Abstract
The Veterans Health Administration (VHA) is implementing a Whole Health System (WHS) of care that empowers and equips Veterans to take charge of their health and well-being and live their lives to the fullest, and increasingly leaders recognize the need and value in implementing a similar approach to support the health and well-being of employees. The purpose of this paper is to do the following: 1) provide an overview of the WHS of care in VHA and applicability in addressing employee resiliency; 2) provide a brief history of employee well-being efforts in VHA to date; 3) share new priorities from VHA leadership as they relate to Employee Whole Health strategy and implementation; and 4) provide a summary of the impacts of WHS of care delivery on employees. The WHS of care utilizes all therapeutic, evidence-based approaches to support self-care goals and personal health planning. Extending these approaches to employees builds upon 10 years of foundational work supporting employee health and well-being in VHA. In 2017, one facility in each of the 18 Veterans Integrated Service Networks (VISNs) in VHA was selected to participate in piloting the WHS of care with subsequent evaluation by VA’s Center for Evaluating Patient-Centered Care (EPCC). Early outcomes, from an employee perspective, suggest involvement in the delivery of the WHS of care and personal use of the whole health approach have a meaningful impact on the well-being of employees and how they experience the workplace. During the COVID-19 pandemic, VHA has continued to support employees through virtual resources to support well-being and resiliency. VHA's shift to this patient-centered model is supporting not only Veteran care but also employee health and well-being at a time when increased support is needed.
Keywords: Whole Health System, implementation and dissemination, Employee Health and Wellbeing, Veterans Health Administration
Introduction
As an organization that embraces innovation, the Veterans Health Administration (VHA) has engaged with cultural transformation to become truly patient-centered for many years. In 2010, VHA stood up the Office of Patient-Centered Care and Cultural Transformation (OPCC&CT) to help bring this philosophy to the employees and Veterans utilizing the VA system. VHA OPCC&CT’s current mission is to transform health care delivery into a Whole Health System (WHS) of care to support the health and well-being of Veterans, VA employees, and the nation with a vision to be a global leader in patient-centered whole health to support all people in achieving their full potential for health and well-being. Efforts were focused on driving innovation in the diverse medical centers throughout the country and learning from promising practices in the field. These practices informed the development of the WHS of care in 2015 leading to pilot implementation efforts at several design sites in 2015–2016 and full-scale deployment at 18 flagship sites in each Veterans Integrated Service Network (VISN) across the country in 2017. An additional 37 sites joined in 2019-2020 to accelerate the implementation of core components of the WHS of care. One of the priorities of OPCC&CT has been to bring the experience of whole health to employees to further support the large-scale transformation of the health care system.
