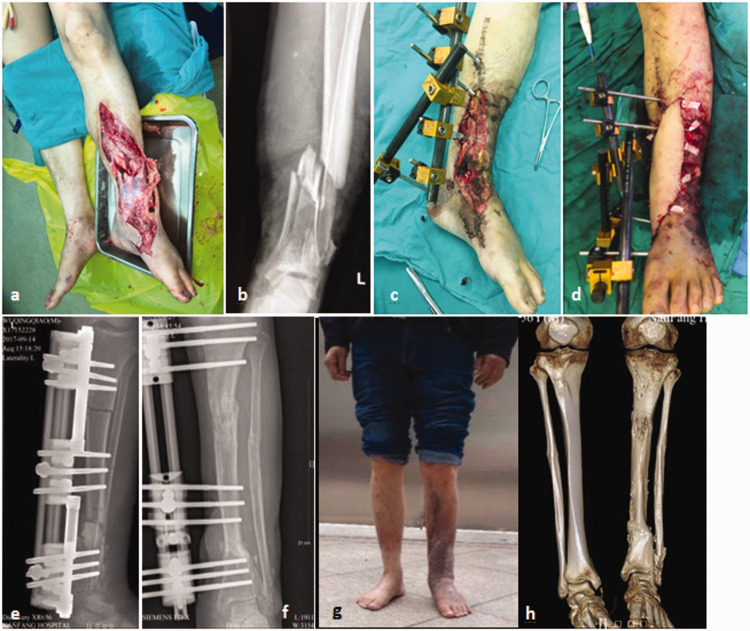
Figure 1.
Representative case. (a, b) A 55-year-old man sustained open injuries (Gustilo IIIB) in the left lower limb caused by a vehicle accident. Debridement, fracture reduction and external fixation, local skin avulsion and grafting, and vacuum sealing drainage of the wounds (twice) were carried out. (c, d) At 14 days postoperatively, a free anterolateral thigh flap (approximately 6.5 × 18 cm) was adopted and the lower limb was temporarily shorter by 3 cm. (e) At 1 month after flap transplantation, the external fixator was adjusted and osteotomy and bone transport were performed; by then, the length of the tibial defects was approximately 8 cm. (f) At 12 months after bone transport, X-ray examination showed healing of the bone fracture, and the external fixator was scheduled to be removed. The patient eventually developed 2-cm shortening of the affected lower limb and approximately 10° dorsiflexion restriction of the ankle joint. The postoperative external fixation time was 11 months, and the external fixation index was 1.375. The postoperative ASAMI functional score of the affected limb was excellent. (h, g) Clinical appearance and computed tomography findings 18 months after bone transport.
Discussion
How to repair and reconstruct large tibial bone and soft tissue defects involves complicated decision-making. Various repair methods are currently used, including the Ilizarov technique15–17 (bone and soft tissue traction), microsurgical technique5,18,19 (vascularized bone and soft tissue transplantation), Masquelet technique,13 stage II cancellous bone grafting after wound closure, and Papineau technique (open bone grafting).20 These methods have respective advantages and disadvantages. In particular, the Masquelet induced membrane technique is another more recent treatment method for bone defects. However, this technique requires a secondary surgery, making it difficult to treat soft tissue defects. In the present study, a free flap was combined with Ilizarov bone transport for repair and reconstruction.
