Abstract
Individuals involved with the US criminal justice system have high rates of opioid use disorder (OUD) but face significant barriers to evidence-based treatment. Using 2008–17 data from the Treatment Episode Data Set–Admissions, we examined trends in receipt of medications for OUD among individuals referred by criminal justice agencies and other sources both before and after Medicaid expansion. Individuals referred by criminal justice agencies were less likely to receive medications for OUD than were those referred by other sources during our study period, although this disparity narrowed slightly after Medicaid expansion. Receipt of medications for OUD increased more for individuals referred by criminal justice agencies in states that expanded Medicaid compared with those in states that did not. Medicaid expansion may improve evidence-based treatment for individuals with criminal justice involvement and OUD, although additional policy change outside the health care sector is likely needed to reduce persistent treatment disparities.
Approximately 6.5 million people are under correctional supervision in the US on any given day.1 Individuals currently or recently in prison or jail, on probation or parole, or recently arrested are often referred to as “justice involved,” and they experience higher rates of substance use disorders than the general population.2 Approximately 60 percent of adults in US prisons and jails have a substance use disorder, and 40 percent were using drugs at the time of committing the offense for which they were incarcerated.3 The high proportion of individuals in prisons and jails with substance use disorder indicates that there is likely a high prevalence of opioid use disorder (OUD) in this population. In fact, among people with OUD, more than half have reported contact with the criminal justice system.3,4
Numerous clinical studies and randomized clinical trials have shown that medications for OUD lead to superior outcomes for retention in treatment, reduced illicit opioid use, and decreased opioid-related overdose rates and serious acute care use compared with treatment modalities that rely on psychosocial interventions alone.5–7 Despite the proven efficacy of medications for OUD, treatment of the disorder among individuals with recent criminal justice involvement has been inadequate because of stigma, health insurance termination during incarceration, and limited access to coverage and services after release.8,9 One study found that only 4.6 percent of justice-referred individuals with OUD received treatment with medications.10 Individuals with criminal justice involvement also face many competing priorities, including lack of employment, housing, and transportation, which further complicates treatment retention and completion.11–13
Medicaid expansion through the Affordable Care Act (ACA) was expected to provide coverage for at least half of justice-involved individuals and to improve access to mental health and substance use treatment. One study found that “following Medicaid expansion, uninsurance declined among justice-involved individuals of all ages by 9.7 percentage points…but remained 16.3 percentage points higher than uninsurance rates for individuals without justice involvement.”14(p1523) In addition, admissions to treatment for OUD have increased in Medicaid expansion states compared with nonexpansion states,15–18 with one study reporting an increase of 18 percentage points.15 Although there is evidence that Medicaid expansion improved access to medications for OUD among small subpopulations of individuals with criminal justice involvement (for example, pregnant women), its impact on the receipt of medications for OUD among the overall population of individuals with criminal justice involvement has not been examined.19 Further, understanding differential trends by service location (ambulatory versus residential) and race/ethnicity among individuals involved with the criminal justice system could help identify key areas for improvement and policy development, but these trends have not been well described.
The goal of this study was to examine changes over time in receipt of medications for OUD among individuals who were referred for treatment by criminal justice agencies in states that did and did not expand Medicaid and to compare these trends with changes among individuals referred by other sources. We also examined differences before and after Medicaid expansion by service location (ambulatory versus residential treatment) and by race/ethnicity among individuals with criminal justice involvement. We hypothesized that individuals referred by criminal justice agencies in states that expanded Medicaid would have higher rates of receiving medications for OUD after the implementation of the ACA compared with individuals living in states that did not expand Medicaid and that this difference would be observed across all service locations and racial/ethnic groups.
Study Data And Methods
DATA SOURCE AND SAMPLE
We used ten years (2008–17) of data from the Treatment Episode Data Set–Admissions (TEDS-A), a national survey of substance treatment facility admissions conducted by the Substance Abuse and Mental Health Services Administration (SAMHSA). Substance use treatment programs that receive public funding are required to report their admissions to the state in which they operate. States then report these data from their state administrative systems to SAMHSA. Most individuals involved with the criminal justice system have low incomes and are eligible to receive publicly funded treatment. Thus, most referrals from the criminal justice system are likely captured in this data set, although empirical validation is not available because other national data sources of criminal justice referrals do not exist. Because the unit of analysis within TEDS-A is a treatment admission, not an individual, some individuals may be represented more than once. Initial admissions to each center are included; transfers between facilities are excluded. TEDS-A contains records on admissions of patients age twelve or older and includes information on admission demographics and substance use characteristics.
TEDS-A includes information about primary, secondary, and tertiary substances that led to a treatment admission. We restricted the sample to individuals whose primary reason for treatment was related to opioid use (heroin, nonprescription methadone, and other synthetic opioids) and who were age eighteen or older. SAMHSA staff informed us that reporting changes in Florida between 2010 and 2017 made it difficult to compare data across years, so we excluded Florida from the sample (Carol Place, communications director, Substance Abuse and Mental Health Data Archive, personal communication, September 24, 2019).
In addition, we excluded admissions to detoxification centers, as detoxification is not evidence-based treatment for OUD.10,20,21 Of the remaining sample, 4.4 percent had missing data for the referral source variable or key outcome variable and were subsequently excluded.
