Our previous 12-year (1998–2009) analysis from the highest volume national academic department (Neurosurgery, Evangelismos Hospital, Greece) provided hospitalization times and in-hospital mortality (IHM) rates on adult CNS tumors patients.[6] Our study indicated relatively high estimates for both parameters that were similar to those from low-volume US centers.[6]
Based on the same tumor registry (ECTR[6]), we have recently conducted analogous analysis on newly diagnosed CNS tumor patients, covering the period between 2010 and 2018 (n = 1785). This period was marked by a national socioeconomic crisis which was characterized by substantial reductions in health-care spending,[2] an issue that had previously raised concerns over the efficiency and quality of health-care provision in the surgical field.[4]
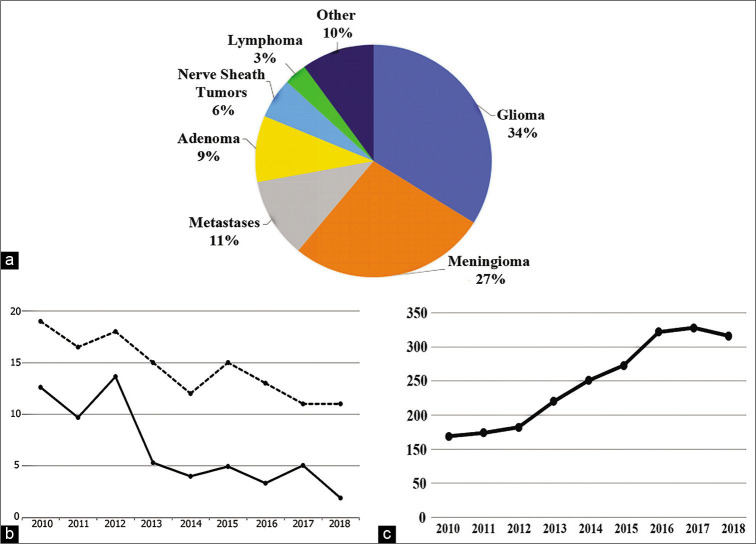
Our recent findings indicate the following trends. The relative frequencies [Figure 1a] of major CNS tumor types do not display substantial (i.e., >5%) differences in comparison to our previous study.[6] Interestingly, while overall IHM rates (5.7%) are largely unaltered and hospitalization times (median: 13 days) are slightly reduced in comparison to our previous analysis, it is noteworthy that both indices display a clear downward trend [Figure 1b], reaching nadirs during the last study year (of 1.9% and 11 days, respectively). At the same time, a steady rise in treated patients across the study period is apparent [Figure 1c]. This rise is likely to reflect increased departmental capacity. In this regard, since 2013, the department operates an academic fellowship program, aimed at improving efficiency and quality of neurosurgical health-care provision and in enhancing academic education, covering up to three placements. It allowed exceptional, newly qualified neurosurgeons as well as those returning from placements abroad, to contribute not only to research activities and resident education but also to surgical practice. It also enabled the recruitment of a departmental neuropsychologist, as well as neuroscientific and administrative personnel in support of a master course in clinical and experimental neurosurgery, now in its fourth 2-year cycle. The course has been attended by one-fifth of departmental residents.
Figure 1:
(a) (Top). Pie chart showing the frequency of major tumor types for the total patient cohort (n = 1785). (b) (Bottom left panel). Annual median length of hospital stay (LOS, days, top dotted line) and mortality rates (%, bottom solid line) across the study period. (c) (Bottom right panel). Annual number of CNS tumor patients (years 2010–2018).
The well-documented relationship between patient volume and outcome may thus, at least partly, explain the observed trends.[1,5] Moreover, previous research indicates that quality improvement programs for surgical trainees can have a substantial impact on patient LOS.[3]
At the time of writing, the Greek health-care system is facing yet more adversity due to the ongoing COVID-19 pandemic. As a corollary, our department has faced significant disruptions to daily operations. The impact of the COVID era on the improving indices of hospital outcome discussed above can be investigated in future analysis.
Footnotes
How to cite this article: Kalamatianos T, Kalyvas A, Komaitis S, Stavridi K, Liouta E, Drosos E, et al. Trends in hospital stay and outcome of CNS tumor patients in Greece during the socioeconomic crisis period (2010–2018): The case of the academic neurosurgical department at Evangelismos Hospital.. Surg Neurol Int 2021;12:211.
Contributor Information
Theodosis Kalamatianos, Email: tkalamatian@med.uoa.gr.
Aristotelis Kalyvas, Email: aristoteliskalyvas@gmail.com.
Spyridon Komaitis, Email: skom.med@gmail.com.
Kleio Stavridi, Email: crtyksl@hotmail.com.
Evangelia Liouta, Email: evangelialiouta286@hotmail.com.
Evangelos Drosos, Email: drosose@gmail.com.
Faidon Liakos, Email: liakosfaidon@gmail.com.
Christos Koutsarnakis, Email: ckouts@hotmail.co.uk.
George Stranjalis, Email: gstranjalis@med.uoa.gr.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Davies JM, Ozpinar A, Lawton MT. Volume-outcome relationships in neurosurgery. Neurosurg Clin N Am. 2015;26:207–18, 8. doi: 10.1016/j.nec.2014.11.015. [DOI] [PubMed] [Google Scholar]
- 2.Global Burden of Disease 2016 Greece Collaborators The burden of disease in Greece, health loss, risk factors and health financing, 2000-16: An analysis of the global burden of disease study 2016. Lancet Public Health. 2018;3:e395–406. doi: 10.1016/S2468-2667(18)30130-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Johnson CE, Peralta J, Lawrence L, Issai A, Weaver FA, Ham SW. Focused resident education and engagement in quality improvement enhances documentation, shortens hospital length of stay, and creates a culture of continuous improvement. J Surg Educ. 2019;76:771–8. doi: 10.1016/j.jsurg.2018.09.016. [DOI] [PubMed] [Google Scholar]
- 4.Karidis NP, Dimitroulis D, Kouraklis G. Global financial crisis and surgical practice: the Greek paradigm. World J Surg. 2011;35:2377–81. doi: 10.1007/s00268-011-1228-y. [DOI] [PubMed] [Google Scholar]
- 5.Ramakrishna R, Hsu WC, Mao J, Sedrakyan A. Surgeon annual and cumulative volumes predict early postoperative outcomes after brain tumor resection. World Neurosurg. 2018;114:e254–e266. doi: 10.1016/j.wneu.2018.02.172. [DOI] [PubMed] [Google Scholar]
- 6.Stranjalis G, Kalamatianos T, Stavrinou LC, Mathios D, Koutsarnakis C, Tzavara C, et al. The Evangelismos hospital central nervous system tumor registry: Analysis of 1414 cases (1998-2009) Surg Neurol Int. 2013;4:23. doi: 10.4103/2152-7806.107893. [DOI] [PMC free article] [PubMed] [Google Scholar]