Compared with vascularized fibular flap transplantation, the treatment regimen in this study has the following advantages. First, it avoids damage to the donor site of the fibula. Second, it is easier to perform isolated soft tissue flap transplantation than to simultaneously transplant both the bone and soft tissue flap. Moreover, the newly transported tibial bone is strong and the time of repair and remodeling is short. Application of Ilizarov bone transport, in which the shortening–lengthening strategy is adopted, can simplify the repair of bone and soft tissue defects.21 Compared with the distraction osteogenesis technique involving open bone transport and wound exposure, this approach has some advantages including earlier coverage of the wound and reduced exposure time, mitigating the inconvenience and fear associated with frequent dressing changes. More importantly, it reduces the risk of infection recurrence and increases the blood supply and nutrient substance of the fracture site.22 In addition, the texture of the flap is better than that of the skin and soft tissues regenerated by the Ilizarov technique because of the lack of bone-attached scarring, less abrasion, an excellent appearance, and a higher level of comfort. This technique also provides an excellent soft tissue environment for subsequent surgeries, such as replacement of the external fixator with a plate for internal fixation and bone grafting for bone nonunion. Previous studies showed that after free flap transplantation, the anastomosed vessels were not affected by Ilizarov bone transport, and no flap necrosis developed secondary to vascular crises occurring during the distraction process.23,24
Despite its advantages, this method has certain risks and limitations. We consider the use of a local flap for repair of the wound after extremity shortening. Therefore, we may not give priority to this method in some cases, such as patients with only a small wound after limb shortening that is expected to be regenerated by the Ilizarov technique in a short time. We prefer treatment by open bone transport in patients with poor soft tissue, with no blood vessels in the receiving area, or who have not undergone treatment by a free skin flap. However, for patients with longitudinal hemi-cortical defects adjacent to joints or the tibia, we recommended free fibular flap transplantation to shorten the treatment time and accelerate the healing of bone defects.
A free flap combined with Ilizarov bone transport was adopted in the present study. How did we combine these two methods organically throughout the treatment procedure? Briefly, we used or replaced the transport external fixator to carry out segmental resection after primary or secondary debridement. Free flaps were transplanted after limb shortening and wound reduction. Tibial osteotomy and bone transport were performed at the same time or 1 week later. Nevertheless, the treatment plan should be adjusted according to the severity of the injury, contamination, and defects as well as the patient’s general condition and economic situation. In this study, 15 patients initially underwent free flap coverage of the wounds, and the final transport-type external fixators were replaced about 1 month later. Among these 15 patients, the wounds were located at the proximal or distal tibia in eight patients. A temporary external fixator was installed across the joint instead of inserting the fixation pin of the external fixator via the exposed bone surface. The tibia was retained in seven patients because the severity of tibial necrosis and infection could not be assessed in the early stage. Initially, the flap was used to cover the wounds; resection of the bone segment and replacement of the external fixator were subsequently performed during the later stage.
We selected different transport-type external fixators according to the type of injury. A unilateral external fixator is comfortable to wear, serving as an optimal choice in clinical practice.25–27 However, a circular external fixator or unilateral–circular combined external fixator is needed if the distal or proximal bone segments are short. During placement of a transport-type external fixator, it is necessary to maintain the mechanical axis in a correct position, minimize the angulation and rotation, and avoid damage to the surrounding vessels and nerves during pin insertion. Because the peroneal nerve is located adjacent to the fibular head, close attention should be paid when inserting the pin into the proximal limb. Baruah et al.28 reported that proximal fibula transfixation wires are safe to pass within 2 cm from the tip of the styloid process of the fibula. Given the possibility of bone sliding at the proximal or distal fibula, pins (or wires) must be used to penetrate the tibiofibular syndesmosis at the upper and lower tibiofibula. The shortening technique is commonly adopted to shrink the wound and accelerate the contact between the bilateral fractured ends. However, the length of shortening should be within a certain range (no more than 4–6 cm). The blood circulation of the extremities should be monitored after shortening to avoid ischemic necrosis at the distal extremity caused by vascular overlap and kinking. Some studies have demonstrated that the “shortening–lengthening technique” shortens the bone healing time and decreases the proportion of bone grafting.6,15,16,29
Free flaps are useful in the donor site with stable dissection and a hidden location. In clinical practice, anterolateral thigh flaps, thoraco-umbilical flaps, and latissimus dorsi flaps are commonly adopted with respective advantages and disadvantages.7 When choosing the flap for the donor site, we give priority to the flap that is most familiar to the surgeon. The anterolateral thigh flap has the most advantages30 and is the most skillfully placed flap in our institution; thus, it is given high priority. Flaps carrying muscle and fascial tissues can simultaneously repair muscle and tendon defects of the affected lower extremity, whereas flaps with cutaneous or muscular nerves can repair nerve defects. Considering the vascular variations of free flaps and recipient vessels, Doppler ultrasound and computed tomography angiography examinations should be conducted before surgery to provide the foundation for an appropriate treatment strategy. When vascular defects occur in the recipient area, bridging with vein transplantation,31 the flow-through vascular anastomosis technique,32 or T-anastomosis33 can be performed as required. However, bridge flap repair is the last option when no vessels are available for anastomosis in the recipient area of the lower extremity.