KEY INDEPENDENT VARIABLE: TREATMENT REFERRAL SOURCES
We examined longitudinal trends in receipt of medications for OUD by referral source to substance use treatment. A referral source was defined as the agency or person referring an individual to treatment. We classified referrals into two categories: criminal justice agency referrals and other/non–criminal justice referrals. Criminal justice referrals included referrals from the police, probation officers, judges, prosecutors, driving under the influence/driving while intoxicated courts, and parole boards. Other referrals included all other referrals including those from individuals (initiated by the patient, a family member, a friend, or another person), providers (alcohol or drug use treatment provider or health care provider), schools, employers, and community referrals.
KEY DEPENDENT VARIABLE: RECEIPT OF MEDICATIONS FOR OPIOID USE DISORDER
Our primary outcome measure was a flag indicating that medications for OUD—specifically, the opioid agonist medications methadone or buprenorphine—were part of the treatment plan during the admission. TEDS-A data do not distinguish between medications, and naltrexone, an opioid antagonist, was added to the flag starting in 2016. Treatment episodes for OUD that do not include medications for OUD include symptomatic management of withdrawal symptoms; individual, family, or group therapy services; and transitional housing.
SOCIODEMOGRAPHIC CHARACTERISTICS
We assessed age, race/ethnicity, employment status, sex, educational attainment, service setting, and region by referral source. We controlled for these characteristics in multivariable models to assess trends in receipt of treatment by year.
STATISTICAL ANALYSIS
We first assessed the sociodemographic characteristics and service settings of our study population by referral source (that is, criminal justice and non–criminal justice) between 2008 and 2017. Next, we examined the number of individuals with a primary diagnosis of OUD referred by criminal justice agencies or other sources who received medications for OUD during each year of our study period. We then used multivariable logistic regression models to estimate receipt of medications for OUD by referral source overall and in each study year, adjusting for covariates. We used postestimation predictive margins with covariates held at observed sample values to depict and compare adjusted probabilities between referral sources across years.22
Finally, we examined changes in receipt of medications for OUD among individuals referred by criminal justice agencies and other sources by state Medicaid expansion status between 2008 and 2017. We first described unadjusted trends by expansion status. Next, we used a standard difference-in-differences approach to compare changes in receipt of medications for OUD among people who lived in states that did and did not expand Medicaid. Difference-in-differences is a quasi-experimental approach that compares changes in outcomes over time between a population that is affected by a policy change (treatment group) with changes in a population that is not (control group). The approach allows for estimation of the treatment effect in the treated and accounts for unobservable differences between the treatment and control groups, as well as for secular trends.23,24 This method allowed us to isolate the change in receipt of medications for OUD that was associated with Medicaid expansion after accounting for changes that would have occurred in the absence of Medicaid expansion. We also stratified our regression model by race/ethnicity and service setting for criminal justice referrals and other referrals, resulting in fourteen difference-in-differences models (see the online appendix for additional details).25
LIMITATIONS
A limitation of this study was that the publicly available TEDS-A data do not differentiate between receipt of buprenorphine and methadone (or naltrexone in 2016 and 2017), so comparisons between these different modalities was not possible. Further, because the variable indicating the payer (expected or actual) of the admission was missing for the majority of observations, we could not control for insurance status or payer in our models. In addition, the data set did not capture buprenorphine received in a health care provider’s office or clinic, which accounts for a significant portion of buprenorphine treatment. The findings of this study might not be generalizable to settings excluded from the TEDS-A database, including office-based and mobile buprenorphine clinics. Finally, our results are limited to people referred to treatment and likely underestimate the criminal justice population with OUD, because many might not be referred to treatment.
Study Results
We identified a total of 3,209,691 adults with OUD between 2008 and 2017. Of these, 674,744 (21.0 percent) were referred by a criminal justice agency, and 2,534,947 (79.0 percent) had another referral source.
As shown in exhibit 1, individuals with criminal justice referral were younger than those with another referral source (ages 18–24: 23.4 percent versus 17.9 percent, respectively), more likely to be non-Hispanic White (64.6 percent versus 60.7 percent), and slightly more likely to receive treatment in a residential setting (26.0 percent versus 23.8 percent). Compared with other referrals, criminal justice referrals were more likely to have lower educational attainment (some college or more: 21.0 percent versus 24.8 percent).
EXHIBIT 1.
Demographic characteristics of individuals in the US with opioid use disorder referred to treatment, by treatment referral source, 2008–17
| Demographic variables | Criminal justice referral (n = 674,744) |
Other referral (n = 2,534,947) |
|---|---|---|
| Age, years | ||
| 18–24 | 23.4% | 17.9% |
| 25–39 | 55.3 | 51.0 |
| 40–54 | 18.2 | 23.6 |
| 55+ | 3.1 | 7.5 |
| Race/ethnicity | ||
| Non-Hispanic White | 64.6 | 60.7 |
| Non-Hispanic Black | 9.6 | 12.1 |
| Hispanic | 14.7 | 14.3 |
| Native American/Alaska Native | 1.6 | 1.5 |
| Other | 8.7 | 10.3 |
| Education | ||
| Less than high school | 29.4 | 27.0 |
| High school complete | 47.8 | 45.2 |
| Some college or more | 21.0 | 24.8 |
| Employment | ||
| Not employed | 78.4 | 80.9 |
| Employed | 21.6 | 19.1 |
| Census region | ||
| Northeast | 40.0 | 42.8 |
| Midwest | 20.5 | 17.5 |
| South | 20.3 | 22.6 |
| West | 19.2 | 17.1 |
| Service setting | ||
| Residential | 26.0 | 23.8 |
| Ambulatory | 74.0 | 76.2 |
SOURCE Authors’ analysis of information for 2008–17 from the Treatment Episode Data Set–Admissions, Substance Abuse and Mental Health Services Administration. NOTE Criminal justice includes referral from police, probation officers, judges, prosecutors, driving under the influence/driving while impaired court, or parole board.