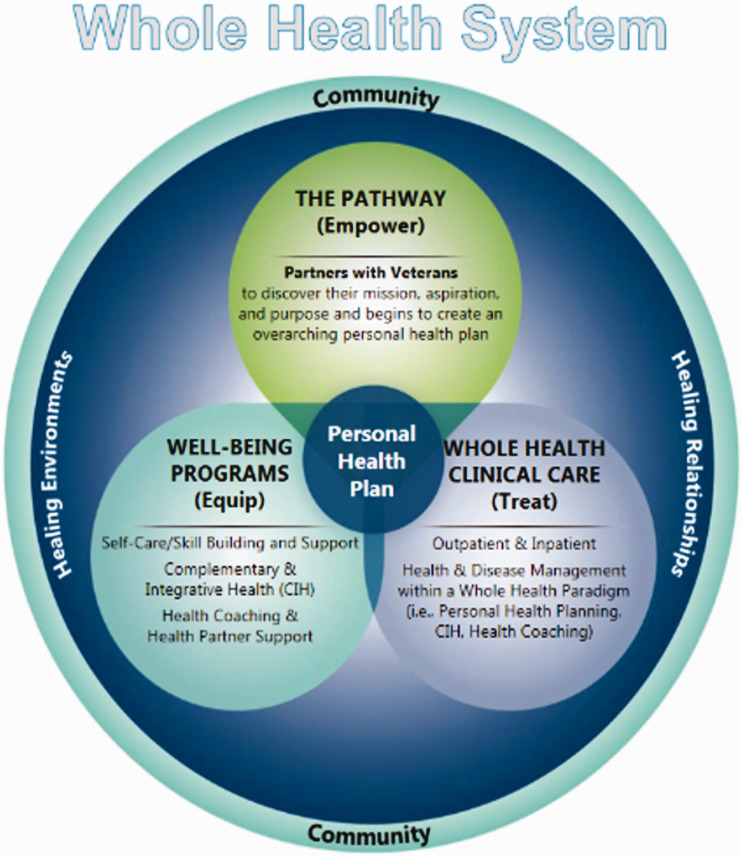
Whole Health System of Care
The WHS of Care (Figure 1) is an approach to health care that empowers and equips people to take charge of their health and well-being and live their life to the fullest (https://www.va.gov/wholehealth/). It is a model that creates space for individual self-awareness as well as self-exploration of core values and purpose in support of their health and well-being goals in life. It integrates all therapeutic approaches informed by evidence and is provided by a diverse team of clinicians, well-being instructors, whole health coaches, Veteran partners, and complementary and integrative health (CIH) providers. During clinical visits, providers help Veterans feel more empowered and equipped to care for themselves by asking about values and purpose and creating shared goals through open communication.1 VHA’s OPCC&CT has committed to bringing the whole health approach to all VHA employees as well because they will be better able to deliver more personalized, whole health care to Veterans when they understand the impact of this model on their health and well-being. While utilization of whole health approaches with employees doesn’t involve clinical care treatment, many features of the model apply equally as well to employees. For example, the pathway to empowerment provides an opportunity for individual self-exploration of health and well-being goals, and well-being programming allows employees to grow skills to accomplish those goals essential to supporting their whole health (Figure 1). A variety of employees and volunteers offer education and self-care well-being classes to VHA employees, including clinical and non-clinical staff who have the proper scope of practice and training. Given these approaches are not rooted in disease-based care, there is no sharing of medical information during these sessions, treatment of specific conditions, nor documentation in the same medical record as patients. This ensures privacy and confidentiality for employees who volunteer to participate in whole health and well-being activities. This opportunity has become critically important during the COVID pandemic as employees seek ways to feel more resilient in the face of adversity, challenges, and increased stressors.
Figure 1.
Whole Health System of Care.
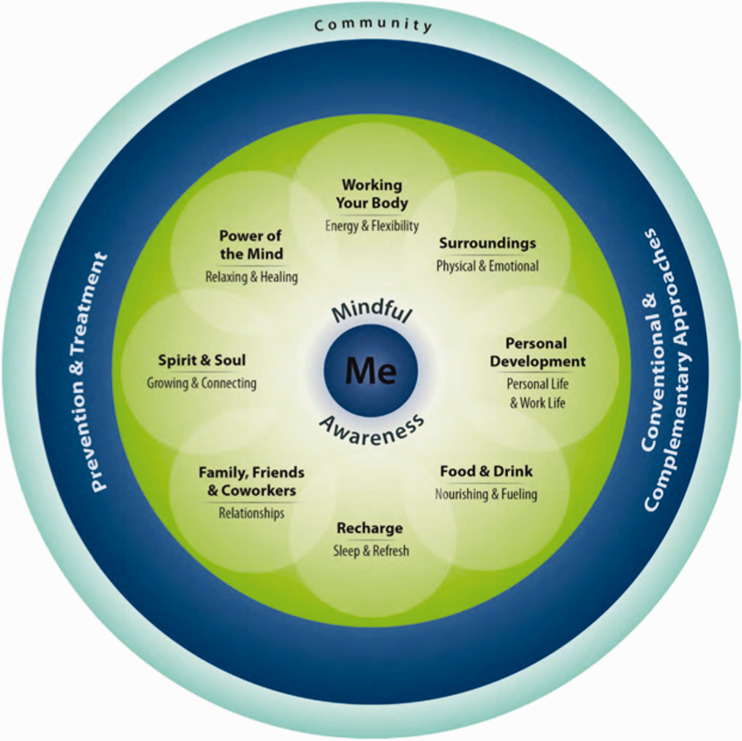
A key facet of the whole health approach is the ability to increase self-awareness through mindful presence and identify where there are opportunities to change behaviors or circumstances to overcome challenges. Employees can do this by reviewing their personal health inventory through the web-based “Livewholehealth” application available for download, online fillable PDFs available through the VHA’s whole health internet site (https://www.va.gov/WHOLEHEALTH/phi.asp), or paper versions. The addition of the web-based application increases access to this valuable tool and connects the user with virtual educational and experiential resources to support any goals they choose for their well-being. Through this process, they can reflect on each of the components of health and well-being (Figure 2). This application of the WHS of care to employees in VHA is called Employee Whole Health (EWH) and is an important strategic focus for OPCC&CT.
