Abstract
The United States is currently experiencing an opioid epidemic, with deaths due to opioid overdoses persisting in many communities. This epidemic is the latest wave in a series of global substance use-related public health crises. As a fundamental cause of health inequities, stigma leads to the development of substance use disorders (SUDs), undermines SUD treatment efforts, and drives persistent disparities within these crises. Given their expertise in mental and behavioral health, psychologists are uniquely positioned to play a frontline role in addressing SUD stigma. The goal of this paper is to set an agenda for psychologists to address SUD stigma through clinical care, research, and advocacy. To set the stage for this agenda, key concepts are introduced related to stigma and SUDs, and evidence is reviewed regarding associations between stigma and substance use-related outcomes. As clinicians, psychologists have opportunities to promote resilience to stigma to prevent the development of SUDs, and leverage acceptance and mindfulness approaches to reduce internalized stigma among people with SUDs. As researchers, psychologists can clarify the experiences and impacts of stigma among people with SUDs over time and adapt the stigma-reduction toolbox to address SUD stigma. As advocates, psychologists can call for changes in structural stigma such as policies that criminalize people with SUDs, protest the intentional use of SUD stigma, and adopt stigma-free language in professional and social settings.
Keywords: alcohol, discrimination, opioids, stigma, substance use disorders
Introduction
We are experiencing an opioid epidemic, with deaths due to opioid overdoses persisting in many communities across the United States (U.S.). Between 1999 and 2018, 446,032 deaths were attributed to overdoses in prescribed opioids, heroin, fentanyl, and other synthetic opioids, with 46,802 of these deaths occurring in 2018 alone (Wilson et al., 2020). The current opioid epidemic is the latest wave in a series of global substance use-related public health crises, surrounding morphine, cocaine, methamphetamine, tobacco, and other substances (Brown, 1981; United Nations Office on Drugs and Crime, 2008). Moreover, the opioid epidemic does not exist in a vacuum: an additional 323,903 overdose deaths due to other substances, such as methamphetamine and cocaine, also occurred between 1999 and 2018, including 20,565 in 2018 (Wilson et al., 2020). As a fundamental cause of health inequities (Hatzenbuehler et al., 2013), stigma leads to the development of substance use disorders (SUDs), undermines SUD treatment efforts, and drives persistent disparities within these epidemics and crises.
Given their expertise in mental and behavioral health, psychologists are uniquely positioned to play a frontline role in addressing stigma within the current opioid epidemic as well as within co-occurring and future substance use crises. They can leverage what they’ve learned within other contexts, including theoretical blueprints and evidence-based stigma-reduction tools, to make swift and effective progress toward understanding and addressing stigma. The goal of this paper is to set an agenda for psychologists to address SUD stigma through clinical care, research, and advocacy. To set this stage for this agenda, key concepts are introduced related to stigma and SUDs, and evidence is reviewed regarding associations between stigma and substance use-related outcomes.
Definitions, Key Concepts, and Processes
Theorists and researchers have constructed a definition of stigma, articulated key concepts related to stigma, and described processes linking stigma with health inequities across the lifespan. Within this section, these definitions, key concepts, and processes are described in the context of SUDs, with a focus on the current opioid epidemic. A conceptual framework, which builds off of previous theory and research on stigma and health inequities (Earnshaw et al., 2013; Earnshaw & Chaudoir, 2009; Hatzenbuehler et al., 2013; Quinn & Earnshaw, 2011; Smith & Earnshaw, 2017), is included to guide this discussion (Figure 1).
Figure 1. Substance Use Stigma Framework.
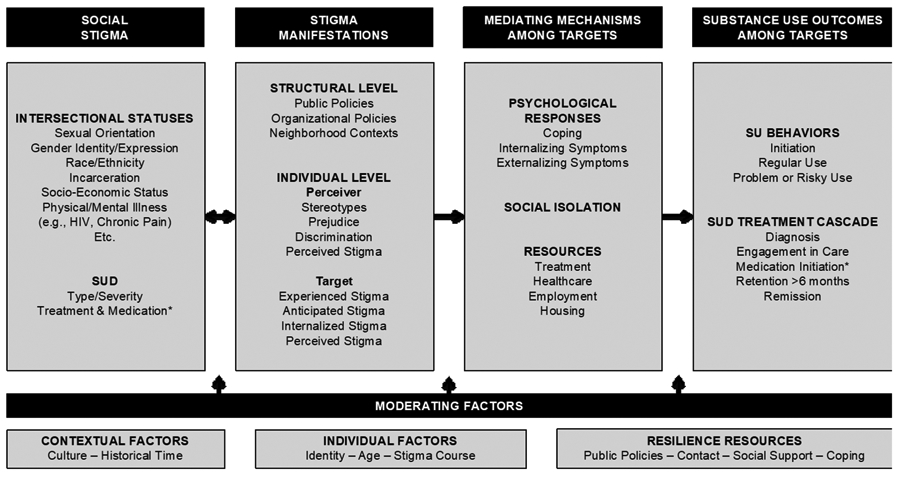
Note: *Medication and medication initiation as applicable to the specific SUD
Social Stigma
Stigma associated with a wide range of socially devalued and discredited identities, behaviors, and other characteristics (i.e., stigmatized statuses), plays a role in substance use-related outcomes. Stigma has been conceptualized as a social process that exists when labeling, stereotyping, separation, status loss, and discrimination occur within a power context (Link & Phelan, 2001). Stigma is recognized to be a fundamental cause of health inequities (Hatzenbuehler et al., 2013). There are several features of stigma that are common, cutting across all stigmatized statuses (Birbeck et al., 2019). As examples, the pathways linking stigma with health inequities (Chaudoir et al., 2013; Hatzenbuehler et al., 2013; Meyer, 1995) and the intervention tools to address stigma (Cook et al., 2014; Rao et al., 2019) are similar across statuses. Given these common and cross-cutting features, psychologists can leverage what they have learned about stigma in a wide range of contexts (e.g., race, HIV) to understand and address stigma in the context of SUDs.
Stigma associated with SUDs is theorized to serve a societal function of enforcing conformity to social norms surrounding non- or moderate use of substances (Phelan et al., 2008). This function of stigma applies when behaviors are viewed as voluntary and thus changeable. In the midst of the current opioid epidemic, debate has returned to the ethical question of whether stigma should ever be used to promote public health, including by preventing opioid use (Bayer, 2008). Advocates of this strategy point out that this is the function of stigma. Advocates further claim that denormalization policies, which ultimately sanctioned stigma towards people who use tobacco, were successful in public health efforts to prevent and reduce tobacco use in the U.S. (Bell et al., 2010). Yet, this strategy has at least two critical flaws. First, it overemphasizes the role of personal control in the initiation of substance use. Environmental, social, and genetic factors play key roles in substance use initiation (Volkow et al., 2016). Stigma cannot prevent people from engaging in a behavior that they do not fully control. Second, the strategy sacrifices the wellbeing of people with SUDs, given that stigma is a barrier to their recovery efforts. An excess of shame undermines recovery; whereas enhanced self-esteem, hope, and inspiration facilitate recovery (Hill & Leeming, 2014). By blocking access to resources that facilitate recovery, stigma can also widen already-existing health inequities surrounding substance use. In the case of tobacco use, stigma had made it particularly difficult for people with limited resources to stop using tobacco (Bell et al., 2010).
