Abstract
Coronavirus disease 2019 (COVID-19) transmits from person to person mainly through respiratory droplets and coughing. Infection severity ranges from asymptomatic and mild infection to those with moderate and severe symptoms which may lead to multiple organ failure and mortality. Infection severity largely depends on individual's immune response, age and co-morbidities. Present study categorized COVID-19 infected patients based on their infection severity and linked COVID-19 severity with age, gender and ABO blood group types. Clinical details of 383 COVID-19 patients were collected from Rajiv Gandhi Super Specialty hospital (RGSSH), India; divided into three groups; mild, moderate and severe patients, based on their symptoms. Present analysis revealed that age plays major role in infection severity, as the symptoms are more severe in patients above 45 years. Infection rate was higher in males compared to females. Most patients with A(+ve) and B(+ve) blood group were severely affected compared to those of blood group type O(+ve) and AB(+ve). O(+ve) blood group was least represented in severe patients. Present findings could be helpful in generating awareness amongst the population regarding susceptibility towards the COVID-19 infection. This supportive information would help clinicians and health workers to propose new strategies and tactical solution against COVID-19 infection.
Keywords: SARS-CoV-2, COVID-19, Blood group, Age, Gender, Indian population
1. Introduction
In December 2019, a novel strain of Coronavirus named as Severe acute respiratory syndrome coronavirus (SARS-CoV-2), was identified in Wuhan, Hubei Province of China, which infected a huge number of patients with severe pneumonia. The identified virus was from the same family of coronavirus as SARS-CoV and Middle East respiratory syndrome coronavirus (MERS-CoV) [1]. This virus spread very rapidly across China and very affected the entire worldwide population [2]. Later on it was declared a global pandemic and WHO officially announced it Public Health Emergency of International Concern on January 30, 2020 and named it as Coronavirus disease 2019 (COVID-19) [3]. Presence of this virus was manifested by broad range of symptoms like fever, cough, dyspnea, myalgia, tiredness, sore throat, loss of taste and/or smell etc. as well as asymptomatic to severe illness and death [4]. The clinical diagnosis of COVID-19 is being performed on the symptoms manifestation of the disease. On the other hand, molecular diagnostics of the COVID-19 viral genome is confirmed by RT –PCR along with chest X-ray or CT scan, and serological blood tests [5]. Literature survey showed that various researches in past have found an association between ABO blood groups and viral infections, and reported a profound linkage between the two. There are various clinical reports which reflect that ABO blood group system is intensely associated with numerous viral infections like Rotavirus, Noroviruses (NoVs), Dengue virus, Norwalk virus and Hepatitis B virus [6,7,8,9]. With the knowledge of association of specific blood type with viral infection there are chances to comprehend the propensity of susceptibility of the individual having specific blood types with viral infection. After SARS- CoV-2 infection, in a short span of time, a few clinical reports are available which are depicting the possible association between blood group types [10,11,12]. However, reports are heterogeneous in nature and are unable to state the specific blood group type association with the severity risk of COVID-19 infection. In the present clinical study, COVID-19 patients are categorized on the basis of their blood group to understand the link between ABO blood group and severity of infection (mild, moderate and severe COVID-19 patients) along with other physiological parameters.
2. Methods
2.1. Data sources
The medical records of COVID-19 patients in Indian population were analyzed by the research team of the Defence Institute of Physiology and Allied Science (DIPAS), DRDO, Delhi. Data on clinical characteristics was obtained from data collection forms of electronic medical records. The data was reviewed by a team of trained clinicians and researchers.
2.2. Study design
Under this clinical study, medical records of 383 patients with COVID-19 were analyzed. All the patients were diagnosed positive for COVID-19 infection after RT-PCR test between July 2020 to October 2020 and reported to Rajiv Gandhi Super Specialty Hospital (RGSSH), Delhi. The study subjects were divided into three groups based on the severity of infection as severe, moderate and mild infected patients. The clinical records data was segregated based on gender wise and age wise distribution of all patients. Also, the records of patients were checked for their blood group type, A, B, O and AB, as well as Rh (D) positive and Rh (D) negative.
The study was approved by the Ethical Committee of ICMR, India. Written informed consent was obtained from all lab confirmed COVID-19 patients at RGSSH, Delhi. All experimental protocols were conducted according to the Strengthening of the Reporting of Observational Studies in Epidemiology guidelines.
2.3. Statistical analysis
Statistical computations were performed using GraphPad Prism 5. Data were analyzed with the χ2 test and Fisher's exact test. ORs with 95% CIs for specific blood types in COVID-19 patients, were assessed with logistic regression models. P < 0.05 was considered statistically significant.