In this study, all patients achieved clinical healing after individualized treatment. However, some patients underwent secondary surgery because of postoperative complications. Venous crises occurred in three patients within 48 hours postoperatively; however, the flaps survived after exploration and repair. Ilizarov bone transport is associated with a risk of multiple complications such as infection of deep and superficial tissues, nonunion or delayed union of bone fractures, re-fracture, and mechanical axis deviation. It is generally believed that mechanical axis deviation occurs during intraoperative placement of the external fixator and is further exaggerated after long-time transport. Therefore, the mechanical axis should be properly adjusted during intraoperative placement of the external fixator. A unilateral external fixator is applied for eccentric fixation, and the traction force is not uniform; this is more likely to cause mechanical axis deviation. Insertion of wires (pins) into the closing ends of the transported bone segments can reduce the mechanical axis deviation. Frequent postoperative follow-up and X-ray examinations are required. Specifically, X-ray examinations should be conducted two or three times a month within 2 to 3 months postoperatively, and corresponding adjustments should be made in a timely manner. The bilateral bone ends should be trimmed and leveled during removal of bone segments, creating a larger area of contact for the bone ends and reducing the incidence of nonunion. In our study, the external fixation index was 1.55 m/cm and the rate of excellent and good functional outcomes was 85%; both of these parameters were higher than the 1.64 m/cm and 72%, respectively, reported by Yin et al.34
This study has two main limitations. First, because this was a retrospective analysis of cases, it was a non-controlled study without comparison with other repair methods. Second, this was a single-center study with a limited number of cases. More rigorous and large-scale research is needed.
Conclusions
Treatment of severe composite tibial bone and soft tissue defects is challenging. Such defects require long treatment periods and demanding techniques, leading to postoperative complications and sequelae in some patients. Following radical debridement, free flap transplantation combined with tibial bone transport is an efficacious treatment for severe composite tibial bone and soft tissue defects. This procedure deserves wider application in clinical practice, with appropriate modification and improvement of certain technical details.
Footnotes
Ethics approval and consent to participate: The study protocol was approved by the ethics committee of Nanfang Hospital, Southern Medical University (ethics approval No. 2020CR008). All patients agreed to participate in this study and provided written informed consent.
Declaration of conflicting interest: The authors declare that there is no conflict of interest.
Funding: This work was supported by the Clinical Research Program of Nanfang Hospital, Southern Medical University (2020CR008); the Shanghai Wang Zhengguo Trauma Medical Development Foundation (2017KJB-GK-001); and the Natural Science Foundation of Guangdong Province (2018A030313640, 2019A1515012176).