Stigma is recognized to be intersectional. Intersectionality theory posits that individuals live with multiple interconnected statuses that represent dimensions of both marginalization and privilege (Rosenthal, 2016). Multiple, interconnected forms of stigma lead to substance use behaviors among people who are at risk of developing a SUD, such as stigma associated with sexual and gender minority identities and expressions, race/ethnicity, incarceration, socioeconomic status, physical and mental illnesses (e.g., HIV and chronic pain), and other statuses. It further recognizes that stigma associated with multiple statuses intersects with stigma associated with SUDs and SUD treatment to shape inequities along the SUD treatment cascade. At the structural level, intersectionality theory emphasizes that systems of oppression are interlocking and reinforcing. For example, racism and substance use stigma have been interwoven throughout the history of the U.S., with substance use stigma often wielded to fortify racism and vice versa (Brown, 1981; Kerr & Jackson, 2016). Racism led to harsher penalties towards the use of crack cocaine, which was associated with Black and African Americans, than powder cocaine, which was associated with White Americans, in the late 20th century (Lowney, 1994). At the individual level, intersectionality theory holds that individuals’ experiences of and responses to stigma are shaped by all aspects of the self. As an example of the intersection of gender and SUD stigma, women (but not men) in recovery from SUDs report that others stereotype them as having engaged in sex work (Earnshaw, Smith et al., 2013).
Stigma Manifestations: Structural and Individual Levels
Stigma is manifested, or expressed and experienced, at the structural and individual levels. These stigma manifestations, in turn, reinforce and sustain stigma (Earnshaw et al., 2013; Link & Phelan, 2001). At the structural level, stigma is manifested within societal-level conditions, cultural norms, and institutional policies (Hatzenbuehler & Link, 2014). At the individual level, stigma is manifested among individuals who are not living with the stigmatized status of focus (referred to herein as perceivers) as well as individuals who are living with the stigmatized status (referred to as targets). Boundaries between structures, perceivers, and targets are porous, interlocking, and reinforcing. Blurring the lines between structures and individuals, individuals populate government systems that pass laws, organizations that construct policies, and neighborhoods that are home to local movements. Individuals can therefore both affect and are affected by structural change (de la Sablonnière, 2017). Blurring the lines between perceivers and targets, a perceiver of SUD stigma may be a target of race/ethnicity or sexual and gender minority stigma (Stangl et al., 2019).
Structural Level
Substance use stigma has been manifested at the structural level within public policy, organizations, and neighborhoods throughout the history of the U.S. Public policies that criminalize people who use substances and have SUDs represent a particularly harmful example of structural level substance use stigma. In 1971, President Nixon declared the “war on drugs” by naming drugs as America’s “public enemy number one.” The war on drugs rested on the theory that drug use is voluntary and controllable, and thus can be prevented and stopped through harsh punishment (Gostin, 1990). The war on drugs has led to a steep increase in incarceration, with rates disproportionately high among racial and ethnic minorities (Moore & Elkavich, 2008; Kerr & Jackson, 2016). Once in the criminal justice system, a low proportion of people who need SUD treatment actually receive it (Chandler et al., 2009).
Stigma is further manifested within organizational policies, including in employment and housing contexts. Drug tests are common in many employment settings with positive results barring hiring or precipitating termination. Although the Americans with Disabilities Act provides protections for people who are in recovery from SUDs in the workplace, it does not protect people who are currently engaged in illicit drug use (Lopez & Reid, 2017). Thus, people who use substances, with active SUDs, and in the early stages of recovery from SUDs (who are at risk of experiencing a recurrence of substance use symptoms) are vulnerable to termination in many workplaces. Similarly, many housing agencies have policies denying services for people engaging in active drug use or with histories of drug use (Lopez & Reid, 2017). Such policies are legal under the Fair Housing Law, and contribute to housing insecurity and homelessness among people with SUDs. Within neighborhood contexts, the not in my back yard (NIMBY) movement has been leveraged to oppose local SUD treatment centers and harm reduction efforts via protest, petition, and harassment of people who use drugs (Tempalski et al., 2007).
Individual Level: Perceivers
Perceivers of substance use stigma may include members of the general public, healthcare providers, police, employers, friends, family members, and others. Stigma manifestations may be explicit, when perceivers are aware of their own bias, or implicit, when perceivers are unaware of their own bias (Dovidio et al. 2008). Stereotypes include beliefs or thoughts about the characteristics and behaviors of people with stigmatized statuses. People with SUDs are perceived as low in both warmth and competence (Cuddy et al., 2008). People with SUDs are additionally viewed as dangerous and unpredictable, not capable of decision making, and responsible for their condition (Yang et al., 2018). Prejudice is an emotional reaction or feeling towards people with stigmatized statuses. Prejudice towards people with SUDs is characterized by contempt, and experienced as feelings that express moral outrage including: anger, disgust, hate, blame and resentment (Cuddy et al., 2008). Prejudice also includes fear of individuals with SUDs (Yang et al., 2018).
Discrimination spans unfair or unjust behavior directed at people with stigmatized statuses. Contempt-related emotions that underlie prejudice towards people with SUDs elicit harmful behaviors, such as those that are demeaning, condescending, and rejecting (Cuddy et al., 2008). Results of a nationally representative survey conducted in 2018 suggest that many U.S. adults are unwilling to have a person with an opioid use disorder (73.0%) or an alcohol use disorder (75.0%) marry into their family, work closely with someone with an opioid use disorder (75.9%) or an alcohol use disorder (79.7%), or become friends with someone with an opioid use disorder (45.1%) or an alcohol use disorder (40.1%) (Perry et al., in press). Additionally, people endorse policies that mandate coercive treatment and social restrictions, such as prohibiting individuals with SUDs from caring for children (Yang et al., 2018). Finally, perceived stigma includes perceptions of prejudice, stereotypes, and discrimination towards people with stigmatized statuses among others within one’s community.
Individual Level: Targets
Targets include people living with stigmatized statuses, including people at risk of or living with SUDs. Experienced stigma (also referred to as enacted stigma or perceived discrimination) includes experiences of stereotypes, prejudice, and discrimination from others in the past or present. As examples, people in recovery from opioid use disorders report receiving poor or cold treatment from healthcare providers, being fired or not hired by employers, and being socially rejected or distrusted by family members and friends (Earnshaw et al., 2013). Anticipated stigma includes expectations of stereotypes, prejudice, and discrimination from others in the future. People with SUDs describe substantial concerns about how others will view them, ultimately undermining disclosure of symptoms and access to treatment (Earnshaw et al., 2019). Internalized stigma includes the extent to which people endorse prejudice and stereotypes associated with a stigmatized status and apply them to the self. Shame has been described as the “emotional core” of internalized stigma, and is common among people with SUDs (Luoma et al., 2012). Similar to people not living with stigmatized statuses, targets of stigma may also perceive stigma within their communities.
These stigma manifestations may also be experienced as associative stigma by individuals who are affiliated with others living with stigmatized statuses. Caregivers of adolescents with SUDs are viewed by some as personally responsible for the onset and relapses of their children’s SUDs, incompetent, and pitiable (Corrigan et al., 2006). Moreover, caregivers report being gossiped about and socially rejected, and worry that they will be blamed for their children’s SUD (Earnshaw et al., 2019). Associative stigma can impact the wellbeing of caregivers and spouses, undermining their ability to provide support to loved ones with SUDs.