3. Results
During the study period, 383 COVID-19 infected patients who visited RGSSH, Delhi were included in the study. Their clinical records were analyzed for COVID-19 infected patients with severe, moderate and mild type of infection. The analysis was performed based on gender, age and the ABO blood group distribution.
3.1. Relationship of COVID-19 infection with gender
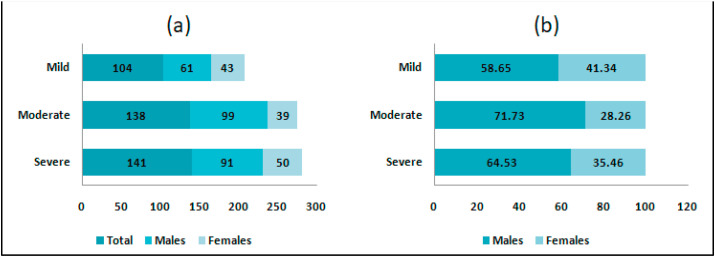
Out of 383 COVID-19 patients, 141 (36.81%) were found to be severely infected, 138 (36.03%) were moderately infected and 104 (27.15%) had mild infection (Fig. 1 a). Twenty four patients (6.2%) under severe category could not recover from infection and deceased (non availability of blood group information of these cases). Amongst the study group, the percentage of COVID-19 infected males was 65.53% compared to females with 34.64%. The infection rate was found to be higher in males in all three sub groups viz. severe patients had 64.53%, moderate group with 71.73% and mild group with 58.65% (Fig. 1b) as compared to 35.46%, 28.26% and 41.34% of female patients respectively.
Fig. 1.
(a). Number of COVID-19 patients (Total, Males and Females) in Severe, Moderate and Mild category (b) % Distribution of COVID-19 patients (Males and Females) in Severe, Moderate and Mild category.
3.2. Relationship of COVID-19 infection with age
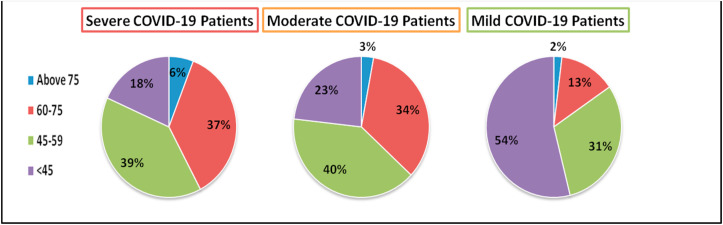
The study population was divided into four age groups, those above 75 years, between 60 and 75 years, 45–59 years and less than 45 years. Interestingly, in severe COVID-19 patients group, 82% of the subjects were above the age of 45, whereas in moderate group, 77% of the subjects were above 45 years and in mild group, only 46% of the patients were above the age of 45 years (Fig. 2 ). This implies that the infection was milder in younger age group. We further divided the COVID-19 patients in each age group into males and females and found that in all age groups, percentage occurrence of infected males was higher than that of infected females (Fig. 3 ).
Fig. 2.
Age wise distribution (in percentage), of COVID-19 patients in severe, moderate and mild category.
Fig. 3.
Age wise distribution (in percentage), of COVID-19 patients in severe, moderate and mild category. The percentage of individuals in each age group has been further divided into males and females.
3.3. Relationship between the ABO blood group distribution and severities of infection (severe, moderate and mild) in COVID-19 patients
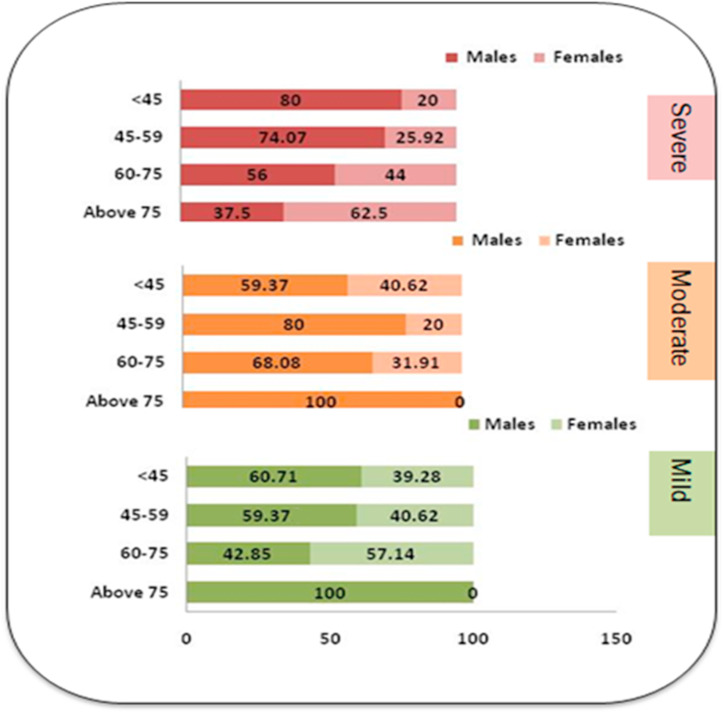
Distribution pattern of ABO and Rh blood group systems show variations in different populations. In the present study population of 383 COVID-19 patients, we could obtain ABO blood group information for 29 severely infected patients, 114 moderately infected patients and 84 patients with mild infection. A (+ve) and B (+ve) blood group was predominant in severe patients (34.48%) as compared to O (+ve) (17.24%) (Fig. 4 a).