TREATMENT REFERRAL SOURCE
The proportion of people with OUD receiving medications for OUD as a part of their treatment increased substantially between 2008 and 2017 across all referral sources (exhibit 2). Among people with OUD referred by a criminal justice agency, the adjusted proportion of people receiving medications for OUD increased from 6.3 percent in 2008 to 16.5 percent in 2017. Among non–criminal justice referrals, the adjusted proportion of people receiving medications for OUD increased from 40.8 percent in 2008 to 51.2 percent in 2017. Linear time trends for each referral source were statistically significant (p < 0:001).
EXHIBIT 2. Adjusted proportion of individuals in the US receiving medications for opioid use disorder, by referral source, 2008–17.
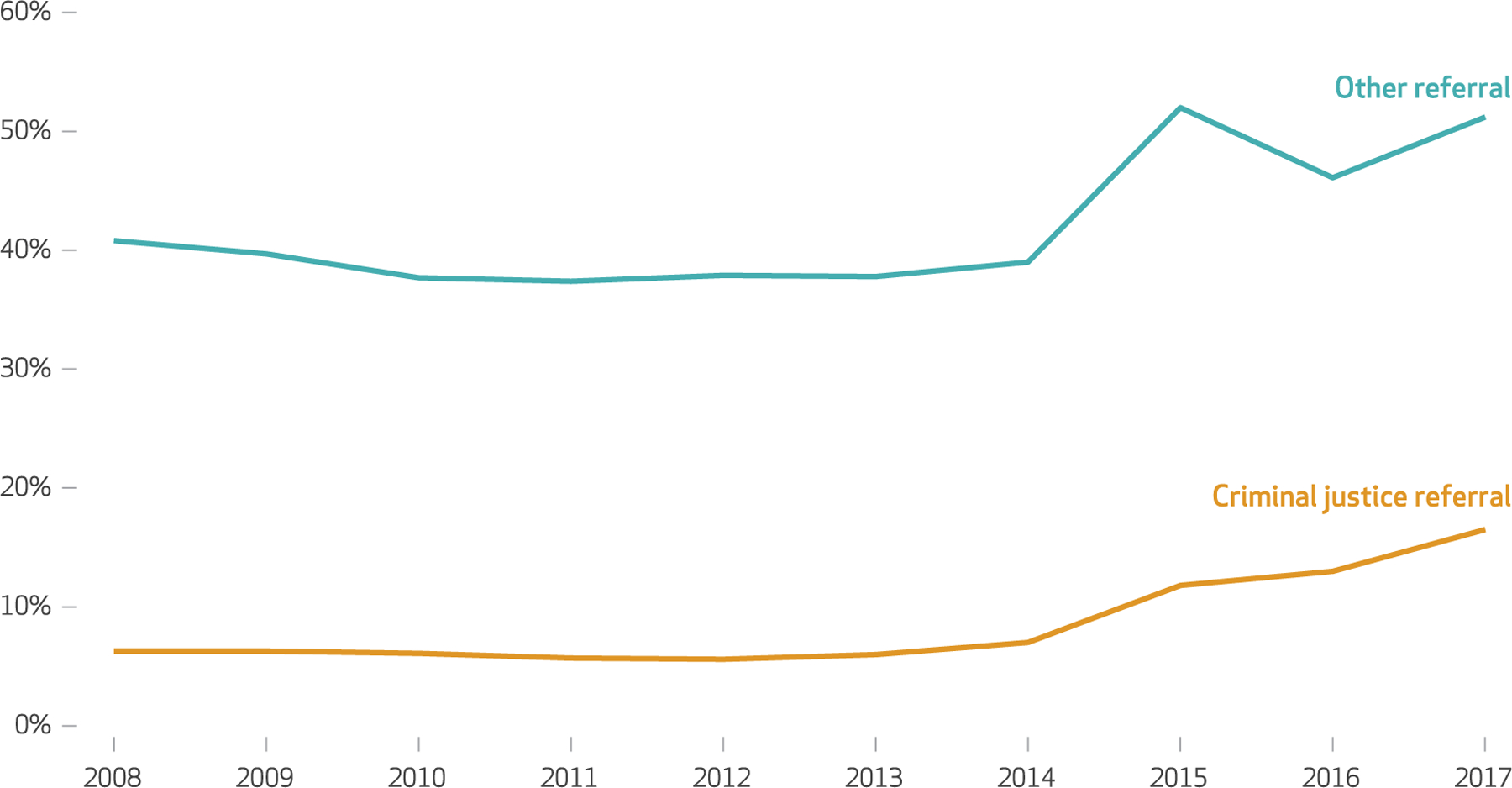
SOURCE Authors’ analysis of information for 2008–17 from the Treatment Episode Data Set–Admissions, Substance Abuse and Mental Health Services Administration. NOTE Adjusted for age, race/ethnicity, educational attainment, employment, census region, service setting, and sex.
As shown in exhibit 2, during the study period, individuals referred for treatment by the criminal justice system were substantially less likely to receive medications for OUD as part of the treatment plan when compared with those referred through all other sources (adjusted risk ratio: 0.21; 95% confidence interval: 0.21, 0.21). This difference was observed in the years before (2008–13) and after (2015–17) the passage of the ACA (pre-ACA ARR: 0.15 [95% CI: 0.15, 0.16]; post-ACA ARR: 0.28 [95% CI: 0.28, 0.28]). Adjusted risk ratios in the two periods were significantly different (p < 0:001).