Mediating Mechanisms and Substance Use Outcomes among Targets
Stigma manifestations may impact substance use outcomes among people at risk of and living with SUDs via mediating mechanisms. Based on previous stigma theory and research (Chaudoir et al., 2013; Hatzenbuehler et al., 2013; Meyer, 1995), three categories of mediating mechanisms linking stigma manifestations with substance use outcomes are highlighted: psychological responses to stigma, social isolation, and access to resources. Among people living with a range of intersectional stigmatized statuses, stigma manifestations and ensuing mediating mechanisms may lead to substance use initiation, regular use, and problem or risky use. For this group, psychological responses to stigma may be a particularly important mediating mechanism given the prominent role of stress and coping processes in substance use. Among people with SUDs, stigma manifestations and ensuing mediating mechanisms may lead to outcomes along the SUD treatment cascade. This cascade is based on the Opioid Use Disorder Cascade of Care, which identifies diagnosis, engagement in care, initiation of medications, retention in care for longer than six months, and remission as progressive stages towards recovery (Williams et al., 2019). For this group, all three mediating mechanisms may play important roles in recovery. Extending the reach of stigma, substance use and under- or untreated SUDs can, in turn, have long-term effects on health (U.S. Department of Health and Human Services, 2016). As examples, alcohol and drug use is associated with cardiovascular, cardiopulmonary, liver, and pancreatic diseases as well as various forms of cancer. Injection drug use is associated with communicable diseases such as HIV and Hepatitis C.
Psychological Responses to Stigma
Experiences of stigma manifestations elicit psychological responses that may lead to substance use among targets. From a stress and coping perspective (Miller & Kaiser, 2001), stigma manifestations are characterized as significant stressors that may elicit both internalizing (e.g., depression, anxiety) and externalizing (e.g., anger, hostility) symptoms among targets. In turn, targets may engage in substance use as a form of distraction coping to draw their attention away from distressing or uncomfortable thoughts and feelings. Supporting this perspective, depressive symptoms mediate associations between experienced and internalized stigma with multiple indicators of substance use among people living with HIV (Earnshaw et al., in press). Depressive and anxiety symptoms similarly mediate associations between experienced stigma and heavy drinking among multiracial gay and bisexual men (English et al., 2018). Anger and hostility mediate the association between experienced stigma and substance use among African American adolescents and their parents, respectively (Gibbons et al., 2010).
Similar processes appear to unfold among people with SUDs. For example, young people with SUDs report continuing to engage in substance use to cope with experienced stigma from others (Earnshaw et al., 2019). Moreover, shame (i.e., the “emotional core” of internalized stigma) is associated with treatment-seeking delays, recurrence of substance use symptoms, and treatment dropout (Luoma et al., 2012).
Social Isolation
Stigma manifestations lead to social isolation among targets, with particularly harmful implications for people with SUDs. Social connection and support are associated with outcomes that facilitate recovery, including decreases in SUD severity over time, greater retention in care, and lower psychological distress (Dobkin et al., 2002). Moreover, family engagement is a key facilitator of SUD prevention, treatment, and recovery (Ventura & Bagley, 2017). At the structural level, incarceration disrupts relationships between people with SUDs and family members (Cochran & Mears, 2013). Upon release from prison, people who are more isolated from family are more likely to engage in drug use. At the individual level, people with SUDs describe substantial social rejection from family members and friends, including not answering phone calls, not being allowed into their homes, and even being disowned (Earnshaw et al., 2013). They note that this social rejection exacerbates self-isolation that they may have engaged in as a result of their SUD. Youth with SUDs and their caregivers additionally report not disclosing their or their child’s substance use to others due to anticipated stigma (Earnshaw et al., 2019), which further contributes to social isolation of families affected by SUDs.
Access to Resources
Stigma undermines access to resources that may promote wellbeing among targets, especially those with SUDs. Underinvestment in policies that would improve the availability of, access to, and uptake of evidence-based treatments represents a pernicious form of structural level stigma that undermines resources that could promote recovery among people with SUDs (Wakeman & Rich, 2018). Results of the National Survey on Drug Use and Health estimated that only 3.7 of the 21.2 million U.S. adults aged 12 or older (17.5%) who needed substance use treatment in 2018 actually received it (SAMHSA, 2019). Similarly, evidence suggests that many people who could benefit from medications for opioid use disorders, which promote abstinence from opioids (Schuckit, 2016), do not receive them. One study demonstrated that less than 5% of adolescents and 23% of adults received medication in the year prior to experiencing a non-fatal overdose, and only 8% of adolescents and 29% of adults received medication in the year after (Chatterjee et al., 2019). Additionally, few people with SUDs who are incarcerated receive treatment, contributing to high rates of re-engagement in substance use upon release (Galea & Vlahov, 2002; Wakeman & Rich, 2018).
Stigma manifestations among healthcare providers can block access to effective healthcare for a wide range of health conditions among people with SUDs. People with SUDs and their family report receiving ineffective and negative treatment from some healthcare workers, particularly in emergency care and surgical settings (Earnshaw et al., 2013; Earnshaw et al., 2019). Additionally, organizational policies and discrimination from employers can block access to employment for people in recovery; employment rates among people with some types of SUDs are low (Richardson & Epp, 2016). Yet, employment is associated with better recovery-related outcomes, including abstinence from substance use and longer retention in treatment. Organizational policies and discrimination further block access to housing. In turn, homelessness exacerbates risks of negative health outcomes, including exposure to infectious disease (e.g., tuberculosis, HIV), engagement in health risk behaviors (e.g., trading drugs for sex), and death (Galea & Vlahov, 2002).
Moderating Factors
Moderating factors shape the ways in which stigma is manifested as well as the processes whereby stigma impacts substance use outcomes. Contextual factors situate stigma processes within places and historical times. Individual factors situate stigma within individual characteristics, including identity processes, age, and stigma course (e.g., substance use stage). Understanding where, when, and among whom stigma is experienced can elucidate how stigma is manifested and impacts outcomes. Resilience resources are factors at the structural and individual levels that may attenuate the impact of stigma on outcomes. Although they may overlap with contextual and individual factors, resilience resources are unique in that they represent promising targets for intervention to protect individuals from the deleterious effects of stigma manifestations on substance use.
Contextual Factors
Stigma unfolds within particular cultural contexts, which may shape stigma manifestations and outcomes of stigma among targets. Reflecting variation in structural stigma, there is variability in drug policies internationally. For example, the Philippines has drawn attention for policies that have led to the deaths of thousands of people who use drugs since 2016 (Human Rights Watch, 2019). In contrast, Switzerland and other countries have experimented with state-sponsored heroin-assisted treatment for people with heroin use disorders who have not benefited from other treatments (Fischer et al., 2007). Due to differences in structural stigma, an individual with an opioid use disorder may experience very different outcomes in the Philippines versus Switzerland. Additionally, stigma is experienced at specific historical times. There have been pronounced evolutions in stigma associated with stigmatized statuses including SUDs over time. For example, representing change in SUD structural stigma, laws permitting access to naloxone (i.e., a medication that can reverse opioid overdoses and was approved by the U.S. Food and Drug Administration in 1971) spread from 6 U.S. states in 2010 to 49 by 2017 (Prescription Drug Abuse Policy System, 2017).
Individual Factors
Stigma manifestations among targets are also shaped by identity processes. Social statuses vary in magnitude, or size and importance, within an individual’s overall self-concept (Quinn & Earnshaw, 2013). Centrality is the extent to which an individual feels that a particular status defines them as a person, and salience is the frequency with which an individual thinks about a particular status. Evidence suggests that people with SUDs and other concealable stigmatized identities experience the most psychological distress when they have internalized stigma associated with a status that is highly central to their self-concept (Quinn et al., 2014).