Fig. 4.
(a) Frequency distribution of ABO blood group types of COVID-19 patients in Severe, Moderate and Mild category (b) Gender wise blood group type distribution in COVID-19 patients.
On one hand the frequency percentage of A(+ve) blood group declined in patients with moderate and mild infection (26.31% and 19.04% respectively), and on the other hand frequency of O (+ve) blood group constantly increased from severe (17.24%), moderate (26.31%) to mild patients (30.95%). Interestingly, AB (+ve) blood group also showed a similar trend as that of O (+ve) blood group, with constant increase in frequency from severe to mild group. Severe COVID-19 patient's category had 3.44% of AB (+ve) patients whereas this percentage increased in moderate (9.64%) and mild patients group (13.09%) (Fig. 4a). The percentage occurrence of Rh(D) –ve type blood group was very less in all three subtypes of patient groups.
ABO blood group type distribution in all three types of infected patients was further divided into males and females (Fig. 4b). A(+ve) blood group in males had highest frequency (%) of occurrence in severe and moderate category (70%) as compared to 30% females in severe and moderate group had A(+ve) blood group. B(+ve) blood group showed equal frequency occurrence in all three subgroups in males as well as females. Frequency of O(+ve) blood group was highest in moderately (73.33%) and mildly infected males (53.84%). In females, AB(+ve) showed highest prevalence in moderate group (45.45%).
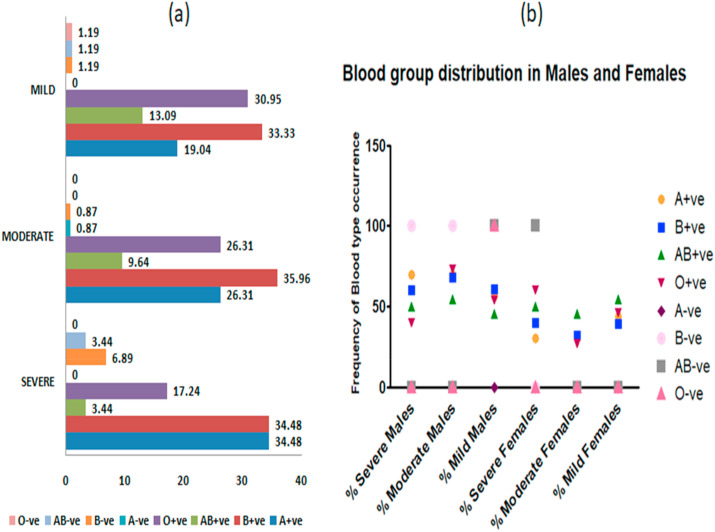
3.4. ABO blood group and Rh(D) frequency distribution in study population in comparison to frequency distribution in Indian population
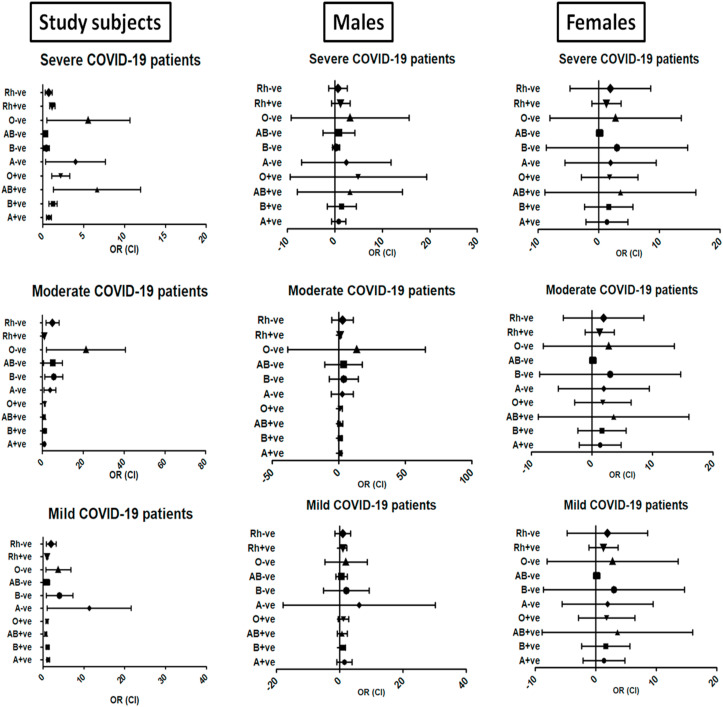
The presence of ABO type of blood group as well as Rh(D) antigen in the study population was compared with their prevalence in general Indian population. We selected four different epidemiological studies [[13], [14], [15], [16]] conducted in different years. The frequency occurrence of different ABO types of blood groups and frequency of Rh(D) factor in these studies was noted (Table 1 ). Their average was calculated and used to compare the prevalence of blood group types in our study (Table 2 ). Odds ratio (OR) and confidence interval (CI) was calculated using MedCalc (statistical software) and forest plots were generated (using GraphPad Prism 5) (Fig. 5 ). The CI in the plots, particularly in females, is wider because of lower sample size.
Table 1.
Distribution of ABO and Rh(D) blood groups expressed in percentage in Indian population.