STATE MEDICAID EXPANSION STATUS
We examined changes in receipt of medications for OUD among individuals with OUD referred by criminal justice agencies or other sources in states that did and did not expand Medicaid through the ACA (exhibit 3). In both Medicaid expansion and nonexpansion states, rates of medications for OUD were relatively consistent between 2008 and 2013 across referral sources. Among individuals referred by criminal justice agencies, those in Medicaid expansion states had higher rates of medications for OUD receipt than those in nonexpansion states during the entire study period, 2008–17 (ARR: 2.07; 95% CI, 2.00, 2.13). Among other referrals, Medicaid expansion states also saw higher rates of receipt of medications for OUD receipt during the entire study period (ARR: 1.60; 95% CI: 1.59, 1.61).
EXHIBIT 3. Proportion of individuals in the US with opioid use disorder receiving medications for opioid use disorder, by referral source and state Medicaid expansion status, 2008–17.
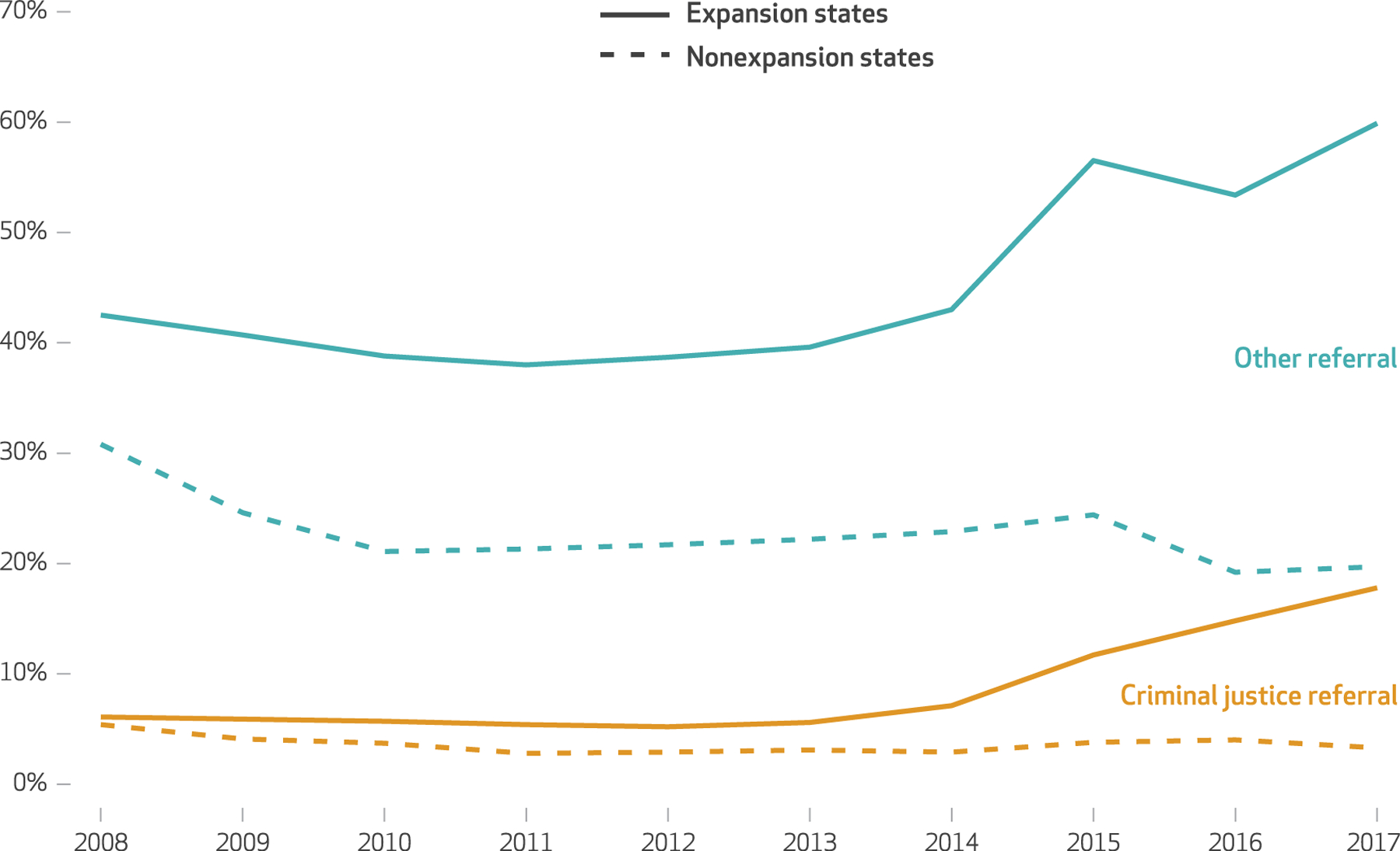
SOURCE Authors’ analysis of information for 2008–17 from the Treatment Episode Data Set–Admissions, Substance Abuse and Mental Health Services Administration, linked to data on years of adoption of the Medicaid expansion. NOTE Unadjusted proportions.
Exhibit 3 provides visual confirmation that unadjusted trends in receipt of medications for OUD in states that did and did not expand Medicaid for criminal justice referrals and other referrals, respectively, were parallel within each referral source before policy implementation (2008–13). In addition, we tested the trends in pre-ACA rates of medications for OUD receipt among criminal justice referrals and other referrals and found that they did not vary significantly by expansion status (adjusted odds ratio of interaction term for criminal justice referrals: 1.10 [95% CI: 0.94, 1.30; p = 0:23]; AOR for other referrals: 1.06 [95% CI: 0.98, 1.15; p = 0:16]).