Figure 2.
Components of Proactive Health and Well-Being.
History of Employee Well-Being Efforts in VHA
EWH aims to build upon early successes from both national efforts around employee well-being as well as the implementation of the WHS of care for Veterans and employees. Since 2008, VHA has steadily worked on growing the employee well-being community and providing increased programming to support the health and well-being of employees. Starting with a successful 3-year pilot program in 11 Midwest hospitals in 2008, program administrators worked to expand efforts system-wide by offering a variety of educational opportunities and resources to the employees at all VA medical centers.2 As a result of these efforts, there have been improvements in the health of employees at an individual level. As an example, the median wellness score for employees participating in the initial pilot increased significantly overall. Efforts to support employee well-being have resulted in improvements at the organizational level as well. Specifically, overall rates of physical inactivity have declined nationally3 and a comprehensive approach to tobacco use cessation for employees including both national policy and practice was deployed.4 Finally, prior research indicated that local investment in resources to support employee health and well-being programming was associated with several important organizational health metrics including higher job satisfaction2 and higher levels of leadership and employee engagement.5
The past 10 years of foundational work supporting employee health and well-being in VA have been very important in laying the groundwork for the future. Early efforts in employee well-being were largely focused on key areas of primary prevention, namely increased opportunities for physical activity, nutrition/weight management classes, stress management interventions, and tobacco use cessation. Future efforts will be aligned with the WHS of care and all of the components of proactive health and well-being (Figures 1 and 2) to emphasize the connection to meaning and purpose and empower employees to reflect on the choices they have in their lives, both personally and professionally. The “empowerment” element of the model is critical to personal engagement and activation around self-care, health, and well-being.
Future Directions for Employee Whole Health
The EWH national strategy now centers around 3 focus areas: 1. Collaboration and integration to ensure a culture of well-being and resiliency; 2. Provision of the experience of whole health to employees; and 3. Evaluation of the impact of employee whole health efforts.
Because there are many program offices and services within the organization that impact employee engagement and experience, EWH efforts strive to increase collaboration and integration with existing education and practice efforts to ensure spread. For example, there has been a concerted effort to provide CIH well-being and self-care opportunities to employees including the development of a “Self-Care Resources for Your Whole Health” section of the VA Insider website.6 This represents a collaborative effort of the VHA’s Organizational Health Council which includes members of the National Center for Organizational Development, Office of Mental Health and Suicide Prevention, Office of Care Management and Social Work Services, Veteran Experience Office, Chaplain Services, and OPCC&CT, to name a few. Employees can explore self-care activities through brief relaxation and mindfulness exercises, find hand-outs on spiritual health and tools for resilience, or participate in a yoga or Tai Chi class by video. To date, there have been more than 60,000-page views to this site and an investment by every VISN to prioritize advertisement of virtual well-being and self-care options to employees.