There are developmental stages, or ages, when targets may be at greater risk of experiencing stigma manifestations and/or may be more vulnerable to the effects of stigma manifestations on outcomes (Gee et al., 2012). Whereas caregivers of adolescents with SUDs are often confident in their own abilities to cope with enacted stigma, some worry about their children’s capacity for coping with these negative experiences (Earnshaw et al., 2019). Regarding stigma course, many stigmatized statuses change over time and stigma manifestations may change with them. For example, evidence suggests that internalized and anticipated HIV and sexually transmitted infection stigma is heightened immediately after diagnosis and then begins to decline over the first year of living with the diagnosis (Eaton et al., 2018). Similarly, stigma manifestations may evolve as people are diagnosed with a SUD and progress through the SUD treatment cascade.
Resilience Resources
There are resources at the structural and individual levels that promote resilience to stigma, helping to reduce the risk of developing stigma manifestations and inoculate targets from the negative effects of stigma on substance use outcomes. At the structural level, some public policies prohibit discrimination. For example, the Americans with Disabilities Act protects people in recovery from SUDs from discrimination in employment and other settings. An additional policy, 42 CFR Part 2, protects confidentiality of people with SUDs from disclosures that may place them at risk of experienced stigma (Lopez & Reid, 2017).
At the individual level among perceivers, contact with people living with stigmatized statuses can prevent and reduce prejudice. Developmental intergroup theory suggests that prejudice may be less likely to develop among children when groups are integrated, facilitating familiarity with targets and promoting perceptions of equality between group members (Bigler & Liben, 2013). Work on the contact hypothesis demonstrates that contact can reduce existing prejudice by enhancing knowledge about targets, reducing anxiety about interacting with targets, and increasing empathy towards targets (Pettigrew & Tropp, 2008).
Among targets, social support and adaptive coping have received attention as resources that buffer targets from the deleterious effects of stigma on health (Earnshaw et al. 2015; Earnshaw et al., 2013). For example, youth experiencing race-based bullying are less likely to initiate smoking if they have at least one adult at school from whom they receive support (Earnshaw et al., 2014). Research has also identified personality characteristics (e.g., spiritual peace, self-efficacy, optimism), as resilience resources with promise to promote well-being among targets (Dulin et al., 2018). Many of these resources block the effects of enacted and anticipated stigma on negative psychological responses to stigma, such as stress and depressive symptoms, that ultimately lead to substance use outcomes.
Agenda for Future Directions
As experts in mental and behavioral health, psychologists are uniquely positioned to play a frontline role in addressing stigma to promote SUD prevention and treatment. Psychologists have remarkable reach via their roles as clinicians, researchers, interventionists, teachers, employers, co-workers, community members, friends, and family members. Below, strategies are identified for psychologists to address stigma via clinical care, research, and advocacy.
Clinical Care
Psychologists have a substantial opportunity to address stigma experienced by targets via clinical care. Psychologists can promote resilience among people living with stigmatized statuses to prevent the development of SUDs. As noted above, research has identified a suite of resilience resources that buffer targets from the deleterious effects of stigma on health. Within this suite, coping shows particular promise for promoting resilience because it appears to both mediate and moderate associations between stigma and substance use outcomes. Thus, promoting adaptive coping may break pathways between experiences of stigma and substance use, promoting resilience to experiences of stigma. Adaptive coping may be promoted via cognitive-behavioral therapies that help targets replace maladaptive coping responses with adaptive ones (Pachankis, 2018).
Psychologists can develop, adapt, and apply evidence-based affirmative treatments for targets. Pachankis (2018) has called for evidence-based affirmative treatments for sexual and gender minority populations that are tailored to address unique life experiences, including those related to stigma, that shape the mental health of these populations but are not shared by heterosexual and cisgender individuals. Pachankis identifies key principles of affirmative treatments as: helping individuals develop insight into how stigma compromises their mental health, desensitizing individuals to negative feelings and cognitive styles that can result from stigma (e.g., shame, hopelessness), promoting resilience, and providing resources and advocacy. These principals could apply to mental health treatments for people living with a wide range of stigmatized statuses including SUDs, ultimately improving mental health outcomes and possibly contributing to the prevention and treatment of SUDs.
Psychologists can leverage acceptance and mindfulness approaches to address internalized stigma among people with SUDs. As noted above, people with SUDs with greater internalized stigma and shame experience worse treatment and recovery-related outcomes. Luoma and colleagues have developed and tested a group-based intervention for people with SUDs targeting shame that is based on the principles of acceptance and commitment therapy (Luoma et al., 2012). This approach encourages individuals to notice and experience, rather than suppress and avoid, feelings of shame. Cognitive diffusion and acceptance techniques are then exercised, including via mindfulness and values exercises. In comparison to a group receiving treatment as usual, people with SUDs receiving the acceptance and commitment therapy intervention showed reduced internalized shame, fewer days of substance use, and higher treatment attendance four months after the intervention (Luoma et al., 2012).
Psychologists can provide support surrounding disclosure decisions and processes among people with SUDs. Disclosure involves the sharing of information surrounding one’s SUD history, resolution, and/or treatment with other people such as family, friends, employers, healthcare providers, and acquaintances (Chaudoir & Fisher, 2011). Disclosure is an important process given that it can act as a gateway to social support, which may facilitate recovery, and/or stigma, which may undermine recovery. Yet, people in recovery from SUDs report struggling with decisions regarding whether, to whom, what, when, and how to disclose to others (Earnshaw et al., 2019). Moreover, evidence from a nationally representative sample suggests that many people in recovery from alcohol and other drug problems are uncomfortable with disclosure (Earnshaw, Bergman, et al., 2019). People who have been in recovery for shorter amounts of time and people who are disclosing to others with whom they are less close (e.g., acquaintances and co-workers) report greater discomfort surrounding disclosure. Psychologists have important roles to play in facilitating disclosure-related decision making, building disclosure skills, and supporting people through the after-math of disclosures.
Research
Psychologists have much to contribute to understanding and addressing the role of stigma in SUDs. In comparison to other areas of stigma research, SUD stigma is arguably understudied (Corrigan et al., 2017). More research is needed to describe the processes whereby stigma manifestations impact mediating mechanisms and substance use outcomes to build a stronger understanding of how stigma impacts substance use. Additionally, more research is needed that adopts an intersectional lens and attends to moderating factors to better understand who is most vulnerable to the impacts of stigma on substance use. Specific recommendations for research are described below.
Basic social and behavioral science research can continue to clarify the experiences and impacts of stigma manifestations among people with SUDs over time (Corrigan et al., 2017). Much of our understanding of associations between stigma and health inequities rests on research with people with stigmatized statuses that are relatively stable over time. People are often born into a stigmatized group (e.g., minority races/ethnicities, female sex), become aware that they are a member of a stigmatized group (e.g., minority sexual and gender identities and expressions), or transition into a stigmatized group (e.g., HIV, incarceration). Their experiences of stigma manifestations may fluctuate some as their identity develops and as they transition into new environments; yet, they may also reach sustained periods of relative stability. For example, some evidence suggests that people experience heightened HIV stigma immediately after an HIV diagnosis but that this stigma decreases and begins to plateau within several months (Eaton et al., 2018). In contrast, SUDs may be considerably more dynamic stigmatized statuses. As people develop SUDs, transition into recovery, and possibly experience relapses of substance use symptoms (Kelly et al., 2017), the ways in which they experience stigma manifestations and how these stigma manifestations impact outcomes may fluctuate. To better understand the dynamic nature of substance use stigma, psychologists conducting cross-sectional research might seek to understand whether and how stigma impacts people differently at various stages of SUD development and recovery. Additionally, psychologists conducting longitudinal research can identify trajectories of stigma manifestations over the course of time. Such research can pinpoint times when people are particularly vulnerable to stigma.