Between 2008–13 and 2015–17, receipt of medications for OUD increased to a greater degree among individuals referred by the criminal justice agencies in states that expanded Medicaid compared with such individuals in states that did not expand Medicaid (unadjusted difference-in-differences estimate: 9.4 percentage points; 95% CI: 9.1, 9.7) (data not shown), and this difference remained significant after adjustment for covariates (adjusted DID estimate: 8.6 percentage points; 95% CI: 2.2, 15.0) (exhibit 4). Among individuals referred by other sources, those living in states that expanded Medicaid had greater receipt of medications compared with those living in states that did not expand Medicaid (unadjusted DID estimate: 20.4 percentage points; 95% CI: 20.1, 20.8) (data not shown), and this difference remained significant after adjustment for covariates (adjusted DID estimate: 16.5 percentage points; 95% CI: 6.2, 26.8) (exhibit 4). The difference-in-differences estimates for criminal justice referrals and other referrals were significantly different (−7.3 percentage points; 95% CI: −13.2, −1.5; p = 0.01) (data not shown).
EXHIBIT 4.
Adjusted rates of medications for opioid use disorder for individuals in the US referred to treatment in Medicaid expansion and nonexpansion states, by treatment referral source, 2008–17
| (1) Pre-ACAa |
(2) Post-ACAa |
Difference (2–1)a |
DIDa | ||||
|---|---|---|---|---|---|---|---|
| Expansion | Nonexpansion | Expansion | Nonexpansion | Expansion | Nonexpansion | ||
| CRIMINAL JUSTICE REFERRALS | |||||||
| All | 5.5 | 4.2 | 14.5 | 4.6 | 9.0 | 0.4 | 8.6*** |
| Race/ethnicity | |||||||
| Non-Hispanic White | 5.0 | 4.2 | 15.0 | 4.3 | 10.0 | 0.1 | 9.8*** |
| Non-Hispanic Black | 6.7 | 3.9 | 12.7 | 3.4 | 6.0 | −0.5 | 6.5** |
| Hispanic | 5.6 | 2.6 | 13.6 | 5.2 | 8.0 | 2.6 | 5.4 |
| Native American/Alaska Native | 5.7 | 4.2 | 12.3 | 4.9 | 6.6 | 0.7 | 5.9*** |
| Other race | 7.8 | 5.8 | 16.5 | 5.3 | 8.6 | −0.5 | 9.1 |
| Service setting | |||||||
| Ambulatory | 6.4 | 5.0 | 16.0 | 5.2 | 9.7 | 0.2 | 9.5*** |
| Residential | 3.2 | 1.6 | 10.4 | 2.9 | 7.2 | 1.3 | 5.9 |
| OTHER REFERRALS | |||||||
| All | 39.5 | 29.7 | 53.1 | 26.8 | 13.6 | −2.9 | 16.5*** |
| Race/ethnicity | |||||||
| Non-Hispanic White | 35.5 | 26.0 | 50.8 | 24.6 | 15.4 | −1.4 | 16.8*** |
| Non-Hispanic Black | 46.1 | 31.7 | 59.5 | 27.9 | 13.4 | −3.7 | 17.1**** |
| Hispanic | 47.2 | 38.7 | 52.9 | 26.8 | 5.7 | −11.9 | 17.6** |
| Native American/Alaskan Native | 39.4 | 31.3 | 51.3 | 25.0 | 12.0 | −6.3 | 18.2** |
| Other race | 51.8 | 45.6 | 62.3 | 28.6 | 10.4 | −17.0 | 27.5** |
| Service setting | |||||||
| Ambulatory | 50.5 | 38.0 | 63.5 | 33.9 | 13.0 | −4.1 | 17.1*** |
| Residential | 6.7 | 4.4 | 20.6 | 6.5 | 14.0 | 2.1 | 11.8** |
SOURCE Authors’ analysis of information for 2008–17 from the Treatment Episode Data Set–Admissions, Substance Abuse and Mental Health Services Administration, linked to data on years of adoption of the Medicaid expansion. NOTES For all states, “pre-ACA” is 2008–13. For nonexpansion states, “post-ACA” is 2015–17. For expansion states, the post-ACA period begins the year after Medicaid expansion was adopted by the individual state, which was 2015 for most expansion states. ACA is Affordable Care Act. DID is difference-in-differences estimate.
Percentage points.
p < 0:05
p < 0:01
p < 0:001
Exhibit 4 also presents results from our stratified analyses. Among individuals referred by criminal justice agencies, receipt of medications for OUD increased significantly in states that expanded Medicaid compared with states that did not for White non-Hispanic, Black non-Hispanic, and Native American/Alaska Native populations, as did admissions to ambulatory treatment centers. Among individuals with other referral sources, the receipt of medications for OUD increased significantly in states that expanded Medicaid compared with states that did not for all racial/ethnic subgroups and for both ambulatory and residential settings. Additional details about our stratified results are in the appendix.25 Last, our results did not vary substantively in our sensitivity analyses. Additional details are in the appendix.25
Discussion
In this analysis of national substance use treatment data during the period 2008–17, we found that individuals with OUD referred for treatment by US criminal justice agencies were less likely to receive medications for OUD than individuals referred by other sources, both before and after the ACA enabled Medicaid expansion. Furthermore, we found that receipt of medications for OUD, regardless of referral source, increased over time by a greater extent in states that expanded Medicaid compared with states that did not. For individuals referred by a criminal justice agency, specifically, use of medications for OUD rose by 165 percent in states that expanded Medicaid after trends in states that did not expand Medicaid are accounted for. Although this represents a large relative increase in receipt of medications for OUD among the justice-referred population, there was a significantly larger absolute difference among those referred from other sources.