| Blood Group types | Patidar et al., 2020 | Shani et al. 2018 | Agrawal et al., 2014 | Das et al. 2001 |
|---|---|---|---|---|
| A (%) | 23.16 | 22.91 | 22.88 | 18.85 |
| B (%) | 34.1 | 38.5 | 32.26 | 32.69 |
| O (%) | 34.56 | 30.12 | 37.12 | 38.75 |
| AB (%) | 8.18 | 8.45 | 7.74 | 5.27 |
| Rh(D) +ve (%) | 94.13 | 95.14 | 94.61 | 94.53 |
| Rh(D) -ve (%) | 5.87 | 4.85 | 5.39 | 5.47 |
Table 2.
Distribution of ABO and Rh(D) blood groups expressed in our study population in comparison to prevalence in general population in India.
| Blood Group types |
Average Prevalence in General population |
Prevalence in COVID-19 infected patients |
||
|---|---|---|---|---|
| Severe | Moderate | Mild | ||
| A (%) | 21.95 | 34.48 | 27.18 | 19.04 |
| B (%) | 34.38 | 41.37 | 36.83 | 34.52 |
| O (%) | 35.13 | 17.24 | 26.31 | 32.14 |
| AB (%) | 7.41 | 6.88 | 9.64 | 14.28 |
| Rh(D) +ve (%) | 94.60 | 89.65 | 98.24 | 96.42 |
| Rh(D) -ve (%) | 5.395 | 10.33 | 1.72 | 3.57 |
Fig. 5.
Forest plot of ABO type blood group distribution in study subjects, males and females in severe, moderate and mild category. Each line in the graph represents a unique data with result plotted as a dot and the 95% confidence interval of result displayed as the line. The vertical line represents the line of null effect (no association) between the different data.
According to published epidemiological data, the prevalence of O type blood group is highest in Indian population. However, we observed a decreased frequency of occurrence in Severe COVID-19 patients. Also, severe patients had highest frequency occurrence of A(+ve) and B(+ve) blood group. There was no notable change in frequency distribution of Rh(D) +ve type amongst the study subgroups. Also, very few patients from our study group had Rh(D) –ve blood group.
4. Discussion
The study is a relative comparison of severity of COVID-19 infection with gender, age and ABO blood group type in males and females Indian population. A cohort of 383 COVID-19 patients, who tested positive for novel coronavirus infection (COVID-19), reported to RGSSH were included in the present study. It was observed that Indian male population is more affected with COVID-19 in comparison to female population. In concurrence with western clinical reports, Indian elderly population is more severely affected than younger population, with mild COVID-19 infection. Clinical data of patients also indicated that severe COVID-19 infection occurred more in A(+ve) and B(+ve) blood group individuals, than O(+ve) blood group individuals who showed mild infection symptoms.