At the medical center level, examples of collaboration include partnering with the High-Reliability Organization (HRO) teams, Employee Assistance Program (EAP) providers, Patient Experience Officers, incorporating whole health education into new employee orientation and supervisor training, and utilizing the All Employee Survey (AES), VA’s annual organizational census survey, results to guide process improvements in the workplace. System redesign efforts are encouraged to bring the experience of whole health into the workflow and involve employees in process improvements to support not only their well-being but also the delivery of highly reliable, safe, and personalized care. Examples include incorporating self-care strategies into team meetings, huddles, and rounds, providing dial-in options for ten to fifteen-minute mindfulness or meditation sessions, virtual breaks for movement such as yoga and Tai Chi, and offering individual or group health and well-being coaching to interested staff. Additionally, VHA OPCC&CT Field Implementation Team consultants help facilities deliver an experiential offering, Whole Health for You and Me, to provide space for a deeper understanding of the whole health model and self-exploration of the components of health and well-being. This allows for empowerment and activation around what matters most to the individual. As of February 2021, 55% of VHA facilities have made this course available to their employees. Efforts at the local, VISN, and national levels to support employee resilience and well-being have increased dramatically over recent months with hundreds of virtual self-care offerings now available weekly.
Finally, national evaluation efforts in fiscal year 2021 will be focused on the analysis of AES results, an assessment of existing infrastructure and resources at each VHA medical facility, focus groups at specific whole health implementation sites to understand the facilitators and barriers to employee whole health implementation, and employee-reported outcomes on stress and resiliency at select pilot sites implementing innovative employee whole health practices.
Outcomes for Employee Whole Health implementation are measured in several ways including both qualitative and quantitative methods. One primary method to collect data is through the AES, the annual organizational census survey in VA. The AES is administered to the entire VHA employee population with an average response rate of 60% annually. Since 2018, questions on whole health have been added to the AES assessing involvement in the provision of whole health services for Veterans, and more recently, questions have been added to assess personal use of whole health. A facility-specific report summarizing this data is provided to whole health points of contact at each VA medical center for their use in future planning. In addition, robust program evaluations assessing pre and post-data are conducted at pilot sites implementing innovative employee whole health practices. Typically, these program evaluations employ a mixed-methods approach with a collection of both qualitative and quantitative data to assess overall impact.
To formalize all of these efforts, VHA leaders have developed a national set of strategic priorities to move the field forward. These include the following: 1) Employee Whole Health is an important part of VHA’s overall modernization efforts 2) VA national leadership is actively encouraging VHA facilities to establish multi-disciplinary Employee Whole Health committees and coordinators to support a culture of well-being and resiliency for the Whole Health transformation; and 3) Finally, VISNs and VA medical centers use an implementation guide called the Designation Framework (DF) and accompanying Self-Assessment Tool (SAT) to support and assess progress towards WHS of care transformation. Employee Whole Health is one of the seven key domains in the framework and there are several milestones for VISNs and VA medical centers to meet to progress in transformational goals. Examples of such milestones include establishing an EWH coordinator and committee, conducting a needs assessment, inclusion of whole health principles into new employee orientation, providing access to self-care education and resources at multiple locations and times, and having an evaluation mechanism in place for employee-facing programs.
Impact of Whole Health System on Employees
In October of 2017, VHA’s OPCC&CT received funding to implement the WHS of care as part of a 3-year pilot. One facility in each of the 18 VISNs was selected to participate in piloting the WHS and subsequent evaluation for research purposes was conducted by the Center for Evaluating Patient-Centered Care (EPCC) in VA.
As WHS implementation represents whole system change, the impact on employees was included as a critical aspect for the EPCC pilot evaluation. By including a key question on VA’s AES survey, EPCC was able to assess employee engagement in WHS activities. They found that employees who had greater involvement in delivering whole health services to Veterans also reported higher rates of identifying their facility as the best place to work, lower turnover, lower burnout, and greater motivation in their jobs. Moreover, they found a positive association between greater employee involvement and overall hospital system performance, as captured by standardized metrics and surveys of patient experiences.7 These trends have continued. Recent data from the 2020 AES indicates consistent patterns when comparing data from 2019 to 2020, and favorable ratings (i.e., best place to work, lower turnover, lower burnout, and greater motivation in their job) increased slightly between 2019 and 2020 among all groups.
So, whereas often large system transformations may have a negative effect on employees, engagement in WHS transformation had a positive impact, perhaps due to an alignment of whole health with health care provider values to provide individualized, patient-centered care.