In previous work, Medicaid expansion was associated with an increase in insurance access among justice-involved individuals.14 These individuals, when they have insurance, increase the use of all types of care, including outpatient care, emergency department care, and overnight hospitalizations.26 Medicaid coverage has been associated in particular with higher rates of substance use treatment compared with other types of coverage for justice-involved individuals.14 When considered with these previous findings, our results indicating that Medicaid expansion was associated with increased receipt of medications for OUD among individuals referred to treatment through criminal justice agencies further demonstrate that on a broad level, public health insurance programs can address the unique health care challenges faced by individuals affected by the criminal justice system. Furthermore, our results reinforce that expanding Medicaid coverage eligibility should be a focus of policy makers looking to improve access to substance use disorder treatment among criminal justice–involved populations to remediate the high rate of fatal overdoses among them.27–29
In our stratified analyses we found that increases in the receipt of medications for OUD associated with Medicaid expansion persisted across racial/ethnic groups and service setting locations (ambulatory versus residential), although the differences did not achieve statistical significance among the Hispanic and “other race” group or in the residential treatment setting, likely as a result of smaller sample sizes. Medicaid expansion, therefore, has an important role in increasing access to medications for OUD for members of racial/ethnic minority groups, who are subject to racist drug policies and endure the consequences of disparate enforcement of drug laws despite similar rates of drug use as White individuals.30,31
Of note, most individuals in our justice-referred OUD cohort were White, which is in stark contrast to the population of individuals in the criminal justice system at large, which grossly overrepresents members of racial minority groups, and particularly Black individuals.32,33 This discrepancy can be partially explained by the higher prevalence of OUD in White communities, although opioid use disorder prevalence has been increasing in racial/ethnic minority groups.34–36 In addition, it is possible that White individuals with OUD may be more likely than individuals from other racial/ethnic groups with OUD to be referred to treatment by criminal justice agencies and thus may be overrepresented in the TEDS-A database.
Ambulatory treatment settings were significantly associated with higher rates of medications for OUD in expansion states compared with nonexpansion states. In nonexpansion states with large community supervision populations, Medicaid expansion could improve access to evidence-based treatment through ambulatory settings and could offset a need to increase residential treatment facilities, which often have limited capacity and may be overly restrictive for some people.37,38
Our findings that Medicaid expansion is associated with substantial improvements in access to medications for OUD for individuals referred by criminal justice agencies should be placed in the context of the abundance of data that consistently show that the receipt of methadone or buprenorphine is associated with reduced risk for overdose and opioid-related morbidity and mortality when compared with other treatment modalities, such as opioid antagonist therapy, abstinence-only approaches, or behavioral interventions.7,34,39 Medicaid expansion therefore could play a role in decreasing overdose risk and opioid-related morbidity in justice-involved individuals.
Unfortunately, despite improvements in access to medications for OUD among individuals referred by criminal justice agencies, we found that in absolute terms, this improvement lagged the improvement in access to medications for OUD among individuals referred from other sources in Medicaid expansion states. Although Medicaid expansion can improve coverage of medications for OUD, policies within criminal justice agencies and practices within treatment facilities may limit the possible impact. For example, Medicaid cannot alter the referral patterns of criminal justice agencies that prefer treatment facilities that do not offer medication for OUD, nor can it influence policy within departments of probation or drug courts that may prioritize treatment plans that do not include medication for OUD. Medicaid also cannot ensure that treatment facilities offering medications for OUD are geographically located in areas that are easily accessible to individuals with justice involvement. In addition, incarceration-related stigma may also influence the treatment plans offered by treatment facilities and providers to individuals referred by criminal justice agencies.
Disruptions in health insurance coverage during reentry that result from Medicaid’s inmate exclusion policy also remain problematic.40 In a 2018 survey, fourteen states reported terminating Medicaid coverage upon incarceration, in compliance with federal regulations, which creates a gap in insurance access upon release. Alternatively, thirty-six states chose to suspend coverage, which could improve the ease of reinstituting Medicaid upon release from incarceration, although it does not eliminate all barriers to Medicaid coverage.35,41 Undisrupted access to health insurance should be included as a critical component of treatment models that aim to improve access and retention to medications for OUD for individuals with criminal justice involvement. Policies that mandate and operationalize suspension of Medicaid coverage upon incarceration, rather than termination, in tandem with more programs that identify and enroll eligible individuals before release, may facilitate immediate insurance coverage upon release and reduce barriers to accessing medications for OUD. Access to insurance has also been associated with reductions in alcohol and tobacco use among justice-involved individuals, although reductions in other substance use have not been seen.36 The growing gap in receipt of medications for OUD between individuals referred from criminal justice agencies and individuals from other referral sources represents a missed opportunity to affect the morbidity, mortality, and criminal justice–related outcomes of a marginalized population.