To help the field make faster progress towards understanding and addressing SUD stigma, psychologists can use validated and theory-based measures when possible. A review of studies measuring mental illness stigma, including those measuring SUD stigma, between 2004 and 2014 highlighted a concerning trend: 444 measures of mental illness stigma had been used during this time period, 304 (68%) of which were developed for a single study and not necessarily psychometrically validated (Fox et al., 2018). Of the remaining 140 scales, only 24 had been cited at least 10 times. Thus, many researchers are creating new scales for their individual studies rather than using existing validated scales. The use of so many scales, many of which represent varying conceptualizations of stigma and/or may not be psychometrically strong, slows progress towards developing shared understanding of the impact of stigma on substance use-related outcomes. Mixed findings between studies may reflect measurement variation rather than substantive differences in associations between stigma and outcomes. Theory-based and validated measures of SUD stigma are available (Smith et al., 2016; Smith et al., 2019). By using these and other common measures whenever possible, we can make faster progress towards understanding SUD stigma as a field.
Psychologists can help to address stigma by adapting the stigma-reduction toolbox to the context of substance use, and then test stigma interventions in longitudinal, multilevel, and multicomponent studies. Decades of research has yielded a stigma-reduction toolbox that contains evidence-based tools to reduce stigma and ways to use these tools to maximize their efficacy (Chaudoir et al., 2017; Cook et al., 2014; Corrigan et al., 2017; Rao et al., 2019). Beyond the tools to address stigma among people with SUDs noted above, these tools include behavioral design at the structural level (i.e., constraining opportunities for stigma to influence decision making, including within care settings; Bohnet, 2016), contact at the interpersonal level (i.e., facilitating interaction between perceivers with targets; Pettigrew & Tropp, 2006), and education at the individual level for perceivers (i.e., providing fact-based information to refute stereotypes; Cook et al., 2014). Many of these tools have been shown to be effective for reducing SUD stigma specifically (Livingston et al., 2012). Interventions implementing these tools should be: (1) longitudinal, because single session interventions are insufficient to generate lasting change in stigma manifestations, especially stereotypes, prejudice, and discrimination (Earnshaw et al., 2018); (2) multilevel, because stigma is manifested at the individual and structural levels, and change at one level is unlikely to be sustained without change at both levels (Cook et al., 2014; Rao et al., 2019); and (3) multicomponent, because there is no known single “silver bullet” intervention strategy that can eliminate stigma but rather many tools that can be used collectively to reduce stigma (Cook et al., 2014; Rao et al., 2019).
Psychologists might prioritize investigating stigma-based interventions to address stigma at early ages to prevent the development of SUDs. Evidence suggests that youth who experience bullying are at risk of substance use (Earnshaw et al., 2017), with youth experiencing stigma-based bullying (i.e., bullying associated with a stigmatized status) at greatest risk of substance use (Russell et al., 2012). This is particularly concerning given that SUDs often onset during late adolescence (National Institute on Drug Abuse, 2014). A review of stigma-based bullying interventions published between 2000 and 2015 found that such interventions have been increasing in popularity, but have been unevenly distributed across stigmatized statuses, locations, and social contexts (Earnshaw et al., 2018). Psychologists have an opportunity to work with school administrators, teachers, students, and parents to investigate stigma-based bullying interventions to prevent substance use among youth.
Advocacy
Psychologists can advocate for changes in stigma manifestations at the structural and individual levels. Psychologists can call for changes in structural stigma, including the repeal of public policies that criminalize people with SUDs and organizational policies that deny services to people with SUDs. They can speak out against neighborhood movements that oppose evidence-based services for people with SUDs by writing op-eds for their local newspapers, sharing their thoughts via social media, and engaging in conversation with their neighbors.
Psychologists can protest the intentional use of stigma to prevent and/or treat SUDs. Public health prevention campaigns have intentionally leveraged and even promoted stigma by associating substance use with criminal or unethical activity, terrorism, violence, and poor health (Corrigan & Nieweglowski, 2018). For example, the iconic “this is your brain on drugs” public service announcements imply that people’s brains are fried, cracked, or destroyed by substance use. As noted above, intentionally leveraging stigma to prevent substance use is a flawed tactic insofar as it overemphasizes the role of personal control in substance use (Volkow et al., 2016). Prevention approaches are needed that work for everyone, not only people who are at low risk for substance use due a lack of environmental, social, or genetic risk factors. Some treatment programs may heighten internalized stigma among people in recovery from SUDs by encouraging them to focus on their character defects, retrospect on ways that they have wronged others, and acknowledge their own powerlessness (Corrigan et al., 2017). Yet, shame, the emotional core of internalized stigma, undermines recovery efforts (Hill & Leeming, 2014). In contrast, treatment approaches are needed that restore self-esteem, self-worth, and hope.
Psychologists are well-positioned to educate others about substance use and SUDs in their classrooms and communities. Knowledge can dismantle stereotypes and misinformation about SUDs (Livingston et al., 2012). For example, people receiving medications for opioid use disorders (e.g., methadone) are often accused of swapping “one drug for another” or “one addiction for another” (Earnshaw et al., 2013). Yet, the National Institute on Drug Abuse (2019) identifies medications as important tools for facilitating detoxification and preventing symptom relapse. Similarly, people view SUDs as difficult or unlikely to resolve. Yet, many people successfully recover from SUDs (Kelly et al., 2017). Engaging in conversations and sharing resources that present scientifically-accurate information about medications and recovery trajectories may help to dispel myths associated with SUDs and their medications.
Finally, psychologists can be mindful of language surrounding SUDs. Language spreads stereotypes about people with SUDs (Broyles et al., 2014). Evoking perceptions of controllability, personal responsibility, and criminality, people with SUDs are referred to as “dope fiends,” “pot heads” and “addicts”, who “abuse” drugs and have “dirty” urine tests (Broyles et al., 2014; Wakeman, 2013). People referred to as “substance abusers” are seen as more deserving of blame and punishment than people referred to as “having a SUD” by clinicians and members of the general public (Kelly et al., 2015). Using language that is scientifically accurate (e.g., “urine sample that tested positive for substance use” rather than “dirty urine”) and person first (e.g., “person with an opioid use disorder” rather than “heroin addict”) can promote perceptions of SUDs as a chronic, yet treatable, health condition. Language can also help with garnering support for policies that promote the wellbeing of people in recovery. For example, referring to “overdose prevention sites” rather than “safe consumption sites” leads to increased public support for an evidence-based harm reduction strategy wherein individuals can legally use pre-obtained drugs under medical supervision to reduce risk of overdose (Barry et al., 2018).
Conclusion
Similar to other health-related contexts (e.g., HIV, mental illness), stigma is a powerful social determinant of SUDs. Stigma can lead to the development of SUDs among people living with a wide range of stigmatized statuses, as well as undermine recovery efforts among people who have developed SUDs. Yet, we are better prepared now than ever before to address this stigma by leveraging what we know about why stigma exists, the ways in which it is manifested within structures and individuals, how it affects outcomes via mediating mechanisms, and what moderates it. As experts in mental and behavioral health, psychologists can play a frontline role in addressing stigma to prevent and treat SUDs via clinical care, research, and advocacy.