ORCID iD: Runguang Li https://orcid.org/0000-0002-4703-7180
References
- 1.Fioravanti M, Maman P, Curvale G, et al. Amputation versus conservative treatment in severe open lower-limb fracture: a functional and quality-of-life study. Orthop Traumatol Surg Res 2018; 104: 277–281. [DOI] [PubMed] [Google Scholar]
- 2.Chimutengwende-Gordon M, Mbogo A, Khan W, et al. Limb reconstruction after traumatic bone loss. Injury 2017; 48: 206–213. [DOI] [PubMed] [Google Scholar]
- 3.Grubor P, Milicevic S, Grubor M, et al. Treatment of bone defects in war wounds: retrospective study. Med Arch 2015; 69: 260–264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Grubor P, Falzarano G, Grubor M, et al. Treatment of the chronic war tibial osteomyelitis, Gustilio type IIIB and Cierny Mader IIIB, using various methods. A retrospective study. EuroMediterr Biomed J 2014; 9: 7–18. [Google Scholar]
- 5.Zhen P, Hu YY, Luo ZJ, et al. One-stage treatment and reconstruction of Gustilo type III open tibial shaft fractures with a vascularized fibular osteoseptocutaneous flap graft. J Orthop Trauma 2010; 24: 745–751. [DOI] [PubMed] [Google Scholar]
- 6.Rozbruch SR, Weitzman AM, Tracey Watson J, et al . Simultaneous treatment of tibial bone and soft-tissue defects with the Ilizarov method. J Orthop Trauma 2006; 20: 197–205. [DOI] [PubMed] [Google Scholar]
- 7.Li RG, Ren GH, Tan XJ, et al. Free flap transplantation combined with skin grafting and vacuum sealing drainage for repair of circumferential or sub-circumferential soft-tissue wounds of the lower leg. Med Sci Monit 2013; 19: 510–517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Li RG, Yu B, Wang G, et al. Sequential therapy of vacuum sealing drainage and free-flap transplantation for children with extensive soft-tissue defects below the knee in the extremities. Injury 2012; 43: 822–828. [DOI] [PubMed] [Google Scholar]
- 9.Nayagam S. Safe corridors in external fixation: the lower leg (tibia, fibula, hindfoot and forefoot). Strategies Trauma Limb Reconstr 2007; 2: 105–110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ilizarov GA. Clinical application of the tension-stress effect for limb lengthening. Clin Orthop Relat Res 1990: 8–26. [PubMed] [Google Scholar]
- 11.Makhdom AM, Cartaleanu AS, Rendon JS, et al. The accordion maneuver: a noninvasive strategy for absent or delayed callus formation in cases of limb lengthening. Adv Orthop 2015; 2015: 912790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rollo G, Luceri F, Falzarano G, et al. Effectiveness of teriparatide combined with the Ilizarov technique in septic tibial non-union. Med Glas (Zenica) 2021; 18: 287–292. doi: 10.17392/1280-21. Online ahead of print [DOI] [PubMed] [Google Scholar]
- 13.Tong K, Zhong Z, Peng Y, et al. Masquelet technique versus Ilizarov bone transport for reconstruction of lower extremity bone defects following posttraumatic osteomyelitis. Injury 2017; 48: 1616–1622. [DOI] [PubMed] [Google Scholar]
- 14.Shahid M, Hussain A, Bridgeman P, et al. Clinical outcomes of the Ilizarov method after an infected tibial non union. Arch Trauma Res 2013; 2: 71–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wu Y, Yin Q, Rui Y, et al. Ilizarov technique: bone transport versus bone shortening-lengthening for tibial bone and soft-tissue defects. J Orthop Sci 2018; 23: 341–345. [DOI] [PubMed] [Google Scholar]
- 16.Tetsworth K, Paley D, Sen C, et al. Bone transport versus acute shortening for the management of infected tibial non-unions with bone defects. Injury 2017; 48: 2276–2284. [DOI] [PubMed] [Google Scholar]
- 17.Peng J, Min L, Xiang Z, et al. Ilizarov bone transport combined with antibiotic cement spacer for infected tibial nonunion. Int J Clin Exp Med 2015; 8: 10058–10065. [PMC free article] [PubMed] [Google Scholar]