Conclusion
Individuals with OUD referred to treatment by criminal justice agencies between 2008 and 2017 were less likely to receive medications for OUD than individuals referred through other sources. Medicaid expansion through the ACA was associated with a significant increase in the receipt of medications for OUD among individuals referred by criminal justice agencies. Medicaid expansion has the potential to improve outcomes for individuals with criminal justice involvement and OUD, although Medicaid policy alone might not fully close disparities in medications for OUD between individuals with and without criminal justice involvement. ▪
Supplementary Material
Acknowledgments
Preliminary results were presented at the National Clinicians Scholars Program Annual Meeting (virtual), October 20–22, 2020. Utsha Khatri’s position is funded by the Department of Veterans Affairs (VA) at the Corporal Michael J. Crescenz VA Medical Center. Benjamin Howell receives funding from the National Institute on Drug Abuse via Grant No. 5K12DA033312. The views reflected in this article are those of the authors and do not reflect the position or policy of the Department of Veterans Affairs or the United States government.
Contributor Information
Utsha G. Khatri, National Clinician Scholars Program with the Corporal Michael J. Crescenz Veterans Affairs Medical Center and Perelman School of Medicine at the University of Pennsylvania, in Philadelphia, Pennsylvania..
Benjamin A. Howell, section of General Internal Medicine and the SEICHE Center at Yale School of Medicine, in New Haven, Connecticut..
Tyler N. A. Winkelman, Division of General Internal Medicine, Department of Medicine, Hennepin Healthcare, and the codirector of the Health, Homelessness, and Criminal Justice Lab, Hennepin Healthcare Research Institute, both in Minneapolis, Minnesota..
NOTES
- 1.Kaeble D, Cowhig M. Correctional populations in the United States, 2016 [Internet] Washington (DC): Department of Justice, Bureau of Justice Statistics; 2018. April 26 [cited 2021 Jan 21]. Available from: https://www.bjs.gov/index.cfm?ty=pbdetail&iid=6226 [Google Scholar]
- 2.Massoglia M, Pridemore WA. Incarceration and health. Annu Rev Sociol 2015;41(1):291–310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bronson J, Stroop J, Zimmer S, Berzofsky M. Drug use, dependence, and abuse among state prisoners and jail inmates, 2007–2009 [Internet] Washington (DC): Department of Justice, Bureau of Justice Statistics; 2017. June [cited 2021 Jan 21]. Available from: https://www.bjs.gov/content/pub/pdf/dudaspji0709.pdf [Google Scholar]
- 4.Winkelman TNA, Chang VW, Binswanger IA. Health, polysubstance use, and criminal justice involvement among adults with varying levels of opioid use. JAMA Netw Open 2018;1(3):e180558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Caldiero RM, Parran TV Jr, Adelman CL, Piche B. Inpatient initiation of buprenorphine maintenance vs. detoxification: can retention of opioid-dependent patients in outpatient counseling be improved? Am J Addict 2006;15(1):1–7. [DOI] [PubMed] [Google Scholar]
- 6.Mattick RP, Kimber J, Breen C, Davoli M. Buprenorphine maintenance versus placebo or methadone maintenance for opioid dependence. Cochrane Database Syst Rev 2008;(2):CD002207. [DOI] [PubMed] [Google Scholar]
- 7.Wakeman SE, Larochelle MR, Ameli O, Chaisson CE, McPheeters JT, Crown WH, et al. Comparative effectiveness of different treatment pathways for opioid use disorder. JAMA Netw Open 2020;3(2): e1920622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Frank JW, Linder JA, Becker WC, Fiellin DA, Wang EA. Increased hospital and emergency department utilization by individuals with recent criminal justice involvement: results of a national survey. J Gen Intern Med 2014;29(9):1226–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cuellar AE, Cheema J. As roughly 700,000 prisoners are released annually, about half will gain health coverage and care under federal laws. Health Aff (Millwood) 2012; 31(5):931–8. [DOI] [PubMed] [Google Scholar]
- 10.Krawczyk N, Picher CE, Feder KA, Saloner B. Only one in twenty justice-referred adults in specialty treatment for opioid use receive methadone or buprenorphine. Health Aff (Millwood) 2017; 36(12):2046–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Couloute L Nowhere to go: homelessness among formerly incarcerated people [Internet] Easthampton (MA): Prison Policy Initiative; 2018. August [cited 2021 Jan 21]. Available from: https://www.prisonpolicy.org/reports/housing.html [Google Scholar]
- 12.Dong KR, Must A, Tang AM, Beckwith CG, Stopka TJ. Competing priorities that rival health in adults on probation in Rhode Island: substance use recovery, employment, housing, and food intake. BMC Public Health 2018;18(1):289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sugarman OK, Bachhuber MA, Wennerstrom A, Bruno T, Springgate BF. Interventions for incarcerated adults with opioid use disorder in the United States: a systematic review with a focus on social determinants of health. PLoS One 2020;15(1):e0227968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Winkelman TN, Kieffer EC, Goold SD, Morenoff JD, Cross K, Ayanian JZ. Health insurance trends and access to behavioral healthcare among justice-involved individuals—United States, 2008–2014. J Gen Intern Med 2016;31(12):1523–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Meinhofer A, Witman AE. The role of health insurance on treatment for opioid use disorders: evidence from the Affordable Care Act Medicaid expansion. J Health Econ 2018; 60:177–97. [DOI] [PubMed] [Google Scholar]
- 16.Wen H, Hockenberry JM, Borders TF, Druss BG. Impact of Medicaid expansion on Medicaid-covered utilization of buprenorphine for opioid use disorder treatment. Med Care 2017;55(4):336–41. [DOI] [PubMed] [Google Scholar]
- 17.Sharp A, Jones A, Sherwood J, Kutsa O, Honermann B, Millett G. Impact of Medicaid expansion on access to opioid analgesic medications and medication-assisted treatment. Am J Public Health 2018;108(5):642–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Saloner B, Maclean JC. Specialty substance use disorder treatment admissions steadily increased in the four years after Medicaid expansion. Health Aff (Millwood) 2020;39(3): 453–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Winkelman TNA, Ford BR, Shlafer RJ, McWilliams A, Admon LK, Patrick SW. Medications for opioid use disorder among pregnant women referred by criminal justice agencies before and after Medicaid expansion: a retrospective study of admissions to treatment centers in the United States. PLoS Med 2020; 17(5):e1003119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sees KL, Delucchi KL, Masson C, Rosen A, Clark HW, Robillard H, et al. Methadone maintenance vs 180-day psychosocially enriched detoxification for treatment of opioid dependence: a randomized controlled trial. JAMA 2000;283(10): 1303–10. [DOI] [PubMed] [Google Scholar]
- 21.Mojtabai R, Mauro C, Wall MM, Barry CL, Olfson M. The Affordable Care Act and opioid agonist therapy for opioid use disorder. Psychiatr Serv 2019;70(7):617–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Norton EC, Dowd BE, Maciejewski ML. Marginal effects—quantifying the effect of changes in risk factors in logistic regression models. JAMA 2019;321(13):1304–5. [DOI] [PubMed] [Google Scholar]
- 23.Dimick JB, Ryan AM. Methods for evaluating changes in health care policy: the difference-in-differences approach. JAMA 2014;312(22): 2401–2. [DOI] [PubMed] [Google Scholar]
- 24.Ryan AM, Burgess JF Jr, Dimick JB. Why we should not be indifferent to specification choices for difference-in-differences. Health Serv Res 2015;50(4):1211–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. To access the appendix, click on the Details tab of the article online.