Table 1.
Key recommendations for future directions to address stigma and substance use
| Clinical Care |
|
|
|
|
| Research |
|
|
|
|
| Advocacy |
|
|
|
|
Public Significance Statement:
This paper describes how stigma, which is a social process of devaluation and discrediting, leads to substance use and undermines the treatment of substance use disorders. It also identifies ways that psychologists can address the role of stigma in substance use through their clinical care, research, and advocacy.
Acknowledgments:
The author would like to thank E. Carly Hill for providing helpful feedback on and assistance with this article.
Funding:
This manuscript was supported by a grant from the National Institute on Drug Abuse (K01DA042881). The content is solely the responsibility of the author and does not necessarily represent the official views of the National Institutes of Health.
References
- Barry CL, Sherman SG, & McGinty EE (2018). Language matters in combatting the opioid epidemic: Safe consumption sites versus overdose prevention sites. American Journal of Public Health, 108(9), 1157–1159. 10.2105/AJPH.2018.304588 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bayer R (2008). Stigma and the ethics of public health: Not can we but should we. Social Science & Medicine, 67, 463–472. 10.1016/j.socscimed.2008.03.017 [DOI] [PubMed] [Google Scholar]
- Bell K, Salmon A, Bowers M, Bell J, & Mccullough L (2010). Smoking, stigma and tobacco ‘denormalization’: Further reflections on the use of stigma as a public health tool. Social Science & Medicine, 70(6), 795–799. 10.1016/j.socscimed.2009.09.060 [DOI] [PubMed] [Google Scholar]
- Bigler RS, & Liben LS (2013). Developmental theory explaining prejudice intergroup and reducing children’s social stereotyping and prejudice. Current Directions in Psychological Science, 16(3), 162–166. [Google Scholar]
- Birbeck GL, Bond V, Earnshaw VA., & El-nasoor ML (2019). Advancing health equity through cross- cutting approaches to health-related stigma. BMC Medicine, 17(40), 1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bohnet I (2016). What works: Gender equality by design. Cambridge, MA: Harvard University Press. [Google Scholar]
- Brown LS (1981). Substance abuse and America: Historical perspective on the federal response to a social phenomenon. Journal of the National Medical Association, 73(6), 497–506. [PMC free article] [PubMed] [Google Scholar]
- Broyles LM, Binswanger IA, Jenkins JA, Finnell DS, Faseru B, Cavaiola A, & Gordon AJ (2014). Confronting inadvertent stigma and pejorative language in addiction scholarship: A recognition and response. Substance Abuse, 35(3), 217–221. 10.1080/08897077.2014.930372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chandler RK, Fletcher BW, & Volkow ND (2009). Treating drug abuse and addiction in the criminal justice system improving public health and safety. Journal of American Medical Association, 301(2), 183–190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chatterjee A, Larochelle MR, Xuan Z, Wang N, Bernson D, Silverstein M, & Bagley SM (2019). Non-fatal opioid-related overdoses among adolescents in Massachusetts 2012 −2014. Drug and Alcohol Dependence, 194, 28–31. 10.1016/j.drugalcdep.2018.09.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaudoir S, & Fisher JD (2011). The disclsoure process model: Understanding disclosure decision-making and post-disclosure outcomes among people living with a concealable stigmatized identity. Psychological Bulletin, 136(2), 236–256. 10.1037/a0018193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaudoir SR, Earnshaw VA, & Andel S (2013). “Discredited” versus “Discreditable”: Understanding how shared and unique stigma mechanisms affect psychological and physical health disparities. Basic and Applied Social Psychology, 35(1), 75–87. 10.1080/01973533.2012.746612 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaudoir SR, Wang K, & Pachankis JE (2017). What reduces sexual minority stress? A review of the intervention “toolkit,” 73(3), 586–617. 10.1111/josi.12233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cochran JC, & Mears DP (2013). Social isolation and inmate behavior: A conceptual framework for theorizing prison visitation and guiding and assessing research. Journal of Criminal Justice, 41(4), 252–261. 10.1016/j.jcrimjus.2013.05.001 [DOI] [Google Scholar]
- Cook JE, Purdie-Vaughns V, Meyer IH, & Busch JTA (2014). Intervening within and across levels: A multilevel approach to stigma and public health. Social Science & Medicine, 103, 101–109. 10.1016/j.socscimed.2013.09.023 [DOI] [PubMed] [Google Scholar]
- Corrigan PW, Miller FE, & Watson AC (2006). Blame, shame, and contamination : The impact of mental illness and drug dependence stigma on family members, 20(2), 239–246. 10.1037/0893-3200.20.2.239 [DOI] [PubMed] [Google Scholar]
- Corrigan PW & Nieweglowski K (2018). Stigma and the public health agenda for the opioid crisis in America. International Journal of Drug Policy, 59, 44–49. [DOI] [PubMed] [Google Scholar]
- Corrigan PW, Schomerus G, Shuman V, Kraus D, Perlick D, Harnish A, Smelson D (2017). Developing a research agenda for understanding the stigma of addictions. Part I: Lessons from the mental health stigma literature. American Journal on Addictions, 26(1), 59–66. 10.1111/ajad.12458 [DOI] [PubMed] [Google Scholar]
- Corrigan PW, Schomerus G, Shuman V, Kraus D, Perlick D, Harnish A, Smelson D (2017). Developing a research agenda for reducing the stigma of addictions. Part II: Lessons from the mental health stigma literature. American Journal on Addictions, 26(1), 67–74. 10.1111/ajad.12436 [DOI] [PubMed] [Google Scholar]
- Corrigan PW, Schomerus G & Smelson D (2017). Are some of the stigmas of addictions culturally sanctioned? The British Journal of Psychiatry, 210, 180–181. [DOI] [PubMed] [Google Scholar]
- Cuddy AJC, Fiske ST, & Glick P (2008). Warmth and competence as universal dimensions of social perception : The stereotype content model and the BIAS Map. Advances in Experimental Social Psychology, 20,61–149. 10.1016/S0065-2601(07)00002-0 [DOI] [Google Scholar]
- de la Sablonnière R (2017). Toward a psychology of social change : A typology of social change. Frontiers in Psychology, 8, 1–20. 10.3389/fpsyg.2017.00397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dobkin PL, De Civita M, Paraherakis A, & Gill K (2002). The role of functional social support in treatment retention and outcomes among outpatient adult substance abusers. Addiction, 97, 347–356. [DOI] [PubMed] [Google Scholar]
- Dovidio JF, Penner LA, Albrecht TL, Norton WE, Gaertner SL, & Shelton JN (2008). Disparities and distrust: The implications of psychological processes for understanding racial disparities in health and health care. Social Science & Medicine, 67, 478–486. 10.1016/j.socscimed.2008.03.019 [DOI] [PubMed] [Google Scholar]
- Dulin AJ, Dale SK, Earnshaw VA, Fava JL, Mugavero MJ, Napravnik S, … Howe CJ (2018). Resilience and HIV: A review of the definition and study of resilience. AIDS Care, 30(5), S6–S17. 10.1080/09540121.2018.1515470 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Earnshaw VA, & Chaudoir SR (2009). From conceptualizing to measuring HIV stigma : A review of HIV stigma mechanism measures. AIDS & Behavior, 13, 1160–1177. 10.1007/s10461-009-9593-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Earnshaw VA, Smith LR, & Copenhaver M (2013). Drug addiction in the context of methadone maintenance therapy: An investigation into understudied sources of stigma. International Journal of Mental Health and Addiction, 11(1), 110–122. 10.1007/s11469-012-9402-5.Drug [DOI] [PMC free article] [PubMed] [Google Scholar]