- 18.Korompilias AV, Lykissas MG, Vekris MD, et al. Microsurgery for lower extremity injuries. Injury 2008; 39: S103–S108. [DOI] [PubMed] [Google Scholar]
- 19.Yazar S, Lin CH, Wei FC. One-stage reconstruction of composite bone and soft-tissue defects in traumatic lower extremities. Plast Reconstr Surg 2004; 114: 1457–1466. [DOI] [PubMed] [Google Scholar]
- 20.Bao T, Han F, Xu F, et al. Papineau technique combined with vacuum-assisted closure for open tibial fractures: clinical outcomes at five years. Int Orthop 2017; 41: 2389–2396. [DOI] [PubMed] [Google Scholar]
- 21.Pierrie SN, Hsu JR. Shortening and angulation strategies to address composite bone and soft tissue defects. J Orthop Trauma 2017; 31: S32–S35. [DOI] [PubMed] [Google Scholar]
- 22.Mehta D, Abdou S, Stranix JT, et al. Comparing radiographic progression of bone healing in Gustilo IIIB open tibia fractures treated with muscle versus fasciocutaneous flaps. J Orthop Trauma 2018; 32: 381–385. [DOI] [PubMed] [Google Scholar]
- 23.Repo JP, Barner-Rasmussen I, Roine RP, et al. Treatment of compound tibia fracture with microvascular latissimus dorsi flap and the Ilizarov technique: a cross-sectional study of long-term outcomes. J Plast Reconstr Aesthet Surg 2016; 69: 524–532. [DOI] [PubMed] [Google Scholar]
- 24.Hollenbeck ST, Woo S, Ong S, et al. The combined use of the Ilizarov method and microsurgical techniques for limb salvage. Ann Plast Surg 2009; 62: 486–491. [DOI] [PubMed] [Google Scholar]
- 25.Bisaccia M, Rinonapoli G, Meccariello L, et al. The challenges of monoaxial bone transport in orthopedics and traumatology. Ortop Traumatol Rehabil 2017; 19: 373–378. [DOI] [PubMed] [Google Scholar]
- 26.Abulaiti A, Yilihamu Y, Yasheng T, et al. The psychological impact of external fixation using the Ilizarov or Orthofix LRS method to treat tibial osteomyelitis with a bone defect. Injury 2017; 48: 2842–2846. [DOI] [PubMed] [Google Scholar]
- 27.Yilihamu Y, Keremu A, Abulaiti A, et al. Outcomes of post-traumatic tibial osteomyelitis treated with an Orthofix LRS versus an Ilizarov external fixator. Injury 2017; 48: 1636–1643. [DOI] [PubMed] [Google Scholar]
- 28.Baruah RK, Harikrishnan SV, Baruah JP. Safe corridor for fibular transfixation wire in relation to common peroneal nerve: a cadaveric analysis. J Clin Orthop Trauma 2019; 10: 432–438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wen H, Zhu S, Li C, et al. Bone transport versus acute shortening for the management of infected tibial bone defects: a meta-analysis. BMC Musculoskelet Disord 2020; 21: 80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Di Candia M, Lie K, Kumiponjera D, et al. Versatility of the anterolateral thigh free flap: the four seasons flap. Eplasty 2012; 12: e21. [PMC free article] [PubMed] [Google Scholar]
- 31.Gao-Hong R, Run-Guang L, Gui-Yong J, et al . A solution to the vessel shortage during free vascularized fibular grafting for reconstructing infected bone defects of the femur: bridging with vein transplantation. Injury 2017; 48: 486–494. [DOI] [PubMed] [Google Scholar]
- 32.Li Z, Yu A, Qi B, et al. Flow-through free fibula osteocutaneous flap in reconstruction of tibial bone, soft tissue, and main artery segmental defects. Ann Plast Surg 2017; 79: 174–179. [DOI] [PubMed] [Google Scholar]
- 33.Kim JT, Kim CY, Kim YH. T-anastomosis in microsurgical free flap reconstruction: an overview of clinical applications. J Plast Reconstr Aesthet Surg 2008; 61: 1157–1163. [DOI] [PubMed] [Google Scholar]
- 34.Yin P, Ji Q, Li T, et al . A systematic review and meta-analysis of Ilizarov methods in the treatment of infected nonunion of tibia and femur. PLoS One 2015; 10: e0141973. [DOI] [PMC free article] [PubMed] [Google Scholar]