- 26.Farrell CM, Gottlieb A. The effect of health insurance on health care utilization in the justice-involved population: United States, 2014–2016. Am J Public Health 2020;110(S1): S78–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Binswanger IA, Blatchford PJ, Mueller SR, Stern MF. Mortality after prison release: opioid overdose and other causes of death, risk factors, and time trends from 1999 to 2009. Ann Intern Med 2013;159(9): 592–600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ranapurwala SI, Shanahan ME, Alexandridis AA, Proescholdbell SK, Naumann RB, Edwards D Jr, et al. Opioid overdose mortality among former North Carolina inmates: 2000–2015. Am J Public Health 2018;108(9):1207–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pizzicato LN, Drake R, Domer-Shank R, Johnson CC, Viner KM. Beyond the walls: risk factors for overdose mortality following release from the Philadelphia Department of Prisons. Drug Alcohol Depend 2018;189:108–15. [DOI] [PubMed] [Google Scholar]
- 30.Netherland J, Hansen HB. The war on drugs that wasn’t: wasted Whiteness, “dirty doctors,” and race in media coverage of prescription opioid misuse. Cult Med Psychiatry 2016;40(4):664–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.James K, Jordan A. The opioid crisis in black communities. J Law Med Ethics 2018;46(2):404–21. [DOI] [PubMed] [Google Scholar]
- 32.Hinton E, Cook D. The mass criminalization of Black Americans: a historical overview. Annu Rev Criminol 2020;4:261–86. [Google Scholar]
- 33.Roberts DE. The social and moral cost of mass incarceration in African American communities. Stanford Law Rev 2004;56(5):1271–305. [Google Scholar]
- 34.National Academies of Sciences, Engineering, and Medicine. Medications for opioid use disorder save lives Washington (DC): National Academies Press; 2019. [PubMed] [Google Scholar]
- 35.Fiscella K, Beletsky L, Wakeman SE. The inmate exception and reform of correctional health care. Am J Public Health 2017;107(3):384–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gottlieb A, McLeod BA, Barutell KF. The impact of health insurance on problematic substance use among justice-involved individuals. J Offender Rehabil 2020;59(2):81–97. [Google Scholar]
- 37.Yang Y, Perkins DR, Stearns AE. Barriers and facilitators to treatment engagement among clients in inpatient substance abuse treatment. Qual Health Res 2018;28(9): 1474–85. [DOI] [PubMed] [Google Scholar]
- 38.Huhn AS, Hobelmann JG, Strickland JC, Oyler GA, Bergeria CL, Umbricht A, et al. Differences in availability and use of medications for opioid use disorder in residential treatment settings in the United States. JAMA Netw Open 2020;3(2):e1920843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Green TC, Clarke J, Brinkley-Rubinstein L, Marshall BDL, Alexander-Scott N, Boss R, et al. Postincarceration fatal overdoses after implementing medications for addiction treatment in a statewide correctional system. JAMA Psychiatry 2018;75(4):405–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Camhi N, Mistak D, Wachino V (Community Oriented Correctional Health Services; Oakland, CA). Medicaid’s evolving role in advancing the health of people involved in the justice system [Internet] New York (NY): Commonwealth Fund; 2020. November 18 [cited 2021 Jan 21]. Available from: https://www.commonwealthfund.org/publications/issue-briefs/2020/nov/medicaid-role-health-people-involved-justice-system [Google Scholar]
- 41.Gifford K, Ellis E, Edwards BC, Lashbrook A, Hinton E, Antonisse L, et al. States focus on quality and outcomes amid waiver changes: results from a 50-state Medicaid budget survey for state fiscal years 2017 and 2018. [Internet] San Francisco (CA): KFF; 2019. [cited 2021 Feb 22]. Available from: http://files.kff.org/attachment/Report-States-Focus-on-Quality-and-Outcomes-Amid-Waiver-Changes-Results-from-a-50-State-Medicaid-Budget-Survey-for-State-Fiscal-Years-2018-and-2019 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