- Earnshaw VA, Bogart LM, Dovidio JF, & Williams DR (2013). Stigma and racial/ethnic HIV disparities: Moving toward resilience. American Psychologist, 68(4), 225–236. 10.1037/a0032705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Earnshaw VA, Rosenthal L, Carroll-Scott A, Peters SM, McCaslin C, & Ickovics JR (2014). Teacher involvement as a protective factor from the association between race-based bullying and smoking initiation. Social Psychology of Education, 17(2). 10.1007/s11218-014-9250-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Earnshaw VA, Lang SM, Lippitt M, Jin H, & Chaudoir SR (2015). HIV stigma and physical health symptoms: Do social support, adaptive coping, and/or identity centrality act as resilience resources? AIDS and Behavior, 19(1). 10.1007/s10461-014-0758-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Earnshaw VA, Elliott MN, Reisner SL, Mrug S, Windle M, Emery ST, … Schuster MA (2017). Peer victimization, depressive symptoms, and substance use: A longitudinal analysis. Pediatrics, 139(6), e20163426. 10.1542/peds.2016-3426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Earnshaw VA, Reisner SL, Menino DD, Poteat VP, Bogart LM, Barnes TN, & Schuster MA (2018). Stigma-based bullying interventions: A systematic review. Developmental Review. 10.1016/j.dr.2018.02.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Earnshaw VA, Bogart LM, Menino DD, Kelly JF, Chaudoir SR, Reed NM, & Levy S (2019). Disclosure, stigma, and social support among young people receiving treatment for substance use disorders and their caregivers: A qualitative analysis. International Journal of Mental Health and Addiction, 17(1535–1549). 10.1007/s11469-018-9930-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Earnshaw VA, Bergman BG, & Kelly JF (2019). Whether, when, and to whom ?: An investigation of comfort with disclosing alcohol and other drug histories in a nationally representative sample of recovering persons. Journal of Substance Abuse Treatment, 101, 29–37. 10.1016/j.jsat.2019.03.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Earnshaw VA, Eaton LA, Collier ZK, Watson RJ, Maksut JL, Rucinski KB, … Kalichman SC (in press). HIV stigma, depressive symptoms, and substance use. AIDS Patient Care & STDs. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eaton LA, Earnshaw VA, Maksut JL, Thorson KR, Watson RJ, & Bauermeister JA (2018). Experiences of stigma and health care engagement among Black MSM newly diagnosed with HIV/STI. Journal of Behavioral Medicine. 10.1007/s10865-018-9922-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- English D, Rendina HJ, & Parsons JT (2018). The effects of intersecting stigma: A longitudinal examination of minority stress, mental health, and substance use among Black, Latino, and multiracial gay and bisexual men. Psychology of Violence, 8(6), 669–679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fischer B, Oviedo-Joekes E, Blanken P, Haasen C, Rehm J, Schechter MT, van den Brink W (2007). Heroin-assisted Treatment (HAT) a decade later: A brief update on science and politics. Journal of Urban Health, 84(4), 552–562. 10.1007/s11524-007-9198-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fox AB, Earnshaw VA, Taverna EC, & Vogt D (2018). Conceptualizing and measuring mental illness stigma : The Mental Illness Stigma Framework and critical review of measures. Stigma and Health, 3(4), 348–376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galea S, & Vlahov D (2002). Social determinants and the health of drug users : socioeconomic status, homelessness, and incarceration. Public Health Reports, 117(1), 135–45. 10.2307/25747647 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gee GC, Walsemann KM, & Brondolo E (2012). A life course perspective on how racism may be related to health inequities. American Journal of Public Health, 102(5), 967–974. 10.2105/AJPH.2012.300666 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibbons FX, Etcheverry PE, Stock ML, Gerrard M, Weng CY, Kiviniemi M, & O’Hara RE (2010). Exploring the link between racial discrimination and substance use: What mediates? What buffers? Journal of Personality and Social Psychology, 99, 785–801. 10.1037/a0019880 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gostin L (1990). Waging a war on drug users: An alternative public health vision. Law, Medicine and Health Care, 385–394. [DOI] [PubMed] [Google Scholar]
- Hatzenbuehler ML, & Link BG (2014). Introduction to the special issue on structural stigma and health. Social Science & Medicine, (103), 1–6. [DOI] [PubMed] [Google Scholar]
- Hatzenbuehler ML, Phelan JC, & Link BG (2013). Stigma as a fundamental cause of population health inequalities. American Journal of Public Health, 103(5), 813–821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill JV, & Leeming D (2014). Reconstructing ‘the alcoholic’ : Recovering from alcohol addiction and the stigma this entails. International Journal of Mental Health and Addiction, 12, 759–771. 10.1007/s11469-014-9508-z [DOI] [Google Scholar]
- Human Rights Watch. (2019). Philippines: Events of 2018. Retrieved from https://www.hrw.org/world-report/2019/country-chapters/philippines
- Kelly JF, Bergman B, Hoeppner BB, Vilsaint C, & White WL (2017). Prevalence and pathways of recovery from drug and alcohol problems in the United States population: Implications for practice, research, and policy. Drug and Alcohol Dependence, 181,162–169. 10.1016/j.drugalcdep.2017.09.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JF, Wakeman SE, & Saitz R (2015). Stop talking “dirty”: Clinicians, language, and quality of care for the leading cause of preventable death in the United States. American Journal of Medicine, 128(1), 8–9. 10.1016/j.amjmed.2014.07.043 [DOI] [PubMed] [Google Scholar]
- Kerr J, & Jackson T (2016) Stigma, sexual risks, and the war on drugs: Examining drug policy and HIV/AIDS inequities among African Americans using the Drug War HIV/AIDS Inequities Model. International Journal of Drug Policy, 37, 31–41. [DOI] [PubMed] [Google Scholar]
- Link BG, & Phelan JC (2001). Conceptualizing stigma. Annual Review of Sociology, 363–385. [Google Scholar]
- Livingston JD, Milne T, Fang ML, & Amari E (2012). The effectiveness of interventions for reducing stigma related to substance use disorders: A systematic review. Addiction, 107(1), 39–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopez K, & Reid D (2017). Discrimination against patients with substance use disorders remains prevalent and harmful: The case for 42 CFR part 2. Retrieved April 2, 2020, from 10.1377/hblog20170413.059618/full/ [DOI] [Google Scholar]
- Lowney KD (1994). Smoked not snorted: Is racism inherent in our crack cocaine laws? Journal of Urban and Contemporary Law, 45, 121–174. [Google Scholar]
- Luoma JB, Kohlenberg BS, Hayes SC, & Fletcher L (2012). Slow and steady wins the race: A randomized clinical trial of acceptance and commitment therapy targeting shame in substance use disorders. Journal of Consulting and Clinical Psychology, 80(1), 43–53. 10.1037/a0026070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer IH (1995). Minority stress and mental health in gay men. Journal of Health and Social Behavior, 36, 38. 10.2307/2137286 [DOI] [PubMed] [Google Scholar]