Since the beginning of COVID-19 pandemic, number of studies have been carried out to understand the association of blood group types and viral infection [17]. In a multi-institutional study, 1289 COVID-19 patients across five hospitals were identified from March 6th to April 16th, 2020. They reported that blood group A had no correlation with positive testing whereas blood type B and AB were associated with higher odds of testing positive for the disease, also O blood group was associated with a lower risk of testing positive [18]. Gullion P et al., observed that blood group O was less frequent in severe COVID -19 patients who required long hospitalization (P < 0.01). Blood group A was more frequent in patients with severe COVID-19 infections compared to the normal population in a cohort of 265 COVID-19 patients [19]. In another study of 186 COVID-19 patients, age, sex, blood groups, comorbidities, need for intubation and intensive care unit follow up and mortalities of the patients were analyzed retrospectively along with 1881 healthy individuals, who reported to the Hacettepe University Blood Bank as healthy subjects. This study also mentioned that blood group A might have a role in increased susceptibility to the COVID-19 infection; and the blood group O might be somewhat protective in nature [10]. All findings profoundly are in resemblance to our present observations in Indian population having COVID -19 infection.
We further categorized patients in three groups such as severe, moderate and mild patients to understand the link between level of infection and prevalence of blood group type in Indian population having COVID-19 infection. We concluded that patients having A(+ve) and B(+ve) blood groups are predominant in severe category with respect to O(+ve) and AB(+ve). In Indian population, it is evident that there is prevalence of O type blood group. There is almost an equal distribution of Rh(D) +ve type in severe, moderate and mild categories. Due to less prevalence of Rh(D) –ve blood group among Indian population, in the present study there were only eight patients, who were almost equally distributed in severe, moderate and mild categories. Limitation of number of patients indicated that there is no significant association of prevalent Rh(D) –ve blood group to COVID-19 infection.
In Indian context, few epidemiological reports are available which show possible role of ABO blood group system with COVID-19 infection. These reports have their own limitations as they are derived from online databases/reports, retrospective observational studies and not from actual COVID-19 patient sample clinical information [[20], [21], [22]]. Present clinical study outcome is strongly supported by earlier reports which showed that ABO blood group is associated with angiotensin converting enzyme (ACE) activity and ACE inhibitor-induced cough among Chinese patients with hypertension as comorbidity. The previous studies observed strong association of GATC haplotype of the ABO gene with non-O blood type patients related with ACE activity [23,24]. This depicts that O blood group individuals have lower expression level of ACE which may be beneficial in present pandemic. In the same line of study, it has also been reported that O-blood group individuals have higher level of interleukin 6 (IL-6), which could be protective against various other diseases like cancer and myocardial infraction. This marginal increase in proinflammatory cytokine may triggers the production of acute phase protein like C-reactive protein, compared to other blood group individuals [25,26]
Recently published GWAS study [25] also showed that O-blood group individuals have increased level of IL-6 than other blood groups which may be the reason of overall less cases of O blood group individual infection rate cumulatively. On the other side, it has been also reported that A blood group individuals have propensity for developing cardiovascular diseases [27]. The A antigen might protect P-selectin and intercellular cell adhesion molecule 1 (ICAM1) from enzymatic cleavage by promoting stronger and longer binding of leukocytes to them on the vascular wall; more adhesion molecules attached to the endothelial cells would on one hand increase adhesion and inflammation but on the other hand decrease circulation [28,29]. These collectively predispose type A carriers to a higher likelihood of developing cardiovascular diseases and aggregate disease situations once these individuals are exposed to redox stresses such as in the case of virus infection. The relationship between ABO blood groups and cardiovascular diseases is well established [27]. It is known that thrombotic risks decrease significantly in blood group O compared to the non-O blood groups [30]. Therefore, O blood group individual have low probability to develop cardiovascular diseases and severe COVID-19. In comparison A blood group individual, especially those already having been diagnosed with cardiovascular diseases in particular hypertension, are more likely to develop severe COVID-19 once infected. These individuals need to be quarantined and protected from SARS-CoV-2 infection or kept under special medical care to prevent health deterioration and severe disease progression.
A few evidences suggest that men also have higher levels of the ACE2, a protein through which virus attaches to enter and infect human cells. ACE2 is found not only in lungs, but also the heart, kidneys and tissues lining blood vessels, and in the testes, which partially explain why men are more vulnerable to severe disease than females. This argument may justify higher number of COVID 19 cases in males [31].