An additional question in 2020 was added to understand how personal behavior changes after involvement in WHS activities may have impacted job attitudes. Employees who reported changing personal behaviors and self-care activities after involvement in WHS activities also reported more favorable workplace ratings, similar to the associations above. While this does not imply causation, it is a promising finding to warrant further trending and evaluation.
The COVID-19 pandemic has highlighted the need to ensure all VA employees, roughly 400,000 in number, harness the power of self-care and optimize their well-being to cope effectively with present stressors and build resiliency in the face of the pandemic.8 A promising model to do this, the WHS of care, already exists in VHA. Simply being involved in the delivery of the WHS of care appears to have a meaningful impact on the well-being of employees and how they experience the workplace. Prior focus group work with employees also illustrates that employees in VHA know that they must feel well themselves to be able to provide the best care to Veterans.9
Conclusion
VHA is deeply committed to serving Veterans and supporting the employees who deliver care on a day-to-day basis. This includes establishing an organizational culture that prioritizes employee whole health and allows for self-reflection, empowerment, and feeling equipped to live life in support of an individual’s meaning and purpose.
Early outcomes suggest improved job attitudes for employees who are using whole health for themselves and practicing whole health with their patients. In order to meet VHA’s mission to honor America's Veterans by providing exceptional health care that improves their health and well-being, there will be a continued emphasis on delivering the WHS of care to VHA employees through the Employee Whole Health implementation efforts.
We’re here to serve the Vets but I think employees have to feel like they’re supported and heard, and you know, they have to feel well enough to wait on patients. You have to feel good yourself to help somebody else feel well. To improve their health… It’s like the airplane, you put the oxygen on yourself before you attend to your children with oxygen, you know, you’ve gotta take care of yourself so you can help others.” [Supervisor, VA Boston HCS].
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Kavitha P Reddy https://orcid.org/0000-0003-1499-1012
References
- 1.Bokhour BG, Haun JN, Hyde J, Charns M, Kligler B. Transforming the Veterans affairs to a whole health system of care. Medical Care. 2020; 58(4):295–300. [DOI] [PubMed] [Google Scholar]
- 2.Schult TM, Galway AM, Awosika ER, Schmunk SK, Hodgson MJ. Management support, worksite culture, and local resources for healthier employees: the VA experience. J Occup Environ Med. 2013; 55;310–317. [DOI] [PubMed] [Google Scholar]
- 3.Schult TM, Schmunk SK, Awosika ER. Decreasing physical inactivity in the Veterans Health Administration employee population. J Occup Environ Med. 2016; 58:1217–1222. [DOI] [PubMed] [Google Scholar]
- 4.Schult TM, Kelly Q, Schmunk SK, Awosika ER. From policy to practice: tobacco use cessation for employees in the Veterans Health Administration. J Occup Environ Med. 2016; 58:525–531. [DOI] [PubMed] [Google Scholar]
- 5.Mohr DC, Schult T, Eaton JL, Awosika E, McPhaul KM. COHN-S integrated employee occupational health and organizational-level registered nurse outcomes, J Occup Environ Med. 2016; 58(5):466–470. [DOI] [PubMed] [Google Scholar]
- 6.Employee Whole Health – Self-Care Resources for Your Whole Health. https://www.va.gov/WHOLEHEALTH/professional-resources/EWH-resources.asp. Accessed May 21, 2021.
- 7.Bokhour BG, Hyde J, Zeliadt S, Mohr D. Whole Health System evaluation of care progress report. https://www.va.gov/WHOLEHEALTH/docs/EPCCWholeHealthSystemof CareEvaluation-2020-02-18FINAL_508.pdf. Accessed May 21, 2021.
- 8.Dzau VJ, Kirch D, Nasca T. Preventing a parallel pandemic: A national strategy to protect clinicians’ well-being. N Engl J Med. 2020; 383(6):513–515. [DOI] [PubMed] [Google Scholar]
- 9.Schult TM, Nagler EM, Sorensen G, et al. Employee perceptions of safety, health, and well-being: focus group findings from one Veterans Affairs medical center. J Occup Environ Med. 2018; 60:e582–e588. [DOI] [PubMed] [Google Scholar]