- Miller CT, & Kaiser CR (2001). A theoretical perspective on coping with stigma. Journal of Social Issues, 57(1), 73–92. 10.1111/0022-4537.00202 [DOI] [Google Scholar]
- Moore LD, & Elkavich A (2008). Who’s using and who’s doing time: Incarceration, the War on Drugs, and public health. American Journal of Public Health, 98(5), 782–786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute on Drug Abuse. (2014). Principles of adolescent substance use disorder treatment: A research-based guide. Retrieved from http://www.drugabuse.gov
- National Institute on Drug Abuse. (2019). Treatment Approaches for Drug Addiction. Retrieved from https://www.drugabuse.gov/publications/drugfacts/treatment-approaches-drug-addiction
- Pachankis JE (2018). The scientific pursuit of sexual and gender minority mental health treatments: Toward evidence-based affirmative practice. American Psychologist, 73(9), 1207–1219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perry B, Pescosolido B, & Krendl A (in pess). The unique nature of public stigma toward opioid use disorders: A national study. Addiction. [DOI] [PubMed] [Google Scholar]
- Pettigrew TF, & Tropp LR (2006). A meta-analytic test of intergroup contact theory. Journal of Personality and Social Psychology, 90, 751–783. 10.1037/0022-3514.90.5.751 [DOI] [PubMed] [Google Scholar]
- Pettigrew TF, & Tropp LR (2008). How does intergroup contact reduce prejudice? Meta-analytic tests of three mediators. European Journal of Social Psychology, 38, 922–934. [Google Scholar]
- Phelan JC, Link BG, & Dovidio JF (2008). Stigma and prejudice: One animal or two? 10.1016/j.socscimed.2008.03.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prescription Drug Abuse Policy System. (2017). Naloxone Overdose Prevention Laws. Retrieved from http://pdaps.org/datasets/laws-regulating-administration-of-naloxone-1501695139
- Quinn DM, & Earnshaw VA (2011). Understanding concealable stigmatized identities: The role of identity in psychological, physical, and behavioral outcomes. Social Issues and Policy Review, 5(1). 10.1111/j.1751-2409.2011.01029.x [DOI] [Google Scholar]
- Quinn DM, & Earnshaw VA (2013). Concealable stigmatized identities and psychological well-being. Social and Personality Psychology Compass, 7(1). 10.1111/spc3.12005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quinn DM, Williams MK, Quintana F, Gaskins JL, Overstreet NM, Pishori A, & Chaudoir SR (2014). Examining effects of anticipated stigma, centrality, salience, internalization, and outness on psychological distress for people with concealable stigmatized identities. PLoS ONE, 9(5). 10.1371/journal.pone.0096977 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rao D, Elshafei A, Nguyen M, Hatzenbuehler ML, Frey S, & Go VF (2019). A systematic review of multi-level stigma interventions: State of the science and future directions. BMC Medicine, 17(41), 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richardson L, & Epp S (2016). Substance use disorders, employment and the return to work. In Schultz IZ & Gatchel RJ (Eds.), Handbook of Return to Work: From Research to Practice (pp. 667–692). New York: Springer. [Google Scholar]
- Rosenthal L (2016). Incorporating intersectionality into psychology: An opportunity to promote social justice and equity. American Psychologist, 71(6), 474. [DOI] [PubMed] [Google Scholar]
- Russell ST, Sinclair KO, Poteat VP, & Koenig BW (2012). Adolescent health and harassment based on discriminatory bias. American Journal of Public Health, 102, 493–495. 10.2105/AJPH.2011.300430 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schuckit MA (2016). Treatment of opioid-use disorders. The New England Journal of Medicine, 375(4), 357–368. 10.1056/NEJMra1604339 [DOI] [PubMed] [Google Scholar]
- Smith LR, & Earnshaw VA (2017). Stigma and substance use: A systematic review and theory-building process model. Annals of Behavioral Medicine. Paper presented at the meeting of the Society of Behavioral Medicine. San Diego, CA. [Google Scholar]
- Smith LR, Earnshaw VA, Copenhaver MM, & Cunningham CO (2016). Substance use stigma: Reliability and validity of a theory-based scale for substance-using populations. Drug and Alcohol Dependence, 162, 34–43. 10.1016/j.drugalcdep.2016.02.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith LR, Mittal ML, Wagner K, Copenhaver MM, Cunningham CO, & Earnshaw VA (2019). Factor structure , internal reliability and construct validity of the Methadone Maintenance Treatment Stigma Mechanisms Scale (MMT-SMS). Addiction, 115, 354–367. 10.1111/add.14799 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stangl AL, Earnshaw VA, Logie CH, Van Brakel W, Simbayi LC, Barré I, & Dovidio JF (2019). The health stigma and discrimination framework: A global, crosscutting framework to inform research, intervention development, and policy on health-related stigmas. BMC Medicine, 17–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SAMHSA: Substance Use and Mental Health Services Admistration. (2019). Key substance Use and Mental Health Indicators in the United States: Results from the 2018 National Survey on Drug Use and Health. Rockville, MD. Retrieved from https://www.samhsa.gov/data/%0A [Google Scholar]
- Tempalski B, Friedman R, Keem M, Cooper H, & Friedman SR (2007). NIMBY localism and national inequitable exclusion alliances: The case of syringe exchange programs in the United States. Geoforum, 38, 1250–1263. 10.1016/j.geoforum.2007.03.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- United Nations Office on Drugs and Crime. (2008). 2008 world drug report. Retrieved from https://www.unodc.org/documents/wdr/WDR_2008/WDR_2008_eng_web.pdf [Google Scholar]
- U.S. Department of Health and Human Services (HHS), Office of the Surgeon General. (November, 2016). Facing Addiction in America: The Surgeon General’s Report on Alcohol, Drugs, and Halth. Washington, DC: HHS. [PubMed] [Google Scholar]
- Ventura AS, & Bagley SM (2017). To improve substance use disorder prevention, treatment and recovery: Engage the family. Journal of Addiction Medicine, 11(5), 339–341. [DOI] [PubMed] [Google Scholar]
- Volkow ND, Koob GF, & McLellan AT (2016). Neurobiologic advances from the brain disease model of addiction. New England Journal of Medicine, 374(4), 363–371. 10.1056/NEJMra1511480 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wakeman SE (2013). Language and addiction: Choosing words wisely. American Journal of Public Health, 103(4), 1–2. 10.2105/AJPH.2012.301191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wakeman SE, & Rich JD (2018). Barriers to medications for addiction treatment: How stigma kills. Substance Use & Misuse, 53(2), 330–333. 10.1080/10826084.2017.1363238 [DOI] [PubMed] [Google Scholar]
- Williams AR, Nunes EV, Bisaga A, Levin FR, Robin A, Nunes EV, & Levin FR (2019). Development of a cascade of care for responding to the opioid epidemic. The American Journal of Drug and Alcohol Abuse, 45(1), 1–10. 10.1080/00952990.2018.1546862 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson N, Karissa M, Puja S, Smith H, & Davis NL (2020). Drug and opioid-involved overdose deaths: United States, 2017 – 2018. Morbidity and Mortality Weekly Report, 69(11), 290–297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang L, Wong LY, Grivel MM, & Hasin DS (2018). Stigma and substance use disorders: An international phenomenon. Current Opinions in Psychiatry, 30(5), 378–388. 10.1097/YCO.0000000000000351 [DOI] [PMC free article] [PubMed] [Google Scholar]