In the current study, propensity of COVID-19 infection was more in males in comparison to females. Number of male patients were more in severe, moderate and mild categories compared to females. It depicts that in Indian population male individuals are at higher risk for COVID-19 infection. To get more clarity, all male and female patients were further divided into four age groups i.e. <75yrs, 60–75yrs, 45–59yrs, >45yrs. Collectively most of the severe patients were above 45yrs of age in comparison to mild and moderate infection which states that young individuals show milder infection. Our results also demonstrate that under severe category, males majorly lie above 45yrs of age group whereas females are predominantly above 75yrs of age. Although there is a little variation in mild and moderate categories. Along with this, it has been also observed that amongst the patients who mainly belonging to B (+ve) blood group, 35.17% were males and 33.73% were females. These observations were further analyzed on the gender basis and we found that male patients have highest frequency of A(+ve) blood group in severe and moderate category. There is approximately equal frequency of occurrence of B(+ve) blood group in severe, moderate and mild category in both male and female patients. One of the interesting facts that we observed was that frequency occurrence of O (+ve) blood group very noticeably increased from severe, moderate to mild COVID 19 infection, which strongly supports that O (+ve) blood group is protective in nature.
There are a few limitations in the present clinical study. First, sample size of COVID-19 patients is not very large. Second, we were not able to include healthy subjects who come for their routine checkup to hospital, due to non availability of data. Third, there is a possibility that other pre-existing diseases may have contributed in COVID-19 infection severity but we didn't have comorbidities information of enrolled COVID-19 patients.
Clinical findings of present study concluded that the blood group O might be protective while the blood group A and B might have increased susceptibility to the COVID-19 infection. There is an urgent need for following stringent measures for non O blood group individuals compared to O blood group individuals in current pandemic on the basis of SARS-CoV-2 infection susceptibility. As per research reports available, we found that this is the first clinical study of COVID-19 infected patients which is showing a correlation with ABO blood groups conducted in Indian population. These kinds of clinical findings necessitate scope for large multicentric molecular studies which will give more insight towards the association of blood groups and the COVID-19 infection. All these findings indicate that ABO blood group system is very well allied with the SARS-CoV-2 susceptibility in Indian population as well. However, further research is needed with more clinical samples to corroborate these findings which may delineate the underlying biological mechanism behind association of COVID-19 infection and blood group system and would be helpful for clinicians to define the countermeasure based on individual ABO blood group against this deadly viral infection.
Author statement
Iti Garg: Conceptualization, Writing- Original draft preparation, Reviewing and Editing, Formal analysis. Swati Srivastava: Conceptualization, Writing- Original draft preparation, Reviewing and Editing, Formal analysis. Vikas Dogra: Methodology, Resources, Investigation, Data curation. Mona Bargotya: Methodology, Resources, Investigation, Data curation. Sonali Bhattar: Methodology, Resources, Investigation, Data curation. Utkarsh Gupta: Methodology, Resources, Investigation, Data curation. Shruti Jain: Methodology, Resources, Investigation, Data curation. Javid Hussain: Methodology, Resources, Investigation, Data curation. Anju A. Hembrom: Data Curation, Visualization, Software, Validation. Nilanjana Ghosh: Data Curation, Visualization, Software, Validation. Vinay Kumar: Data Curation, Visualization, Software, Validation. Bhuvnesh Kumar: Resources, Supervision, Project Administration.Rajeev Varshney: Resources, Supervision, Project Administration. Lilly Ganju: Resources, Supervision, Project Administration.
Funding
The authors have received funding for this work from DIPAS, DRDO.
Declaration of competing interest
The authors declare that there is no conflict of interest or financial disclosure related to this publication.
References
- 1.Yin Y., Wunderink R.G. MERS, SARS and other coronaviruses as causes of pneumonia. spirology (Carlton, Vic) 2018;23(2):130–137. doi: 10.1111/resp.13196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wang C., Horby P.W., Hayden F.G., Gao G.F. A novel coronavirus outbreak of global health concern. Lancet (London, England) 2020;395(10223):470–473. doi: 10.1016/S0140-6736(20)30185-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gao J., Tian Z., Breakthrough X. Yang. Chloroquine phosphate has shown apparent efficacy in treatment of COVID-19 associated pneumonia in clinical studies. Biosci. Trends. 2020;14(1):72–73. doi: 10.5582/bst.2020.01047. [DOI] [PubMed] [Google Scholar]
- 4.Lovato A., de Filippis C., Marioni G. Upper airway symptoms in coronavirus disease 2019 (COVID-19) Am. J. Otolaryngol. 2020;41(3):102474. doi: 10.1016/j.amjoto.2020.102474. [Epub] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Paranjpe I., Russak A., De Freitas J.K., Lala A., Miotto R., Vaid A., et al. Clinical characteristics of hospitalized Covid-19 patients in New York city. medRxiv. 2020 doi: 10.1101/2020.04.19.20062117. [DOI] [Google Scholar]
- 6.Kalayanarooj, Gibbons R.V., Vaughn D., Green S., Nisalak A., Jarman R.G., Mammen M.P., Perng G.C., Jr. Blood group AB is associated with increased risk for severe dengue disease in secondary infections. J. Infect. Dis. 2007;195(7):1014–1017. doi: 10.1086/512244. [DOI] [PubMed] [Google Scholar]
- 7.Hennessy E.P., Green A.D., Connor M.P., Darby R., MacDonald P. Norwalk virus infection and disease is associated with ABO histo-blood group type. J. Infect. Dis. 2003;188(1):176–177. doi: 10.1086/375829. [DOI] [PubMed] [Google Scholar]
- 8.Kazi A.M., Cortese M.M., Yu Y., Lopman B., Morrow A.L., Fleming J.A., McNeal M.M., Steele A.D., Parashar U.D., Zaidi A.K.M., et al. Secretor and salivary ABO blood group antigen status predict rotavirus vaccine take in infants. J. Infect. Dis. 2017;215(5):786–789. doi: 10.1093/infdis/jix028. [DOI] [PubMed] [Google Scholar]
- 9.Liu J., Zhang S., Liu M., Wang Q., Shen H., Zhang Y. Distribution of ABO/Rh blood groups and their association with hepatitis B virus infection in 3.8 million Chinese adults: a population-based cross-sectional study. J. Viral Hepat. 2018;25(4):401–411. doi: 10.1111/jvh.12829. [DOI] [PubMed] [Google Scholar]
- 10.Göker H., AladağKarakulak E., Demiroğlu H., AyazCeylan Ç.M., Büyükaşik Y., Inkaya A.Ç., Aksu S., Sayinalp N., Haznedaroğlu I.C., Ö Uzun, Akova M., Özcebe O.I., Ünal S. The effects of blood group types on the risk of COVID-19 infection and its clinical outcome. Turk. J. Med. Sci. 2020 Jun 4;50(4):679–683. doi: 10.3906/sag-2005-395. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wu Y., Feng Z., Li P., Yu Q. Relationship between ABO blood group distribution and clinical characteristics in patients with COVID-19. Clin. Chim. Acta. 2020 Oct;509:220–223. doi: 10.1016/j.cca.2020.06.026. Epub 2020 Jun 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zhao J., Yang Y., Huang H., Li D., Gu D., Lu X., Zhang Z., Liu L., Liu T., Liu Y., He Y., Sun B., Wei M., Yang G., Wang X., Zhang L., Zhou X., Xing M., Wang P.G. Relationship between the ABO blood group and the COVID-19 susceptibility. Clin. Infect. Dis. 2020 doi: 10.1093/cid/ciaa1150. Aug 4:ciaa1150. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sahani N., Pathak C., Chowdhury S., Sharma P., Sushmita S., Dhawan I. The prevalence of abo and rh blood groups in general population and comparing male and female blood group distribution. Ann. Appl. Bio-Sci. 2018;5:A77–A82. [Google Scholar]
- 14.Patidar, G. K., & Dhiman, Y. Distribution of ABO and Rh (D) Blood groups in India: a systematic review. ISBT Sci. Ser.. doi/epdf/10.1111/voxs.12576.
- 15.Agrawal A., Tiwari A.K., Mehta N., Bhattacharya P., Wankhede R., Tulsiani S., Kamath S. ABO and Rh (D) group distribution and gene frequency; the first multicentric study in India. Asian J. Transfus. Sci. 2014;8(2):121. doi: 10.4103/0973-6247.137452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Das P.K., Nair S.C., Harris V.K., Rose D., Mammen J.J., Bose Y.N., Sudarsanam A. Distribution of ABO and Rh-D blood groups among blood donors in a tertiary care centre in South India. Trop. Doct. 2001;31(1):47–48. doi: 10.1177/004947550103100121. [DOI] [PubMed] [Google Scholar]
- 17.Zietz M., Zucker J., Tatonetti N.P. Associations between blood type and COVID-19 infection, intubation, and death. Nat. Commun. 2020;11(1):1–6. doi: 10.1038/s41467-020-19623-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Latz C.A., DeCarlo C., Boitano L., Png C.M., Patell R., Conrad M.F., Dua A. Blood type and outcomes in patients with COVID-19. Ann. Hematol. 2020;99(9):2113–2118. doi: 10.1007/s00277-020-04169-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Guillon P., Clement M Sebille, V Rivain, JG Chou C.F. Inhibition of the interaction between the SARS-CoV spike protein and its cellular receptor by anti-histo-blood group antibodies. Glycobiology. 2008;18:1085–1093. doi: 10.1093/glycob/cwn093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Padhi S., Suvankar S., Dash D., Panda V.K., Pati A., Panigrahi J., Panda A.K. ABO blood group system is associated with COVID-19 mortality: an epidemiological investigation in the Indian population. Transfus. Clin. Biol. 2020;27(4):253–258. doi: 10.1016/j.tracli.2020.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bommanavar S., Smitha T. ABO blood grouping and COVID 19: is there any correlation in suspectibility? J. Oral Maxillofac. Pathol.: JOMFP. 2020;24(2):212. doi: 10.4103/jomfp.JOMFP_240_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bhandari S., Shaktawat A.S., Tak A., Patel B., Shukla J., Singhal S., Wehner T.C. 2020. Relationship between Blood Group Phenotypes (ABO, Rh and Kell) and nCOVID-19 Susceptibility–A Retrospective Observational Study. [DOI] [Google Scholar]
- 23.Luo J.Q., He F.Z., Luo Z.Y., Wen J.G., Wang L.Y., Sun N.L., Zhang W. Rs495828 polymorphism of the ABO gene is a predictor of enalapril-induced cough in Chinese patients with essential hypertension. Pharmacogenetics Genom. 2014;24(6):306–313. doi: 10.1097/FPC.0000000000000050. [DOI] [PubMed] [Google Scholar]
- 24.Gassó P., Ritter M.A., Mas S., Lafuente A. Influence of ABO genotype and phenotype on angiotensin-converting enzyme plasma activity. J. Renin-Angiotensin-Aldosterone Syst. JRAAS. 2014;15(4):580–584. doi: 10.1177/1470320313510583. [DOI] [PubMed] [Google Scholar]
- 25.Naitza S., Porcu E., Steri M., Taub D.D., Mulas A., Xiao X., Cucca F. A genome-wide association scan on the levels of markers of inflammation in Sardinians reveals associations that underpin its complex regulation. PLoS Genet. 2012;8(1) doi: 10.1371/journal.pgen.1002480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Grilo A., Sáez-Rosas M.P., Santos-Morano J., Sánchez E., Moreno-Rey C., Real L.M., Sáez M.E. Identification of genetic factors associated with susceptibility to angiotensin-converting enzyme inhibitors-induced cough. Pharmacogenetics Genom. 2011;21(1):10–17. doi: 10.1097/FPC.0b013e328341041c. [DOI] [PubMed] [Google Scholar]
- 27.Wu O., Bayoumi N., Vickers M.A., Clark P. ABO (H) blood groups and vascular disease: a systematic review and meta‐analysis. J. Thromb. Haemostasis. 2008;6(1):62–69. doi: 10.1111/j.1538-7836.2007.02818.x. [DOI] [PubMed] [Google Scholar]
- 28.Paré G., Chasman D.I., Kellogg M., Zee R.Y., Rifai N., Badola S., Ridker P.M. Novel association of ABO histo-blood group antigen with soluble ICAM-1: results of a genome-wide association study of 6,578 women. PLoS Genet. 2008;4(7) doi: 10.1371/journal.pgen.1000118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dai X. ABO blood group predisposes to COVID-19 severity and cardiovascular diseases. Eur. J. Prev. Cardiol. 2020;27(13):1436–1437. doi: 10.1177/2047487320922370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jenkins P.V., O'Donnell J.S. ABO blood group determines plasma von Willebrand factor levels: a biologic function after all? Transfusion. 2006;46(10):1836–1844. doi: 10.1111/j.1537-2995.2006.00975.x. [DOI] [PubMed] [Google Scholar]
- 31.Zhao Y., Zhao Z., Wang Y., Zhou Y., Ma Y., Zuo W. Single-cell RNA expression profiling of ACE2, the receptor of SARS-CoV-2. Am. J. Respir. Crit. Care Med. 2020;202(5):756–759. doi: 10.1164/rccm.202001-0179LE. [DOI] [PMC free article] [PubMed] [Google Scholar]